Abstract
Legionella pneumophila is an opportunistic waterborne pathogen of public health concern. It is the causative agent of Legionnaires’ disease (LD) and Pontiac fever and is ubiquitous in manufactured water systems, where protozoan hosts and complex microbial communities provide protection from disinfection procedures. This review collates the literature describing interactions between L. pneumophila and protozoan hosts in hospital and municipal potable water distribution systems. The effectiveness of currently available water disinfection protocols to control L. pneumophila and its protozoan hosts is explored. The studies identified in this systematic literature review demonstrated the failure of common disinfection procedures to achieve long term elimination of L. pneumophila and protozoan hosts from potable water. It has been demonstrated that protozoan hosts facilitate the intracellular replication and packaging of viable L. pneumophila in infectious vesicles; whereas, cyst-forming protozoans provide protection from prolonged environmental stress. Disinfection procedures and protozoan hosts also facilitate biogenesis of viable but non-culturable (VBNC) L. pneumophila which have been shown to be highly resistant to many water disinfection protocols. In conclusion, a better understanding of L. pneumophila-protozoan interactions and the structure of complex microbial biofilms is required for the improved management of L. pneumophila and the prevention of LD.
Keywords: Legionella pneumophila, protozoa, Vermamoeba, Acanthamoeba, potable water, hospital water, water disinfection, legionellosis
1. Introduction
Legionella pneumophila is an opportunistic pathogen associated with community-acquired and nosocomial infections. It is the causative agent of legionellosis, which includes Legionnaires’ disease (LD), a severe atypical pneumonia infection, and Pontiac fever, an acute “flu-like” illness [1]. Globally, the incidence of LD has been increasing. In Europe, the number of notified cases increased from 4921 in 2011 to 11,343 in 2018 [2]. In the US, the number of notified LD cases has increased from 2301 in 2005 [3] to 7104 in 2018 [4], a 300% increase. Globally, the fatality rate of LD ranges from 2.2–10.3%, with the lowest in Singapore and the highest in European countries [5]. In nosocomial outbreaks the fatality rate can reach up to 48% [6,7,8].
The genus Legionella is comprised of 60 species and 80 distinct serogroups [9]. Globally, L. pneumophila is the primary aetiological agent of LD. In Europe and the US, L. pneumophila serogroup (SG1) is responsible for 70–92% reported cases [8]. According to WHO, 20–30% infections are caused by other L. pneumophila serogroups and only 5–10% are caused by other Legionella species (L. micdadei, L. bozemanii, L. dumoffii and L. longbeachae) [10]. However, unlike rest of the world, in Australia and New Zealand, L. longbeachae is associated with ≈ 50% reported cases of legionellosis [11,12].
L. pneumophila is ubiquitous in manufactured water systems [10] and in the USA has been identified as the primary cause of all potable water related outbreaks [13]. Manufactured water systems, building plumbing systems, recreational water, cooling towers and humidifiers are major sources of L. pneumophila [10]. Inside these plumbing structures, Legionella and protozoan hosts are incorporated within biofilms. Factors like water stagnation, higher levels of organic carbon and moderate temperatures can increase the rate of biofilm formation [14,15]. Transmission occurs through inhalation or aspiration of contaminated aerosols or water [16]. L. pneumophila maintains long term contamination of manufactured water systems through its growth within protozoan hosts, association with biofilms and disinfectant resistance or tolerance [17,18]. Freshwater amoebae are the natural eukaryotic hosts of Legionella; whereas, humans are considered accidental hosts [19]. In the human body, Legionella–contaminated aerosols are inhaled into the lungs and phagocytosed by alveolar macrophages. The alveolar macrophages behave like amoebae hosts and facilitate the intracellular division and propagation of Legionella, resulting in LD [20,21].
Understanding the interactions between L. pneumophila and protozoan hosts is essential to inform water treatment and risk management strategies for the prevention of LD. Protozoan hosts play an important role in the ability of L. pneumophila to survive exposure to physiochemical and environmental stresses. Protozoans facilitate the intracellular replication and packaging of live bacterial cells in the stress resistant membrane bound infectious export vesicles [22,23]. The cysts of cyst-forming amoebae provide a protective shelter from prolonged environmental stress [24]. There are numerous reports describing existence of L. pneumophila harboring within protozoans from thermally-, chemically-, and UV radiation-treated potable water supplies and storage reservoirs [25]. Protozoan hosts and environmental stress may facilitate the genesis of highly resistant and potentially infectious viable but non-culturable (VBNC) L. pneumophila [26,27]. Importantly, water storage facilities and distribution networks of many countries have been shown to be highly contaminated with protozoans that may act as hosts for L. pneumophila (>0–4500 cell/L cell density) [28].
This systematic literature review collated studies which detected L. pneumophila in association/connection with protozoan hosts from hospital or municipal potable water distribution systems and discusses this relationship under diverse environmental conditions. The effectiveness of different physical and chemical water treatment methods to control the L. pneumophila and its protozoan hosts is described and implications for the control and management of these water distribution systems is explored.
2. Results
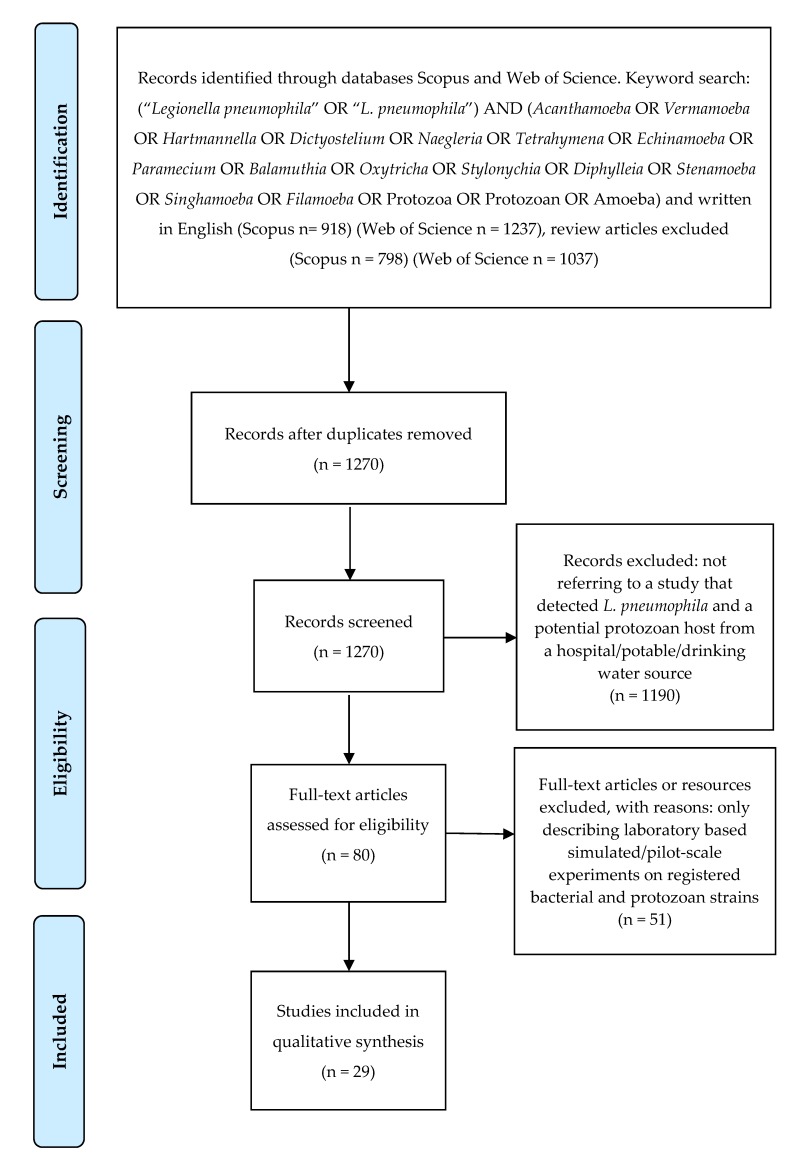
One thousand two hundred and seventy abstracts were obtained from the Web of Science and SCOPUS. After applying the described criteria (see Figure 1 and the Materials and Methods section), 29 research manuscripts discussing L. pneumophila and its protozoan hosts in hospital and potable water systems were included in the study (Table 1). Potential protozoan hosts playing crucial role(s) in the L. pneumophila life-cycle and living in both types of water systems are compiled in Table 2. These protozoan hosts have the potential to provide an appropriate habitat for replication and survival of L. pneumophila.
Figure 1.
Overview of search methods and articles inclusion and exclusion criteria.
Table 1.
Potential protozoan hosts of Legionella pneumophila isolated from and hospital and potable water systems.
