Abstract
Background/Objective
Neurostimulants may improve or accelerate cognitive and functional recovery after intracerebral hemorrhage (ICH), ischemic stroke (IS), or subarachnoid hemorrhage (SAH), but few studies have described their safety and effectiveness in the intensive care unit (ICU). The objective of this study was to describe amantadine and modafinil administration practices during acute stroke care starting in the ICU and to evaluate safety and effectiveness.
Methods
Consecutive adult ICU patients treated with amantadine and/or modafinil following acute non-traumatic IS, ICH, or SAH were evaluated. Neurostimulant administration data were extracted from the electronic medication administration record, including medication (amantadine, modafinil, or both), starting dose, time from stroke to initiation, and whether the neurostimulant was continued at hospital discharge. Patients were considered responders if they met two of three criteria within 9 days of neurostimulant initiation: increase in Glasgow coma scale (GCS) score ≥ 3 points from pre-treatment baseline, improved wakefulness or participation documented in caregiver notes, or clinical improvement documented in physical or occupational therapy notes. Potential confounders of the effectiveness assessment and adverse drug effects were also recorded.
Results
A total of 87 patients were evaluable during the 3.7-year study period, including 41 (47%) with ICH, 29 (33%) with IS, and 17 (20%) with SAH. The initial neurostimulant administered was amantadine in 71 (82%) patients, modafinil in 13 (15%), or both in 3 (3%) patients. Neurostimulants were initiated a median of 7 (4.25, 12.75) days post-stroke (range 1–27 days) for somnolence (77%), not following commands (32%), lack of eye opening (28%), or low GCS (17%). The most common starting dose was 100 mg twice daily for both amantadine (86%) and modafinil (54%). Of the 79 patients included in the effectiveness evaluation, 42 (53%) were considered responders, including 34/62 (55%) receiving amantadine monotherapy and 8/24 (33%) receiving both amantadine and modafinil at the time they met the definition of a responder. No patient receiving modafinil monotherapy was considered a responder. The median time from initiation to response was 3 (2, 5) days. Responders were more frequently discharged home or to acute rehabilitation compared to non-responders (90% vs 62%, p = 0.006). Among survivors, 63/72 (88%) were prescribed a neurostimulant at hospital discharge. The most common potential adverse drug effect was sleep disruption (16%).
Conclusions
Neurostimulant administration during acute stroke care may improve wakefulness. Future controlled studies with a neurostimulant administration protocol, prospective evaluation, and discretely defined response and safety criteria are needed to confirm these encouraging findings.
Electronic supplementary material
The online version of this article (10.1007/s12028-020-00986-4) contains supplementary material, which is available to authorized users.
Keywords: Amantadine, Modafinil, Neurostimulant, Stroke, Critical care, Ischemic stroke, Subarachnoid hemorrhage, Intracerebral hemorrhage, Rehabilitation
Introduction
Approximately 800,000 Americans suffer a new or recurrent stroke each year, including 87% that are ischemic (IS), 10% that are intracerebral hemorrhages (ICH), and 3% that are subarachnoid hemorrhages (SAH) [1]. Stroke is a leading cause of disability, with 2.4% of non-institutionalized adults reporting stroke-related disability, including 43–94% reporting ≥ 2 long-term comorbid medical conditions [2, 3]. The National Institute of Neurological Disorders and Stroke recently identified early recovery after stroke as a research priority, highlighting specific interventions (including pharmacologic agents), for future investigation [4].
Early rehabilitation is a central component of post-stroke care, with clinical practice guidelines recommending early mobilization and rehabilitation within 24–72 h [5] and inpatient rehabilitation rather than skilled nursing care whenever possible [6]. Efforts to provide early rehabilitation following acute stroke can be compromised by a variety of conditions, including apathy and hypersomnia, which may occur in up to 35% and 18% of stroke survivors, respectively [7, 8]. Disordered consciousness after ischemic or hemorrhagic stroke can result from damage to many different structures, including bilateral cerebral cortical injury, pontine tegmentum, midbrain, basal forebrain, hypothalamus and central thalamus, putamen, caudate, and pallidum [9]. Strategies to circumvent these impairments and increase participation in early rehabilitation are needed.
Neurostimulants such as amantadine and modafinil promote wakefulness and may increase patient participation in early rehabilitation, with data largely extrapolated from patients with traumatic brain injury (TBI). Although amantadine is commonly administered to patients with disorders of consciousness, its mechanism of action remains unclear. It may modulate dopamine activity by increasing its release, blocking its reuptake, and increasing postsynaptic dopamine receptors or altering their conformation and may also antagonize n-methyl-d-aspartate (NMDA) receptors [10, 11]. The mechanism of action of modafinil has been attributed to stimulation of alpha1B noradrenergic receptors, reduced gamma-aminobutyric acid (GABA) release, increased glutamate or histamine release, or altered hypocretin activity [12]. Modafinil’s effects appear independent of serotonin, dopamine, GABA, adenosine, histamine-3, melatonin, and benzodiazepine receptors. Compared to conventional neurostimulants, modafinil appears to be devoid of dopaminergic effects, which may be of significance as post-stroke dopaminergic system dysfunction has been recently described [12, 13].
Among the many neurostimulants available, amantadine has the strongest evidence supporting its administration. When started 4 weeks post-TBI during acute rehabilitation, amantadine accelerates functional recovery [14]. Smaller controlled studies treating TBI patients with amantadine during their acute hospitalization have shown improved Glasgow coma scale (GCS) and Mini Mental Status Examination (MMSE) scores [15, 16], but whether similar benefits would occur during acute hospitalization after stroke is unknown.
Amantadine and modafinil are administered to patients following acute stroke in our intensive care unit (ICU) on an ad hoc basis, but data supporting this practice are largely limited to delayed treatment in rehabilitation or outpatient facilities with very few reports during the acute care hospitalization [17–19]. The primary purpose of this study was to describe amantadine and modafinil administration practices during acute stroke care in patients initially treated in an ICU. We also sought to evaluate the safety and effectiveness of this practice.
