Abstract
Introduction
The current COVID-19 pandemic has prompted a timely response from the healthcare system train a large and diverse group of healthcare workers/responders swiftly.
Methods
In order to address this need, we created a downloadable pedagogical video content through first-person point-of-view to rapidly train users on COVID-19 procedures in the Revinax® Handbook mobile App. Eight new tutorials were designed through this technology platform to assist healthcare workers/responders caring for COVID-19 patients. A survey was then sent to assess their interest.
Results
In one-month since the App was created, it was downloaded by 12,516 users and a feedback survey determined that the users valued the tutorials in helping them learn COVID-19 procedures efficiently in real-time. The fast-growing number of downloads and positive user feedback evidences that we created a valuable educational tool with an emergent- and growing-demand.
Discussion
The 71.48% App user response rate, showed largely positive feedback of the COVID-19 tutorial. The fact that these healthcare workers/responders took the time to complete the survey during a pandemic was indicative of its immediate value. Further, the App users indicated that they FPV tutorial was rather helpful in addressing their training needs regarding their roles in COVID-19 patient care during the pandemic.
Conclusion
The tutorials were deployed to offer efficient and rapid global public health educational outreach as a tool to address COVID-19 healthcare training in a timely manner.
Keywords: COVID-19, Educational technology, Health personnel, Interactive tutorial, Mobile applications, Public health informatics, Video recording
Highlights
-
•
COVID-19 has caused a need for rapid training of healthcare workers/responders.
-
•
The Revinax Handbook was used to deploy globally COVID-19 tutorials as an App.
-
•
The tutorials were downloaded and well received by 12,516 App users, mostly nurses.
-
•
The 71.48% response rate, during a pandemic, evidenced the value of this App.
-
•
Data show that deploying FPV content through an App can help global health crises.
1. Introduction
Time to act has never been more crucial than the current coronavirus (hereon referred to as COVID-19) pandemic that has forced the immediate utilization of technology due to social distancing requirements and has also increased a complex set of challenges for the applied medical and public health systems to address in coordination with other countries globally. This situation is truly unprecedented, yet a major concern has been to institute a concerted effort in limiting sources of contamination from the greater population by limiting the number of patients seen that are only symptomatic to hospitals. The rationale for this strategy was to not overwhelm the hospitals capacity to operate and delivery adequate patient care during these trying times and is consistent from what we have learned from flattening the curve as the initial response (Branas et al., 2020). In the current COVID-19 surge that the world is facing, there is an eminent need to rapidly train many healthcare workers/responders to adapt their job duties to meet the new COVID-19 guidelines (World Health Organization [WHO], 2020). To implement appropriate patient care in response to COVID-19, healthcare workers/responders must first protect themselves to ensure patient care can be delivered and second, in order to limit the spread of COVID-19 via patient, person, and other surface contaminations (Huh, 2020). Notably, this patient care control response requires an ever-changing adaptation of workplace, hygiene, and patient care practices for healthcare workers/responders to be able to safely work in a hospital environment that will be contaminated by COVID-19 through the patients they care for within the environment. Moreover, depending on the hospital environment, healthcare workers are also facing staffing shortages (i.e., as co-workers and support staff contract and fall ill to COVID-19 and if unaffected by COVID-19 are over worked to help curb its spread), which are a significant factor contributing to overwhelming the hospital capacity (Adams and Walls, 2020).
Thus, in an effort to reduce these challenges, some healthcare professionals are being transferred, re-deployed (i.e., both elective and non-elective) to work in different hospital environments (i.e., between city, county, state, or even country), and perhaps not within their original specialty to help address the COVID-19 pandemic. In some cases of predicted healthcare worker/responder shortages and increases trends for overwhelming hospital capacity, current university/college medical doctors, nurses, etc. are graduating earlier than their degree timeline in an effort to deploy more healthcare workers/responders to support the individuals already in the frontlines (Harvey, 2020). A fundamental problem that is directly attached to this issue of healthcare worker/responder supply and demand during the COVID-19 pandemic, is how can the healthcare system adequately train such a large number of and diverse group of health-care workers/responders in such a short time-period? The frontline health-care workers/responders must be as best prepared as possible in order to take care of patients. Depending upon the healthcare and/or hospital centers in which these health-care workers/responders were stationed, some had time to be trained in a simulated environment, whereas others were trained through online courses for their students (Rose, 2020). This is also consistent with the social distance requirements to reduce unnecessary close proximity of a formal in-person educational classroom in order to educate and train students as well as healthcare workers/responders.
