Abstract
Background
Over 40 000 patients with COVID-19 have been hospitalised in New York City (NY, USA) as of April 28, 2020. Data on the epidemiology, clinical course, and outcomes of critically ill patients with COVID-19 in this setting are needed.
Methods
This prospective observational cohort study took place at two NewYork-Presbyterian hospitals affiliated with Columbia University Irving Medical Center in northern Manhattan. We prospectively identified adult patients (aged ≥18 years) admitted to both hospitals from March 2 to April 1, 2020, who were diagnosed with laboratory-confirmed COVID-19 and were critically ill with acute hypoxaemic respiratory failure, and collected clinical, biomarker, and treatment data. The primary outcome was the rate of in-hospital death. Secondary outcomes included frequency and duration of invasive mechanical ventilation, frequency of vasopressor use and renal replacement therapy, and time to in-hospital clinical deterioration following admission. The relation between clinical risk factors, biomarkers, and in-hospital mortality was modelled using Cox proportional hazards regression. Follow-up time was right-censored on April 28, 2020 so that each patient had at least 28 days of observation.
Findings
Between March 2 and April 1, 2020, 1150 adults were admitted to both hospitals with laboratory-confirmed COVID-19, of which 257 (22%) were critically ill. The median age of patients was 62 years (IQR 51–72), 171 (67%) were men. 212 (82%) patients had at least one chronic illness, the most common of which were hypertension (162 [63%]) and diabetes (92 [36%]). 119 (46%) patients had obesity. As of April 28, 2020, 101 (39%) patients had died and 94 (37%) remained hospitalised. 203 (79%) patients received invasive mechanical ventilation for a median of 18 days (IQR 9–28), 170 (66%) of 257 patients received vasopressors and 79 (31%) received renal replacement therapy. The median time to in-hospital deterioration was 3 days (IQR 1–6). In the multivariable Cox model, older age (adjusted hazard ratio [aHR] 1·31 [1·09–1·57] per 10-year increase), chronic cardiac disease (aHR 1·76 [1·08–2·86]), chronic pulmonary disease (aHR 2·94 [1·48–5·84]), higher concentrations of interleukin-6 (aHR 1·11 [95%CI 1·02–1·20] per decile increase), and higher concentrations of D-dimer (aHR 1·10 [1·01–1·19] per decile increase) were independently associated with in-hospital mortality.
Interpretation
Critical illness among patients hospitalised with COVID-19 in New York City is common and associated with a high frequency of invasive mechanical ventilation, extrapulmonary organ dysfunction, and substantial in-hospital mortality.
Funding
National Institute of Allergy and Infectious Diseases and the National Center for Advancing Translational Sciences, National Institutes of Health, and the Columbia University Irving Institute for Clinical and Translational Research.
Introduction
As of April 28, 2020, nearly 1 million laboratory-confirmed cases of COVID-19 associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection have been reported in the USA.1 Of these, over 295 000 were reported in New York State.2 In New York City, over 160 000 cases were reported, of which approximately 40 000 (25%) had been admitted to hospital.2
Available data suggest that 5–20% of patients with COVID-19 develop critical illness that is characterised primarily by acute respiratory distress syndrome.3, 4, 5, 6 Although the clinical spectrum of severe COVID-19 has been characterised in reports from China and Italy,3, 4, 5, 6, 7, 8 detailed understanding of critical illness related to COVID-19 in the USA has been limited to a small case series from Washington State.9, 10 Here, we characterise the epidemiology, clinical course, and risk factors for in-hospital mortality among a cohort of adults with COVID-19-related critical illness admitted to two hospitals in New York City during the first month of the city's outbreak.
Research in context.
Evidence before this study
We searched PubMed on April 18, 2020, for articles using the search terms (“SARS-CoV-2” OR “COVID-19”) AND (“critical illness” OR “critical care” OR “intensive care”). Of 518 papers identified, we found 35 publications which included original clinical data from patients admitted to hospital with COVID-19, primarily reported from China (66%) and Italy (14%). We identified three studies that described the clinical course and outcomes of critically ill patients with COVID-19 in the USA. However, two of these studies were small (fewer than 25 patients each) and the third study, while larger (n=121), reported only summary statistics.
Added value of this study
We prospectively characterised the epidemiology, clinical course, and outcomes of 257 critically ill patients with laboratory-confirmed COVID-19 admitted to two hospitals in New York City over the first month of the city's outbreak. Consistent with reports from Italy and China, older age and cardiopulmonary comorbidities were associated with increased mortality. Novel findings in this study include determining independent associations between biomarkers for inflammation (interleukin-6) and thrombosis (D-dimer) and mortality, as well as identifying a high incidence of critical illness among racial and ethnic minorities in the current epicentre of the COVID-19 pandemic. Strengths of this study include prospective and complete collection of detailed clinical data and outcomes, and use of multivariable, time-varying analyses to quantify independent risk factors for in-hospital death in one of the largest studies to date of critically ill patients with COVID-19 in the USA.
Implications of all the available evidence
Critical illness among patients hospitalised with COVID-19 in New York City is common and associated with a high frequency of invasive mechanical ventilation, extrapulmonary organ dysfunction, and substantial in-hospital mortality.