| Isolation Source (Temperature at Time of Sampling) |
Water Treatment Method | L. pneumophila | Potential Protozoan Host | Comments | Country of Origin (Sampling Site) | Reference | ||
|---|---|---|---|---|---|---|---|---|
| Identification Method | Serogroup Sequence-Type |
Genus/Species | Identification Method | |||||
| Hospital Settings | ||||||||
| Hot (45–52 °C) water tanks | - | Culturing, co-culture assay and serological identification | SG1 |
Hartmannella cantabrigiensis
Vermamoeba vermiformis Echinamoeba exudans |
Culturing, light and transmission electron microscopy | Nosocomial legionellosis investigation | USA | [31] |
| Potable water sites (39–40 °C) | - | Culturing and monoclonal antibody based serotyping | SG1 |
Acanthamoeba hatchetti
Hartmannella cantabrigiensis Vermamoeba vermiformis Vahlkampfia Filamoeba nolandi Comandonia operculata Paravahlkampfia ustiana |
Culturing and light microscopy | Nosocomial legionellosis investigation Thermal treatment (70 °C) and chlorination (1.5–2.0 mg/L) controlled the bacteria for 6 months but not amoebae. The treatment reduced incidence of legionellosis |
South Dakota, USA | [35] |
| Cooling tower, humidifier, hot water tank and supply | - | Culturing and co-culture assay | - |
Vermamoeba vermiformis
Naegleria |
Culturing, light and transmission electron microscopy | - | Paris, France | [32] |
| Hot (39–60 °C) and cold water supply | - | Culturing (ODR: 1 × 103–9.7 × 104 CFU/L), direct fluorescent antibody and monoclonal antibody based serotyping | SG1 SG5 |
Hartmannella (Hartmannellidae/limax amoebae) |
Culturing and light microscopy | Post nosocomial outbreak surveillance | Halifax, Nova Scotia, Canada | [36] |
| Organ transplant unit hot (mean 56.2 °C) and cold water (mean 16.6 °C) supplies | - | Culturing and serological assay | SG1 |
Acanthamoeba
Hartmannella Echinamoeba Vahlkampfia Tetrahymena Vannella |
Culturing and light microscopy | Population density of amoebae was greater in hot water supplies than cold water supplies Along amoebae other diverse eukaryotic microbes were detected as well |
UK | [37] |
| Water supplies | Thermal treatment (60 and 70 °C) | Culturing (Legionella ODR: 2.89–6.74 × 105 CFU/L), co-culture, latex agglutination, indirect and immunofluorescence assays, and PFGE | SG1 SG2 |
Acanthamoeba
Vahlkampfia Mayorella |
Culturing and light microscopy | Thermal treatment (70 °C) only controlled bacterial contamination for 3 months SG1 is more thermotolerant than SG2 at 60 °C |
Germany | [38] |
| Water network system (mean 56 °C) | - | Amoebae co-culture assay, PCR and sequencing | - | Vermamoeba vermiformis | Culturing, PCR and sequencing | Detection of thermotolerant Vermamoeba vermiformis | Lausanne, Switzerland | [39] |
| Water distribution system (18.9–32.6 °C) | Chlorine dioxide treatment Thermal treatment (<50 °C) |
Culturing (ODR: L. pneumophila SG1: 1 × 102–3.5 × 104 CFU/L and L. pneumophila SG2-14: 1 × 102–4 × 104 CFU/L) and latex agglutination assay | SG1 SG2-14 |
Acanthamoeba
Hartmannella |
Culturing and light microscopy | - | Messina, Italy | [40] |
| Tap water | Chloramine (1.93 ± 1.04 mg/L) treatment | Culturing (protocol: ISO 11731-2:2004, LOD: 1 CFU/100 mL, ODR: 100–1.4 × 105 ± 1.3 × 105 CFU/L), qPCR (LOD: 5 GU, LOQ: 25 GU, Legionella ODR: 100–109 gu/L) and EMA-qPCR | ST269 | Acanthamoeba polyphaga | Culturing, light microscopy and PCR | Italy | [27] | |
| Cold (14.9 °C) and warm (45.1 °C) potable water | Thermal treatment, chlorination (hypochlorates, chloramine), bacterial filters and chlorine dioxide treatment | Culturing (protocols: ISO 11731:1998 and ISO 11731-2:2004, LOD: 1 CFU/100 mL, ODR: 0–3 × 103 CFU/100 mL) and MALDI-TOF MS | - |
Acanthamoeba
Vermamoeba vermiformis |
Culturing and light microscopy | - | Bratislava, Slovakia | [41] |
| Cold water system (20–27.3 °C) | Chlorine contents 0.01–0.32 mg/L | qPCR (protocol: ISO/TS 12869:2012, LOD: 5 GU, LOQ: 25 GU, ODR: 2.7–3.8 × 102 gu/L) | - |
Acanthamoeba
Vermamoeba vermiformis |
Culturing and light microscopy | Johannesburg, South Africa | [42] | |
| Dental unit waterlines | H2O2 treatment (occasionally) | Heterotrophic plate counts, culturing (protocol: ISO 11731-2:2004, LOD: 1 CFU/100 mL, ODR: 0–2700 CFU/L) and agglutination test | - | Vermamoeba vermiformis | Culturing, light microscopy, PCR and sequencing | Italy | [43] | |
| Potable Water System | ||||||||
| Unchlorinated water supplies (9.5–13.5 °C) | - | qPCR | - |
Acanthamoeba
Acanthamoeba polyphaga Vermamoeba vermiformis |
qPCR (LOD: 1 cell/reaction), T-RFLP, cloning and sequencing | Along amoebae other diverse eukaryotic microbes were detected as well | Netherlands | [44] |
| Ground water supplies (5–39 °C) | Aeration, lime stone, granular activated carbon slow sand and rapid sand filtration, ozonisation and pellet softening | Culturing, biofilm batch test and qPCR | - |
Acanthamoeba
Vermamoeba vermiformis |
18S rDNA sequencing, PCR, T-RFLP and sequencing | Along amoebae other eukaryotic microbes were detected as well | Netherlands | [45] |
| Water supplies (mean 30 °C) | Reverse osmosis, distillation (82%), chlorination (<0.005–0.2 mg/L), dolomite, limestone and granular activated carbon filtration, fluoride addition (0.3–0.7 mg/L), UV treatment (7.5–35.99 mJ/cm2) | Culturing (LOD: 250 CFU/L, Legionella ODR: 2.5 × 102–2.5 × 105 CFU/L) and latex agglutination assay | - |
Acanthamoeba
Vermamoeba vermiformis Echinamoeba exundans Echinamoeba thermarum Neoparamoeba |
qPCR (LOD: 2 C/L, ODR: Acanthamoeba < 2–56 C/L and V. vermiformis < 2–1670 C/L) | - | Caribbean islands, Leeward Antilles | [46] |
| Water distribution systems (mean 37.3 ± 8.4 °C) | Chloramine treatment (Chlorine contents 1.8 mg/L), flocculation, sedimentation, and dual-medium filtration | Culturing, qPCR (LOQ: 1–10 copies/reaction, maximum ODR: 13.7 ± 5.1 gc/mL) and T-RFLP | - |
Acanthamoeba
Vermamoeba vermiformis |
qPCR (LOQ: 1–10 copies/reaction, maximum ODR: Acanthamoeba 6.8 ± 2.9 gc/mL and V. vermiformis 7.1 × 104 ± 4.4 × 103 gc/mL) | High concentration of chloramine is unable to disinfect water | Southwest Virginia, USA | [47] |
| Water treatment plant (7–21 °C) | - | Multiplex PCR | - | Vermamoeba vermiformis | Culturing, light microscopy, PCR and sequencing | Amoebae were frequently detected at 17 °C | Aragon, Spain | [33] |
| Water treatment facility (25 ± 3.4–28.2 ± 1.1 °C) | - | PCR (Legionella ODR: 1.2 × 104–2.4 × 105 gc/L) and sequencing | - |
Acanthamoeba
Vermamoeba vermiformis Naegleria |
Culturing, PCR, qPCR (ODR: Acanthamoeba 2.1 × 102–7.7 × 102 gc/L and Naegleria 7.6 × 102–9.4 × 102 gc/L) and sequencing | - | Kaoping River, Taiwan | [48] |
| Sediments of municipal water storage tank (2.2–28.9 °C) | Chlorination (<4 mg/L) | qPCR (LOD: 2 CE/reaction, Legionella ODR: 51 ± 114–7.98 × 104 ± 2.49 × 104 CE/g), cloning and sequencing | SG1 |
Acanthamoeba
Vermamoeba vermiformis |
qPCR (LOD: 2 CE/reaction, ODR: Acanthamoeba 22 ± 50–391 ± 243 CE/g and V. vermiformis 17 ± 23 CE/g), cloning and sequencing | - | Northeast, East Coast, Midwest, South and West Coast, USA | [49] |
| Water distribution system | - | qPCR (LOD: 2 CE/reaction, Legionella ODR: 2 ± 4–391 ± 17 CE/L), cloning and sequencing | - |
Acanthamoeba
Acanthamoeba castellanii Vermamoeba vermiformis |
qPCR (LOD: 2 CE/reaction, ODR: Acanthamoeba 1 ± 2–16 ± 2 * CE/L and V. vermiformis 1 ± 1–9 ± 11 * CE/L), cloning and sequencing | - | USA | [50] |
| Domestic water systems (mean 20.6 ± 3.8 °C) | - | Culturing, co-culture assay, PCR and sequencing | - | Vermamoeba vermiformis | Culturing, light microscopy, PCR and sequencing | - | Geneva, Lausanne and Sion, Switzerland | [51] |
| Sediments of water storage tank | - | qPCR (ODR: 25 ± 51–300 ± 38 gn/g) and NGS | - |
Acanthamoeba
Vermamoeba vermiformis |
qPCR (ODR: Acanthamoeba 3–7 gn/g, V. vermiformis 99 ± 43–120 ± 60 gn/g) and NGS | - | Ohio, West Virginia and Texas, USA | [52] |
| Potable water | Polyaluminium chloride coagulation, sedimentation, sand and biologically activated carbon filtration and chlorination | qPCR (LOQ: 1–10 copy/reaction, minimum ODR: 3.5 log(gc)/mL) | - |
Acanthamoeba
Vermamoeba vermiformis |
qPCR (LOD: 1–10 copy/reaction, minimum ODR: 2 log(gc)/mL for V. vermiformis and 4 log(gc)/mL for Acanthamoeba) and sequencing | Antibiotics (sulfadiazine and ciprofloxacin) promote growth of both bacterium and amoebae | Northern China | [53] |
| Potable water | Polyaluminium chloride coagulation, sedimentation, sand and biologically activated carbon filtration, chlorination and ozonisation | qPCR (LOQ: 1–10 copies/reaction, minimum ODR ≈ 1 log(gc)/g) | - |
Acanthamoeba
Naegleria |
qPCR (LOQ: 1–10 copies/reaction, minimum ODR: ≈ 0.5 log(gc)/g for Naegleria and ≈ 1 log(gc)/g for Acanthamoeba) | Combined chlorination and ozonisation are effective than chlorination only | Northern China | [54] |
| Potable water | Coagulation, ozonisation, pellet softening, granular activated carbon filtration, rapid and slow sand filtration | Heterotrophic plate counts, culturing (protocol: NEN 6275, LOD: 1 log(CFU)/cm2) epifluorescence microscopy, bioluminescence assay, PCR and sequencing | - | Vermamoeba vermiformis | qPCR (ODR: 0.7–384 CE/cm2) | - | Netherlands | [55] |
| Residential secondary water supply systems (13.9 ± 4.0–17.4 ± 2.9 °C) | Chloramine treatment (Chlorine contents 0.19–0.89 mg/L) |
qPCR (LOQ: 10 copies/reaction, maximum ODR: ≈ 102 gc/mL) and sequencing | - |
Acanthamoeba
Vermamoeba vermiformis |
qPCR (LOQ: 10 copies/reaction, ODR: 101–103 gc/mL for both Acanthamoeba and V. vermiformis) and sequencing | - | Shanghai, China | [56] |
| Water treatment facility | Coagulation, sedimentation, chlorination, ozonisation, granular activated carbon and sand filtration | qPCR (LOQ: 10 copies/reaction, minimum ODR: 102 log(gc)/mL) and sequencing | - | Vermamoeba vermiformis | qPCR (LOQ: 10 copies/reaction) and sequencing | Sand filtration after granular activated carbon treatment improves water quality | Southeast China | [57] |
| Water from private wells after flood | - | Culturing (protocol: ISO 11731, LOD: 1 CFU/100 mL) and qPCR (LOQ: 9.5 gc/mL, maximum ODR: 52.4 gc/mL) | - | Naegleria fowleri | qPCR (ODR: 11–610 gc/mL) | - | Louisiana, USA | [58] |
| Potable water | - | Culturing and DVC-FISH | - |
Acanthamoeba
Vermamoeba vermiformis |
Culturing and PCR | - | Valencia, Spain | [34] |
Vermamoeba vermiformis was previously known as Hartmannella vermiform. Paravahlkampfia ustiana was previously known as Vahlkampfia ustiana. ODR: Observed detection range, the amount of bacteria/amoebae/DNA experimentally determined from the samples; CFU/L: colony forming unit/liter; PFGE: pulsed-field gel electrophoresis; PCR: polymerase chain reaction; ISO: International organization for standardization; MALDI-TOF MS: matrix assisted laser desorption ionization-time of flight mass spectrometry; qPCR: quantitative PCR; gu/L: genome unit/liter; LOQ: limit of quantification; LOD: limit of detection; EMA-qPCR: ethidium monoazide-qPCR; T-RFLP: terminal-restriction fragment length polymorphism; C/L: cells/liter; gc/mL: gene copy/milliliter; gc/L: gene copy/liter; CE/reaction: cell equivalent/reaction; CE/g: cell equivalent/gram; CE/L: cell equivalent/liter; * CE/L: cyst equivalent/liter; gn/g: genome copy number/gram; gc/g: gene copy/gram; NGS: next generation sequencing; NEN: Nederlands normalisatie instituut; CE/cm2: cell equivalent/cm2; DVC-FISH: direct viable count combined with fluorescence in situ hybridization.
