Abstract
Background: We aimed to investigate the association between physical activity and successful aging among middle-aged and older adults and study how this association changes with age and time.
Results: The mean score of Newcastle-Ottawa Scale assessment was 8.0±0.8. Physically active middle-aged and older adults were more likely to age successfully than sedentary adults (OR=1.64, 95%CI: 1.40–1.94). The effect of physical activity was stronger in the younger group (OR=1.71, 95%CI: 1.41–2.08) than on the older group (OR=1.54, 95%CI: 1.13–2.08). However, the protective effect of physical activity reduced annually by approximately 3%.
Conclusions: Physical activity promotes successful aging among middle-aged and older adults especially in the younger population. Being physically active at middle and old age is beneficial to successful aging.
Methods: We searched for the relevant studies in three online databases: Pubmed, Web of Science, and Embase. Fifteen community-based cohort studies were included. The Newcastle-Ottawa Scale assessment Form was used for quality assessment. Overall, 189,192 participants aged 43.9-79.0 years were analyzed. The odds ratio for successful aging of the most physically active group compared with sedentary group was analyzed. Subgroup analysis was conducted by age group. Univariate Meta-regression was performed according to follow-up years.
Keywords: successful aging, healthy aging, physical activity, exercise, older people
INTRODUCTION
Aging is a global problem. According to the World Health Organization’s report about global health and aging, the number of people aged ≥ 65 will increase to approximately 1.6 billion in 2050 and comprise 16% of the world’s population [1]. Aging is associated with health-related problems and substantial medical cost. Disease patterns among the elderly also shift to chronic non-communicable diseases such as cardiovascular disease, hypertension, diabetes, cancer, and dementia [1]. In the US, England, and Europe, approximately 43%–59% of adults aged 50–74 years experienced more than one mobility impairment [2]. Aging with disability demands long-term care [3]. The estimated duration of long-term care for Americans is approximately 2 years, and one-seventh of the US population need long-term care for more than 5 years [4]. There is a global trend of increase in the demand for long-term care. This means that people will experience a period of disability and dependence on others in their daily living before death.
Studies about successful aging have emerged in the past 20 years. Older adults who aged successfully maintain their function and experience morbidity and disability for a shorter period [5]. Successful aging means preserving life quality and reducing the health burden caused by aging [6]. Successful aging was proved to decrease the risk of long-term care [7]. Successful aging is a multidimensional concept and overlaps with “healthy aging,” “aging well,” and “positive aging” [8, 9]. In 1997, Rowe and Kahn proposed the biomedical theories of successful aging [10]. The biomedical theory included three components: the absence of disease and related risk factors, maintenance of physical and cognitive function, and active engagement with life. While the biomedical theory emphasized physical and cognitive functions, the psychosocial model highlighted life satisfaction and well-being, social participation and activity, personal growth, and psychological resources [11]. Additional views of successful aging included accomplishments, enjoyment of diet, financial security, neighborhood, and physical appearance [11]. Some review articles tried to organize the definition of successful aging into three domains: physiological, psychological, and social domains [12]. At present, successful aging is a complete and multi-aspect concept.
Many factors affect successful aging, including physiological, psychological, social, and lifestyle factors [13, 14]. Physical activity is an important lifestyle factor that can delay the onset of chronic diseases [15, 16], increase longevity and survival [17, 18], and improve cognitive and physical functions in the older people [19, 20]. However, previous studies on physical activity and successful aging reported inconsistent results. Some studies observed a strong correlation between physical activity and successful aging [21–23], while others showed a weak association [24–26].
Although previous a meta-analysis [27] integrated existing evidences to clarify the association between physical activity and successful aging, to our knowledge, no article has focused on middle-aged and older adults. In addition, studies discussing the effects of time on the association between physical activity and successful aging are also limited. Thus, the primary aim of this meta-analysis was to investigate the association between physical activity and successful aging for the middle-aged and older adults. The secondary aim was to demonstrate the effects of age and time. We hoped to shed light on how to promote successful aging in the global aging society.
RESULTS
Description of studies and quality assessment
We obtained 1,664 articles through the three research databases. Among the 1,394 articles without duplicate, only 43 discussed the association between physical activity and successful aging. To identify the causal inference of physical activity and successful aging, we excluded 19 cross-sectional studies. Finally, 15 cohort studies were included for analysis (Figure 1).
Figure 1.
Flow chart of search strategy.
Among the included articles, 10 were published in the recent 10 years (Table 1). The study population included older populations from Australia, United States, Britain, Europe, Nigeria, Cuba, Dominican Republic, Peru, Mexico, and Puerto Rico. The total sample size at baseline was 189,192. The mean age of participants ranged from 43.9-79.0 years. Participants of the seven studies were a mixture of middle-aged and older people. The follow-up duration in 10 studies was > 10 years.
