Abstract
Little is known about dissemination and implementation in safety net settings. The authors conducted a literature review of innovation/implementation studies in US safety net health care settings between 2008 and 2017. Each article was coded for (1) intervention characteristics, (2) implementation stage, (3) internal versus external ownership, and (4) prespecified implementation outcomes (eg, acceptability and fidelity). Twenty studies were identified; the majority were implemented within community clinics or integrated safety net systems (15 articles), most involved care process improvements (13 articles), and most were internally developed (13 articles). The internally developed innovations reported fewer barriers to acceptability among staff/providers, higher leadership involvement and organizational alignment, greater amounts of customization to the local setting, and better sustainment. Future work should harness the high levels of alignment and acceptability in implementation research within safety net settings, with an eye toward maintaining fidelity to facilitate dissemination across sites.
Keywords: implementation science, safety net, care process innovations, systematic review
Innovation is often defined as “the implementation of a new or significantly improved product (good or service) or process, a new marketing method, or a new organizational method,”1 often to replace older processes altogether.2 Alongside the concept of innovation, translating evidence into practice requires changes in current practices and is known to occur variably and slowly.3–6 The concepts of innovating and translating evidence into practice are often discussed separately, but especially in underresourced health care settings, the delivery of new and improved care processes is often intertwined with the implementation of practices known to work in other health care settings.3
Implementation of innovations in the health care safety net is particularly important because these systems face additional challenges in order to meet the demands of providing high-quality care to diverse, low-income populations, under conditions of significant resource constraints.7,8 Specifically, safety net settings care for patients who have higher levels of both medical and social complexity, yet they operate primarily on federal and state funds, which reimburse health care services at lower rates than private insurance. Therefore, implementation in safety net health systems often requires specific efforts to tailor or adapt practices.3,7,9
There have been several overarching frameworks that attempt to provide a means to understand the complex process of implementing successful new interventions and programs into health care settings.10,11 Various factors, such as organizational leadership support and resource availability, affect the successful spread of practices in health care,3,12,13 and much has been written about these factors.10,14–20 However, few studies directly compare or review implementation processes across multiple programs.
The study team completed a review of articles reporting on implementation of interventions or programs in US safety net settings. The objectives of this review were to both describe the landscape of this body of literature as well as to examine how specific implementation outcomes (such as fidelity and sustainment) are addressed within these studies.
Methods
Search Strategy
The study team searched both PubMed and Google Scholar databases for “safety net” or “low income” in combination with “innovation”/“innovate” and “implement”/“implementation” between January 2008 and April 2017, to be sure to capture articles post health care reform. The team also searched the reference lists of included articles to identify additional articles describing different elements of the same program implementation.
Inclusion Criteria
First, in a joint meeting, 2 coauthors (GG, CRL) collaboratively screened 40 abstracts from the initial search to generate the inclusion criteria categories and definitions. Then, the remaining abstracts were divided among coauthors to eliminate articles that did not meet these criteria, which included full-text review of any articles that could not be categorized from the abstract alone. Any uncertainty was resolved by discussion between at least 2 coauthors.
Articles were included as follows: (1) original research (ie, not commentaries/editorials), (2) US focus (ie, not global/international focus), (3) presence of empirical data (eg, not case studies without qualitative or quantitative outcome assessments), (4) implementation of a specific program or intervention (ie, not broad processes covering multiple programs), (5) conducted within safety net clinical health care settings (ie, based at least partially at a health care system serving predominantly low-income or publically insured patient populations), (6) containing staff/provider- or organizational-level data (ie, not solely patient outcome data), and (7) focused on local programs/interventions (ie, not evaluating the impact of a broader health care policy).
Because the criteria excluded articles without empirical data or intervention descriptions, this ensured that the articles met the Standards for Quality Improvement Reporting Excellence (SQUIRE) criteria.21
Article Coding
For each article, 4 coauthors (CRL, MAH, PW, MW) then summarized (1) the main intervention (a summary of the intervention, including whether it was an evidence-based practice), (2) study design (qualitative, quantitative, or mixed methods, as well as a study sample description), and (3) implementation setting.
The study team also summarized the stage of implementation. The vast majority of studies included data collection in an active implementation phase. An additional set of planning studies encompassed research that had a “protocol” focus that explained future implementation data collection or pre-implementation data to inform a future program or intervention.
Studies were categorized as “internal” versus “external.” Externally developed programs were defined as partnerships/collaborations with outside institutions (such as interventions proposed by external researchers). Internally developed programs were described as resulting from a specific internal health care system need. Further specified within the internal category were any studies that were implemented because of an internal motivation but funded by an existing grant opportunity (“internal with grant support”) or conceptualized and executed through an equal partnership between the clinic and an outside entity (“cocreated” projects).
Implementation Outcomes.
Finally, a set of established implementation outcomes were used to explore major themes within the active implementation studies: acceptability (at the staff/provider level in the context of their existing work/roles), appropriateness (at the level of both organizational alignment and fit/relevance), fidelity (in terms of customization vs standardization of the program implemented), cost (unforeseen financial barriers to implementation), and sustainment (program continuation in the future).22 The study team coded whether this implementation outcome was mentioned/discussed in the article and, if mentioned, how this implementation outcome was perceived as a barrier or facilitator to success.
The team also examined each of the implementation outcomes by the internal versus external development categorization because previous literature has documented improved success based on internal motivation and ownership of the program.23–27
Results
In total, 346 articles were identified using the search terms; 27 were included in the final sample: 20 active implementation and 7 planning articles (Figure 1).
Figure 1.