Table 2.
Taxonomic description of potential protozoan hosts.
| Hospital Settings | Potable Water System |
|---|---|
| Phylum: Amoebozoa Class: Tubulinea Genera: Vermamoeba, Echinamoeba, Hartmannella, Filamoeba Class: Discosea Genera: Acanthamoeba, Comandonia, Mayorella, Vannella Class: Heterolobosea Genera: Vahlkampfia, Paravahlkampfia Phylum: Percolozoa Class: Heterolobosea Genus: Naegleria Phylum: Ciliophora Class: Oligohymenophorea Genus: Tetrahymena |
Phylum: Amoebozoa Class: Tubulinea Genera: Vermamoeba, Echinamoeba Class: Discosea Genera: Acanthamoeba, Neoparamoeba Phylum: Percolozoa Class: Heterolobosea Genus: Naegleria |
The articles from hospital settings showed that L. pneumophila Serogroup 1 (hereafter SG1) is the most common serogroup causing infection in USA and European countries. Globally, SG1 is also associated with community acquired legionellosis [29,30]. However, a limitation was that most municipal potable water supply studies did not characterize the L. pneumophila serogroups. To investigate the different L. pneumophila-protozoan interactions, some studies used co-isolation and co-culturing techniques or PCR. Other approaches included techniques like scanning electron microscopy or DVC-FISH to demonstrate the fate of internalized bacteria. The electron microscope studies conducted in hospital settings found that L. pneumophila SG1 is able to multiply inside Echinamoeba exudans [31] and Vermamoeba vermiformis (formerly Hartmannella vermiformis) [32]. Likewise, PCR-based examination of potable water also demonstrated the presence of L. pneumophila inside V. vermiformis [33]. Another study used DVC-FISH to detect intracellular L. pneumophila inside Acanthamoeba and V. vermiformis from a potable water supply [34]. Other studies (mentioned in the Table 1), demonstrated the co-existence of free-living L. pneumophila and protozoan hosts, but did not characterize the specific interaction or fate of internalized bacteria. The systematic literature review identified a more diverse number of potential protozoan hosts from hospitals compared with municipal potable water systems. This could be due to the more diverse dynamics of hospital water distributions systems (Table 2). The hosts identified in the hospital settings consisted of three phyla, five classes and twelve genera, whereas the hosts isolated from potable water consisted of only two phyla, three classes and five genera. Two genera of Amoebozoa namely, Vermamoeba and Acanthamoeba, are frequently reported from both types of facilities as potential hosts. Available literature demonstrated that non-cyst-forming and ciliated protozoans can also be potential hosts for L. pneumophila. Most of the studies were designed specifically to explore the interactions between L. pneumophila - Vermamoeba/Acanthamoeba, and the diversity and the role of other possible protozoans were not investigated.
In the studies identified, diverse physical and chemicals methods were used to disinfect the hospital and municipal potable water systems. Chlorination (<0.05–<4 mg/L) using different chlorine compounds was frequently reported as being used in both settings. Protozoans and L. pneumophila could still be isolated from both hospital and municipal potable water systems despite chlorination (<0.05–<4 mg/L), and/or ozonisation and thermal (<50–70 °C) disinfection protocols being in place. Importantly, several studies from hospital settings reported regular outbreaks of legionellosis. This represents a failure of existing disinfection protocols. The systematic literature review revealed that L. pneumophila–Acanthamoeba/Vermamoeba were extensively co-isolated from chlorinated and thermally treated water. This demonstrates the potential tolerance of L. pneumophila and protozoan hosts to survive under a wide range of disinfection conditions.
3. Discussion
The studies identified in this review have demonstrated the failure of many common disinfection protocols to achieve long term elimination of L. pneumophila from hospital and potable water supplies when protozoan hosts are present [35,38] (as mentioned in Table 1). This long term survival could be attributed to association with biofilms, inherent tolerance of L. pneumophila to high temperature and chemical disinfectants, and constant reseeding from source water [59]. However, perhaps the most interesting and undervalued relationship is the interactions with protozoan hosts. The studies identified (Table 1) are from 14 different countries, which demonstrates the need for further research to understand the L. pneumophila–protozoan interaction under different environmental conditions found globally. Proper management of legionellosis requires a better understanding of L. pneumophila–protozoan interaction, the diversity of protozoan hosts in hospital and potable water systems and the role of the host in bacterial survival under different environmental conditions.
3.1. Implications for the Control of L. pneumophila
Numerous studies have demonstrated the presence of L. pneumophila in disinfected water supplies [60,61]. An important factor enabling L. pneumophila survival in the built environment is its interaction with a protozoan host [62,63,64] (as mentioned in Table 3). Thermal treatment is one of the most common methods used to disinfect hospitals and building water supplies. In the USA [35], Germany [38] and Slovakia [41], thermal disinfection was adopted for management of nosocomial outbreaks of legionellosis. This strategy was unable to maintain water control for a long period of time [35,38] (as mentioned in Table 1). Rhoads et al. [64] reported that L. pneumophila associated with V. vermiformis can tolerate thermal (58 °C) treatment, and this disinfection protocol is unable to reduce microbial load in water. Published evidence suggests Legionella associated with Acanthamoeba are more thermos-tolerant and can survive at even higher temperatures ranging from 68–93 °C [63]. According to Steinert et al. [38] members of L. pneumophila SG1 are more thermo-tolerant than SG2. This is significant given the high number of legionellosis cases associated with L. pneumophila SG1.
Table 3.
Efficacy of available potable water disinfection protocols on Legionella pneumophila and host protozoans.
| Organisms | Disinfectant Dose | |||||
|---|---|---|---|---|---|---|
| Temperature (°C) |
Chlorine (mg-min/L) |
Monochloramine (mg-min/L) |
Chlorine Dioxide (mg-min/L) |
Ozone (mg-min/L) |
UV Rays (mJ/cm2) |
|
| Legionella pneumophila studies | ||||||
| Legionella pneumophila 1 | 70 °C [35,38] |
6 mg/L/6 h (5 log reduction) [66] |
17 (3 log reduction) [69] |
0.4 (3 log reduction) [69] |
1–2 mg/L/5 h (5 log reduction) [66] |
30 (5 log reduction) 2 [66] |
| Legionella pneumophila–potential host protozoans coculture studies | ||||||
| Legionella pneumophila Acanthamoeba coculture | 93 °C 3 [63] |
>50 mg/L [67] |
23 (3 log reduction) [69] |
2.8 (3 log reduction) [69] |
- | 10.8 (4 log reduction) [73] |
|
Legionella pneumophila Vermamoeba coculture |
58 °C [64] |
- | - | - | - | - |
| Potential host protozoans studies | ||||||
|
Acanthamoeba (trophozoite) |
65 °C/10 min (inactivation) [90] |
28 (2 log reduction) [79] |
40 (2 log reduction) [69] |
>5 (2 log reduction) [79] |
10 (3 log reduction) [82] |
72.2 (3 log reduction) [73] |
|
Acanthamoeba (cyst) |
80 °C/10 min [81] |
3500 (4 log reduction) [82] |
352 (2 log reduction) [79] |
80 (4 log reduction) [82] |
15 (4 log reduction) [82] |
800 [91] |
|
Vermamoeba (trophozoite) |
60 °C/5 min (4 log reduction) [113] |
2–4 mg/L/30 min inactivation) [78] |
- | - | - | 26 (3 log reduction) [73] |
|
Vermamoeba (cyst) |
60 °C/5 min (2 log reduction) [113] |
15 mg/L/10 min (inactivation) [83] |
- | - | - | 76.2 (3 log reduction) [73] |
|
Hartmannella (trophozoite) |
53 °C [114] |
15 (2 log reduction) [79] |
12 2 log reduction) [79] |
5 (2 log reduction) [79] |
- | - |
|
Hartmannella (cyst) |
- | 156 (2 log reduction) [79] |
34 (2 log reduction) [79] |
1 (2 log reduction) [79] |
- | - |
|
Naegleria (trophozoite) |
55 °C/15 min [89] |
5 (2 log reduction) [79] |
4–17 (2 log reduction) [88] |
1 (2 log reduction) [79] |
6.75 mg/L 30 min (3 log reduction) [84] |
24 (4 log reduction) [92] |
|
Naegleria (cyst) |
65 °C/3 min [89] |
29 (2 log reduction) [79] |
13 (2 log reduction) [79] |
5.5 (2 log reduction) [115] |
- | 121 (4 log reduction) [92] |
|
Vahlkampfia (trophozoite) |
- | 1 mg/L (inactivation) [77] |
- | - | - | - |
|
Vahlkampfia (cyst) |
- | 2 mg/L/2 h (3 log reduction) [77] |
- | - | - | - |
1 Most of the studies focus on culturable bacteria, and non-culturable cells are not estimated. 2 No further bacterial inactivation possible, 1–2 × 102 CFU/mL L. pneumophila remain stable. 3 Experiments conducted on Legionella sp.
