Abstract
The incidence of bone tuberculosis is less than 5% of all tuberculosis cases. Furthermore, multifocal bone tuberculosis is uncommon, which rarely occurs without primary foci. It is difficult to diagnose, particularly if it is localized in both humeral heads. On the other hand, the isolated iliac bone tuberculosis is exceptional; it constitutes, also, a challenging diagnosis, which requires a high index of clinical suspicion and advanced investigations. Herein, we first report a case of multifocal tuberculosis of both humeral heads with no primary foci, and we secondarily report a case of isolated iliac bone tuberculosis. At last, however, the histological exam and polymerase chain reaction for the Mycobacterium tuberculosis complex are not always positives; they are mandatory as tests to ascertain the diagnosis.
Keywords: bone tuberculosis, polymerase chain reaction, anti-bacillary
INTRODUCTION
Multifocal bone tuberculosis (MBT) is rare, which rarely occurs without primary foci [1]. Given that it is frequently confused with a malignant tumour, the MBT presents a real challenging diagnosis, especially if it is localized in both humeral heads. Additionally, the isolated iliac bone tuberculosis is extremely rare, and it accounts for less than 1% of all skeletal tuberculosis cases. Its diagnosis is not easy to ascertain because it can mimic many pathologies [2]. Herein, we report two cases that represent, respectively, these two rare entities of extra-pulmonary tuberculosis and report how they were best managed.
CASE REPORT
Case 1
An 81-year-old patient, with a history of prostate disease, presented gradual pain of both shoulders for 1 year. He was put under oral analgesics and anti-inflammatory drugs by several physicians, while no radiograph was performed. At home, the patient reported a decrease of the pain, but he continued to present a recurrent pain in the same localization burning in type with night sweats. Because of pain got worst, he was transferred to our orthopaedic department. On admission, he was cachectic with no signs of pulmonary disease. The examination of both shoulders revealed only a limitation of joint mobility due to pain. The X-rays of both shoulders showed geodes and lytic lesions at both humeral heads (Fig. 1). The computed tomography scan was performed that suggested either multiple myeloma or diffuse bone tuberculosis (Fig. 2). The Technetium 99-m bone scan revealed increased uptake at the skull, both clavicles and both humeral heads (Fig. 3). Biologically: Mantoux test was positive, erythrocyte sedimentation was at 110 mm/h; C-reactive protein was at 15 mg/l; and white blood cell count, serum calcium, serum phosphorus, protein electrophoresis and QuantiFERON test were normal. A few days later, a biopsy of the left humeral head was performed. Two weeks later, the histopathological finding showed a non-specific chronic inflammations. At 6 weeks, the polymerase chain reaction for Mycobacterium tuberculosis on obtained bone tissue biopsies revealed sensitive Mycobacterium tuberculosis, so the patient was put on antitubercular drugs (isoniazid (5 mg/kg/day), rifampicin (10 mg/kg/day), ethambutol (20 mg/kg/day) and pyrazinamide (20 mg/kg/day)) for 2 months, and she continued rifampicin and isoniazid for 8 additional months. At the last follow-up of 2 years, his shoulders were painless with regain of weight and recovery of a satisfactory range of motion of both shoulders. The control radiographs showed stable lesions of both humeral heads.
Figure 1.
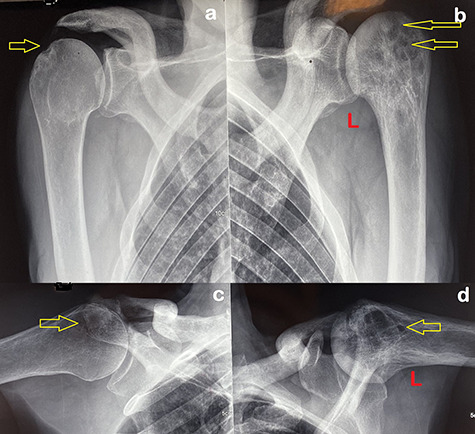
Radiographs of both shoulders (anterior-posterior views (a, b) lateral views (c, d) revealed lytic lesions and geodes in humeral heads (arrows)).