Methods
Study design and participants
This prospective observational cohort study took place at two NewYork-Presbyterian hospitals affiliated with Columbia University Irving Medical Center in northern Manhattan. The two hospitals, a 700-bed quaternary referral hospital (Milstein Hospital) and a 230-bed community-based hospital (Allen Hospital), included 117 and 12 intensive care unit (ICU) beds before the COVID-19 pandemic. Over the course of the study period, ICU capacity at each hospital was increased from 117 to 258 beds in the 700-bed quaternary referral hospital and from 12 to 24 beds in the 230-bed community-based hospital. At both hospitals, patients are admitted primarily through the emergency department from surrounding neighbourhoods in northern Manhattan and the southern Bronx.
We prospectively identified adult patients (aged ≥18 years) admitted to both hospitals from March 2 to April 1, 2020, who were diagnosed with laboratory-confirmed COVID-19 and were critically ill with acute hypoxaemic respiratory failure. Patients with acute hypoxaemic respiratory failure were defined as those receiving mechanical ventilation (invasive or non-invasive) or high-level supplemental oxygen (via high-flow nasal cannula or non-rebreathing face mask at a flow rate of 15 L per min or greater), at or during hospitalisation. All critically ill patients were admitted to either a high-dependency unit or ICU; patients requiring non-invasive respiratory support were admitted to high-dependency units while those requiring invasive mechanical ventilation were admitted to ICUs. Laboratory testing for SARS-CoV-2 infection was done using RT-PCR of nasopharyngeal or oropharyngeal swab samples. Testing was performed by the New York State Department of Health from March 2 to March 10, 2020, after which testing capacity was developed by clinical microbiology laboratories at NewYork-Presbyterian hospitals. We identified critically ill patients with COVID-19 through daily review of hospital admission logs in the electronic medical record. No sample size calculation was performed; the sample size was established by the time window of the study.
This study was approved by the institutional review board at Columbia University Irving Medical Center (protocol AAAS8916). The requirement for informed consent was waived because of the study design and ongoing public health emergency.
Procedures
We reviewed electronic medical records, laboratory results, and radiographic findings for all admitted patients with critical illness and laboratory-confirmed COVID-19. Using a standardised case record form developed by the International Severe Acute Respiratory and Emerging Infection Consortium and WHO, we recorded data on demographics, known medical history and co-morbidities, illness onset and symptoms, vital signs, and biochemical studies performed within 24 h of diagnosis of acute respiratory failure. We also recorded concentrations of plasma-based and serum-based biomarkers drawn within 72 h of hospital admission, including high-sensitivity C-reactive protein, D-dimer, ferritin, high-sensitivity troponin, procalcitonin, and interleukin-6 (IL-6). We prospectively collected data on management interventions delivered during hospitalisation including initiation and duration of mechanical ventilation, administration of advanced therapies for acute respiratory failure (neuromuscular blocking agents, inhaled pulmonary vasodilators, prone-positioning ventilation, and extracorporeal membrane oxygenation), vasopressor agents, renal replacement therapy, antibacterial agents, antiviral agents, and immunomodulatory agents (IL-6 receptor antagonists and corticosteroids).
Outcomes
The primary outcome was the rate of in-hospital death. Follow-up time was right-censored on April 28, 2020. Secondary outcomes included frequency and duration of invasive mechanical ventilation, frequency of vasopressor use and renal replacement therapy, and time to in-hospital clinical deterioration following admission, defined as an increase of at least 1 point from baseline on a 7-point ordinal scale. This scale, designed to assess clinical status over time, was based on that recommended by WHO for use in clinical research among hospitalised patients with COVID-19 (appendix p 1).11
Statistical analysis
Continuous variables were expressed as means (SD) and medians (IQR). Categorical variables were summarised as counts and percentages. Missing data was not imputed. We created Kaplan-Meier cumulative incidence plots. We estimated hazard ratios (HRs) for death using the Cox proportional hazards model. We measured time-to-event in days from the date of hospital admission to the date of in-hospital death. We included nine independent variables in our multivariable Cox model that we considered relevant to in-hospital mortality. We chose this number of variables considering the total number of deaths in our study, to avoid overfitting in the model. We included IL-6 and D-dimer concentrations because there is emerging evidence of dysregulated immune activation and coagulopathy in patients with severe COVID-19, and interest in treating this patient population with targeted immunomodulatory therapies and anticoagulants.12, 13 We included age and sex, as older age and male sex have been associated with poor clinical outcomes among patients with COVID-19.6, 7 We included symptom duration before hospital presentation because delayed initiation of supportive care might affect clinical outcomes and illness duration might affect host immune-inflammatory and thrombotic responses. We included specific comorbidity variables (hypertension, chronic cardiac and pulmonary disease, and diabetes) as these variables were significantly associated with mortality in univariable analyses. We also tested a separate multivariable Cox model including Sequential Organ Failure Assessment (SOFA) score as a covariable to evaluate the association between our independent variables of interest and in-hospital mortality, while adjusting for the initial severity of illness. We confirmed the proportional hazards assumption of the Cox models using the Schoenfeld residuals test. All analyses were done using Stata (version 16; StataCorp, College Station, TX, USA).
Results
Between March 2 and April 1, 2020, 1150 adults were admitted to both hospitals with laboratory-confirmed COVID-19, of which 257 (22%) were critically ill (table 1 ; appendix p 4). The median period of observation following hospital admission was 19 days (IQR 9–30). The median age of patients was 62 years (51–72), 171 (67%) of 257 patients were men, 159 (62%) were Hispanic or Latino, and 13 (5%) were health-care workers. 212 (82%) patients had at least one chronic illness (table 1). 119 (46%) patients had obesity (defined as body-mass index [BMI] ≥30), including 39 (71%) of 55 patients who were less than 50 years of age. Patients presented to hospital a median of 5 days (2–7) after symptom onset; black or African American and Hispanic or Latino patients presented later in their illness course than white patients. The most common presenting symptoms were shortness of breath, fever, cough, myalgia, and diarrhoea.