Table 1. Characteristics of included studies.
| Study (Year) | Population | Age range (Baseline) | Mean age (Baseline) | Follow-up years | Follow-up rate (%) | Sample Size (Baseline) | Men (%) | Percentage of successful aging | Quality Score |
| Gopinath (2018) | Australia | ≥ 49 | 65.2 | 10 | 62.4 | 3,654 | 43.4 | 15.7 | 9 |
| Daskalopoulou (2018) | Cuba, Dominican Republic, Peru, Mexico and Puerto Rico | ≥ 65 | 74.2 | 4 | 66.4 | 10,900 | 33.8 | 15.1 | 8 |
| LaCroix (2016) | United States | 50-79 | 68.9 | 20 | 77.1 | 88,404 | 0 | 31 | 7 |
| Almeida (2014) | Australia | 65-83 | 72.1 | 11 | 43.6 | 12,201 | 100 | 11.7 | 6 |
| Bell (2014) | American men of Japanese ancestry | 72-82 | 75.7 | 21 | 77.4 | 1,292 | 100 | 34 | 6 |
| Gureje (2014) | Nigeria | ≥ 65 | 79 | 5 | 44.5 | 2,149 | 61.1 | 7.5 | 8 |
| Hodge (2014) | Australia | ≥ 57 | 64.1 | 13 | 74 | 25,607 | 38.6 | 18.6 | 8 |
| Hamer (2014) | British | ≥ 50 | 63.7 | 8 | 33.7 | 11,391 | 42.5 | 19.3 | 7 |
| Sabia (2012) | British | 35-55 | 51.3 | 18 | 77.3 | 6,599 | 70.5 | 18.7 | 8 |
| Sun (2010) | United States | 40-65 | 60 | 14 | >95 | 13,535 | 0 | 10.8 | 8 |
| Kaplan (2008) | Canada | 65-85 | 72.6 | 10 | 88.8 | 2,740 | 40.5 | 7.8 | 8 |
| Britton (2008) | British | 35-55 | 43.9 | 17 | 78.6 | 7,410 | 71.1 | 13.6 | 7 |
| Haveman-Nies (2003) | Europe | 70-75 | 72.5 | 10 | 58.7 | 2,200 | 49.6 | 28.8 | 7 |
| Ford (2000) | United States | ≥ 70 | 77.5 | 2 | 80.9 | 602 | 29.7 | 20.1 | 6 |
| Strawbridge (1996) | United States | ≥ 65 | 71.9 | 6 | 70.1 | 508 | 41 | 35 | 7 |
The criteria of physically active group differed among studies (Supplementary Table 1). Some studies used standard rating scale of physical activity such as international physical activity questionnaire [28], physical activity index [25], or Voorrips score [5]. Other studies used questionnaires to classify the level of physical activity. The included studies had varied definitions of successful aging. Most studies followed the biomedical model [10] that defines successful aging as the absence of chronic diseases and preservation of physical and cognitive functions. In eight studies [21, 22, 28–33], the rate of successful aging range from 10% to 20% (Table 1). Two cohort studies reported relatively low rate of successful aging. Kaplan et al. [34] reported 7.8% and Gureje et al. [35] reported 7.5% of successful aging.
Some studies recruited a special population. For example, Bell et al. [25] reported life factors associated with successful aging in American men of Japanese ancestry. LaCroix et al. [36] reported the predictors of successful aging for postmenopausal female veterans. Sun et al. [21] investigate the association of physical activity at midlife with successful survival for female registered nurses. Almeida et al. [30] investigated successful aging in older men. In other included studies, the participants were general population from communities. For the quality assessment, the quality score of the included studies, assessed by the Newcastle-Ottawa Quality Assessment Form, ranged from 7 to 9 (mean score: 8.0±0.8, Table 2).
Table 2. The quality assessment of included studies by the Newcastle-Ottawa Quality Assessment Form for cohort studies.