However, a real challenge arises from quality controls regarding the ability to acquire and/or apply new behavioral skills in the most realistic environment; nevertheless, an environment that is ever changing. Thus, in order to address this timely issue, the present rapid communication sought to provide COVID-19 healthcare workers/responders a means to rapidly create educational content that can be deployed (i.e., at any time including just before any medical/surgical procedure) adequately, efficiently, and meaningfully to best alleviate the issues faced by hospitals, health-care workers/responders, and patients.
In particular, the healthcare and/or hospital centers have used videos to share the challenges they faced along with their expertise to better inform their constituents among and within their healthcare worker/responder and hospital communities. Notably, scientific societies have worked towards producing online courses with video content to help translate and explain the behavioral skills that they would like healthcare workers/responders to acquire and reliably replicate within the real world/applied healthcare environment (e.g., how to properly don and remove personal protective equipment [PPE] to reduce the likelihood of contamination; Rush University Medical Center, 2020). It is important to note that training videos are easier to create, facilitate, and deploy in such hospital care settings, but offer a passive learning approach that may lack necessary levels of engagement (i.e., lack of sustained and focused attention by the learner). This is critical as such a passive learning format may also create inadvertent lapses or gaps in learning that is expected to be acquired by the health-care worker/responder. Ros et al. (2017) have previously described more actively engaging and meaningful way to create and develop pedagogical video content to acquire new skills through the following: 1) first person point-of-view (FPV); 2) shorter refined chapter modules; 3) with additional pedagogical data to reinforce learning new behavioral skills. The FPV has demonstrated a greater value that has shown to translate into increase learner comprehension and a reduction in learner mistakes within the real environment (Fiorella et al., 2017). This FPV method in creating content that can be more easily acquired and retained by the learner, was initially described using an Immersive Virtual Reality Application (IVRA; i.e., which requires a head-mounted display [HMD]), but also can be deployed more economically and efficiently through a smartphone. Given the unprecedented COVID-19 situation, we anticipated the release of a new healthcare worker/responder application with guidelines to scale up and provide rapid training content that could be used on the healthcare workers/responders personal smartphones to increase the efficiency, transferability, and reliability across local and more distant environments through technology as a responsible global public health educational outreach.
2. Methods
The content that was developed complied with general data protection regulations (GDPR) for users that chose to download it on their smartphones. The current content was developed to address the COVID-19 healthcare worker/responder needs was modeled from the FPV content that was used to create neurosurgical physician and medical care content (Ros et al., 2017), but with the aim to apply it to a wider healthcare worker/responder audience. The creation of the learning content (i.e., tutorial) involved the following three steps: First, the procedure was recorded in 3D from the expert medical professional's FPV (i.e., using the equipment worn by the expert performing the procedure). The Fig. 1 presents the hardware set-up on an expert.
Fig. 1.
Illustrates the recording hardware set up (black arrow) that are attached to the medical healthcare professional expert that performed the procedures in real-time. The medical healthcare professional is wearing a harness with an arm extending from his back permitting the recording to occur above his head during the procedures. At the tip of the arm, a case containing two cameras (white arrow) records his first-person point-of-view (FPV).