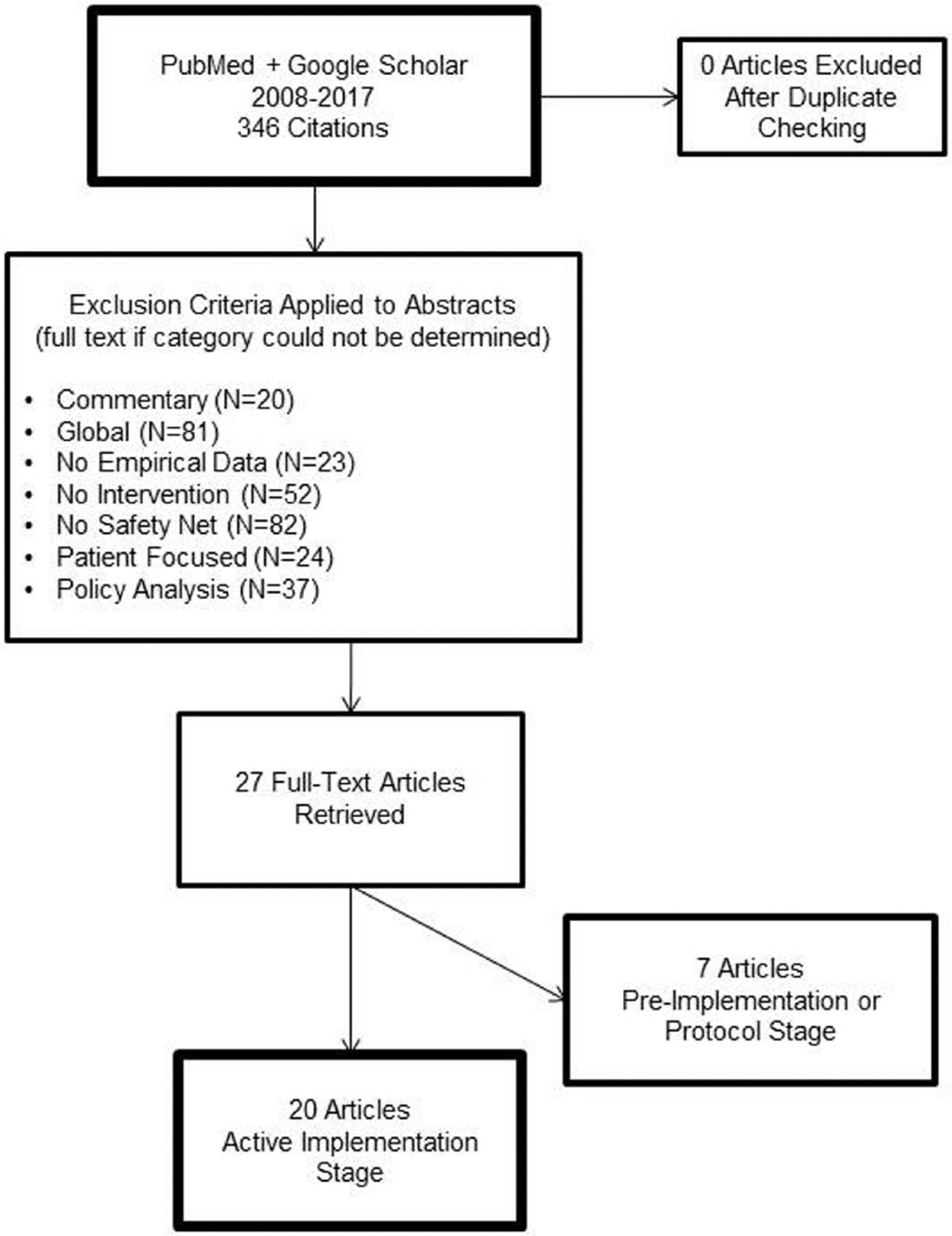
Manuscript selection flow diagram.
Active Implementation Articles
Of the 20 active implementation studies (Table 1), 19 programs are summarized because 2 of the articles discussed implementation of the same program.28,29 Eleven articles employed mixed methods.30–40 This included in-depth interviewing of health care system leaders and/or staff as the most common methodology,28–30,32,33,36,41–46 followed by descriptive data collection involving observations,39,40,42 document review,33 and/or detailed case studies of implementation.31,34,35,37,38
Table 1.
Overview of Active Implementation Studiesa.
| Author | Year | Evaluation Methods | Intervention/Program | Clinical Setting | Implementation Stage |
|---|---|---|---|---|---|
| Bolin JN | 2013 | Mixed methods (patient surveys, key stakeholder interviews, quantitative usage tracking) | Patient education, technology (touchscreen diabetes education kiosk) | 2 community clinics, 1 community center, and 2 pharmacies in a predominantly Latino community in South Texas | During, Post |
| Borkowski N | 2013 | Mixed methods (case study combined with quantitative analyses of membership and cost data) | Care processes (clinic-wide efficiency improvements) | Community clinics in Jackson Health System in Miami-Dade County, Florida | Pre, Post |
| Braun PA | 2013 | Mixed methods (n = 13 qualitative interviews with staff/leaders combined with parent surveys) | Co-location (dental hygienist based in primary care practice) | Community clinics serving disadvantaged children in Colorado | Post |
| Breslau ES | 2010; 2015 | Qualitative (n = 24 qualitative interviews with leaders) | Community engagement, care processes (state and community partnerships for increased screening for cervical and breast cancer) | Clinic and community clinic partnerships in underserved counties in Southern rural states with high breast and cervical cancer mortality | Pre, During, Post |
| Clark NM | 2014 | Mixed methods (Document review combined with n=60 qualitative interviews with leaders) | Care processes (enhanced diabetes care and coordination) | 5 regional sites (Camden, NJ; Chicago, IL; Dallas, TX; Memphis, TN; Wind River, WY) with partnerships between community clinics and community organizations (applied for grant support) | Pre, During, Post |
| Dennehy P | 2011 | Mixed methods (case study combined with quantitative provider/staff survey data) | Capacity building, technology (EHR installation and optimization) | 2 nurse-managed health centers serving low-income primary care patients (Glide Health Services in California and Campus Health Center Detroit in Michigan) | Pre, During, Post |
| Drainoni ML | 2016 | Qualitative (n = 50 participants, 7 focus groups, 6 individual interviews) | Care processes (improvement in naloxone prescribing implementation in emergency department) | Emergency department staff at Boston University Medical Center | Post |
| Garg SK | 2016 | Qualitative (n = 8 in-depth interviews of leaders/staff across sites) | Care processes, technology (clinic-wide patient text messaging programs) | 8 California community clinics or integrated safety net health care systems (applied for grant support) | Pre, During, Post |
| Johnson TL | 2015 | Mixed methods (case study combined with quantitative analyses of the high-utilizing patient population) | Care processes, technology (patient risk stratification for new care models) | Urban integrated safety net health care system in Denver, Colorado | Pre, During, Post |
| Labbok MH | 2013 | Mixed methods (quantitative staff/provider survey assessments combined with qualitative interviews) | Care processes (hospital-based breastfeeding support program) | 6 hospitals serving low-income women in North Carolina | During, Post |
| McMullen CK | 2013 | Qualitative (n = 9 in-depth interviews with leadership and clinic observations) | Capacity building, care processes (patient-centered medical home implementation) | 6 community clinics in Portland, Oregon | Pre, During |