Table 1.
Patient characteristics
| Study population (n=257) | ||
|---|---|---|
| Sex | ||
| Women | 86 (33%) | |
| Men | 171 (67%) | |
| Age (years) | ||
| Median | 62 (51–72) | |
| 20–29 | 8 (3%) | |
| 30–39 | 19 (8%) | |
| 40–49 | 28 (11%) | |
| 50–59 | 52 (20%) | |
| 60–69 | 69 (27%) | |
| 70–79 | 52 (20%) | |
| 80–89 | 23 (9%) | |
| ≥90 | 6 (2%) | |
| Race or ethnic group* | ||
| Hispanic or Latino | 159 (62%) | |
| Black or African American | 49 (19%) | |
| White | 32 (12%) | |
| Asian | 8 (3%) | |
| Other | 5 (2%) | |
| Body-mass index† (kg/m2) | ||
| Mean | 30·8 (7·7) | |
| ≥30 | 119 (46%) | |
| ≥35 | 68 (26%) | |
| ≥40 | 33 (13%) | |
| Employed as health-care worker | 13 (5%) | |
| Comorbidities | ||
| Median | 2 (1–3) | |
| Hypertension | 162 (63%) | |
| Diabetes | 92 (36%) | |
| Chronic cardiac disease‡ (excluding hypertension) | 49 (19%) | |
| Chronic kidney disease of any stage | 37 (14%) | |
| Current or former smoker | 33 (13%) | |
| Chronic obstructive pulmonary disease or interstitial lung disease | 24 (9%) | |
| Chronic neurological disease§ or dementia | 24 (9%) | |
| Asthma | 21 (8%) | |
| Active solid or haematological malignancy or dysplasia | 18 (7%) | |
| Solid organ transplant recipient | 10 (4%) | |
| HIV infection | 8 (3%) | |
| Liver cirrhosis of any Child-Pugh class | 5 (2%) | |
| Duration of illness before hospital presentation (days) | ||
| Overall | 5 (2–7) | |
| Black or African American | 7 (3–8) | |
| Hispanic or Latino | 5 (2–7) | |
| White | 3 (1–7) | |
| Symptoms reported | ||
| Shortness of breath | 190 (74%) | |
| Fever | 183 (71%) | |
| Cough | 169 (66%) | |
| Myalgia | 67 (26%) | |
| Diarrhoea | 32 (12%) | |
| Rhinorrhea | 19 (7%) | |
| Sore throat | 15 (6%) | |
| Headache | 10 (4%) | |
| Vital signs at hospital presentation | ||
| Temperature (°C) | 38·0 (1·1) | |
| Heart rate (beats per min) | 101 (20) | |
| Respiratory rate (breaths per min) | 22 (6) | |
| Systolic blood pressure (mm Hg) | 129 (23) | |
| Oxygen saturation (%) | 89 (10) | |
| Altered mental status | 23 (9%) | |
| Infiltrates present on initial chest radiograph | 252 (98%) | |
Data are n (%), median (IQR), or mean (SD).
Data available for 253 patients.
Data available for 249 patients.
Coronary artery disease or congestive heart failure.
Chronic neurodegenerative disease or history of stroke.
Median serum creatinine was 1·5 (IQR 1·9–2·4) and 189 (87%) of 218 patients who had a urinalysis performed had proteinuria. Lymphocytopaenia was common, as was mildly elevated concentrations of aspartate aminotransferase. Concentrations of IL-6, high-sensitivity C-reactive protein, ferritin, D-dimer, high-sensitivity troponin, and procalcitonin were elevated in most patients (table 2 ).
Table 2.
Biochemical and biomarker values
| Study population (n=257) | |
|---|---|
| Lactate (mmol/L) | 1·5 (1·1–2·2), 223 |
| Creatinine (mg/dL) | 1·5 (0·9–2·4) |
| Proteinuria | 189/218 (87%) |
| Urine protein concentration (mg/dL) | 100 (30–300) |
| White blood cell count (×103 cells per μL) | 9·8 (6·6–12·7) |
| Lymphocyte count (×103 cells per μL) | 0·8 (0·6–1·2), 228 |
| Platelet count (×103 cells per μL) | 199 (148–270) |
| Bilirubin (mg/dL) | 0·6 (0·4–0·8), 242 |
| Aspartate aminotransferase (U/L) | 61 (42–104), 242 |
| Alanine aminotransferase (U/L) | 39 (27–67), 242 |
| Creatine kinase (U/L) | 236 (103–646), 223 |
| Prothrombin time (s) | 14·7 (14·0–15·8), 241 |
| Interleukin-6 (pg/mL) | 26 (11–69), 237 |
| High-sensitivity C-reactive protein (mg/L) | 158 (92–254), 253 |
| Ferritin (ng/mL) | 924 (472–1789), 253 |
| D-dimer (μg/mL) | 1·6 (0·9–3·5), 244 |
| High-sensitivity cardiac troponin T (ng/L) | 19 (9–52), 254 |
| Procalcitonin (ng/mL) | 0·35 (0·17–1·1), 255 |
Data are median (IQR) or n (%). Data are median (IQR), n if fewer patients were assessed for those laboratory studies than the total number of patients in the study.
