Introduction
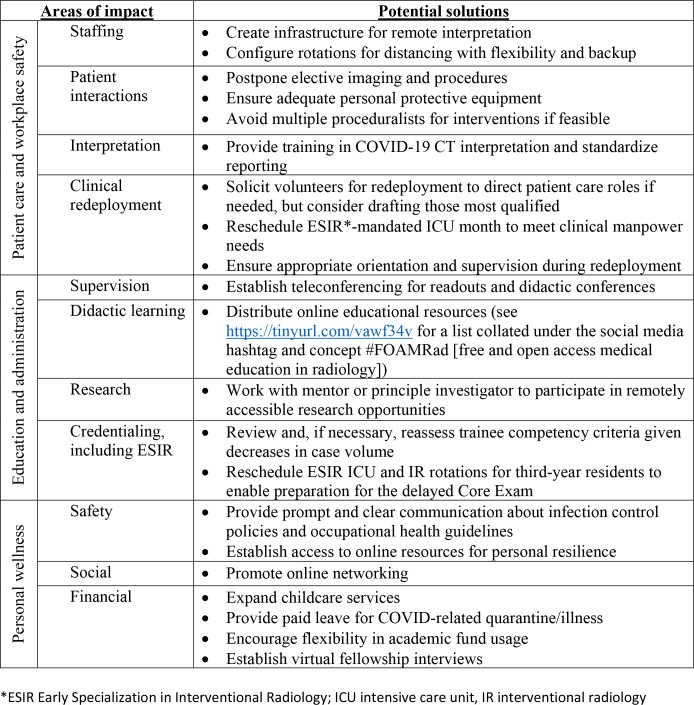
The Coronavirus Disease 2019 (COVID-19) pandemic is evolving rapidly in the United States, widely disrupting personal and professional life, including that of radiology trainees. Reducing the rate at which COVID-19 cases are diagnosed, so-called “flattening the curve,” is a goal both for the public to alleviate strain on the healthcare system, and for healthcare providers to stabilize our workforce. As residents and fellows at multiple institutions throughout the country working in both diagnostic and interventional radiology, the authors of this report provide an overview of major problems that our colleagues and training programs currently face and offer some potential solutions (Figure). We hope this report may serve as a starting point for radiology training programs to proactively assess the impact of the current pandemic on their resident and fellow trainees.
Figure:
Summary of COVID-19 impact on radiology trainees and potential solutions
Patient Care and Workplace Safety
Staffing
Loss of trainees from illness and quarantine has severely strained hospital operations. Infection control requires isolation of symptomatic workers and social distancing to dampen transmission from asymptomatic carriers. Risk mitigation measures include separating workstations by at least 6 feet, curtailing in-person consultations and conferences, and rotating colocalized workers off and on service together to contain contagion within small teams (1). Radiology departments should rapidly deploy technology solutions that allow radiologists to contribute remotely at distant work sites or from home, including examination protocolling, interpretation, and multidisciplinary case discussions. For trainees, these measures may mean decreased need for on-site work and increased scheduling flexibility. For example, some programs have begun instituting a 1-week-on, 1-week-off work schedule in the hope of ensuring an adequate reserve capacity.
Patient Interactions
To protect both patients and medical staff, many radiology departments are postponing elective imaging examinations and interventions while continuing to provide urgent care. Access to personal protective equipment (PPE) and training on proper PPE use are critical to the safety of workers. Given shortages of PPE, faculty and program directors should carefully consider the role of the interventional radiology (IR) trainee in the care of patients with COVID-19. Training programs must balance the risk to trainees versus the educational opportunity to participate in an IR procedure (2).
Interpretation
Chest CT has been discussed as an adjunctive tool in diagnosing COVID-19 and related complications (3). Radiology curricula in training programs should add specific training in image interpretation of COVID-19 on chest CT and chest radiograph, including the use of standardized report templates.