Methods
Study Design
Consecutive acute stroke patients treated in the 32-bed medical, surgical, and neurological ICU and the 12-bed cardiac ICU at Maine Medical Center between December 2012 and July 2016 were evaluated in this retrospective cohort study. Patients were included if they were ≥ 18 years of age, admitted with an acute non-traumatic ICH, IS, or SAH, and were treated with amantadine, modafinil, or both for at least 72 h starting in an ICU. The 72-h window was chosen based on our anecdotal observation that patients generally respond within this time frame and shorter treatment intervals may be inadequate to assess response. Patients were excluded if they were receiving amantadine or modafinil prior to hospitalization, were admitted with TBI, encephalopathy (including hypoxic ischemic encephalopathy after cardiac arrest), brain tumor, encephalitis, or had a history of seizures. Patients were identified using a pharmacy-generated report. The Institutional Review Board at Maine Medical Center reviewed this study design and determined it was exempt from regulatory review.
Demographics and Clinical Characteristics
Demographic information (age, gender, ethnicity), clinical characteristics including type of stroke (ICH, IS, or SAH), stroke-specific severity grading (ICH score for ICH, Hunt and Hess scale for SAH, and National Institutes of Health Stroke Scale [NIHSS] for IS), laterality for ICH and IS, and presence or absence of an aneurysm for SAH were recorded. Descriptive clinical outcomes included ICU and hospital length of stay, ICU and hospital mortality, and discharge disposition (home, acute rehabilitation, skilled nursing facility, hospice, or death). All information was obtained from the electronic medical record, including notes entered by physicians, nurse practitioners, physician assistants, nurses, pharmacists, and occupational, speech, and physical therapists.
Neurostimulant Administration Practices
A single pharmacist investigator (CSB) extracted amantadine and modafinil administration data from the electronic medication administration record (MAR), including specific neurostimulant(s) initiated (amantadine, modafinil, or both), starting dose, time from stroke to initiation, changes in dosing, and whether or not the neurostimulant was continued at hospital discharge. Discharge prescriptions were assessed for dose taper instructions, no taper instructions, or no mention of the neurostimulant. No protocol for neurostimulant administration following acute stroke existed during the study.
Clinical Effectiveness Outcomes
No single clinical effectiveness measure following neurostimulant administration after an acute stroke has been defined. Accordingly, we adapted the approach used by studies evaluating acute administration of amantadine to TBI patients [15, 20]. Acute stroke patients were characterized as responders if they met two of the following three criteria on any one calendar day within 9 days after neurostimulant initiation: increase in GCS score ≥ 3 points from pre-treatment baseline, clinical improvement in wakefulness or responsiveness documented in caregiver notes, or clinical improvement in wakefulness or responsiveness documented in physical or occupational therapy notes. Caregiver notes and GCS scores were assessed by a neurocritical care Physician Assistant (AML), and physical and occupational therapy notes were assessed by a Doctor of Physical Therapy (KN) and a registered, licensed Occupational Therapist (JC). Supplement 1 describes the approach used by these chart reviewers. Patients who did not meet the definition for responsiveness were classified as non-responders. If patients had an additional neurostimulant added or substituted, the timing of this change was considered when interpreting which drug the patient responded to or did not respond to. Since there was no published literature to establish an expected duration of treatment prior to a response, if a patient responded after at least 24 h of a new combination, we considered them a responder to the new regimen.
Potential confounders of the clinical effectiveness assessment were identified a priori, including hydrocephalus, intracranial pressure (ICP) crisis, seizure, cerebral vasospasm or ischemia, craniotomy for hematoma evacuation, and receipt of a concomitant psychoactive medication (including sedation for mechanical ventilation). Hydrocephalus was defined as placement of a cerebrospinal fluid (CSF) shunting device with radiographic evidence of ventriculomegaly. Intracranial pressure crisis was defined as an ICP > 20 mmHg and/or dilated pupils requiring decompressive surgery or hyperosmolar therapy. New seizures were defined as treatment (not prophylaxis) with an antiepileptic drug and/or electroencephalographic seizures beginning after neurostimulant initiation. Radiographic cerebral vasospasm was present if diagnosed by transcranial Doppler ultrasound, computed tomography angiography, or digital subtraction angiography. Delayed cerebral ischemia was present if focal neurological deterioration requiring fluid bolus, vasopressors, or intraarterial vasodilators occurred. Craniotomy for hematoma evacuation was identified by reviewing neurosurgical procedure notes. Mechanical ventilation was identified by reviewing respiratory flow sheets and required an endotracheal tube or tracheostomy with use of a ventilator. Administration of psychoactive medications (sedatives, opioids, antiepileptics, antipsychotics, or sleep aids) was identified by reviewing the electronic MAR. Supplement 2 includes a list of the potential confounders encountered in this study and suggested approaches to account for them in future studies.
Safety Outcomes
Potential adverse drug effects were selected based on published studies [14, 21], the prescribing information for amantadine and modafinil [22, 23], and our anecdotal experience. These included spasticity, confusion, sleep disruption, seizures, QTc prolongation (amantadine), agitation, and delirium. Spasticity and confusion were identified by reviewing caregiver notes. Sleep disruption was present if the patient received a new sleep medication after starting a neurostimulant, and for the other adverse events, the medical record was reviewed for the 48 h prior to initiating neurostimulant therapy, and if the adverse event was not described prior to initiation but was identified afterward, we considered it possibly drug related. Measurements of QTc were obtained from 12-lead electrocardiograms (ECG) and were considered prolonged if > 450 ms after an initial ECG with a normal QTc. Agitation and delirium were assessed using a previously published algorithm [24]. The probability that an adverse reaction was related to neurostimulant administration was not assessed using grading scales (e.g., Naranjo scale or Bradford Hill criteria) because of the numerous confounders present in ICU patients, and the lack of demonstrated validity and reliability in critically ill patients. Instead, as is standard with good clinical practice for research, we reported all potential adverse drug effects [25].
