Abstract
Psoriasis is a chronic, immune mediated, systemic inflammatory skin disease with a reported prevalence of 0.6%–4.8% in the general population. Bipolar disorder (BP) is a severe episodic psychiatric disorder that ranks as the fourth leading cause of disability. Recent evidence suggests that genetic and immunological factors play a significant role in the development of both disorders. Studies have also shown a higher association of psychiatric disorders among patients with psoriasis. Moreover, several autoimmune comorbidities have been reported in association with BP. Here, we describe a young woman with BP who developed psoriasis after 1 year of developing BP and showed exacerbations in psoriasis lesions with each manic episode. We also highlight the safe and efficacious use of apremilast for psoriatic lesions in the woman.
Keywords: bipolar and related disorders
Introduction
Psoriasis is a chronic, immune-mediated, systemic inflammatory skin disease with a reported prevalence of 0.6%–4.8% in the general population.1 Recent evidence suggests that genetic and immunological factors play a significant role in its development.2 Studies have shown that patients with psoriasis are more prone to psychiatric illness than patients with other skin diseases.2
Bipolar disorder (BP) is a severe episodic psychiatric disorder that ranks as the fourth leading cause of disability.3 Several autoimmune comorbidities have been reported in association with BP, including Crohn disease, Guillain-Barré syndrome, autoimmune thyroiditis, autoimmune hepatitis, multiple sclerosis, rheumatoid arthritis and systemic lupus erythematosus.4 However, the association between BP and psoriasis is not frequently reported. Here, we describe a young woman with BP who developed psoriasis after 1 year of developing BP and showed exacerbations in psoriasis lesions with each manic episode. We also highlight the safe and efficacious use of apremilast for psoriatic lesions in the woman.
Case history
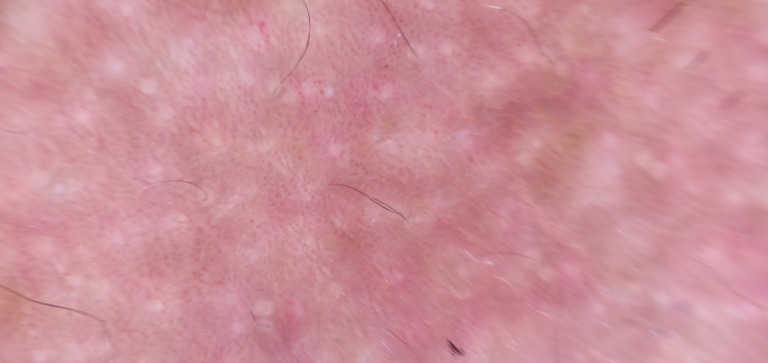
A 30-year-old married woman came with her father with complaints of talkativeness, irritability, hyperactivity, decreased sleep, increased religiosity and tall claims for the last 2 weeks. She had four similar episodes in the past 5 years. Treatment details were not available. She also developed psoriasis for the past 4 years. She reported exacerbation of psoriasis lesions with each psychiatric episode. There was no history of a depressive episode, drug abuse or suicidal behaviour. She had extensive psoriasis lesions at the time of presentation mainly in face, trunk and exposed extremities (figure 1). There was no history of significant medical or psychiatric illness before developing BP. A mental status examination revealed overprotective speech, euphoric affect, grandiosity and poor insight. She was diagnosed with bipolar affective disorder, current episode mania with psychotic symptoms according to ICD 10 (International Classification of Diseases 10th Revision), and oral sodium valproate 700 mg/day and oral olanzapine 5 mg/day were started. A dermatological consultation was taken for psoriasis. The diagnosis of psoriasis was confirmed by clinical and dermoscopic findings. The cutaneous lesions in the patient was found to be well-defined erythematous plaques with silvery scales. Regular red dots were noted on dermoscopy confirming a diagnosis of psoriasis (figure 2). Laboratory parameters including total WBC (White Blood Cells) count, eosinophil and CRP (C-reactive protein) were within normal limits. She was started on oral apremilast 30 mg/day along with topical medications. During initial follow-up after 2 weeks, she reported significant improvement in manic and dermatological symptoms. Written informed consent was obtained from the patient for the publication of this report.
Figure 1.

Cutaneous lesions in the patient: well-defined erythematous plaques with silvery scales.
Figure 2.
Regular red dots were noted on dermoscopy confirming a diagnosis of psoriasis.
