Abstract
Hypoxia-inducible factor-1α (HIF-1α), which accumulates in mammalian host organisms during infection, supports the defense against microbial pathogens. However, whether and to what extent HIF-1α expressed by myeloid cells contributes to the innate immune response against Leishmania major parasites is unknown. We observed that Leishmania-infected humans and L. major–infected C57BL/6 mice exhibited substantial amounts of HIF-1α in acute cutaneous lesions. In vitro, HIF-1α was required for leishmanicidal activity and high-level NO production by IFN-γ/LPS-activated macrophages. Mice deficient for HIF-1α in their myeloid cell compartment had a more severe clinical course of infection and increased parasite burden in the skin lesions compared with wild-type controls. These findings were paralleled by reduced expression of type 2 NO synthase by lesional CD11b+ cells. Together, these data illustrate that HIF-1α is required for optimal innate leishmanicidal immune responses and, thereby, contributes to the cure of cutaneous leishmaniasis.
Hypoxia inducible factor-1α (HIF-1α) promotes the adaption of cells to low O2 microenvironments. Low O2 conditions result in HIF-1α stabilization by impairing the enzymatic activity of prolyl hydroxylase domain enzymes (PHDs) and subsequent hydroxylation of two critical proline residues that target HIF-1α for proteasomal degradation (reviewed in Refs. 1, 2). However, under conditions of ample O2, HIF-1α accumulation can be induced by a plethora of other nonhypoxic signals (reviewed in Refs. 3–5). Accordingly, HIF-1α accumulation was found in mouse and human tissues infected with various pathogens (6).
In myeloid cells, exposure to inflammatory and pathogen-associated molecular pattern molecules, such as LPS, results in HIF-1α accumulation even under normoxic conditions, which requires transcriptional and posttranslational signaling events (7–10). This inflammatory HIF-1α stabilization in myeloid cells is necessary for their proinflammatory, antibacterial, and antifungal activity (11–15). Moreover, inflammatory HIF-1α expression in myeloid cells provides the metabolic basis for innate immune memory termed “trained immunity” (16).
In parasitic infections, the role of HIF-1α is less clear. In bovine macrophages infected with Theileria annulata, HIF-1α is required to transform these cells into aggressive leukemic-like cells (17). Toxoplasma gondii and Leishmania donovani induce HIF-1α stabilization in host cells to promote their survival within the intracellular niche (18, 19). In a mouse model of visceral leishmaniasis elicited by L. donovani, HIF-1α signaling in CD11c+ dendritic cells (DCs) was linked to an impaired DC function and CD8+ T cell response and supported parasite survival (20). Leishmania amazonensis infection of mice led to accumulation of HIF-1α in cutaneous lesions, but the functional role of HIF-1α in this model of nonhealing progressive cutaneous leishmaniasis has not been investigated (21, 22). There is circumstantial evidence that HIF-1α signaling might affect microRNA-210 expression in self-healing human leishmaniasis caused by L. major (23). However, it is unknown whether HIF-1α expression is necessary for the control of self-healing L. major infections in vivo. Given that control of cutaneous L. major infection requires type 2 NO synthase (NOS2)-dependent production of leishmanicidal NO (24–27) and that HIF-1α promotes the expression of NOS2 in macrophages (12, 28–30), we hypothesized that HIF-1α might support macrophage-driven antileishmanial control. Therefore, we tested the contribution of myeloid cell–specific HIF-1α to antileishmanial defense in vitro and in vivo.
Materials and Methods
Reagents
LPS (Escherichia coli O111:B4) was purchased from Sigma-Aldrich (Taufkirchen, Germany). Recombinant murine IFN-γ and TNF were purchased from eBioscience (Frankfurt, Germany). 2-(1-Chloro-4-hydroxyisoquinoline-3-carboxamido) acetate (ICA) was synthesized as previously described (31) and kindly provided by Prof. Nicolai Burzlaff (Department of Chemistry and Pharmacy, Friedrich-Alexander-Universität Erlangen-Nürnberg).
Parasites
Promastigotes of L. major strain MHOM/IL/81/FEBNI were propagated as described earlier (32, 33) in vitro in RPMI 1640 (10% FCS) on Novy-MacNeal-Nicolle blood agar slants for a maximum of five passages.
Abs
For flow cytometry analysis, fluorochrome-labeled Abs against CD11b (M1/70; BD Biosciences), NOS2 (6/iNOS/NOS Type II; BD Transduction Laboratories, Heidelberg, Germany), and the respective isotype controls were used. For Western blot analysis, primary rabbit Abs were used against the following mouse target proteins: actin (catalog [cat.] no. A2066; Sigma-Aldrich, Taufkirchen, Germany), HIF-1α (cat. no. 10006421; Cayman Chemical, Ann Arbor, MI), and HSP90 (cat. no. sc-7947, Santa Cruz Biotechnology, Heidelberg, Germany). HRP-conjugated polyclonal swine antirabbit IgG (P0399; Dako, Hamburg, Germany) was used as secondary Ab.
Murine model of cutaneous leishmaniasis infection
All animal experiments were carried out according to protocols approved by the Animal Welfare Committee of the local governmental authorities (Regierung von Mittelfranken, Ansbach and Regierung von Unterfranken Wurzburg, Germany). Hif1αflox/flox mice (34) were crossed with lysozyme M-driven Cre (LysMCre)-transgenic mice (35), both on a C57BL/6 background (36), as described earlier (37), to obtain mice deficient for Hif1α in their myeloid cell compartment (Hif1αΔmyel). At the age of 8–9 wk, female C57BL/6 Hif1αΔmyel mice and littermate controls were injected in the hind footpads with 3 × 106 stationary-phase L. major promastigotes (of low in vitro passage [≤5]) in 50 μl of PBS to induce infection.
Immunohistochemical analysis
Paraffin sections (2–4 μm) were dewaxed in xylene and rehydrated in a series of ethanol washes. The following primary Abs were used for immunodetection: polyclonal rabbit anti-HIF-1α (1:10,000; cat no. 10006421; Cayman Chemical) and polyclonal rabbit anti-mouse CD68 (1:500; cat. no. ab125212; Abcam, Cambridge, U.K.). Biotinylated secondary goat anti-rabbit (cat. no. BA1000; Vector Laboratories, Peterborough, U.K.) was used at a dilution of 1:1000. Abs were detected by a catalyzed signal amplification system (Dako) and counterstained. Use of human tissue in this study was approved by the Yale Human Investigation Committee, as part of the Yale Dermatopathology Stored Specimen Repository.
In vitro restimulation with soluble Leishmania Ag and quantification of Leishmania burden
In vitro restimulation of immune cells from popliteal lymph nodes of infected animals was performed as described earlier using soluble Leishmania Ag (26). Quantification of the number of parasites in the tissue was determined by limiting dilution analysis, as described earlier (26).