| Novick G | 2015 | Qualitative (n = 24 qualitative interviews with providers, staff, and leaders) | Care processes (group prenatal care visits) | 6 urban community clinics or hospitals serving low-income, minority women | During |
| Ramos-Gomez FJ | 2014 | Mixed methods (case study combined with data measurement of program uptake) | Co-location, community engagement (oral care program for children ages 0–5) | Community clinics and community sites such as WIC and Head Start | During |
| Samaan ZM | 2016 | Quantitative (clinic- and provider-level data measurement) | Care processes (bundled infant preventative services delivery) | Cincinnati Children’s Hospital Medical Center pediatric clinic sites (community and hospital) | Pre, Post |
| Smith MG | 2017 | Qualitative (n = 73 interviews with various pharmacy staff members) | Care processes, community engagement (use of clinic- and community-based pharmacies to manage medication review for high-risk patients) | Network consisted of 123 community and health center pharmacies in North Carolina | Post |
| Steiner BD | 2008 | Mixed methods (case study combined with quantitative cost estimates) | Capacity building, care processes, community engagement (establishment of community health primary care network) | Community Care of North Carolina (including hospitals/clinics, social service agencies, and public health departments serving mostly rural Medicaid recipients) | During, Post |
| Sugarman JR. | 2014 | Mixed methods (observations of implementation processes at each site combined with surveys of providers/staff); n = 65 sites | Capacity building, care processes (patient-centered medical home implementation) | 65 clinics including homeless clinics, private practices, residency training centers, and other safety net practices | During, Post |
| Wagner EH | 2014 | Qualitative (n = 7 qualitative interviews with leaders) | Capacity building, care processes (patient-centered medical home implementation) | 3 diverse community clinic locations (urban site in Oregon, rural site Colorado, multisite urban and rural in Idaho) | Post |
| Waitzkin H | 2011 | Mixed methods (quantitative intake surveys completed with patients, combined with n = 35 qualitative interviews with patients, providers, and staff, as well as observations) | Care processes (use of lay health workers to facilitate depression care) | 2 community clinics in New Mexico | During, Post |
Abbreviations: EHR, electronic health record; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
The 20 active implementation phase articles include during- or post-implementation data, 2 of which are the same author describing the same intervention and are therefore presented jointly.
The vast majority of studies were implemented within community clinics or integrated safety net health care systems (16 articles), while the other 4 articles focused on hospital care. A total of 6 articles also discussed explicit linkages between the health care setting and other organizations, such as community-based organizations and pharmacies.
Fifteen active implementation articles focused on care process improvements covering a range of topics, such as patient-centered medical homes, group prenatal visits, bundled infant preventive care, naloxone prescribing, or diabetes care delivery. Five articles described capacity building techniques to foster internal support and skill building to implement the new program, 4 articles reported community engagement strategies to partner with external organizations, and 2 articles addressed implementing co-location of care (such as dental care into existing primary care). Five of the articles also examined technology implementation, and 2 focused on patient education.
In all, 6 external28–30,32,36,40,43 and 13 internal programs were studied,31,33–35,37–39,41,42,44–47 and the specific implementation outcomes assessed are summarized in Table 2.
Table 2.
Implementation Outcome Assessment Among Active Implementation Studies.
