Abstract
Background/Objectives:
Little is known about the relationship between loneliness and end of life experience, including (1) symptom burden, (2) intensity of care, (3) and advance care planning among older adults.
Design:
Secondary analysis of the Health and Retirement Study (HRS)
Setting:
Population-based
Participants:
Decedents over age 50 who died between 2004 and 2014 (n=8700). Exclusions included those who (a) were ineligible for surveys assessing loneliness (n=2932) or (b) had missing or incomplete loneliness or symptom data (n=2872).
Measurements:
Individuals were characterized as lonely based on responses to the 3-item Revised University of California Los Angeles Loneliness Scale in the most recent HRS survey prior to death. Outcomes included proxy-reports of total end of life symptom burden, intensity of end of life care (e.g., late hospice enrollment, place of death, hospitalizations, use of life support) and advance care planning. Results were expressed as adjusted odds ratios (aOR) with 95% confidence intervals (CI).
Results:
One-third of 2896 decedents (n=942) were lonely. After adjusting for demographics, socioeconomic status, multimorbidity, depressive symptoms, family and friends, and social support, loneliness was independently associated with increased total symptom burden at end of life (ß=0.13; p=0.004). Compared to non-lonely individuals, lonely decedents were more likely to use life support in the last 2 years of life (35.5% vs 29.4%; aOR=1.36; 95% CI, 1.08-1.71), and more likely to die in a nursing home (18.4% vs 14.2%; aOR=1.78; 95% CI, 1.30-2.42). No significant differences in other measures of intense care (late hospice enrollment, number of hospitalizations, or dialysis use) or likelihood of advance care planning were observed.
Conclusion:
Lonely older people may be burdened by more symptoms and be exposed to more intense end of life care compared to non-lonely people. Interventions aiming to screen for, prevent, and mitigate loneliness during the vulnerable end of life period are necessary.
Keywords: end of life, loneliness, aggressive care, advance care planning, symptoms
Introduction
Loneliness – the subjective feeling of isolation, lack of belonging, or lack of companionship1 – afflicts approximately 40% of older adults2,3 and is associated with poor health outcomes, including depression,4 accelerated functional2 and cognitive decline,5 and early mortality.1,6 As such, loneliness and social isolation – an objective measure of social networks and connection – are deemed important social determinants of health worthy of routine screening by the National Academies and the Centers for Medicare & Medicaid Services.7,8 Poor health outcomes related to loneliness are frequently linked with poor quality of life in older adults9 and may also be associated with suffering at end of life (EOL). Role transitions, shrinking social networks, and mounting multimorbidity are common at EOL and can increase both the risk of loneliness and its downstream health consequences.10
Important markers of EOL experience and care quality include symptom burden, exposure to aggressive or intense EOL care and presence of advance care planning.11 Yet, little is known about how loneliness affects these markers. What is known is that older adults are prone to high symptom burden and experience a peak in symptom burden in the months preceding death,12 and more experience burdensome symptoms at EOL than ever before.12-15 It is plausible that the increased disease burden experienced by lonely older adults may contribute to higher symptom burden at EOL, but studies assessing this relationship are lacking. Similarly, older adults are frequently exposed to intense or aggressive EOL care despite evidence that it can cause suffering for patients and families.16,17 Whether this construct holds true for lonely adults, and how it relates to use of invasive interventions such as life support, hemodialysis, hospitalizations, and use of hospice, remains unclear. Furthermore, given that loneliness affects an individuals’ ability to connect with others,18 it may potentially affect their ability to participate in advance care planning. Understanding the relationship between loneliness and markers of EOL experience is important given that loneliness may be modifiable.1 Mitigating EOL loneliness may help improve EOL experience in this vulnerable population.
Therefore, using a cohort of older decedents from 2004-2014 in the Health and Retirement Study (HRS), we examined the impact of subjective loneliness on EOL experience as measured by symptom burden, intensity of care, and advance care planning at EOL. We hypothesized that loneliness would be an independent predictor of increased symptom burden, increased exposure to intense EOL care and decreased use of advance care planning.
Methods
Data Source and Study Participants
The HRS is a nationally representative, longitudinal survey of adults 51 years of age and older that is conducted every 2 years19 and has a similar sample mortality rate as the age-matched US population.20 Using publicly available data from the HRS, we examined participants who died between 2004 to 2014. After an HRS participant dies, proxy informants (often a spouse/partner or other family member) familiar with the decedent’s health, finances, and social interactions complete an exit interview that includes information about the participant’s EOL experience (including symptoms, advance care planning, and healthcare utilization and exposure to intense EOL care measures).
Approximately half of HRS participants are eligible for a Psychosocial and Lifestyle Questionnaire containing a 3-item loneliness scale during alternating waves (every 4 years).21 We selected 2004 as the initial starting point for the sample since it was the first year in which the Psychosocial and Lifestyle Questionnaire was administered.
Of the 8700 decedents in HRS from 2004 to 2014, 2896 decedents met all inclusion criteria and were included in our final sample. Others were excluded due to lack of exit interviews (n=961); lack of loneliness data due to Psychosocial and Lifestyle Questionnaire ineligibility (n=2932), nonresponse (n=1555), or partial response (n=187); or incomplete EOL symptom data (n=169) (Figure 1). The HRS complies with the requirements of the University of Michigan’s Institutional Review Board (IRB).
