Abstract
Objective
To use data from the Global Burden of Disease Study between 1990 and 2017 to report the rates and trends of point prevalence, annual incidence, and years lived with disability for neck pain in the general population of 195 countries.
Design
Systematic analysis.
Data source
Global Burden of Diseases, Injuries, and Risk Factors Study 2017.
Main outcome measures
Numbers and age standardised rates per 100 000 population of neck pain point prevalence, annual incidence, and years lived with disability were compared across regions and countries by age, sex, and sociodemographic index. Estimates were reported with uncertainty intervals.
Results
Globally in 2017 the age standardised rates for point prevalence of neck pain per 100 000 population was 3551.1 (95% uncertainty interval 3139.5 to 3977.9), for incidence of neck pain per 100 000 population was 806.6 (713.7 to 912.5), and for years lived with disability from neck pain per 100 000 population was 352.0 (245.6 to 493.3). These estimates did not change significantly between 1990 and 2017. The global point prevalence of neck pain in 2017 was higher in females compared with males, although this was not significant at the 0.05 level. Prevalence increased with age up to 70-74 years and then decreased. Norway (6151.2 (95% uncertainty interval 5382.3 to 6959.8)), Finland (5750.3 (5058.4 to 6518.3)), and Denmark (5316 (4674 to 6030.1)) had the three highest age standardised point prevalence estimates in 2017. The largest increases in age standardised point prevalence estimates from 1990 to 2017 were in the United Kingdom (14.6% (10.6% to 18.8%)), Sweden (10.4% (6.0% to 15.4%)), and Kuwait (2.6% (2.0% to 3.2%)). In general, positive associations, but with fluctuations, were found between age standardised years lived with disability for neck pain and sociodemographic index at the global level and for all Global Burden of Disease regions, suggesting the burden is higher at higher sociodemographic indices.
Conclusions
Neck pain is a serious public health problem in the general population, with the highest burden in Norway, Finland, and Denmark. Increasing population awareness about risk factors and preventive strategies for neck pain is warranted to reduce the future burden of this condition.
Introduction
Neck pain is a highly prevalent condition that leads to considerable pain, disability, and economic cost.1 It not only constitutes a major personal burden but also affects families and the health system and economic structure of countries.2 3 Despite the impact of neck pain, its global burden has not been comprehensively presented, in a way that can serve as the basis for different types of epidemiological studies and for evaluating diverse healthcare systems worldwide. For example, only one study has reported the specific burden of neck pain at global and regional level, using data from the Global Burden of Disease Study 2010.4 More recently, a few studies have reported the combined burden of musculoskeletal conditions at global or regional level but have not provided specific data on neck pain.5 6 Moreover, national estimates on the burden from neck pain have not been reported for all countries despite systematic reviews having reported prevalence for a few specific countries.7 8 A comprehensive analysis can also guide healthcare providers and policymakers in identifying successful strategies used in regions where the burden has been shown to decrease over time; and apply them in regions with a higher burden. We report the global, regional, and national level prevalence, incidence, and years lived with disability from neck pain in the general population in terms of numbers and age standardised rates for 195 countries from 1990 to 2017 by age, sex, and sociodemographic index (a composite of sociodemographic factors).
Methods
Overview
Global Burden of Disease Study is a resource that measures epidemiological levels and trends comprehensively and comparably across the world. In the Global Burden of Diseases, Injuries, and Risk Factors Study 2017, about 354 diseases and injuries, 282 causes of death, and 84 risk factors were systematically studied for 195 countries, 7 super regions, and 21 regions during 1990-2017.9 The 7 super regions are high income (Asia Pacific and North America); Latin America and the Caribbean; sub-Saharan Africa; North Africa and the Middle East; South East Asia, east Asia, and Oceania; south Asia; and central Europe, eastern Europe, and central Asia. The general methodology of Global Burden of Disease 2017 is presented elsewhere.9 10 11 12 See https://vizhub.healthdata.org/gbd-compare/ and http://ghdx.healthdata.org/gbd-results-tool for detailed information on publicly available non-fatal estimates of Global Burden of Disease 2017.
The Global Burden of Disease Study adheres to the guidelines for accurate and transparent health estimates reporting (GATHER) statement.13 As the Institute for Health Metrics and Evaluation (IHME), the institute responsible for administering the Global Burden of Disease, uses deidentified and aggregated data only, informed consent is not applicable to the Global Burden of Disease Study.
Case definition and data sources
In the current study, Global Burden of Disease Study defined neck pain as pain in the cervical spine region (with or without pain referred to the arms) that lasts for at least 24 hours. The anatomical region of the neck was defined based on the recommendation by the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and its Associated Disorders.14 Global Burden of Disease Study considered pain in the neck or shoulder as a proxy for neck pain.9
Ovid Medline, Embase, CINAHL, CAB abstracts, WHOLIS, and SIGLE databases were searched for the Global Burden of Disease Study 2010, and additionally PubMed was searched to end of October 2017 for the Global Burden of Disease 2017. IHME performed the searches. No age, sex, or language restrictions were applied. The terms “neck pain”, “neck ache”, “neckache”, and “cervical pain” were searched individually and combined with each of the following terms: “prevalen*”, “inciden*”, “cross-sectional”, “cross sectional”, “epidemiol*”, “survey”, “population-based”, “population based”, “population study”, and “population sample”.9 IHME used the following as exclusion criteria: subpopulations clearly not representative of the national population, not a population based study, low sample size (<150), and review rather than original studies.9
Moreover, for the current analyses a second systematic review was performed by IHME, searching for published studies on neck pain from 2016 to 2017. In this additional search, a total of 211 studies were identified and 30 studies retrieved after screening of the title and abstract. After a full text review, four studies were included in the current analyses.9 Additional information was derived from unit record data of surveys in the Global Burden of Disease’s repository of population health data, including the National Health and Nutrition Examination Survey (NHANES) and National Health Interview Survey (NHIS) in the USA.9 In addition, Global Burden of Disease Study included data from US claims data for 2000 and 2010-14 by state, as well as Taiwan claims data for 2016.9 Global Burden of Disease Study then estimated the prevalence of neck pain based on 388 site years, where a site year was defined as a country or other subnational geographical unit contributing data in a given year. Only 23 out of 195 countries representing 11 out of 21 Global Burden of Disease regions provided data for estimating the prevalence of neck pain.9 The Global Burden of Disease 2017 data input sources tool (http://ghdx.healthdata.org/gbd-2017/data-input-sources) shows the data sources used for estimating the burden of neck pain in different countries.