| Study (Years) | Selection | Comparability | Outcome | Total quality | |||||
| Representativeness of the exposed cohort | Selection of the non-exposed cohort | Ascertainment of exposures | Demonstration that outcome of interest was not present at start of study | Comparability of cohorts on the basis of the design or analysis controlled for confounders | Assessment of outcome | Was follow up long enough for outcomes to occur? | Adequacy of follow up of cohort | ||
| Acceptable | From community of general population | From the same community as exposed cohort | From structured interview | Yes | Yes, at least age and sex | Contained objective indicators | At least 4 years | Follow up rate more than 80%, or subjects lost to follow up unlikely to introduce bias | |
| Gopinath (2018) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| Daskalopoulou (2018) | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 1 | 8 |
| LaCroix (2016) | 0 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 8 |
| Almeida (2014) | 0 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 7 |
| Bell (2014) | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 |
| Gureje (2014) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 |
| Hodge (2014) | 1 | 1 | 0 | 1 | 2 | 1 | 1 | 1 | 8 |
| Hamer (2013) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 |
| Sabia (2012) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| Sun (2010) | 0 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 8 |
| Kaplan (2008) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| Britton (2008) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 9 |
| Haveman-Nies (2003) | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 0 | 8 |
| Ford (2000) | 1 | 1 | 0 | 1 | 2 | 1 | 0 | 1 | 7 |
| Strawbridge (1996) | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 7 |
Overall effect size
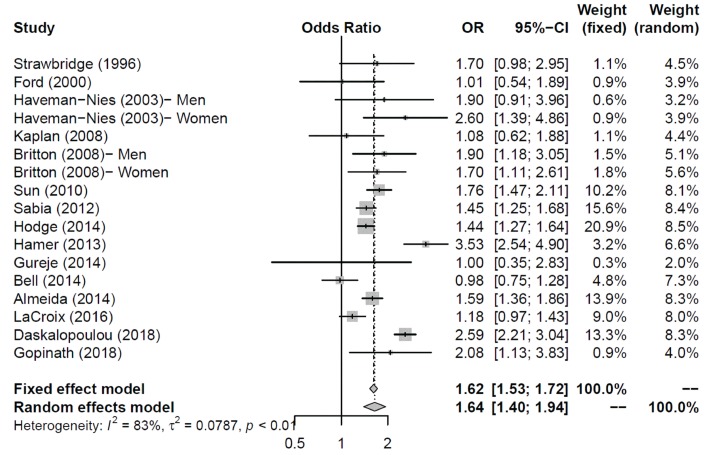
The overall odds ratio (OR) of physical activity to successful aging was 1.64 [95% confidence interval (CI) = 1.40–1.94] in the random-effects model (Figure 2). I2 (83%) revealed a high heterogeneity among the included studies. We further performed Egger’s test, and its p-value was 0.87. Thus, the publication bias did not exist at the 5% significant level. Although publication bias was not obvious in Egger’s test, the trim-and-fill method was still performed. However, no study was filled by the trim-and-fill method.
Figure 2.
The overall effect (odds ratio) of physical activity to successful aging.
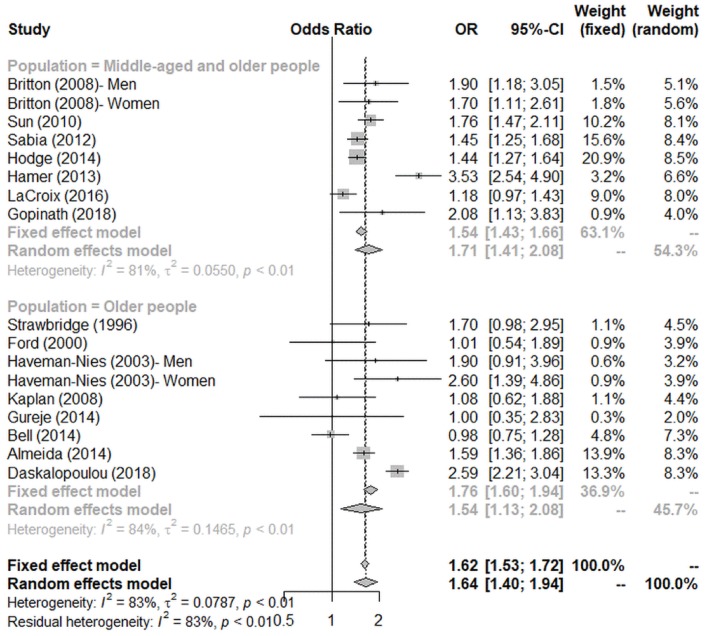
Subgroup analysis
Subgroup analysis (Figure 3) was conducted according to the age group of participants. When all the participants aged >65 years, the effect size became smaller (OR = 1.54, 95% CI = 1.13–2.08). On the contrary, we observed a larger effect in studies in which the recruited participants were a mixture of middle-aged and older adults (OR = 1.71, 95% CI = 1.41–2.08).
Figure 3.
Subgroup analysis by age on the association between physical activity and successful aging.