Generation and infection of primary macrophages
Mouse bone marrow-derived macrophages (BM-MΦs) were generated from C57BL/6 mice (Charles River Breeding Laboratories, Sulzfeld, Germany), Hif1α-deficient (Hif1αΔmyel) mice, or control mice and cultured in Teflon bags (FT FEP 100 C; Dupont) purchased via American Durafilm (Holliston, MA), as described earlier (38, 39). On day 7–8, macrophages were harvested and transferred onto polystyrene plates. Infection was carried out by coculturing of BM-MFs with L. major promastigotes at a 1:30 ratio for 4 h under normoxic conditions (37°C, 5% CO2, ~20% O2), as described earlier (26). Postinfection, extracellular L. major promastigotes were washed using PBS and cultured in the absence or presence of TNF (20 ng/ml), TNF/IFN-γ (each at 20 ng/ml), or LPS/IFN-γ (10 and 20 ng/ml, respectively) for 18–24 or 72 h under normoxic or hypoxic conditions. Normoxic conditions were achieved in a regular humidified incubator (37°C, 5% CO2, ~20% O2), whereas hypoxic conditions (37°C, 5% CO2, 2.8% O2) were generated using an adjustable hypoxic chamber suitable for cell culture experiments (Whitley H35 hypoxystation purchased via Meintrup DWS Laborgeräte, Herzlake, Germany). After 72 h, the cell cultures were analyzed microscopically using Diff-Quik staining (Medion Diagnostics, Düdingen, Switzerland) to determine the percentage of infected cells and the number of parasites per infected cell. The parasite load was calculated as the number of L. major in ~100 BM-MFs after 72 h/the number of L. major in ~100 BM-MFs after 4 h.
Immunoblotting
Extraction of proteins, preparation of cell lysates, and immunoblotting were performed as described earlier (9, 30). Signals were visualized by the Chemo Star Imager (Intas Science Imaging Instruments, Göttingen, Germany) or the ChemiDoc XRS+ System in combination with Image Lab Software (Bio-Rad, München, Germany). Images were processed with Adobe Photoshop CS6 software (Adobe Systems, San Jose, CA).
RNA isolation, reverse transcription, real-time PCR, and relative quantification
Total RNA was extracted from infected and stimulated cells and reverse transcribed as described earlier (9, 30). The following TaqMan assays were used for quantitative real-time PCR (Applied Biosystems, Darmstadt, Germany): Hprt1 (Mm00446968_m1), phosphoglycerate kinase 1 (Pgk1; Mm01225301_m1), Nos2 (Mm00440485_m1), Hif1a (Mm01283760_m1), and Tnfaip3 (Mm00437121_m1). Quantitative real-time PCR was carried out with an ABI Prism 7900 sequence detector (Applied Biosystems) and FastStart Universal Probe Master (Rox) (Roche Diagnostics, Mannheim, Germany). Data were analyzed using the ΔΔCT method. The normalized ratio of target mRNA/control Hprt1 in unstimulated and/or uninfected cells was set to 1.
RNA interference in macrophages
Nonsilencing small interfering RNA oligonucleotides (cat. no. 1027281) and small interfering RNA duplexes directed against Hif1α (cat. no. L-04065–01-0005) were purchased from QIAGEN (Hilden, Germany) and Thermo Fisher Scientific (Darmstadt, Germany), respectively. Small interfering RNAwas transferred via electroporation, as described earlier (39, 40).
Nitrite production
Nitrite accumulation in cell supernatants was determined by a Griess reaction, as described earlier (41, 42).
Statistical analysis
Results are expressed as mean + SEM and “n” represents the number of biological samples, analyzed murine tissue specimens, and/or quantified high power fields obtained from independent experiments. Statistical significance was calculated with Prism v6.0 software (GraphPad, La Jolla, CA). Normality distribution was tested with the Kolmogorov–Smirnov test. When comparing two groups, the unpaired two-tailed Student t test and Mann–Whitney U test were used for normally and nonnormally distributed data sets, respectively. When comparing more than two groups, one-way ANOVA, followed by the Tukey multiple-comparison test and the Kruskal–Wallis test, followed by the Dunn multiple-comparison test were used for normally and nonnormally distributed data sets, respectively. The p values < 0.05 were deemed statistically significant (unless indicated otherwise).
Results
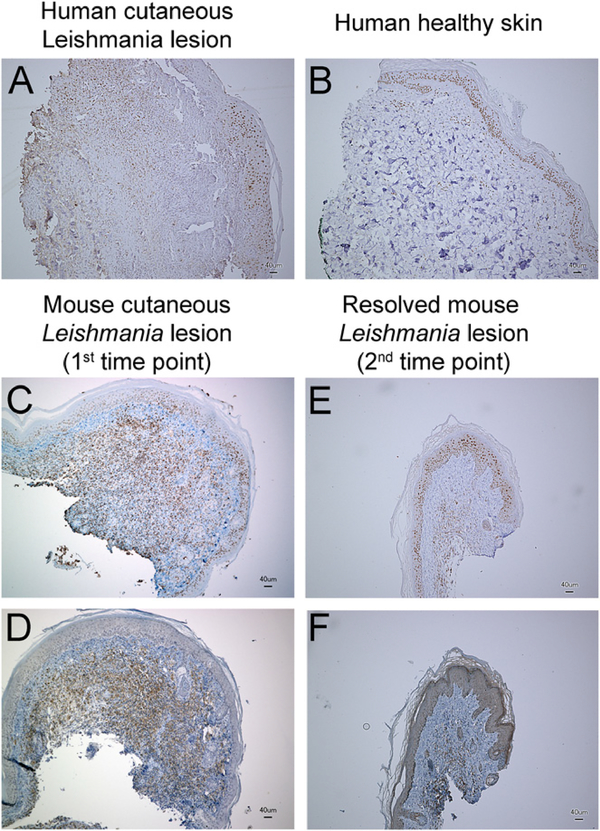
HIF-1α accumulation in cutaneous Leishmania lesions
As the first step, lesions from patients with human cutaneous leishmaniasis were analyzed for the expression of HIF-1α protein. In accordance with earlier observations (43), HIF-1α expression was detectable to comparable extents in the epidermal layers of Leishmania-infected skin and healthy skin. In contrast, elevated HIF-1α protein levels were seen in the dermal infiltrates of Leishmania skin lesions (Fig. 1A), whereas the dermis of uninfected control specimens was HIF-1α negative (Fig. 1B). Next, we assessed whether HIF-1α also accumulates in a mouse model of cutaneous leishmaniasis. Infection of C57BL/6 mice with L. major results in the development of a transient cutaneous lesion (reviewed in Refs. 44–47) (Supplemental Fig. 1). We analyzed the lesional HIF-1α levels and macrophage infiltration when the lesion reached maximum size at 14 d postinfection (first time point). We detected robust lesional HIF-1α accumulation (Fig. 1C) in macrophage-rich dermal and s.c. infiltrates (Fig. 1D). Resolution of the disease (second time point) was paralleled by diminished levels of lesional HIF-1α (Fig. 1E) and reduced numbers of infiltrating macrophages (Fig. 1F). From these findings, we concluded that infection with L. major triggers lesional HIF-1α accumulation in vivo.
FIGURE 1.
Infection with L. major induces HIF-1α accumulation in cutaneous lesions. Human cutaneous Leishmania lesions (A) and uninfected controls (B) were analyzed for HIF-1α expression. A representative staining obtained from five infected patients with confirmed cutaneous leishmaniasis or healthy skin from two patients without cutaneous leishmaniasis is shown. (C–F) C57BL/6 mice were infected with L. major At 14 d postinfection, skin lesions were analyzed for HIF-1α (C) and CD68 (D) expression (a representative staining from three similar independent experiments is shown). At 55 d postinfection, skin lesions were analyzed for HIF-1α (E) and CD68 (F) expression. One of two similar independent experiments is shown.
