The coronavirus disease-19 (COVID-19) pandemic has emerged as an unprecedented international humanitarian crisis. Several recent publications and multi-society guidelines have focused on the clinical manifestations of this disease and best practices in gastroenterology and endoscopy during this pandemic.1, 2, 3, 4, 5, 6, 7, 8, 9
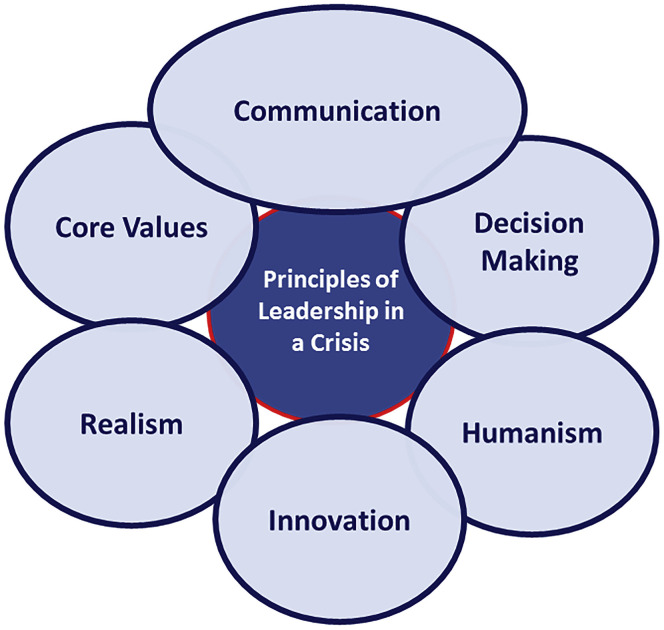
In times like these, there is volatility, uncertainty, complexity, and ambiguity that need rapid, high-impact decisions in a limited information setting. Leaders have to manage these elements, learn new lessons along the way, and help to develop various creative problem-solving strategies to keep their enterprise operational and our patients safe and well cared for. We have selected and summarized several characteristics and practices that effective leaders embody during a time of crisis and discussed them in the context of the COVID-19 pandemic (Figure 1 ).10 , 11
Figure 1.
Core principles of effective crisis leadership.
Core Leadership Principles during a Crisis
Communication
The macro forces that are driving the spread of the pandemic as well as the statistics and predictive models about the incidence and fatality are well-publicized through mass media and social networks. It may not seem likely that the quantity or quality of communications coming from a local leader would make a difference, but it does. Uncertainty produces anxiety throughout the workforce and the leader’s silence will be interpreted as bad “local” news. It is essential to communicate to define reality and reinforce a clear perspective on what is happening and what it means for the unit that you are leading, the organization, and the region. Communication needs to be clear and consistent, but also adaptive.
Realistic View of the Current State with Optimism for the Future
Great leaders communicate credible hope that the group has the resources needed to meet the threats it faces each day, both material (eg, personal protective equipment [PPE], wellness resources, ability to work remotely) as well as psychological (eg, determination, solidarity, shared purpose). These leaders also communicate the gravity of the challenge transparently and are humble enough to admit that they do not have all the answers. Doing so bolsters their credibility, allowing them to share an optimistic vision that is both reassuring and realistic.
Focus on Mission and Core Values
A crisis is an opportune time to rediscover one’s core values. Our profession and organizations’ mission and core values are put to the test in turbulent times and effective leaders take this opportunity to reemphasize these values to motivate and galvanize those around them. It is also important to recognize and applaud champions such as volunteers, frontline clinical workers in the intensive care unit, emergency responders and others who are caring for COVID-19 patients to set a visible example as those who are reinforcing the culture and values of putting our patients first.
Decision Making in the Setting of Ambiguity
Successful leaders cut through the clutter of conflicting data and opinions, identify the areas that need attention, and allocate effort and resources accordingly. They quickly develop and communicate a point of view on the best path forward, providing a sense of direction. Effective leaders during a crisis are also flexible in changing course, adopting novel, more promising ideas, while abandoning dogma or prior diktat.