Statistical Analysis
Continuous data are reported as median (interquartile range 25–75%), and categorical or dichotomous variables as number and percentage. Discharge status was grouped into two outcomes, either “home or acute rehabilitation,” or “skilled nursing facility, hospice or death.” Response rates according to neurostimulant administered and discharge locations were compared using Chi-square analysis or Fisher’s exact testing and p < 0.05 was statistically significant. If a patient transitioned to another neurostimulant for non-response or adverse event, they were counted in both medication categories. Adverse events and responsiveness were assigned to the medication they were receiving at the time these were first detected.
Results
Demographics and Clinical Characteristics
Two hundred five patients received amantadine and/or modafinil during the 3.7 year study period and 118 patients were initially excluded: neurostimulant administered for an indication other than acute stroke (TBI [n = 50], cardiac arrest [n = 15], brain tumor [n = 6], encephalitis [n = 5], or encephalopathy [n = 4]); neurostimulant prescribed prior to hospital admission (n = 27) or administered for < 72 h (n = 8); or history of seizures (n = 3). After our initial chart review of 87 patients, inconsistent data prompted a second review in which 8 patients were confirmed to have received drug for < 72 h; these 8 were excluded from the effectiveness analysis but maintained in the safety analysis. The final evaluable cohort for effectiveness included 79 acute stroke patients.
The median age was 66 (56, 73) years, and most patients were male (n = 56; 64%) and Caucasian (n = 84; 97%) (Table 1). The cohort included 41 patients (47%) with an ICH, 29 (33%) with an IS, and 17 (20%) with a SAH (all aneurysmal). At the time of neurostimulant initiation, 30 (34%) patients were receiving mechanical ventilatory support. The hospital mortality rate was 15/87 (17%); no death was associated with neurostimulant administration, and most patients (50/79; 63%) were discharged to acute rehabilitation (Table 2).
Table 1.
Demographics and patient characteristics at time of neurostimulant initiation
| All (n = 87) | Amantadine (n = 71) | Modafinil (n = 13) | Both (n = 3) | |
|---|---|---|---|---|
| Age, years | 66 (56, 73) | 66 (55, 74) | 66 (61, 71) | 64 (64, 67) |
| Male, no. (%) | 56 (64%) | 43 (61%) | 10 (77%) | 3 (100%) |
| Caucasian, no. (%) | 84 (97%) | 68 (96%) | 13 (100%) | 3 (100%) |
| ICH, no. (%) | 41 (47%) | 32 (45%) | 9 (69%) | 0 |
| ICH score | 2 (1, 3) | 2 (1, 3) | 3 (3, 3) | 0 |
| Laterality (L vs. R) | L 10 versus R 23a | L 7 versus R 14 | L 3 versus R 5 | 0 |
| Ischemic, no. (%) | 29 (33%) | 24 (34%) | 4 (31%) | 1 (33%) |
| NIHSS | 23 (16, 30) | 23 (16, 33) | 22 (17, 25) | 28 |
| Laterality (L vs. R) | L 14 versus R 13b | L 10 versus R 12 | L 3 versus R 1 | L 1 versus R 0 |
| SAH, no. (%) | 17 (20%) | 15 (21%) | 0 | 2 (67%) |
| Hunt and Hess scale | 4 (3, 4) | 4 (3, 5) | 0 | 5c |
Continuous variables are reported as median (IQR) and frequencies as number (%)
ICH, intracerebral hemorrhage; L, left; NIHSS, National Institutes of Health Stroke Scale; R, right; SAH, subarachnoid hemorrhage
aFive patients had a primary intraventricular hemorrhage, and 3 had brainstem ICH
bTwo patients had multiple bilateral embolic ischemic strokes
cBoth patients had a Hunt and Hess scale score of 5
Table 2.
Descriptive clinical outcomes and final response data
| All (n = 79)a | ICH (n = 38) | Ischemic (n = 25) | SAH (n = 16) | |
|---|---|---|---|---|
| ICU length of stay, days | 14 (7, 18) | 15 (11, 18) | 8 (6, 14) | 20 (14, 24) |
| Hospital length of stay, days | 19 (13, 27) | 21 (16, 26) | 14 (10, 19) | 24 (17, 32) |
| ICU mortality, no. (%) | 5 (6%) | 1 (3%) | 3 (12%) | 1 (6%) |
| Discharge disposition, no. (%) | ||||
| Acute rehabilitation | 50 (63%) | 24 (63%) | 17 (64%) | 9 (56%) |
| Home | 11 (14%) | 2 (8%) | 5 (24%) | 4 (25%) |
| Death | 9 (11%) | 4 (10%) | 3 (12%) | 2 (12%) |
| SNF | 8 (10%) | 8 (21%) | 0 | 0 |
| Hospiceb | 1 (1%) | 0 | 0 | 1 (6%) |
| Amantadine monotherapy responders, no. (%) | 34/62 (55%) | 16/30 (53%) | 11/18 (61%) | 7/14 (50%) |
| Modafinil monotherapy responders, no. (%) | 0/15 (0%) | 0/8 (0%) | 0/6(0%) | 0/1 (0%) |
| Amantadine + modafinil responders, no. (%) | 8/24 (33%) | 4/15 (27%) | 3/5 (60%) | 1/4 (25%) |
Continuous variables are reported as median (IQR) and frequencies as number (%). Responder denominators sum to more than 79 patients because patients were included in multiple groups if they transitioned to different medications
ICH, intracerebral hemorrhage; ICU, intensive care unit; SAH, subarachnoid hemorrhage; SNF, skilled nursing facility
aFrom the 87 enrolled subjects, 8 were excluded from effectiveness analysis, including 5 who died and 3 who were transferred to rehabilitation or skilled nursing facilities
bThis single patient was discharged to hospice, expired 48 h after transfer, and was counted as a death in Fig. 1
Neurostimulant Administration Practices
The initial neurostimulant administered was amantadine in 71 (82%) patients, modafinil in 13 (15%), or both amantadine and modafinil simultaneously in 3 (3%). Neurostimulants were initiated a median of 7 (4.25, 12.75) days post-stroke (range 1–27 days). Indications for neurostimulant administration in caregiver notes included somnolence (77%), not following commands (32%), lack of eye opening (28%), or low GCS (17%); more than one indication could be documented for each patient. Time of day for neurostimulant administration was variable, but most twice daily doses were administered at 06:00 and 14:00, and most daily doses were administered at 06:00.