Data processing and disease model
Global Burden of Disease Study used a bayesian metaregression tool, DisMod-MR, to pool heterogeneous data (eg, age groups). The tool, used by IHME, produces a full set of age, sex, region, and year specific estimates.15 Our disease model using DisMod-MR included setting excess mortality to 0, and assumed no incident or prevalent neck pain before age 5 years. Study covariates were used for studies that reported broader anatomical region, episode duration greater than three months, recall periods of one week to one month, recall periods between two months and one year, activity limiting neck pain, and studies conducted among schoolchildren.9
With the exception of broad anatomical region, activity limiting neck pain, and studies among schoolchildren populations, in which coefficients were consistent with their reasonable ranges, Global Burden of Disease Study calculated means and the upper and lower uncertainty interval bounds for all other covariates by crosswalking (ie, data comparing and merging) with NHANES data as baseline. The prior values for those coefficients are reported elsewhere.9
Severity and years lived with disability
Supplementary table S1 shows the lay descriptions and disability weights for neck pain severity levels, where disability weight is defined as a weight factor that reflects the severity of the disease or condition on a scale from 0 (perfect health) to 1 (equivalent to death).
The severity distributions are derived from the Medical Expenditure Panel Surveys (MEPS) analysis conducted in the USA (http://www.meps.ahrq.gov/survey_comp/hc_data_collection.jsp). MEPS is a panel survey of the American community dwelling population used to collect information on the use and cost of healthcare. A panel lasts for two years, is conducted in five rounds, and typically contains 30 000 to 35 000 respondents.9
MEPS data from 2000 to 2014 were used for the Global Burden of Disease Study 2016, and respondents self-administered the SF-12 twice for each panel, at rounds 2 and 4, typically about a year apart. Only adults aged 18 years and older complete the SF-12. MEPS also collects information on diagnoses based on self-report of reasons for healthcare encounters. Although diagnoses can also be derived from additional questions on “problems that bother you” or conditions that led to “disability days,” information on neck pain was mostly derived from data on healthcare encounters.9 Professional coders translate the verbatim text into three digit ICD (international classification of diseases, ninth and 10th revisions) codes. The codes for neck pain are 723.1 (ICD-9) and M54.2 (ICD-10).
To derive SF-12 values comparable with those used by the Global Burden of Disease disability weights, small studies on convenience samples were conducted, asking respondents to fill in SF-12 to reflect 62 lay descriptions of different levels of severity.15 16 From these responses, a relation between the SF-12 summary score and the Global Burden of Disease disability weights was derived. Using regression modelling, average disability weights were calculated while controlling for any comorbidity by adding dummy variables for each comorbid condition. As the case definition was point prevalence of neck pain, Global Burden of Disease Study disregarded the proportion of MEPS respondents with an existing neck pain diagnosis if no disability attributable to neck pain was found. For the remaining cases, the disability weight attributed to neck pain was binned across the four health states, and thresholds were assumed at the midpoint values.9
Compilation of results
Disability adjusted life year (DALY) is the standard metric used to quantify burden11 and is calculated by combining years of life lost due to premature mortality and years lived with disability. One DALY can be considered as one lost year of “healthy” life. As no evidence for mortality from neck pain was found in the Global Burden of Disease Study, years lived with disability and DALY estimates were the same.9 Global Burden of Disease Study multiplied the average disability weight by the age, sex, and region specific prevalence to derive years lived with disability, and uncertainty was incorporated by sampling 1000 draws at each computational step. Uncertainty was combined from multiple sources (eg, input data, corrections of measurement error, and estimates of residual non-sampling error). Uncertainty intervals were defined as the 25th and 975th values of the ordered draws.
We also used smoothing splines models to determine the shape of the association between neck pain burden in terms of years lived with disability and sociodemographic index for 21 regions and 195 countries.17 The sociodemographic index is a composite indicator and includes lag distributed income per capita and gross domestic product per capita smoothed over the preceding 10 years, average years of schooling for the population older than 15 years, and total fertility rate under age 25 years. The index ranges from 0 (less developed) to 1 (most developed). R software version 3.5.2 was used to map the age standardised point prevalence, the annual incidence, and rates of years lived with disability.
Patient and public involvement
No patients were involved in setting the research question or the outcome measures, nor were they involved in the design and implementation of the study.
Results
Global level
Globally, the number of prevalent cases of neck pain was 288.7 million (95% uncertainty interval 254.7 to 323.5 million) in 2017, with an age standardised point prevalence per 100 000 population of 3551.1 (95% uncertainty interval 3139.5 to 3977.9), which did not change significantly from 1990 (−0.9%, 95% uncertainty interval −2.1% to 0.4% per 100 000 population). Moreover, neck pain accounted for 65.3 million (95% uncertainty interval 57.7 to 73.9 million) incident cases, with an age standardised rate per 100 000 population of 806.6 (95% uncertainty interval 713.7 to 912.5), which also did not change significantly from 1990 (−0.7%, 95% uncertainty interval −1.8% to 0.4% per 100 000 population) (table 1). The number of years lived with disability due to neck pain in 2017 at the global level was 28.6 million (95% uncertainty interval 20.0 to 40.2 million), with an age standardised rate per 100 000 population of 352 (95% uncertainty interval 245.6 to 493.3) years lived with disability, and this was also unchanged from 1990 to 2017 (−0.7%, 95% uncertainty interval −2.0% to 0.6% per 100 000 population) (table 1).
Table 1.
