Abstract
BACKGROUND
Some recent studies reported an inverse association between obesity and risk of cardiovascular diseases (CVD), heart failure related mortality rate, outcomes of myocardial infarction (MI), and the consequences of cardiovascular events interventions; this inverse association was named the obesity paradox. The present study was conducted with the aim to determine whether the obesity paradox will be detectable when the 10-year risk of CVD is estimated using CVD risk assessment tools.
METHODS
The related data of 2910 subjects aged 40-74 years obtained in our cohort study that was carried out among 6140 subjects in Amol, in northern Iran, was included in this study. CVD risk assessment tools were used to estimate the 10-year risk of CVD. Obesity was evaluated using 4 indices, including waist circumference (WC), waist to height ratio (WHtR), waist to hip ratio (WHR), and body mass index (BMI). The receiver operating characteristic (ROC) curve analysis was utilized to evaluate the discriminatory power of obesity indices for 10-year risk of CVD.
RESULTS
Categorizing the participants to with and without obesity according to BMI showed that a significantly higher proportion of men with obesity had a 10-year risk of CVD ≥ 7.5% and ≥ 10% according to American College of Cardiology/American Heart Association (ACC/AHA) and the Framingham approaches, respectively. A higher proportion of women without obesity had a 10-year risk of CVD ≥ 7.5% than women with obesity based on the ACC/AHA equation (28.54% vs. 24.15%; P = 0.0707). BMI had a non-significant AUC (< 0.5) according to the the ACC/AHA equation.
CONCLUSION
BMI showed a weak and non-significant inverse association with 10-year risk of CVD estimated using pooled cohort equations of ACC/AHA in women. However, this result cannot directly provide enough evidence for the obesity paradox.
Keywords: Obesity, Cardiovascular Diseases, Risk Assessment, Body Mass Index
Introduction
Obesity is a very common condition worldwide. Between 1980 and 2013, the proportion of over-weigh adults and those with obesity increased from 28.8% to 36.9% in men, and from 29.8% to 38.0% in women.1
The rising trend of obesity in many countries led to very serious consequences at both individual and community levels.2 Obesity is an independent and modifiable risk factor for all-cause mortality including cardiovascular disease (CVD) related mortality rates.3-5 However, some recent studies have reported an inverse association between obesity and CVD risk, heart failure related mortality rate, myocardial infarction (MI) outcomes, and the consequences of CVD events interventions; this inverse association was named the obesity paradox.6,7
CVD risk assessment tools have been utilized to estimate the 10-year risk of CVD for years. In these tools, several modifiable and non-modifiable risk factors of CVD are utilized to predict the 10-year risk of CVD. The pooled cohort equations of the American College of Cardiology/American Heart Association (ACC/AHA) and the Framingham general cardiovascular risk profile (for use in primary care) were developed using some CVD risk factors including age, history of diabetes mellitus (DM), current smoking status, systolic blood pressure (SBP), total cholesterol and high density lipoprotein (HDL) in men and women, separately.8,9
Two versions of the Systematic Coronary Risk Evaluation (SCORE) equations were also developed according to the abovementioned risk factors, except for HDL and history of DM.10 None of the obesity indices are utilized in the abovementioned CVD risk assessment tools, Although, there are several simple indices to evaluate obesity, none of the obesity indices are utilized to predict the 10-year CVD risk in the abovementioned CVD risk assessment tools. Since the obesity paradox was confirmed for some CVD outcomes based on some obesity indices, particularly BMI, we aimed to determine whether the obesity paradox would be detectable when the 10-year risk of CVD and obesity are determined by mentioned risk assessment tools and obesity indices, respectively.