Clinical Redeployment
To manage an influx of patients requiring hospitalization during the peak of the outbreak, radiology residents and fellows may be redeployed from radiology to direct patient care settings, such as internal medicine wards and intensive care units (ICUs). This potential redeployment is an opportunity for radiology trainees to stand in solidarity with our colleagues from other specialties in caring for patients. However, this redeployment to nonradiology settings should be performed on a voluntary basis when possible. Radiology trainees who most recently completed internship positions at the same institution, or those in the Early Specialization in IR (ESIR) pathway, will be best equipped to adapt to return to the wards and ICUs. In order to improve safety for radiology trainees, redeployment plans should feature orientation and training sessions, appropriate supervision, and adherence to duty hour limits.
Education and Administration
Supervision
Social distancing measures have circumvented the traditional trainee-faculty member workstation teaching, which is especially disadvantageous for residents who may be rotating on a service for the first or second time in their training. Teleconferencing and remote readout with screen sharing may help mitigate the loss of these side-by-side readout sessions.
Didactic Learning
In-person teaching conferences, a crucial component of radiology education, have been widely replaced by virtual live or recorded conferences, or canceled altogether (4). To better engage trainees in remote locations, we encourage educators to integrate audience response systems or other instructional methods for active learning (5). If longstanding national lecture courses and meetings (eg, the American Institute for Radiologic Pathology) were to move to online delivery, trainees would have access to state of the art teaching despite diminished conferences at their institution. For example, the American College of Radiology 2020 Annual Meeting has transitioned to a fully virtual platform. There are also various digital learning resources for trainees offered by individual educators, institutions, and professional societies, which provide alternatives to in-person teaching (See Figure, Didactic Learning).
Research
Research has been suspended at many institutions with laboratory closures and IRB mandates to stop in-person participant visits. Many radiology society meetings have been canceled, resulting in decreased collaborative and networking opportunities for trainees. We encourage trainees and their mentors to have discussions regarding other projects able to be worked on during the pandemic, securing grant funding for future studies, and reshaping disrupted works-in-progress into publishable or presentable material so as not to lose value from the work already performed.
Credentialing
The American Board of Radiology (ABR) has postponed the Core Exam until at least September 1, 2020. At minimum, this change will alter trainee clinical scheduling, including call shifts, for not only the residents entering their 4th year, but the entire residency. Delayed graduation and credentialing would impact start time for fellows and for incoming radiology residents in the 2020–2021 academic year.
With the decrease in imaging procedures, senior residents may find increased difficulty in meeting the training requirements of the Mammography Quality Standards Act (MQSA) or the Nuclear Regulatory Commission (NRC). Notably, the Accreditation Council for Graduate Medical Education (ACGME) case requirements have been established for program accreditation and not individual graduate competency. Program directors should work closely with their local clinical competency committee on this issue (6). The ABR will also need to clarify what impact lost workdays from self-quarantine will have on board eligibility.
Early Specialization in IR (ESIR)
The delay in the ABR Core Exam poses unique challenges for ESIR postgraduate year 4 (PGY-4) residents. Trainees may find it difficult to meet IR rotation requirements and the other mandated clinical rotations, such as vascular surgery and ICU, while preparing for the delayed Core Exam. One possible solution is to move the time-intensive ICU month to the upcoming months. ESIR PGY-5 residents may also have difficulties meeting the ESIR requirements as the case volume in many IR departments has decreased substantially. We encourage residents to have discussion with their program leadership to find a solution to meet the case requirements while taking into account the need to conserve PPE and minimize exposure risk.
Personal Wellness
Safety
The COVID-19 pandemic is likely to cause psychologic distress to radiology trainees as well as other healthcare providers. Trainees are concerned that they may contract the illness and expose their potentially more vulnerable family members at home. These fears are exacerbated by the nationwide PPE shortages (7). Trainee wellness is closely associated with the clarity, adequacy, and reliability of relevant information (8). Prompt continuous channels of communication should be available to address concerns of the medical staff, including the trainees, including recommendations on PPE usage, viral testing, self-quarantine, and return to work after illness. Guidelines for backup coverage in personal or family emergencies should be in place. Finally, leaders should acknowledge the additional demands that the pandemic is creating on their trainees and advocate for resources to reinforce personal resilience (eg, online meditation, psychotherapy, exercise) for trainees as well as the medical staff.