Figure 1:
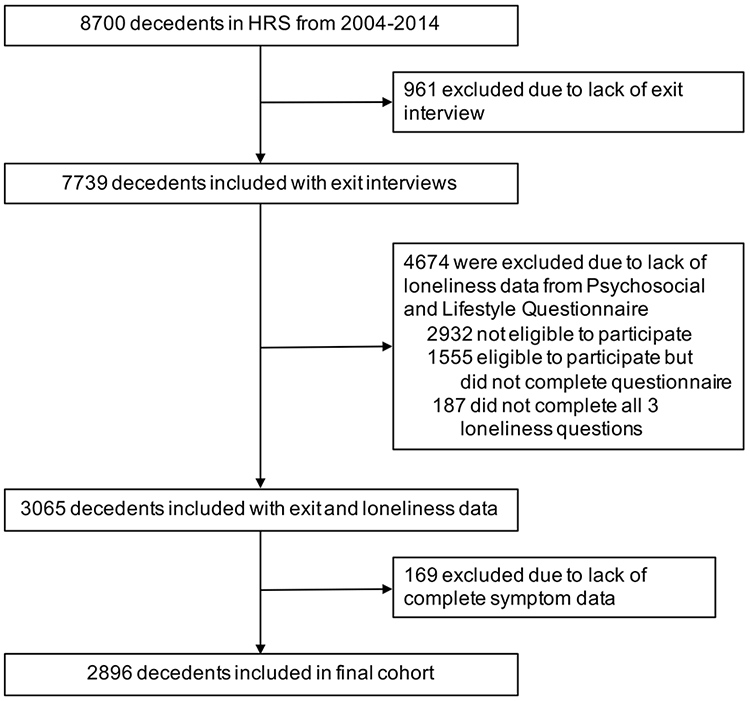
Construction of the HRS decedent cohort from 2004-2014
Variables
1. Predictor Variable: Loneliness
We used the most recent loneliness data from the Psychosocial and Lifestyle Questionnaire before death to approximate loneliness status close to death. Consistent with prior studies2,22 and recommendations from the HRS,21 we constructed a dichotomous loneliness measure using the validated 3-item Revised UCLA Loneliness Scale (R-UCLA).23 The 3 items include whether the participant (a) feels left out, (b) feels isolated, and/or (c) lacks companionship (Cronbach’s alpha = 0.81). The participant is asked to rate each as “Often,” “Some of the time,” or “Hardly ever or never.” The responses were reverse coded on a 1 to 3 scale, and an average score was calculated for all 3 components.21 We classified individuals with an average score of 1.9 or less as “non-lonely” and those with an average score of 2.0 or more as “lonely,” which corresponded to previously established cut points for the dichotomous loneliness variable.2,22
2. Primary Outcome: Total Symptom Burden
HRS proxies report the presence or absence of specific symptoms for one or more months during the last year of the decedent’s life, including pain, difficulty breathing, severe fatigue, very little appetite, frequent vomiting, difficulty controlling limbs, periodic confusion, and difficulty awakening. Because the HRS does not contain “gold standard” symptom scales (due to their length and time-intensive nature), 24 we created a composite scale for total symptom burden in the last year of life. We used a composite scale since symptoms are often experienced in aggregate, with each symptom contributing variably to suffering.25 We used principle-component factor analysis to construct the composite scale26 using an Eigenvalue threshold of greater than 1.0 and factor loading of greater than 0.3. All symptoms were included in the final factor, which used predictive regression models to assign weights to each individual symptom (Cronbach’s alpha = 0.65).
2. Secondary Outcomes:
Secondary outcomes were assessed individually and included:
Intensity of EOL care: We used outcome variables traditionally associated with low-value, intense EOL care27,28 including: proportion spending 3 or fewer days in hospice (late hospice referral); place of death; use of intensive care units (ICUs), hospitals, and nursing homes; and use of life-support and dialysis in the last 2 years of life.
Advance care planning: Markers of advance care planning included whether the decedent had: (1) discussed EOL care preferences with next of kin; (2) assigned a durable power of attorney (DPOA); (3) written EOL instructions; or (4) participated in EOL decisions prior to death.28
4. Covariates:
We used the most recent HRS survey prior to death corresponding with the wave in which the loneliness questions were administered. We included covariates known to influence loneliness and/or our outcomes of interest1 in multivariable models, including:
Demographic and socioeconomic measures (age at death, gender, ethnicity, education, income, and employment status);
Multimorbidity (i.e., multiple chronic conditions), via a validated multimorbidity-weighted index (MWI) computed from participant self-report of 15 physician-diagnosed conditions.29,30 Since the MWI is strongly associated with current and future physical functioning, activities of daily living (ADLs), instrumental activities of daily living (IADLs), and cognitive decline,29,27 these variables were omitted to prevent multicollinearity;
Depressive symptoms, determined using the Center for Epidemiological Studies Depression Scale (CESD) self-report of symptoms:31 the HRS uses an 8-item version of the CESD which includes a question about whether the individual feels lonely. Given concerns for confounding with our predictor variable, this loneliness question was removed from the CESD for our analysis and depressive symptoms were reported on a scale of 0 to 7 based on responses to the remaining CESD questions (Cronbach’s alpha = 0.75);
Family and friends (partner status, having children, having children living within 10 miles, having friends, and having any other immediate family),32 and social support (reliance on their spouse, children, or friends for serious problems).32
Statistical Analysis
We used population survey weights33 to account for the complex survey design of the HRS for all of our analyses, including imputation models. We first summarized characteristics for participants who were “lonely” and “non-lonely,” estimating differences using chi-square tests for categorical variables and t-tests for continuous variables. A two-tailed p-value of <0.05 was considered statistically significant. Next, we assessed the relationship between loneliness and individual symptoms using bivariate logistic regression. We then used both bivariate and multivariable regressions with ordinary least squares (OLS) models to assess the relationship of loneliness to total symptom burden at EOL, adjusting for covariates. Our initial model adjusted for baseline covariates, including demographic characteristics, socioeconomic status, and multimorbidity (Model 1). We then added the following covariates to the baseline model sequentially to assess various confounders: depressive symptoms (Model 2); family and friends (Model 3) and social support (Model 4). Some measures of family, friends, and social support were excluded because their baseline relationship with loneliness was not significant (Table 1). In the final model (Model 5), we adjusted for all covariates in Models 1-4 (Supplementary Table 1).