Second, the movie was organized into refined chapter modules corresponding to the different steps of the surgery (i.e., the editing process comprised calibration, synchronization, and stabilization of the two videos). Finally, the voice over comments were recorded and the imaging was then drawn along with data that were incorporated into the tutorial. The learning content was extended to create content specifically dedicated to nurses as what was done previously (Ros et al., 2017). In response to the COVID-19 pandemic and the need for ongoing surgical interventions, the current tutorial was created and deployed within one week and the first eight novel tutorials were specifically designed for healthcare workers/responder taking care of COVID-19 patients. The rapid production of these tutorials comprised a step-by-step assessment to reliably ensure the learners interest. This included adding three more tutorials on how to safely approach a COVID-19 positive patient. The first tutorials were produced and captures outside of the hospital setting:
-
–
Best practices for disinfecting hands with alcohol-based solutions
-
–
Proper use and functions of protective masks
-
–
Radial arterial sample for ABGs in a COVID-19-positive patient
-
–
Dressing/Undressing for “Contact - Droplets”: Protective equipment with a COVID-19 positive patient
-
–
Taking a nasopharyngeal sample for COVID-19 diagnosis
This was followed by tutorials within the Medical Simulation Center demonstrating the aforementioned steps on a respiratory mannequin:
-
–
Endotracheal intubation in a COVID-19 positive patient
-
–
Endotracheal extubation in a COVID-19 positive patient
-
–
Cardiopulmonary resuscitation of a COVID-19 positive patient
Through the access of an Intensive Care Unit (ICU), the following recording was conducted in an empty room:
-
–
Starting a respiratory machine in a hospital
An additional two tutorials are under production on a COVID-19 patient in ICU:
-
–
“Closed suction for intubated patients”
-
–
“Prone Decubitus” (we already recorded this, but for operating room, not for an intensive care unit).
The tutorials have been deployed since that can be easily accessed as a the Revinax® Handbook — Nurses App on any healthcare workers'/responders' smart phone that is released as a download on the Appstore and the Playstore, for both iPhone and Android users, respectively. Fig. 2 shows the user interface of the app.
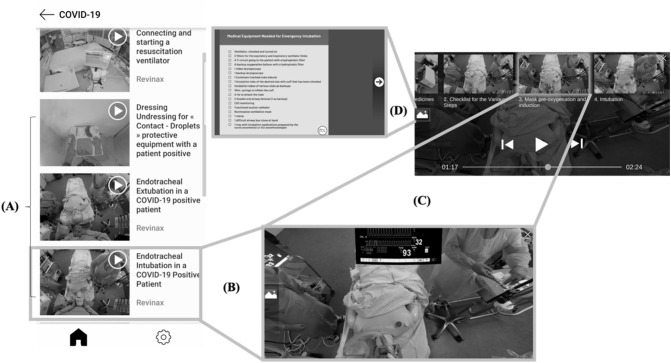
Fig. 2.
Illustrates the screenshot of the App tutorial as viewed by the user. (A) shows the User Interface with the library content. (B) depicts the movie in the first-person point-of-view (FPV) of an Endo-Tracheal Intubation procedure adapted to a COVID19+ patient. (C) Illustrates the chapters that correspond to the different procedural steps for that medical procedure. (D) Is an example of additional data that are available to the user by tapping the icon that is located on the left side of the screen.
Following the download and tutorial usage, the healthcare workers/responders were asked to complete a short survey in order to obtain user feedback on this responsible global public health educational outreach technology.
The survey questions were as follows:
-
–
Is the Revinax® App a good tool to support you to gain competencies? (Answers from 1 “not at all” to 10 “absolutely”)
-
–
Did you get a better understanding of certain procedures expected of you through the tutorials? (Yes or No)
-
–
More specifically, did the tutorials from the COVID-19 category make you feel ready to take care of these patients? (Answers from 1 “not at all” to 10 “absolutely”)
-
–
More generally, did the tutorials address your training/learning need right now? (Not at all/not really/rather/absolutely)
-
–
After having watched the COVID-19 tutorial, do you feel confident to perform the procedures yourself? (Not confident at all/Not that much confident/Quite confident/Very confident)
-
–
Would you recommend the Revinax® App to other healthcare workers/responders?