| Author | Year | Evidence-Based Practice? | Implementation Outcomes of Interest | ||||
|---|---|---|---|---|---|---|---|
| Acceptability | Appropriateness | Fidelity | Implementation Cost | Sustainment | |||
| External studies | |||||||
| Bolin JN | 2013 | No | Clinics and pharmacies did not have existing staff person dedicated to monitor kiosks | Leadership lightly involved in MOU process and evaluation interviews | Standardized—everyone used same kiosk | Resource/$ limitations to pay for Wi-Fi, etc | Potential continuation for some sites |
| Braun PA | 2013 | No | Challenge to keep regular hygienists in this new position | Leadership involved in implementation and evaluation | Not mentioned | Resource/$ limitations in getting reimbursed for dental care | Ongoing for 5+ years |
| Breslau ES | 2010; 2015 | Yes | Understaffed—felt that this new initiative was extra work on top of other responsibilities | Engagement of community partners was challenging; leadership was a clear barrier for community organizations/clinics feeling invested in projects | Option to customize—each local partnership chose their own evidence-based practice | Resource/$ limitations for clinics to provide cancer care to more patients in need | Sustained in only a few cases; success stemmed from relationship building |
| Labbok MH | 2013 | Yes | Challenge in relying solely on lactation consultants to do all the work and lack of self-efficacy among other staff members | Leadership buy-in present, but not aligned with existing health system culture | Standardized 10-step breastfeeding program | Expense of baby-friendly designation as a barrier | Not mentioned |
| Novick G | 2015 | Yes | Understaffed to handle the more challenging group scheduling process | Some sites aligned with organizational culture (especially with a great staff champion) while others faced major cultural barriers and apprehension about the program | Standardized group prenatal visit program among intervention sites | Resource/$ limitations, mainly major organizational financial shortfalls | Sustained at only half of sites able to address implementation barriers |
| Waitzkin H | 2011 | Yes | Understaffed in times of staff turnover | Structural bureaucracy/leadership limits in terms of professional roles of promotoras vs other staff; Some leadership buy-in | Standard approach to promotora work with patients identified with depression | Not mentioned | Not mentioned |
| Internal studies | |||||||
| Borkowski N | 2013 | No | Not mentioned | Innovation aligned with the shared health system culture of the coalition; leaders very engaged in establishing a coalition with change management strategies | Option to customize—each primary care site determined their own redesign projects | Not mentioned (beyond context for the program) | Sustainment bolstered by monthly data reports and scheduled meetings over first 2 years of program deployment |
| Clark NM | 2014 | No | Not mentioned | Aligned with organizational culture—greatest success when diabetes programs aligned with other programmatic goals and with substantial leadership buy-in | Option to customize specific diabetes programmatic activities | Not mentioned | Striving toward sustainment with necessary policy changes |
| Dennehy P | 2011 | No | Lack of existing sufficient computer skills themselves | Aligned with health system culture—huge emphasis on the partnership/leadership model to ensure long-term success | Option to customize their EHR implementation plans | Resource/$ limitations—one institution removed IT funds shortly after program got under way | Sustained with another grant as a part of an ongoing community-based research network |
| Drainoni ML | 2016 | Yes | Strong acceptability by all staff | Strong associated appropriateness of intervention at leadership level | Standardized—original policy deployed | Not mentioned | Not mentioned |
| Garg SK | 2016 | No | Lack of existing staff IT expertise | Leadership and staff buy-in for the overall goals of the texting program; structural bureaucracy/leadership limits, particularly around HIPAA regulations | Option to customize, each clinic chose their own texting use case | Not mentioned (beyond grant funding) | Not mentioned |
| Johnson TL | 2015 | No | Appropriate staffing/tech support to build the new algorithm to identify high-utilizer patients | Innovation aligned/meeting organizational needs across multidisciplinary teams; leadership buy-in to create the program | Not mentioned | Not mentioned (beyond grant funding) | Sustained use of algorithm system-wide |
| McMullen CK* | 2013 | No | Not mentioned | Innovation aligned with health system culture; leadership buy-in, especially in the inspiration/motivational phase of the work | Option to customize the specific primary care redesign process | Provided modest financial incentives | Sustained due to “incubator” experience shared by organizational leaders |
| Ramos-Gomez FJ | 2014 | No | Not mentioned | Program worked because dental students were required to do rotations in this community-based dental program, and the community partners already had relationships with underserved patient populations to refer | Standardized trainings and use of standardized forms | Limited funds for program, but free labor because dental students provided the care as a part of training | Sustained by integrating program into covered prenatal care bundle |
| Samaan ZM* | 2016 | Yes | Appropriate staffing/tech support, especially for the QI consultant to manage the day-to-day work and paid protected time for some staff to participate | Innovation aligned with health system culture (multidisciplinary team represented all relevant stakeholders); leadership buy-in on steering committee | Customized over time and then became a standard process | Internal funds provided to launch and sustain program | Sustained by developing standardized orientation and training process |
| Smith MG | 2017 | No | Not mentioned | Appropriate local primary care providers and pharmacy leaders collaborated to build partnership | Standardized protocol requested from all pharmacies and care teams | Not mentioned | 40% had difficulty maintaining consistency of medication reviews month to month |
| Steiner BD* | 2008 | No | Early physician buy-in; case managers and physicians need more time to meet together | Innovation aligned with health system cultures, largely because of the local control of the work; leadership buy-in | Option to customize as each site focuses on their own specific QI projects | Existing payment models not sustaining work for highly complex patients, but Medicaid funding key to overall program coordination | Sustained through ongoing support by state office of rural health |
| Sugarman JR | 2014 | Yes | Understaffed, particularly with high staff and provider turnover and low staff morale in some instances | Innovation aligned with health system culture; leadership buy-in | Standardized the 8 change concepts for all clinics to work on | Barrier to getting full insurance reimbursement for a new model of care | Sustained but facing ongoing financial constraints |
| Wagner EH | 2014 | Yes | Not mentioned | Innovation aligned with health system culture; leadership buy-in as central to mission of organization | Standardized the 8 change concepts for all clinics to work on | Not mentioned | Sustained through established trust in the improvement process |
Abbreviations: EHR, electronic health record; HIPAA, Health Insurance Portability and Accountability Act; IT, information technology; MOU, memorandum of understanding; QI, quality improvement.
These studies provided key examples of note, especially in combining various implementation methods.
Implementation Outcomes.
1. Acceptability was conceptualized as the ability of staff to take on implementation related activities in their daily work. This is particularly relevant in safety net health care settings that are often resource limited with respect to staffing. Among the 19 studies included in this review, 13 discussed acceptability, 9 of which classified it as an inhibitor or barrier to widespread success.
The most common reason for lack of acceptability of the intervention within the health care system was understaffing and high rates of staff turnover. For example, Bolin et al30 mentioned that the new educational kiosk was not able to be monitored by existing staff members in the midst of their busy days, and therefore might go offline without anyone realizing the problem. In fact, it was common throughout the studies that staff and providers were expected to take on the new intervention/program in addition to their existing work responsibilities, which set up an inherent challenge to engagement by frontline workers. Another aspect of reduced acceptability was the need for staff to have specific technical assistance or skills to implement the program. For example, in the study by Garg et al41 on implementing texting systems to communicate with patients, one of the barriers was a lack of existing staff technological expertise to manage vendors or troubleshoot glitches.