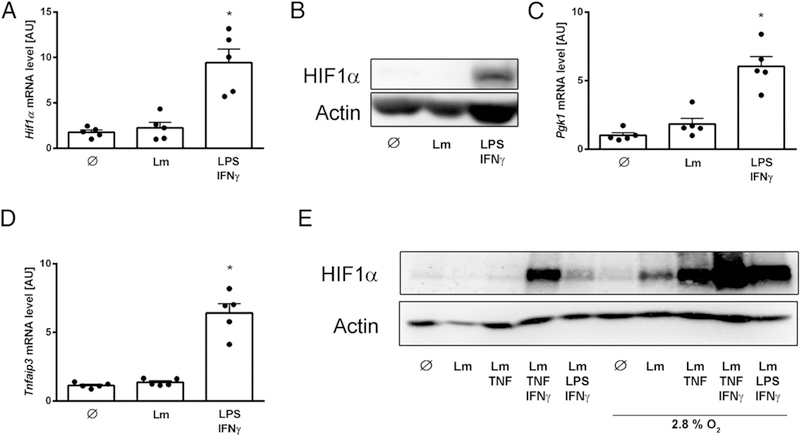
Inflammatory signaling is required for HIF-1α accumulation in macrophages upon infection with L. major
Given that several pathogens and pathogen-derived danger signals are able to induce HIF-1α accumulation in innate immune cells under conditions of ample O2 (reviewed in Refs. 3–5), we analyzed whether infection of macrophages with L. major is sufficient to induce HIF-1α accumulation on its own. Infection of mouse macrophages with L. major was not able to induce Hif1α mRNA (Fig. 2A) or to mediate HIF-1α stabilization under normoxic conditions (Fig. 2B). Accordingly, infection of macrophages with L. major did not promote expression of the HIF-1α target gene Pgk1 (Fig. 2C). In contrast, stimulation of macrophages with LPS/IFN-γ resulted in robust induction of Hif1α mRNA and protein, as well as expression of a glycolytic HIF-1α target gene Pgk1 (Fig. 2A–C). Because inflammatory HIF-1α accumulation under normoxic conditions requires NF-κB activation (reviewed in Refs. 3–5), we tested expression of the NF-κB response gene Tnfaip3 (A20) upon infection of macrophages with L. major, which is known to impair NF-κB activation of macrophages (48–50). We observed that infection of macrophages with L. major did not induce the NF-κB response gene Tnfaip3, whereas stimulation with LPS/IFN-γ resulted in robust Tnfaip3 induction (Fig. 2D). We conclude that infection of macrophages with L. major alone is not sufficient to allow for HIF-1α accumulation, most likely as a result of insufficient NF-κB activation.
FIGURE 2.
Inflammatory signaling and low O2 tension promote HIF-1α accumulation in L. major–infected macrophages. (A–D) Macrophages were left untreated (∅), infected with L. major (Lm), or stimulated with LPS (10 ng/ml) and IFN-γ (20 ng/ml). (A) Hif1α mRNA levels (mean + SEM from five independent experiments). *p < 0.05 versus ∅, ANOVA and the Tukey post hoc test. (B) HIF-1α and actin protein levels (five similar independent experiments). (C) Pgk1 mRNA levels (mean + SEM from five independent experiments). *p < 0.05 versus ∅, Kruskal–Wallis test and the Dunn post hoc test. (D) Tnfaip3 mRNA levels (mean + SEM from five independent experiments). *p < 0.05 versus ∅, ANOVA and the Tukey post hoc test. (E) Macrophages were left untreated (∅), infected with L. major (Lm), or stimulated with TNF (20 ng/ml), TNF/IFN-γ (20 ng/ml), and LPS (10 ng/ml)/IFN-γ under normoxic or 2.8% O2 conditions. HIF-1α and actin protein levels are shown. A representative of two independent experiments is shown.
We hypothesized that signals from the tissue microenvironment, such as the O2 levels found in L. major-infected tissue and/or inflammatory signals, might account for HIF-1α accumulation in macrophages in vivo. Our previous analyses revealed that O2 levels in L. major-infected tissue corresponded to ~2.8% O2 when the L. major skin lesions reach maximum size (26). IFN-γ–dependent (25, 51), TNF-dependent (52), and TLR-dependent (53–55) signals play a key role in macrophage activation and the anti-leishmanial response. We tested whether these factors allow for HIF-1α accumulation in L. major-infected macrophages. Stimulation of L. major-infected macrophages with TNF/IFN-γ or LPS/IFN-γ under conditions of ample O2 promoted robust HIF-1α accumulation.
Incubation of L. major-infected macrophages under the reduced O2 tensions found in infected tissues (2.8% O2) resulted in HIF-1α accumulation but did not augment the induction of the NF-κB response gene Tnfaip3 (Fig. 2E, Supplemental Fig. 2). In the presence of exogenous inflammatory signals, low O2 environments (2.8% O2) enhanced HIF-1α accumulation (Fig. 2E). Moreover, in the context of LPS/IFN-γ costimulation, low O2 levels (2.8% O2) significantly boosted the expression of the NF-κB-response gene Tnfaip3 (Supplemental Fig. 2). From these results, we conclude that inflammatory signals from the tissue microenvironment, rather than L. major itself, drive HIF-1α accumulation in macrophages upon L. major infection in vivo. Moreover, our data demonstrate that reduced atmospheric O2 levels (2.8% O2) cannot induce significant proinflammatory responses in macrophages on their own but require exogenous inflammatory signals.
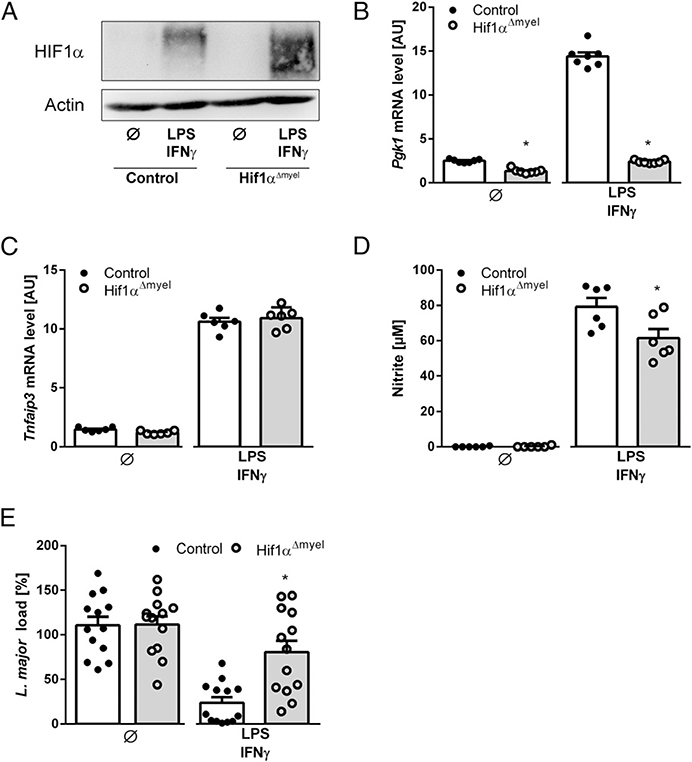
Inflammatory HIF-1α is required for antileishmanial control in macrophages
Given that the antileishmanial activity of cytokine-activated macrophages depends on NOS2 (24, 25) and that NOS2 expression can be regulated by HIF-1α in myeloid cells (12, 28–30), we tested whether inflammatory HIF-1α contributes to the antileishmanial defense of macrophages.