As per WHO guidelines [65], 0.2 mg/L of free residual chlorine at point of delivery is recommended in potable water for disinfection. A pilot scale study conducted by Muraca et al. [66] demonstrated that 4 to 6 mg/L chlorine treatment for 6 h resulted in 5–6 log reduction of L. pneumophila. It was also observed that the efficacy of chlorine against Legionella was enhanced at 43 °C. However, at high temperatures a continuous flow of chlorine was required to overcome thermal decomposition. In vitro studies demonstrated higher level of tolerance to free chlorine (up to >50 mg/L) when bacteria are associated with host Acanthamoeba cysts [67]. According to Kool et al. [68], water disinfection with monochloramine resulted in a reduction of nosocomial LD outbreaks in USA. However, other studies have shown that some strains of L. pneumophila can tolerate high levels of monochloramine disinfection (17 mg-min/L for 3 log reduction) [69]. Donlan et al. [70] reported that L. pneumophila associated with amoebae in biofilm are less susceptible to chlorine and monochloramine treatment. It is also reported that monochloramine disinfection in hospital settings results in transformation of L. pneumophila vegetative cells to VBNC state [27].
According to Walker et al. [71] chlorine dioxide can effectively control L. pneumophila from hospital water system. In vitro studies demonstrated that 0.4 mg-min/L residual chlorine dioxide achieved a 3 log reduction of L. pneumophila. However, this procedure was not effective for amoebae associated L. pneumophila [69]. According to Schwartz et al. [72] Legionella biofilms on polyvinyl chloride, polyethylene and stainless steel materials can tolerate chlorine dioxide treatment. Muraca et al. [66] conducted a pilot scale study and reported that 1–2 mg/L residual concentration O3 treatment for 5 h resulted in 5 log reduction of L. pneumophila. However, half-life of ozone in water is very short, so it is difficult to maintain residual concentration in water supplies. According to Wang et al. [54], if chlorination and ozonisation is used in combination, it can target both L. pneumophila and its host protozoans effectively. In combination both treatments effectively eliminated planktonic L. pneumophila and free living Naegleria from water, whereas this combination could only reduce the population of Acanthamoeba (≈0.9 log10 gene copies/g). In comparison to chlorination alone, this combination method significantly reduced the population of L. pneumophila (≈3 log10 gene copies/g) and host amoebae (≈3 log10 Naegleria gene copies/g and ≈6.1 log10 Acanthamoeba gene copies/g) co-existing in biofilms.
UV irradiation is another method of disinfection. These radiations harbor strong genotoxic attributes. Cervero-Arago et al. [73] demonstrated that 5–6 mJ/cm2 UV dose was sufficient to achieve 4 log reduction L. pneumophila population. According to Muraca et al. [66] 30 mJ/cm2 UV rays treatment for 20 min resulted in 5 log reduction of L. pneumophila. However, continued exposure to same fluence rate for 6 h unable to eliminate all culturable L. pneumophila (1–2 × 102 CFU/mL). Schwartz et al. [72] reported that Legionella biofilms on stainless steel, polyvinyl chloride and polyethylene surfaces can tolerate UV treatment. It was also reported that amoebae associated L. pneumophila can tolerate much higher doses of UV rays [73].
3.2. Protozoan Host Control Strategies
Protozoans present in water supplies play an important role in L. pneumophila survival and resistance against disinfection protocols. Interesting, it has also been suggested that some protozoans infected by L. pneumophila have increased resistance to disinfection procedures compared to those uninfected [74]. As such, an understanding of protozoan disinfectant resistance and L.pneuophila–protozoan interactions is essential for the improved management of manufactured water systems. According to Loret et al. [75], common water chemical disinfection protocols, i.e., ozonisation (0.5 mg/L), chlorination (free chlorine 2 mg/L), electro-chlorination (free chlorine 2 mg/L), monochloramine (free chlorine 2 mg/L), chlorine dioxide (0.5 mg/L) and Cu+/Ag+ ions (0.5/0.001 mg/L) treatments, are unable to completely eliminate amoebae cysts hosting Legionella from water supplies (Table 3). These methods appear to be only effective against the free living amoebae population, as they are not feasible for targeting biofilm-associated amoebae [76]. The non-standardized approach to evaluating disinfection limits is one of the gaps in knowledge raised in the discussion section.
In vitro studies have shown 1 mg/L chlorine is sufficient to inhibit the growth of Acanthamoeba, Vermamoeba and Vahlkampfia trophozoites. Importantly, after two hours exposure, chlorine produced complete die-off of trophozoites [77]. According to Kuchta et al. [78] 2–4 mg/L chlorine treatment for 30 min can completely inactivate Vermamoeba trophozoites. Whereas, trophozoites of some strains of Hartmannella required 15 mg-min/L chlorine treatment for only 2 log reduction [79]. Mogoa et al. [80] reported that Acanthamoeba trophozoites exposed to 5 mg/L chlorine for 30 s resulted in a 3 log population reduction. It was also demonstrated that in Acanthamoeba, chlorination induces various cellular changes including reduction in cell size and alterations in cellular permeability. Dupuy et al. [79] noticed that Acanthamoeba trophozoites treated with 28 mg/L chlorine for 1 min only resulted in a 2 log reduction. In comparison with uninfected Acanthamoeba trophozoites, L. pneumophila infected Acanthamoeba trophozoites were more resistant against sodium hypochlorite (1024 mg/L) treatment [74].
Generally, inactivation of Acanthamoeba and Vermamoeba cysts required 5 mg/L chlorine, whereas for Vahlkampfia 2 mg/L chlorine treatment. It is important to note that cysts of Acanthamoeba were found highly resistant and only a 2 log reduction was noticed after eight hours exposure [77]. It was also reported that Acanthamoeba cysts can tolerate 100 mg/L of chlorine for 10 min [81]. According to Dupuy et al. [79] treatment of Acanthamoeba cysts with 856 mg-min/L results in only 2 log reduction. Loret et al. [82] reported that to achieve 4 log reduction for Acanthamoeba polyphaga cysts 3500 mg-min/L chlorine treatment is required. Likewise certain strains of Hartmannella cysts can tolerate high dose of chlorine (2 log reduction by 156 mg-min/L) [79]. Exposure of Vermamoeba cysts to 15 mg/L of chlorine for 10 min was lethal and resulted in complete inactivation [83].
Unlike Acanthamoeba and Vermamoeba, trophozoites and cysts of Naegleria were found sensitive to available disinfection protocols. Naegleria trophozoites were sensitive to 0.79 mg/L chlorine treatment for 30 min [84], whereas cysts were inactivated after exposure to 1.5 mg/L chlorine for 1 h [85]. Dupuy et al. [79] reported that chlorine treatment of Naegleria trophozoites with 5 mg-min/L resulted in only 2 log reduction and cysts can tolerate much higher levels of chlorine (29 mg-min/L for 2 log reduction). In potable water Naegleria fowleri associated with biofilms was able to tolerate 20 mg/L chlorine for 3 h [86].
In comparison to chlorine, chloramine is regarded as more stable disinfectant and capable to penetrate complex biofilms [68]. Dupuy et al. [79] suggested that instead of chlorine, monochloramine is effective chemical disinfectants against trophozoites and cysts of Acanthamoeba, Vermamoeba and Naegleria. It is possible that monochloramine harbors greater penetrating power than chlorine and easily enter in trophozoites and cysts. According to Mogoa et al. [87] monochloramine specifically targets the cell surface of Acanthamoeba. Dupuy et al. [79] identified that 352 mg-min/L monochloramine exposure resulted in 2 log reduction of Acanthamoeba cysts. Goudot et al. [88] noticed that 4–17 mg/L monochloramine exposure for 1 min only resulted in 2 log reduction of both planktonic and biofilm associated Naegleria. According to Dupuy et al. [79] to achieve 2 log reduction of Hartmannella trophozoites and cysts 12 mg-min/L and 34 mg-min/L monochloramine dose is required, respectively. Although in vitro studies demonstrate that higher concentration of chlorine-based disinfectants can inhibit the proliferation of protozoans; however, it can corrode the plumbing system pipes.
Chlorine dioxide has been shown to easily penetrate into amoeba trophozoites and cysts and specifically promotes cytoplasmic vacuolization in Acanthamoeba [87]. However the efficacy of chlorine dioxide varies from amoeba strains. The cyst form of some Acanthamoeba strains have been demonstrated to be highly tolerant to chlorine dioxide (35 mg-min/L for 2 log reduction) [79]. Loret et al. [82] demonstrated that an 80 mg-min/L dose of chlorine dioxide is required to achieve 4 log reduction of Acanthamoeba polyphaga cysts. Importantly, most studies were designed to investigate the effect of disinfection procedures on amoeba and there are limited studies on L. pneumophila-amoebae interactions during disinfection.
Ozonisation is an effective method of water disinfection. According to Cursons et al. [84], a dose of ozone 6.75 mg/L (0.08 mg/L residual level after 30 min) was sufficient to kill 99.9% (3 log reduction) trophozoites of Acanthamoeba and Naegleria. However, biofilm associated Acanthamoeba, Hartmannella, and Vahlkampfia were always found resistant to such treatments [76]. Loret et al. [82] demonstrated that 10 mg-min/L ozone dose resulted in 3 log reduction of Acanthamoeba trophozoites, however cysts retained viability.
Thermal treatment is a common physical disinfection protocol used for potable water supplies. According to Chang [89] trophozoites of Naegleria can survive at 55 °C for 15 min, whereas cysts can tolerate 65 °C for 3 min. Vermamoeba trophozoites and cysts have been shown to be completely inactivated by exposure to 60 °C for 30 min [78,83]. Thermal treatment of Acanthamoeba trophozoites and cysts at 65 °C for 10 min resulted in full inactivation [90]. Loret et al. [82] demonstrated that thermal treatment of Acanthamoeba polyphaga cysts at 65 °C for 120 min resulted in 5 log reduction. However, Storey et al. [81] reported that Acanthamoeba castellanii cysts are thermally stable and retain viability at 80 °C for 10 min. It has also been reported that thermal treatment can enhance the efficiency of chlorination. Although at high temperature (50 °C) the solubility of chlorine gas in water decreases significantly and very corrosive to pipe work, but its amoebicidal activity increases slightly [69].