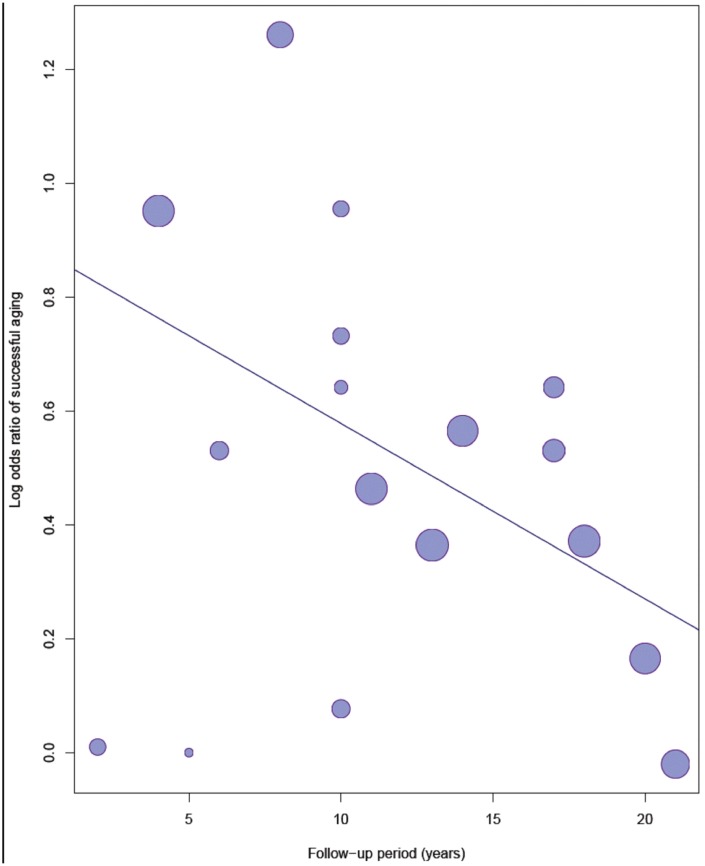
Meta-regression analysis
Figure 4 shows the bubble plot with fitted meta-regression line of the log OR of successful aging and follow-up years. In the univariate regression model, the regression line showed a significantly decreased trend of successful aging over time (OR= 0.97, 95% CI = 0.94–0.99, p = 0.045). The effect of physical activity on successful aging reduced annually by approximately 3%.
Figure 4.
Meta-regression analysis of the log odds ratio of physical activity to successful ageing and follow-up years.
DISCUSSION
This meta-analysis showed a protective effect of physical activity to successful aging among the middle-aged and older adults. The protective effect of physical activity to successful aging was larger on the younger group than the older group. Being physically active in earlier life is beneficial to successful aging in later life. However, the effect of physical activity on successful aging decreased as time elapsed.
Physical activity prevents the development of many chronic diseases, including metabolic syndrome, type 2 diabetes, coronary artery disease, hypertension, stroke, dyslipidemia, cognitive impairment, depression, osteoarthritis, osteoporosis, colon cancer, breast cancer, non-alcoholic fatty liver disease and sarcopenia [37]. Physical activity also increases longevity and survival [5, 38]. For middle-aged and older people, a dose-response relationship was found between physical activity and decrease in mortality [38]. Compared with sedentary older people, physically active older adults were more likely to remain living independently [17]. Physical activity in old age preserves the cognitive and physical functions [17, 39]. These previous findings supported the main finding of the present meta-analysis.
Physical activity is a protective factor of successful aging in the middle-aged and older adults. Although some included studies showed a weak association between physical activity and successful aging [24–26, 34–36], most studies reported a consistent positive relationship. Some studies with insignificant results [25, 36] included a specific population. Thus, the representativeness of the exposed cohort might be limited. Besides, the use of a very simple questionnaire to classify physical activity might lead to misclassification bias of exposure and influence the results [26]. The ratio of successful aging was relatively low in two studies. The rigorous definition of successful aging contributed to the low percentage of successful aging and reduced the effect of physical activity. Gureje et al. [35] defined successful aging as the absence of chronic diseases, including hypertension. Nevertheless, hypertension is very common in older people. In a survey for non-institutionalized population in England, US, and Canada, the prevalence of hypertension for older people aged 60-80 years was 63.7%, 63.6%, and 53.2%, respectively [40]. The strict definition of successful aging might result in the null effects of physical activity on successful aging.
Our main results were consistent with the past meta-analysis about physical activity and successful aging. Daskalopoulou et al. reported that physical activity had an effect size of 1.39 (95% CI = 1.23–1.57) on healthy aging [27]. In our study, the effect size of physical activity on successful aging was stronger because the included studies were not the same. Our results showed that the protective effects of physical activity to successful aging decreased over time. Time plays an important role in the aging process [41]. Thus, how to reduce the influence of time and preserve the benefits of physical activity would be issues we need to focus on. Further research is warranted if the effects of time could be attenuated by increasing the intensity of physical activity or combining other protective factors.
High heterogeneity was observed among the included studies. The diversity was caused by the different definitions of physical activity and successful aging. Unlike some diseases with diagnostic guideline, there are no standard criteria for defining successful aging. Although previous review articles [12, 13, 42] tried to organize the components of successful aging, researchers engaging in successful aging still used different domains and different weightings of the domains. The diversity resulted in the heterogeneity of successful aging in our analysis.