Materials and Methods
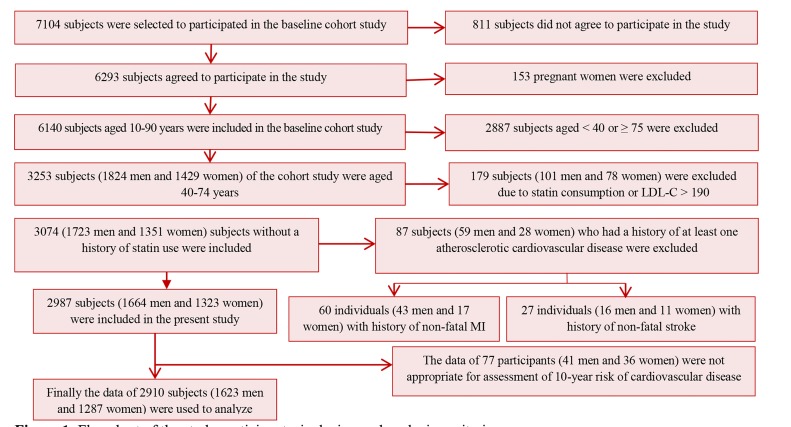
The present cohort study was conducted among 6140 subjects aged 10-90 years in northern Iran (Amol) in 2009-2010. We obtained the study sampling frame from health centers, where all residents had a health record file. The population of the city was categorized into 16 categories based on sex and age at the intervals of 10 years. We randomly selected the study participants from each category based on the proportion to size approach. All study arrangements were in accordance with the Helsinki Declaration. Informed consent was obtained from all study subjects, and the study was approved by the Ethics Committee of Iran University of Medical Sciences, Iran. Since the risk assessment tools are generally applied to the population aged 40-74 years (8-10), the data of 2910 subjects (1623 men and 1287 women) aged 40-74 years were utilized in this study. The study population and the study inclusion and exclusion criteria are displayed in figure 1.
Figure 1.
Flowchart of the study participants, inclusion and exclusion criteria
Anthropometric data and BP were measured by trained health care providers for each participant. The participants’ weight was measured without excess clothes and shoes. Their height was measured while they stood upright with their heels and buttocks in contact with the wall. The midpoint of the distance between the lowest costal ridge and the upper border of the iliac crest was considered as the waist circumference (WC). The largest circumference between the waist and knee was considered the hip circumference (HC). The health care providers measured BP in sitting position using a fitted cuff, following at least 5 minutes of rest.
Lipid profiles and fasting blood sugar (FBS) were evaluated following 12 hours of fasting. All tests, including FBS and lipid profiles, were assessed enzymatically according to protocol using an autoanalyzer (BS200, Mindray, China).
To determine the 10-year risk of CVD in the present study, 4 risk assessment tools, including pooled cohort equations of the ACC/AHA, SCORE equations for low and high risk European countries, and the Framingham general cardiovascular risk profile (for use in primary care), were used.8-10 While the ACC/AHA equations and Framingham tool estimate fatal and non-fatal 10-year risk of CVD, SCORE equations only estimate the fatal risk.
We changed the estimated risks into dichotomous scales according to a cut off point of 0.075 (7.5%) for ACC/AHA, 0.05 (5%) for SCORE equations, and 0.1 (10%) for the Framingham tool (8-10). Receiver operating characteristic (ROC) curve was used to assess the capability of BMI, WC, waist to hip ratio (WHR), and waist to height ratio (WHtR) in the discrimination of people with a 10-year risk ≥ 5%, ≥ 7.5%, and ≥ 10% (according to the related thresholds of the abovementioned CVD risk assessment tools) from people with a lower risk. In ROC curves, the sensitivities of infinite thresholds of obesity measures were plotted versus the associated false positive rates. Consequently, the associated areas under the curves (AUCs) were computed. The lowest threshold for AUC was considered as 0.5, meaning a significantly greater area than 0.5 signifies the power of obesity indices to distinguish participants with a higher 10-year risk of CVD than related thresholds in participants without those indices.
Furthermore, the values of obesity indices were categorized into dichotomous variables according to related data in previous literature. Thus, BMI was classified into a dichotomous variable based on a cut off point of 30 kg/m2 in women and men, WC was categorized based on a cut off point of 88 cm in women and 102 cm in men, WHR was categorized based on a cut off point of 0.85 in women and 0.9 in men, and WHtR was categorized based on a cut off point of 0.5 in women and men.11-13 Obesity was defined based on the abovementioned thresholds of each related obesity indice, and the 10-year risk of CVD was estimated in participants with and without obesity. The proportion of individuals who had a 10-year risk of CVD ≥ 7.5% based on ACC/AHA, ≥ 5% based on SCORE equations (low and high risk European countries), and ≥ 10% based on Framingham approach were compared between the groups with and without obesity using independent two group proportion test. Since the 10-year risk of CVD was estimated based on 4 risk assessment tools and obesity was determined according to 4 indices, 16 two group proportion tests were performed in men and women, separately.