UV treatment is another method of disinfection recommended by WHO. As per recommendation in 10 mJ/cm2 dose is sufficient for 99.9% (3 log) inactivation of protozoans like Giardia and Cryptosporidium [65]. According to Cervero-Arago et al. [73] to achieve 3 log reduction of V. vermiformis trophozoites 26 mJ/cm2 UV dose was required, whereas 76.2 mJ/cm2 for cysts. It was also noticed that exposure to 72.2 mJ/cm2 irradiance resulted in 3 log reduction of Acanthamoeba trophozoites [73]. Aksozek et al. [91] reported viability of Acanthamoeba castellanii cysts after exposure to high doses of UV rays (800 mJ/cm2). According to Sarkar and Gerba [92] to achieve 4 log reduction of Naegleria fowleri trophozoites and cysts 24 mJ/cm2 and 121 mJ/cm2 UV irradiance is required, respectively. A pilot scale study conducted by Langmark et al. [93] demonstrated inability of UV irradiation to reduce biofilm associated amoebae. In contrast with other protozoans, members of the Acanthamoeba genera are more resistant to both chemical and physical disinfection protocols.
As per water quality guidelines of WHO [65], 41 mg-min/L chlorine at 25 °C OR 1000 mg-min/L monochloramine at 15 °C OR 7.3 mg-min/L chlorine dioxide 25 °C OR 0.63 mg-min/L O3 at 15 °C OR 10 mJ/cm2 UV rays, treatments are required for inactivation of pathogenic protozoan (reference protozoa Giardia), as mentioned earlier in this section protozoans facilitating growth of L. pneumophila can thrive in these conditions (Table 3).
So far, studies have investigated the efficacy of water disinfection protocols against Acanthamoeba, Hartmannella, Naegleria and Vermamoeba. However, there are numerous other waterborne cyst-forming, non-cyst forming and ciliated protozoans which support the proliferation of L. pneumophila. Therefore, there is a need for more research and a standardized approach to evaluating disinfection protocol(s) that target both L. pneumophila and potential protozoan hosts. According to our literature survey, the effectiveness of available disinfection protocols depends upon the species, strain and cellular state of protozoans, as well as the type of disinfection technique and exposure time.
3.3. Detection Methods
The most commonly used methods to investigate potential L. pneumophila protozoan hosts are co-culture and co-isolation assays [19]. The co-culture assay is widely used in the laboratory to study Legionella-protozoan interactions. In this method, Legionella is allowed to grow in a protozoan host and fate of bacterium is determined microscopically [94]. In vitro laboratory studies showed that Acanthamoeba [95] and Tetrahymena [96] allow intracellular replication and packaging of live L. pneumophila into export vesicles. Other protozoan genera; Balamuthia [97], Dictyostelium [98], Echinamoeba [31], Naegleria [99], Paramecium [100], and Vermamoeba [32], facilitate intracellular replication of L. pneumophila. The second method is used to detect naturally co-existing Legionella-protozoans from environment, but microscopically it is very difficult to find protozoans containing Legionella in the natural environment [101]. As an alternative approach, a sample is screened for the presence of both Legionella and protozoan hosts. Generally, samples are screened by PCR [102,103], fluorescence in situ hybridization [104], classical culturing techniques and microscopy [105,106]. These methods are good for screening environmental samples but are unable to delineate the underlying interactions between Legionella and host protozoans. Nowadays, PCR based protocols are widely used to detect L. pneumophila and protozoan hosts from engineered water systems. In comparison to classical culturing methods, these protocols are rapid and highly sensitive. However, most of the nucleic acid-based protocols are unable to differentiate viable and dead organisms. Propidium monoazide-PCR or ethidium monoazide-PCR are modified nucleic acid detection protocols to enumerate the live bacteria [107,108] and protozoan hosts [109,110]. To estimate burden of L. pneumophila and protozoan hosts in water distribution system, it is necessary to measure the quantity of alive and dead organisms regularly. This literature review demonstrates that Vermamoeba and Acanthamoeba are predominant hosts of L. pneumophila in the context of hospital and potable water systems. Many cyst-forming, non-cyst forming and ciliated protozoans have been found associated with L. pneumophila and are identified as potential hosts; however, in vitro co-culture assays and microscopic studies are required for confirmation and characterization of this interaction.
During stress (i.e., thermal, nutrient, chemical and radiation), L. pneumophila can enter into a VBNC state. After the end of such a stress period, in presence of a suitable host or favorable environmental conditions, the VBNC state can transform back into metabolically active cellular state [111]. Importantly, the underlying mechanisms of resuscitation from VBNC are not yet well understood. However, as the VBNC form is by definition a non-culturable state, classical microbiology culturing techniques cannot be used to monitor viability. Thus, in vitro co-culture assays can be used to resuscitate VBNC in the laboratory [74]. Alternative approaches to analyze VBNC are the analysis of membrane integrity and molecular screening [112]. There are also studies that have shown that intracellular replication of L. pneumophila induces VBNC state. According to Buse et al. [26] transformation of V. vermiformis trophozoites into cysts promotes biogenesis of VBNC L. pneumophila. Therefore, the interaction with protozoan hosts may also affect the ability to monitor the efficacy of disinfection protocols against L. pneumophila, because the bacteria may be in the VBNC form. Available literature only discusses disinfection protocols, which target culturable L. pneumophila. To our knowledge, there are limited studies investigating the effectiveness of disinfection protocols to eliminate VBNC L. pneumophila. It is our suggestion to adopt membrane integrity and in vitro co-culture assays to evaluate the disinfection procedure against VBNC L. pneumophila.
4. Materials and Methods
The databases Scopus and Web of Science were searched for articles written in English containing the keywords (“Legionella pneumophila” OR “L. pneumophila”) AND (Acanthamoeba OR Vermamoeba OR Hartmannella OR Dictyostelium OR Naegleria OR Tetrahymena OR Echinamoeba OR Paramecium OR Balamuthia OR Oxytricha OR Stylonychia OR Diphylleia OR Stenamoeba OR Singhamoeba OR Filamoeba OR Protozoa OR Protozoan OR Amoeba). The above search terms were modified from the review conducted by Boamah et al. [19]. Figure 1 presents the systematic approach to article inclusion or exclusion. Articles were screened by reading the titles and abstracts and initially excluded if they did not refer to a study that detected L. pneumophila and a potential protozoan host from a hospital or potable/drinking water source. Articles were then read in full and excluded if they only described laboratory based simulated or pilot-scale experiments on registered bacterial and protozoan strains.
5. Conclusions
Protozoans present in potable water play an important role in L. pneumophila survival. Further research is needed to better understand L. pneumophila-protozoan interactions and the implications for the prevention of Legionnaires’ disease. To achieve long term disinfection of a water system the control protocols need to be effective against potential hosts harboring L. pneumophila. Additionally, an understanding of the mechanisms of VBNC state transformation, and the role of protozoans in this, is needed to effectively evaluate the efficacy of disinfection techniques.
Author Contributions
M.A.N. and H.W. drafted and edited the manuscript, H.W., K.E.R., M.H.B. and R.B. corrected and contributed to the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Cunha B.A., Burillo A., Bouza E. Legionnaires’ disease. Lancet. 2016;387:376–385. doi: 10.1016/S0140-6736(15)60078-2. [DOI] [PubMed] [Google Scholar]
- 2.The European Legionnaires’ Disease Surveillance Network. The European Centre for Disease Prevention and Control Surveillance Atlas of Infectious Diseases. [(accessed on 4 October 2019)]; Available online: https://atlas.ecdc.europa.eu/public/index.aspx.