Prevalence, incidence, and years lived with disability (YLDs) from neck pain in general population in 2017 for males and females, and percentage change of age standardised rates (ASRs) per 100 000 population between 1990 and 2017 by Global Burden of Disease regions (generated from data available at http://ghdx.healthdata.org/gbd-results-tool)
| Regions | Prevalence | Incidence | YLDs | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No (95% UI) | ASRs per 100 000 population (95% UI) | % change in ASRs per 100 000 population (95% UI) | No (95% UI) | ASRs per 100 000 population (95% UI) | % change in ASRs per 100 000 population (95% UI) | No (95% UI) | ASRs per 100 000 population (95% UI) | % change in ASRs per 100 000 population (95% UI) | |||
| Global | 288 718 637 (254 715 305 to 323 482 959) | 3551.1 (3139.5 to 3977.9) | −0.9 (−2.1 to 0.4) | 65 310 272 (57 678 178 to 73 917 203) | 806.6 (713.7 to 912.5) | −0.7 (−1.8 to 0.4) | 28 631 074 (19 951 796 to 40 202 298) | 352.0 (245.6 to 493.3) | −0.7 (−2.0 to 0.6) | ||
| High income Asia Pacific | 9 495 920 (8 371 926 to 10 686 578) | 3192.1 (2813.4 to 3605.6) | −1.0 (−1.5 to −0.5) | 2 054 594 (1 807 307 to 2 350 947) | 734.7 (647.1 to 835.3) | −1.1 (−1.4 to −0.7) | 936 249 (652 200 to 1 315 556) | 318.6 (221.4 to 449.8) | −1.0 (−1.9 to −0.1) | ||
| High income North America | 20 722 958 (19 036 919 to 22 539 759) | 4182.6 (3849.3 to 4542.3) | 4.1 (−2.0 to 11.1) | 4 182 954 (3 738 498 to 4 678 373) | 906.4 (812.5 to 1012.5) | 3.0 (−2.0 to 7.8) | 2 015 719 (1 437 154 to 2 755 825) | 410.2 (294.0 to 559.1) | 3.8 (−2.4 to 10.8) | ||
| Western Europe | 28 849 363 (25 318 179 to 32 358 471) | 4636.1 (4077.2 to 5250.5) | 2.0 (1.2 to 2.7) | 5 149 081 (4 558 321 to 5 828 329) | 890.9 (784.6 to 1006.2) | 1.5 (1.0 to 2.2) | 2 836 657 (1 977 989 to 3 948 673) | 461.0 (321.7 to 639.1) | 2.0 (1.1 to 3.0) | ||
| Australasia | 989 881 (869 532 to 1 117 817) | 2605.9 (2294.4 to 2952.4) | −1.4 (−2.1 to −0.7) | 227 788 (201 032 to 259 368) | 624.5 (552.4 to 710.8) | −1.1 (−1.8 to −0.4) | 97 207 (67 960 to 136 154) | 257.8 (179.8 to 360.4) | −1.4 (−3.4 to 0.9) | ||
| Andean Latin America | 1 449 411 (1 276 198 to 1 638 746) | 2511.6 (2212.7 to 2832.5) | 0.0 (0.0 to 0.0) | 364 135 (321 637 to 414 665) | 624.0 (550.3 to 708.3) | 0.0 (0.0 to 0.0) | 144 990 (100 046 to 205 524) | 250.7 (173.4 to 355.1) | 0.3 (−1.4 to 1.9) | ||
| Tropical Latin America | 6 079 026 (5 315 308 to 6 906 885) | 2505.6 (2194.4 to 2842.9) | −1.2 (−4.2 to 1.7) | 1 533 633 (1 348 350 to 1 751 610) | 633.4 (558.2 to 721.3) | −0.9 (−3.4 to 1.6) | 603 231 (416 994 to 848 970) | 248.3 (172.2 to 349.3) | −0.8 (−3.9 to 2.2) | ||
| Central Latin America | 6 462 315 (5 672 208 to 7 312 549) | 2582.6 (2271.4 to 2914.6) | 0.1 (0.0 to 0.2) | 1 619 705 (1 429 212 to 1 850 344) | 642.7 (568.0 to 730.8) | 0.0 (−0.1 to 0.1) | 646 288 (445 443 to 925 195) | 257.7 (179.0 to 367.2) | 0.3 (−0.4 to 1.0) | ||
| Southern Latin America | 2 549 298 (2 223 811 to 2 869 033) | 3382.8 (2949.8 to 3817.0) | 0.0 (−0.1 to 0.0) | 553 332 (486 910 to 631 021) | 746.9 (658.9 to 849.9) | 0.0 (0.0 to 0.0) | 252 202 (175 981 to 355 854) | 335.6 (234.3 to 474.0) | 0.0 (−1.5 to 1.5) | ||
| Caribbean | 1 264 130 (1 110 849 to 1 427 024) | 2514.0 (2215.4 to 2834.7) | 0.1 (0.0 to 0.1) | 311 023 (274 023 to 353 016) | 624.4 (550.6 to 708.6) | 0.0 (0.0 to 0.1) | 125 749 (86 485 to 17 7865) | 250.2 (172.5 to 354.5) | 0.1 (−1.2 to 1.3) | ||
| Central Europe | 5 061 385 (4 418 024 to 5 706 039) | 3015.6 (2642.0 to 3397.6) | −0.2 (−0.2 to −0.1) | 116 7813 (1 030 182 to 1 330 135) | 726.9 (638.1 to 832.1) | −0.1 (−0.1 to 0.0) | 491 277 (343 469 to 686 249) | 296.0 (206.9 to 413.9) | 0.2 (−0.8 to 1.1) | ||
| Eastern Europe | 9 260 164 (8 129 721 to 10 486 582) | 3163.8 (2793.8 to 3574.2) | −0.2 (−0.3 to 0.0) | 218 1643 (1 912 969 to 2 478 318) | 772.7 (681.1 to 877.3) | −0.1 (−0.2 to 0.0) | 901 262 (628 653 to 1 263 018) | 310.2 (216.2 to 434.7) | 0.1 (−0.5 to 0.7) | ||
| North Africa and Middle East | 23 769 992 (20 781 749 to 27 077 226) | 4458.4 (3917.7 to 5022.4) | 0.2 (−0.5 to 0.9) | 5 411 903 (4 751 191 to 6 211 636) | 975.6 (864.6 to 1109.0) | 0.0 (−0.5 to 0.6) | 2 349 957 (1 619 825 to 3 304 202) | 437.4 (305.3 to 611.3) | 0.6 (−0.3 to 1.5) | ||
| Central Asia | 2 631 078 (2 297 726 to 3 001 217) | 3023.2 (2648.1 to 3404.0) | −0.2 (−0.3 to −0.1) | 642 335 (563 808 to 737 353) | 727.7 (638.8 to 832.8) | −0.1 (−0.2 to 0.0) | 261 072 (182 450 to 370 400) | 298.1 (208.5 to 417.3) | 0.0 (−1.1 to 1.0) | ||
| South Asia | 41 007 649 (36 008 253 to 46 563 533) | 2582.2 (2276.9 to 2910.0) | −0.1 (−0.2 to 0.1) | 10 480 063 (9 226 596 to 12 001 779) | 643.6 (568.7 to 731.0) | −0.1 (−0.2 to 0.0) | 4 050 148 (2 816 209 to 5 702 960) | 253.3 (176.6 to 355.7) | 0.4 (−0.2 to 1.0) | ||