The criteria for grouping of physical activity differed among studies. Because most studies did not provide the quantitative data of physical activity, further analysis of the dose-response relationship between physical activity and successful aging is challenging. In our study, we used the effect size of the most vigorous activity group compared with the most sedentary group in each study to perform the meta-analysis. We could not conclude a quantitative suggestion of physical activity to successful aging for middle-aged and older adults. For the recommendations of physical activity for adults aged >65, WHO suggested that older adults should perform at least 150 min of moderate-intensity or 75 min of vigorous-intensity physical activity per week to improve cardiorespiratory function and muscle fitness [43].
The present study has some limitations. First, we included cohort studies, but not randomized control trails (RCTs). RCTs are undoubtedly the golden standard of study designs to clarify causal-inference. However, for physical activity and successful aging, it is difficult to blind the participants to the exposure (physical activity). Furthermore, the contamination effects in RCTs unavoidably occur with time. Current RCTs discussing the effects of physical activity on successful aging have short follow-up period and the small sample size [44, 45]. Well-designed observational studies were quite suitable for the discussions of such issue. Among the non-experimental study designs, cohort studies established a clear temporality to confirm the causal inference between exposure and outcome. Therefore, we included only cohort studies and excluded cross-sectional studies. Most of our included studies enrolled a representative population from the community. Thus, the generalizability of our results was feasible. Second, the dose-response relationship between physical activity and successful aging could not be established. Because the included studies lacked quantitative data of physical activity, we can only conclude that physical activity promotes successful aging in middle-aged and older adults. The dose-response relationship can be analyzed only if future studies used quantitative grouping of physical activity such as metabolic equivalents. Third, publication bias was possible. Studies with the null results might not be published. Studies not enrolled in Pubmed, Web of Science, and Embase as well as studies without using the keywords we used in our search process might be omitted. However, we conducted the Egger’s test, and the potential publication bias was not significant.
Despite these limitations, our study was the first meta-analysis to analyze the association between physical activity and successful aging especially for the middle-aged and older adults. In addition, we found that the protective effect of physical activity to successful aging attenuated over time. Our study contributed to the discussions of public health policy in the global aging society. The main focus of health promotion policy in the aging society is to encourage middle-aged and older adults to be physically active. Future research should aim at the quantitative suggestions of physical activity to reduce the effects of time.
CONCLUSIONS
This meta-analysis found a positive effect of physical activity to successful aging in middle-aged and older adults. However, the effect attenuated over time. Further research is warranted to establish the dose-response relationship between physical activity and successful aging as well as to reduce the effects of time.
MATERIALS AND METHODS
Search strategy
Literature review was conducted in the online databases of PubMed, Web of Science, and Embase from May 6, 2019, to July 5, 2019. We used the keywords “successful aging,” “healthy aging,” and “aging well” in the title and “physical activity” in all searching fields. We further limited the article type to original article and language to English. Cohort studies discussing the association of physical activity and successful aging were eligible for our analysis. Articles were excluded if (1) studies discussed other issues, (2) research objects were not humans, (3) the study design was cross-sectional, (4) the study population was not middle-aged or old people, (5) OR was not available, (6) full-text article was not available, and (7) studies other than original research such as review article, meta-analysis, letters, or case series. If two studies used the same data source and adjusted finely in methods, only one article was adopted.
Data extraction
The following information was extracted from the included studies: study population, baseline age, follow-up years, follow-up rate, sample size, proportion of men, rate of successful aging, definition of physical activity and successful aging, adjusted covariates, and treatment effects (OR). For studies that classified physical activity to more than two groups, the effect size of the most vigorous physically active group compared with the most sedentary group was considered for analysis. For studies that provided the OR of men and women separately, we considered the effects of both sexes in the overall analysis.
Quality assessment
We used the Newcastle-Ottawa Quality Assessment Form for Cohort Studies [46] to evaluate the quality of the included studies. The scale included three sections and eight items as follows: (1) representativeness of the exposed cohort, (2) selection of the non-exposed cohort, (3) ascertainment of exposure, (4) demonstration that the outcome of interest was not present at the start of the study, (5) comparability of cohorts on the basis of the design or analysis controlled for confounders, (6) assessment of outcome, (7) follow-up was long enough for outcomes to occur, (8) adequacy of follow-up of cohorts. The total score was 9 stars. Quality assessment was performed by two investigators. In case of differing opinions, a consensus was reached by discussion.
Data analysis
Statistical analysis was performed using R version 3.5.1 (R Foundation for Statistical Computing, Vienna, Austria). The overall effect was shown by the forest plot. As the included studies had different study population and design, we used the random-effects model to incorporate the heterogeneity [47]. We perform Egger’s test [48] to examine possible publication bias. Subgroup analysis was conducted to evaluate the effect size of different age groups. Meta-regression was then performed to show the effect of follow-up years. A p-value of <0.05 (two-tailed) was considered statistically significant.