Finally, several logistic regression analyses were separately performed in which each of the categorized obesity indices was considered a predictor and a 10-year risk of CVD ≥ 7.5%, ≥ 5%, and ≥ 10% was considered an outcome based on pooled cohort equations, SCORE equations, and the Framingham tool, respectively. In multiple logistic regression analyses, in addition to the evaluated obesity indices, LDL-C level, TG level, and diastolic blood pressure (DBP) were entered into the associated models. It is worth noting that these risk factors are not directly utilized in risk assessment tools to compute the 10-year risk of CVD.
A threshold of 0.05 (less than 0.05) was taken into account as the significance level for all analyses. All analyses were performed using Stata software (version 12; StataCorp, Texas, USA).
Results
The demographic characteristics of the participants are presented in table 1. The prevalence of diabetes in women was significantly higher than men (26.01% vs 13.4%; P < 0.0001). While the percentage of current smoking was 30.2% in men, it was only 0.84% in women (P < 0.0001).
Table 1.
Characteristics and clinical biomarkers of the study participants (n = 2910)
| Characteristics | Men (n = 1623) |
Women (n = 1287) |
P* |
|---|---|---|---|
| Means ± SD | |||
| Age (year) | 53.91 ± 9.36 | 53.50 ± 9.01 | 0.1890 |
| BMI (kg/m2) | 27.23 ± 4.27 | 31.23 ± 5.04 | < 0.0010 |
| WC (cm) | 93.54 ± 11.23 | 96.20 ± 11.55 | < 0.0010 |
| WHR | 0.93 ± 0.07 | 0.89 ± 0.08 | < 0.0010 |
| WHtR | 0.56 ± 0.07 | 0.62 ± 0.08 | < 0.0010 |
| DBP (mm Hg) | 78.10 ± 13.15 | 79.32 ± 12.90 | 0.0080 |
| SBP (mm Hg) | 119.01 ± 16.87 | 120.93 ± 18.21 | 0.0020 |
| FBS (mg/dl) | 103.01 ± 34.86 | 113.16 ± 48.67 | < 0.0010 |
| TG (mg/dl) | 155.21 ± 100.19 | 159.04 ± 108.57 | 0.3080 |
| Total cholesterol (mg/dl) | 187.13 ± 41.13 | 200.57 ± 43.28 | < 0.0010 |
| LDL (mg/dl) | 110.16 ± 30.61 | 117.48 ± 31.52 | < 0.0010 |
| HDL (mg/dl) | 42.83 ± 11.61 | 44.67 ± 12.01 | 0.0010 |
Significance level was considered at P < 0.0500.
SD: Standard deviation; BMI: Body mass index; WC: Waist circumference; WHR: Waist to hip ratio; WHtR: Waist to height ratio; DBP: Diastolic blood pressure; SBP: Systolic blood pressure; FBS: Fasting blood sugar; TG: Triglyceride; LDL: Low-density lipoprotein; HDL: High-density lipoprotein
Table 2 shows the percentage of study population who had a 10-year risk of CVD ≥ 7.5%, ≥ 5%, ≥ 5%, and ≥10% according to pooled cohort equations of ACC/AHA, SCORE equations for low risk European countries, SCORE equations for high risk European countries, and the Framingham general cardiovascular risk profile in men and women with and without obesity, respectively.
Table 2.