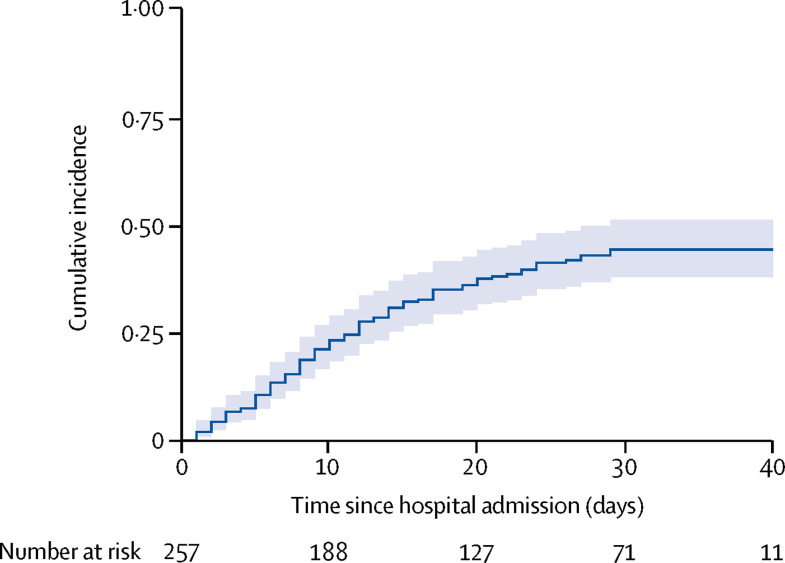
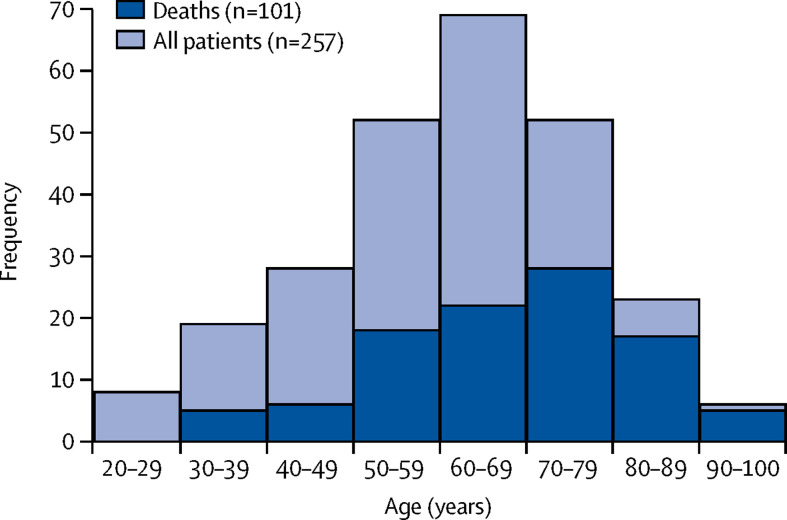
As of April 28, 2020, 101 (39%) of 257 patients had died following a median of 9 days (IQR 5–15) in the hospital (figure 1 ). This included 84 (41%) of 203 patients who received invasive mechanical ventilation (IMV) during hospitalisation. Across racial and ethnic groups, death occurred in 20 (41%) of 49 black or African American patients, 61 (38%) of 159 Hispanic or Latino patients, and 15 (47%) of 32 white patients. The median time to clinical deterioration following admission was 3 days (1–6). Most deaths occurred in patients who were at least 50 years of age (figure 2 ). 94 (37%) of 257 patients remained hospitalised with a median duration of hospitalisation of 33 days (29–36). 58 (23%) patients were discharged alive, 12 (21%) of which required supplemental oxygen, and four (2%) were transferred to another institution.
Figure 1.
Kaplan-Meier cumulative incidence curve for in-hospital death among critically ill patients with COVID-19
Figure 2.
Age distribution of critically ill patients with COVID-19
During hospitalisation, 115 (45%) of 257 patients initially received non-invasive respiratory support via non-rebreathing oxygen face mask, 12 (5%) via high-flow nasal cannula, and three (1%) via non-invasive ventilation (table 3 ). 203 (79%) patients received IMV for a median of 18 days (IQR 9–28). Survivors had a median of 27 days (15–32) of IMV and non-survivors had a median of 10 days (4–16). Among 52 (26%) of 203 patients who were extubated alive, median duration of IMV was 14 days (10–21). 71 (62%) of 115 patients who initially received non-invasive respiratory support ultimately received IMV after a median of 3 days (1–5).
Table 3.