3. Results
3.1. APP download user demographics
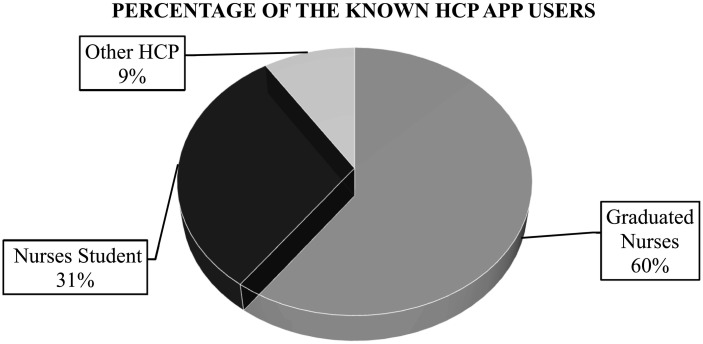
Since the initiation of this responsible global public health educational outreach effort, the Revinax® Handbook — Nurses App has been downloaded by 12,516 users/learners/healthcare workers/responders in one month (i.e., that is 3129 downloads per week, 447 downloads per day, and 18.63 downloads per hour evidencing a translatable emergent- and growing-demand). Furthermore, of the 12,516 downloads, 2671 were from non-qualified users (21.24%), whereas of the remaining 9845 downloads, 8729 were identified as nurses/nursing students (69.74% of all users and 88.66% of all qualified health-care workers/responders), and the 1116 were a mixture of medical assistants, students, physicians and undefined healthcare workers/responders (8.92%). Fig. 3 illustrates the user population demographics for the study.
Fig. 3.
Illustrates the percentage of the known healthcare professionals (HCP) App tutorial users. Note that two-thirds of the App tutorial users were graduated professional nurses, whereas one-third of the App tutorial users were currently enrolled nursing students. The remaining HCP comprised 9% of the App users.
Further, of the 8941 nurses that downloaded the App, 5921 disclosed (66.22%) that they were registered nurses (i.e., among them 5310 were graduated nurses [89.68%], 226 were scrub nurses [3.82%], and 173 were nurses anesthetist [2.92%], respectively). Moreover, of the 8941 nurses that downloaded the App, 3020 were nursing students (33.78%). Of these 3020 nursing students, 2837 were not specialized (93.94%), whereas 121 were specialized as nurse anesthetist (4.01%), and 62 were specialized as scrub nurses (2.05%), respectively. Notably, of the 904 remaining mixture of medical assistants, students, and physicians, 352 self-disclosed as nurses' assistant (38.94%), 311 self-disclosed as medical students (34.40%), and 241 self-disclosed as physicians (26.66%), respectively.
3.2. COVID-19 tutorial feedback survey outcomes
From the 12,516 downloads, we sent out a feedback survey during the first 72 h of deploying the survey and we obtained 366 replies. During this precise time-period, the number of downloaded subscribers were 512 (i.e., 122 responses per day from an estimated 171 downloads per day — which is a 71.48% response rate with a ±10% margin of error making it statistically significant). Notably, despite the COVID-19 pandemic, the users found that the tutorials through the App were very useful and took the time to complete the survey even during these trying times. This is a critical point as typical respondent data from surveys is hard to obtain, and one would have suspected a lower respondent rate given a pandemic. Thus, having a 71.48% response rate with positive user results suggests that the users valued and found the tutorials helpful in translating the skills they needed for COVID-19 patient care. The survey results showed that healthcare workers/responders and/or students in these fields considered this App appropriate to learn and review skills related to the COVID-19 pandemic. Further, more than 95% of the respondents gave a score equal to or higher than 5 for gaining competencies, whereas 88% of the respondents said it corresponded to their healthcare related needs. Additionally, 93% of the respondents said it gave them a better understanding, compared to 87% of the respondents that felt quite or very confident to perform the procedures as shown in the tutorials. Lastly, 94% of respondents indicated that the COVID-19 specific tutorial made them feel ready to care for COVID-19 patients, and finally, 95% of respondents recommended the App.