First, we analyzed whether pharmacological stabilization of HIF-1α under normoxic conditions and without exogenous macrophage activation by LPS/IFN-γ was sufficient to promote clearance of intracellular L. major. To this end, we treated L. major-infected macrophages with the lipophilic α-ketoglutarate analog PHD inhibitor ICA (31). ICA stabilized HIF-1α (Fig. 3A) and promoted upregulation of the metabolic HIF-1α-dependent target gene Pgk1 in comparison with vehicle treatment (Fig. 3B). However, ICA treatment on its own did not upregulate expression of the NF-κB response gene Tnfaip3 (Fig. 3C) or induce the production of NO (Fig. 3D). Accordingly, ICA treatment alone did not enhance the antileishmanial activity of macrophages, whereas LPS/IFN-γ was able to do so (Fig. 3E). Interestingly, despite remarkable HIF-1α accumulation due to ICA alone, ICA per se did not amplify Tnfaip3 induction or NO production; subsequently, it did not reduce L. major load in macrophages (Fig. 3). From these data, we conclude that HIF-1α accumulation in the absence of exogenous inflammatory macrophage-activating signals does not promote leishmanicidal activity of macrophages.
FIGURE 3.
HIF-1α stabilization in the absence of inflammatory signals does not promote antileishmanial activity of macrophages. (A) Macrophages were costimulated with LPS (10 ng/ml)/IFN-γ (20 ng/ml) or left unstimulated (∅) under normoxic conditions. Where indicated, cells were treated with ICA (100 μM). HIF-1α and HSP90 protein levels are shown (representative of four similar independent experiments). (B–E) Macrophages were infected with L. major or costimulated with LPS (10 ng/ml)/IFN-γ (20 ng/ml) or left unstimulated (∅) under normoxic conditions. Where indicated, infected cells were treated with ICA (100 μM). (B) Pgk1 mRNA levels (mean + SEM, n = 5 biological samples from two independent experiments). *p < 0.05, versus ∅, ANOVA and the Tukey post hoc test. (C) Tnfaip3 mRNA levels (mean + SEM, n = 6 biological samples from three independent experiments). *p < 0.05 versus ∅, ANOVA and the Tukey post hoc test. (D) Nitrite content of supernatants (mean + SEM, n = 6 biological samples from four independent experiments). *p < 0.05 versus ∅, Mann-Whitney U test. ▼, not detectable. (E) L. major load of macrophages (mean + SEM, n = 9 quantified high power fields from four independent experiments). *p < 0.05 versus ∅ Mann–Whitney U test.
Next, we examined whether LPS/IFN-γ-induced inflammatory HIF-1α accumulation was required for the killing of intracellular Leishmania in macrophages. For that purpose, we silenced HIF-1α in macrophages by using RNA interference, as described earlier (39, 40). Hif1α-specific small interfering RNA effectively abolished HIF-1α protein accumulation in LPS/INF-γ-treated macrophages (Supplemental Fig. 3A). Blunting of HIF-1α impaired LPS/INF-γ-induced NO release and abolished the leishmanicidal activity of macrophages (Supplemental Fig. 3B).
As an alternative approach to address the importance of inflammatory HIF-1α in the antileishmanial response, we used macrophages from Hif1αΔmyel mice. In line with earlier observations (56), immunoblotting demonstrated a truncated HIF-1α protein in macrophages generated from Hif1αΔmyel mice (Fig. 4A). This most likely reflects deletion of the loxP-flanked exons (Fig. 4A), which encode for the dimerization and transactivation domain of HIF-1α (34). In macrophages derived from Hif1α-deficient mice (Hif1αΔmyel), LPS/INF-γ-induced upregulation of the HIF-1α target gene Pgk1 (Fig. 4B) was abolished. In line with earlier observations (30), inflammatory HIF-1α signaling in macrophages did not affect the induction of the NF-κB response gene Tnfaip3 (Fig. 4C). However, LPS/INF-γ–induced NO release was diminished (Fig. 4D), which was paralleled by significant impairment of antileishmanial macrophage activity (Fig. 4E).
FIGURE 4.
Inflammatory HIF-1α stabilization promotes antileishmanial activity of macrophages. (A–E) Macrophages from Hif1αΔmyel and controls were infected with L. major and costimulated with LPS (10 ng/ml)/IFN-γ (20 ng/ml) or left unstimulated (∅) under normoxic conditions. (A) HIF-1α and actin protein levels (representative of three similar independent experiments). (B) Pgk1 mRNA levels (mean + SEM, n = 7 biological samples from three independent experiments). *p < 0.01 versus control, Student t test. (C) Tnfaip3 mRNA levels (mean + SEM, n = 6 biological samples from two independent experiments). *p < 0.01 versus control, Student t test. (D) Nitrite content of supernatants (mean + SEM from six independent experiments). *p < 0.05 versus control, Student t test or Mann–Whitney U test. (E) L. major load of macrophages (mean + SEM, n =13 quantified high power fields from seven independent experiments). *p < 0.05 versus control, Mann–Whitney U test.
From these data, we conclude that HIF-1α stabilization in the absence of a proinflammatory macrophage-activating signal is insufficient to allow for production of leishmanicidal NO. However, in the context of classical macrophage activation, inflammatory HIF-1α is required for high-level NO production and for induction of a robust leishmanicidal activity.
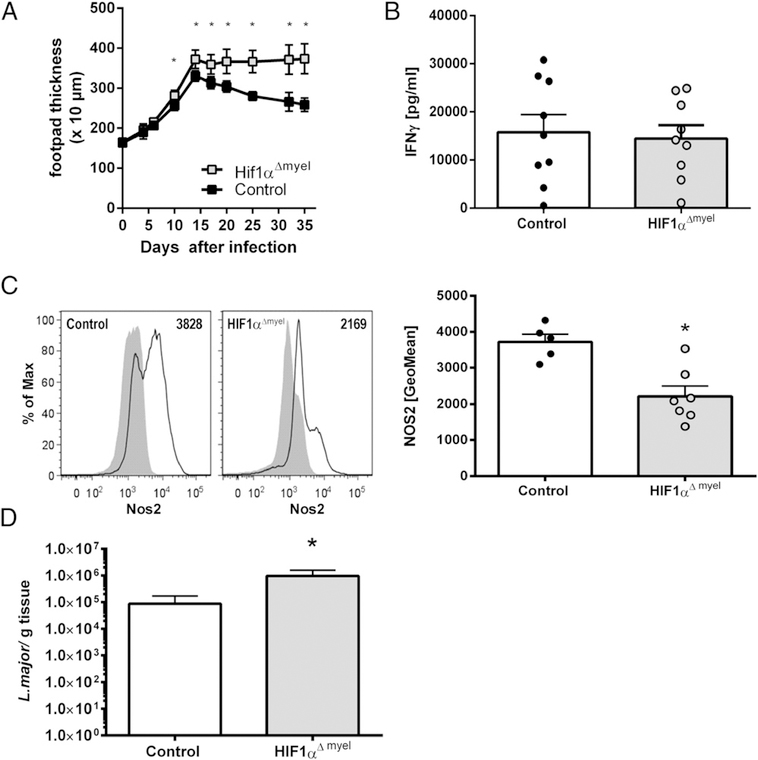
Myeloid cell-specific ablation of HIF-1α impairs cutaneous antileishmanial control
Based on the findings described above, we hypothesized that HIF-1α in myeloid cells might also contribute to the control of L. major infection in vivo. Therefore, we infected Hif1αΔmyel mice and littermate controls with L. major. They showed comparable development of cutaneous lesions during the first 2 wk postinfection; however, the lesion sizes in the control animals decreased steadily thereafter, whereas Hif1αΔmyel mice showed a non-resolving course of infection (Fig. 5A). Restimulation of draining lymph node cells with soluble Leishmania Ag demonstrated that deficiency of HIF-1α in myeloid cells did not affect the Leishmania-specific IFN-γ T cell responses (Fig. 5B). In contrast, expression of NOS2 protein by CD11b+ myeloid cells from skin lesions of Hif1αΔmyel mice was diminished compared with littermate controls (Fig. 5C). This was paralleled by an increase in the parasite load in the infected cutaneous lesion compared with littermate controls (Fig. 5D). From these data, we conclude that HIF-1α in myeloid cells plays an important role in controlling cutaneous L. major infection in vivo.