Discussion
Our case illustrates the occurrence of psoriasis in a young female patient with BP. She had no family history of BP or psoriasis. There was also an interesting association between bipolar cyclicity and exacerbation of psoriatic lesions and remission episodes. Our patient reported having manic episodes consecutively for the last 5 years, and with each episode there was worsening of psoriatic lesions even before starting psychotropic medications and a reduction in lesions during remission. Another past report showed an exacerbation in psoriatic lesions during depressive episodes and a dramatic decrease during a hypomanic episode and in remission.5
The association of psoriasis with various psychiatric disorders has been explored extensively. Psoriasis has been reported to be associated with an elevated risk of various mental disorders, including depression, anxiety and suicidal behaviour.6 However, its association with BP is not very well covered in the published literature. A study exploring the association of psoriasis with mental health disorders in South Korea found that the risk of depressive episodes, anxiety disorders, somatoform disorders, neurotic disorders and non-organic sleep disorders was 2.19 (1.97–2.44), 2.92 (2.67–3.20), 2.62 (2.24–3.08), 2.66 (2.29–3.09) and 2.58 (2.27–2.93) times higher in patients with psoriasis than in control patients, respectively.7 However, another study exploring psoriasis and the risk of mental disorders in Denmark found a heightened risk of BP among individuals with psoriasis (HR: 2.33 (95% CI: 1.59 to 3.41).8 A primary care cohort study from the UK exploring psychiatric morbidities in psoriasis also found higher prevalence for histories of alcohol misuse, BP, depression, anxiety disorder and self-harm in patients with psoriasis.9
The pathophysiology of the association between BP and psoriasis is not yet clear. Psoriasis has a strong association with psychological stressors. There are plenty of published observational studies suggesting a link between preceding psychological stress and psoriasis onset and exacerbation.10 Patients with BP often experience persistent residual symptoms, difficulties in psychosocial functioning and poor quality of life, which in turn leads to significant psychological stress.11 One of the potential causes for the precipitation of psoriasis in our case after 1 year of onset of BP could be the psychological stress associated with bipolar illness. Moreover, both these conditions also have various shared lifestyle risk factors. Another possible aetiological link between BP and psoriasis seems to be genetic and shared pathophysiological processes. A past study found a correlation between immunological changes (high CD4/CD8 ratio) and chromosomal aberrations (aneuploidy of chromosome 8) in a family with BP and psoriasis.12 Furthermore, recent candidate gene studies of psoriasis also found that SNPs (single nucleotide polymorphisms) at three loci, 1q24, 6p22 and 21q22, were significantly associated with psoriasis. 21q22 is one important chromosomal region identified as possibly harbouring a locus for susceptibility to BP as well.13 There is accumulating evidence recently that activation of the immune system plays an important role in the pathogenesis of BP. Studies have described a higher expression of a coherent set of 34 inflammatory genes, an inflammatory gene expression ‘signature’, in the circulating monocytes of 60%–70% of patients with BP.14 Moreover, a recent study also showed significantly higher levels of sCD25 and higher percentages of circulating CD4+CD25highFoxP3+regulatory T cells in patients with BP, which regulates the inflammation-inducing effects of Th1 cells, Th17 cells, monocytes and macrophages. Th17 cells are a newly discovered T helper subset that produce the proinflammatory cytokine IL-17 (Interleukin 17) and play a significant role in the pathogenesis of psoriasis.15 However, most of these mechanisms are hypothetical in our case as we have not performed any immunological studies in our patient, which is a major limitation of our report.
Another potential aetiological factor precipitating psoriasis in our case could be medications. We could not get the details of the medications she was on when psoriasis developed. Lithium has been found to be associated with inducing and exacerbating psoriasis.16 There are also few reports of sodium valproate–induced psoriasis.17 Among antipsychotics, olanzapine, quetiapine and aripiprazole have been shown to induce psoriasis.18 However, drug-induced psoriasis resolves after discontinuing the causative drug most of the time. Our case had repeated exacerbations associated with a manic episode even when she was off medication.
We would also like to highlight the safety and efficacy of apremilast, an oral phosphodiesterase-4 inhibitor, in psoriasis with BP. An altered PDE-4 expression and cyclic AMP (cAMP) activation is a common pathogenic step in psoriasis and BP.19 This assumes importance as our patient had shown an increase in the severity of her cutaneous lesions along with a manic episode, signifying the role of PDE-4 (phosphodiesterase 4) inhibition which may block the common pathogenic pathway, the cAMP (adenosine monophosphate) activation. Our patient had a marked response to apremilast in her skin lesions. Even though the product monograph warns about a possibility of depression with apremilast, a long-term safety analysis did not show an increase in its incidence.20 The lack of any mood swings in our patient while on apremilast also supports the safe use of apremilast in patients with BP.
In conclusion, our case highlights the comorbidity of BP with psoriasis. Such co-occurrences of heritable disorders help us to deepen our understanding of the neurobiology of both disorders, especially the role of genes and inflammatory markers associated with BP in the pathophysiology of psoriasis. The successful and safe use of apremilast that blocks the common pathogenic pathway—the altered PDE-4 expression and cAMP activation—also translates the basic aetiopathogenic knowledge into clinical practice.
Biography
Dr. N. A. Uvais is a consultant in psychiatry at Iqraa International Hospital and Research Centre, Calicut, India. He completed MBBS from Calicut medical college, Calicut in 2007. He completed his post-graduate training (DPM) in psychiatry at Central Institute of psychiatry (CIP), Ranchi, India in 2011. He is currently working as a consultant psychiatrist in Iqraa International Hospital and Research Centre, Calicut since 2012. His research interests include liaison psychiatry, community psychiatry, obsessive compulsive disorder, and spirituality and mental health.