Table 1:
Characteristics of lonely and non-lonely decedents from 2004-2014 (n=2986)a
| Characteristic | Lonely (n= 942) n (%) |
Non-lonely (n=1954) n (%) |
P-value |
|---|---|---|---|
| Demographic | |||
| Age at death, mean (SE), years | 77.3 (0.5) | 78.5 (0.4) | 0.03 |
| Age at death categoryb | |||
| <60 years | 88 (9.3) | 110 (5.6) | 0.05 |
| 60-65 y | 96 (10.2) | 178 (9.1) | |
| 66-75 y | 201 (21.3) | 446 (22.8) | |
| 76-85 y | 291 (30.9) | 614 (31.4) | |
| >85 y | 266 (28.3) | 606 (31.0) | |
| Female | 533 (56.6) | 914 (46.8) | 0.002 |
| Raceb | |||
| White | 819 (87.0) | 1729 (88.5) | 0.24 |
| Black | 97 (10.3) | 158 (8.1) | |
| Other | 26 (2.8) | 67 (3.5) | |
| Ethnicity | |||
| Hispanic | 58 (6.2) | 100 (5.1) | 0.18 |
| Foreign born (n=2894) | 68 (7.2) | 102 (5.2) | 0.11 |
| Socioeconomic Measures | |||
| <High school education | 266 (28.2) | 502 (25.7) | 0.22 |
| In labor force | 96. (10.2) | 293 (15.0) | 0.01 |
| Total wealth, median, $ | 75,000 | 158,000 | 0.009 |
| Income, median. $ | 20,600 | 29,749 | 0.001 |
| Family and Friends Measures | |||
| Partnered (n=2895) | 386 (41.0) | 2117 (59.8) | <0.001 |
| Have children (n=2741) | 779 (87.4) | 1542 (90.0) | 0.14 |
| Children live within 10 miles (n=2554) | 486 (58.6) | 864 (54.1) | 0.08 |
| Have friends (n=2791) | 765 (84.3) | 1624 (93.1) | <0.001 |
| Have other immediate family (n=2812) | 914 (88.5) | 1585 (90.2) | 0.35 |
| Social Support Measures | |||
| Rely on spouse for serious problem (n=2780) | 352 (39.0) | 1033 (59.5) | <0.001 |
| Rely on children for serious problem (n=2823) | 648 (70.6) | 1456 (82.5) | <0.001 |
| Rely on friends for serious problem (n=2578) | 466 (55.6) | 1189 (73.8) | <0.001 |
| Comorbid Conditions | |||
| Multimorbidity-weighted index, mean (SE) (n=2889) | 8.6 (0.2) | 7.8 (0.1) | 0.01 |
| Depressive symptoms, mean (SE) (n=2747) | 2.7 (0.0) | 1.3 (0.1) | <0.001 |
| Proxy Status | |||
| Decedent had proxy-report during last HRS wave while alive | 48 (5.1) | 76 (3.9) | 0.14 |
SE: Standard error; HRS: Health and Retirement Study
n=2896 for each characteristic unless otherwise defined.
Percentages do not add to 100-percent due to rounding.
Using the final adjusted model, we also examined the relationship of loneliness to intense EOL care and advance care planning. We used multivariable logistic regression for dichotomized outcomes and negative binomial regression for count measures.
Missing Data
Approximately 10% of covariates in our baseline sample had missing data. Four covariates (depressive symptoms, relying on spouse, having friends, and relying on children) accounted for roughly 9% of missing data. Missing covariates were imputed using chained equations with 10 iterations.34
We conducted analyses with Stata 15.1 IC (StataCorp, College Station, Texas). All analyses were performed by NA and HC (Supplement).
Evaluation for multicollinearity
The variance inflation factor (VIF) was calculated for the covariates in our final adjusted imputed model. Multicollinearity was mild based on a maximum VIF of 1.45 for all covariates.
Additional Analyses
To assess for selection bias, we evaluated the relationship between loneliness and the likelihood of having an exit interview in our baseline decedent cohort. Lonely decedents had similar odds of having an exit interview (OR 0.93, p=0.53).
To account for possible variance in loneliness over time, we introduced a time-varying covariate representing the duration of time between completion of the loneliness scale and death. Similarly, to assess for recall bias, we introduced another time-varying covariate representing the duration of time between death and the exit interview. Additionally, HRS participants who were unable (due to physical or cognitive deficits) to provide self-report during the main survey may have had proxy reports of covariates, which may be less reliable than self-report. Hence, we included a covariate related to proxy status in the most recent HRS survey prior to death. Point estimates adjusting for each of these covariates were similar for symptoms and measures of intense care. Thus, these duration covariates and proxy status were excluded from the final regression models.
Finally, to assess the influence of missing data, all multivariable analyses were performed with and without imputed data with no differences in estimates for both (Supplementary Tables S2 and S3).