Clinical management and outcomes of study population
| Study population (n=257) | ||
|---|---|---|
| Sequential Organ Failure Assessment score on day 1 of critical illness* | 11 (8–13), 221 | |
| Lowest PaO2 to FiO2 ratio on day 1 of critical illness (mm Hg)† | 129 (80–203), 222 | |
| Respiratory support | ||
| Non-rebreathing oxygen face mask | 115 (45%, 39–51) | |
| High-flow nasal cannula oxygen therapy | 12 (5%, 3–8) | |
| Non-invasive ventilation | 3 (1%, 0–3) | |
| Invasive mechanical ventilation | 203 (79%, 74–84) | |
| Duration of invasive mechanical ventilation (days) | 18 (9–28) | |
| Settings and parameters during first 24 h of invasive mechanical ventilation | ||
| Highest PEEP (cm H2O) | 15 (12–18) | |
| Highest FiO2 (%) | 1·0 (0·8–1·0) | |
| Tidal volume (mL per kg predicted bodyweight) | 6·2 (5·9–7·2), 195 | |
| Minute ventilation (L/min) | 8 (6–10) | |
| Plateau airway pressure (cm H2O) | 27 (23–31), 165 | |
| Respiratory system compliance (mL/cm H2O) | 27 (22–36), 165 | |
| Driving pressure (cm H2O) | 15 (11–18), 165 | |
| Advanced therapies for acute respiratory failure | ||
| Early neuromuscular blockade‡ | 51/203 (25%, 20–32) | |
| Inhaled nitric oxide | 22/203 (11%, 7–16) | |
| Prone-positioning ventilation | 35/203 (17%, 13–23) | |
| Extracorporeal membrane oxygenation | 6/203 (3%, 1–6) | |
| Received tracheostomy | 17/203 (8%, 5–13) | |
| Vasopressors | 170 (66%, 60–72) | |
| Renal replacement therapy | 79 (31%, 25–37) | |
| Antiviral agent | ||
| Hydroxychloroquine | 185 (72%, 66–77) | |
| Remdesivir | 23 (9%, 6–13) | |
| Antibacterial agent | 229 (89%, 85–92) | |
| Immunomodulatory agent | ||
| Corticosteroid | 68 (26%, 21–32) | |
| Interleukin-6 receptor antagonist | 44 (17%, 13–22) | |
| Outcomes | ||
| Died in hospital | 101 (39%, 34–45) | |
| Duration of hospitalisation prior to death (days) | 9 (5–15) | |
| Remained hospitalised | 94 (37%, 31–43) | |
| Transferred to another hospital | 4 (2%, 0–4) | |
| Discharged alive | 58 (23%, 18–28) | |
| Required supplemental oxygen at discharge | 12/58 (21%, 12–33) | |
Data are median (IQR) or n (%), with 95% Wilson score CIs. Data are median (IQR), n if fewer patients were assessed for those outcomes than the total number of patients in the study. The study population was admitted to hospital between March 2 and April 1, 2020. Follow-up time was right-censored on April 28, 2020. PaO2=partial pressure of arterial oxygen. FiO2=fraction of inspired oxygen. PEEP=positive end-expiratory pressure.
Mental status assessment of alert, responsive to voice, pain, or unresponsive also converted to Glasgow Coma Scale for calculation.14
FiO2of 0·90 used for patients receiving supplemental oxygen at 15 L/min through non-rebreathing face mask.
Administered within 48 h of initiation of invasive mechanical ventilation.
On the first day of critical illness, the median SOFA score14 was 11 (IQR 8–13) and the median value of the lowest partial pressure of arterial oxygen (PaO2) to fraction of inspired oxygen (FiO2) ratio recorded on this day was 129 (80–203; table 3). 170 (66%) of 257 patients received vasopressors and 79 (31%) received renal replacement therapy (RRT) during hospitalisation.
As the incidence of bacterial superinfection in our setting was unknown early in the outbreak, antibacterial agents were administered empirically to nearly all critically ill patients (229 [89%] of 257). Antibiotics were de-escalated based on pertinent culture data at the discretion of treating clinicians in collaboration with infectious diseases consultants. Antiviral agents were also administered to most patients: 185 (72%) received hydroxychloroquine and 23 (9%) received remdesivir. Remdesivir was administered through enrolment in clinical trials or compassionate use access. 68 (26%) patients received corticosteroids and 44 (17%) received IL-6 receptor antagonists. These agents were administered if there was a high suspicion of severe hyperinflammatory state, based on assessment of inflammatory markers, and lower suspicion for concurrent uncontrolled secondary infection, at the discretion of treating clinicians in collaboration with infectious diseases consultants.
In the multivariable Cox model (table 4 ), older age (adjusted HR [aHR] 1·31 [95% CI 1·09–1·57] per 10-year increase), chronic cardiac disease (aHR 1·76 [1·08–2·86]), chronic pulmonary disease (aHR 2·94 1·48–5·84]), higher concentrations of IL-6 (aHR 1·11 [1·02–1·20] per decile increase), and higher concentrations of D-dimer (aHR 1·10 [1·01–1·19] per decile increase) were independently associated with in-hospital mortality. The HRs generated in this model were consistent with those generated in a similar model adjusted for SOFA score (appendix p 2).
Table 4.
Risk factors for in-hospital mortality
| Univariable HR (95% CI) | Multivariable HR (95% CI) | |
|---|---|---|
| Age (per 10-year increase) | 1·49 (1·29–1·73) | 1·31 (1·09–1·57) |
| Male sex | 0·85 (0·57–1·27) | 1·13 (0·71–1·81) |
| Symptom duration before hospital presentation (per day) | 0·98 (0·93–1·02) | 1·01 (0·96–1·05) |
| Hypertension | 2·24 (1·40–3·59) | 1·58 (0·89–2·81) |
| Chronic cardiac disease* | 2·21 (1·44–3·39) | 1·76 (1·08–2·86) |
| Chronic obstructive pulmonary disease or interstitial lung disease | 3·15 (1·84–5·39) | 2·94 (1·48–5·84) |
| Chronic kidney disease | 1·50 (0·92–2·45) | .. |
| Diabetes | 1·65 (1·11–2·44) | 1·31 (0·81–2·10) |
| Body-mass index ≥40 | 0·76 (0·40–1·47) | .. |
| Interleukin-6 (per decile increase) | 1·12 (1·04–1·21) | 1·11 (1·02–1·20) |
| D-dimer (per decile increase | 1·18 (1·10–1·27) | 1·10 (1·01–1·19) |
HR=hazard ratio.