4. Discussion
Movies in medicine became available following advances in cinematography that have been more recently truncated to shorter video clips or segments (Essex-Lopresti, 1998a). Further, the first medical movie published was in 1897 corresponding to animated X-ray pictures. Dr. John Macintyre took a series of photographs of a knee in various degrees of flexion and extension, then suturing them and projected the procedures. It helped medical students to study different aspects of the animated movement. The first time a video was used in lectures was the same year that Paul Schister filmed patients with Parkinson's disease to explain and illustrate their different motor symptoms. Notably, the first surgical video was recorded during the first half of the 20th century. At that time, there were skeptics regarding the pedagogic value of movies, when compared to traditional lectures and more hands-on applied practicum training. For example, medical videos portraying clinical examinations relevant to the discussion of new types of syndromes were shown to students. As the demographic of new generations of students have changed over time (e.g., first-generation immigrant and first-generation college students, etc.; Mukherji et al., 2017), students may prefer different applied learning formats over a traditional lecture (Neuwirth et al., 2018, Neuwirth et al., 2019) and the traditional practicum applied learning can be leveraged through an active FPV tutorial (Ros et al., 2020) perhaps better than the passive medical videos.
Regardless, medical movies have been used progressively and in a variety of ways for public health purposes. They have been most recently used to provide medical explanations and promote disease prevention programs, thereby underlining the pedagogical of transferring education through the power of movies. During the latter half of the 20th century, British universities developed a large database that includes a variety of medical movies explicitly for study purposes (Essex-Lopresti, 1998b). At the beginning of the 21st century, it became clear that watching medical movies represented an effective way, at least for learning about surgical techniques (Hayden et al., 2015). Thus, surgeons should be encouraged to develop movie databases for use in their schools or for publication in modern peer-reviewed journals (Brunaud, 2013).
One of the main advantages of the immersive tutorial, in contrast to medical videos, is that it enables the user to live the experience from a FPV: to learn through “the expert's own eyes.” An interesting study published by Fiorella et al. (2017) compared learning a procedure from a FPV to learning from the opposite side (i.e., non-FPV or opposing observer perspective to mirror the person doing the task). Compared to the group that learned from the FPV, the learning from the opposite side group made up to 50% more mistakes, while reproducing the assembly of an electronic system. These results suggest that FPV learning increases the learners' skill acquisition, comprehension, and behaviors as evidenced by less errors. Further, these results may be uniquely explained by the way that mirror neurons (i.e., neural circuits that are explicitly involved in our visual monitoring of others, encode empathy, and facilitate the learning of watching others doing a task, assigning it value, and then implementing the tasks ourselves; Rizzolatti and Craighero, 2004) work more optimally by reducing its “cognitive load” (Van Gog et al., 2008).
Such a reduction of cognitively load, may in turn, free up more cognitive reserves to further aid in the skill acquisition, comprehension, and behavioral exhibition of transformative learning via FPV. This situation presents yet another fundamental question, as to what would be the value of a FPV tutorial world-wide system in contrast to a university's medical video library? Would it have greater potential for transformative learning? How could it further shape the medical healthcare system? These ideas are not far-fetched as 30 years ago educators were skeptical of online degrees and the learning outcomes of students. Today, as standards and different uses of technology have evolved, so too has the rigor of such educational online formats. Thus, an analogous argument can be made here with respect to medical movies compared to FPV tutorials within a pandemic directly effecting people globally. An advantage to the learning in FPV compared to medical videos is that the possibility for an immediate local download on a healthcare workers'/responders' smart phone can be accessed at any time in real-time prior to, during, or after patient care interactions. In addition, if it is downloaded on the users' smartphone, it can then be accessed and viewed at any time irrespective of network signal or service issues. Since the FPV tutorial is edited, it permits the healthcare worker/responder with the possibility to self-navigate through or to skip to chapters/modules of most relevance to them. This feature has been shown to have a distinct pedagogical value (Zhang et al., 2006) as healthcare workers/responders can easily browse the necessary information, thereby increasing efficiency of patient care services. The survey results showed that the tutorials offered a better understanding of the procedures the healthcare workers/responders were to complete, thereby making them more confident and feeling ready to face the situations to care for COVID-19 patients. The results of the survey suggested that the learning content delivered to them through the App seemed to address their needs. It is important to note that the majority of the audience here were nurses, but these tutorials has also piqued the interest of some physicians. More importantly, these tutorials have also piqued the interest of next generation medical/healthcare professional students, which is consistent with a generational shift in learning format displays.