Results
Participant Characteristics
Our final sample consisted of 2896 decedents (Figure 1). The mean duration of time from completion of the Psychosocial and Lifestyle Questionnaire to death was 2.7 years ± 1.8 years and was not significantly different for lonely versus non-lonely individuals (p=0.72). The mean duration of time from death to exit interview completion was 1.0 years ± 0.7 years, and was not different for lonely versus non-lonely individuals (p=0.78).
Decedent characteristics in the 2004 to 2014 HRS cohort are summarized in Table 1. Of the 2896 decedents, 942 (34%) were lonely in the final sample. At the time of death, lonely decedents were younger (mean age=77.3 years versus 78.5 years in non-lonely individuals; p=0.03), and more often female (p=0.002). Similarly, they were less likely to be partnered or have friends than those that were non-lonely (p<0.001 for both). Lonely decedents had a significantly higher mean multimorbidity-weighted index score (8.6 versus 7.8; p=0.01), suggesting higher overall disease burden and worse functioning. They were also significantly less likely to rely on their spouse, children, or friends for serious problems (p<0.001 for all outcomes). Lonely decedents were more likely to have more depressive symptoms on average (p<0.001). Finally, lonely individuals had similar proportions of proxy informants while alive (5.1%) compared to non-lonely individuals (3.9%, p=0.14).
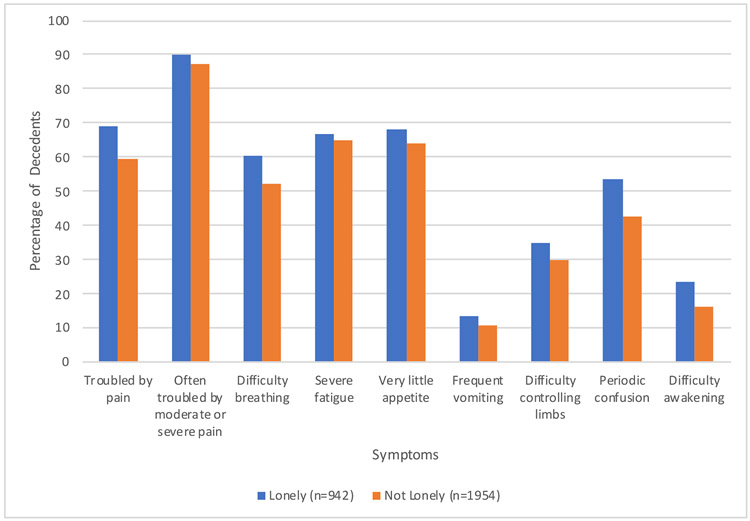
Loneliness and Symptom Burden
We first assessed the relationship between loneliness at EOL and individual symptoms. Compared to non-lonely decedents, a larger proportion of lonely decedents experienced each individual symptom, the most prevalent being pain (69.1% vs 59.5%) (Figure 2). In bivariate analyses, lonely decedents had increased odds of being troubled by pain of any severity (p<0.001), difficulty breathing (p=0.001), severe fatigue (p=0.02), difficulty controlling limbs (p=0.01), periodic confusion (p<0.001), and difficulty awakening (p<0.001) (Figure 3).
Figure 2:
Proportion of lonely versus non-lonely older adults experiencing individual symptoms in the last year of life (n=2896)
Figure 3:
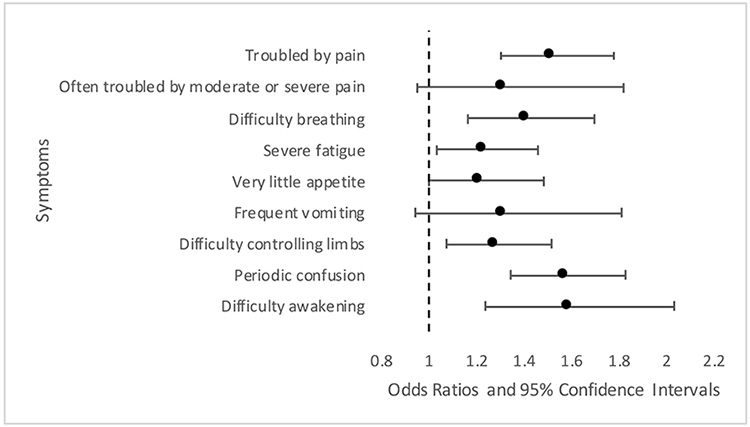
Unadjusted odds of symptoms experienced by lonely versus non-lonely older adults in the last year of life (n=2896)
We next examined the relationship between loneliness and total symptom burden. Loneliness was associated with increased total symptom burden in an unadjusted model (p<0.001) (Supplementary Table S1) and remained significant after adjusting for demographics, socioeconomic status, and multimorbidity (Model 1; p<0.001); depressive symptoms (Model 2; p=0.006); family and friends (Model 3; p<0.001); and social support (Model 4; p<0.001). The fully adjusted model included all covariates in Models 1-4 and remained statistically significant (Model 5, p=0.004), indicating that loneliness was an independent predictor of total symptom burden at EOL.
Loneliness and end of life care and advance care planning
Compared with non-lonely decedents, lonely decedents had greater odds of dying in a nursing home (aOR=1.78; 95% CI, 1.30-2.42; p<0.001) and using life support equipment in the last 2 years of life (aOR=1.36; 95% CI, 1.08-1.71; p=0.01) (Table 2). However, loneliness was not associated with other measures of intense EOL care (like late hospice referral, ICU use, or dialysis use), or measures of advance care planning.