Coronary artery disease or congestive heart failure.
Discussion
Among critically ill adults with COVID-19 admitted to two hospitals in New York City during the first month of the city's outbreak, the majority were men over 60 years of age with hypertension and diabetes, nearly half had obesity, and 5% were health-care workers. 79% of patients received IMV and a third received RRT. As of April 28, 2020, 39% of patients had died in hospital.
Novel findings in this study include establishing independent associations between biomarkers for inflammation (IL-6) and thrombosis (D-dimer) and in-hospital mortality, as well as identifying a high incidence of critical illness among racial and ethnic minorities in the current epicentre of the COVID-19 pandemic. Strengths of this study include prospective and complete collection of detailed clinical data and outcomes, and use of multivariable, time-varying analyses to quantify independent risk factors for in-hospital death in one of the largest studies to date of critically ill patients with COVID-19 in the USA.
257 (22%) of 1150 patients admitted to hospital with COVID-19 were critically ill with acute hypoxaemic respiratory failure. This is consistent with reports from China,3, 4 Italy,5 and preliminary data released by the US Centers for Disease Control and Prevention,15 in which the incidence of ICU admission among patients admitted with COVID-19 ranged from 7–26%. This high incidence of critical illness among hospitalised patients has acute implications for US hospital systems, specifically the potential need to increase ICU surge capacity in preparation for large numbers of patients requiring IMV and other forms of organ support.
79% of patients received IMV during hospitalisation for median durations of 27 days among survivors and 10 days among non-survivors. This included 62% of patients who initially received less invasive methods of respiratory support. Although the proportion of patients in our cohort receiving IMV was higher than that reported in observational studies from China3, 4, 6, 7 and Washington state,9, 10 it is similar to the rate recently reported from Italy,8 in which IMV was provided to 88% of critically ill patients with COVID-19. As in Italy, where the median ratio of PaO2 to FiO2 at ICU admission was 160,8 the higher proportion of patients requiring IMV in our cohort could be explained by the severity of hypoxaemia, as the median nadir PaO2 to FiO2 ratio in our population was 129.
In our cohort of patients with acute hypoxaemic respiratory failure, whose respiratory system compliance was severely reduced (median 27 mL/cm H2O), frequency of adherence to standard-of-care lung-protective ventilation was high (median tidal volume 6·2 mL per kg predicted bodyweight, median plateau airway pressure 27 cm H2O), as were levels of positive end-expiratory pressure (PEEP; median maximum PEEP 15 cm H2O within the first 24 h). 25% of intubated patients received early neuromuscular blockade, 17% received prone positioning ventilation, and 3% received extracorporeal membrane oxygenation (ECMO). The sudden surge of critically ill patients admitted with severe acute respiratory distress syndrome initially outpaced our capacity to provide prone-positioning ventilation, which was only performed in three of eight ICUs at our institution at the start of the outbreak. We have since expanded our capacity for prone-positioning ventilation by deploying dedicated proning teams to all ICUs, including non-traditional ICU locations. The low volume of ECMO used during the study period is primarily a reflection of the low number of patients within our hospital system meeting criteria after initiating other therapies, such as lung-protective IMV and prone-positioning ventilation. As an ECMO referral center for regional hospitals, we received a moderate-to-high volume of ECMO referrals during that period, the majority of which were optimised with conventional management strategies and did not ultimately meet criteria for ECMO or were excluded on the basis of low probability of benefit.
As of April 28, 2020, 101 (39%) patients had died and 94 (37%) remained hospitalised. Similar to data reported elsewhere,3, 7, 16 we identified older age, cardiopulmonary comorbidities, and higher concentrations of D-dimer as independent risk factors for poor outcomes. Higher concentrations of IL-6, which have been observed among patients with COVID-19 with more severe clinical illness,16, 17 were also associated with in-hospital mortality. Although the pathogenesis of severe COVID-19 remains to be completely understood, emerging data suggest that organ dysfunction and poor outcomes could be mediated by high concentrations of proinflammatory cytokines, including IL-6 and dysregulated coagulation and thrombosis.12, 13, 18 Continued investigation of these pathological processes and the utility of their biomarkers is needed, given increasing reports of corticosteroid use and ongoing clinical trials of IL-6 receptor antagonists among critically ill patients with COVID-19 (eg, NCT04315298 registered with ClinicalTrials.gov) as well as rapidly evolving guidelines19 for anticoagulant use in this population.
Consistent with data from China,3 and Italy,8 hypertension was associated with poor in-hospital survival. Given the globally high burden of hypertension and emerging understanding of interactions between SARS-CoV-2 and angiotensin-converting-enzyme-2,20 further investigations are needed to better define a relation—if any—between hypertension, exposure to renin angiotensin aldosterone system antagonists, and severe COVID-19.