- 3.Smith P., Moore M., Alexander N., Hicks L., O’Loughlin R. Surveillance for travel-associated Legionnaires disease-United States, 2005–2006. Mmwr-Morb Mortal Wkly. Rep. 2007;56:1261–1263. [PubMed] [Google Scholar]
- 4.National Notifiable Diseases Surveillance System. Centers for Disease Control and Prevention . National Notifiable Infectious Diseases: Weekly Tables. Centers for Disease Control and Prevention; Atlanta, GA, USA: 2018. National Notifiable Diseases Surveillance System. [Google Scholar]
- 5.Phin N., Parry-Ford F., Harrison T., Stagg H.R., Zhang N., Kumar K., Lortholary O., Zumla A., Abubakar I. Epidemiology and clinical management of Legionnaires’ disease. Lancet Infect. Dis. 2014;14:1011–1021. doi: 10.1016/S1473-3099(14)70713-3. [DOI] [PubMed] [Google Scholar]
- 6.O’Mahony M.C., Stanwell-Smith R.E., Tillett H.E., Harper D., Hutchison J.G., Farrell I.D., Hutchinson D.N., Lee J.V., Dennis P.J., Duggal H.V., et al. The Stafford outbreak of Legionnaires’ disease. Epidemiol. Infect. 1990;104:361–380. doi: 10.1017/S0950268800047385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Soda E.A. Vital Signs: Health care–associated Legionnaires’ disease surveillance data from 20 states and a large metropolitan area-United States, 2015. Mmwr-Morb Mortal Wkly. Rep. 2017;66:584–589. doi: 10.15585/mmwr.mm6622e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mercante J.W., Winchell J.M. Current and emerging Legionella diagnostics for laboratory and outbreak investigations. Clin. Microbiol. Rev. 2015;28:95–133. doi: 10.1128/CMR.00029-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miyashita N., Higa F., Aoki Y., Kikuchi T., Seki M., Tateda K., Maki N., Uchino K., Ogasawara K., Kiyota H., et al. Distribution of Legionella species and serogroups in patients with culture-confirmed Legionella pneumonia. J. Infect. Chemother. 2020 doi: 10.1016/j.jiac.2019.12.016. [DOI] [PubMed] [Google Scholar]
- 10.Bartram J., Chartier Y., Lee J.V., Pond K., Surman-Lee S. Legionella and the Prevention of Legionellosis. World Health Organization; Geneva, Switzerland: 2007. [Google Scholar]
- 11.NNDSS Annual Report Working Group Australia’s notifiable disease status, 2015: Annual report of the national notifiable diseases surveillance system. Commun. Dis. Intel. (2018) 2019;43 doi: 10.33321/cdi.2019.43.6. [DOI] [PubMed] [Google Scholar]
- 12.Graham F.F., White P.S., Harte D.J., Kingham S.P. Changing epidemiological trends of legionellosis in New Zealand, 1979–2009. Epidemiol. Infect. 2012;140:1481–1496. doi: 10.1017/S0950268811000975. [DOI] [PubMed] [Google Scholar]
- 13.Benedict K.M. Surveillance for waterborne disease outbreaks associated with drinking water—United States, 2013–2014. Mmwr.-Morb. Mortal Wkly. Rep. 2017;66:1216. doi: 10.15585/mmwr.mm6644a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abdel-Nour M., Duncan C., Low D.E., Guyard C. Biofilms: The stronghold of Legionella pneumophila. Int. J. Mol. Sci. 2013;14:21660. doi: 10.3390/ijms141121660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liu Z., Lin Y.E., Stout J.E., Hwang C.C., Vidic R.D., Yu V.L. Effect of flow regimes on the presence of Legionella within the biofilm of a model plumbing system. J. Appl. Microbiol. 2006;101:437–442. doi: 10.1111/j.1365-2672.2006.02970.x. [DOI] [PubMed] [Google Scholar]
- 16.Prussin A.J., 2nd, Schwake D.O., Marr L.C. Ten questions concerning the aerosolization and transmission of Legionella in the built environment. Build. Environ. 2017;123:684–695. doi: 10.1016/j.buildenv.2017.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ashbolt N.J. Environmental (Saprozoic) Pathogens of Engineered Water Systems: Understanding Their Ecology for Risk Assessment and Management. Pathogens. 2015;4:390. doi: 10.3390/pathogens4020390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Falkinham J.O., Pruden A., Edwards M. Opportunistic premise plumbing pathogens: Increasingly important pathogens in drinking water. Pathogens. 2015;4:373. doi: 10.3390/pathogens4020373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boamah D.K., Zhou G., Ensminger A.W., O’Connor T.J. From many hosts, one accidental pathogen: The diverse protozoan hosts of Legionella. Front. Cell Infect. Microbiol. 2017;7:477. doi: 10.3389/fcimb.2017.00477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Newton H.J., Ang D.K., van Driel I.R., Hartland E.L. Molecular pathogenesis of infections caused by Legionella pneumophila. Clin. Microbiol. Rev. 2010;23:274–298. doi: 10.1128/CMR.00052-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oliva G., Sahr T., Buchrieser C. The Life Cycle of L. pneumophila: Cellular Differentiation Is Linked to Virulence and Metabolism. Front. Cell Infect. Microbiol. 2018;8:3. doi: 10.3389/fcimb.2018.00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bouyer S., Imbert C., Rodier M.H., Hechard Y. Long-term survival of Legionella pneumophila associated with Acanthamoeba castellanii vesicles. Environ. Microbiol. 2007;9:1341–1344. doi: 10.1111/j.1462-2920.2006.01229.x. [DOI] [PubMed] [Google Scholar]
- 23.Koubar M., Rodier M.H., Garduno R.A., Frere J. Passage through Tetrahymena tropicalis enhances the resistance to stress and the infectivity of Legionella pneumophila. Fems Microbiol. Lett. 2011;325:10–15. doi: 10.1111/j.1574-6968.2011.02402.x. [DOI] [PubMed] [Google Scholar]
- 24.Jjemba P.K., Johnson W., Bukhari Z., LeChevallier M.W. Occurrence and control of Legionella in recycled water systems. Pathogens. 2015;4:470. doi: 10.3390/pathogens4030470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim B.R., Anderson J.E., Mueller S.A., Gaines W.A., Kendall A.M. Literature review--efficacy of various disinfectants against Legionella in water systems. Water Res. 2002;36:4433–4444. doi: 10.1016/S0043-1354(02)00188-4. [DOI] [PubMed] [Google Scholar]
- 26.Buse H.Y., Donohue M.J., Ashbolt N.J. Hartmannella vermiformis inhibition of Legionella pneumophila cultivability. Microb. Ecol. 2013;66:715–726. doi: 10.1007/s00248-013-0250-z. [DOI] [PubMed] [Google Scholar]
- 27.Casini B., Baggiani A., Totaro M., Mansi A., Costa A.L., Aquino F., Miccoli M., Valentini P., Bruschi F., Lopalco P.L., et al. Detection of viable but non-culturable Legionella in hospital water network following monochloramine disinfection. J. Hosp. Infect. 2018;98:46–52. doi: 10.1016/j.jhin.2017.09.006. [DOI] [PubMed] [Google Scholar]
- 28.Thomas J.M., Ashbolt N.J. Do free-living amoebae in treated drinking water systems present an emerging health risk? Environ. Sci. Technol. 2011;45:860–869. doi: 10.1021/es102876y. [DOI] [PubMed] [Google Scholar]
- 29.Yu V.L., Plouffe J.F., Pastoris M.C., Stout J.E., Schousboe M., Widmer A., Summersgill J., File T., Heath C.M., Paterson D.L., et al. Distribution of Legionella species and serogroups isolated by culture in patients with sporadic community-acquired legionellosis: An international collaborative survey. J. Infect. Dis. 2002;186:127–128. doi: 10.1086/341087. [DOI] [PubMed] [Google Scholar]
- 30.Beaute J., Zucs P., de Jong B., European Legionnaires’ Disease Surveillance Network Legionnaires disease in Europe, 2009–2010. Euro Surveill. 2013;18:20417. doi: 10.2807/ese.18.10.20417-en. [DOI] [PubMed] [Google Scholar]
- 31.Fields B.S., Sanden G.N., Barbaree J.M., Morrill W.E., Wadowsky R.M., White E.H., Feeley J.C. Intracellular multiplication of Legionella pneumophila in amoebae isolated from hospital hot water tanks. Curr. Microbiol. 1989;18:131–137. doi: 10.1007/BF01570838. [DOI] [Google Scholar]
- 32.Nahapetian K., Challemel O., Beurtin D., Dubrou S., Gounon P., Squinazi F. The intracellular multiplication of Legionella pneumophila in protozoa from hospital plumbing systems. Res. Microbiol. 1991;142:677–685. doi: 10.1016/0923-2508(91)90081-K. [DOI] [PubMed] [Google Scholar]
- 33.Garcia A., Goni P., Cieloszyk J., Fernandez M.T., Calvo-Begueria L., Rubio E., Fillat M.F., Peleato M.L., Clavel A. Identification of free-living amoebae and amoeba-associated bacteria from reservoirs and water treatment plants by molecular techniques. Environ. Sci. Technol. 2013;47:3132–3140. doi: 10.1021/es400160k. [DOI] [PubMed] [Google Scholar]
- 34.Moreno Y., Moreno-Mesonero L., Garcia-Hernandez J. DVC-FISH to identify potentially pathogenic Legionella inside free-living amoebae from water sources. Environ. Res. 2019;176:108521. doi: 10.1016/j.envres.2019.06.002. [DOI] [PubMed] [Google Scholar]
- 35.Breiman R.F., Fields B.S., Sanden G.N., Volmer L., Meier A., Spika J.S. Association of shower use with Legionnaires’ disease-possible role of ameobas. JAMA-J. Am. Med. Assoc. 1990;263:2924–2926. doi: 10.1001/jama.1990.03440210074036. [DOI] [PubMed] [Google Scholar]
- 36.Bezanson G., Burbridge S., Haldane D., Yoell C., Marrie T. Diverse populations of Legionella pneumophila present in the water of geographically clustered institutions served by the same water reservoir. J. Clin. Microbiol. 1992;30:570–576. doi: 10.1128/JCM.30.3.570-576.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Patterson W.J., Hay J., Seal D.V., McLuckie J.C. Colonization of transplant unit water supplies with Legionella and protozoa: Precautions required to reduce the risk of legionellosis. J. Hosp. Infect. 1997;37:7–17. doi: 10.1016/S0195-6701(97)90068-2. [DOI] [PubMed] [Google Scholar]
- 38.Steinert M., Ockert G., Luck C., Hacker J. Regrowth of Legionella pneumophila in a heat-disinfected plumbing system. Zent. Bakteriol. 1998;288:331–342. doi: 10.1016/S0934-8840(98)80005-4. [DOI] [PubMed] [Google Scholar]
- 39.Thomas V., Herrera-Rimann K., Blanc D.S., Greub G. Biodiversity of amoebae and amoeba-resisting bacteria in a hospital water network. Appl. Environ. Microbiol. 2006;72:2428–2438. doi: 10.1128/AEM.72.4.2428-2438.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lagana P., Caruso G., Piccione D., Gioffre M.E., Pino R., Delia S. Legionella spp., amoebae and not-fermenting Gram negative bacteria in an Italian university hospital water system. Ann. Agric. Environ. Med. 2014;21:489–493. doi: 10.5604/12321966.1120623. [DOI] [PubMed] [Google Scholar]