The most common initial dose of amantadine in patients with an estimated creatinine clearance (CrCl) > 60 mL/min was 100 mg twice daily (n = 61; 86%), followed by 100 mg once daily (n = 6; 8%) or 200 mg once daily (n = 1; 1%). Among three patients with impaired kidney function, the initial dose was 50 mg once every other day (n = 1; 1%, CrCl = 13 ml/min), or once weekly doses of 100 mg or 200 mg (one patient each) for two patients receiving hemodialysis. The amantadine dose was increased in 15 (21%) patients a median of 6 (4, 7) days after initiation for persistent somnolence (n = 13; 87%), not following commands (n = 8; 53%), lack of eye opening (n = 2; 13%), low GCS (n = 1; 7%), aphasia (n = 1; 7%), or an undocumented reason (n = 4; 27%); more than one reason could be documented for each patient. The amantadine dose was decreased in 5 (7%) patients a median of 4.5 (3, 6) days after initiation due to delirium (n = 1; 20%), agitation (n = 1; 20%), or an unknown reason (n = 3; 60%). Modafinil was added to 18 patients who initially received amantadine monotherapy a median of 4 (2, 5) days following amantadine initiation, with an initial modafinil dose of 200 mg once daily in 11 (61%), 100 mg twice daily in 5 (28%), and 100 mg daily in 2 (11%) patients.
The most common initial dose of modafinil was 100 mg twice daily (n = 7; 54%), less frequently 200 mg twice daily (n = 4; 31%), 200 mg once daily (n = 1; 8%), or 100 mg three times daily (n = 1; 8%). The modafinil dose was increased in 2 (15%) patients 5 and 6 days after modafinil initiation for somnolence or not following commands (n = 1 each). The modafinil dose was decreased in 2 (15%) patients 2 and 7 days after modafinil initiation for agitation (n = 1) or an unknown reason (n = 1). Amantadine was added to 5 (38%) patients who initially received modafinil monotherapy a median of 6 (1, 6.5) days following modafinil initiation, with an initial amantadine dose of 100 mg twice daily (n = 3; 60%), 100 mg once daily (n = 1; 20%), or 100 mg every 48 h (n = 1; 20%).
In patients starting both amantadine and modafinil simultaneously, the initial dose of amantadine was 100 mg twice daily (n = 2; 67%) or 50 mg twice daily (n = 1; 33%) and for modafinil it was 100 mg twice daily (n = 2; 67%) or 200 mg twice daily (n = 1; 33%). The amantadine dose was increased from 100 mg twice daily to 200 mg twice daily 8 days after initiation in 1 (33%) patient because they were not following commands. With transitions to different medication groups, and including patients in every medication group they received, a total of 73 patients received amantadine monotherapy, 27 received combined amantadine/modafinil therapy, and 15 received modafinil monotherapy at some time during their hospitalization.
Of the 72 (83%) patients who survived to hospital discharge, 9 (12%) patients had their neurostimulant stopped prior to discharge, and 63 (86%) were provided neurostimulant prescriptions. Amantadine prescriptions were provided to 33 (52%) patients, 8 (13%) received a modafinil prescription, and 22 (35%) received a prescription for both neurostimulants. Among the 63 discharge neurostimulant prescriptions, 45 (71%) included dosing without taper instructions, 4 (6%) had taper instructions, and 14 (22%) included no information about continuing or tapering the neurostimulant.
Clinical Effectiveness
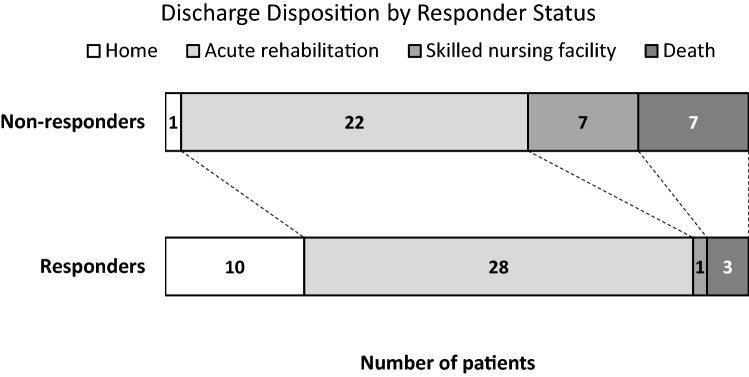
Among the 79 patients included in the clinical effectiveness analysis, 42 (53%) were considered responders, including 34/62 (55%) receiving amantadine monotherapy and 8/24 (33%) receiving both amantadine and modafinil at the time they first met the definition of a responder; no patient receiving modafinil monotherapy was a responder (p < 0.001; Fig. 1, Table 2). The median time from neurostimulant initiation to responder status was 3 (2, 5) days (range 1–9 days). Responders were more frequently discharged to home or acute rehabilitation compared to non-responders (90% vs 62%, p = 0.006; Fig. 2).
Fig. 1.
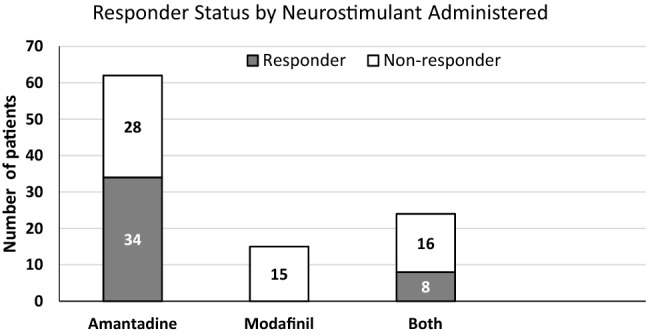
Responder status according to neurostimulant administered. Responder status according to neurostimulant administered (i.e., amantadine, modafinil, or both) on the day responder status was first documented is reported. Of the 42 responders, 34 (81%) were receiving amantadine monotherapy and 8 (19%) were receiving both amantadine and modafinil (p < 0.001). Patients receiving modafinil monotherapy were never classified as responders
Fig. 2.
Discharge disposition for responders versus non-responders. Responders were more frequently discharged home or to an acute rehabilitation facility compared to non-responders (p = 0.006)
Many factors potentially confounded the effectiveness assessment. The most common was hydrocephalus (n = 36; 41%), including 18/41 (44%) patients with ICH, 16/17 (94%) with SAH, and 2/29 (7%) with IS. Most of these patients (n = 35; 97%) required CSF diversion. Supplement 2 includes a complete list of confounders, their estimated impact on our assessments, and a recommended approach for future studies.
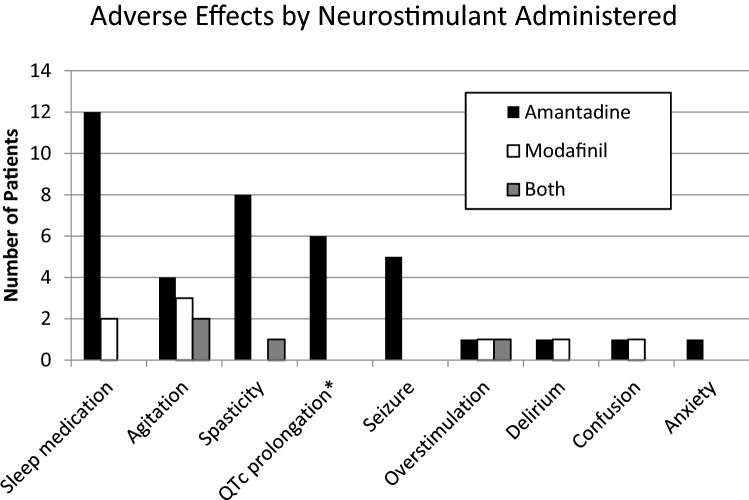
Safety Outcomes
Among the 87 patients included in the safety analysis, the most common potential adverse drug effect was sleep disruption requiring administration of a new sleep medication (n = 14; 16%) (Fig. 3). Other potential adverse drug effects occurring after neurostimulant initiation included agitation (n = 9; 10%), spasticity (n = 9; 10%), and QTc prolongation (n = 6; 7%) with amantadine. New onset seizures requiring antiepileptic drug administration occurred in 5 (6%) patients (n = 3 with ICH and n = 2 with IS). Amantadine was discontinued due to seizure in one IS patient and continued in the other four.
Fig. 3.
Potential adverse drug effects during neurostimulant administration. Potential adverse drug effects were identified by reviewing provider progress notes, the medication administration record, electrocardiograms, and nursing flow sheets. Causality assessments were not conducted due to the presence of confounding variables in this patient population. *QTc prolongation was only assessed in patients receiving amantadine
Amantadine was discontinued in 10 patients a median of 6 (2, 18) days after initiation. The decision to stop was made by clinical teams, and included sustained wakefulness after 8 and 9 days of treatment (n = 2; 20%), or adverse drug effects including agitation (n = 2; 20%), anxiety (n = 1; 10%), delirium (n = 1; 10%), seizures (n = 1; 10%), QT prolongation without arrhythmia (n = 1; 10%), and decision to transition to comfort measures only (CMO) (n = 2; 20%). Modafinil was discontinued in one patient 5 days after initiation due to insomnia and agitation.
Discussion
Participation in rehabilitation activities during acute stroke care and eventually in specialized rehabilitation settings is an important component of stroke recovery and is prioritized in stroke guidelines [5, 6]. Neurostimulants have proven beneficial for TBI patients when administered in rehabilitation units and, with weaker evidence, earlier in their recovery during acute care [14–16]. This study represents the largest cohort of stroke patients treated with neurostimulants during their acute hospitalization, and suggests amantadine started in the first week after stroke may be associated with improved wakefulness or responsiveness in approximately half of treated patients. Responders showed a promising trend with more frequent discharge to home or acute rehabilitation compared to non-responders, but these findings must be considered hypothesis-generating.
Early rehabilitation after stroke is recommended by the American Heart Association and American Stroke Association [6], and efforts to increase rehabilitation participation during acute stroke care with neurostimulants may be beneficial in somnolent or non-participatory patients. In our study, patients were started on neurostimulants a median of 7 days after stroke, with a single patient starting in the first 24 h. The best time to start neurostimulants is not known, and caution has been advised to avoid very early, high-intensity mobilization in the first 24 h after acute stroke, since this has been associated with a reduction in favorable outcome at 3 months [26, 27]. Several patients had neurostimulants started late in their hospital course and were either transferred or had support withdrawn prior to 72 h of treatment. It is not clear if a longer duration of monitored dosing would have resulted in a response or not, but because of the short administration time, we excluded them from our effectiveness analysis. Among our 42 responders, the median time to response was 3 days, providing some justification for this a priori threshold for minimal duration.
No valid and reliable clinical effectiveness measure exists to assess response to neurostimulants in the acute care setting after stroke. Studies describing amantadine administration to one rehabilitation and five acutely hospitalized stroke patients utilized the Coma Recovery Scale-Revised (CRS-R) and Disability Rating Scale (DRS) [18, 28]. A randomized study comparing modafinil and placebo administration within 14 days of stroke reported the multidimensional fatigue inventory at 30, 90, and 180 days post-stroke [17]. The lack of consensus supporting a specific clinical effectiveness measure in the acute stroke setting and the retrospective nature of our study necessitated the development of a novel method. Glasgow coma scale was shown to increase during acute administration of amantadine to 19 and 41 TBI patients [15, 20]; we utilized a similar approach.
Assessing the effectiveness of neurostimulant administration during acute stroke care is complicated by patient care needs, which often persist into the rehabilitation phase (e.g., mechanical ventilation or medications for sedation, analgesia, or seizures). Even in the rehabilitation setting, medications confounded assessment of responsiveness in prior studies for up to a third of patients [14]. The common sequelae of stroke (e.g., pain, seizures, vasospasm, hydrocephalus, and intracranial hypertension) also complicated our neurostimulant response assessments. For example, hydrocephalus (which required CSF diversion 97% of the time) may have induced somnolence, while CSF diversion or unclamping external drains may have induced wakening. Similarly, intubated patients who are liberated from mechanical ventilation may become more interactive as their communication improves and sedation is reduced. A recent study of TBI patients treated acutely with neurostimulants in the ICU encountered many of the same confounders [21]. Supplement 2 includes a list of the potential confounders we encountered in this study and suggested approaches to them in future studies.
The most common potential adverse drug effect was need for a new sleep medication, suggesting sleep disruption may have been occurring. Our most common administration schedule of amantadine at 06:00 and 14:00 may alleviate this, but this remains unproven. Two subjects were initially prescribed twice daily doses at 08:00 and 20:00; both had insomnia noted and the timing of doses was adjusted to 06:00 and 14:00. The ideal dose and whether a predictable dose–response relationship exists for amantadine during acute stroke care is unclear. Amantadine may increase the number of postsynaptic dopamine receptors or alter their conformation over several weeks, suggesting time of daily administration may not influence sleep [29]. The most concerning potential adverse drug effect during amantadine therapy was seizures, though it was impossible to assess causality since seizures are not rare after the types of stroke we studied. Amantadine has been safely administered to patients with epilepsy since the mid-1980’s [30], but caution is still required. Many patients had multiple other reasons for potential adverse effects (i.e., confusion potentially caused by amantadine or modafinil, urinary tract infection, steroids, vasospasm, hydrocephalus, or hypernatremia). Prior studies examining the accuracy of delirium screening following acute stroke using the CAM-ICU have suggested decreased accuracy results [31–33]. The number of patients with delirium in our study was low but use of accurate screening tests after stroke in future studies may increase recognition. All adverse events identified have been previously reported, though it is possible other adverse drug effects occurred and were not identified in our retrospective study.
Several limitations of this study warrant comment. Due to the paucity of published data for stroke patients treated with neurostimulants in the acute setting, no protocols or robust data were available to guide us or allow for a power calculation. We performed this retrospective evaluation to obtain baseline data and response estimates to help design future studies. Reliance on caregiver notes was an additional limitation but prompted us to incorporate more consistent documentation regarding neurostimulant administration and response. It was not possible to control for changes in the quality of caregiver and PT/OT documentation over time as neurostimulants were more frequently administered. Physical and occupational therapists used a semi-structured template including initial and subsequent evaluations, which differ in frequency and domains evaluated from patient-to-patient. Future studies in the acute care setting should utilize a clinical effectiveness measure that evaluates the indication for neurostimulant use and regularly assesses response.
Whether adding a second neurostimulant (if no improvement is observed from the initial neurostimulant) adds benefit, risk, neither, or both is unclear. Herrold and colleagues retrospectively evaluated 115 TBI patients treated with neurostimulants in a rehabilitation center, finding that those treated with multiple agents had no better outcome than those treated with a single medication [34]. Given the lack of an untreated control group in this retrospective study, we cannot be certain that any improvements resulted from the medications and it is possible they reflect the natural phase of recovery over time after stroke. Not all patients were monitored for the full 9-day period after starting or changing a neurostimulant, due to transfers to rehabilitation or skilled nursing facilities or decisions to withdraw life-sustaining therapy. Ideally, a consistent follow-up period would have been maintained for all patients. Similarly, after a change in neurostimulant, a response within the first few days could be from the new regimen or a delayed response from the initial treatment. It is possible our approach to assign credit for a response to the new regimen if > 24 h of drug had been given was incorrect.
Our results suggest modafinil may not be effective as monotherapy in the acute care setting, but larger, prospective studies are needed. In a non-randomized study, potential bias related to gender, comorbidities, severity of illness, or other factors must be considered. Lack of response to modafinil in our study may have been the result of a mechanism of action separate from dopamine neurotransmission. Pre-clinical and clinical data suggest dopamine activity is disturbed following acute stroke, and dopamine supplementation or augmentation may be of benefit, but this requires confirmation [13, 35].
Analysis by stroke type and location was not possible due to the small sample size. Such an analysis may be important as previous studies have suggested stroke location may play a role in neurostimulant responsiveness [36]. Due to small numbers, we did not include patients who received other neurostimulants, such as dextroamphetamine or methylphenidate. Prior data have been published for these agents [37, 38], and amantadine and modafinil were the two most prescribed stimulants in a recent acute TBI study [21]. Continuing medications started in the ICU at the time of hospital discharge may be inappropriate in some settings [39], but in the case of neurostimulants, declines were seen when medication was stopped after 4 weeks in TBI patients [14], suggesting continuation may be appropriate.
Conclusion
Initiation of neurostimulants during the acute care of patients admitted with IS, ICH, or SAH is potentially associated with improved wakefulness. Those who responded were more frequently discharged home or to acute rehabilitation, but we can neither confirm these improvements were medication related, nor that these outcomes are generalizable to other settings. These results are encouraging but must be considered hypothesis-generating given the uncontrolled nature of the study, and the many potential biases and confounders. Further study using standard dosing and escalation strategies, prospective assessment of response and drug safety, and appropriate controls is needed.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author contributions
AML, RRR, and DJG contributed to study design, data collection and manuscript development. TM and DBS contributed to study design and manuscript development. CSB, KN, and JC contributed to data collection. AE contributed to study design. All authors approved the final manuscript prior to submission.
Source of support
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors report no conflicts of interest.
Ethical Approval
We adhered to ethical guidelines. The Institutional Review Board at Maine Medical Center reviewed this study design and determined it to represent exempt research.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139:e56–e528. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) Prevalence and most common causes of disability among adults—United States, 2005. MMWR Morb Mortal Wkly Rep. 2009;58:421–426. [PubMed] [Google Scholar]
- 3.Gallacher KI, Jani BD, Hanlon P, Nicholl BI, Mair FS. Multimorbidity in stroke. Stroke. 2019;50:1919–1926. doi: 10.1161/STROKEAHA.118.020376. [DOI] [PubMed] [Google Scholar]
- 4.Vickrey BG, Brott TG, Koroshetz WJ, Stroke Research Priorities Meeting Steering Committee and the National Advisory Neurological Disorders and Stroke Council. National Institute of Neurological Disorders and Stroke Research priority setting: a summary of the 2012 NINDS Stroke Planning Meeting Report. Stroke. 2013;44:2338–2342. doi: 10.1161/STROKEAHA.113.001196. [DOI] [PubMed] [Google Scholar]
- 5.Bernhardt J, English C, Johnson L, Cumming TB. Early mobilization after stroke: early adoption but limited evidence. Stroke. 2015;46:1141–1146. doi: 10.1161/STROKEAHA.114.007434. [DOI] [PubMed] [Google Scholar]
- 6.Winstein CJ, Stein J, Arena R, Bates B, Cherney LR, Cramer SC, American Heart Association Stroke Council. Council on Cardiovascular and Stroke Nursing. Council on Clinical Cardiology. Council on Quality of Care and Outcomes Research et al. Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2016;47:e98–e169. doi: 10.1161/STR.0000000000000098. [DOI] [PubMed] [Google Scholar]
- 7.van Dalen JW, Moll van Charante EP, Nederkoorn PJ, van Gool WA, Richard E. Poststroke apathy. Stroke. 2013;44:851–860. doi: 10.1161/STROKEAHA.112.674614. [DOI] [PubMed] [Google Scholar]
- 8.Harris AL, Elder J, Schiff ND, Victor JD, Goldfine AM. Post-stroke apathy and hypersomnia lead to worse outcomes from acute rehabilitation. Transl Stroke Res. 2014;5:292–300. doi: 10.1007/s12975-013-0293-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rohaut B, Doyle KW, Reynolds AS, Igwe K, Couch C, Matory A, et al. Deep structural brain lesions associated with consciousness impairment early after hemorrhagic stroke. Sci Rep. 2019;12:4174. doi: 10.1038/s41598-019-41042-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gualtieri T, Chandler M, Coons TB, Brown LT. Amantadine: a new clinical profile for traumatic brain injury. Clin Neuropharmacol. 1989;12(4):258–270. doi: 10.1097/00002826-198908000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Stoof JC, Booij J, Drukarch B. Amantadine as N-methyl-d-aspartic acid receptor antagonist: new possibilities for therapeutic applications? Clin Neurol Neurosurg. 1992;94(Suppl):S4–S6. doi: 10.1016/0303-8467(92)90006-O. [DOI] [PubMed] [Google Scholar]
- 12.Ballon JS, Feifel D. A systematic review of modafinil: potential clinical uses and mechanisms of action. J Clin Psychiatry. 2006;67:554–566. doi: 10.4088/JCP.v67n0406. [DOI] [PubMed] [Google Scholar]
- 13.Gower A, Tiberi M. The Intersection of central dopamine system and stroke: potential avenues aiming at enhancement of motor recovery. Front Synaptic Neurosci. 2018;10:18. doi: 10.3389/fnsyn.2018.00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Giacino JT, Whyte J, Bagiella E, Kalmar K, Childs N, Khademi A, et al. Placebo-controlled trial of amantadine for severe traumatic brain injury. N Engl J Med. 2012;366:819–826. doi: 10.1056/NEJMoa1102609. [DOI] [PubMed] [Google Scholar]
- 15.Ghalaenovi H, Fattahi A, Koohpayehzadeh J, et al. The effects of amantadine on traumatic brain injury outcome: a double-blind, randomized, controlled, clinical trial. Brain Inj. 2018;32:1050–1055. doi: 10.1080/02699052.2018.1476733. [DOI] [PubMed] [Google Scholar]
- 16.Meythaler JM, Brunner RC, Johnson A, Novack TA. Amantadine to improve neurorecovery in traumatic brain injury-associated diffuse axonal injury: a pilot double-blind randomized trial. J Head Trauma Rehabil. 2002;17:300–313. doi: 10.1097/00001199-200208000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Poulsen MB, Damgaard B, Zerahn B, Overgaard K, Rasmussen RS. Modafinil may alleviate poststroke fatigue: a randomized, placebo-controlled, double-blinded trial. Stroke. 2015;46:3470–3477. doi: 10.1161/STROKEAHA.115.010860. [DOI] [PubMed] [Google Scholar]
- 18.Akçıl EF, Dilmen ÖK, Vehid H, Tunalı Y. Can amantadine ameliorate neurocognitive functions after subarachnoid haemorrhage? A preliminary study. Turk J Anaesthesiol Reanim. 2018;46(2):100–107. doi: 10.5152/TJAR.2018.20280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pokryszko-Dragan A, Słotwiński K, Budrewicz SP, Podemski R, Zagrajek M, Bilińska M. Attention level and event-related evoked potentials in patients with cerebrovascular disease treated with amantadine sulfate: a pilot study. Adv Clin Exp Med. 2008;17:553–558. [Google Scholar]
- 20.Saniova B, Drobny M, Kneslova L, Minarik M. The outcome of patients with severe head injuries treated with amantadine sulphate. J Neural Transm (Vienna) 2004;111:511–514. doi: 10.1007/s00702-004-0112-4. [DOI] [PubMed] [Google Scholar]
- 21.Barra ME, Izzy S, Sarro-Schwartz A, Hirschberg RE, Mazwi N, Edlow BL. Stimulant therapy in acute traumatic brain injury: Prescribing patterns and adverse event rates at 2 level 1 trauma centers. J Intensive Care Med. 2019 doi: 10.1177/0885066619841603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amantadine [package insert]. Chadds Ford: Endo Pharmaceuticals Inc.; 2009.
- 23.Modafinil [package insert]. North Wales: Teva Pharmaceuticals USA, Inc.; 2015.
- 24.Gagnon DJ, Fontaine GV, Smith KE, Riker RR, Miller RR, 3rd, Lerwick PA, et al. Valproate for agitation in critically ill patients: a retrospective study. J Crit Care. 2017;37:119–125. doi: 10.1016/j.jcrc.2016.09.006. [DOI] [PubMed] [Google Scholar]
- 25.ICH Harmonised Tripartite Guideline. Guideline For Good Clinical Practice E6(R1). https://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E6/E6_R1_Guideline.pdf. Accessed 20 June 2019.
- 26.Langhorne P, Collier JM, Bate PJ, Thuy MN, Bernhardt J. Very early versus delayed mobilisation after stroke. Cochrane Database Syst Rev. 2018;10:CD006187. doi: 10.1002/14651858.CD006187.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.AVERT Trial Collaboration group Efficacy and safety of very early mobilisation within 24 h of stroke onset (AVERT): a randomised controlled trial. Lancet. 2015;386:46–55. doi: 10.1016/S0140-6736(15)60690-0. [DOI] [PubMed] [Google Scholar]
- 28.Lehnerer SM, Scheibe F, Buchert R, Kliesch S, Meisel A. Awakening with amantadine from a persistent vegetative state after subarachnoid haemorrhage. BMJ Case Rep. 2017; pii: bcr-2017-220305. [DOI] [PMC free article] [PubMed]
- 29.Gianutsos G, Chute S, Dunn JP. Pharmacological changes in dopaminergic systems induced by long-term administration of amantadine. Eur J Pharmacol. 1985;110(3):357–361. doi: 10.1016/0014-2999(85)90564-3. [DOI] [PubMed] [Google Scholar]
- 30.Turner AL, Perry MS. Outside the box: medications worth considering when traditional antiepileptic drugs have failed. Seizure. 2017;50:173–185. doi: 10.1016/j.seizure.2017.06.022. [DOI] [PubMed] [Google Scholar]
- 31.van Eijk MM, van den Boogaard M, van Marum RJ, Benner P, Eikelenboom P, Honing ML, et al. Routine use of the confusion assessment method for the intensive care unit: a multicenter study. Am J Respir Crit Care Med. 2011;184:340–344. doi: 10.1164/rccm.201101-0065OC. [DOI] [PubMed] [Google Scholar]
- 32.Reznik ME, Drake J, Margolis SA, Moody S, Murray K, Costa S, et al. Deconstructing poststroke delirium in a prospective cohort of patients with intracerebral hemorrhage. Crit Care Med. 2020;48:111–118. doi: 10.1097/CCM.0000000000004031. [DOI] [PubMed] [Google Scholar]
- 33.Riker RR, Fraser GL. In the middle of difficulty lies opportunity-Albert Einstein. Crit Care Med. 2018;46:1881–1882. doi: 10.1097/CCM.0000000000003399. [DOI] [PubMed] [Google Scholar]
- 34.Herrold AA, Pape TL, Guernon A, Mallinson T, Collins E, Jordan N. Prescribing multiple neurostimulants during rehabilitation for severe brain injury. Sci World J. 2014;2014:964578. doi: 10.1155/2014/964578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stinear CM. Dopamine for motor recovery after stroke: where to from here? Lancet Neurol. 2019;18:514–515. doi: 10.1016/S1474-4422(19)30162-0. [DOI] [PubMed] [Google Scholar]
- 36.Brioschi A, Gramigna S, Werth E, Staub F, Ruffieux C, Bassetti C, et al. Effect of modafinil on subjective fatigue in multiple sclerosis and stroke patients. Eur Neurol. 2009;62:243–249. doi: 10.1159/000232927. [DOI] [PubMed] [Google Scholar]
- 37.Goldstein LB, Lennihan L, Rabadi MJ, Good DC, Reding MJ, Dromerick AW, et al. Effect of dextroamphetamine on poststroke motor recovery: a randomized clinical trial. JAMA Neurol. 2018;75:1494–1501. doi: 10.1001/jamaneurol.2018.2338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Delbari A, Salman-Roghani R, Lokk J. Effect of methylphenidate and/or levodopa combined with physiotherapy on mood and cognition after stroke: a randomized, double-blind, placebo-controlled trial. Eur Neurol. 2011;66(1):7–13. doi: 10.1159/000329275. [DOI] [PubMed] [Google Scholar]
- 39.Kovacic NL, Gagnon DJ, Riker RR, Wen S, Fraser GL. An analysis of psychoactive medications initiated in the ICU but continued beyond discharge: a pilot study of stewardship. J Pharm Pract. 2019; 897190019830518. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.