Supplementary Material
ACKNOWLEDGMENTS
I would like to express my deep gratitude to Prof. Kuo-Liong Chien and Yi-Chun Yeh PhD, Department of Public Health, College of Public Health, National Taiwan University, for their recommendations on the data processing and discussion. They provided useful suggestions about this work.
Abbreviations:
- CI
confidence interval
- OR
odds ratio
- RCTs
randomized control trails
- WHO
World Health Organization
Footnotes
AUTHOR CONTRIBUTIONS: YHL and YHT conceived and designed the study. YHL, YCC, YCT and STT performed literature review and data extraction. YHL and YCC analyzed the data. YHL and YHT wrote the paper. YHL, YCC, YCT, STT and YHT approved final manuscript.
CONFLICTS OF INTEREST: The authors declare that they have no conflict of interests.
FUNDING: This work was funded as a research project of Cheng Hsin General Hospital [CHGH109-(FA)01].
REFERENCES
- 1.World Health Organization, US National Institute of Aging. Global health and aging. Available at: https://www.who.int/ageing/publications/global_health/en/
- 2.Avendano M, Glymour MM, Banks J, Mackenbach JP. Health disadvantage in US adults aged 50 to 74 years: a comparison of the health of rich and poor Americans with that of Europeans. Am J Public Health. 2009; 99:540–48. 10.2105/AJPH.2008.139469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Meijer C, Koopmanschap M, D’ Uva TB, van Doorslaer E. Determinants of long-term care spending: age, time to death or disability? J Health Econ. 2011; 30:425–38. 10.1016/j.jhealeco.2010.12.010 [DOI] [PubMed] [Google Scholar]
- 4.Nguyen V. AARP Public Policy Institute. Long-term support and services. Available at: https://www.aarp.org/content/dam/aarp/ppi/2017-01/Fact%20Sheet%20Long-Term%20Support%20and%20Services.pdf
- 5.Haveman-Nies A, de Groot LC, van Staveren WA. Dietary quality, lifestyle factors and healthy ageing in Europe: the SENECA study. Age Ageing. 2003; 32:427–34. 10.1093/ageing/32.4.427 [DOI] [PubMed] [Google Scholar]
- 6.Michel JP, Sadana R. “Healthy Aging” Concepts and Measures. J Am Med Dir Assoc. 2017; 18:460–64. 10.1016/j.jamda.2017.03.008 [DOI] [PubMed] [Google Scholar]
- 7.Nosraty L, Pulkki J, Raitanen J, Enroth L, Jylhä M. Successful Aging as a Predictor of Long-Term Care Among Oldest Old: The Vitality 90+ Study. J Appl Gerontol. 2019; 38:553–71. 10.1177/0733464817716968 [DOI] [PubMed] [Google Scholar]
- 8.Zanjari N, Sharifian Sani M, Chavoshi MH, Rafiey H, Mohammadi Shahboulaghi F. Successful aging as a multidimensional concept: an integrative review. Med J Islam Repub Iran. 2017; 31:100. 10.14196/mjiri.31.100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Özsungur F. Women’s successful aging. Health Care Women Int. 2019; 1–21. [Epub ahead of print]. 10.1080/07399332.2019.1667994 [DOI] [PubMed] [Google Scholar]
- 10.Rowe JW, Kahn RL. Successful aging. Gerontologist. 1997; 37:433–40. 10.1093/geront/37.4.433 [DOI] [PubMed] [Google Scholar]
- 11.Bowling A, Dieppe P. What is successful ageing and who should define it? BMJ. 2005; 331:1548–51. 10.1136/bmj.331.7531.1548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Young Y, Frick KD, Phelan EA. Can successful aging and chronic illness coexist in the same individual? A multidimensional concept of successful aging. J Am Med Dir Assoc. 2009; 10:87–92. 10.1016/j.jamda.2008.11.003 [DOI] [PubMed] [Google Scholar]
- 13.Depp CA, Jeste DV. Definitions and predictors of successful aging: a comprehensive review of larger quantitative studies. Am J Geriatr Psychiatry. 2006; 14:6–20. 10.1097/01.JGP.0000192501.03069.bc [DOI] [PubMed] [Google Scholar]
- 14.Özsungur F. Gerontechnological factors affecting successful aging of elderly. Aging Male. 2019; 1–13. [Epub ahead of print]. 10.1080/13685538.2018.1539963 [DOI] [PubMed] [Google Scholar]
- 15.Marques A, Santos T, Martins J, Matos MG, Valeiro MG. The association between physical activity and chronic diseases in European adults. Eur J Sport Sci. 2018; 18:140–49. 10.1080/17461391.2017.1400109 [DOI] [PubMed] [Google Scholar]