The proportion [confidence interval (95%CI)] of the study population who had a 10-years risk of cardiovascular disease (CVD) ≥ 7.5%, ≥ 5%, ≥ 5%, and ≥ 10% based on related risk assessment tools in individuals with and without obesity defined by different obesity indices
| Obesity indices (BMI) | BMI < 30 in men and women |
BMI ≥ 30 in men and women |
P* |
BMI < 30 in men and women |
BMI ≥ 30 in men and women |
P* |
||
|---|---|---|---|---|---|---|---|---|
| Risk assessment tools | Men (n = 1623) | Women (n = 1287) | ||||||
| A risk of ≥ 7.5% based on pooled cohort equations of ACC/AHA £ | 54.46 (51.76-57.16) | 62.04 (57.44-66.64) | 0.0060 | 28.54 (24.77-32.32) | 24.12 (21.13-27.11) | 0.0710 | ||
| A risk of ≥ 5% based on SCORE equations for low risk European countries £ | 10.28 (8.66-11.90) | 10.47 (7.63-13.31) | 0.9130 | 2.23 (1.03-3.43) | 2.03 (1.08-2.99) | 0.8030 | ||
| A risk of ≥ 5% based on SCORE equations for high risk European countries £ | 24.44 (22.15-26.73) | 25.00 (20.99-29.01) | 0.8140 | 5.49 (3.64-7.34) | 4.91 (3.44-6.38) | 0.6270 | ||
| A risk of ≥ 10% based on the Framingham general cardiovascular risk profile for use in primary care £ | 50.47 (47.76-53.18) | 59.02 (54.35-63.68) | 0.0020 | 21.62 (18.18-25.06) | 21.86 (18.98-24.74) | 0.9180 | ||
| Obesity indices (WC) |
WC < 102 in men |
WC ≥ 102 in men |
P* |
WC < 88 in women |
WC ≥ 88 in women |
P* |
||
| Risk assessment tools | Men (n = 1623) | Women (n = 1287) | ||||||
| A risk of ≥ 7.5% based on pooled cohort equations of ACC/AHA £ | 52.95 (50.27-55.63) | 67.55 (63.00-72.10) | < 0.0010 | 18.32 (13.86-22.78) | 27.90 (25.20-30.60) | 0.0010 | ||
| A risk of ≥ 5% based on SCORE equations for low risk European countries £ | 9.73 (8.17-11.29) | 12.80 (9.61-15.98) | 0.0710 | 1.66 (0.22-3.10) | 2.23 (1.37-3.09) | 0.5370 | ||
| A risk of ≥ 5% based on SCORE equations for high risk European countries £ | 22.75 (20.54-24.96) | 30.80 (26.40-35.20) | 0.0080 | 4.30 (2.01-6.59) | 5.35 (4.03-6.67) | 0.4640 | ||
| A risk of ≥ 10% based on the Framingham general cardiovascular risk profile for use in primary care £ | 48.74 (46.06-51.42) | 65.34 (60.71-69.97) | < 0.0010 | 12.46 (8.65-16.26) | 24.20 (21.62-26.78) | < 0.0010 | ||
| Obesity indices (WHR) |
WHR < 0.9 in men |
WHR ≥ 0.9 in men |
P* |
WHR < 0.85 in women |
WHR ≥ 0.85 in women |
P* |
||
| Risk assessment tools | Men (n = 1623) | Women (n = 1287) | ||||||
| A risk of ≥ 7.5% based on pooled cohort equations of ACC/AHA £ | 42.27 (38.33-46.21) | 63.86 (61.06-66.65) | < 0.0010 | 10.41 (7.49-13.32) | 32.93 (29.90-35.96) | < 0.0010 | ||
| A risk of ≥ 5% based on SCORE equations for low risk European countries £ | 6.70 (4.74-8.66) | 12.43 (10.55-14.31) | 0.0010 | 0.45 (-0.17-1.07) | 2.86 (1.82-3.90) | 0.0340 | ||
| A risk of ≥ 5% based on SCORE equations for high risk European countries £ | 16.11 (13.23-18.99) | 29.16 (26.57-31.75) | < 0.0010 | 1.81 (0.57-3.05) | 6.64 (5.08-8.02) | 0.0010 | ||
| A risk of ≥ 10% based on the Framingham general cardiovascular risk profile for use in primary care £ | 36.80 (32.95-40.65) | 61.04 (58.20-63.87) | < 0.0010 | 6.87 (4.46-9.28) | 28.47 (25.56-31.38) | < 0.0010 | ||
| Obesity indices (WHtR) |
WHtR < 0.5 in men and women |
WHtR ≥ 0.5 in men and women |
P* |
WHtR < 0.5 in men and women |
WHtR ≥ 0.5 in men and women |
P* |
||
| Risk assessment tools | Men (n = 1623) | Women (n = 1287) | ||||||
| A risk of ≥ 7.5% based on pooled cohort equations of ACC/AHA £ | 38.87 (33.56-44.18) | 60.38 (57.83-62.93) | < 0.0010 | 10.45 (3.12-17.77) | 26.64 (24.22-29.06) | 0.0030 | ||
| A risk of ≥ 5% based on SCORE equations for low risk European countries £ | 6.57 (3.91-9.22) | 11.32 (9.70-12.94) | 0.0100 | 0.00 (0.00-0.00) | 2.22 (1.43-3.00) | 0.2080 | ||
| A risk of ≥ 5% based on SCORE equations for high risk European countries £ | 15.22 (11.38-19.07) | 26.78 (24.52-29.04) | < 0.0010 | 0.00 (0.00-0.00) | 5.40 (4.19-6.60) | 0.0460 | ||
| A risk of ≥ 10% based on the Framingham general cardiovascular risk profile for use in primary care £ | 33.31 (28.18-38.44) | 57.05 (54.47-59.63) | < 0.0010 | 7.46 (1.17-13.75) | 22.43 (20.14-24.72) | 0.0040 | ||
The proportion (percentage) of individuals with a 10-year risk of CVD of ≥ 0.075 for pooled cohort equations, ≥ 0.05 for SCORE equations (both low and high risk countries versions), and ≥ 0.1 for the Framingham general cardiovascular risk profile for use in primary care
Significance level was considered at P < 0.0500.