Figure 2.

Computed tomography scan of the left shoulder showed intramedullary lytic lesions of the left humeral head.
Figure 3.

Technetium 99-m bone scan demonstrated increased uptake at the skull, both clavicles and both humeral heads.
Case 2
A 38-year-old female, with congenital malformation of the pelvis, suffered from chronic pain at the left iliac fossa with constipation for 6 months. She consulted several physicians who prescribed oral analgesics and laxatives. At home, she temporarily did well, but the pain reappeared at the same localization. Given that the pain got worst, she was transferred to the emergency department. On arrival, an X-ray of the pelvis was performed; it showed lytic bone lesions, and then she was referred to our orthopaedic department. On examination, she was in poor general health. The palpation of the left iliac fossa was painful as well as the mobilization of the ipsilateral hip. The neurovascular examination was normal. At this follow-up, the patient did not report night sweats or pulmonary symptoms; however, she reported that her father had a pulmonary tuberculosis, which was treated, 2 years ago, with good outcomes. The pelvic X-ray revealed: multiple circumference lytic lesions at the left iliac bone (Fig. 4). Therefore, we performed a pelvic computed tomography scan that showed fluid collection within the left iliopsoas muscle and osteitis of the ipsilateral iliac bone (Fig. 5). Biologically: Mantoux test was positive, hemoglobin was at 12 g/dl, white-blood-cell count was at 15100/mm3; C reactive protein was at 115 mg/l; QuanTIFERON test was positive; and her serum ionized calcium, serum phosphate levels and serum protein electrophorese were normal. Few days later, the patient underwent surgery. We performed a vertical approach centred on the left iliac crest; the bacteriological samples and bone biopsy were taken, followed by copious irrigation with saline serum, after which a redon drain was inserted for 24 hours. The post-operative care was uneventful. She was discharged with oral analgesics to be reviewed in 2 weeks. At this follow-up, the histological examination revealed a chronic granulomatous inflammation with epithelioid and giant cells and central necrosis (Fig. 6), while the PCR was negative. Based on clinical, biological and histological findings, and given that the patient’s health got worse, we decided to put the patient on anti-bacillary treatment following the same protocol as the previous case. At 3 months of follow-up, the patient reported no recurrent pain; she was at good general health with considerable regain of weight. However, since this follow-up, the patient did not return to the consultation.
Figure 4.
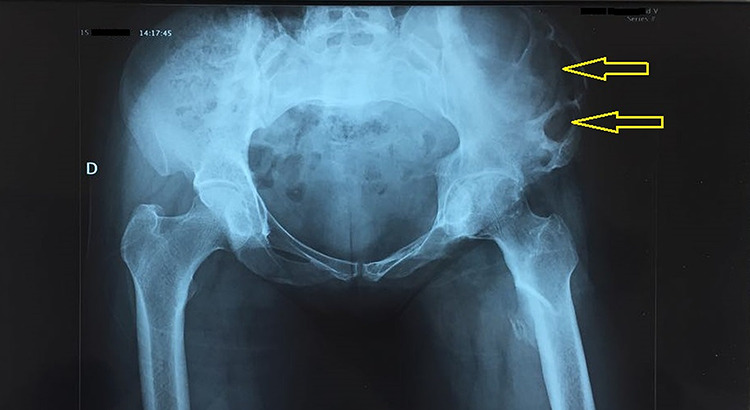
Radiograph of the pelvis showed the multiple circumference lytic lesions on the left iliac bone (arrows).
Figure 5.

Computed tomography scan of the pelvis (without contrast (A), with contrast (B)) showed a fluid collection of the iliopsoas muscle (red arrows) along with osteitis and lytic lesions of the left iliac bone (yellow arrows).
Figure 6.