FIGURE 5.
HIF-1α stabilization in myeloid cells contributes to antileishmanial control in vivo. (A–D) Hif1αΔmyel mice and littermates (controls) were infected with L. major in their hind footpads. (A) Clinical course of cutaneous L. major infection (mean ± 95% confidence interval, n ≥ 3, representative of three similar independent experiments). *p < 0.01, Student t test or Mann–Whitney U test. (B) At day 28–29 postinfection, restimulation of draining lymph node cells from L. major–infected mice with soluble Leishmania Ag was performed. IFN-γ was determined in the culture supernatants (mean + SEM, n = 9 biological samples from two independent experiments). Student t test was performed and showed no significant difference. (C) At day 29 postinfection, NOS2 protein expression was determined in lesional CD11b+ cells from Hif1αΔmyel mice and littermates (control). Representative line graphs of NOS2 expression in lesional CD11b+ cells (left panels). Black line: NOS2 expression. Shaded area: isotype control. Geometric mean fluorescence of NOS2 (mean + SEM, n = 5–7) (right panel). A representative of two independent experiments is shown. *p < 0.05, Student t test. (D) At day 32 postinfection, L. major burden in skin lesion of infected mice was analyzed (mean + SEM, n = 8). A representative of two similar independent experiments is shown. *p < 0.05 Mann–Whitney U test.
Discussion
In this study, we demonstrated that HIF-1α is present in the macrophage-rich cutaneous Leishmania lesions of mice and humans. We further show that HIF-1α expression by myeloid cells contributes to the control of L. major parasites in vitro and in vivo. Our results extend earlier findings in mice infected with L. amazonensis (a causative agent of chronic nonhealing cutaneous leishmaniasis) or L. donovani (which causes visceral leishmaniasis), in which an accumulation of HIF-1α in the skin lesions (57) or parasitized spleens was noted (20).
Importantly, although the function of HIF-1α was not analyzed in L. amazonensis–infected mice (21, 22, 57), it appeared to be rather detrimental for the host immune response in L. donovani–infected mice (20). This contrasts with our observations obtained from self-healing cutaneous leishmaniasis of L. major–infected mice (this study). However, similar to our findings earlier reports established a critical role of myeloid cell-derived HIF1α in the defense against various bacterial pathogens including Streptococcus pyogenes (11, 12), Pseudomonas aeruginosa (13), Mycobacterium avium (14), and M. tuberculosis (58).
Infection of macrophages with L. major alone was not sufficient to promote HIF-1α accumulation in vitro; it required additional exogenous inflammatory signals, such as costimulation with LPS/IFN-γ or TNF/IFN-γ. In line with this, Hammami et al. (20) observed that in vivo HIF-1α accumulation in DCs was not directly elicited by L. donovani parasites but was secondary to IRF5-mediated signaling in CD11c+ cells. In other studies, infection of macrophages with L. donovani or L. amazonensis per se resulted in HIF-1α accumulation under normoxic conditions, and L. donovani or L. amazonensis was required for pathogen survival within the host cell (19, 59). Given that Leishmania species differ greatly in their metabolism (60, 61) and that HIF-1α plays an important role in reprogramming the metabolism of macrophages (reviewed in Refs. 62, 63), it is tempting to speculate that certain Leishmania species, such as L. donovani or L. amazonensis, require host cell HIF-1α to fuel their metabolic demands. In contrast, L. major’s metabolic requirements might even be met in the absence of HIF-1α signaling in macrophages. However, further studies are required to understand the divergent role of HIF-1α in macrophages infected with different Leishmania species.
Although L. major does not induce HIF-1α on its own, our data suggest that the context of HIF-1α induction is critical for its biological effect. Despite the fact that inflammatory HIF-1α accumulation promotes the production of NO and the leishmanicidal activity of macrophages, pharmacological HIF-1α stabilization with the PHD inhibitor ICA in the absence of inflammatory macrophage activation was not sufficient to induce NO production and did not exert antileishmanial activity in macrophages. In contrast to our findings, pharmacological HIF-1α stabilization helped to contain Streptococcus pyogenes–infected and M. tuberculosis–infected phagocytes (58, 64). However, unlike S. pyogenes and M. tuberculosis, L. major is a silent intruder that is able to shut down inflammatory responses, including NF-κB activation (48–50). Hence, in the absence of inflammatory signaling, canonical hypoxia-induced HIF-1α stabilization did not significantly enhance the expression of inflammatory genes, including Nos2 (30). Nevertheless, for instance, in the context of mycobacterial cord factor– or LPS-mediated activation of mononuclear phagocytes, HIF-1α promoted the expression of NOS2 and other inflammatory genes (30, 56). Consistent with this finding, our results demonstrate that LPS/IFN-γ costimulation required HIF-1α to establish high levels of NO production and leishmanicidal activity. This further supports the idea that the context of HIF-1α activation critically affects its function.
In a previous study, we demonstrated that, at the time point of maximal skin lesion sizes, O2 tension in the infected cutaneous tissues dropped to levels that impaired O2-dependent NO production and leishmanicidal activity of LPS/INF-γ-costimulated macrophages (26). Normalization of tissue O2 levels was paralleled by cure of the disease (26). After 14 days postinfection, when the size of the leishmanial lesions reached their maximum size and skin O2 levels reached their lowest point, tissue O2 tension of the leishmanial lesions started to increase steadily (26). At day 29 postinfection, tissue O2 levels allowed for substantial leishmanicidal activity of activated macrophages resulting in a reduced cutaneous parasite burden (26). In the current study, we analyzed the effect of HIF-1α in myeloid cells in vivo around day 29 postinfection. The cutaneous burden of L. major in control animals was of the same order of magnitude as the number of L. major parasites in the skin lesions obtained in the previous study (32). However, we noted increased parasite load at the site of infection and decreased NOS2 expression in lesional myeloid cells from Hif1αΔmyel mice. Moreover, the antileishmanial activity of Hif1α-deficient macrophages under normoxic conditions was impaired in vitro and was associated with impaired NO production. In summary, our data suggest that, in cutaneous L. major infection, HIF-1α plays a key role in arming the macrophages with the antileishmanial effector enzyme NOS2, whereas a sufficient supply of molecular O2 as a cosubstrate of NOS2 is required for the production of high levels of NO (6–67).