Of note, there were 4 examples of high acceptability among providers and staff. In the study of implementing bundled infant preventive services by Samaan et al,47 the authors described how hiring a dedicated quality improvement consultant, coupled with paid protected time for frontline staff to work on the design of the program, led to high engagement. In addition, with the implementation of improved naloxone prescribing procedures for patients on opioids,46 very high acceptability was noted because of staff and leadership alignment with the public health mission.
All of the external programs mentioned acceptability as a barrier, while only 3 of 13 internal programs did. The other internally developed programs either did not mention acceptability explicitly (6 studies) or discussed it as a strength of implementation (4 studies).
2. The study team assessed appropriateness as the fit, suitability/relevance, and practicality of the intervention/program based on the existing work and culture of the organization. Sixteen studies discussed leadership as a positive element of their implementation process. The level of leadership engagement varied somewhat, with some studies such as Waitzkin et al40 evaluating leadership perspectives through interviews, while other studies such as Dennehy et al34 described a deep collaborative/partnership process with leaders in the health care system. Four of 6 externally developed programs had leadership buy-in, compared to 12 of 13 internally developed programs.
The team also evaluated appropriateness as alignment of the intervention/program with the culture or mission of the health care system. A total of 16 studies discussed alignment: 11 described it as contributing to the success of their program, while another 5 described inadequate alignment. Alignment was critical for the new program to be seen as adding value to existing priorities and workflows, given that there were a number of new projects at any given time. Borkowski et al31 describe a process in which the entire health care system coalition agreed on a shared vision for primary care, and the specific implementation of efficiency improvements tied directly to that shared vision. Alternatively, Breslau et al28,29 describe community organization integration into the implementation process too late to give input on the specific project goals. There also were more structural types of barriers that made alignment more challenging, such as Waitzkin et al40 documenting the lack of formalized job responsibilities for lay health workers that made workflows challenging.
Of note, all 6 of the externally developed programs either did not discuss appropriateness of the program or reported challenges with this process. This was in contrast to 10 of the 13 internally developed studies in which organizational alignment was mentioned as a strength.
3. Next, the study team examined the fidelity of the program implementation, or the degree to which implementation was tied to an external standard (such as a detailed protocol for program components) versus allowed to be customized by the setting. A total of 9 studies mentioned standardization, while 8 studies explicitly mentioned the ability of local sites to customize or choose the program elements they would implement. Types of standardization included a network of safety net clinics in Wagner et al45 that all implemented the same change concepts to work toward primary care redesign. This coordinated approach can be juxtaposed against the description presented in Steiner et al,38 in which each rural primary care site focused on its own quality improvement projects supported by a centralized state administrative office.
Of the externally developed programs, 4 of 6 studies described standardized implementation, while 7 of the 13 internally developed programs were customizable and 5 were standardized (one study did not mention fidelity).
4. With respect to implementation cost, the team assessed whether financial resources were considered during program rollout. A majority of studies mentioned finances related to implementation (11 studies in total, 8 of which described financial barriers and 3 that described appropriate internal resource allocation). The financial challenges were primarily medical care reimbursement challenges (eg, Sugarman et al39). Other examples of unmet financial needs included lack of funds for supplies/services (such as Wi-Fi access in Bolin et al30) or certification processes (such as paying to become designated as a “baby friendly” hospital in Labbok et al36).
Five of the 6 external programs mentioned financial barriers to implementation. This was in contrast to 3 of 13 internally developed programs that mentioned successful financial planning, another 3 that described financial barriers, and 7 that did not mention implementation costs.
5. Finally, it was noted whether each article discussed the sustainment plans for the program. Overall, 14 articles mentioned sustainment. Assessment of sustainment was somewhat less strict than the other implementation outcomes because in most of the articles not enough time had elapsed since program launch to definitively comment about sustainment. However, it was noted if they mentioned concrete plans or first steps toward maintaining the program. In the case of Braun et al,32 the authors had 2 years of evaluation data and more than 5 total years of implementation experience co-locating dental hygienists into community clinics. Similarly, Dennehy et al34 described their ability to obtain additional grant funding to maintain a community-based practice research network to pull data from electronic health records that were implemented during the initial project. In contrast, the diabetes improvement efforts described in Clark et al33 mentioned plans for spread without evidence of sustainment.
Three of 6 externally developed programs described continuation of the intervention at limited sites and only 1 article mentioned widespread maintenance. Of the internal articles, 9 of 13 studies described sustainment positively, with examples such as shared vision and trust for continuing the program, plans for ongoing staff training and engagement, and intermediate billing mechanisms to ensure reimbursement.
Articles of Interest.
Several included studies provided key examples of note, especially in combining various implementation methods, highlighted with an asterisk in Table 2.
Planning Articles
Of the 7 planning articles (Table 3), 4 described the collection of qualitative pre-implementation data to plan an implementation,48–51 while the other 3 were protocols.52–54
Table 3.