A good leader understands that no decision or a delayed decision may lead to a worse outcome. In the case of pandemics, chasing the events is an indicator of losing ground. As we now know, delays of even a few days made a considerable difference in the spread of COVID-19. Because high-quality data are scarce or hard to come by early on, decisions may have to be taken based on prior or best available knowledge, experience, intuition, consensus and common sense. Several opportunities to mitigate harm are missed in the initial stages of a crisis (eg, use of face coverings, canceling travel, screening employees and patients) as we tend to rely on traditional models of data and evidence-based decision making. However, as new information becomes available, a leader has to be flexible to change prior decisions or adopt alternate pathways. A successful leadership team encourages “outside the box” thinking to deal with catastrophic events. As the crisis evolves, the successful leader makes nimble and decisive moves and subscribes to a strategy that is iterative. An example in the COVID-19 setting is allocation and use of PPE where recommendations change rapidly based on PPE availability, disease prevalence, and emerging knowledge of viral transmission.
Plan for the Long and Short Term
Successful leaders have the ability to devote the appropriate short-term resources to urgent needs while maintaining a focus on long-term strategic goals. They do not hesitate to make the hard choices (eg, work from home, social distancing, hiring freeze, canceling elective procedures and in-person meetings, or even total lockdown) to address short-term priorities. They also demonstrate the courage and foresight to preserve investments that are essential to the long-term health of the organization. In the face of uncertainty, some leaders are guided primarily by concerns over the “optics” of their decisions; strong leaders are guided by a view of the sacrifices required to preserve strategic direction.
Engage with Purpose and Humility
Great leaders engage purposefully with those around them to harness the energy of the broader workforce. This engagement creates a sense of togetherness by having the humility to listen to a wide range of opinions and focus on asking questions. It also connects with colleagues and shows that you genuinely care about them and their welfare. With the stress of crisis, it is easy to assign blame, find fault, and criticize. Purposeful engagement enables leaders to steer the process in the chosen path through the power of respectful dialogue emphasizing connection over correction. A crisis is not the time to dwell on mistakes, but rather to instill confidence in the team members through empathy, support, and reassurance.
Flattening the Leadership Structure
The organization needs many leaders in times of rapid and unpredictable change. During a crisis, senior executives have a natural tendency to assert control, stripping away leadership responsibility from their direct reports in an effort to reduce risk and increase efficiency. As a result, others become operators and executors, not leaders and decision makers. The resultant weakening of the team's leadership skills may echo through the ranks for years afterward. Strong leaders who enable others to leads are catalysts for widespread change. This is referred to as “horizontal” or “agile leadership.
Look Outward
The best leaders actively resist the instinct of withdrawing inward. They look outward to colleagues, employees, suppliers, and customers and other organizations for gathering the insight required to enable better decision making. For example, in February 2020, leaders of the Texas-based grocery chain HEB contacted leaders of similar retailers in China (and with their supply chain providers around the world) to understand the effects of the lockdown to ensure effective operations.12 Similarly, leaders in GI have been in constant communication through different national platforms (eg, AGA GI Chief’s Consortium), sharing knowledge and experience with each other.
Managing the Tripartite Mission in the Setting of a Crisis
Clinical Enterprise Management
Early assessment of the overall impact of a crisis such as COVID-19 on clinical practice is an essential and complex exercise. The initial decisions revolve around determination of clinical urgency and understanding true capacity. Although multisociety guidelines have been proposed on this topic, triaging the timing of patient care (urgent, semiurgent, elective) is a difficult exercise with potentially significant clinical, ethical, and medicolegal as well as financial implications.13 These decisions need to incorporate the nuances of subspecialty GI practices and are best taken with the input of the provider teams and institutional leadership.
On the operations front, the capacity depends on staffing levels, PPE, COVID-19 testing, degree of redeployment of providers and staff to other clinical areas, and the availability of consumable supplies and inventory. It is advisable to put together an operations team that addresses these issues in real time and moves nimbly to address problems that arise both in the hospital, clinic, and endoscopy unit.