In addition to the indirect antimicrobial actions of HIF-1α that are exerted via its targets NOS2 [this study and (58)] and cathelicidin (12), HIF-1α expression in myeloid cells might have immunoregulatory functions in infectious diseases. For instance, in mouse models of Histoplasma capsulatum infection, HIF-1α suppressed the production of IL-10 and, thereby, helped to fight the infection (68). Moreover, infection of mice with Helicobacter pylori resulted in HIF-1α accumulation in myeloid cells, which was not required for H. pylori elimination by phagocytes but was required for termination of tissue inflammation. The mechanism by which myeloid cell-derived HIF-1α contributes to resolution in this model remains to be determined (69). Although our data suggest that HIF-1α deficiency in myeloid cells results in impaired leishmanicidal activity in vivo, largely as a result of impaired induction of Nos2 in lesional macrophages, further studies are needed to investigate whether other Hif1α-regulated targets, such as vascular endothelial growth factor A (70), contribute to the control of Leishmania parasites in the skin.
Supplementary Material
Acknowledgments
We thank Kirstin Castiglione, Vincent Klump, and Monika Nowottny for technical assistance.
J.J. and C.B. were supported by grants from the Deutsche Forschungsgemeinschaft (JA 2-1 and SFB 1181, project C4) and the Interdisciplinary Center for Clinical Research of the Medical Faculty of the Friedrich-Alexander-Universität Erlangen-Nürnberg (project A61).
Abbreviations used in this article
- BM-MΦ
mouse bone marrow–derived macrophage
- cat.
catalog
- HUF-1α
hypoxia-inducible factor-1α
- ICA
2-(1-chloro-4-hydroxyisoquinoline-3-carboxamido) acetate
- NOS2
type 2 NO synthase
- Pgk1
phosphoglycerate kinase 1
- PHD
prolyl hydroxylase domain enzyme
Footnotes
Disclosures
The authors have no financial conflicts of interest.
The online version of this article contains supplemental material.
References
- 1.Semenza GL 2012. Hypoxia-inducible factors in physiology and medicine. Cell 148: 399–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaelin WG Jr., and Ratcliffe PJ 2008. Oxygen sensing by metazoans: the central role of the HIF hydroxylase pathway. Mol. Cell 30: 393–402. [DOI] [PubMed] [Google Scholar]
- 3.Dehne N, and Brüne B 2009. HIF-1 in the inflammatory microenvironment. Exp. Cell Res 315: 1791–1797. [DOI] [PubMed] [Google Scholar]
- 4.Palazon A, Goldrath AW, Nizet V, and Johnson RS 2014. HIF transcription factors, inflammation, and immunity. Immunity 41: 518–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jantsch J, and Schödel J 2015. Hypoxia and hypoxia-inducible factors in myeloid cell-driven host defense and tissue homeostasis. Immunobiology 220: 305–314. [DOI] [PubMed] [Google Scholar]
- 6.Werth N, Beerlage C, Rosenberger C, Yazdi AS, Edelmann M, Amr A, Bernhardt W, von Eiff C, Becker K, Schäfer A, et al. 2010. Activation of hypoxia inducible factor 1 is a general phenomenon in infections with human pathogens. PLoS One 5: e11576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frede S, Stockmann C, Freitag P, and Fandrey J 2006. Bacterial lipopolysaccharide induces HIF-1 activation in human monocytes via p44/42 MAPK and NF-kappaB. Biochem. J 396: 517–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tannahill GM, Curtis AM, Adamik J, Palsson-McDermott EM, McGettrick AF, Goel G, Frezza C, Bernard NJ, Kelly B, Foley NH, et al. 2013. Succinate is an inflammatory signal that induces IL-1β through HIF-1α. Nature 496: 238–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Siegert I, Schödel J, Nairz M, Schatz V, Dettmer K, Dick C, Kalucka J, Franke K, Ehrenschwender M, Schley G, et al. 2015. Ferritin-mediated iron sequestration stabilizes hypoxia-inducible factor-1α upon LPS activation in the presence of ample oxygen. Cell Rep. 13: 2048–2055. [DOI] [PubMed] [Google Scholar]
- 10.Rius J, Guma M, Schachtrup C, Akassoglou K, Zinkernagel AS, Nizet V, Johnson RS, Haddad GG, and Karin M 2008. NF-kappaB links innate immunity to the hypoxic response through transcriptional regulation of HIF-1alpha. Nature 453: 807–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cramer T, Yamanishi Y, Clausen BE, Förster I, Pawlinski R, Mackman N, Haase VH, Jaenisch R, Corr M, Nizet V, et al. 2003. HIF-1alpha is essential for myeloid cell-mediated inflammation. Cell 112: 645–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peyssonnaux C, Datta V, Cramer T, Doedens A, Theodorakis EA, Gallo RL, Hurtado-Ziola N, Nizet V, and Johnson RS 2005. HIF-1alpha expression regulates the bactericidal capacity of phagocytes. J. Clin. Invest 115: 1806–1815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berger EA, McClellan SA, Vistisen KS, and Hazlett LD 2013. HIF-1α is essential for effective PMN bacterial killing, antimicrobial peptide production and apoptosis in Pseudomonas aeruginosa keratitis. PLoS Pathog. 9: e1003457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cardoso MS, Silva TM, Resende M, Appelberg R, and Borges M 2015. Lack of the transcription factor hypoxia-inducible factor 1α (HIF-1α) in macrophages accelerates the necrosis of Mycobacterium avium-induced granulomas. Infect. Immun. 83: 3534–3544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shepardson KM, Jhingran A, Caffrey A, Obar JJ, Suratt BT, Berwin BL, Hohl TM, and Cramer RA 2014. Myeloid derived hypoxia inducible factor 1-alpha is required for protection against pulmonary Aspergillus fumigatus infection. PLoS Pathog. 10: e1004378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cheng SC, Quintin J, Cramer RA, Shepardson KM, Saeed S, Kumar V, Giamarellos-Bourboulis EJ, Martens JH, Rao NA, Aghajanirefah A, et al. 2014. mTOR- and HIF-1α-mediated aerobic glycolysis as metabolic basis for trained immunity. [Published erratum appears in 2014 Science 346: aaa1503.] Science 345: 1250684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Metheni M, Echebli N, Chaussepied M, Ransy C, Chéreau C, Jensen K, Glass E, Batteux F, Bouillaud F, and Langsley G 2014. The level of H2O2 type oxidative stress regulates virulence of Theileria-transformed leukocytes. Cell. Microbiol 16: 269–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wiley M, Sweeney KR, Chan DA, Brown KM, McMurtrey C, Howard EW, Giaccia AJ, and Blader IJ 2010. Toxoplasma gondii activates hypoxia-inducible factor (HIF) by stabilizing the HIF-1alpha subunit via type I activin-like receptor kinase receptor signaling. J. Biol. Chem 285: 26852–26860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Singh AK, Mukhopadhyay C, Biswas S, Singh VK, and Mukhopadhyay CK 2012. Intracellular pathogen Leishmania donovani activates hypoxia inducible factor-1 by dual mechanism for survival advantage within macrophage. PLoS One 7: e38489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hammami A, Charpentier T, Smans M, and Stäger S 2015. IRF-5-mediated inflammation limits CD8+ T cell expansion by inducing HIF-1α and impairing dendritic cell functions during Leishmania infection. PLoS Pathog. 11: e1004938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Araújo AP, Arrais-Silva WW, and Giorgio S 2012. Infection by Leishmania amazonensis in mice: a potential model for chronic hypoxia. Acta Histochem. 114: 797–804. [DOI] [PubMed] [Google Scholar]