Social Relationships
Social distancing is an effective strategy to contain virus spread but does not have to result in social isolation. In fact, it is more important now than ever for trainees to remain connected via online portals and exchange ideas with each other through social media (eg, Twitter with hashtags such as #RadRes) and radiology society public forums (eg, American College of Radiology Engage [engage.acr.org]). Time away from work for personal relationships have now become especially important and trainees should interact with family and friends in ways compliant with social distancing.
Financial Future
Trainees, many with medical school debt and limited earnings and savings, are especially vulnerable to the economic consequences of this pandemic. Radiology departments and practices are scaling down elective imaging and procedures, resulting in lost revenue that is unlikely to be fully recovered. Should this pandemic-induced recession be prolonged, many will lose their health insurance, decreasing the number of patients seeking radiology services. With losses in savings, senior radiologists may delay retirement (9). Given this outlook, trainees are concerned about the security of existing job offers and the likelihood of future job openings.
While the long-term outcomes are uncertain, institutions can take steps to support trainees in their short-term financial concerns. Perhaps the most immediate is childcare. Widespread school closures have affected all healthcare providers, trainees among them, which institutions could address by expanding childcare services, potentially with volunteering from nonessential employees (4). Paid leave for COVID-19 exposure related quarantine and sickness as well as more flexibility in work hours would relieve uncertainty. Measures to maintain moonlighting opportunities and more discretionary use of academic funds would help. Given travel restrictions, many fellowship programs are planning for virtual interviews, which will hopefully decrease applicant expenses and prevent further delays in training.
Final Thoughts
The impact of COVID-19 on radiology training programs has been profound and continues to increase as case counts rise. While pandemics are, by their nature, self-limited, no clear end date is in sight for this one. It is important for all radiology trainees to stay informed and compliant with measures to contain COVID-19 without complacency or panic. We can work together to create sustainable solutions to ensure safety, promote education, and encourage wellbeing.
Footnotes
IRB approval was not required for this manuscript.
No funding or conflicts of interest are pertinent to this study.
M.D.A .and E.G. contributed equally to this article.
References
- 1.Mossa-Basha M, Meltzer CC, Kim DC, Tuite MJ, Kolli KP, Tan BS. Radiology Department Preparedness for COVID-19: Radiology Scientific Expert Panel. Radiology. 2020:200988 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pepe D, Martinello RA, Juthani-Mehta M. Involving Physicians-in-Training in the Care of Patients During Epidemics. J Grad Med Educ. 2019;11(6):632-634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kanne JP, Little BP, Chung JH, Elicker BM, Ketai LH. Essentials for Radiologists on COVID-19: An Update-Radiology Scientific Expert Panel. Radiology. 2020:200527 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gupta Y. Residents Remaining Flexible During COVID-19 Pandemic. 2020; https://www.theabr.org/blogs/residents-remaining-flexible-during-covid-19-pandemic. Accessed March 24, 2020. [Google Scholar]
- 5.Lim EC, Oh VM, Koh DR, Seet RC. The challenges of "continuing medical education" in a pandemic era. Ann Acad Med Singapore. 2009;38(8):724-726. [PubMed] [Google Scholar]
- 6.Nasca T. ACGME Response to the Coronavirus (COVID-19) [press release]. March 18, 2020. https://acgme.org/Newsroom/Newsroom-Details/ArticleID/10111/ACGME-Response-to-the-Coronavirus-COVID-19 . Accessed March 24, 2020.
- 7.American Medical Association. Caring for our caregivers during COVID-19. https://www.ama-assn.org/delivering-care/public-health/caring-our-caregivers-during-covid-19. Accessed March 24, 2020. [Google Scholar]
- 8.Goulia P, Mantas C, Dimitroula D, Mantis D, Hyphantis T. General hospital staff worries, perceived sufficiency of information and associated psychological distress during the A/H1N1 influenza pandemic. BMC Infect Dis. 2010;10:322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cronan JJ, Coleman BG, Harolds JA, Bluth EI. Retirement Issues for Radiologists and the Radiology Practice, Part 1: A Report of the ACR Commission on Human Resources, Subcommittee on Retirement. J Am Coll Radiol. 2013;10(2):101–7. [DOI] [PubMed] [Google Scholar]