| South East Asia | 19 222 822 (16 803 626 to 21 921 275) | 2836.8 (2492.9 to 3209.8) | −0.1 (−0.2 to 0.0) | 4 760 408 (4 201 654 to 5 431 012) | 697.6 (616.3 to 792.5) | −0.1 (−0.2 to −0.1) | 1 919 636 (1 330 211 to 2 687 347) | 281.9 (196.7 to 395.5) | 0.3 (−0.4 to 1.1) | ||
| East Asia | 90 969 608 (79 345 777 to 102 768 081) | 4589.7 (4042.7 to 5168.9) | 2.1 (−1.7 to 6.0) | 19 811 508 (17 390 568 to 22 514 874) | 1029.0 (910.5 to 1166.1) | 1.7 (−1.4 to 5.1) | 9 120 129 (6 318 151 to 12 798 100) | 461.0 (320.1 to 643.9) | 2.4 (−1.4 to 6.4) | ||
| Oceania | 299 965 (262 581 to 343 806) | 3171.0 (2788.8 to 3580.3) | 0.1 (0.0to 0.1) | 75 293 (66 016 to 86 935) | 758.5 (671.4 to 863.6) | 0.1 (0.0 to 0.1) | 29 664 (20 570 to 41 668) | 309.3 (216.3 to 431.6) | −0.3 (−1.8 to 1.5) | ||
| Western sub‐Saharan Africa | 8 789 653 (7 701 690 to 10 070 267) | 3401.1 (2981.9 to 3832.8) | 1.9 (−0.1 to 4.2) | 2 186 850 (1911528 to 2525795) | 788.2 (695.4 to 899.1) | 1.0 (−0.5 to 2.8) | 872 560 (608 158 to 1 223 096) | 333.6 (234.0 to 466.6) | 2.6 (0.3 to 5.2) | ||
| Eastern sub‐Saharan Africa | 5 736 656 (5 034 504 to 6 559 552) | 2511.6 (2204.8 to 2846.1) | 0.1 (0.0 to 0.2) | 1 544 027 (1363963 to 1774784) | 630.2 (557.1 to 717.2) | 0.1 (0.0 to 0.2) | 572 452 (395 897 to 807 094) | 247.5 (171.9 to 347.1) | 0.9 (0.2 to 1.6) | ||
| Central sub‐Saharan Africa | 2 116 513 (1 842 710 to 2 413 215) | 2863.6 (2501.5 to 3243.1) | 0.0 (−0.2 to 0.2) | 548 291 (480 439 to 629 454) | 695.8 (615.0 to 791.6) | −0.1 (−0.2 to 0.1) | 208 852 (144 564 to 294 716) | 278.4 (194.7 to 393.0) | 0.8 (−0.9 to 2.6) | ||
| Southern sub‐Saharan Africa | 1 990 850 (1 746 880 to 2 275 371) | 2983.5 (2631.8 to 3387.5) | 0.3 (0.1 to 0.4) | 503 891 (443 802 to 576 993) | 730.6 (646.0 to 829.9) | 0.2 (0.0 to 0.3) | 195 771 (136 617 to 275 386) | 291.2 (202.5 to 408.9) | −0.1 (−0.9 to 0.7) | ||
UI=uncertainty interval.
Regional level
The highest age standardised point prevalences of neck pain per 100 000 population in 2017 were in western Europe (4636.1 (95% uncertainty interval 4077.2 to 5250.5)), east Asia (4589.7 (4042.7 to 5168.9)), and North Africa and the Middle East (4458.4 (3917.7 to 5022.4)). The lowest age standardised rates per 100 000 population were in tropical Latin America (2505.6 (2194.4 to 2842.9)), eastern sub-Saharan Africa (2511.6 (2204.8 to 2846.1)), and Andean Latin America (2511.6 (2212.7 to 2832.5)) (table 1).
The highest age standardised annual incidences of neck pain per 100 000 population were in east Asia (1029.0 (95% uncertainty interval 910.5 to 1166.1)), North Africa and the Middle East (975.6 (864.6 to 1109.0)), and high income North America (906.4 (812.5 to 1012.5)). These rates were lowest for Andean Latin America (624.0 (550.3 to 708.3)), the Caribbean (624.4 (550.6 to 708.6)), and Australasia (624.5 (552.4 to 710.8)) (table 1).
East Asia (461.0 (320.1 to 643.9)), western Europe (461.0 (321.7 to 639.1)), and North Africa and the Middle East (437.4 (305.3 to 611.3)) also had the highest age standardised rate for years lived with disability from neck pain per 100 000 population in 2017; whereas eastern sub-Saharan Africa (247.5 (171.9 to 347.1)), tropical Latin America (248.3 (172.2 to 349.3)), and the Caribbean (250.2 (172.5 to 354.5)) had the lowest age standardised rates for years lived with disability per 100 000 population (table 1). Supplementary figures S1 and S2 show the age standardised point prevalence and annual incidence of neck pain per 100 000 population for all Global Burden of Disease regions in 2017 for males and females, respectively.
Generally, the age standardised point prevalence, annual incidence, and rates of years lived with disability from neck pain have not changed over the past three decades. A statistically significant increase in the age standardised point prevalence of neck pain per 100 000 population was found in western Europe (2.0% (95% uncertainty interval 1.2% to 2.7%)), southern sub-Saharan Africa (0.3% (0.1% to 0.4%)), and eastern sub-Saharan Africa (0.1% (0.0% to 0.2%)) between 1990 and 2017 (table 1). The highest percentage change in the age standardised annual incidence of neck pain per 100 000 population from 1990 to 2017 was in western Europe (1.5% (1.0% to 2.2%)), southern sub-Saharan Africa (0.2% (0.0% to 0.3%)), and eastern sub-Saharan Africa (0.1% (0.0% to 0.2%)) (table 1). In addition, the highest increase in age standardised years lived with disability from neck pain per 100 000 population during 1990 to 2017 was in western sub‐Saharan Africa (2.6% (0.3% to 5.2%)), western Europe (2% (1.1% to 3.0%)), and eastern sub‐Saharan Africa (0.9% (0.2% to 1.6% (table 1). Supplementary figures S3 and S4 show the sex specific percentage in age standardised point prevalence and annual incidence of neck pain during 1990 to 2017, respectively.