- 22.Araujo VC, Fukutani KF, Oshiro ET, Rodrigues PO, Rizk YS, Carollo CA, and Arruda CC 2015. Hairless mice as an experimental model of infection with Leishmania (Leishmania) amazonensis. Exp. Parasitol 157: 138–144. [DOI] [PubMed] [Google Scholar]
- 23.Lemaire J, Mkannez G, Guerfali FZ, Gustin C, Attia H, Sghaier RM, Dellagi K, Laouini D, and Renard P, Sysco-Consortium. 2013. MicroRNA expression profile in human macrophages in response to Leishmania major infection. PLoS Negl. Trop. Dis 7: e2478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liew FY, Millott S, Parkinson C, Palmer RM, and Moncada S 1990. Macrophage killing of Leishmania parasite in vivo is mediated by nitric oxide from L-arginine. J. Immunol. 144: 4794–4797. [PubMed] [Google Scholar]
- 25.Diefenbach A, Schindler H, Donhauser N, Lorenz E, Laskay T, MacMicking J, Röllinghoff M, Gresser I, and Bogdan C 1998. Type 1 interferon (IFNalpha/beta) and type 2 nitric oxide synthase regulate the innate immune response to a protozoan parasite. Immunity 8: 77–87. [DOI] [PubMed] [Google Scholar]
- 26.Mahnke A, Meier RJ, Schatz V, Hofmann J, Castiglione K, Schleicher U, Wolfbeis OS, Bogdan C, and Jantsch J 2014. Hypoxia in Leishmania major skin lesions impairs the NO-dependent leishmanicidal activity of macrophages. J. Invest. Dermatol 134: 2339–2346. [DOI] [PubMed] [Google Scholar]
- 27.Schleicher U, Paduch K, Debus A, Obermeyer S, König T, Kling JC, Ribechini E, Dudziak D, Mougiakakos D, Murray PJ, et al. 2016. TNF-mediated restriction of arginase 1 expression in myeloid cells triggers type 2 NO synthase activity at the site of infection. Cell Rep. 15: 1062–1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Melillo G, Taylor LS, Brooks A, Musso T, Cox GW, and Varesio L 1997. Functional requirement of the hypoxia-responsive element in the activation of the inducible nitric oxide synthase promoter by the iron chelator desferrioxamine. J. Biol. Chem 272: 12236–12243. [DOI] [PubMed] [Google Scholar]
- 29.Melillo G, Musso T, Sica A, Taylor LS, Cox GW, and Varesio L 1995. A hypoxia-responsive element mediates a novel pathway of activation of the inducible nitric oxide synthase promoter. J. Exp. Med 182: 1683–1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jantsch J, Wiese M, Schödel J, Castiglione K, Gläsner J, Kolbe S, Mole D, Schleicher U, Eckardt KU, Hensel M, et al. 2011. Toll-like receptor activation and hypoxia use distinct signaling pathways to stabilize hypoxia-inducible factor 1α (HIF1A) and result in differential HIF1A-dependent gene expression. J. Leukoc. Biol 90: 551–562. [DOI] [PubMed] [Google Scholar]
- 31.Schley G, Klanke B, Schödel J, Kröning S, Türkoglu G, Beyer A, Hagos Y, Amann K, Burckhardt BC, Burzlaff N, et al. 2012. Selective stabilization of HIF-1α in renal tubular cells by 2-oxoglutarate analogues. Am. J. Pathol 181: 1595–1606. [DOI] [PubMed] [Google Scholar]
- 32.Solbach W, Forberg K, Kammerer E, Bogdan C, and Röllinghoff M 1986. Suppressive effect of cyclosporin A on the development of Leishmania tropica-induced lesions in genetically susceptible BALB/c mice. J. Immunol 137: 702–707. [PubMed] [Google Scholar]
- 33.Stenger S, Donhauser N, Thuring H, Röllinghoff M, and Bogdan C 1996. Reactivation of latent leishmaniasis by inhibition of inducible nitric oxide synthase. J. Exp. Med 183: 1501–1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ryan HE, Poloni M, McNulty W, Elson D, Gassmann M, Arbeit JM, and Johnson RS 2000. Hypoxia-inducible factor-1alpha is a positive factor in solid tumor growth. Cancer Res. 60: 4010–4015. [PubMed] [Google Scholar]
- 35.Clausen BE, Burkhardt C, Reith W, Renkawitz R, and Förster I 1999. Conditional gene targeting in macrophages and granulocytes using LysMcre mice. Transgenic Res. 8: 265–277. [DOI] [PubMed] [Google Scholar]
- 36.Weigert A, Weichand B, Sekar D, Sha W, Hahn C, Mora J, Ley S, Essler S, Dehne N, and Brune B 2012. HIF-1α is a negative regulator of plasmacytoid DC development in vitro and in vivo. Blood 120: 3001–3006. [DOI] [PubMed] [Google Scholar]
- 37.Roda JM, Sumner LA, Evans R, Phillips GS, Marsh CB, and Eubank TD 2011. Hypoxia-inducible factor-2α regulates GM-CSF-derived soluble vascular endothelial growth factor receptor 1 production from macrophages and inhibits tumor growth and angiogenesis. J. Immunol 187: 1970–1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schleicher U, and Bogdan C 2009. Generation, culture and flow-cytometric characterization of primary mouse macrophages. Methods Mol. Biol 531: 203–224. [DOI] [PubMed] [Google Scholar]
- 39.Siegert I, Schatz V, Prechtel AT, Steinkasserer A, Bogdan C, and Jantsch J 2014. Electroporation of siRNA into mouse bone marrow-derived macrophages and dendritic cells. Methods Mol. Biol 1121: 111–119. [DOI] [PubMed] [Google Scholar]
- 40.Wiese M, Castiglione K, Hensel M, Schleicher U, Bogdan C, and Jantsch J 2010. Small interfering RNA (siRNA) delivery into murine bone marrow-derived macrophages by electroporation. J. Immunol. Methods 353: 102–110. [DOI] [PubMed] [Google Scholar]
- 41.Vodovotz Y, Bogdan C, Paik J, Xie QW, and Nathan C 1993. Mechanisms of suppression of macrophage nitric oxide release by transforming growth factor beta. J. Exp. Med 178: 605–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ding AH, Nathan CF, and Stuehr DJ 1988. Release of reactive nitrogen intermediates and reactive oxygen intermediates from mouse peritoneal macrophages. Comparison of activating cytokines and evidence for independent production. J. Immunol 141: 2407–2412. [PubMed] [Google Scholar]