Table 2:
Relationship of loneliness to measures of intense care, healthcare utilization, and advance care planning at end of life
| Outcome | Lonely n (%) |
Non-lonely n (%) |
Unadjusted Odds Ratio (95% CI) |
P-Value | Adjusted Oddsb Ratio (95% CI) |
P-Value |
|---|---|---|---|---|---|---|
| Measures of Intense EOL Care | ||||||
| 3 or less days in hospice (n=2484) | 665 (82.7) | 1297 (83.6) | 0.94 (0.75-1.17) | 0.57 | 0.93 (0.73-1.19) | 0.57 |
| Death location (n=2481) | ||||||
| Home | 242 (30.0) | 557 (35.9) | Ref | Ref | Ref | Ref |
| Hospital | 278 (34.5) | 519 (33.5) | 1.23 (0.99-1.52) | 0.06 | 1.28 (1.01-1.62) | 0.04 |
| Nursing home | 148 (18.4) | 220 (14.2) | 1.56 (1.23-1.96) | <0.001 | 1.78 (1.30-2.42) | <0.001 |
| Spent time in ICU in last 2 years of life (n=904) | 151 (51.5) | 275 (48.7) | 1.12 (0.90-1.39) | 0.32 | 1.09 (0.84-1.39) | 0.52 |
| Used life support equipment in last 2 years of life (n=1949) | 225 (35.5) | 358 (29.4) | 1.32 (1.08-1.62) | 0.01 | 1.36 (1.08-1.71) | 0.01 |
| Dialysis in last 2 years of life (n=1968) | 43 (6.8) | 101 (8.2) | 0.81 (0.52-1.27) | 0.35 | 0.71 (0.43-1.17) | 0.17 |
| Other Healthcare Utilization in Last 2 years of Life | ||||||
| Hospital nights, IRRa (n=1740) | - | - | 1.18 (0.81-1.71) | 0.37 | 0.95 (0.66-1.36) | 0.78 |
| Nursing home nights, IRR (n=365) | - | - | 0.69 (0.38-1.27) | 0.22 | 0.90 (0.50-1.60) | 0.71 |
| Advance Care Planning | ||||||
| Discussed EOL care (n=2460) | 524 (65.6) | 985 (64.1) | 1.07 (0.86-1.33) | 0.54 | 1.08 (0.87-1.35) | 0.46 |
| Assigned durable power of attorney (n=2417) | 521 (66.3) | 971 (64.3) | 1.09 (0.90-1.32) | 0.36 | 1.13 (0.88-1.46) | 0.34 |
| Written EOL care instructions (n=2440) | 404 (51.0) | 828 (54.3) | 0.88 (0.71-1.08) | 0.21 | 0.95 (0.78-1.15) | 0.57 |
| Subject participated in EOL decisions (n=1051) | 121 (35.3) | 260 (39.6) | 0.83 (0.61-1.14) | 0.24 | 0.77 (0.55-1.06) | 0.10 |
IRR: Incidence risk ratio
Adjusted for race, age, gender, education, total income, multimorbidity-weighted index, depressive symptoms, family and friends (partner status, has friends), social support (relies on spouse, relies on children, relies on friends
Discussion
In this study of 2896 older decedents from a large nationally-representative sample, we found that loneliness affected over a third of older adults near EOL. Lonely older adults were more likely to suffer from bothersome symptoms and were more likely to experience higher total symptom burden, even after controlling for confounders. While lonely older adults had similar odds of advance care planning, they were exposed to more intense EOL care compared to non-lonely decedents. High symptom burden and exposure to intense or aggressive EOL care are major drivers of patient suffering and healthcare overuse.11,16 Thus, our findings have important implications for lonely individuals’ well-being, care quality, and healthcare costs at EOL.
Greater exposure to aggressive and painful interventions may be partially responsible for the increased symptom burden lonely individuals experience at EOL.17 We observed that lonely individuals were more likely to receive life support at EOL; however, we did not observe an association between loneliness and other measures of aggressive care and healthcare overuse in the last 2 years of life, including ICU stays. Our findings are consistent with other studies that have shown no difference in hospitalizations22,35 among lonely versus non-lonely older adults. A study by Shaw and colleagues found that lonely individuals have lower Medicare expenditures compared to non-lonely individuals, some of which may be related to lower inpatient expenditures after adjusting for socioeconomic and health status.36 However, this study did not specifically evaluate changes in healthcare expenditures or utilization near death. While it suggests that lonely individuals may be less likely to present for care in the years preceding death, it is possible loneliness may still be associated with more intense EOL care and higher expenditures near death. Additionally, studies suggest that lonely older adults are more likely to experience emergent hospitalizations37 and subsequent rehospitalization.35 Increased acuity may necessitate more intense and costly interventions in emergent situations or near EOL. The broad EOL time period in our study may have prevented discernment of important differences that arise just proximal to death, when use of life-sustaining measures like life support are more common. Future qualitative and ethnographic studies could better characterize these differences.
Additionally, our study found that overall nursing home utilization (as indicated by number of nursing home nights) is similar for lonely and non-lonely individuals, which is supported by others using Medicare claims data.36 However, we also observed that lonely older adults have higher odds of dying in a nursing home, a troubling finding as it may further isolate lonely people from their communities and support systems, and worsen quality of life near death. However, this finding is not surprising given lonely individuals’ propensity towards multimorbidity, cognitive decline, and poor physical functioning earlier in life.2,4-6 These health conditions, along with lower engagement in health-promoting behaviors,38,39 can place lonely individuals at risk for higher symptom burden throughout life, not just near death. Longitudinal studies could shed light on the onset and duration of symptom-related suffering for lonely older adults, informing interventions to improve quality of life in this population.