5. Conclusion
The present rapid communication sought to evaluate the interest, usage, and potential of the FPV COVID-19 tutorial for healthcare workers/responders during a pandemic as a responsible global public health educational outreach technological tool. The findings of this adjunctive pedagogy have shown to be well received by frontline nurses and future nursing students. Further, the information allows the healthcare worker/responder a wide range of flexibility to initial learn, relearn, and review the material as needed to help as a powerful and rapid transferable medical intervention. There may be limitations to this technology as not all countries and hospitals may employ the same procedures, which have to be taken into consideration. However, for the most part, these tutorials were developed keeping in mind the most universal applications possible to help alleviate this important concern. Moreover, these tutorials have been translated from French and the voice-over recording has begun in English, as a universal language, to be deployed in many other countries. In closing, it is better to be ready to face an emergency and to have this material already available, but in case of a change of the evolving recommendations, concerns for re-infection of or resurgence of COVID-19, the current tutorials were designed and deployed to offer efficient, effective, and rapid responsible global public health educational outreach technology tool direct towards alleviate the overwhelming experiences that hospitals, healthcare workers/responders, and patients face due to the COVID-19 pandemic.
Contributors
Dr. Maxime Ros conceived of, conducted, and implemented the technological design of the FPV tutorials, and acquired the data. Drs. Maxime Ros and Lorenz S. Neuwirth analyzed and interpreted the data, then wrote and approved the final version of the manuscript ensuring it contained important intellectual content to be submitted.
Declaration of competing interest
Dr. Maxime ROS is a neurosurgeon. He was practicing at the Montpellier University Hospital before founding Revinax®, the company that developed and created the methodology for the immersive first person POV tutorials as described herein.
Acknowledgments
We thank Pr. Thomas Geeraheart, Head of the Medical Simulation Center of Toulouse Hospital, for granting us the permission to record the Intubation, Extubation, and ACR procedures. In addition, we would like to thank Dr. Marc Beaussier, M. Vincent Roques, and Ms. Vinciane Mysliwice from the Institut Mutualiste Montouris (Paris) for recording the Ventilator tutorial. Lastly, we would like to thank Ms. Sarah Daudé for recording the extra-hospital tutorials.
References
- Adams J.G., Walls R.M. Supporting the health care workforce during the COVID-19 global epidemic. JAMA [Internet] 2020;323(15):1439–1440. doi: 10.1001/jama.2020.3972. https://jamanetwork.com/journals/jama/fullarticle/2763136 2020 Mar 12 [cited 2020 Apr 18]; Available from: [DOI] [PubMed] [Google Scholar]
- Branas C.C., Rundle A., Pei S., Yang W., Carr B.G., Sims S. Flattening the curve before it flattens us: hospital critical care capacity limits and mortality from novel coronavirus (SARS-CoV2) cases in US counties [internet] Epidemiology. 2020 http://medrxiv.org/lookup/doi/10.1101/2020.04.01.20049759 2020 Apr [cited 2020 Apr 18]. Available from: [Google Scholar]
- Brunaud L. Will watching videos make us better surgeons? J. Visc. Surg. 2013;150(5):295–296. doi: 10.1016/j.jviscsurg.2013.09.005. [DOI] [PubMed] [Google Scholar]
- Essex-Lopresti M. The medical film 1897–1997: part I. the first half-century. J. Audiov. Media Med. 1998;21(1):7–12. doi: 10.3109/17453059609063115. [DOI] [PubMed] [Google Scholar]
- Essex-Lopresti M. The medical film 1897–1997: part II. The second half-century. J. Audiov. Media Med. 1998;21(2):48–55. doi: 10.3109/17453059809167238. [DOI] [PubMed] [Google Scholar]
- Fiorella L., van Gog T., Hoogerheide V., Mayer R. It’s all a matter of perspective: viewing first-person video modeling examples promotes learning of an assembly task. J. Educ. Psychol. 2017;12(109):653–665. [Google Scholar]