31% of patients in our cohort developed severe acute kidney injury requiring RRT during hospitalisation. Consistent with emerging data from China,21 a high proportion of patients (87%) had proteinuria. The high frequency of RRT in our patient population has considerable implications for resource allocation, given the limited available supplies of RRT machines and consumables, and staffing requirements necessary to provide continuous or intermittent RRT to critically ill patients. As the general incidence and underlying mechanisms of severe COVID-19-related kidney injury remain poorly understood,21 epidemiological, clinical, and biological investigations are necessary to inform hospital preparedness strategies and development of targeted preventive and treatment interventions.
46% of critically ill patients had obesity. This observation is consistent with trends seen in hospitalised patients with COVID-19 in the UK, where obesity has been associated with increased incidence of ICU admission and mortality.22 However, although obesity was more common in our adult patient population than in the general New York City adult population (where prevalence of obesity is 22%),23 we did not identify severe obesity (BMI ≥40) as an independent risk factor for mortality. Similar to other cardiometabolic comorbidities, further studies are needed to identify the mechanisms that mediate the association of obesity with susceptibility to or severity of COVID-19.
Hydroxychloroquine or remdesivir, antiviral agents which have shown activity against SARS-CoV-2 in vitro,24 were administered to 81% of patients in this study. The efficacy of remdesivir among patients with severe COVID-19 remains uncertain. A randomised, double-blind, placebo-controlled clinical trial from China reported no significant differences in time to clinical improvement or 28-day mortality among patients with laboratory-confirmed SARS-CoV-2 infection admitted to hospital receiving remdesivir.25 However, this trial was underpowered, given a lack of patients eligible for enrolment. More recently, based on preliminary, unpublished data from an adaptive, placebo-controlled clinical trial sponsored by the US National Institute of Allergy and Infectious Diseases (NCT04280705 registered with ClinicalTrials.gov) and an open-label trial sponsored by Gilead Sciences (NCT04292899 registered with ClinicalTrials.gov), the US Food and Drug Administration issued an emergency use authorisation for remdesivir among severely ill inpatients with COVID-19.26 For hydroxychloroquine, emerging observational data from the USA have not reported signals of clinical benefit for use of this agent among inpatients with COVID-19.27 To better evaluate the safety and efficacy of hydroxychloroquine in this setting, investigators at Oxford University (Oxford, UK) and the US National Heart, Lung, and Blood Institute have launched randomised clinical trials among hospitalised patients with COVID-19 in the UK (ISRCTN50189673 registered with ISRCTN) and the USA (NCT04332991 registered with ClinicalTrials.gov).
5% of critically ill patients were health-care workers. Although nosocomial SARS-CoV-2 infection cannot be determined with certainty given widespread community transmission, COVID-19-related critical illness in these individuals highlights the risks facing frontline health-care workers in the USA, where at least 9000 health-care workers have been infected as of April 9, 2020.28 Continued and consistent access to personal protective equipment for hospital staff is imperative to prevent nosocomial transmission, optimise health-care worker safety, and ensure an adequate workforce.
This study has a number of strengths. First, our study represents one of the largest cohorts of patients with COVID-19-related critical illness reported to date in the USA. Second, we prospectively identified patients and collected data. Thus, our findings reflect the ongoing outbreak of COVID-19 in New York City, currently the epicentre of the pandemic. Third, we collected data using a globally harmonised, WHO-endorsed case record form. Fourth, we augmented collection of standard clinical and laboratory data with clinically and pathologically relevant biomarkers, concentrations of which were available for nearly all patients. Lastly, given the prospective nature of our study, our analyses were done with near-complete data, with in-hospital outcomes known for all included patients through April 28, 2020.
This study has several limitations. First, our study took place in two hospitals in northern Manhattan, potentially limiting generalisability to hospital settings elsewhere in New York City, especially in terms of the demographic characteristics of the patient population. Specifically, our cohort included a high proportion of Hispanic or Latino and black or African American patients who are known to have higher prevalence of cardiometabolic comorbidities and socioeconomic vulnerabilities that may make social distancing and access to care more difficult.29 Studies among more racially, ethnically, and geographically diverse cohorts are needed to confirm our findings. Despite these limitations, our sites included both a large quaternary referral hospital and a smaller, community-based hospital, thereby increasing generalisability to other clinical settings. Second, our analyses incorporated outcome data collected through April 28, 2020. As vital status is not yet known for patients who remained hospitalised after this date, the 39% mortality reported here represents the minimum in-hospital case fatality rate for our cohort. Third, patients presented to the hospital at varying times in their illness course, which could have affected their clinical course and outcomes. To mitigate the potential effect of this variance on our analyses, we included time from symptom onset to hospital presentation as a covariable in our regression models. Fourth, of available biomarkers, we included IL-6 and D-dimer in our multivariable models because of the pathophysiological and treatment implications. We did not analyse serial concentrations of these and other biomarkers, which might fluctuate considerably over the course of the illness.
In conclusion, critical illness among patients admitted to hospital with COVID-19 in New York City is common and associated with a high frequency of invasive mechanical ventilation, extrapulmonary organ dysfunction, and substantial in-hospital mortality.
Acknowledgments
Acknowledgments
This work was supported by the National Institute of Allergy and Infectious Diseases (F32AI147528-01) and the National Center for Advancing Translational Sciences (UL1TR001873), National Institutes of Health, and the Columbia University Irving Institute for Clinical and Translational Research. The authors would like to thank their patients and fellow health-care workers for providing outstanding patient care at considerable personal risk.