The number of prevalent cases of neck pain increased from 164.3 million (95% uncertainty interval 144.9 to 185.9 million) in 1990 to 288.7 million (254.7 to 323.5 million) in 2017. The highest number of prevalent cases in 2017 were in East Asia, south Asia, and western Europe (supplementary fig S5, supplementary table S2).
Likewise, the number of incident cases of neck pain increased substantially, from 38.2 million (33.7 to 43.5 million) in 1990 to 65.3 million (57.7 to 73.9 million) in 2017. The highest numbers of incident cases of neck pain in 2017 were in east Asia, south Asia, and North Africa and the Middle East (supplementary fig S6, supplementary table S3).
National level
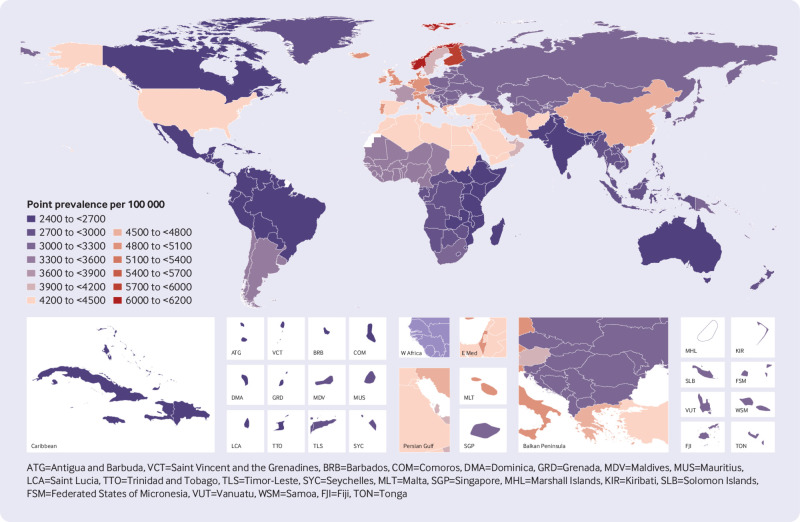
The national age standardised point prevalence of neck pain in 2017 ranged from 2443.9 to 6151.2 cases per 100 000 population. The countries with the highest age standardised point prevalence estimates per 100 000 population in 2017 were Norway (6151.2 (5382.3 to 6959.8)), Finland (5750.3 (5058.4 to 6518.3)), and Denmark (5316 (4674 to 6030.1)), whereas Djibouti (2443.9 (2146.4 to 2771.9)), South Sudan (2449.8 (2149.8 to 2781.1)), and Burundi (2450.1 (2150 to 2778.9)) had the lowest rates (fig 1 and supplementary table S2).
Fig 1.
Age standardised point prevalence of neck pain per 100 000 population in 2017, by country. Generated from data available at http://ghdx.healthdata.org/gbd-results-tool
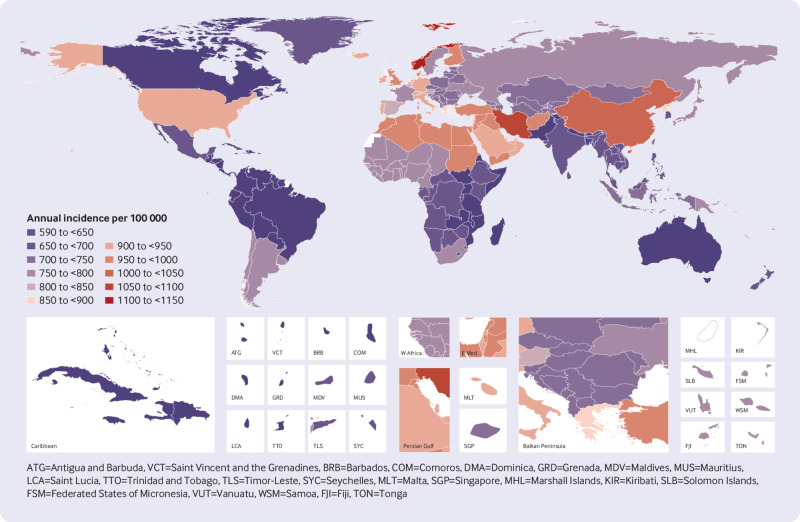
The national age standardised annual incidence of neck pain in 2017 varied from 599.6 in Canada to 1145 cases per 100 000 population in Norway. The highest rates were observed in Norway (1145 (1008.8 to 1304.9)), Iran (1055.5 (927.8 to 1199.6)), and China (1037.7 (917.3 to 1176.9)), with the lowest rates reported in Canada (599.6 (528.8 to 679.1)), Bhutan (612.4 (542.1 to 696.3)), and Pakistan (613.6 (543.4 to 698.3)) (fig 2 and supplementary table S3).
Fig 2.
Age standardised annual incidence of neck pain per 100 000 population in 2017, by country. Generated from data available at http://ghdx.healthdata.org/gbd-results-tool
In addition, the national age standardised years lived with disability from neck pain in 2017 ranged from 237.4 to 609.2 cases per 100 000 population. The highest rates were observed in Norway (609.2 (425.5 to 849.8)), Finland (569.7 (389.3 to 797.1)), and Denmark (527.1 (369.2 to 740.6)) and the lowest were observed in South Sudan (237.4 (165.1 to 332.4)), Mozambique (241.1 (168.4 to 335.1)), and Eritrea (241.2 (168.1 to 338.7)) (supplementary fig S7 and table S4).
The percentage change in age standardised point prevalence estimates per 100 000 population from 1990 to 2017 differed substantially between countries, with the largest increases in the UK (14.6% (10.6% to 18.8%)), Sweden (10.4% (6.0% to 15.4%)), and Kuwait (2.6% (2.0% to 3.2%)). In contrast, Taiwan (−10.5% (−18.4% to −1.5%)), New Zealand (−7.4% (−11.2% to −3.5%)), and Qatar (−2.6% (−3.0% to −2.1%)) showed the largest decreases from 1990 to 2017 (supplementary table S2).