- 16.Zhou P, Hughes AK, Grady SC, Fang L. Physical activity and chronic diseases among older people in a mid-size city in China: a longitudinal investigation of bipolar effects. BMC Public Health. 2018; 18:486. 10.1186/s12889-018-5408-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stessman J, Hammerman-Rozenberg R, Cohen A, Ein-Mor E, Jacobs JM. Physical activity, function, and longevity among the very old. Arch Intern Med. 2009; 169:1476–83. 10.1001/archinternmed.2009.248 [DOI] [PubMed] [Google Scholar]
- 18.Manini TM, Everhart JE, Patel KV, Schoeller DA, Colbert LH, Visser M, Tylavsky F, Bauer DC, Goodpaster BH, Harris TB. Daily activity energy expenditure and mortality among older adults. JAMA. 2006; 296:171–79. 10.1001/jama.296.2.171 [DOI] [PubMed] [Google Scholar]
- 19.Lautenschlager NT, Cox KL, Flicker L, Foster JK, van Bockxmeer FM, Xiao J, Greenop KR, Almeida OP. Effect of physical activity on cognitive function in older adults at risk for Alzheimer disease: a randomized trial. JAMA. 2008; 300:1027–37. 10.1001/jama.300.9.1027 [DOI] [PubMed] [Google Scholar]
- 20.Villareal DT, Chode S, Parimi N, Sinacore DR, Hilton T, Armamento-Villareal R, Napoli N, Qualls C, Shah K. Weight loss, exercise, or both and physical function in obese older adults. N Engl J Med. 2011; 364:1218–29. 10.1056/NEJMoa1008234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sun Q, Townsend MK, Okereke OI, Franco OH, Hu FB, Grodstein F. Physical activity at midlife in relation to successful survival in women at age 70 years or older. Arch Intern Med. 2010; 170:194–201. 10.1001/archinternmed.2009.503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sabia S, Singh-Manoux A, Hagger-Johnson G, Cambois E, Brunner EJ, Kivimaki M. Influence of individual and combined healthy behaviours on successful aging. CMAJ. 2012; 184:1985–92. 10.1503/cmaj.121080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Newman AB, Arnold AM, Naydeck BL, Fried LP, Burke GL, Enright P, Gottdiener J, Hirsch C, O’Leary D, Tracy R, and Cardiovascular Health Study Research Group. “Successful aging”: effect of subclinical cardiovascular disease. Arch Intern Med. 2003; 163:2315–22. 10.1001/archinte.163.19.2315 [DOI] [PubMed] [Google Scholar]
- 24.Ford AB, Haug MR, Stange KC, Gaines AD, Noelker LS, Jones PK. Sustained personal autonomy: a measure of successful aging. J Aging Health. 2000; 12:470–89. 10.1177/089826430001200402 [DOI] [PubMed] [Google Scholar]
- 25.Bell CL, Chen R, Masaki K, Yee P, He Q, Grove J, Donlon T, Curb JD, Willcox DC, Poon LW, Willcox BJ. Late-life factors associated with healthy aging in older men. J Am Geriatr Soc. 2014; 62:880–88. 10.1111/jgs.12796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Strawbridge WJ, Cohen RD, Shema SJ, Kaplan GA. Successful aging: predictors and associated activities. Am J Epidemiol. 1996; 144:135–41. 10.1093/oxfordjournals.aje.a008900 [DOI] [PubMed] [Google Scholar]
- 27.Daskalopoulou C, Stubbs B, Kralj C, Koukounari A, Prince M, Prina AM. Physical activity and healthy ageing: A systematic review and meta-analysis of longitudinal cohort studies. Ageing Res Rev. 2017; 38:6–17. 10.1016/j.arr.2017.06.003 [DOI] [PubMed] [Google Scholar]
- 28.Gopinath B, Kifley A, Flood VM, Mitchell P. Physical Activity as a Determinant of Successful Aging over Ten Years. Sci Rep. 2018; 8:10522. 10.1038/s41598-018-28526-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Daskalopoulou C, Koukounari A, Ayuso-Mateos JL, Prince M, Prina AM. Associations of Lifestyle Behaviour and Healthy Ageing in Five Latin American and the Caribbean Countries-A 10/66 Population-Based Cohort Study. Nutrients. 2018; 10:10. 10.3390/nu10111593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Almeida OP, Khan KM, Hankey GJ, Yeap BB, Golledge J, Flicker L. 150 minutes of vigorous physical activity per week predicts survival and successful ageing: a population-based 11-year longitudinal study of 12 201 older Australian men. Br J Sports Med. 2014; 48:220–25. 10.1136/bjsports-2013-092814 [DOI] [PubMed] [Google Scholar]
- 31.Hodge AM, O’Dea K, English DR, Giles GG, Flicker L. Dietary patterns as predictors of successful ageing. J Nutr Health Aging. 2014; 18:221–27. 10.1007/s12603-013-0405-0 [DOI] [PubMed] [Google Scholar]