- 41.Trnkova K., Kotrbancova M., Spalekova M., Fulova M., Boledovicova J., Vesteg M. MALDI-TOF MS analysis as a useful tool for an identification of Legionella pneumophila, a facultatively pathogenic bacterium interacting with free-living amoebae: A case study from water supply system of hospitals in Bratislava (Slovakia) Exp. Parasitol. 2018;184:97–102. doi: 10.1016/j.exppara.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 42.Muchesa P., Leifels M., Jurzik L., Barnard T.G., Bartie C. Detection of amoeba-associated Legionella pneumophila in hospital water networks of Johannesburg. S. Afr J. Infect. D. 2018;33:72–75. doi: 10.4102/sajid.v33i3.8. [DOI] [Google Scholar]
- 43.Spagnolo A.M., Sartini M., Cave D.D., Casini B., Tuvo B., Cristina M.L. Evaluation of microbiological and free-living protozoa contamination in dental unit waterlines. Int. J. Environ. Res. Public Health. 2019;16:2468. doi: 10.3390/ijerph16152648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Valster R.M., Wullings B.A., Bakker G., Smidt H., van der Kooij D. Free-living protozoa in two unchlorinated drinking water supplies, identified by phylogenic analysis of 18S rRNA gene sequences. Appl. Environ. Microbiol. 2009;75:4736–4746. doi: 10.1128/AEM.02629-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Valster R.M., Wullings B.A., van der Kooij D. Detection of protozoan hosts for Legionella pneumophila in engineered water systems by using a biofilm batch test. Appl. Environ. Microbiol. 2010;76:7144–7153. doi: 10.1128/AEM.00926-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Valster R.M., Wullings B.A., van den Berg R., van der Kooij D. Relationships between free-living protozoa, cultivable Legionella spp., and water quality characteristics in three drinking water supplies in the Caribbean. Appl. Environ. Microbiol. 2011;77:7321–7328. doi: 10.1128/AEM.05575-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wang H., Edwards M., Falkinham J.O., 3rd, Pruden A. Molecular survey of the occurrence of Legionella spp., Mycobacterium spp., Pseudomonas aeruginosa, and amoeba hosts in two chloraminated drinking water distribution systems. Appl. Environ. Microbiol. 2012;78:6285–6294. doi: 10.1128/AEM.01492-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ji W.T., Hsu B.M., Chang T.Y., Hsu T.K., Kao P.M., Huang K.H., Tsai S.F., Huang Y.L., Fan C.W. Surveillance and evaluation of the infection risk of free-living amoebae and Legionella in different aquatic environments. Sci. Total Environ. 2014;499:212–219. doi: 10.1016/j.scitotenv.2014.07.116. [DOI] [PubMed] [Google Scholar]
- 49.Lu J., Struewing I., Yelton S., Ashbolt N. Molecular survey of occurrence and quantity of Legionella spp., Mycobacterium spp., Pseudomonas aeruginosa and amoeba hosts in municipal drinking water storage tank sediments. J. Appl. Microbiol. 2015;119:278–288. doi: 10.1111/jam.12831. [DOI] [PubMed] [Google Scholar]
- 50.Lu J., Struewing I., Vereen E., Kirby A.E., Levy K., Moe C., Ashbolt N. Molecular Detection of Legionella spp. and their associations with Mycobacterium spp., Pseudomonas aeruginosa and amoeba hosts in a drinking water distribution system. J. Appl. Microbiol. 2016;120:509–521. doi: 10.1111/jam.12996. [DOI] [PubMed] [Google Scholar]
- 51.Lienard J., Croxatto A., Gervaix A., Levi Y., Loret J.F., Posfay-Barbe K.M., Greub G. Prevalence and diversity of Chlamydiales and other amoeba-resisting bacteria in domestic drinking water systems. New Microbes New Infect. 2017;15:107–116. doi: 10.1016/j.nmni.2016.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Qin K., Struewing I., Domingo J.S., Lytle D., Lu J. Opportunistic pathogens and microbial communities and their associations with sediment physical parameters in drinking water storage tank sediments. Pathogens. 2017;6:54. doi: 10.3390/pathogens6040054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang H., Shen Y., Hu C., Xing X., Zhao D. Sulfadiazine/ciprofloxacin promote opportunistic pathogens occurrence in bulk water of drinking water distribution systems. Environ. Pollut. 2018;234:71–78. doi: 10.1016/j.envpol.2017.11.050. [DOI] [PubMed] [Google Scholar]
- 54.Wang H., Hu C., Zhang S., Liu L., Xing X. Effects of O3/Cl2 disinfection on corrosion and opportunistic pathogens growth in drinking water distribution systems. J. Environ. Sci. (China) 2018;73:38–46. doi: 10.1016/j.jes.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 55.Van der Kooij D., Veenendaal H.R., Italiaander R., van der Mark E.J., Dignum M. Primary colonizing Betaproteobacteriales play a key role in the growth of Legionella pneumophila in biofilms on surfaces exposed to drinking water treated by slow sand filtration. Appl. Environ. Microbiol. 2018;84:e01732–e01818. doi: 10.1128/AEM.01732-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li H., Li S., Tang W., Yang Y., Zhao J., Xia S., Zhang W., Wang H. Influence of secondary water supply systems on microbial community structure and opportunistic pathogen gene markers. Water Res. 2018;136:160–168. doi: 10.1016/j.watres.2018.02.031. [DOI] [PubMed] [Google Scholar]
- 57.Wang H., Xu J., Tang W., Li H., Xia S., Zhao J., Zhang W., Yang Y. Removal efficacy of opportunistic pathogens and bacterial community dynamics in two drinking water treatment trains. Small. 2019;15:1804436. doi: 10.1002/smll.201804436. [DOI] [PubMed] [Google Scholar]
- 58.Dai D.J., Rhoads W.J., Katner A., Strom L., Edwards M.A., Pruden A., Pieper K.J. Molecular survey of Legionella and Naegleria fowleri in private well water and premise plumbing following the 2016 Louisiana flood. Environ. Sci.-Wat. Res. 2019;5:1464–1477. doi: 10.1039/C9EW00109C. [DOI] [Google Scholar]
- 59.Lau H.Y., Ashbolt N.J. The role of biofilms and protozoa in Legionella pathogenesis: Implications for drinking water. J. Appl. Microbiol. 2009;107:368–378. doi: 10.1111/j.1365-2672.2009.04208.x. [DOI] [PubMed] [Google Scholar]
- 60.Lin Y.S., Stout J.E., Yu V.L., Vidic R.D. Disinfection of water distribution systems for Legionella. Semin. Respir. Infect. 1998;13:147–159. [PubMed] [Google Scholar]
- 61.Whiley H., Bentham R., Brown M.H. Legionella persistence in manufactured water systems: Pasteurization potentially selecting for thermal tolerance. Front. Microbiol. 2017;8:1330. doi: 10.3389/fmicb.2017.01330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Fields B.S., Benson R.F., Besser R.E. Legionella and Legionnaires’ disease: 25 years of investigation. Clin. Microbiol. Rev. 2002;15:506–526. doi: 10.1128/CMR.15.3.506-526.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Dobrowsky P.H., Khan S., Cloete T.E., Khan W. Molecular detection of Acanthamoeba spp., Naegleria fowleri and Vermamoeba (Hartmannella) vermiformis as vectors for Legionella spp. in untreated and solar pasteurized harvested rainwater. Parasit. Vectors. 2016;9:539. doi: 10.1186/s13071-016-1829-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rhoads W.J., Ji P., Pruden A., Edwards M.A. Water heater temperature set point and water use patterns influence Legionella pneumophila and associated microorganisms at the tap. Microbiome. 2015;3:67. doi: 10.1186/s40168-015-0134-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.World Health Organization . Guidelines for Drinking-Water Quality. WHO; Geneva, Switzerland: 2004. [Google Scholar]
- 66.Muraca P., Stout J.E., Yu V.L. Comparative assessment of chlorine, heat, ozone, and UV light for killing Legionella pneumophila within a model plumbing system. Appl. Environ. Microbiol. 1987;53:447–453. doi: 10.1128/AEM.53.2.447-453.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kilvington S., Price J. Survival of Legionella pneumophila within cysts of Acanthamoeba polyphaga following chlorine exposure. J. Appl. Bacteriol. 1990;68:519–525. doi: 10.1111/j.1365-2672.1990.tb02904.x. [DOI] [PubMed] [Google Scholar]
- 68.Kool J.L., Carpenter J.C., Fields B.S. Effect of monochloramine disinfection of municipal drinking water on risk of nosocomial Legionnaires’ disease. Lancet. 1999;353:272–277. doi: 10.1016/S0140-6736(98)06394-6. [DOI] [PubMed] [Google Scholar]
- 69.Dupuy M., Mazoua S., Berne F., Bodet C., Garrec N., Herbelin P., Menard-Szczebara F., Oberti S., Rodier M.H., Soreau S., et al. Efficiency of water disinfectants against Legionella pneumophila and Acanthamoeba. Water Res. 2011;45:1087–1094. doi: 10.1016/j.watres.2010.10.025. [DOI] [PubMed] [Google Scholar]
- 70.Donlan R.M., Forster T., Murga R., Brown E., Lucas C., Carpenter J., Fields B. Legionella pneumophila associated with the protozoan Hartmannella vermiformis in a model multi-species biofilm has reduced susceptibility to disinfectants. Biofouling. 2005;21:1–7. doi: 10.1080/08927010500044286. [DOI] [PubMed] [Google Scholar]
- 71.Walker J.T., Mackerness C.W., Mallon D., Makin T., Williets T., Keevil C.W. Control of Legionella pneumophila in a hospital water system by chlorine dioxide. J. Ind. Microbiol. 1995;15:384–390. doi: 10.1007/BF01569995. [DOI] [PubMed] [Google Scholar]
- 72.Schwartz T., Hoffmann S., Obst U. Formation of natural biofilms during chlorine dioxide and UV disinfection in a public drinking water distribution system. J. Appl. Microbiol. 2003;95:591–601. doi: 10.1046/j.1365-2672.2003.02019.x. [DOI] [PubMed] [Google Scholar]
- 73.Cervero-Arago S., Sommer R., Araujo R.M. Effect of UV irradiation (253.7 nm) on free Legionella and Legionella associated with its amoebae hosts. Water Res. 2014;67:299–309. doi: 10.1016/j.watres.2014.09.023. [DOI] [PubMed] [Google Scholar]
- 74.Garcia M.T., Jones S., Pelaz C., Millar R.D., Abu Kwaik Y. Acanthamoeba polyphaga resuscitates viable non-culturable Legionella pneumophila after disinfection. Environ. Microbiol. 2007;9:1267–1277. doi: 10.1111/j.1462-2920.2007.01245.x. [DOI] [PubMed] [Google Scholar]
- 75.Loret J.F., Robert S., Thomas V., Cooper A.J., McCoy W.F., Levi Y. Comparison of disinfectants for biofilm, protozoa and Legionella control. J. Water Health. 2005;3:423–433. doi: 10.2166/wh.2005.047. [DOI] [PubMed] [Google Scholar]
- 76.Thomas V., Bouchez T., Nicolas V., Robert S., Loret J.F., Levi Y. Amoebae in domestic water systems: Resistance to disinfection treatments and implication in Legionella persistence. J. Appl. Microbiol. 2004;97:950–963. doi: 10.1111/j.1365-2672.2004.02391.x. [DOI] [PubMed] [Google Scholar]
- 77.Critchley M., Bentham R. The efficacy of biocides and other chemical additives in cooling water systems in the control of amoebae. J. Appl. Microbiol. 2009;106:784–789. doi: 10.1111/j.1365-2672.2008.04044.x. [DOI] [PubMed] [Google Scholar]