BMI: Body mass index; ACC/AHA: American College of Cardiology/American Heart Association; SCORE: Systematic Coronary Risk Evaluation; WC: Waist circumference; WHR: Waist to hip ratio; WHtR: Waist to height ratio; CVD: Cardiovascular disease
The categorization of individuals to with obesity and without obesity according to BMI showed that a higher proportion of women without obesity had a 10-year risk of CVD ≥ 7.5% compared to women with obesity based on the ACC/AHA equations (28.54% vs. 24.15%), although the difference was not statistically significant (P = 0.0707).
Table 3 shows the results of the univariate logistic regression analysis in which obesity indices were separately considered as predictors and 10-year risk of CVD ≥ 7.5%, ≥ 5%, and ≥ 10% were considered outcomes based on pooled cohort equations, SCORE equations, and the Framingham tool, respectively. According to these results, WHR and WHtR had a significant relationship with estimated 10-year risk of CVD in all risk assessment tools. Furthermore, WHR showed the strongest relationships with 10-year risk of CVD compared to other obesity indices, particularly in women. In multiple logistic regression analysis with the elimination of the effects of other risk factors, which were applied to calculate 10-year risk of CVD, none of the obesity indices showed a significant association with the related 10-year risk of CVD.
Table 3.
Univariate logistic regression results
| Obesity indices | Men (n = 1623) |
Women (n = 1287) |
||||
|---|---|---|---|---|---|---|
| Wald |
OR (95%CI) |
P* |
Wald |
OR (95%CI) |
P* |
|
| Outcomes of risk assessment tools | ||||||
| A 10-year CVD risk ≥ 0.075 of pooled cohort equations for ACC/AHA tool£ | ||||||
| BMI ≥ 30 kg/m2 both in men and women | 6.50 | 1.34 (1.07-1.69) | 0.0110 | 2.250 | 0.83 (0.64-1.06) | 0.1340 |
| WC ≥ 102 cm in men and ≥ 88 cm in women | 26.92 | 1.89 (1.48-2.40) | < 0.0010 | 10.420 | 1.73 (1.24-2.24) | 0.0010 |
| WHR ≥ 0.9 in men and ≥ 0.85 in women | 81.65 | 2.56 (2.08-3.13) | < 0.0010 | 63.600 | 4.12 (2.91-5-83) | < 0.0010 |
| WHtR ≥ 0.50 both in men and women | 51.47 | 2.47 (1.95-3.16) | < 0.0010 | 10.570 | 5.42 (1.96-15.00) | 0.0110 |
| A 10-year CVD risk ≥ 0.050 of SCORE equations for low risk European countries£ | ||||||
| BMI ≥ 30 kg/m2 both in men and women | 0.01 | 1.02 (0.72-1.45) | 0.9130 | 0.060 | 0.91 (0.44-1.89) | 0.8030 |
| WC ≥ 102cm in men and ≥ 88cm in women | 3.24 | 1.36 (0.97-1.91) | 0.0720 | 0.380 | 1.36 (0.51-3.57) | 0.5390 |
| WHR ≥ 0.9 in men and ≥ 0.85 in women | 13.94 | 1.98 (1.38-2.83) | 0.0020 | 6.490 | 6.49 (1.54-27.37) | 0.0110 |
| WHtR ≥ 0.50 both in men and women | 6.43 | 1.82 (1.14-2.80) | 0.0110 | - $ | - $ | - $ |
| A 10-year CVD risk ≥ 0.050 of SCORE equations for high risk European countries£ | ||||||
| BMI ≥ 30 kg/m2 both in men and women | 0.06 | 1.03 (0.81-1.32) | 0.8140 | 0.235 | 0.89 (0.55-1.43) | 0.6280 |
| WC ≥ 102 cm in men and ≥ 88 cm in women | 11.17 | 1.51 (1.19-1.92) | 0.0080 | 0.534 | 1.26 (0.68-2.32) | 0.4650 |
| WHR ≥ 0.9 in men and ≥ 0.85 in women | 36.60 | 2.14 (1.68-2.75) | < 0.0010 | 12.722 | 3.87 (1.84-8.13) | 0.0040 |