The largest increases in age standardised annual incidence of neck pain per 100 000 population from 1990 to 2017 were in the UK (9.1% (6.1% to 12.4%)), Sweden (6.5% (3.7% to 9.7%)), and Kuwait (1.6% (1.1% to 2%)). In contrast, Taiwan (−8.2% (−15.8% to −0.5%)), New Zealand (−6.0% (−9.7% to −2.3%)), and Cape Verde (−1.5% (−2.0% to −0.9%)) showed the largest decreases (supplementary table S3).
The change in age standardised years lived with disability from neck pain per 100 000 population from 1990 to 2017 also varied between countries. The UK (14.2% (10.2% to 18.5%)), Sweden (10.3% (5.5% to 15.6%)), and Kuwait (2.7% (0.5% to 4.8%)) showed the largest increases in that period, whereas Taiwan (−10.8% (−18.9% to −1.6%)), New Zealand (−7.4% (−11.6% to −2.9%)), and the United Arab Emirates (−2.2% (−4.3% to −0.1%)) showed the largest decreases (supplementary table S4).
Age and sex patterns
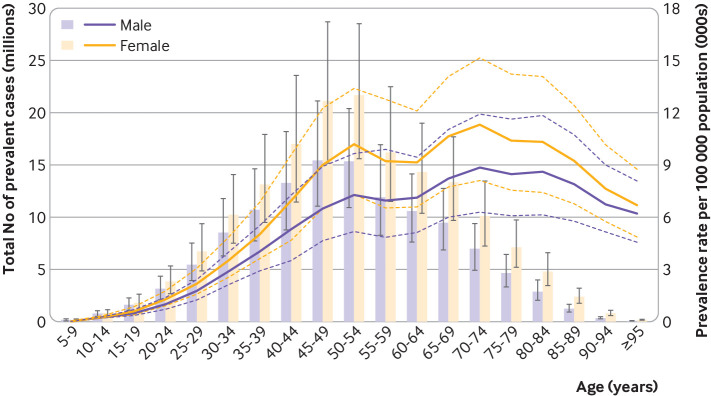
The global point prevalence of neck pain in 2017 was higher in females and increased with age up to 70-74 years, then decreased with older age. Similarly, the number of prevalent cases increased with age and peaked at the 45-49 and 50-54 age groups for males and females, respectively, then decreased with older age (fig 3). In 2017, the global annual incidence of neck pain was also found to be higher in females and generally increased with age, peaking at the 65-69 age group. The number of incident cases were highest at age 45-49 years, after which a declining trend was observed at older ages (supplementary fig S8). The pattern of years lived with disability by sex across age groups was relatively similar to that of point prevalence estimate (supplementary fig S9). Notably, no statistically significant differences were found between males and females for prevalence, incidence, and years lived with disability across the age groups.
Fig 3.
Global number of prevalent cases and age standardised point prevalence of neck pain per 100 000 population by age and sex, 2017. Dashed lines indicate 95% upper and lower uncertainty intervals, respectively. Generated from data available at http://ghdx.healthdata.org/gbd-results-tool
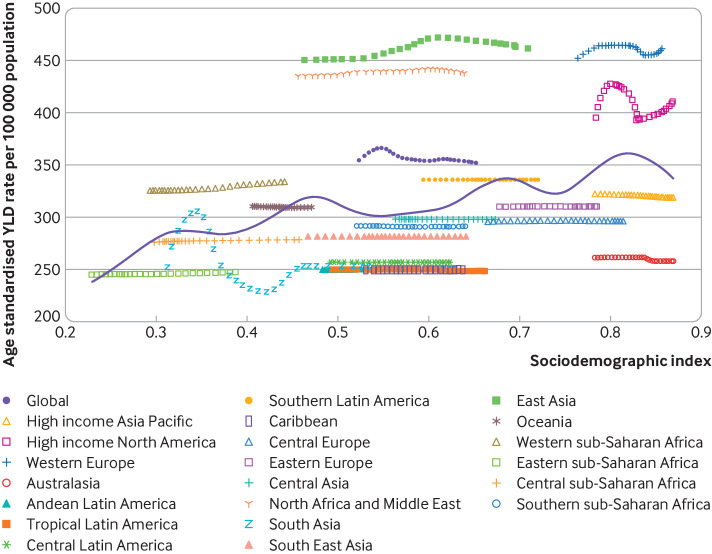
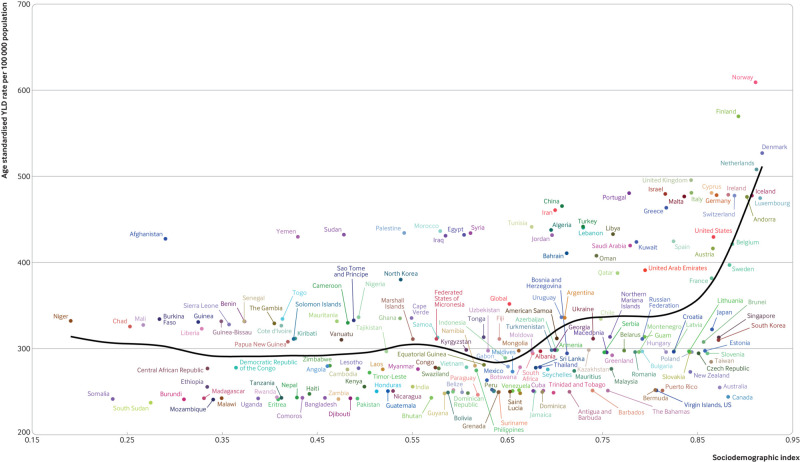
Observed burden of neck pain compared with expected by sociodemographic index
Overall, a positive association was observed between the age standardised years lived with disability from neck pain and sociodemographic index at a global level as well as across Global Burden of Disease regions. Namely, the burden of neck pain is increased at higher levels of socioeconomic development (fig 4).
Fig 4.