Footnotes
Contributors: All authors participated in planning, designing, conducting literature search, writing and editing the manuscript. They equally participated in reporting of the work done in the manuscript. Corresponding author, NAU, will be responsible for the overall content of the manuscript and will act in the capacity of the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kim GK, Del Rosso JQ. Drug-provoked psoriasis: is it drug induced or drug aggravated?: understanding pathophysiology and clinical relevance. J Clin Aesthet Dermatol 2010;3:32–8. [PMC free article] [PubMed] [Google Scholar]
- 2.Ferreira BIRC, Abreu JLPDC, Reis JPGD, et al. Psoriasis and associated psychiatric disorders: a systematic review on etiopathogenesis and clinical correlation. J Clin Aesthet Dermatol 2016;9:36–43. [PMC free article] [PubMed] [Google Scholar]
- 3.Kupfer DJ. The increasing medical burden in bipolar disorder. JAMA 2005;293:2528–30. 10.1001/jama.293.20.2528 [DOI] [PubMed] [Google Scholar]
- 4.Kridin K, Zelber-Sagi S, Comaneshter D, et al. Bipolar disorder associated with another autoimmune Disease-Pemphigus: a population-based study. Can J Psychiatry 2018;63:474–80. 10.1177/0706743717740344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Demirdaş A, Yaman AR, Aslan IH, et al. Bipolar cyclicity and psoriasis: a case presentation. CausaPedia 2017;6:115–20. [Google Scholar]
- 6.Kurd SK, Troxel AB, Crits-Christoph P, et al. The risk of depression, anxiety, and suicidality in patients with psoriasis: a population-based cohort study. Arch Dermatol 2010;146:891–5. 10.1001/archdermatol.2010.186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bang CH, Yoon JW, Chun JH, et al. Association of psoriasis with mental health disorders in South Korea. JAMA Dermatol 2019;155:747–9. 10.1001/jamadermatol.2019.0315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leisner MZ, Riis JL, Schwartz S, et al. Psoriasis and risk of mental disorders in Denmark. JAMA Dermatol 2019;155:745–7. 10.1001/jamadermatol.2019.0039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parisi R, Webb RT, Kleyn CE, et al. Psychiatric morbidity and suicidal behaviour in psoriasis: a primary care cohort study. Br J Dermatol 2019;180:108–15. 10.1111/bjd.17004 [DOI] [PubMed] [Google Scholar]
- 10.Snast I, Reiter O, Atzmony L, et al. Psychological stress and psoriasis: a systematic review and meta-analysis. Br J Dermatol 2018;178:1044–55. 10.1111/bjd.16116 [DOI] [PubMed] [Google Scholar]
- 11.Bonnín CDM, Reinares M, Martínez-Arán A, et al. Improving functioning, quality of life, and well-being in patients with bipolar disorder. Int J Neuropsychopharmacol 2019;22:467–77. 10.1093/ijnp/pyz018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Demirhan O, Demirbek B, Tunç E, et al. Identification of chromosome abnormalities in screening of a family with manic depression and psoriasis: predisposition to aneuploidy. Asian J Psychiatr 2012;5:169–74. 10.1016/j.ajp.2012.02.005 [DOI] [PubMed] [Google Scholar]
- 13.Smith RL, Warren RB, Griffiths CE, et al. Genetic susceptibility to psoriasis: an emerging picture. Genome Med 2009;1:72. 10.1186/gm72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aita VM, Liu J, Knowles JA, et al. A comprehensive linkage analysis of chromosome 21q22 supports prior evidence for a putative bipolar affective disorder locus. Am J Hum Genet 1999;64:210–7. 10.1086/302185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Drexhage RC, Hoogenboezem TH, Versnel MA, et al. The activation of monocyte and T cell networks in patients with bipolar disorder. Brain Behav Immun 2011;25:1206–13. 10.1016/j.bbi.2011.03.013 [DOI] [PubMed] [Google Scholar]
- 16.Jafferany M. Lithium and psoriasis: what primary care and family physicians should know. Prim Care Companion J Clin Psychiatry 2008;10:435–9. 10.4088/pcc.v10n0602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gul Mert G, Incecik F, Gunasti S, et al. Psoriasiform drug eruption associated with sodium valproate. Case Rep Pediatr 2013;2013:1–3. 10.1155/2013/823469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bujor C-E, Vang T, Nielsen J, et al. Antipsychotic-associated psoriatic rash - a case report. BMC Psychiatry 2017;17:242. 10.1186/s12888-017-1411-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McDonald ML, MacMullen C, Liu DJ, et al. Genetic association of cyclic AMP signaling genes with bipolar disorder. Transl Psychiatry 2012;2:e169. 10.1038/tp.2012.92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Crowley J, Thaçi D, Joly P, et al. Long-term safety and tolerability of apremilast in patients with psoriasis: Pooled safety analysis for ≥156 weeks from 2 phase 3, randomized, controlled trials (ESTEEM 1 and 2). J Am Acad Dermatol 2017;77:310–7. 10.1016/j.jaad.2017.01.052 [DOI] [PubMed] [Google Scholar]