The considerable negative financial impact is felt throughout the system. Division administrators (and practice managers) and chiefs/chairs (and managing partners in private practice) need to grapple with this reality and work in partnership with senior leadership at the institutional level, factoring in revised revenue projections and strategies to mitigate the losses. It is in this arena that effective communication, addressing staff and provider anxiety, and maintaining transparency are essential tools to help keep the team together and focused on their main missions. The strategies vary by place and time and include redeployment (eg, hospitalists, employee health), change in delivery (eg, telehealth), and transparent equitable reductions in compensations as a last resort.
Educational Enterprise Management
Training and education, which are critical missions for academic programs, have been disrupted during the COVID-19 crisis. Core program leadership has to define priorities for teaching and education that need to be fulfilled and implement a strategy to achieve that goal. Fortunately, there are well-established platforms available to deliver remote learning digitally and these must be harnessed to facilitate curricular needs both now and in the future. In addition, key clinical rotations need to be identified and trainees rotated through those in a limited fashion, to maximize trainee safety. Endoscopy simulators might be a good training platform to consider during this time. Such times may represent opportunities for trainees to catch up on research or academic projects or examination preparation. Downtime owing to COVID-19 also represents an opportunity to have deeper discussions on strategy and transformative change going forward with re-imagined educational models to test after the crisis.
Research Enterprise Management
Most institutions have provided regulatory guidance, including a moratorium on non-critical human subjects enrollment, for a specified time period. Communication with research subjects and the importance of PI compliance with crisis mode regulatory guidance needs to be emphasized at all levels. Budget reassessment, reallocation of research staff to other areas of the program and communication with study sponsors are priorities in this realm during a crisis. This relative hiatus represents a good opportunity for the research teams to reassess their portfolio, develop new or revised strategic priorities, and ensure that the regulatory documentation is complete. The hiatus is also an ideal time to reevaluate one’s competitive advantage and value proposition of their personal and departmental research strategies, and develop new focused multidisciplinary groups to pursue new areas of research. It provides an opportunity to leverage COVID-19 relevant work, which will have increased value for at least the midterm future.
Crisis Breeds Opportunity
A disruptive, chaotic event of such magnitude will leave institutions, teams, and individuals with varying levels of trauma. The most important priorities for a leader in the early postcrisis phase include a rapid assessment of the existing landscape at all levels (administrative, clinical, academic, and financial) as well as the humility and wisdom to recognize the lessons learned. How did we do? What did we do well? What did we not handle well? These are critical questions that will guide the rebuilding process and help prepare the team for recovery and resumption and possibly future events. The forward-thinking leader will use this opportunity to incorporate innovative strategies and systems into the rebuilding process, such that the new product is a stronger, more robust and progressive version. The instinct of “returning to normal” may not be the best philosophy. However, crises generate a “burning platform” that is often the opportunity needed to drive transformational change. Indeed COVID-19 may eventually be known as the event that finally tipped medicine and education into the digital care era!
The progressive leader will identify new paradigms and opportunities that present themselves as a result of such a crisis. An example of this is the jumpstart of the telemedicine platform during the COVID crisis. Before COVID, telemedicine was not mainstream in American medicine, despite having been around for more than a decade. However, the rigors of this pandemic have sharply focused the attention of administrators, providers and insurance companies. It is because of telemedicine, that the “work from home” platform may finally be adopted in a meaningful way in our medical field, which may have significant implications for reducing provider burnout while enhancing efficiencies in care delivery.
Based on the best information, data, and trends available, it is important to establish a target date for resumption of operations, in alignment with institutional as well as societal and governmental plans. Decisions will need to be taken regarding a graduated versus more acute ramp up of activities. One example of a postsurge challenge is how to manage the clinical backlog. This will require a formal operational strategy, additional resources, and institutional support. It will require creativity, flexibility, and the ability of the leadership team to develop innovative approaches to problem solving. New schedules may need to be developed, evening and weekend work shifts may have to be contemplated, and providers may have to work from different locations to allow consolidation of activities and economies of scale. An effective leader will champion these novel solutions, and facilitate in the implementation.