- Harvey A. Covid-19: medical schools given powers to graduate final year students early to help NHS. BMJ. 2020;368 doi: 10.1136/bmj.m1227. https://www.bmj.com/content/368/bmj.m1227 [DOI] [PubMed] [Google Scholar]
- Hayden E.L., Seagull F.J., Reddy R.M. Developing an educational video on lung lobectomy for the general surgery resident. J. Surg. Res. 2015;196(2):216–220. doi: 10.1016/j.jss.2015.02.020. [DOI] [PubMed] [Google Scholar]
- Huh S. How to train health personnel to protect themselves from SARS-CoV-2 (novel coronavirus) infection when caring for a patient or suspected case. J. Educ. Eval. Health Prof. 2020;7(17):10. doi: 10.3352/jeehp.2020.17.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukherji B.R., Neuwirth L.S., Limonic L. Making the case for real diversity: redefining underrepresented minority students in public universities. Sage Open, Special Diversity Edition. 2017:1–10. doi: 10.1177/2158244017707796. (Apr.-June): [DOI] [Google Scholar]
- Neuwirth L.S., Ebrahimi A., Mukherji B.R., Park L. Addressing diverse college students and interdisciplinary learning experiences through online virtual laboratory instruction: a theoretical approach to error-based learning in biopsychology. In: Ursyn A., editor. Visual Approaches to Cognitive Education with Technology Integration. 2018. pp. 283–303.https://www.igi-global.com/chapter/addressing-diverse-college-students-and-interdisciplinary-learning-experiences-through-online-virtual-laboratory-instruction/195070 [Google Scholar]
- Neuwirth L.S., Ebrahimi A., Mukherji B.R., Park L. Addressing diverse college students and interdisciplinary learning experiences through online virtual laboratory instruction: a theoretical approach to error-based learning in biopsychology. In: Information Resources Management Association, editor. Virtual Reality in Education: Breakthroughs in Research and Practice: IGI Global. 2019. pp. 511–531.https://www.igi-global.com/chapter/addressing-diverse-college-students-and-interdisciplinary-learning-experiences-through-online-virtual-laboratory-instruction/195070 [Google Scholar]
- Rizzolatti G., Craighero L. The mirror-neuron system. Annu. Rev. Neurosci. 2004;27(1):169–192. doi: 10.1146/annurev.neuro.27.070203.144230. [DOI] [PubMed] [Google Scholar]
- Ros M., Trives J.V., Lonjon N. From stereoscopic recording to virtual reality headsets: designing a new way to learn surgery. Neurochirurgie. 2017;63(1):1–5. doi: 10.1016/j.neuchi.2016.08.004. [DOI] [PubMed] [Google Scholar]
- Ros M., Weaver L., Neuwirth L.S. Virtual reality stereoscopic 180-degree video-based environments: applications for training surgeons and other medical professionals. In: Stefaniak J., editor. Cases on Instructional Design and Performance Outcomes in Medical Education. 2020. https://www.igi-global.com/book/cases-instructional-design-performance-outcomes/244674 [Manuscript accepted and in press] [Google Scholar]
- Rose S. Medical student education in the time of COVID-19. JAMA [Internet] 2020 doi: 10.1001/jama.2020.5227. https://jamanetwork.com/journals/jama/fullarticle/2764138 2020 Mar 31 [cited 2020 Apr 18]; Available from: [DOI] [PubMed] [Google Scholar]
- Rush University Medical Center Personal Protective Equipment for COVID-19 Care [Video] 2020, April 18. https://www.youtube.com/watch?v=84CydmuHXD8 Youtube.
- Van Gog T., Paas F., Marcus N., Ayres P., Sweller J. The mirror neuron system and observational learning: implications for the effectiveness of dynamic visualizations. Educ. Psychol. Rev. 2008;1(21):21–30. [Google Scholar]
- World Health Organization Critical preparedness readiness and response actions COVID-10 2020-03-22_FINAL-eng.Pdf [internet] 2020, April 18. https://apps.who.int/iris/bitstream/handle/10665/331511/Critical%20preparedness%20readiness%20and%20response%20actions%20COVID-10%202020-03-22_FINAL-eng.pdf
- Zhang D., Zhou L., Briggs R.O., Nunamaker J.F. Instructional video in e-learning: assessing the impact of interactive video on learning effectiveness. Inf. Manag. 2006;43(1):15–27. [Google Scholar]