- 32.Hamer M, Lavoie KL, Bacon SL. Taking up physical activity in later life and healthy ageing: the English longitudinal study of ageing. Br J Sports Med. 2014; 48:239–43. 10.1136/bjsports-2013-092993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Britton A, Shipley M, Singh-Manoux A, Marmot MG. Successful aging: the contribution of early-life and midlife risk factors. J Am Geriatr Soc. 2008; 56:1098–105. 10.1111/j.1532-5415.2008.01740.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kaplan MS, Huguet N, Orpana H, Feeny D, McFarland BH, Ross N. Prevalence and factors associated with thriving in older adulthood: a 10-year population-based study. J Gerontol A Biol Sci Med Sci. 2008; 63:1097–104. 10.1093/gerona/63.10.1097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gureje O, Oladeji BD, Abiona T, Chatterji S. Profile and determinants of successful aging in the Ibadan Study of Ageing. J Am Geriatr Soc. 2014; 62:836–42. 10.1111/jgs.12802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.LaCroix AZ, Rillamas-Sun E, Woods NF, Weitlauf J, Zaslavsky O, Shih R, LaMonte MJ, Bird C, Yano EM, LeBoff M, Washington D, Reiber G. Aging Well Among Women Veterans Compared With Non-Veterans in the Women’s Health Initiative. Gerontologist. 2016. (Suppl 1); 56:S14–26. 10.1093/geront/gnv124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol. 2012; 2:1143–211. 10.1002/cphy.c110025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gebel K, Ding D, Chey T, Stamatakis E, Brown WJ, Bauman AE. Effect of Moderate to Vigorous Physical Activity on All-Cause Mortality in Middle-aged and Older Australians. JAMA Intern Med. 2015; 175:970–77. 10.1001/jamainternmed.2015.0541 [DOI] [PubMed] [Google Scholar]
- 39.Reas ET, Laughlin GA, Bergstrom J, Kritz-Silverstein D, Richard EL, Barrett-Connor E, McEvoy LK. Lifetime physical activity and late-life cognitive function: the Rancho Bernardo study. Age Ageing. 2019; 48:241–46. 10.1093/ageing/afy188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Joffres M, Falaschetti E, Gillespie C, Robitaille C, Loustalot F, Poulter N, McAlister FA, Johansen H, Baclic O, Campbell N. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: a cross-sectional study. BMJ Open. 2013; 3:e003423. 10.1136/bmjopen-2013-003423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Harman D. The aging process. Proc Natl Acad Sci USA. 1981; 78:7124–28. 10.1073/pnas.78.11.7124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kim SH, Park S. A Meta-Analysis of the Correlates of Successful Aging in Older Adults. Res Aging. 2017; 39:657–77. 10.1177/0164027516656040 [DOI] [PubMed] [Google Scholar]
- 43.World Health Organization. Physical Activity and Older Adults- Recommended levels of physical activity for adults aged 65 and above. Available at: https://www.who.int/dietphysicalactivity/factsheet_olderadults/en/
- 44.Lara J, O’Brien N, Godfrey A, Heaven B, Evans EH, Lloyd S, Moffatt S, Moynihan PJ, Meyer TD, Rochester L, Sniehotta FF, White M, Mathers JC. Pilot Randomised Controlled Trial of a Web-Based Intervention to Promote Healthy Eating, Physical Activity and Meaningful Social Connections Compared with Usual Care Control in People of Retirement Age Recruited from Workplaces. PLoS One. 2016; 11:e0159703. 10.1371/journal.pone.0159703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bernardelli G, Roncaglione C, Damanti S, Mari D, Cesari M, Marcucci M. Adapted physical activity to promote active and healthy ageing: the PoliFIT pilot randomized waiting list-controlled trial. Aging Clin Exp Res. 2019; 31:511–18. 10.1007/s40520-018-1002-1 [DOI] [PubMed] [Google Scholar]
- 46.National Center for Biotechnology Information. Newcastle-Ottawa Quality Assessment Form for Cohort Studies. Available at: https://www.ncbi.nlm.nih.gov/books/NBK115843/figure/appe.fm3/?report=objectonly
- 47.Kriston L. Dealing with clinical heterogeneity in meta-analysis. Assumptions, methods, interpretation. Int J Methods Psychiatr Res. 2013; 22:1–15. 10.1002/mpr.1377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997; 315:629–34. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.