Planning Studiesa.
| Author | Year | Methods | Intervention/Program | Clinical Setting | Implementation Stage | Internal vs External |
|---|---|---|---|---|---|---|
| Angier H | 2015 | Mixed methods (quantitatively assess health insurance coverage continuity and utilization of health care services, assess implementation process with staff) | Care processes; technology (identify and outreach to uninsured patients) | 4 community clinics in Oregon | Protocol | Internal |
| Coker TR | 2014 | Mixed methods (expert panel ranking of models, and focus groups of WCC stakeholders) | Community engagement, care processes (redesign structure of pediatric care) | Multisite community clinic system and 2 independent practices serving Medicaid-insured children in Los Angeles area | Pre | External |
| Cole AM | 2015 | Qualitative (n = 13 interviews to assess facilitators and barriers to implementing program) | Care processes (mail-based colorectal cancer screening) | 7 community clinics in Washington, Wyoming, Alaska, Montana, and Idaho practice-based research network | Pre | External |
| Gold R | 2015 | Mixed methods (baseline surveys of study clinic characteristics, intervention uptake rates, document review, and qualitative observations/interviews) | Care processes (diabetes quality improvement intervention) | 29 community clinics through OCHIN, Inc. national network | Protocol | External |
| Nguyen OK | 2015 | Qualitative (n = 50 interviews with health care and social service providers to determine feasibility) | Community engagement; care processes; technology (electronic data exchange between health care systems and social service departments) | Urban integrated safety net system in Dallas County, Texas | Pre | Internal |
| Patterson ME | 2016 | Qualitative (n = 6 providers in semistructured interviews) | Care processes; technology (develop an EHR tool to categorize high-risk heart failure patients) | Urban safety net hospital in Kansas City | Pre | Internal |
| Quanbeck AR | 2014 | Mixed methods (interrupted time-series analysis of treatment attendance, staff interviews to assess adaptations to implementation protocol) | Care processes; technology (electronic communication for substance abuse treatment) | 3 community clinics (one affiliated with University of Wisconsin, one independent rural site, and one urban site) | Protocol | External |
Abbreviations: EHR, electronic health record; WCC, well-child care.
The 7 planning articles encompassed research that had (1) a protocol focus or (2) pre-implementation data collection to inform a future program or intervention.
Four planning-phase articles were conducted within community health centers, and all of the studies described programs that were focused on care process in terms of implementing new communication modalities (eg, health information exchanges), care management programs (eg, risk stratification for heart failure patients), and patient tracking systems (eg, insurance coverage tracking). The implementation outcomes among these planning articles were not examined, as they did not include data from the actual implementation phase.
Discussion
This review aimed to directly compare studies by evaluating implementation outcomes in a systematic way. This study found that internally developed programs within safety net sites were more likely to be aligned with overall organizational priorities, and demonstrated higher rates of acceptability and local customization by staff and providers. Moreover, internally developed interventions included more up-front planning efforts for system-wide integration and sustainment. However, the findings also highlight common challenges faced by safety net health care organizations, including diffusing successful programs across systems, and working with external collaborators/networks.
For internally developed innovations, lack of standardization across sites may impede the innovative practices from functioning as intended. Further shortcomings common among internally developed programs are understaffing and high staff turnover. This near-universal barrier must be addressed in order for safety net health care systems to be able to innovate in meaningful and sustainable ways. Finally, a focus on generating innovative practices internally may result in “self-siloing,” a failure to look outward for innovations, resulting in delayed uptake of novel evidence-based practices that have been developed in other health care settings. This may contribute to the slow translation of evidence into practice.55 Ideally, safety net health systems would regularly survey health system evidence that is relevant to their patient populations to identify innovative practices to implement and would have structures in place to judge the benefit of, and incorporate, these innovations.
Limitations
Despite its strengths, this study does have some limitations. Relevant studies may have been overlooked in the search process, despite adherence to guidelines for systematic reviews.56 Because interventions were included based on the setting—the US ambulatory safety net health system—rather than a specific clinical area, outcomes could not be combined across studies. The study team believes that there are shared lessons in implementing new practices across a variety of clinical problems across safety net delivery systems, and therefore chose to structure the review to encompass diverse interventions.
Conclusions
The findings suggest that there are unrealized opportunities for sharing innovations across like-minded institutions and for bidirectional engagement between external stakeholders and frontline staff to enhance acceptability and permit internal customization. Because external stakeholders often bring expertise and resources, enhancing collaboration between them and safety net health centers has the potential to catalyze innovation. Practice-based research networks serve as a model for this type of engagement.56
Implications.
Future work on safety net health system innovation should examine how programs and novel interventions are “made” or “remade” internally in order to benefit from the advantages of internally developed programs, while maintaining some standard features that would make their outcomes comparable across sites/settings. This may require a closer alignment with teams that incorporate implementation science as well as practice-based research methods.52,57 Both external stakeholders and safety net leadership will need to change the way they partner on innovation. Key strategies that fostered internal innovation in this review—such as emphasis on local ownership, scope for customization, and planning for sustainment—could be combined with continued emphasis on standard benchmarks for both key processes and outcomes.
Moving forward, additional evidence will be needed to determine if safety net organizations are able to sustain long-term health improvements from their implementation, as well as how implementation research can be used to optimize how innovative practices are incorporated into clinical settings. Systematic discussion of acceptability, appropriateness, fidelity, cost, and diffusion/sustainment would advance the study of health system improvement and permit more rapid spread and scale of innovations.
Acknowledgments
This work was made possible with funding from Blue Shield of California Foundation. Drs. Lyles, Schillinger, Handley, and Ackerman received support.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: through a grant from the Agency for Healthcare Research and Quality (AHRQ; R24HS022047). Dr Sarkar has grant support from the NIH National Cancer Institute (NCI; K24CA212294-01). Dr Schillinger receives support from the National Institute of Diabetes and Digestive and Kidney Diseases through the HMORN-UCSF Center for Diabetes Translational Research (NIDDK; 2P30 NIDDK092924-06). The remaining authors have no disclosures. No funders had a role in the study design, data collection and analysis, or preparation of the manuscript.