Our study has limitations. First, we used loneliness data from the most proximal HRS interview prior to death; this data may not have accurately depicted participants’ EOL experience. However, prior studies have assessed loneliness as an exposure variable and found that its health effects can persist over time.2 Additionally, variability in loneliness over time would have biased our results towards the null. Second, use of proxy-reported symptoms and EOL care may introduce recall bias, but have shown moderate to good reliability when describing objectively observable symptoms and EOL care quality.40-42 Third, we lacked data on specific stigma-carrying diagnoses (like human immunodeficiency virus) that could exacerbate loneliness and lead to unmeasured confounding. Fourth, there are challenges with current loneliness measurement tools that frequently treat loneliness as a disease state rather than a complex psychological and social phenomenon. However, the 3-item UCLA Loneliness Scale is widely used and comparable to other national studies of loneliness, making it our best approximation of loneliness. Additionally, using a dichotomous measure for loneliness may have reduced statistical power, limiting ability to discern an effect if one did exist even though other studies have successfully used this approach.2,22 Fifth, while we determined that loneliness did not predict why individuals may have lacked exit interviews (and hence were excluded from our study), over 1,700 decedents in the Health and Retirement Study were excluded for having incomplete or missing loneliness data. Whether these individuals were lonely or socially isolated is unclear. Finally, given the cross-sectional nature of our study, we cannot make conclusions about causality or exclude potential longitudinal interactions between other potential contributors to EOL experience.
Our study also has strengths. First, to our knowledge, this is the first study to explore the association between loneliness, symptom burden, and intensity of care at EOL. Second, we used a large, nationally representative sample, using survey weights. Third, we utilized multivariable models adjusting for multiple potential factors that could contribute to differences in EOL experience. Importantly, we controlled for measures of social support that may have impacted our outcomes of interest. Finally, we incorporated additional sensitivity analyses to assess for variability in loneliness variable over time and potential sources of recall and reporting bias.
Our findings have important implications for clinical practice and policy. Loneliness can have profound effects on symptom burden and quality of life near death. Thus, we must be able to identify at-risk lonely patients43 near EOL as well as throughout the life continuum. Value-based repayment models to incentivize screening for loneliness in routine medical care have been proposed,7,44 and such tools can be particularly important as individuals near EOL, when social networks become scarcer and community engagement wanes.10 Ultimately, after an initial loneliness screen, an important starting point is a candid conversation between patients and their providers to explore whether and how loneliness impacts their experiences, hopes, fears, and future care preferences, particularly near EOL. Some health systems are even forming partnerships with community-based groups targeting socially isolated and vulnerable older adults to further identify and mitigate loneliness among individuals who may have difficulty presenting for care and linking them with providers who can further support them.45
In addition to identifying at-risk lonely individuals near EOL through screening, unique interventions addressing the complex nature of loneliness at EOL are needed. Prior studies have indicated that targeting maladaptive thinking (for example, teaching ways to reframe one’s thinking about social interactions, promoting positive coping, and managing social anxiety) may be the most effective intervention to address loneliness.1,46 Other interventions promoting social support, social access, and social skills training were also effective, but to a lesser degree.1 Given this context, during the EOL period, interventions such as referrals to mental health providers or social workers to perform life review and engage in reflection around role or identify loss as a result of debility or disease. It may also include referral to social services or chaplaincy to help lonely individuals reconnect with loved ones, their faith, or spirituality near EOL. Where these connections are absent, volunteer-based community social support interventions have been helpful.47,48
Conclusions
In conclusion, we found that lonely older adults appear to have more symptom burden at EOL, are more likely to die in a nursing home, and are exposed to more intense EOL care, which may contribute to more suffering near death. Screening for loneliness is thus important, particularly near EOL as disease burden mounts and social connections wane. Interdisciplinary interventions must target the complex psychological, social, existential, and health underpinnings related to loneliness. Future work to design and evaluate effective interventions to address the vulnerable EOL period are necessary.
Supplementary Material
Impact Statement: We certify that this work is novel. Little is known about the end of life experience of older lonely adults, including symptom burden, exposure to intense care measures, and rates of advance care planning, all of which are important indicators of end of life care and quality of life. In this secondary dataset analysis of 2896 decedents in the Health and Retirement Study – a longitudinal, nationally represented survey of older Americans – we observed that loneliness is associated with (1) higher end of life symptom burden, (2) increased odds of using invasive life support, and (3) increased likelihood of dying in a nursing home. This is despite similar odds of advance care planning between lonely and non-lonely decedents. These observations suggest that lonely older adults are subject to worse health-related suffering at end of life. This further validates the need for more research, interventions, and policies aiming to reduce loneliness and its downstream health effects in older adults.
Acknowledgments
Funding/Support: The Health and Retirement Study is sponsored by the National Institute on Aging (U01 AG009740) and is conducted at the Institute for Social Research, University of Michigan. Dr. Abedini is supported by the National Clinician Scholars Program at the Institute for Healthcare Policy and Innovation. Dr. Choi is supported by a grant from the National Institute on Aging (K01AG057820). Dr. Wei is supported by a grant from the National Institute on Aging (K23AG056638). Dr. Langa is supported by grants from the National Institute on Aging (P30 AG053760, P30 AG024824). Dr. Chopra is supported by grants from the Agency for Healthcare Research and Quality (1-R18-HS-025891-01), Department of Veterans Affairs HSR&D (I01 HX001101-01), and Blue Cross/Blue Shield of Michigan.