| WHtR ≥ 0.50 both in men and women | 19.03 | 2.04 (1.48-2.80) | < 0.0010 | - $ | - $ | - $ |
| A 10-year CVD risk ≥ 0.100 of Framingham general cardiovascular risk profile for use in primary care£ | ||||||
| BMI ≥ 30 kg/m2 both in men and women | 9.33 | 1.41 (1.13-1.76) | 0.0020 | 0.010 | 1.01 (0.78-1.32) | 0.9180 |
| WC ≥ 102 cm in men and ≥ 88 cm in women | 33.79 | 1.98 (1.57-2.50) | < 0.0010 | 17.750 | 2.25 (1.54-3.27) | < 0.0010 |
| WHR ≥ 0.9 in men and ≥ 0.85 in women | 90.41 | 2.69 (2.19-3.30) | < 0.0010 | 67.160 | 5.40 (3.61-8.08) | < 0.0010 |
| WHtR ≥ 0.50 both in men and women | 57.01 | 2.66 (2.06-3.43) | < 0.0010 | 7.400 | 3.59 (1.43-9.01) | < 0.0010 |
Significance level was considered at P < 0.0500.
outcomes are a 10-year risk of CVD ≥ 0.075 for pooled cohort equations, ≥ 0.05 for SCORE equations (both low and high risk countries versions), and ≥ 0.1 for the Framingham general cardiovascular risk profile for use in primary care.
$ No women with WHtR < 0.5 had a 10-year risk of CVD ≥ 0.05 based on SCORE equations (based on both high and low risk European countries).
OR: Odd ratio; CI: Confidence interval; CVD: Cardiovascular disease; ACC/AHA: American College of Cardiology/American Heart Association; BMI: Body mass index; WC: Waist circumference; WHR: Waist to hip ratio; WHtR: Waist to height ratio; SCORE: Systematic Coronary Risk Evaluation
The present study results showed that BMI had a non-significant AUC (< 0.5) based on pooled cohort equations of ACC/AHA tool [0.4742 (0.4391-0.5093)] and SCORE equations for high-risk European countries [0.4717 (0.4022-0.5412)] in women.
Discussion
The present study was conducted to determine whether the obesity paradox will be detectable when 10-year risk of CVD and obesity are determined by related risk assessment tools and obesity indices, respectively.
The results showed a weak and non-significant obesity paradox in women whose obesity and 10-year risk of CVD were determined based on BMI and ACC/AHA equation, respectively. A lower proportion (but non-significant) of women with obesity, based on a BMI ≥ 30, had a10-year risk of CVD ≥ 7.5% compared to women without obesity when the ACC/AHA equation was applied. BMI had the lowest discriminatory ability among the mentioned obesity indices. The discriminatory ability of BMI was even less than 0.5 in women whose 10-year risk of CVD was estimated based on pooled cohort equations of ACC/AHA and SCORE equations for high risk European countries.
McAuley et al. showed that obesity (BMI ≥ 30) was related to a lower mortality risk in a clinical population of individuals without heart failure, which was in agreement with the obesity paradox.7 While a high WHR is primarily associated with increased central fat stores (notably with visceral fat), decreased thigh muscle mass, and reduced physical fitness, a high BMI is associated with increased thigh muscle mass and peripheral fat stores without association with visceral fat.14 A growing body of evidence still supports purposeful weight reduction in the control and treatment of CVDs.15 Moreover, it has been suggested that the obesity paradox is largely confounded by fitness.