Contributors
MJC and MRO'D conceived the study and its design, had full access to the data, and take responsibility for the integrity of the data and accuracy of the analysis. MJC, MRB, DA, SDJ, BJM, and EMB organised and entered data. MJC, MRB, and MRO'D contributed to data analyses. MJC, MRB, DA, JGA, JC, LER, JH, BRH, JS-S, NHY, DB, and MRO'D contributed to data interpretation. MJC and MRO'D drafted the manuscript. All authors critically revised the drafted manuscript and approve of the submitted manuscript.
Declaration of interests
JC is a minority shareholder at iCE Neurosystems. This does not relate to the current work. DB receives research support from ALung Technologies and he was previously on their medical advisory board. He has been on the medical advisory boards for Baxter, BREETHE, Xenios, and Hemovent. None of these activities relate to the current work. MRO'D and MJC are investigators for clinical trials evaluating the efficacy and safety of remdesivir (sponsored by Gilead Sciences) and convalescent plasma (sponsored by Amazon) in hospitalised patients with COVID-19. Support for this work is paid to Columbia University. JGA is an investigator for a clinical trial evaluating the activity and safety of selinexor in hospitalised patients with COVID-19, sponsored by Karyopharm Therapeutics. Support for this work is paid to Columbia University. All other authors declare no competing interests.
Supplementary Material
References
- 1.Centers for Disease Control and Prevention Coronavirus disease 2019 (COVID-19): cases in the U.S. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html
- 2.New York State Department of Health COVID-19 tracker. https://covid19tracker.health.ny.gov/views/NYS-COVID19-Tracker/NYSDOHCOVID-19Tracker-Map?%3Aembed=yes&%3Atoolbar=no&%3Atabs=n
- 3.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. published online Feb 24. [DOI] [PubMed] [Google Scholar]
- 4.Guan WJ, Ni ZY, Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA. 2020 doi: 10.1001/jama.2020.4031. published online March 13. [DOI] [PubMed] [Google Scholar]
- 6.Yang X, Yu Y, Xu J. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30079-5. published online Feb 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou F, Yu T, Du R. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grasselli G, Zangrillo A, Zanella A. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020 doi: 10.1001/jama.2020.5394. published online April 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arentz M, Yim E, Klaff L. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington State. JAMA. 2020 doi: 10.1001/jama.2020.4326. published online March 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhatraju PK, Ghassemieh BJ, Nichols M. COVID-19 in critically ill patients in the Seattle region—case series. N Engl J Med. 2020 doi: 10.1056/NEJMoa2004500. published online March 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.WHO R&D Blueprint: COVID-19 therapeutic trial synopsis. Feb 18, 2020. https://www.who.int/blueprint/priority-diseases/key-action/COVID-19_Treatment_Trial_Design_Master_Protocol_synopsis_Final_18022020.pdf
- 12.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Helms J, Tacquard C, Severac F. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020 doi: 10.1007/s00134-020-06062-x. published online May 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kelly CA, Upex A, Bateman DN. Comparison of consciousness level assessment in the poisoned patient using the alert/verbal/painful/unresponsive scale and the Glasgow Coma Scale. Ann Emerg Med. 2004;44:108–113. doi: 10.1016/j.annemergmed.2004.03.028. [DOI] [PubMed] [Google Scholar]
- 15.CDC COVID-19 Response Team Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu C, Chen X, Cai Y. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.0994. published online March 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05991-x. published online March 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhou Y, Fu B, Zheng X. Pathogenic T cells and inflammatory monocytes incite inflammatory storm in severe COVID-19 patients. Natl Sci Rev. 2020 doi: 10.1093/nsr/nwaa041. published online March 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thachil J, Tang N, Gando S. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020;18:1023–1026. doi: 10.1111/jth.14810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17:259–260. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Naicker S, Yang CW, Hwang SJ, Liu BC, Chen JH, Jha V. The novel coronavirus 2019 epidemic and kidneys. Kidney Int. 2020;97:824–828. doi: 10.1016/j.kint.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Intensive Care National Audit & Research Centre ICNARC report on COVID-19 in critical care. https://www.icnarc.org/Our-Audit/Audits/Cmp/Reports
- 23.New York State Department of Health New York State Community Health Indicator Reports (CHIRS) https://www.health.ny.gov/statistics/chac/indicators/
- 24.Wang M, Cao R, Zhang L. Remdesivir and chloroquine effectively inhibit the recently emerged novel coronavirus (2019-nCoV) in vitro. Cell Res. 2020;30:269–271. doi: 10.1038/s41422-020-0282-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang Y, Zhang D, Guanhua D. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet. 2020 doi: 10.1016/S0140-6736(20)31022-9. published online April 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.US Food and Drug Administration Remdesivir Emergency Use Authorization. May 1, 2020. https://www.fda.gov/media/137564/download
- 27.Geleris J, Sun Y, Platt J. Observational study of hydroxychloroquine in hospitalized patients with COVID-19. N Engl J Med. 2020 doi: 10.1056/NEJMoa2012410. published online May 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.CDC COVID-19 Response Team Characteristics of health care personnel with COVID-19—United States, February 12–April 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:477–481. doi: 10.15585/mmwr.mm6915e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bhala N, Curry G, Martineau AR, Agyemang C, Bhopal R. Sharpening the global focus on ethnicity and race in the time of COVID-19. Lancet. 2020 doi: 10.1016/S0140-6736(20)31102-8. published online May 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.