Sponsor Role: No funder/sponsor had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Meeting Presentation: Presented as a poster at the Society of Hospital Medicine Annual Conference; March 25-27, 2019; National Harbor, Maryland. Presented orally in the Hamolsky Junior Faculty Scientific Presentation Award Competition at the Society of General Internal Medicine Annual Meeting; May 8-11, 2019; Washington, District of Columbia.
Prior Presentations: Society of Hospital Medicine Meeting (National Harbor, MD, March 2019); Hamolsky Junior Faculty Scientific Award Presentation at the Society of General Internal Medicine meeting (Washington, DC, May 2019).
Conflict of Interest: The authors have no disclosures.
References
- 1.Masi CM, Chen HY, Hawkley LC, Cacioppo JT. A meta-analysis of interventions to reduce loneliness. Pers Soc Psychol Rev. 2011;15(3):219–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Perissinotto CM, Stijacic Cenzer I, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med. 2012;172(14):1078–1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilson C, Moulton B. Loneliness among older adults: a national survey of adults 45+. In. AARP. Washington, DC: Knowledge Networks and Insight Policy Research; 2010. [Google Scholar]
- 4.Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol Aging. 2010;25(2):453–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cacioppo JT, Hawkley LC. Perceived social isolation and cognition. Trends Cogn Sci. 2009;13(10):447–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rico-Uribe LA, Caballero FF, Martín-María N, Cabello M, Ayuso-Mateos JL, Miret M. Association of loneliness with all-cause mortality: A meta-analysis. PLoS One. 2018;13(1):e0190033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Academies of Sciences, Engineering, and Sciences. The Health and Medical Dimensions of Social Isolation and Loneliness in Older Adults. https://www8.nationalacademies.org/pa/projectview.aspx?key=51322. Published 2019. Accessed January 12, 2019.
- 8.Centers for Medicare and Medicaid Services. The Accountable Health Communities Health-Related Social Needs Screening Tool. Published 2019. Accessed January 12, 2019.
- 9.Baernholdt M, Hinton I, Yan G, Rose K, Mattos M. Factors associated with quality of life in older adults in the United States. Qual Life Res. 2012;21(3):527–534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gott M, Wiles J, Moeke-Maxwell T, et al. What is the role of community at the end of life for people dying in advanced age? A qualitative study with bereaved family carers. Palliat Med. 2018;32(1):268–275. [DOI] [PubMed] [Google Scholar]
- 11.Lorenz KA, Rosenfeld K, Wenger N. Quality indicators for palliative and end-of-life care in vulnerable elders. J Am Geriatr Soc. 2007;55 Suppl 2:S318–326. [DOI] [PubMed] [Google Scholar]
- 12.Smith AK, Cenzer IS, Knight SJ, et al. The epidemiology of pain during the last 2 years of life. Ann Intern Med. 2010;153(9):563–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singer AE, Meeker D, Teno JM, Lynn J, Lunney JR, Lorenz KA. Symptom trends in the last year of life from 1998 to 2010: a cohort study. Ann Intern Med. 2015;162(3):175–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patel KV, Guralnik JM, Phelan EA, et al. Symptom Burden Among Community-Dwelling Older Adults in the United States. J Am Geriatr Soc. 2019;67(2):223–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hunt LJ, Smith AK. High Symptom Burden in Older Adults: A Clarion Call for Geriatrics and Palliative Care Research and Training. J Am Geriatr Soc. 2019;67(2):208–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Earle CC, Landrum MB, Souza JM, Neville BA, Weeks JC, Ayanian JZ. Aggressiveness of cancer care near the end of life: is it a quality-of-care issue? J Clin Oncol. 2008;26(23):3860–3866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wright AA, Keating NL, Ayanian JZ, et al. Family Perspectives on Aggressive Cancer Care Near the End of Life. JAMA. 2016;315(3):284–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cacioppo JT, Cacioppo S. Loneliness in the modern age: an evolutionary theory of loneliness (ETL). Vol 58: Acacemic Press; 2018. [Google Scholar]
- 19.Health and Retirement Study, public use dataset. In: Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant NIA U01AG009740). Ann Arbor M-, ed. [Google Scholar]
- 20.Weir DR. Validating mortality ascertainment in the Health and Retirement Study. Survey Research Center; https://hrs.isr.umich.edu/sites/default/files/biblio/Weir_mortality_ascertainment.pdf. Published November 3, 2016. Accessed August 12, 2018. [Google Scholar]
- 21.Smith J, Ryan L, Fisher GG, Sonnega A, Weir DR. Psychosocial and Lifestyle Questionnaire 2006-2016. Survey Research Center, Institute for Social Research. https://hrs.isr.umich.edu/sites/default/files/biblio/HRS%202006-2016%20SAQ%20Documentation_07.06.17_0.pdf. Published 2017. Accessed August 12, 2018.