Consequently, individuals who are more fit usually have a better prognosis than others, and no clear obesity paradox is apparent in these individuals.7
Some theories attempted to explain the protective effect of obesity by altered cytokines, plasma rennin, epinephrine, and larger coronary arteries.16 Some other studies proposed smoking as a confounding variable in the obesity paradox; smokers usually lose weight and they also have a higher risk of CVD.16-18 However, in the present study, the obesity paradox was weakly confirmed only in women and only 0.84% of them were currently smoking, suggesting that smoking might not play a critical role in this context.
Although no obesity indices showed a relationship with 10-year risk of CVD in a multivariate model, WHR had the strongest association with 10-year risk of CVD in a univariate binary regression model. Previous studies showed that WC and HC have an independent relationship with MI. Consequently, it is reasonable that a combined measure of these two indices (such as WHR) has a strong association with CVD events, as the present study results suggested. An inverse association was observed between HC and risk of DM, hypertension (HTN), dyslipidemia, and CVD.19-22 Furthermore, DM, HTN, and lipid profiles are the variables commonly utilized to estimate the 10-year risk of CVD. From a different perspective, estrogens have an important role in the accumulation of subcutaneous gluteal and femoral fat, and a higher WHR indicates decreased muscle mass in the legs and gluteal region.21 Furthermore, the protective effect of estrogen on the cardiovascular system was emphasized in a previous study.23 Thus, it is reasonable to assume that a higher WHR, which is usually associated with a lower estrogen level, can lead to a higher CVD risk.
This study had some limitations. Although we utilized 4 popular risk assessment tools, none of these risk assessment tools were developed for our country. However, similar results particularly in the context of the association between obesity indices and CVD risk may approve the validity of our findings. In addition, a weak inverse relationship between BMI and estimated CVD risk is not equal to the inverse association between BMI and CVD events. However, this can signify that there is at least a non-strong, negative relationship between BMI as a general index of obesity and a cluster of CVD risk factors that may lead to CVD events in the next decade.
Conclusion
BMI showed a weak and non-significant inverse association with 10-year risk of CVD estimated by pooled cohort equations of ACC/AHA in women. However, this result cannot directly provide enough evidence for the obesity paradox.
Acknowledgments
This study was financially supported by Gastrointestinal and Liver Diseases Research Center (GILDRC), Tehran Firoozgar Hospital, Iran University of Medical Sciences, Tehran, Iran.
Footnotes
Conflicts of Interests
Authors have no conflict of interests.
REFERENCES
- 1.Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384(9945):766–81. doi: 10.1016/S0140-6736(14)60460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA. 2012;307(5):491–7. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 3.Eckel RH, Krauss RM. American Heart Association call to action: Obesity as a major risk factor for coronary heart disease. AHA Nutrition Committee. Circulation. 1998;97(21):2099–100. doi: 10.1161/01.cir.97.21.2099. [DOI] [PubMed] [Google Scholar]
- 4.Finucane MM, Stevens GA, Cowan MJ, Danaei G, Lin JK, Paciorek CJ, et al. National, regional, and global trends in body-mass index since 1980: Systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377(9765):557–67. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: A systematic review and meta-analysis. JAMA. 2013;309(1):71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lavie CJ, McAuley PA, Church TS, Milani RV, Blair SN. Obesity and cardiovascular diseases: implications regarding fitness, fatness, and severity in the obesity paradox. J Am Coll Cardiol. 2014;63(14):1345–54. doi: 10.1016/j.jacc.2014.01.022. [DOI] [PubMed] [Google Scholar]