- 43.Peyssonnaux C, Boutin AT, Zinkernagel AS, Datta V, Nizet V, and Johnson RS 2008. Critical role of HIF-1alpha in keratinocyte defense against bacterial infection. J. Invest. Dermatol 128: 1964–1968. [DOI] [PubMed] [Google Scholar]
- 44.Sacks D, and Noben-Trauth N 2002. The immunology of susceptibility and resistance to Leishmania major in mice. Nat. Rev. Immunol 2: 845–858. [DOI] [PubMed] [Google Scholar]
- 45.Mougneau E, Bihl F, and Glaichenhaus N 2011. Cell biology and immunology of Leishmania. Immunol. Rev 240: 286–296. [DOI] [PubMed] [Google Scholar]
- 46.Olekhnovitch R, and Bousso P 2015. Induction, propagation, and activity of host nitric oxide: lessons from Leishmania infection. Trends Parasitol. 31: 653–664. [DOI] [PubMed] [Google Scholar]
- 47.Kaye P, and Scott P 2011. Leishmaniasis: complexity at the host-pathogen interface. Nat. Rev. Microbiol 9: 604–615. [DOI] [PubMed] [Google Scholar]
- 48.Ghosh S, Bhattacharyya S, Sirkar M, Sa GS, Das T, Majumdar D, Roy S, and Majumdar S 2002. Leishmania donovani suppresses activated protein 1 and NF-kappaB activation in host macrophages via ceramide generation: involvement of extracellular signal-regulated kinase. Infect. Immun 70: 6828–6838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gregory DJ, Godbout M, Contreras I, Forget G, and Olivier M 2008. A novel form of NF-kappaB is induced by Leishmania infection: involvement in macrophage gene expression. Eur. J. Immunol 38: 1071–1081. [DOI] [PubMed] [Google Scholar]
- 50.Ben-Othman R,Guizani-Tabbane L, and Dellagi K 2008. Leishmania initially activates but subsequently down-regulates intracellular mitogen-activated protein kinases and nuclear factor-kappaB signaling in macrophages. Mol. Immunol. 45: 3222–3229. [DOI] [PubMed] [Google Scholar]
- 51.Wang ZE, Reiner SL, Zheng S, Dalton DK, and Locksley RM 1994. CD4+ effector cells default to the Th2 pathway in interferon gamma-deficient mice infected with Leishmania major J. Exp. Med 179: 1367–1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wilhelm P, Ritter U, Labbow S, Donhauser N, Röllinghoff M, Bogdan C, and Korner H 2001. Rapidly fatal leishmaniasis in resistant C57BL/6 mice lacking TNF. J. Immunol 166: 4012–4019. [DOI] [PubMed] [Google Scholar]
- 53.Muraille E, De Trez C, Brait M, De Baetselier P, Leo O, and Carlier Y 2003. Genetically resistant mice lacking MyD88-adapter protein display a high susceptibility to Leishmania major infection associated with a polarized Th2 response. J. Immunol 170: 4237–4241. [DOI] [PubMed] [Google Scholar]
- 54.Kropf P, Freudenberg MA, Modolell M, Price HP, Herath S, Antoniazi S, Galanos C, Smith DF, and Müller I 2004. Toll-like receptor 4 contributes to efficient control of infection with the protozoan parasite Leishmania major. Infect. Immun 72: 1920–1928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liese J, Schleicher U, and Bogdan C 2007. TLR9 signaling is essential for the innate NK cell response in murine cutaneous leishmaniasis. Eur. J. Immunol 37: 3424–3434. [DOI] [PubMed] [Google Scholar]
- 56.Schoenen H, As J Jantsch B Lepenies V. Bronte, and Lang R 2014. Differential control of Mincle-dependent cord factor recognition and macrophage responses by the transcription factors C/EBPβ and HIF1α. J. Immunol 193: 3664–3675. [DOI] [PubMed] [Google Scholar]
- 57.Arrais-Silva WW, Paffaro VA Jr., Yamada AT, and Giorgio S 2005. Expression of hypoxia-inducible factor-1alpha in the cutaneous lesions of BALB/c mice infected with Leishmania amazonensis. Exp. Mol. Pathol 78: 49–54. [DOI] [PubMed] [Google Scholar]
- 58.Braverman J, Sogi KM, Benjamin D, Nomura DK, and Stanley SA 2016. HIF-1α is an essential mediator of IFN-γ-dependent immunity to mycobacterium tuberculosis. J. Immunol 197: 1287–1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Degrossoli A, Bosetto MC, Lima CB, and Giorgio S 2007. Expression of hypoxia-inducible factor 1alpha in mononuclear phagocytes infected with Leishmania amazonensis. Immunol. Lett 114: 119–125. [DOI] [PubMed] [Google Scholar]
- 60.Westrop GD, Williams RA, Wang L, Zhang T, Watson DG, Silva AM, and Coombs GH 2015. Metabolomic analyses of Leishmania reveal multiple species differences and large differences in amino acid metabolism. PLoS One 10: e0136891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhang WW, McCall LI, and Matlashewski G 2013. Role of cytosolic glyceraldehyde-3-phosphate dehydrogenase in visceral organ infection by Leishmania donovani. Eukaryot. Cell 12: 70–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.O’Neill LA, and Pearce EJ 2016. Immunometabolism governs dendritic cell and macrophage function. J. Exp. Med 213: 15–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ganeshan K, and Chawla A 2014. Metabolic regulation of immune responses. Annu. Rev. Immunol 32: 609–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zinkernagel AS, Peyssonnaux C, Johnson RS, and Nizet V 2008. Pharmacologic augmentation of hypoxia-inducible factor-1alpha with mimosine boosts the bactericidal capacity of phagocytes. J. Infect. Dis 197: 214–217. [DOI] [PubMed] [Google Scholar]
- 65.Albina JE, Henry WL Jr., Mastrofrancesco B, Martin BA, and Reichner JS 1995. Macrophage activation by culture in an anoxic environment. J. Immunol 155: 4391–4396. [PubMed] [Google Scholar]
- 66.Wiese M, Gerlach RG, Popp I, Matuszak J, Mahapatro M, Castiglione K, Chakravortty D, Willam C, Hensel M, Bogdan C, and Jantsch J 2012. Hypoxia-mediated impairment of the mitochondrial respiratory chain inhibits the bactericidal activity of macrophages. Infect. Immun 80: 1455–1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Robinson MA, Tuttle SW, Otto CM, and Koch CJ 2010. pO(2)-dependent NO production determines OPPC activity in macrophages. Free Radic. Biol. Med 48: 189–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fecher RA, Horwath MC, Friedrich D, Rupp J, and Deepe GS Jr. 2016. Inverse correlation between IL-10 and HIF-1α in macrophages infected with Histoplasma capsulatum. J. Immunol 197: 565–579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Matak P, Heinis M, Mathieu JR, Corriden R, Cuvellier S, Delga S, Mounier R, Rouquette A, Raymond J, Lamarque D, et al. 2015. Myeloid HIF-1 is protective in Helicobacter pylori-mediated gastritis. J. Immunol 194: 3259–3266. [DOI] [PubMed] [Google Scholar]
- 70.Weinkopff T, Konradt C, Christian DA, Discher DE, Hunter CA, and Scott P 2016. Leishmania major infection-induced VEGF-A/VEGFR-2 signaling promotes lymphangiogenesis that controls disease. J. Immunol 197: 1823–1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.