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.OECD/Eurostat. Oslo Manual: Guidelines for Collecting and Interpreting Innovation Data. Paris, France: OECD Publishing; 2005. [Google Scholar]
- 2.Hwang J, Christensen CM. Disruptive innovation in health care delivery: a framework for business-model innovation. Health Aff (Millwood). 2008;27:1329–1335. [DOI] [PubMed] [Google Scholar]
- 3.Lyles CR, Aulakh V, Jameson W, Schillinger D, Yee H, Sarkar U. Innovation and transformation in California’s safety net health care settings: an inside perspective. Am J Med Qual. 2014;29:538–545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McNulty T, Ferlie E. Process transformation: limitations to radical organizational change within public service organizations. Organization Studies. 2004;25:1389–1412. [Google Scholar]
- 5.Fleuren M, Wiefferink K, Paulussen T. Determinants of innovation within health care organizations: literature review and Delphi study. Int J Qual Health Care. 2004;16:107–123. [DOI] [PubMed] [Google Scholar]
- 6.Scott T, Mannion R, Davies HT, Marshall MN. Implementing culture change in health care: theory and practice. Int J Qual Health Care. 2003;15:111–118. [DOI] [PubMed] [Google Scholar]
- 7.Bindman AB, Chen A, Fraser JS, Yee HF Jr, Ofman D. Healthcare reform with a safety net: lessons from San Francisco. Am J Manag Care. 2009;15:747–750. [PubMed] [Google Scholar]
- 8.Institute of Medicine. America’s Health Care Safety Net: Intact but endangered. http://www.nationalacademies.org/hmd/Reports/2000/Americas-Health-Care-Safety-Net-Intact-but-Endangered.aspx. Published January 1, 2000. Accessed July 1, 2016.
- 9.California HealthCare Foundation. California’s Health Care Safety Net: facts and figures. https://www.chcf.org/wp-content/uploads/2017/12/PDF-CAHealthCareSafetyNetFactsFigures.pdf. Published 2010. Accessed August 28, 2018.
- 10.Greenhalgh T, Robert G, Macfarlane F, Bate P, Kyriakidou O. Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Q. 2004;82:581–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Team CR. Consolidated framework for Implementation Research. http://cfirguide.org/. Accessed June 1, 2017.
- 12.McMullen H, Griffiths C, Leber W, Greenhalgh T. Explaining high and low performers in complex intervention trials: a new model based on diffusion of innovations theory. Trials. 2015;16:242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stetler CB, Ritchie JA, Rycroft-Malone J, Schultz AA, Charns MP. Institutionalizing evidence-based practice: an organizational case study using a model of strategic change. Implement Sci. 2009;4:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berwick DM. Disseminating innovations in health care. JAMA. 2003;289:1969–1975. [DOI] [PubMed] [Google Scholar]
- 15.Brewster AL, Curry LA, Cherlin EJ, Talbert-Slagle K, Horwitz LI, Bradley EH. Integrating new practices: a qualitative study of how hospital innovations become routine. Implement Sci. 2015;10:168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dilling JA, Swensen SJ, Hoover MR, et al. Accelerating the use of best practices: the Mayo Clinic model of diffusion. Jt Comm J Qual Patient Saf. 2013;39:167–176. [DOI] [PubMed] [Google Scholar]
- 17.Evashwick C, Ory M. Organizational characteristics of successful innovative health care programs sustained over time. Fam Community Health. 2003;26:177–193. [DOI] [PubMed] [Google Scholar]
- 18.Fitzgerald L, Ferlie E, Wood M, Hawkins C. Interlocking interactions, the diffusion of innovations in health care. Human Relations. 2002;55:1429–1449. [Google Scholar]
- 19.Hernandez SE, Conrad DA, Marcus-Smith MS, Reed P, Watts C. Patient-centered innovation in health care organizations: a conceptual framework and case study application. Health Care Manag Rev. 2013;38:166–175. [DOI] [PubMed] [Google Scholar]
- 20.ten Ham W, Minnie K, van der Walt C. Integrative review of benefit levers’ characteristics for system-wide spread of best healthcare practices. J Adv Nurs. 2016;72(1):33–49. [DOI] [PubMed] [Google Scholar]
- 21.SQUIRE. SQUIRE 2.0 Guidelines. http://www.squire-statement.org/index.cfm?fuseaction=Page.ViewPage&pageId=471. Accessed June 1, 2017.
- 22.Leeman J, Calancie L, Kegler MC, et al. Developing theory to guide building practitioners’ capacity to implement evidence-based interventions. Health Educ Behav. 2017;44:59–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harrison MI, Kimani J. Building capacity for a transformation initiative: system redesign at Denver Health. Health Care Manag Rev. 2009;34:42–53. [DOI] [PubMed] [Google Scholar]
- 24.Abdallah A Implementing quality initiatives in healthcare organizations: drivers and challenges. Int J Health Care Qual Assur. 2014;27:166–181. [DOI] [PubMed] [Google Scholar]
- 25.Longo F Implementing managerial innovations in primary care: can we rank change drivers in complex adaptive organizations? Health Care Manag Rev. 2007;32:213–225. [DOI] [PubMed] [Google Scholar]
- 26.Lessard S, Bareil C, Lalonde L, et al. External facilitators and interprofessional facilitation teams: a qualitative study of their roles in supporting practice change. Implement Sci. 2016;11:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stetler CB, Legro MW, Rycroft-Malone J, et al. Role of “external facilitation” in implementation of research findings: a qualitative evaluation of facilitation experiences in the Veterans Health Administration. Implement Sci. 2006;1:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Breslau ES, Weiss ES, Williams A, Burness A, Kepka D. The implementation road: engaging community partnerships in evidence-based cancer control interventions. Health Promot Pract. 2015;16:46–54. [DOI] [PubMed] [Google Scholar]
- 29.Breslau ES, Rochester PW, Saslow D, Crocoll CE, Johnson LE, Vinson CA. Developing partnerships to reduce disparities in cancer screening. Prev Chronic Dis. 2010;7(3):A62. [PMC free article] [PubMed] [Google Scholar]
- 30.Bolin JN, Ory MG, Wilson AD, Salge L. Diabetes education kiosks in a Latino community. Diabetes Educ. 2013;39:204–212. [DOI] [PubMed] [Google Scholar]
- 31.Borkowski N, Gumus G, Deckard GJ. Modifying physician behavior to improve cost-efficiency in safety-net ambulatory settings. J Ambul Care Manage. 2013;36:129–139. [DOI] [PubMed] [Google Scholar]