- 78.Kuchta J.M., Navratil J.S., Shepherd M.E., Wadowsky R.M., Dowling J.N., States S.J., Yee R.B. Impact of chlorine and heat on the survival of Hartmannella vermiformis and subsequent growth of Legionella pneumophila. Appl. Environ. Microbiol. 1993;59:4096–4100. doi: 10.1128/AEM.59.12.4096-4100.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Dupuy M., Berne F., Herbelin P., Binet M., Berthelot N., Rodier M.H., Soreau S., Hechard Y. Sensitivity of free-living amoeba trophozoites and cysts to water disinfectants. Int. J. Hyg. Environ. Health. 2014;217:335–339. doi: 10.1016/j.ijheh.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 80.Mogoa E., Bodet C., Legube B., Hechard Y. Acanthamoeba castellanii: Cellular changes induced by chlorination. Exp. Parasitol. 2010;126:97–102. doi: 10.1016/j.exppara.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 81.Storey M.V., Winiecka-Krusnell J., Ashbolt N.J., Stenstrom T.A. The efficacy of heat and chlorine treatment against thermotolerant Acanthamoebae and Legionellae. Scand. J. Infect. Dis. 2004;36:656–662. doi: 10.1080/00365540410020785. [DOI] [PubMed] [Google Scholar]
- 82.Loret J., Jousset M., Robert S., Anselme C., Saucedo G., Ribas F., Martinez L., Catalan V. Elimination of free-living amoebae by drinking water treatment processes. Eur. J. Water Qual. 2008;39:37–50. doi: 10.1051/wqual/2008011. [DOI] [Google Scholar]
- 83.Fouque E., Hechard Y., Hartemann P., Humeau P., Trouilhe M.C. Sensitivity of Vermamoeba (Hartmannella) vermiformis cysts to conventional disinfectants and protease. J. Water Health. 2015;13:302–310. doi: 10.2166/wh.2014.154. [DOI] [PubMed] [Google Scholar]
- 84.Cursons R.T., Brown T.J., Keys E.A. Effect of disinfectants on pathogenic free-living amoebae: In axenic conditions. Appl. Environ. Microbiol. 1980;40:62–66. doi: 10.1128/AEM.40.1.62-66.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.De Jonckheere J., van de Voorde H. Differences in destruction of cysts of pathogenic and nonpathogenic Naegleria and Acanthamoeba by chlorine. Appl. Environ. Microbiol. 1976;31:294–297. doi: 10.1128/AEM.31.2.294-297.1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Miller H.C., Wylie J., Dejean G., Kaksonen A.H., Sutton D., Braun K., Puzon G.J. Reduced efficiency of chlorine disinfection of Naegleria fowleri in a drinking water distribution biofilm. Environ. Sci. Technol. 2015;49:11125–11131. doi: 10.1021/acs.est.5b02947. [DOI] [PubMed] [Google Scholar]
- 87.Mogoa E., Bodet C., Morel F., Rodier M.H., Legube B., Hechard Y. Cellular response of the amoeba Acanthamoeba castellanii to chlorine, chlorine dioxide, and monochloramine treatments. Appl. Environ. Microbiol. 2011;77:4974–4980. doi: 10.1128/AEM.00234-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Goudot S., Herbelin P., Mathieu L., Soreau S., Banas S., Jorand F.P. Biocidal efficacy of monochloramine against planktonic and biofilm-associated Naegleria fowleri cells. J. Appl. Microbiol. 2014;116:1055–1065. doi: 10.1111/jam.12429. [DOI] [PubMed] [Google Scholar]
- 89.Chang S.L. Resistance of pathogenic Naegleria to some common physical and chemical agents. Appl. Environ. Microbiol. 1978;35:368–375. doi: 10.1128/AEM.35.2.368-375.1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Coulon C., Collignon A., McDonnell G., Thomas V. Resistance of Acanthamoeba cysts to disinfection treatments used in health care settings. J. Clin. Microbiol. 2010;48:2689–2697. doi: 10.1128/JCM.00309-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Aksozek A., McClellan K., Howard K., Niederkorn J.Y., Alizadeh H. Resistance of Acanthamoeba castellanii cysts to physical, chemical, and radiological conditions. J. Parasitol. 2002;88:621–623. doi: 10.1645/0022-3395(2002)088[0621:ROACCT]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 92.Sarkar P., Gerba C.P. Inactivation of Naegleria fowleri by chlorine and ultraviolet light. J. Am. Water Work Assoc. 2012;104:E173–E180. doi: 10.5942/jawwa.2012.104.0041. [DOI] [Google Scholar]
- 93.Langmark J., Storey M.V., Ashbolt N.J., Stenstrom T.A. The effects of UV disinfection on distribution pipe biofilm growth and pathogen incidence within the greater Stockholm area, Sweden. Water Res. 2007;41:3327–3336. doi: 10.1016/j.watres.2007.04.024. [DOI] [PubMed] [Google Scholar]
- 94.Dietersdorfer E., Cervero-Arago S., Sommer R., Kirschner A.K., Walochnik J. Optimized methods for Legionella pneumophila release from its Acanthamoeba hosts. BMC Microbiol. 2016;16:74. doi: 10.1186/s12866-016-0691-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Berk S.G., Ting R.S., Turner G.W., Ashburn R.J. Production of respirable vesicles containing live Legionella pneumophila cells by two Acanthamoeba spp. Appl. Environ. Microbiol. 1998;64:279–286. doi: 10.1128/AEM.64.1.279-286.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Berk S.G., Faulkner G., Garduno E., Joy M.C., Ortiz-Jimenez M.A., Garduno R.A. Packaging of live Legionella pneumophila into pellets expelled by Tetrahymena spp. does not require bacterial replication and depends on a Dot/Icm-mediated survival mechanism. Appl. Environ. Microbiol. 2008;74:2187–2199. doi: 10.1128/AEM.01214-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Shadrach W.S., Rydzewski K., Laube U., Holland G., Ozel M., Kiderlen A.F., Flieger A. Balamuthia mandrillaris, free-living ameba and opportunistic agent of encephalitis, is a potential host for Legionella pneumophila bacteria. Appl. Environ. Microbiol. 2005;71:2244–2249. doi: 10.1128/AEM.71.5.2244-2249.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Solomon J.M., Rupper A., Cardelli J.A., Isberg R.R. Intracellular growth of Legionella pneumophila in Dictyostelium discoideum, a system for genetic analysis of host-pathogen interactions. Infect. Immun. 2000;68:2939–2947. doi: 10.1128/IAI.68.5.2939-2947.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Newsome A.L., Baker R.L., Miller R.D., Arnold R.R. Interactions between Naegleria fowleri and Legionella pneumophila. Infect. Immun. 1985;50:449–452. doi: 10.1128/IAI.50.2.449-452.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Watanabe K., Nakao R., Fujishima M., Tachibana M., Shimizu T., Watarai M. Ciliate Paramecium is a natural reservoir of Legionella pneumophila. Sci. Rep. 2016;6:24322. doi: 10.1038/srep24322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kao P.M., Tung M.C., Hsu B.M., Hsu S.Y., Huang J.T., Liu J.H., Huang Y.L. Differential Legionella spp. survival between intracellular and extracellular forms in thermal spring environments. Environ. Sci. Pollut. Res. Int. 2013;20:3098–3106. doi: 10.1007/s11356-012-1159-7. [DOI] [PubMed] [Google Scholar]
- 102.International Organization for Standardization . ISO/TS12869:2019 Water Quality-Detection and Quantification of LEGIONELLA spp. and/or Legionella pneumophila by Concentration and Genic amplification by Quantitative Polymerase Chain Reaction (qPCR) International Organization for Standardization; Geneva, Switzerland: 2019. [Google Scholar]
- 103.Qvarnstrom Y., Visvesvara G.S., Sriram R., da Silva A.J. Multiplex real-time PCR assay for simultaneous detection of Acanthamoeba spp., Balamuthia mandrillaris, and Naegleria fowleri. J. Clin. Microbiol. 2006;44:3589–3595. doi: 10.1128/JCM.00875-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Whiley H., Taylor M., Bentham R. Detection of Legionella species in potting mixes using fluorescent in situ hybridisation (FISH) J. Microbiol. Methods. 2011;86:304–309. doi: 10.1016/j.mimet.2011.05.023. [DOI] [PubMed] [Google Scholar]
- 105.Health Protection Agency . Isolation and Identification of Acanthamoeba Species. Health Protection Agency; London, UK: 2004. [Google Scholar]
- 106.Standards Australia . AS5132:2017 Waters-Examination for Legionella spp. Includeing Legionella Pneumophila-Using Concentration. Standards Australia; Sydney, Australia: 2017. [Google Scholar]
- 107.Nocker A., Cheung C.Y., Camper A.K. Comparison of propidium monoazide with ethidium monoazide for differentiation of live vs. dead bacteria by selective removal of DNA from dead cells. J. Microbiol. Methods. 2006;67:310–320. doi: 10.1016/j.mimet.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 108.Yanez M.A., Nocker A., Soria-Soria E., Murtula R., Martinez L., Catalan V. Quantification of viable Legionella pneumophila cells using propidium monoazide combined with quantitative PCR. J. Microbiol. Methods. 2011;85:124–130. doi: 10.1016/j.mimet.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 109.Brescia C.C., Griffin S.M., Ware M.W., Varughese E.A., Egorov A.I., Villegas E.N. Cryptosporidium propidium monoazide-PCR, a molecular biology-based technique for genotyping of viable Cryptosporidium oocysts. Appl. Environ. Microbiol. 2009;75:6856–6863. doi: 10.1128/AEM.00540-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Fittipaldi M., Pino Rodriguez N.J., Adrados B., Agusti G., Penuela G., Morato J., Codony F. Discrimination of viable Acanthamoeba castellani trophozoites and cysts by propidium monoazide real-time polymerase chain reaction. J. Eukaryot. Microbiol. 2011;58:359–364. doi: 10.1111/j.1550-7408.2011.00557.x. [DOI] [PubMed] [Google Scholar]
- 111.Dietersdorfer E., Kirschner A., Schrammel B., Ohradanova-Repic A., Stockinger H., Sommer R., Walochnik J., Cervero-Arago S. Starved viable but non-culturable (VBNC) Legionella strains can infect and replicate in amoebae and human macrophages. Water Res. 2018;141:428–438. doi: 10.1016/j.watres.2018.01.058. [DOI] [PubMed] [Google Scholar]
- 112.Kirschner A.K.T. Determination of viable Legionellae in engineered water systems: Do we find what we are looking for? Water Res. 2016;93:276–288. doi: 10.1016/j.watres.2016.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Cervero-Arago S., Rodriguez-Martinez S., Canals O., Salvado H., Araujo R.M. Effect of thermal treatment on free-living amoeba inactivation. J. Appl. Microbiol. 2014;116:728–736. doi: 10.1111/jam.12379. [DOI] [PubMed] [Google Scholar]
- 114.Rohr U., Weber S., Michel R., Selenka F., Wilhelm M. Comparison of free-living amoebae in hot water systems of hospitals with isolates from moist sanitary areas by identifying genera and determining temperature tolerance. Appl. Environ. Microbiol. 1998;64:1822–1824. doi: 10.1128/AEM.64.5.1822-1824.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Chen Y.-S.R., Sproul O.J., Rubin A.J. Inactivation of Naegleria gruberi cysts by chlorine dioxide. Water Res. 1985;19:783–789. doi: 10.1016/0043-1354(85)90127-7. [DOI] [Google Scholar]