A key observation from the COVID-19 crisis is how underprepared we were as a profession and as a country to deal with such a crisis. Building strong relationships with key stakeholders, having a clear understanding of each leader’s role in a future crisis, and developing effective supply chains and other processes are a few examples. These plans need to be at the divisional, departmental, institutional and regional levels. Key questions to ask would be: How do we ensure that we maximally prepare for known threats? What are the tools? What are the systems in place? What is the playbook? The answers will be unique for each individual scenario, but the exercise has to be undertaken proactively and the basic principles will be the same.
Conclusion
Leading during the acute COVID-19 crisis has been a stress test for leaders. This test will hopefully allow GI leaders, teams, and institutions in health care to be better prepared for managing a sustained period of pandemic related disruption that many are now anticipating. It will also stimulate proactive planning for crisis preparedness and a renewed commitment to leadership training in medicine.
Footnotes
Conflicts of interest The authors disclose no conflicts.
References
- 1.Repici A., Maselli R., Colombo M. Coronavirus (COVID-19) outbreak: what the department of endoscopy should know. Gastrointest Endosc. 2020;92:192–197. doi: 10.1016/j.gie.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Soetikno R., Teoh A.Y., Kaltenbach T. Considerations in performing endoscopy during the COVID-19 pandemic. Gastrointest Endosc. 2020;92:176–183. doi: 10.1016/j.gie.2020.03.3758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gross S.A., Robbins D.H., Greenwald D.A. Preparation in the Big Apple: New York City, a new epicenter of the COVID-19 pandemic. Am J Gastroenterol. 2020;115:801–804. doi: 10.14309/ajg.0000000000000636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ang T.L. Gastrointestinal endoscopy during COVID-19 pandemic. J Gastroenterol Hepatol. 2020;35:701–702. doi: 10.1111/jgh.15048. [DOI] [PubMed] [Google Scholar]
- 5.Ungaro R.C., Sullivan T., Colombel J.F. What Should Gastroenterologists and Patients Know About COVID-19? Clin Gastroenterol Hepatol. 2020;18:1409–1411. doi: 10.1016/j.cgh.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gu J., Han B., Wang J. COVID-19: Gastrointestinal manifestations and potential fecal-oral transmission. Gastroenterology. 2020;158:1518–1519. doi: 10.1053/j.gastro.2020.02.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ong J., Young B.E., Ong S. COVID-19 in gastroenterology: a clinical perspective. Gut. 2020;69:1144–1145. doi: 10.1136/gutjnl-2020-321051. [DOI] [PubMed] [Google Scholar]
- 8.Wong S.H., Lui R.N., Sung J.J. Covid-19 and the digestive system. J Gastroenterol Hepatol. 2020;35:744–748. doi: 10.1111/jgh.15047. [DOI] [PubMed] [Google Scholar]
- 9.Sultan S., Lim J.K., Altayar O. AGA rapid recommendations for gastrointestinal procedures during the COVID-19 pandemic. Gastroenterology. 2020;159:739–758. doi: 10.1053/j.gastro.2020.03.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Here are the top five leadership challenges during the coronavirus pandemic. www.forbes.com/sites/niharchhaya/2020/03/23/here-are-the-top-five-leadership-challenges-during-the-coronavirus-pandemic/#77a8f5e75984 Available:
- 11.Leadership through uncertainty. www.russellreynolds.com/insights/thought-leadership/leadership-through-uncertainty Available:
- 12.The HEB story. http://a.msn.com/05/en-us/BB11ZzaZ?ocid=se Available:
- 13.Gastroenterology Professional Society Guidance on Endoscopic Procedures During the COVID-19 Pandemic Joint statement of the AASLD, ACG, AGA and ASGE. Mar, 2020. www.asge.org/home/advanced-education-training/covid-19-asge-updates-for-members/gastroenterology-professional-society-guidance-on-endoscopic-procedures-during-the-covid-19-pandemic Available: