Abstract
Introduction
Insomnia is a highly prevalent and costly condition that is associated with increased health risks and healthcare utilisation. Anecdotally, cannabis use is frequently reported by consumers to promote sleep. However, there is limited research on the effects of cannabis on sleep and daytime function in people with insomnia disorder using objective measures. This proof-of-concept study will evaluate the effects of a single dose of an oral cannabis-based medicine on sleep and daytime function in participants with chronic insomnia disorder.
Methods and analysis
A randomised, crossover, placebo-controlled, single-dose study design will be used to test the safety and efficacy of an oral oil solution (‘ETC120’) containing 10 mg Δ9-tetrahydrocannabinol (THC) and 200 mg cannabidiol (CBD) in 20 participants diagnosed with chronic insomnia disorder. Participants aged 35–60 years will be recruited over an 18-month period commencing August 2019. Each participant will receive both the active drug and matched placebo, in a counterbalanced order, during two overnight study assessment visits, with at least a 1-week washout period between each visit. The primary outcomes are total sleep time and wake after sleep onset assessed via polysomnography. In addition, 256-channel high-density electroencephalography and source modelling using structural brain MRI will be used to comprehensively examine brain activation during sleep and wake periods on ETC120 versus placebo. Next-day cognitive function, alertness and simulated driving performance will also be investigated.
Ethics and dissemination
Ethics approval was received from Bellberry Human Research Ethics Committee (2018-04-284). The findings will be disseminated in a peer-reviewed open-access journal and at academic conferences.
Trial registration number
ANZCTRN12619000714189.
Keywords: cannabinoids, insomnia, high-density EEG, protocol
Strengths and limitations of this study.
This is the first study to use novel assessment techniques including high-density electroencephalography (EEG) with structural brain MRI to comprehensively examine and localise differences in brain activation during sleep and wake periods in participants with insomnia disorder.
This study uses a randomised, controlled trial design to investigate the effects of a pharmaceutical-grade oral oil solution containing 10mg Δ9-tetrahydrocannabinol (THC) and 200mg cannabidiol (CBD) on sleep and daytime function in a clinical population.
Participants will have sleep physician-confirmed insomnia disorder and will be thoroughly screened to rule out other sleep disorders.
This study is a single-dose design investigating only the acute effects of a cannabis-based medicine over a 24-hour period in a controlled in-laboratory environment.
This study cannot assess the individual contribution of THC and CBD.
Introduction
Insomnia is a common sleep disorder that can present in isolation or comorbid to other medical or psychiatric conditions.1 Despite often emerging as a transient response to stress or change to one’s normal sleep–wake cycle,2 approximately 30% of individuals with insomnia display chronic symptoms.3 Chronic insomnia is characterised by sleep disturbances (difficulties with falling asleep, maintaining sleep, or inability to return to sleep on awakening) occurring at least three nights per week and for at least 3 months.4 5 The sleep disturbance is often coupled with clinically significant daytime impairments in social life, occupational function and/or educational achievement.4 5 It is often the perceived daytime impairments, as opposed to the noctural insomnia symptoms per se, that prompt patients to seek treatment.6 Chronic insomnia tends to either ‘wax and wane’ or persist over a lifetime, with the latter course predicted by more severe insomnia symptoms at baseline, female gender and older age.7 8There are emerging associations between chronic insomnia and increased health risks such as cardiovascular disease,9 depression10–12 and dementia,13 14 as well as high rates of absenteeism15 16 and healthcare utilisation.17 Indeed, longitudinal studies with follow-up period ranging from 1 to 34 years have found a substantial risk for developing depression (both first onset and recurrent major depressive disorder) in patients with insomnia, an association that is bidirectional.18 As such, there is a strong need for early clinical intervention.
The goal of treatment for insomnia is to improve sleep (both duration and quality) and alleviate daytime impairments. Psychological therapies such as cognitive behavioural therapy for insomnia (CBT-I) and psychoeducation regarding sleep hygiene can be effective.19 However, these often require access to a therapist and can involve substantial effort, time and financial commitment.20 Furthermore, the perceived benefits from these approaches are typically delayed. Thus, patients with persistent symptoms often seek strategies offering short-term relief to maintain normal daytime functioning; highlighting a specific role for adjunctive use of pharmacological treatments such as benzodiazepines, sedating antidepressants, and Z-drugs.21 However, these are associated with undesirable side effects such as cognitive impairment, tolerance/dependence and impaired driving due to sedative effects that can persist into the following day.22 Moreover, many of these medications disturb sleep architecture; increasing sleep fragmentation and one’s sense of having non-restorative sleep and ultimately impair the ability to undertake normal daily activities.23 Thus, novel approaches are needed to address the needs of people with chronic insomnia disorder.
Anecdotally, consumers of cannabis commonly report that the drug promotes uninterrupted sleep.24 The plant Cannabis sativa contains >100 different cannabinoids—the most abundant of which are the main psychoactive component, Δ9-tetrahydrocannabinol (THC), and the non-intoxicating cannabinoid, cannabidiol (CBD).25 Both CBD and THC affect components of the endogenous cannabinoid system which are involved in the regulation of the circadian sleep–wake cycle, including the maintenance and promotion of sleep.26 27 THC is a partial agonist of the cannabinoid 1 (CB1) receptor, found primarily within the central nervous system28 and the cannabinoid 2 (CB2) receptor, found primarily in the immune system and on peripheral organs.29 THC is known to have sedating properties via its action at the CB1 receptor, which is notably dense in areas of the central nervous system such as the thalamus, hypothalamus, hippocampus, basal ganglia and cortex, suggesting a diverse role in the modulation of physiological functions including sleep.30 31 CBD is an indirect CB1 and CB2 receptor agonist, and has shown to increase concentrations of the major endogenous cannabinoid, anandamide, by inhibiting its degradative enzyme, fatty acid amid hydrolase (FAAH).32 33 Increasing endogenous anandamide via FAAH inhibition normalised deficits in stage N3 sleep in cannabis-dependent men experiencing withdrawal,34 consistent with preclinical data showing that anandamide promotes slow wave sleep, possibly through increases in extracellular adenosine concentrations.35–37 This effect can be blocked by administration of the CB1 antagonist, rimonabant.38 Indeed, clinical trials of rimonabant have reported an increased risk of sleep disturbances,39 suggesting a role for the CB1 receptor in mediating sleep. CBD is also a negative allosteric modulator of CB1 receptor40 and may reduce the effects of THC and anandamide on the brain.41 42 There is an emerging viewpoint that coadministration of CBD with THC may enhance therapeutic outcomes by attenuating the adverse effects of THC (e.g., on emotion recognition,43 next-day memory performance,44 appetitive effects45 and acute psychotic symptoms46 47); however, findings are inconsistent with a recent study showing CBD exacerbating THC-induced impairment on driving and cognition, possibly via a pharmacokinetic interaction.48 Furthermore, CBD is a promiscuous molecule that exhibits activity on a wide array of molecular targets beyond CB1 and CB2 receptors such as inhibitory GABAA receptors,49 which may also influence sleep. Administration of THC alone (15 mg) in the evening was associated with next-day changes in mood, sleepiness and memory in healthy adults,44 emphasising the need for careful consideration of dose and ratio of cannabinoids when administered in clinical insomnia populations.
To date, there have been no well-designed randomised controlled trials employing objective measures assessing the effects of cannabis on sleep duration and quality in a clinical insomnia population.50–52 Previous studies have shown potential benefits in the therapeutic use of nabiximols (Sativex), an oromucosal spray containing equal parts THC and CBD, in the relief of pain and other chronic symptoms including improved sleep, with the latter only assessed as a secondary outcome using subjective rating scales.53 Other studies using synthetic THC (nabilone) showed improvements in subjective sleep quality in patients with post-traumatic stress disorder (PTSD)54 55 and fibromyalgia,56 while CBD was found to be effective in reducing the frequency of rapid eye movement sleep behaviour disorder events in Parkinson’s disease.57 One case study showed that 25 mg CBD daily reduced anxiety symptoms and improved sleep disturbances in a young child with PTSD.58 Indeed, preclinical evidence has demonstrated anxiolytic effects of CBD, likely dependant on CB1 and 5-HT1A receptor action, with early human experimental evidence supporting preclinical findings.59 To address the lack of studies in a clinical insomnia population, we will investigate the acute effects of a plant-derived, pharmaceutical-grade, oral formulation containing 10 mg THC and 200 mg CBD relative to placebo on sleep and next-day function (cognitive function, alertness, simulated driving performance) in participants with physician-confirmed chronic insomnia disorder. This study will be the first to employ 256-channel high-density electroencephalography (EEG) coupled with structural MRI brain scans to examine and localise differences in sleep depth and brain activation during both sleep and wakefulness in this clinical population.
Methods and analysis
Study design
A double-blind, randomised, placebo-controlled, crossover study design will be used to evaluate the effects of 10 mg THC and 200 mg CBD on sleep and daytime function in participants diagnosed with chronic insomnia disorder. Participants will be recruited over an 18-month period commencing August 2019. The recruitment target is 20 participants, which will provide the proof-of-concept evaluation of the study drug to determine whether future larger studies in insomnia disorder are warranted. The study site and sponsor is the Woolcock Institute of Medical Research; a research institute and specialist sleep clinic in inner suburban Sydney, Australia. Participants will undergo two separate overnight study assessment visits. Each study assessment visit will be scheduled at least one week apart to avoid any carryover effects, as informed by previous studies of this nature.60 61 The protocol (Version 2.3, July 2019) has been prepared in accordance with the SPIRIT statement (see online supplementary file 1).62
bmjopen-2019-034421supp001.pdf (88.3KB, pdf)
Recruitment and enrolment
The study population will be adults aged 35–60 years with chronic insomnia disorder as per International Classification of Sleep Disorders–Third Edition (ICSD-3) criteria.63 This age range was chosen to limit age-related variability in sleep architecture for better interpretation of EEG changes.64 Participation will be voluntary under conditions of informed consent. A list of the inclusion and exclusion criteria is presented in box 1. Participants will be recruited through the following strategies: (1) referral from sleep physicians and psychologists at the Woolcock Institute of Medical Research, Australia; (2) via two databases that host the details of people who have provided consent to be contacted about future clinical trials (”Woolcock Volunteer Database” and the “Lambert Initiative for Cannabinoid Therapeutics Expression of Interest database”); (3) physical study advertisements displayed around the local University area; and (4) study advertisements posted on social and news media. All participants will receive financial compensation for their time commitment to the study.
Box 1. Inclusion and exclusion criteria.
Inclusion criteria
Aged 35–60 years
Diagnosis of insomnia disorder made by a physician or a psychologist
Insomnia Severity Index (ISI) score≥15
Insomnia symptoms for >3 times per week and present longer than 3 months
Exclusion criteria
Shift worker
Medical condition (e.g., chronic pain) or medication that is the cause of the insomnia
Sleep apnoea (defined as Apnoea Hypopnoea Index (AHI)>15 and Oxygen Desaturation Index (ODI)>10) or sleep-related movement disorder based on in-laboratory polysomnography
Advanced or delayed sleep–wake phase disorder based on actigraphy
Used any modality of treatment for insomnia, including cognitive–behavioural therapy (CBT) and CNS-active drugs, within 3 months before screening or at the medical doctor’s discretion
Transmeridian travel (two time zones) in the past month
Use of medications that may influence cannabinoid metabolism (e.g. inhibitors/inducers of the CYP450 pathway)
Clinically relevant cardiovascular abnormalities (as determined by 12-lead ECG at screening)
Pregnancy or lactation (females)
History of a major psychiatric disorder within the past 12 months (except clinically-managed mild depression or anxiety) as per the Diagnostic and Statistical Manual of Mental Disorders (DSM)-5 or at the medical doctor’s discretion
History of attempted suicide or current suicidal ideation as determined by a score >0 on Q9 of the Patient Health Questionnaire (PHQ)-9
History of drug or alcohol abuse/dependency within the past 2 years
Urinary drug screen positive for drugs (benzodiazepines, opiates, cannabis, amphetamines, cocaine)
Known hypersensitivity to cannabis
Cannabis use within the past 3 months (confirmed by negative urine drug screen)
Unable to undergo brain MRI due to implanted device or other reason
Excessive caffeine use that, in the opinion of the medical doctor contributes to the participant's insomnia, or is unable to abstain from caffeine use ≥24 hours prior to each overnight study assessment visit
Inability to refrain from alcohol consumption ≥24 hours prior to each overnight study assessment visit
Medical conditions that result in frequent need to get out of bed (e.g., nocturia)
Required to complete mandatory drug testing for cannabis (e.g., workplace testing, court order)
Study intervention
The investigational product (‘ETC120’) is a plant-derived oral formulation containing a 1:20 ratio of THC to CBD suspended in medium-chain triglycerides (MCT) oil. ETC120 will be purchased from Linnea (Ticino, Switzerland). Participants will be administered a single fixed dose of ETC120 (2 mL containing 10 mg THC and 200 mg CBD) or matched placebo (2 mL containing no cannabinoids). The 1:20 ratio of THC to CBD was chosen to harness the sedating properties of THC while including some of the potential anti-anxiety properties of CBD,65 given that anxiety is a very common comorbidity in people with insomnia disorder.66 67 As noted above, there is also possibility that this dose of CBD might reduce some of the possible adverse effects of THC (e.g., anxiety, memory impairment). The chosen ratio also mimics naturalistic findings in recent surveys where individuals reported using cannabis with higher CBD concentrations in addition to THC to effectively manage insomnia symptoms.68 69 The THC dose (10 mg) was chosen as being the maximum dose that is likely to induce subjective drug effects of feeling ‘sleepy/tired’ without impairing cognitive performance (e.g., reaction time tasks) or producing significant intoxication in naïve or occasional cannabis users.60 A significant intoxicating effect might inadvertently cause a stimulatory response and interfere with sleep induction.60 70
Randomisation and allocation concealment
Each participant will be randomly allocated to one of two treatment sequences: (1) ETC120–placebo, or (2) placebo–ETC120. As this is a blinded study, the participant, the study staff (including the medical doctor) and the outcome assessors will not be aware of which treatment order participants have been allocated to. Method of allocation concealment will involve central randomisation by computer prepared by the trial statistician (NSM) and identical containers numbered according to the randomisation sequence prepared by the drug distributor. Neither the drug distributer or the trial statistician will meet any prospective or enrolled participants or be involved in any day-to-day trial process. The sequence will be computer-generated using a simple 1:1 randomisation ratio by the trial statistician, and by the order of participant enrolment. The sequence will be stored in a password-protected data management system and cannot be accessed by blinded study staff who have contact with participants. The order of treatment will only be known by the drug distributer and the trial statistician. In the event of a serious adverse event (SAE) or reaction, the allocation list will be retrieved from the unblinded trial statistician or drug distributer to reveal the participant’s allocated treatment during the trial.
Study objectives
The primary outcome of the study is to assess the effect of 10 mg THC and 200 mg CBD on sleep continuity (wake after sleep onset) and quantity (total sleep time) assessed using attended overnight full polysomnography in participants with chronic insomnia disorder.
Secondary objectives include:
To determine changes in sleep microarchitecture metrics measured using high-density EEG and source modelling in participants with chronic insomnia disorder treated with ETC120 relative to placebo.
To assess next-day neurobehavioural functioning (cognition, alertness and simulated driving performance) in participants with chronic insomnia disorder treated with ETC120 relative to placebo.
To demonstrate feasibility of a cannabinoid study in chronic insomnia and establish clinical trial procedures for future trials in this area.
The ANZCTR trial registry has a comprehensive list of the trial’s primary and secondary outcomes. See online supplementary file 2 for WHO Trial Registration Data Set.
bmjopen-2019-034421supp002.pdf (26.6KB, pdf)
Study visits and procedures
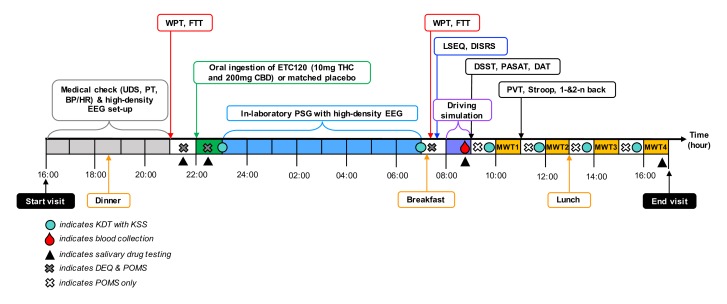
Screening
A flowchart of the study is depicted in figure 1. Initial suitability assessment via a brief online questionnaire and a follow-up telephone screen will be conducted by the study investigator. Written informed consent will be obtained by the study medical doctor before conducting an interview to ascertain sleep difficulties and diagnose ICSD-3 chronic insomnia disorder (Visits 1–2). Individuals will then undergo comprehensive screening to be completed within one month of study entry, which will include a diagnostic sleep study at the Woolcock Clinic to exclude sleep disorders other than insomnia disorder (unless one has already been conducted in the past 12 months). The Insomnia Severity Index71 (ISI; measure of nature, severity, and impact of insomnia), the Pittsburgh Sleep Quality Inventory72 (PSQI; measure of sleep quality and sleep habits), the Epworth Sleepiness Scale73 (ESS; measure of daytime sleepiness), the Hospital Anxiety Depression Scale74 (HADS; measure of anxiety and depression) and the Patient Health Questionnaire75 (PHQ-9; multi-purpose tool for assessing severity of depression) will be administered to phenotype insomnia symptoms and to assess suitability for study inclusion. All participants will be screened for prior cannabis use history (ie, whether they have consumed cannabis in the past, the form(s) in which it was consumed, and frequency of use) as well as for past or present cannabis use disorder as per the ICD-10 criteria.76 A urine specimen will be screened (DrugCheck NxStep OnSite Drug Test, Minnesota, USA) to rule out recent drug use. Participants testing positive for any drug (cannabis, cocaine, benzodiazepines, opiates or amphetamines/MDMA/methamphetamines) will result in exclusion or rescheduled at the studymedical doctor’s discretion. A standard 12-lead electrocardiogram (ECG) will be recorded to screen for any clinically relevant cardiovascular abnormalities. Rapid urine pregnancy test (Alere HCG Combo Cassette, Massachusetts, USA) will be administered to female participants, and identification of pregnancy will result in exclusion. Participants will then be instructed to maintain a sleep diary and wear a wrist-worn commercially available device (Actiwatch 2, Philips Respironics) to monitor sleep and wake periods for one week. These data will allow the study team to estimate the participant’s individual typical sleep-onset and wake-onset times for the study assessment visits as well as rule out advanced or delayed sleep-wake phase syndrome.
Figure 1.
Study flow diagram.
Following screening, the participants will undergo a structural brain MRI at a medical imaging clinic (Visit 3). Then, participants will attend the sleep clinic for an orientation session (Visit 4) to practise wearing the high-density EEG sensor cap during a short nap opportunity as well as complete a familiarisation and practice drive on the driving simulator. Participants will then be asked to maintain consistent sleep-onset and wake-onset times, confirmed by at-home sleep diary and actigraphy for one week prior to each study assessment visit. Participants will be instructed to abstain from illicit drug use for the duration of the study (ie, from pre-enrolment until after the final study assessment visit) and to refrain from consuming alcohol and caffeine for 24 hours prior to and during the study assessment visits, but to continue use of any regular prescribed medications (except those listed in the exclusion criteria). Standardised meals and snacks will be provided for participants at each study assessment visit. Table 1 depicts the schedule of visits and procedures from pre-enrolment to study completion.
Table 1.
Schedule of study visits and procedures
| Measure | Visit 1: Medical assessment | Visit 2: Diagnostic sleep study | At-home sleep monitoring | Visit 3: Brain MRI | Visit 4: Practice session | At-home sleep monitoring | Visit 5: Study assessment visit 1 | Washout & at-home sleep monitoring | Visit 6: Study assessment visit 2 | ||
| Evening | Daytime | Evening | Daytime | ||||||||
| Informed consent | ⚫ | ||||||||||
| Physical assessment (vital signs) | ⚫ | ⚫ | ⚫ | ||||||||
| ECG | ⚫ | ||||||||||
| Baseline questionnaires (ISI, PSQI, ESS, HADS, PHQ-9) | ⚫ | ||||||||||
| Urinary drug/alcohol screen | ⚫ | ⚫ | ⚫ | ||||||||
| Pregnancy test | ⚫ | ⚫ | ⚫ | ||||||||
| Overnight PSG (standard clinical EEG) | ⚫ | ||||||||||
| Brain MRI | ⚫ | ||||||||||
| Actigraphy | ⚫ | ⚫ | ⚫ | ||||||||
| Karolinska sleep diary | ⚫ | ⚫ | ⚫ | ||||||||
| Salivary drug screen (Securetec DrugWipe & Dräger 5000) | ⚫ | ⚫ | ⚫ | ⚫ | |||||||
| Saliva collection (Quantisal) | ⚫ | ⚫ | ⚫ | ⚫ | |||||||
| Mood (POMS abbreviated) | ⚫ | ⚫ | ⚫ | ⚫ | |||||||
| Memory Tasks – Consolidation (WPT & FTT) | ⚫ | ⚫ | |||||||||
| Study drug administration | ⚫ | ⚫ | |||||||||
| DEQ | ⚫ | ⚫ | ⚫ | ⚫ | |||||||
| KDT | ⚫ | ⚫ | ⚫ | ⚫ | |||||||
| Overnight PSG (Research high-density EEG) | ⚫ | ⚫ | |||||||||
| Blood plasma collection | ⚫ | ⚫ | |||||||||
| Memory Tasks - Test (WPT & FTT) | ⚫ | ⚫ | |||||||||
| Simulated driving performance task | ⚫ | ⚫ | |||||||||
| DISRS | ⚫ | ⚫ | |||||||||
| LSEQ | ⚫ | ⚫ | |||||||||
| Cognitive test battery (DSST, DAT, PASAT, PVT, Stroop test and 1 and 2 n-back task) | ⚫ | ⚫ | |||||||||
| MWT | ⚫ | ⚫ | |||||||||
DAT, Divided Attention Task; DEQ, Drug Effects Questionnaire; DISRS, Daytime Insomnia Symptoms Response Scale; DSST, Digit Symbol Substitution Test; ECG, electrocardiogram; EEG, electroencephalography; ESS, Epworth Sleepiness Scale; FTT, Finger Tapping Task; HADS, Hospital Anxiety Depression Scale; ISI, Insomnia Severity Index; KDT, Karolinska Drowsiness Test; KSS, Karolinska Sleepiness Scale; LSEQ, Leeds Sleep Evaluation Questionnaire; MRI, magnetic resonance imaging; MWT, Maintenance of Wakefulness Test; PASAT, Paced Auditory Serial Addition Task; PHQ-9, Patient Health Questionnaire; POMS, Profile of Mood States; PSG, polysomnography; PSQI, Pittsburgh Sleep Quality Inventory; PVT, Psychomotor Vigilance Task; WPT, Word Pairs Task.
Study assessment visits
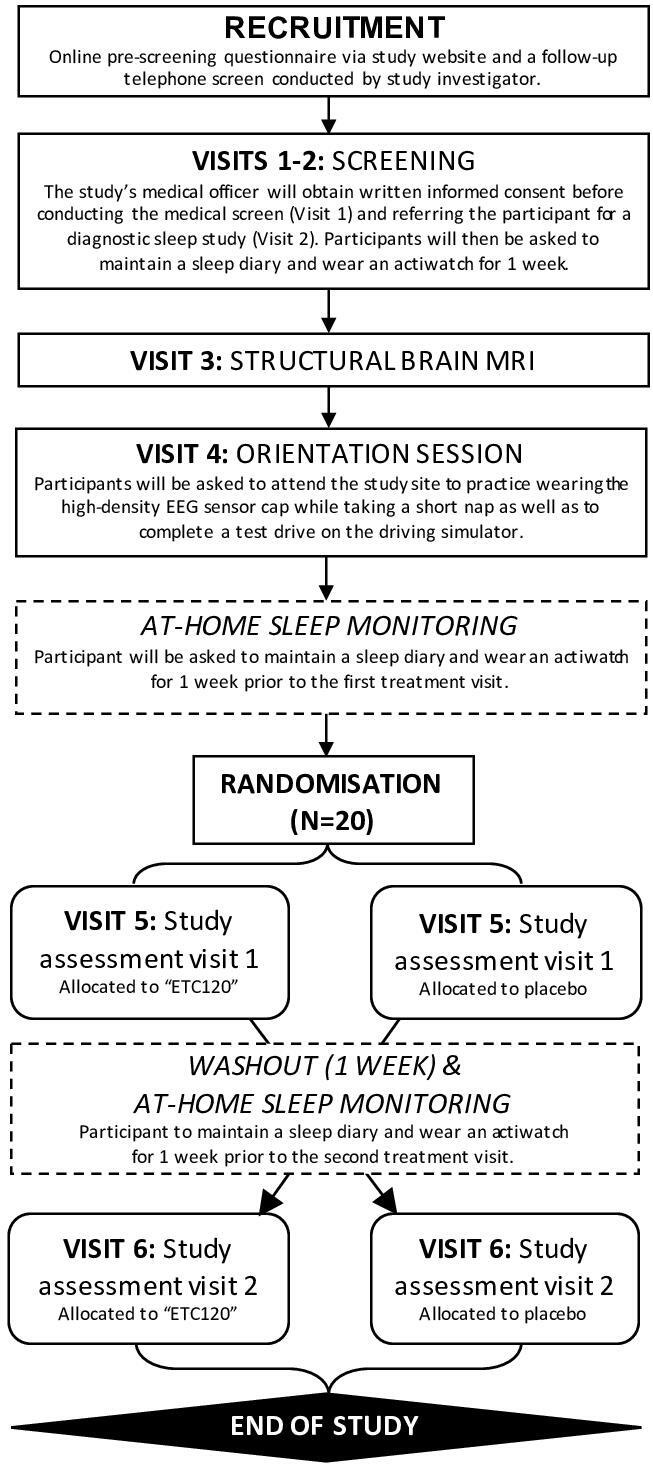
Participants will arrive at the clinic at approximately 16:00 hours for each study assessment visit (Visit 5 and 6; see figure 2). Drug-free and alcohol-free status and pregnancy status will be confirmed as described earlier.
Figure 2.
Schedule of events during study assessment visits. BP/HR, blood pressure/heart rate; CBD, cannabidiol; DAT, Divided Attention Task; DEQ, Drug Effects Questionnaire; DISRS, Daytime Insomnia Symptom Response Scale; DSST, Digit Symbol Substitution Task; EEG, electroencephalography; FTT, Finger Tapping Task; KDT, Karolinska Drowsiness Test; KSS, Karolinska Sleepiness Scale; LSEQ, Leeds Sleep Evaluation Questionnaire; MWT, Maintenance of Wakefulness Test; PASAT, Paced Auditory Serial Addition Task; POM, Profile of Mood States; PT, pregnancy test; PSG, polysomnography; PVT, Psychomotor Vigilance Task; THC, delta-9-tetrahydrocannabinol; UDS, urinary drug screen; WPT, Word Pairs Task.
Memory consolidation
To assess the next-day effects of ETC120 on memory consolidation, participants will be required to learn the Word Pairs Task (WPT; a declarative memory task) and the Finger Tapping Task (FTT; a procedural memory task) prior to drug administration at approximately 21:00 hours on the night of each study assessment visit and will be re-tested the following morning at approximately 07:30 hours.
Study drug administration
The study’s medical doctor will prepare the study drug on the same day of the study assessment visit by drawing 2 mL of the active drug or matched placebo in an amber plastic syringe secured with a tip cap. To mask smell and taste, participants will be instructed to consume one peppermint lozenge (Fisherman’s Friend Mint; Lofthouse of Fleetwood, England) immediately prior to drug administration. One hour prior to the participant’s typical sleep-onset time, the study investigator will then instruct and directly observe the participant to orally ingest the fixed dose of the study drug. This timeframe was chosen to represent the THC Tmax following a single oral dose of 10 mg THC.60 All participants will be given an 8-hour sleep opportunity. Time of drug administration is relative to the participant’s typical sleep-onset time, which may vary up to a maximum of 45 min.
Assessment of sleepiness
Participants will be administered the Karolinska Drowsiness Test (KDT) in conjunction with the Karolinska Sleepiness Scale (KSS), two measures that assess physiological and subjective sleepiness respectively,77 78 immediately before bedtime, immediately upon awakening, and at 10:00, 12:00, 14:00, and 16:00 hours coinciding with the Maintenance of Wakefulness Tests (MWT) described later. The main outcome measure is resting wake EEG power during the KDT before and after polysomnography.
Polysomnography with high-density EEG
Participants will undergo an in-laboratory 256-electrode high-density EEG (Electrical Geodesics, Oregon, USA) full polysomnography which includes electrooculogram (EOG), electromyogram (EMG), ECG, pulse oximetry and a position sensor. Sleep recordings will be scored by a sleep technologist specialising in high-density EEG and reviewed by a certified sleep physician. The GeoScan device will be used to measure, identify and create a three-dimensional coordinate file of the 256-electrode locations on the high-density EEG sensor cap. This will be combined with each individual participant’s structural brain MRI scan to localise the source of brain activity to specific brain regions.
Subjective measurements
Mood will be assessed using the Profile of Mood States (POMS) abbreviated version79 at baseline, 60 min post-drug administration, and the next-day at approximately 08:00, 10:00, 12:00, 14:00 and 16:00 hours. Subjective drug effects will be assessed using the Drug Effects Questionnaire (DEQ) which includes a series of visual analogue scales at baseline, 60 min post-drug administration and the next-day at approximately 08:00. Measurements will stop after the 08:00 timepoint because subjective drug effects following a single acute dose are not expected to persist beyond this time. On the DEQ, participants will rate on a 100 mm line their responses to the statements: ‘Strength of drug effect’, ‘Liking of drug effect’, ‘Feeling stoned’ and ‘Feeling sedated’, with all scales unipolar. Perceived changes in sleep and daytime function will be assessed using the Leeds Sleep Evaluation Questionnaire (LSEQ)80 and the Daytime Insomnia Symptom Response Scale (DISRS)81 at approximately 07:30 hours the morning post-drug administration.
Driving performance
At 08:00 hours the next day, participants will be asked to complete a 30 min simulated driving task using a custom-built fixed-base computerised driving simulator (Hyperdrive, Adelaide, Australia) equipped with original vehicle controls (steering wheel, indicators, seat, safety belt), hi-resolution Fanatec pedals, and a servo motor wheel base (Endor AG, Landshut, Germany) linked to four networked computers running the SCANeR Studio simulation engine software (V.1.6, AVSimulation, Paris, France). The driving scenario is identical to that previously employed in a study examining the effects of vaporised cannabis on driving performance in healthy volunteers.61 Outcome measures include standard deviation of lateral position (SDLP) and number of lane crossings as measures of lateral vehicle control (ie, lane swerving behaviour), and average speed and standard deviation of speed (SDSP) as measures of longitudinal vehicle control. These outcome parameters have previously demonstrated sensitivity to the impairing effects of sleep disturbance,82 hypnotic medication83 and cannabis administration.84
Salivary drug testing
Given the current legal framework for driving under the influence of cannabis in Australia (ie, detection of THC in saliva with no functional assessment),85 all participants will undergo salivary drug testing to test for the presence of THC. Oral fluid samples will be collected using Quantisal collection devices (Immunalysis, Pomona, California, USA) at baseline, 30 min post-drug administration, and the next-day after completing the driving simulation (approximately 09:00 hours) and at completion of the study visit (17:00 hours). Samples will be kept at −80°C prior to analysis for THC and CBD using liquid chromatography-tandem mass spectrometry (LC-MS/MS). Oral fluid will also be screened for cannabis (THC) using two devices: DrugWipe 5 s (Securetec, Neubiberg, Germany) and Dräger Drug Test 5000 (Drägerwerk AG & Co., Lübeck, Germany) at four timepoints: baseline (30 min prior to drug administration), T1 (30 min after drug administration), T2 (08:30 hours; the next day immediately after completing the driving task) and T3 (17:00 hours; prior to leaving the study site). Both devices have a manufacturer-specified detection limit of 10 ng/mL THC. Participants will be provided with taxi vouchers to and from the study site at both study assessment visits as they will not be permitted to drive. Participants will be given explicit instruction not to drive for at least 24 hours after leaving the study site to allow adequate time for drug washout following a single dose.
Blood collection and plasma cannabinoid levels
Blood will be collected once via venepuncture into EDTA vacutainer tubes (Becton, Dickinson and Company, New Jersey, USA) at approximately 08:45 hours, immediately after the driving performance task, to measure levels of THC and other cannabinoids the morning post-drug administration. Blood will be centrifuged at 1500×g for 10 min at 4°C with the supernatant plasma aliquoted and stored in 1.8 mL cryotubes at −80°C until subsequent analysis. Plasma will be analysed via LC-MS/MS according to previously published methods85 86 for cannabinoids (CBD, THC) and their metabolites (11-OH-THC, THC-COOH; 7-COOH-CBD, 7-OH-CBD and 6-OH-CBD) as well as a range of endocannabinoid and related molecules (anandamide, 2-AG, 1-AG, oleoylethanolamide (OEA), palmitoylethanolamide (PEA), linoyl-ethanolamide (LEA) and oleamide).
Cognitive performance
Cognitive assessment will take place the morning post-drug administration (see table 1), to explore the functional consequences of 10 mg THC and 200 mg CBD on next-day daytime function. This will be measured from approximately 09:00 hours using the following battery of computerised cognitive/psychomotor tasks known to be sensitive to the impairing effects of THC60 70: Digit Symbol Substitution Test (DSST; measure of processing speed, working memory and attention), Divided Attention Task (DAT; measure of processing speed, working memory and attention) and Paced Auditory Serial Addition Task (PASAT; measure of processing speed and sustained attention). Other cognitive tasks to be administered in conjunction include the Psychomotor Vigilance Task (PVT; simple reaction time task measuring sustained attention), Stroop test (a measure of executive functioning), and the 1- and 2-n back test (a measure of working memory and information processing).
Maintenance of Wakefulness Test
The Maintenance of Wakefulness Test (MWT) is a validated, objective measure of an individual’s ability to stay awake in a room with low levels of stimulation that will test for drowsiness the next-day post-drug administration.86 As recommended by American Academy of Sleep Medicine (AASM) practice parameters,87 four 40 min MWT trials will be administered at 10:00, 12:00, 14:00 and 16:00 hours on the day post-drug administration. Participants will be instructed to lay semi-recumbent on a bed (above the covers) in a darkened room and try to remain awake for 40 min. An experienced sleep technician will record the polysomnography using high-density EEG. Trials will end after 40 min if no sleep occurs, or after unequivocal sleep, defined as three consecutive epochs of non-rapid eye movement stage 1 (N1) sleep or one epoch of any other sleep stage (N2, N3, N4 or REM). The main outcome measure is the mean sleep latency of the four MWT trials.
Patient and public involvement
The present trial was developed by the investigators based on previous clinical experience and gaps identified in the existing literature. Patients were not involved in the design of the study. The outcomes are commonly used assessments of insomnia in research. The cost of interventions and outcome measurements are covered by the study funding. All participants will be offered a clinical follow-up appointment with a sleep physician on conclusion of the study. Participants will receive a summary of the study results once published.
Data collection and management
All clinical data and information obtained for the purpose of this research that could identify participants will be treated as confidential and securely stored, adhering to the University regulations and the Australian Code for the Responsible Conduct of Research. Participant data will be identified by a unique code number that will be allocated after the participant gives consent to participate in the study. The unique code linking the participant’s identity/personal details (e.g., name, date of birth) will be stored in a password-encrypted file that will not be accessible from the internet. All data will be stored at the Woolcock Institute of Medical Research in written and computerised formats. Participant information will reside on a secure server that is regularly backed up. All data will be stored securely for at least 15 years. Only researchers affiliated with the study will have access to participant data. Study progress and safety will be monitored and evaluated internally in an ongoing fashion by the Trial Management Group consisting of the principal investigators, trial coordinator, research assistants, trial statistician, data manager and sleep clinic manager. There are no planned interim analyses. The final decision to terminate the trial lies with the principal investigators and will be based on (1) safety data and (2) target recruitment number. The investigator team will conduct an internal 3-monthly review of all adverse events and reactions and if after discussion, the rate of such events is deemed unacceptable then the study will be stopped and the human research ethics committee will be advised of the decision.
Sample size and statistical analyses
This protocol was designed to be a single dose, proof-of-concept study to ascertain initial safety and efficacy of the study drug in participants with chronic insomnia disorder. As there is no commercially available power calculation software for mixed-model analyses available at present, using a simple paired t-test, a crossover trial of 20 participants is adequately powered to detect an effect size of 0.67 with 80% power at an alpha level of 0.05 (two-tailed). Data obtained will guide future studies by providing 95% confidence limits for sensitivity analyses for power calculations of a larger trial if warranted. Data will be analysed using mixed-model analyses of variance in SAS (SAS Institute, V.9.4) to test whether either of the treatments are different from the other. Order and treatment will be fixed effects and the patient code will be used as a random effect.88 Treatment by order effect will not be tested. All variables are suitable for mixed-model analyses except for the adverse event profile which will be tabulated but not statistically tested. The least-squares means procedure will be used in the mixed-model analyses to handle missing data. All participants will be analysed in the groups they have been randomised to. Primary outcomes will be interpreted as affected if either are significant at 0.05.
Significance
Cannabis is commonly believed to be a useful sleep aid. However, there are no published studies to-date assessing its effects on sleep in people with physician-confirmed chronic insomnia disorder. Given the increased consumer interest and expansion of legal prescription for cannabis globally, it is important to better understand how cannabis-based medicines affect sleep and next-day function prior to becoming a routine intervention in clinical practice. This is particularly important as sleep disturbances are fiercely comorbid in many chronic health conditions such as pain; key indications for the prescription of cannabis-based medicines around the world.89 Of note, this is a proof-of-concept trial that is limited by its small sample size and single-dose design, precluding examination of the long-term effects of this cannabis-based medicine in this clinical population. Moreover, the study cannot assess the individual contribution of THC and CBD. Nonetheless, the current study is a rigorous double-blinded, placebo-controlled, within-subjects, crossover design that will provide a preliminary signal on the efficacy and safety of a pharmaceutical-grade cannabis-based medicine in people with chronic insomnia disorder, and will hopefully help inform the development of future longer-term research trials.
Ethics and dissemination
Ethics approval was received from Bellberry Human Research Ethics Committee (2018-04-284). The findings of this trial will be disseminated in peer-reviewed journal publications and at academic conferences. The sponsor controls the final decision regarding all aspects of the trial including dissemination of results. The study investigator is responsible for communicating important protocol modifications to relevant parties.
Supplementary Material
Footnotes
Twitter: @NatSleep
Contributors: AS, RRG, NSM, ALD, CJG, DJB, KW, BJY, RV, CI, JCA, ISM and CMH were involved in the methodological design and drafting of the trial protocol. RRG and CMH are the medical and non-medical principal investigator, respectively, who have overall responsibility for the design, conduct and decision to submit for publication. NSM is the trial statistician who designed and wrote the analysis plan. AS is the trial coordinator responsible for collecting trial data. AS drafted the manuscript. All authors read and approved the final manuscript.
Funding: This study is funded by the Lambert Initiative for Cannabinoid Therapeutics, a philanthropically funded centre for cannabinoid research at the University of Sydney. AS was supported by the Australian Government Research Training Program (RTP) and the Vice-Chancellor’s Research Scholarship (VCRS) at the University of Sydney. CMH (APP1104003) and ALD (APP1107716) were supported by Dementia Research Development Fellowships of the Australian National Health and Medical Research Council-Australian Research Council (NHMRC-ARC). RRG was supported by an NHMRC Senior Principal Research Fellowship (APP1106974). The investigational product was purchased from Linnea (Ticino, Switzerland) who were not involved in the conception or design of this study.
Competing interests: ISM is Academic Director of the Lambert Initiative for Cannabinoid Therapeutics. He has served as an expert witness in various medicolegal cases involving cannabis, has received honoraria from Janssen, is currently a consultant to Kinoxis Therapeutics, and has received research funding and fellowship support from the Lambert Initiative for Cannabinoid Therapeutics, National Health and Medical Research Council (NHMRC) and Australian Research Council. He holds a variety of patents for cannabinoid and non-cannabinoid therapeutics. RV has received financial compensation from Zynerba Pharmaceuticals, Canopy Health Innovations and Brain Solutions. JCA is Deputy Academic Director of the Lambert Initiative for Cannabinoid Therapeutics. He has served as an expert witness in various medicolegal cases involving cannabis and recently served as a temporary advisor to the WHO on their review of cannabis and the cannabinoids. His research is funded by the NHMRC, Canopy Growth Corporation and the Lambert Initiative for Cannabinoid Therapeutics. JCA also holds several patents on novel cannabinoid therapies. All other authors have no conflicts of interest to disclose.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Morin CM, Benca R. Chronic insomnia. The Lancet 2012;379:1129–41. 10.1016/S0140-6736(11)60750-2 [DOI] [PubMed] [Google Scholar]
- 2.Van Reeth O, Weibel L, Spiegel K, et al. Interactions between stress and sleep: from basic research to clinical situations. Sleep Med Rev 2000;4:201–20. [Google Scholar]
- 3.Roth T. Insomnia: definition, prevalence, etiology, and consequences. J Clin Sleep Med 2007;3:S7. 10.5664/jcsm.26929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Psychiatric Association (ASA) Diagnostic and statistical manual of mental disorders. 5th Edition Arlington, VA, 2013. [Google Scholar]
- 5.American Academy of Sleep Medicine International classification of sleep disorders. 3rd Edition Darien: IL, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morin CM, LeBlanc M, Daley M, et al. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med 2006;7:123–30. 10.1016/j.sleep.2005.08.008 [DOI] [PubMed] [Google Scholar]
- 7.Morin CM, Bélanger L, LeBlanc M, et al. The natural history of insomnia: a population-based 3-year longitudinal study. Arch Intern Med 2009;169:447–53. 10.1001/archinternmed.2008.610 [DOI] [PubMed] [Google Scholar]
- 8.Ji X, Ivers H, Savard J, et al. Residual symptoms after natural remission of insomnia: associations with relapse over 4 years. Sleep 2019;42:zsz122. 10.1093/sleep/zsz122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bertisch SM, Pollock BD, Mittleman MA, et al. Insomnia with objective short sleep duration and risk of incident cardiovascular disease and all-cause mortality: sleep heart health study. Sleep 2018;41:zsy047. 10.1093/sleep/zsy047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord 2011;135:10–19. 10.1016/j.jad.2011.01.011 [DOI] [PubMed] [Google Scholar]
- 11.Leggett AN, Sonnega AJ, Lohman MC. The association of insomnia and depressive symptoms with all-cause mortality among middle-aged and old adults. Int J Geriatr Psychiatry 2018;33:1265–70. 10.1002/gps.4923 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Riemann D, Voderholzer U. Primary insomnia: a risk factor to develop depression? J Affect Disord 2003;76:255–9. 10.1016/S0165-0327(02)00072-1 [DOI] [PubMed] [Google Scholar]
- 13.de Almondes KM, Costa MV, Malloy-Diniz LF, et al. Insomnia and risk of dementia in older adults: systematic review and meta-analysis. J Psychiatr Res 2016;77:109–15. 10.1016/j.jpsychires.2016.02.021 [DOI] [PubMed] [Google Scholar]
- 14.Hung C-M, Li Y-C, Chen H-J, et al. Risk of dementia in patients with primary insomnia: a nationwide population-based case-control study. BMC Psychiatry 2018;18:38. 10.1186/s12888-018-1623-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sivertsen B, Øverland S, Pallesen S, et al. Insomnia and long sleep duration are risk factors for later work disability. The Hordaland health study. J Sleep Res 2009;18:122–8. 10.1111/j.1365-2869.2008.00697.x [DOI] [PubMed] [Google Scholar]
- 16.Lallukka T, Haaramo P, Rahkonen O, et al. Joint associations of sleep duration and insomnia symptoms with subsequent sickness absence: the Helsinki health study. Scand J Public Health 2013;41:516–23. 10.1177/1403494813481647 [DOI] [PubMed] [Google Scholar]
- 17.Bin YS, Marshall NS, Glozier N. The burden of insomnia on individual function and healthcare consumption in Australia. Aust N Z J Public Health 2012;36:462–8. 10.1111/j.1753-6405.2012.00845.x [DOI] [PubMed] [Google Scholar]
- 18.Franzen PL, Buysse DJ. Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications. Dialogues Clin Neurosci 2008;10:473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Okajima I, Komada Y, INOUE Y. A meta-analysis on the treatment effectiveness of cognitive behavioral therapy for primary insomnia. Sleep Biol Rhythms 2011;9:24–34. 10.1111/j.1479-8425.2010.00481.x [DOI] [Google Scholar]
- 20.Cheung JMY, Bartlett DJ, Armour CL, et al. To drug or not to drug: a qualitative study of patients' decision-making processes for managing insomnia. Behav Sleep Med 2018;16:1–26. 10.1080/15402002.2016.1163702 [DOI] [PubMed] [Google Scholar]
- 21.Miller CB, Valenti L, Harrison CM, et al. Time trends in the family physician management of insomnia: the Australian experience (2000-2015). J Clin Sleep Med 2017;13:785–90. 10.5664/jcsm.6616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mendelson WB, Roth T, Cassella J, et al. The treatment of chronic insomnia: drug indications, chronic use and abuse liability. summary of a 2001 new clinical drug evaluation unit meeting symposium. Sleep Med Rev 2004;8:7–17. 10.1016/S1087-0792(03)00042-X [DOI] [PubMed] [Google Scholar]
- 23.Bastien CH, LeBlanc M, Carrier J, et al. Sleep EEG power spectra, insomnia, and chronic use of benzodiazepines. Sleep 2003;26:313–7. 10.1093/sleep/26.3.313 [DOI] [PubMed] [Google Scholar]
- 24.Bachhuber M, Arnsten JH, Wurm G. Use of cannabis to relieve pain and promote sleep by customers at an adult use dispensary. J Psychoactive Drugs 2019;51:400–4. 10.1080/02791072.2019.1626953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pertwee RG. The pharmacology of cannabinoid receptors and their ligands: an overview. Int J Obes 2006;30:S13–18. 10.1038/sj.ijo.0803272 [DOI] [PubMed] [Google Scholar]
- 26.Sanford AE, Castillo E, Gannon RL. Cannabinoids and hamster circadian activity rhythms. Brain Res 2008;1222:141–8. 10.1016/j.brainres.2008.05.048 [DOI] [PubMed] [Google Scholar]
- 27.Vaughn LK, Denning G, Stuhr KL, et al. Endocannabinoid signalling: has it got rhythm? Br J Pharmacol 2010;160:530–43. 10.1111/j.1476-5381.2010.00790.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pertwee R. The diverse CB1 and CB2 receptor pharmacology of three plant cannabinoids: Δ9‐tetrahydrocannabinol, cannabidiol and Δ9‐tetrahydrocannabivarin. Br J Clin Pharmacol 2008;153:199–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Herkenham M, Lynn AB, Little MD, et al. Cannabinoid receptor localization in brain. Proc Natl Acad Sci U S A 1990;87:1932–6. 10.1073/pnas.87.5.1932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Murillo-Rodríguez E. The role of the CB1 receptor in the regulation of sleep. Prog Neuropsychopharmacol Biol Psychiatry 2008;32:1420–7. 10.1016/j.pnpbp.2008.04.008 [DOI] [PubMed] [Google Scholar]
- 31.Pava MJ, Makriyannis A, Lovinger DM. Endocannabinoid signaling regulates sleep stability. PLoS One 2016;11:e0152473. 10.1371/journal.pone.0152473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Elmes MW, Kaczocha M, Berger WT, et al. Fatty acid-binding proteins (FABPs) are intracellular carriers for Δ9-tetrahydrocannabinol (THC) and cannabidiol (CBD). J Biol Chem 2015;290:8711–21. 10.1074/jbc.M114.618447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McPartland JM, Duncan M, Di Marzo V, et al. Are cannabidiol and Δ(9) -tetrahydrocannabivarin negative modulators of the endocannabinoid system? A systematic review. Br J Pharmacol 2015;172:737–53. 10.1111/bph.12944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.D'Souza DC, Cortes-Briones J, Creatura G, et al. Efficacy and safety of a fatty acid amide hydrolase inhibitor (PF-04457845) in the treatment of cannabis withdrawal and dependence in men: a double-blind, placebo-controlled, parallel group, phase 2A single-site randomised controlled trial. Lancet Psychiatry 2019;6:35–45. 10.1016/S2215-0366(18)30427-9 [DOI] [PubMed] [Google Scholar]
- 35.Murillo-Rodriguez E, Blanco-Centurion C, Sanchez C, et al. Anandamide enhances extracellular levels of adenosine and induces sleep: an in vivo microdialysis study. Sleep 2003;26:943–7. 10.1093/sleep/26.8.943 [DOI] [PubMed] [Google Scholar]
- 36.Mechoulam R, Fride E, Hanus L, et al. Anandamide may mediate sleep induction. Nature 1997;389:25–6. 10.1038/37891 [DOI] [PubMed] [Google Scholar]
- 37.Murillo-Rodríguez E, Sánchez-Alavez M, Navarro L, et al. Anandamide modulates sleep and memory in rats. Brain Res 1998;812:270–4. 10.1016/S0006-8993(98)00969-X [DOI] [PubMed] [Google Scholar]
- 38.Murillo-Rodríguez E, Cabeza R, Méndez-Díaz M, et al. Anandamide-Induced sleep is blocked by SR141716A, a CB1 receptor antagonist and by U73122, a phospholipase C inhibitor. Neuroreport 2001;12:2131–6. 10.1097/00001756-200107200-00018 [DOI] [PubMed] [Google Scholar]
- 39.Padwal RS, Majumdar SR. Drug treatments for obesity: orlistat, sibutramine, and rimonabant. Lancet 2007;369:71–7. 10.1016/S0140-6736(07)60033-6 [DOI] [PubMed] [Google Scholar]
- 40.Tham M, Yilmaz O, Alaverdashvili M, et al. Allosteric and orthosteric pharmacology of cannabidiol and cannabidiol-dimethylheptyl at the type 1 and type 2 cannabinoid receptors. Br J Pharmacol 2019;176:1455–69. 10.1111/bph.14440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Laprairie RB, Bagher AM, Kelly MEM, et al. Cannabidiol is a negative allosteric modulator of the cannabinoid CB1 receptor. Br J Pharmacol 2015;172:4790–805. 10.1111/bph.13250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Todd SM, Arnold JC. Neural correlates of interactions between cannabidiol and Δ(9) -tetrahydrocannabinol in mice: implications for medical cannabis. Br J Pharmacol 2016;173:53–65. 10.1111/bph.13333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hindocha C, Freeman TP, Schafer G, et al. Acute effects of delta-9-tetrahydrocannabinol, cannabidiol and their combination on facial emotion recognition: a randomised, double-blind, placebo-controlled study in cannabis users. Eur Neuropsychopharmacol 2015;25:325–34. 10.1016/j.euroneuro.2014.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nicholson AN, Turner C, Stone BM, et al. Effect of delta-9-tetrahydrocannabinol and cannabidiol on nocturnal sleep and early-morning behavior in young adults. J Clin Psychopharmacol 2004;24:305–13. 10.1097/01.jcp.0000125688.05091.8f [DOI] [PubMed] [Google Scholar]
- 45.Morgan CJA, Freeman TP, Schafer GL, et al. Cannabidiol attenuates the appetitive effects of delta 9-tetrahydrocannabinol in humans smoking their chosen cannabis. Neuropsychopharmacology 2010;35:1879–85. 10.1038/npp.2010.58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bhattacharyya S, Morrison PD, Fusar-Poli P, et al. Opposite effects of delta-9-tetrahydrocannabinol and cannabidiol on human brain function and psychopathology. Neuropsychopharmacology 2010;35:764–74. 10.1038/npp.2009.184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schubart CD, Sommer IEC, van Gastel WA, et al. Cannabis with high cannabidiol content is associated with fewer psychotic experiences. Schizophr Res 2011;130:216–21. 10.1016/j.schres.2011.04.017 [DOI] [PubMed] [Google Scholar]
- 48.Arkell TR, Lintzeris N, Kevin RC, et al. Cannabidiol (CBD) content in vaporized cannabis does not prevent tetrahydrocannabinol (THC)-induced impairment of driving and cognition. Psychopharmacology 2019;236:2713–24. 10.1007/s00213-019-05246-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bakas T, van Nieuwenhuijzen PS, Devenish SO, et al. The direct actions of cannabidiol and 2-arachidonoyl glycerol at GABAA receptors. Pharmacol Res 2017;119:358–70. 10.1016/j.phrs.2017.02.022 [DOI] [PubMed] [Google Scholar]
- 50.Kuhathasan N, Dufort A, MacKillop J, et al. The use of cannabinoids for sleep: a critical review on clinical trials. Exp Clin Psychopharmacol 2019;27:383–401. 10.1037/pha0000285 [DOI] [PubMed] [Google Scholar]
- 51.Babson KA, Sottile J, Morabito D. Cannabis, cannabinoids, and sleep: a review of the literature. Curr Psychiatry Rep 2017;19:23. 10.1007/s11920-017-0775-9 [DOI] [PubMed] [Google Scholar]
- 52.Gates PJ, Albertella L, Copeland J. The effects of cannabinoid administration on sleep: a systematic review of human studies. Sleep Med Rev 2014;18:477–87. 10.1016/j.smrv.2014.02.005 [DOI] [PubMed] [Google Scholar]
- 53.Russo EB, Guy GW, Robson PJ. Cannabis, pain, and sleep: lessons from therapeutic clinical trials of Sativex, a cannabis-based medicine. Chem Biodivers 2007;4:1729–43. 10.1002/cbdv.200790150 [DOI] [PubMed] [Google Scholar]