- 22.Gerst-Emerson K, Jayawardhana J. Loneliness as a public health issue: the impact of loneliness on health care utilization among older adults. Am J Public Health. 2015;105(5):1013–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hughes ME, Waite LJ, Hawkley LC, Cacioppo JT. A Short Scale for Measuring Loneliness in Large Surveys: Results From Two Population-Based Studies. Res Aging. 2004;26(6):655–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wallace R, Herzog A. Overview of the Health Measures in the Health and Retirement Study. The Journal of Human Resources. 1995;30(Supplement):S84–S107. [Google Scholar]
- 25.Klinkenberg M, Willems DL, van der Wal G, Deeg DJ. Symptom burden in the last week of life. J Pain Symptom Manage. 2004;27(1):5–13. [DOI] [PubMed] [Google Scholar]
- 26.Basilevsky A Statistical Factor Analysis and Related Methods: Theory and Applications. New York: Wiley; 1994. [Google Scholar]
- 27.Earle CC, Park ER, Lai B, Weeks JC, Ayanian JZ, Block S. Identifying potential indicators of the quality of end-of-life cancer care from administrative data. J Clin Oncol. 2003;21(6):1133–1138. [DOI] [PubMed] [Google Scholar]
- 28.Bischoff KE, Sudore R, Miao Y, Boscardin WJ, Smith AK. Advance care planning and the quality of end-of-life care in older adults. J Am Geriatr Soc. 2013;61(2):209–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wei MY, Kabeto MU, Langa KM, Mukamal KJ. Multimorbidity and Physical and Cognitive Function: Performance of a New Multimorbidity-Weighted Index. J Gerontol A Biol Sci Med Sci. 2018;73(2):225–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wei MY, Mukamal KJ. Multimorbidity, Mortality, and Long-Term Physical Functioning in 3 Prospective Cohorts of Community-Dwelling Adults. Am J Epidemiol. 2018;187(1):103–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wallace R, Herzog A, Ofstedal MB, Steffick D, Fonda S, Langa K. Documentation of Affective Functioning Measures in the Health and Retirement Study. Survey Research Center, University of Michigan. http://hrsonline.isr.umich.edu/sitedocs/userg/dr-005.pdf. Published 2000. Accessed Aug 12, 2018. [Google Scholar]
- 32.Cornwell EY, Waite LJ. Measuring social isolation among older adults using multiple indicators from the NSHAP study. J Gerontol B Psychol Sci Soc Sci. 2009;64 Suppl 1:i38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ofstedal MB, Weir DR, Chen K, Wagner J. Updates to HRS Sample Weights. 2011.
- 34.White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Statistics in Medicine. 2011;30:377–399. [DOI] [PubMed] [Google Scholar]
- 35.Newall N, McArthur J, Menec VH. A longitudinal examination of social participation, loneliness, and use of physician and hospital services. J Aging Health. 2015;27(3):500–518. [DOI] [PubMed] [Google Scholar]
- 36.Shaw JG, Farid M, Noel-Miller C, et al. Social Isolation and Medicare Spending: Among Older Adults, Objective Social Isolation Increases Expenditures while Loneliness Does Not. J Aging Health. 2017;29(7):1119–1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Molloy GJ, McGee HM, O'Neill D, Conroy RM. Loneliness and emergency and planned hospitalizations in a community sample of older adults. J Am Geriatr Soc. 2010;58(8):1538–1541. [DOI] [PubMed] [Google Scholar]
- 38.Schrempft S, Jackowska M, Hamer M, Steptoe A. Associations between social isolation, loneliness, and objective physical activity in older men and women. BMC Public Health. 2019;19(1):74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kobayashi LC, Steptoe A. Social Isolation, Loneliness, and Health Behaviors at Older Ages: Longitudinal Cohort Study. Ann Behav Med. 2018;52(7):582–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kutner JS, Bryant LL, Beaty BL, Fairclough DL. Symptom distress and quality-of-life assessment at the end of life: the role of proxy response. J Pain Symptom Manage. 2006;32(4):300–310. [DOI] [PubMed] [Google Scholar]
- 41.Makaroun LK, Teno JM, Freedman VA, Kasper JD, Gozalo P, Mor V. Late Transitions and Bereaved Family Member Perceptions of Quality of End-of-Life Care. J Am Geriatr Soc. 2018;66(9):1730–1736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McPherson CJ, Wilson KG, Lobchuk MM, Brajtman S. Family caregivers' assessment of symptoms in patients with advanced cancer: concordance with patients and factors affecting accuracy. J Pain Symptom Manage. 2008;35(1):70–82. [DOI] [PubMed] [Google Scholar]
- 43.Murthy V Work and the loneliness epidemic. Harvard Business Review. https://hbr.org/cover-story/2017/09/work-and-the-loneliness-epidemic. Published October 12, 2017. Accessed Nov 11, 2018. [Google Scholar]
- 44.Perissinotto C, Holt-Lunstad J, Periyakoil VS, Covinsky K. A Practical Approach to Assessing and Mitigating Loneliness and Isolation in Older Adults. J Am Geriatr Soc. 2019. [DOI] [PubMed]
- 45.Abedini NC, Solway E, Piette J, Malani P. Cross-Sector Collaborations To Decrease Loneliness And Social Isolation In Older Adults. Health Affairs Blog Web site. https://www.healthaffairs.org/do/10.1377/hblog20190618.629601/full/ Published June 20, 2019. Accessed October 10, 2019. [Google Scholar]
- 46.Cacioppo S, Grippo AJ, London S, Goossens L, Cacioppo JT. Loneliness: clinical import and interventions. Perspect Psychol Sci. 2015;10(2):238–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McLoughlin K, Rhatigan J, McGilloway S, et al. INSPIRE (INvestigating Social and PractIcal suppoRts at the End of life): Pilot randomised trial of a community social and practical support intervention for adults with life-limiting illness. BMC Palliat Care. 2015;14:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dodd S, Hill M, Ockenden N, et al. 'Being with' or 'doing for'? How the role of an end-of-life volunteer befriender can impact patient wellbeing: interviews from a multiple qualitative case study (ELSA). Support Care Cancer. 2018;26(9):3163–3172. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.