Age standardised years lived with disability (YLD) from neck pain per 100 000 population for 21 Global Burden of Disease regions by sociodemographic index, 1990-2017. Purple line represents expected values based on sociodemographic index and disease rates in all locations. Twenty eight points are plotted for each Global Burden of Disease region and show observed age standardised years lived with disability from 1990 to 2017 for that region. Generated from data available at http://ghdx.healthdata.org/gbd-results-tool
Globally, the observed burden of neck pain was higher than expected on the basis of sociodemographic development (as measured by the sociodemogaphic index) over the past 28 years. At the regional level, the observed burden was higher than expected given the sociodemographic index for east Asia, western Europe, North Africa and the Middle East, high income North America, and western sub-Saharan Africa, and mostly lower than expected for the remaining Global Burden of Disease regions (fig 4).
High burden of neck pain was not, however, limited to developed countries—Canada, Australia, and New Zealand had much lower than expected burdens, whereas in developing countries such as Afghanistan, Yemen, and Sudan, the burden of neck pain was much higher than the expected level on the basis of the sociodemographic index (fig 5).
Fig 5.
Age standardised years lived with disability (YLD) from neck pain per 100 000 population by 195 countries and sociodemographic index, 2017. Black line represents expected values. Each point shows observed age standardised years lived with disability for specified country in 2017. Generated from data available at http://ghdx.healthdata.org/gbd-results-tool
Discussion
In this study, we report the prevalence, incidence, years lived with disability, and age standardised rates for neck pain in the general population for 195 countries, from 1990 to 2017. In 2017, there were 288.7 million prevalent cases, 65.3 million incident cases, and 28.6 million years lived with disability. Although the age standardised rates of point prevalence, annual incidence, and years lived with disability from neck pain have not changed significantly over the measurement period, the number of prevalent cases, incident cases, and years lived with disability has increased, possibly as a result of population growth and aging—not specifically reported in previous studies.
Since the last Global Burden of Disease report using data from 20104 a small but statistically significant decrease in global age standardised point prevalence estimate from 4.9% in 2010 to 3.5% has been observed. Moreover, the Global Burden of Disease Study 20104 found that high income North American and western Europe had the highest age standardised point prevalence estimates. In contrast, our study found that in 2017 western Europe and east Asia had the global highest age standardised point prevalence estimates. These differences can be mainly attributable to the methodologies and data sources used in the two studies. Unfortunately, most previous systematic reviews7 8 18 19 provide results that are incomparable to ours, given they used different definitions for neck pain and failed to include global prevalence or incidence data.
In our study, age standardised point prevalence, annual incidence, and years lived with disability in 2017 and percentage changes since 1990, were provided for 195 countries, enabling the burden of neck pain to be compared across different nations. The results presented here were mainly derived from modelled data through processes in the bayesian metaregression tool DISMOD-MR 2.1, as only a few countries had actual national data on prevalence and incidence of neck pain. Hence, national level estimates should be interpreted with caution. Importing data on neck pain in specific national health surveys, if available, is therefore encouraged to ensure the capture of more representative data for each country. In fact, this strategy not only will strengthen future Global Burden of Disease studies but could also be used to monitor county specific burden of neck pain as well as the long term efficiency and effectiveness of prevention and treatment strategies used to tackle it. We acknowledge this approach would require resources that are not always available in low to middle income countries, and that a more globally coordinated effort might be required.
The point prevalence estimate of neck pain was found to be higher in females across all age groups, confirming the findings of previous studies.4 8 19 In addition, point prevalence estimates in our study peaked at middle ages, which is also confirmed by other studies.4 8 19 The highest burden was among men aged 45-49 years and women aged 45-54 years. This has direct implications for clinical practice and policy, as preventive and educational approaches targeting these specific groups should be encouraged globally. Whereas neck pain has been a relatively understudied condition, a strong evidence base exists for low back pain. It is likely that the guidance for low back pain—to keep imaging to a minimum and to provide advice and education to remain active—can be extrapolated to neck pain, but this remains to be determined.
The developing status of regions and countries is one of the important factors of neck pain burden that has not been dealt with in previous studies.4 7 19 At a regional level, generally a positive association was found between regional level sociodemographic index and age standardised years lived with disability from neck pain between 1990 and 2017. This means that the burden of neck pain is generally higher at higher socioeconomic levels of development. This phenomenon could possibly be driven by increased levels of physical inactivity, obesity, and aging.
Detection and control of risk factors are common approaches in prevention programmes. The risk factors for neck pain are classified into different categories, such as demographic and socioeconomic factors, previous health or past pain or comorbidities, road traffic injuries or workplace factors, psychological and social factors, genetics, and health behaviours.19 Unfortunately, the attributable burden of neck pain due to these risk factors has not yet been assessed in these Global Burden of Disease estimates. Policymakers might also want to consider country specific patterns of risk factors for neck pain in their management recommendations.
Strengths and limitations of this study
Although using the US derived Medical Expenditure Panel Surveys (MEPS) has allowed Global Burden of Disease to estimate the severity distribution of neck pain while taking morbidity into account, some limitations should be considered. Recall bias is possible as data were collected at five follow-up points over two years. Also, MEPS might not be representative of the health state experience for neck pain across the globe. In low to middle income countries, where prevention and management strategies for neck pain might not be as efficient as in high income countries, the health state experience could be different.
Conclusions and policy implications
Neck pain is a public health issue in general populations gobally, but varies considerably between countries. Improving health data on all musculoskeletal conditions such as neck pain in all countries and regions is strongly suggested for improving the Global Burden of Disease estimates. Although the age standardised point prevalence, annual incidence, and years lived with disability from neck pain did not change between 1990 and 2017, its burden remains high, with middle aged men and women particularly at risk. Increasing population awareness about neck pain and its risk factors as well as the importance of early detection and management is warranted to reduce the future burden of this condition.
What is already known on this topic
Neck pain varies widely between countries but is a highly prevalent condition that leads to considerable pain, disability, and economic cost
The Global Burden of Disease Study 2010 highlighted the high global burden of neck pain
What this study adds
In this study, the global age standardised point prevalence, annual incidence, and years lived with disability from neck pain per 100 000 population in 2017 were estimated to be 3551, 807, and 352, respectively
Western Europe, east Asia and North Africa and the Middle East had the highest age-standardised point prevalence of neck pain in 2017
Norway, Finland, and Denmark had the highest age standardised point prevalence estimates for neck pain in 2017, whereas the UK, Sweden, and Kuwait showed the largest increases between 1990 and 2017
Acknowledgments
We thank the staff at the Institute for Health Metrics and Evaluation and its collaborators who prepared these publicly available data and the support of the Social Determinants of Health Research Center of Shahid Beheshti University of Medical Sciences. This study is based on publicly available data and solely reflects the opinion of its authors and not that of the Institute for Health Metrics and Evaluation.