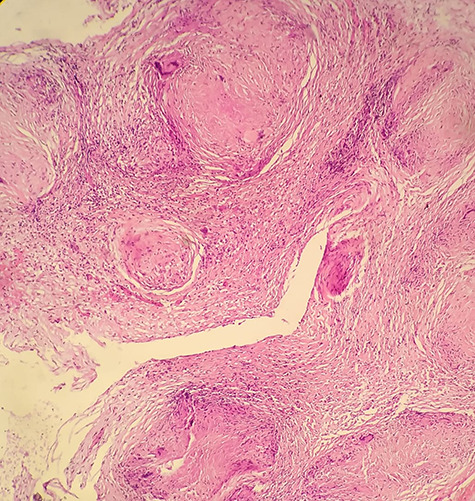
The histopathological examination revealed chronic granulomatous inflammation with epithelioid and giant cells and central necrosis.
DISCUSSION
The Multifocal bone involvement occurs at two or more locations in the skeletal system, which is uncommon even in endemic areas [3]. The pain constitutes the main and the first symptom reported by all patients, followed by weight loss at an advanced stage [4]. Given the lack of specificity and its rarity, its diagnosis is difficult to achieve, which increased considerably the cases misdiagnosed. The presence of primary foci can orient the diagnosis. As a reflex, every patient who presents long-term bone pain with fever and weight loss should raise the clinical suspicion of probable bone tuberculosis. Once suspected, the Mantoux test and the QuanTIFERON test, used as an ‘aid’ in the diagnosis, should be performed [5, 6]. On radiography, it showed geodic and lytic lesions, but no image is pathognomonic. Computed tomography scan revealed bone destruction with adjacent soft-tissue masses. Magnetic resonance imaging is useful in delineating the extent of disease, particularly for the spinal axis. Surely, it would be useful if we had performed the MRI for the second case [7]. Histology is the most sensitive single procedure. The diagnosis of tuberculosis requires the detection of Mycobacterium tuberculosis from the biological sample by at least one of the current microbiological techniques: microscopical analysis, isolation in culture or molecular methods [6]. Currently, the use of polymerase chain reaction on obtained tissue biopsies seems to be a valuable diagnostic tool [8].
CONFLICT OF INTEREST
All authors declare that they don’t have a conflict of interest.
FUNDING
There were no sources of funding.
CONSENT
The patient had given his written consent for publication.
GUARANTOR
The guarantor is Dr Naoufal Elghoul.
ACKNOWLEDGEMENT
Nil.
REFERENCES
- 1. Zhang L, Wang J, Feng X, Tao Y, Yang J, Zhang S et al. Multifocal skeletal tuberculosis: a case report. Exp Ther Med 2016;11:1288–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Stingo FE, Rodriguez-Fontan F, Burger-Van der Walt E, Arce J, Garcia SN, Munafo RM. Isolated iliac crest tuberculosis: a case report. JBJS Case Connect 2018;8:e31. [DOI] [PubMed] [Google Scholar]
- 3. Yilmaz MH, Kantarci F, Mihmanli I, Kanberoglu K. Multifocal skeletal tuberculosis. South Med J 2004;97:785–7. [DOI] [PubMed] [Google Scholar]
- 4. Polley P, Dunn R. Noncontiguous spinal tuberculosis: incidence and management. Eur Spine J 2009;18:1096–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Davidson PT, Horowitz I. Skeletal tuberculosis: a review with patient presentations and discussion. Am J Med 1970;48:77–84. [DOI] [PubMed] [Google Scholar]
- 6. Delogu G, Sali M, Fadda G. The biology of mycobacterium tuberculosis infection. Mediterr J Hematol Infect Dis 2013;5:e2013070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Omari B, Robertson JM, Nelson RJ, Chiu LC. Pott’s disease: a resurgent challenge to the thoracic surgeon. Chest 1989;95:145–50. [DOI] [PubMed] [Google Scholar]
- 8. Titov AG, Vyshnevskaya EB, Mazurenko SI, Santavirta S, Konttinen Y. Use of polymerase chain reaction to diagnose tuberculous arthritis from joint tissues and synovial fluid. Arch Pathol Lab Med 2004;128:205–9. [DOI] [PubMed] [Google Scholar]