- 7.McAuley P, Myers J, Abella J, Froelicher V. Body mass, fitness and survival in veteran patients: another obesity paradox? Am J Med. 2007;120(6):518–24. doi: 10.1016/j.amjmed.2006.07.032. [DOI] [PubMed] [Google Scholar]
- 8.D'Agostino RB, Vasan RS, Pencina MJ, Wolf PA, Cobain M, Massaro JM, et al. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation. 2008;117(6):743–53. doi: 10.1161/CIRCULATIONAHA.107.699579. [DOI] [PubMed] [Google Scholar]
- 9.Goff DC, Lloyd-Jones DM, Bennett G, Coady S, D'Agostino RB, Gibbons R, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2935–59. doi: 10.1016/j.jacc.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Conroy RM, Pyorala K, Fitzgerald AP, Sans S, Menotti A, De Backer G, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur Heart J. 2003;24(11):987–1003. doi: 10.1016/s0195-668x(03)00114-3. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. Waist circumference and waist-hip ratio: Report of a WHO expert consultation. Geneva, Switzerland: WHO; 2011. [Google Scholar]
- 12.Hsieh SD, Yoshinaga H. Waist/height ratio as a simple and useful predictor of coronary heart disease risk factors in women. Intern Med. 1995;34(12):1147–52. doi: 10.2169/internalmedicine.34.1147. [DOI] [PubMed] [Google Scholar]
- 13.Ware LJ, Rennie KL, Kruger HS, Kruger IM, Greeff M, Fourie CM, et al. Evaluation of waist-to-height ratio to predict 5 year cardiometabolic risk in sub-Saharan African adults. Nutr Metab Cardiovasc Dis. 2014;24(8):900–7. doi: 10.1016/j.numecd.2014.02.005. [DOI] [PubMed] [Google Scholar]
- 14.Seidell JC, Bjorntorp P, Sjostrom L, Sannerstedt R, Krotkiewski M, Kvist H. Regional distribution of muscle and fat mass in men-new insight into the risk of abdominal obesity using computed tomography. Int J Obes. 1989;13(3):289–303. [PubMed] [Google Scholar]
- 15.Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: Risk factor, paradox, and impact of weight loss. J Am Coll Cardiol. 2009;53(21):1925–32. doi: 10.1016/j.jacc.2008.12.068. [DOI] [PubMed] [Google Scholar]
- 16.Gruberg L, Mercado N, Milo S, Boersma E, Disco C, van Es, et al. Impact of body mass index on the outcome of patients with multivessel disease randomized to either coronary artery bypass grafting or stenting in the ARTS trial: The obesity paradox II? Am J Cardiol. 2005;95(4):439–44. doi: 10.1016/j.amjcard.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 17.Hoffmans MD, Kromhout D, de Lezenne Coulander C. The impact of body mass index of 78,612 18-year old Dutch men on 32-year mortality from all causes. J Clin Epidemiol. 1988;41(8):749–56. doi: 10.1016/0895-4356(88)90161-8. [DOI] [PubMed] [Google Scholar]
- 18.Manson JE, Willett WC, Stampfer MJ, Colditz GA, Hunter DJ, Hankinson SE, et al. Body weight and mortality among women. N Engl J Med. 1995;333(11):677–85. doi: 10.1056/NEJM199509143331101. [DOI] [PubMed] [Google Scholar]
- 19.Lissner L, Bjorkelund C, Heitmann BL, Seidell JC, Bengtsson C. Larger hip circumference independently predicts health and longevity in a Swedish female cohort. Obes Res. 2001;9(10):644–6. doi: 10.1038/oby.2001.85. [DOI] [PubMed] [Google Scholar]
- 20.Okura T, Nakata Y, Yamabuki K, Tanaka K. Regional body composition changes exhibit opposing effects on coronary heart disease risk factors. Arterioscler Thromb Vasc Biol. 2004;24(5):923–9. doi: 10.1161/01.ATV.0000125702.26272.f6. [DOI] [PubMed] [Google Scholar]
- 21.Seidell JC, Han TS, Feskens EJ, Lean ME. Narrow hips and broad waist circumferences independently contribute to increased risk of non-insulin-dependent diabetes mellitus. J Intern Med. 1997;242(5):401–6. doi: 10.1046/j.1365-2796.1997.00235.x. [DOI] [PubMed] [Google Scholar]
- 22.Snijder MB, Zimmet PZ, Visser M, Dekker JM, Seidell JC, Shaw JE. Independent and opposite associations of waist and hip circumferences with diabetes, hypertension and dyslipidemia: The AusDiab Study. Int J Obes Relat Metab Disord. 2004;28(3):402–9. doi: 10.1038/sj.ijo.0802567. [DOI] [PubMed] [Google Scholar]
- 23.Mendelsohn ME. Protective effects of estrogen on the cardiovascular system. Am J Cardiol. 2002;89(12A):12E–7E. doi: 10.1016/s0002-9149(02)02405-0. [DOI] [PubMed] [Google Scholar]