Web extra.
Extra material supplied by authors
Web appendix: Supplementary figures
Web appendix: Supplementary tables
Contributors: SS, AAK, LM, and MLF designed the study. SS, AAK, MAM, AA-H, and AA-A analysed the data and performed the statistical analyses. SS, AAK, DB, ES, MS, MC, and MLF drafted the initial manuscript. All authors reviewed the drafted manuscript for critical content and approved the final version. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. SS and MLF are the guarantors.
Funding: The Global Burden of Disease Study is funded by the Bill and Melinda Gates Foundation. The funder was not involved in the preparation of this manuscript. The present report was also supported by Shahid Beheshti University of Medical Sciences, Tehran, Iran (grant No 20732-4-7). MLF holds a National Health and Medical Research Council of Australia research fellowship.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: Global Burden of Disease Study is funded by the Bill and Melinda Gates Foundation, and this study was supported by Shahid Beheshti University of Medical Sciences, Tehran, Iran (grant No 20732-4-7); no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: This study was approved by ethics committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran (IR.SBMU.RETECH.REC.1398.446).
Data sharing: The data used for the analyses are publicly available from the Institute of Health Metrics and Evaluation website (www.ihme.org).
The lead authors (SS and MLF are manuscript’s guarantors) affirms that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and any discrepancies have been explained.
Dissemination to participants and related patient and public communities: Our results will be disseminated through media outlets and presentations at scientific conferences and academic events. Given that no patients were recruited for the study, there are no plans to disseminate the results to study participants.
Publisher’s note: Published maps are provided without any warranty of any kind, either express or implied. BMJ remains neutral with regard to jurisdictional claims in published maps.
References
- 1. Henschke N, Kamper SJ, Maher CG. The epidemiology and economic consequences of pain. Mayo Clin Proc 2015;90:139-47. 10.1016/j.mayocp.2014.09.010 [DOI] [PubMed] [Google Scholar]
- 2. Manchikanti L, Singh V, Datta S, Cohen SP, Hirsch JA, American Society of Interventional Pain Physicians Comprehensive review of epidemiology, scope, and impact of spinal pain. Pain Physician 2009;12:E35-70. [PubMed] [Google Scholar]
- 3. Haldeman S, Carroll L, Cassidy JD. Findings from the bone and joint decade 2000 to 2010 task force on neck pain and its associated disorders. J Occup Environ Med 2010;52:424-7. 10.1097/JOM.0b013e3181d44f3b [DOI] [PubMed] [Google Scholar]
- 4. Hoy D, March L, Woolf A, et al. The global burden of neck pain: estimates from the global burden of disease 2010 study. Ann Rheum Dis 2014;73:1309-15. 10.1136/annrheumdis-2013-204431 [DOI] [PubMed] [Google Scholar]
- 5. Sebbag E, Felten R, Sagez F, Sibilia J, Devilliers H, Arnaud L. The world-wide burden of musculoskeletal diseases: a systematic analysis of the World Health Organization Burden of Diseases Database. Ann Rheum Dis 2019;78:844-8. 10.1136/annrheumdis-2019-215142 [DOI] [PubMed] [Google Scholar]
- 6. Moradi-Lakeh M, Forouzanfar MH, Vollset SE, et al. Burden of musculoskeletal disorders in the Eastern Mediterranean Region, 1990-2013: findings from the Global Burden of Disease Study 2013. Ann Rheum Dis 2017;76:1365-73. 10.1136/annrheumdis-2016-210146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population: a systematic critical review of the literature. Eur Spine J 2006;15:834-48. 10.1007/s00586-004-0864-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hoy DG, Protani M, De R, Buchbinder R. The epidemiology of neck pain. Best Pract Res Clin Rheumatol 2010;24:783-92. 10.1016/j.berh.2011.01.019 [DOI] [PubMed] [Google Scholar]
- 9. James SL, Abate D, Abate KH, et al. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1789-858. 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Roth GA, Abate D, Abate KH, et al. GBD 2017 Causes of Death Collaborators Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1736-88. 10.1016/S0140-6736(18)32203-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kyu HH, Abate D, Abate KH, et al. GBD 2017 DALYs and HALE Collaborators Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1859-922. 10.1016/S0140-6736(18)32335-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Stanaway JD, Afshin A, Gakidou E, et al. GBD 2017 Risk Factor Collaborators Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1923-94. 10.1016/S0140-6736(18)32225-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Stevens GA, Alkema L, Black RE, et al. The GATHER Working Group ). Guidelines for Accurate and Transparent Health Estimates Reporting: the GATHER statement. Lancet 2016;388:e19-23. 10.1016/S0140-6736(16)30388-9 [DOI] [PubMed] [Google Scholar]
- 14. Guzman J, Hurwitz EL, Carroll LJ, et al. A new conceptual model of neck pain: linking onset, course, and care: the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. J Manipulative Physiol Ther 2009;32(Suppl):S17-28. 10.1016/j.jmpt.2008.11.007 [DOI] [PubMed] [Google Scholar]
- 15. Hoy DG, Smith E, Cross M, et al. The global burden of musculoskeletal conditions for 2010: an overview of methods. Ann Rheum Dis 2014;73:982-9. 10.1136/annrheumdis-2013-204344 [DOI] [PubMed] [Google Scholar]
- 16. Salomon JA, Vos T, Hogan DR, et al. Common values in assessing health outcomes from disease and injury: disability weights measurement study for the Global Burden of Disease Study 2010. Lancet 2012;380:2129-43. 10.1016/S0140-6736(12)61680-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wang Y. Smoothing splines: methods and applications. Chapman and Hall/CRC, 2011. 10.1201/b10954. [DOI] [Google Scholar]
- 18. Cohen SP. Epidemiology, diagnosis, and treatment of neck pain. Mayo Clin Proc 2015;90:284-99. 10.1016/j.mayocp.2014.09.008 [DOI] [PubMed] [Google Scholar]
- 19. Hogg-Johnson S, van der Velde G, Carroll LJ, et al. Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders The burden and determinants of neck pain in the general population: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine (Phila Pa 1976) 2008;33(Suppl):S39-51. 10.1097/BRS.0b013e31816454c8 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Supplementary figures
Web appendix: Supplementary tables