- 32.Braun PA, Kahl S, Ellison MC, Ling S, Widmer-Racich K, Daley MF. Feasibility of colocating dental hygienists into medical practices. J Public Health Dent. 2013;73:187–194. [DOI] [PubMed] [Google Scholar]
- 33.Clark NM, Quinn M, Dodge JA, Nelson BW. Alliance system and policy change: necessary ingredients for improvement in diabetes care and reduction of disparities. Health Promot Pract. 2014;15(2 suppl):11S–22S. [DOI] [PubMed] [Google Scholar]
- 34.Dennehy P, White MP, Hamilton A, et al. A partnership model for implementing electronic health records in resource-limited primary care settings: experiences from two nurse-managed health centers. J Am Med Inform Assoc. 2011;18:820–826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Johnson TL, Brewer D, Estacio R, et al. Augmenting predictive modeling tools with clinical insights for care coordination program design and implementation. EGEMS (Wash DC). 2015;3(1):1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Labbok MH, Taylor EC, Nickel NC. Implementing the ten steps to successful breastfeeding in multiple hospitals serving low-wealth patients in the US: innovative research design and baseline findings. Int Breastfeed J. 2013;8(1):5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ramos-Gomez FJ. A model for community-based pediatric oral heath: implementation of an infant oral care program. Int J Dent. 2014;2014:156821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Steiner BD, Denham AC, Ashkin E, Newton WP, Wroth T, Dobson LA Jr. Community care of North Carolina: improving care through community health networks. Ann Fam Med. 2008;6:361–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sugarman JR, Phillips KE, Wagner EH, Coleman K, Abrams MK. The safety net medical home initiative: transforming care for vulnerable populations. Med Care. 2014;52(11 suppl 4):S1–S10. [DOI] [PubMed] [Google Scholar]
- 40.Waitzkin H, Getrich C, Heying S, et al. Promotoras as mental health practitioners in primary care: a multi-method study of an intervention to address contextual sources of depression. J Community Health. 2011;36:316–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Garg SK, Lyles CR, Ackerman S, et al. Qualitative analysis of programmatic initiatives to text patients with mobile devices in resource-limited health systems. BMC Med Inform Decis Mak. 2016;16:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McMullen CK, Schneider J, Firemark A, Davis J, Spofford M. Cultivating engaged leadership through a learning collaborative: lessons from primary care renewal in Oregon safety net clinics. Ann Fam Med. 2013;11(suppl 1):S34–S40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Novick G, Womack JA, Lewis J, et al. Perceptions of barriers and facilitators during implementation of a complex model of group prenatal care in six urban sites. Res Nurs Health. 2015;38:462–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Smith MG, Ferreri SP, Brown P, Wines K, Shea CM, Pfeiffenberger TM. Implementing an integrated care management program in community pharmacies: a focus on medication management services. J Am Pharm Assoc (2003). 2017;57:229–235.e221. [DOI] [PubMed] [Google Scholar]
- 45.Wagner EH, Gupta R, Coleman K. Practice transformation in the safety net medical home initiative: a qualitative look. Med Care. 2014;52(11 suppl 4):S18–S22. [DOI] [PubMed] [Google Scholar]
- 46.Drainoni ML, Koppelman EA, Feldman JA, et al. Why is it so hard to implement change? A qualitative examination of barriers and facilitators to distribution of naloxone for overdose prevention in a safety net environment. BMC Res Notes. 2016;9:465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Samaan ZM, Brown CM, Morehous J, Perkins AA, Kahn RS, Mansour ME. Implementation of a preventive services bundle in academic pediatric primary care centers. Pediatrics. 2016;137:e20143136. [DOI] [PubMed] [Google Scholar]
- 48.Coker TR, Moreno C, Shekelle PG, Schuster MA, Chung PJ. Well-child care clinical practice redesign for serving low-income children. Pediatrics. 2014;134:e229–e239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cole AM, Esplin A, Baldwin LM. Adaptation of an evidence-based colorectal cancer screening program using the consolidated framework for implementation research. Prev Chronic Dis. 2015;12:E213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nguyen OK, Chan CV, Makam A, Stieglitz H, Amarasingham R. Envisioning a social-health information exchange as a platform to support a patient-centered medical neighborhood: a feasibility study. J Gen Inter Med. 2015;30:60–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Patterson ME, Miranda D, Schuman G, Eaton C, Smith A, Silver B. A focus group exploration of automated case-finders to identify high-risk heart failure patients within an urban safety net hospital. EGEMS (Wash DC). 2016;4(3):1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Angier H, Marino M, Sumic A, et al. Innovative methods for parents and clinics to create tools for kids’ care (IMPACCT Kids’ Care) study protocol. Contemp Clin Trials. 2015;44:159–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gold R, Hollombe C, Bunce A, et al. Study protocol for “Study of Practices Enabling Implementation and Adaptation in the Safety Net (SPREAD-NET)”: a pragmatic trial comparing implementation strategies. Implement Sci. 2015;10:144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Quanbeck AR, Gustafson DH, Marsch LA, et al. Integrating addiction treatment into primary care using mobile health technology: protocol for an implementation research study. Implement Sci. 2014;9:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- 56.Agency for Healthcare Research and Quality. Early AHRQ support for Practice-Based Research Networks (PBRNs). https://archive.ahrq.gov/research/findings/factsheets/primary/earlypbrn/index.html. Accessed June 1, 2017.
- 57.Berkowitz SA, Percac-Lima S, Ashburner JM, et al. Building equity improvement into quality improvement: reducing socioeconomic disparities in colorectal cancer screening as part of population health management. J Gen Intern Med. 2015;30:942–949. [DOI] [PMC free article] [PubMed] [Google Scholar]