- 54.Cameron C, Watson D, Robinson J. Use of a synthetic cannabinoid in a correctional population for posttraumatic stress disorder-related insomnia and nightmares, chronic pain, harm reduction, and other indications: a retrospective evaluation. J Clin Psychopharmacol 2014;34:559–64. 10.1097/JCP.0000000000000180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fraser GA. The use of a synthetic cannabinoid in the management of treatment-resistant nightmares in posttraumatic stress disorder (PTSD). CNS Neurosci Ther 2009;15:84–8. 10.1111/j.1755-5949.2008.00071.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ware MA, Fitzcharles M-A, Joseph L, et al. The effects of nabilone on sleep in fibromyalgia: results of a randomized controlled trial. Anesth Analg 2010;110:604–10. 10.1213/ANE.0b013e3181c76f70 [DOI] [PubMed] [Google Scholar]
- 57.Chagas MHN, Eckeli AL, Zuardi AW, et al. Cannabidiol can improve complex sleep-related behaviours associated with rapid eye movement sleep behaviour disorder in Parkinson's disease patients: a case series. J Clin Pharm Ther 2014;39:564–6. 10.1111/jcpt.12179 [DOI] [PubMed] [Google Scholar]
- 58.Shannon S, Opila-Lehman J. Effectiveness of cannabidiol oil for pediatric anxiety and insomnia as part of posttraumatic stress disorder: a case report. Perm J 2016;20:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Blessing EM, Steenkamp MM, Manzanares J, et al. Cannabidiol as a potential treatment for anxiety disorders. Neurotherapeutics 2015;12:825–36. 10.1007/s13311-015-0387-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vandrey R, Herrmann ES, Mitchell JM, et al. Pharmacokinetic profile of oral cannabis in humans: blood and oral fluid disposition and relation to pharmacodynamic outcomes. J Anal Toxicol 2017;41:83–99. 10.1093/jat/bkx012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Arkell TR, Kevin R, Stuart J, et al. Detection of Δ9THC in oral fluid following vaporised cannabis with varied cannabidiol (CBD) content: an evaluation of two point‐of‐collection testing devices. Drug Test Anal 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chan A-W, Tetzlaff JM, Gøtzsche PC, et al. Spirit 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ 2013;346:e7586. 10.1136/bmj.e7586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.American Academy of Sleep Medicine Diagnostic and Coding Manual In: International classification of sleep disorders, 2005: 51–5. [Google Scholar]
- 64.Sprecher KE, Riedner BA, Smith RF, et al. High resolution topography of age-related changes in non-rapid eye movement sleep electroencephalography. PLoS One 2016;11:e0149770. 10.1371/journal.pone.0149770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Linares IM, Zuardi AW, Pereira LC, et al. Cannabidiol presents an inverted U-shaped dose-response curve in a simulated public speaking test. Braz J Psychiatry 2019;41:9–14. 10.1590/1516-4446-2017-0015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Taylor DJ, Lichstein KL, Durrence HH, et al. Epidemiology of insomnia, depression, and anxiety. Sleep 2005;28:1457–64. 10.1093/sleep/28.11.1457 [DOI] [PubMed] [Google Scholar]
- 67.Belleville G, Cousineau H, Levrier K, et al. Meta-Analytic review of the impact of cognitive-behavior therapy for insomnia on concomitant anxiety. Clin Psychol Rev 2011;31:638–52. 10.1016/j.cpr.2011.02.004 [DOI] [PubMed] [Google Scholar]
- 68.Belendiuk KA, Babson KA, Vandrey R, et al. Cannabis species and cannabinoid concentration preference among sleep-disturbed medicinal cannabis users. Addict Behav 2015;50:178–81. 10.1016/j.addbeh.2015.06.032 [DOI] [PubMed] [Google Scholar]
- 69.Pearce DD, Mitsouras K, Irizarry KJ. Discriminating the effects of cannabis sativa and cannabis indica: a web survey of medical cannabis users. J Altern Complement Med 2014;20:787–91. 10.1089/acm.2013.0190 [DOI] [PubMed] [Google Scholar]
- 70.Cousens K, DiMascio A. (−) δ 9 THC as an hypnotic. Psychopharmacologia 1973;33:355–64. [DOI] [PubMed] [Google Scholar]
- 71.Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med 2001;2:297–307. 10.1016/S1389-9457(00)00065-4 [DOI] [PubMed] [Google Scholar]
- 72.Buysse DJ, Reynolds CF, Monk TH, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 73.Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness scale. Sleep 1991;14:540–5. 10.1093/sleep/14.6.540 [DOI] [PubMed] [Google Scholar]
- 74.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. 10.1111/j.1600-0447.1983.tb09716.x [DOI] [PubMed] [Google Scholar]
- 75.Martin A, Rief W, Klaiberg A, et al. Validity of the brief patient health questionnaire mood scale (PHQ-9) in the general population. Gen Hosp Psychiatry 2006;28:71–7. 10.1016/j.genhosppsych.2005.07.003 [DOI] [PubMed] [Google Scholar]
- 76.World Health Organisation The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: World Health Organization, 1992. [Google Scholar]
- 77.Putilov AA, Donskaya OG. Construction and validation of the EEG analogues of the Karolinska sleepiness scale based on the Karolinska drowsiness test. Clin Neurophysiol 2013;124:1346–52. 10.1016/j.clinph.2013.01.018 [DOI] [PubMed] [Google Scholar]
- 78.Kaida K, Takahashi M, Åkerstedt T, et al. Validation of the Karolinska sleepiness scale against performance and EEG variables. Clinical Neurophysiology 2006;117:1574–81. 10.1016/j.clinph.2006.03.011 [DOI] [PubMed] [Google Scholar]
- 79.Curran SL, Andrykowski MA, Studts JL. Short form of the profile of mood states (POMS-SF): psychometric information. Psychol Assess 1995;7:80–3. 10.1037/1040-3590.7.1.80 [DOI] [Google Scholar]
- 80.Parrott AC, Hindmarch I. The Leeds Sleep Evaluation Questionnaire in psychopharmacological investigations - a review. Psychopharmacology 1980;71:173–9. 10.1007/BF00434408 [DOI] [PubMed] [Google Scholar]
- 81.Carney CE, Harris AL, Falco A, et al. The relation between insomnia symptoms, mood, and rumination about insomnia symptoms. J Clin Sleep Med 2013;9:567–75. 10.5664/jcsm.2752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Perrier J, Bertran F, Marie S, et al. Impaired driving performance associated with effect of time duration in patients with primary insomnia. Sleep 2014;37:1565–73. 10.5665/sleep.4012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Verster JC, Veldhuijzen DS, Volkerts ER. Residual effects of sleep medication on driving ability. Sleep Med Rev 2004;8:309–25. 10.1016/j.smrv.2004.02.001 [DOI] [PubMed] [Google Scholar]
- 84.Kevin RC, Allsop DJ, Lintzeris N, et al. Urinary cannabinoid levels during nabiximols (Sativex®)-medicated inpatient cannabis withdrawal. Forensic Toxicol 2017;35:33–44. 10.1007/s11419-016-0330-0 [DOI] [Google Scholar]
- 85.Schwope DM, Scheidweiler KB, Huestis MA. Direct quantification of cannabinoids and cannabinoid glucuronides in whole blood by liquid chromatography-tandem mass spectrometry. Anal Bioanal Chem 2011;401:1273–83. 10.1007/s00216-011-5197-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Baiardi S, Mondini S. Inside the clinical evaluation of sleepiness: subjective and objective tools. Sleep Breath 2019:1–9. 10.1007/s11325-019-01866-8 [DOI] [PubMed] [Google Scholar]
- 87.Littner MR, Kushida C, Wise M, et al. Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test. Sleep 2005;28:113–21. 10.1093/sleep/28.1.113 [DOI] [PubMed] [Google Scholar]
- 88.Marshall NS, Neill AM, Campbell AJ, et al. Randomised controlled crossover trial of humidified continuous positive airway pressure in mild obstructive sleep apnoea. Thorax 2005;60:427–32. 10.1136/thx.2004.032078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Aguilar S, Gutierrez V, Sanchez L, et al. Medicinal cannabis policies and practices around the world. International drug policy Consortium, 2018. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-034421supp001.pdf (88.3KB, pdf)
bmjopen-2019-034421supp002.pdf (26.6KB, pdf)