Abstract
Purpose
There is ambiguity in the clinical and research communities regarding whether children with mild bilateral hearing loss (MBHL) are at risk for delays. The goal of the current article is to expand the evidence base surrounding outcomes for the current generation of children with MBHL.
Method
Using independent-samples t tests, we compared children with MBHL to same-age peers with normal hearing (NH) on measures of vocabulary, morphological awareness, listening comprehension, and reading. We completed regression analyses to explore the foundational linguistic skills that influenced reading abilities in both groups. For the children with MBHL, we examined whether hearing aid (HA) dosage was associated with individual differences in language scores.
Results
Group comparisons indicated that children with NH significantly outperformed children with MBHL on tests of morphological awareness and listening comprehension. There were no differences in vocabulary size or reading achievement; however, children with MBHL displayed significant differences in the factors that accounted for variability in reading scores compared to children with NH. HA dosage was significantly associated with variation in listening comprehension scores, but not vocabulary, reading, or morphological awareness.
Conclusions
The current results provide evidence that children with MBHL are at risk for persistent language deficits by 4th grade, particularly in aspects of language that involve form. Reading skills in children with MBHL appear to be commensurate with same-age hearing peers. Consistent use of well-fit HAs supports listening comprehension, although the amount of benefit from HAs may be reduced for children with higher unaided hearing levels.
Congenital hearing loss is the most common health condition that can be diagnosed at birth. Children with mild hearing loss make up approximately one third of children with hearing loss (Fitzpatrick, Durieux-Smith, & Whittingham, 2010). While the risks of communication delays for children with bilateral sensorineural hearing loss of moderate or greater degree are well established (Ching et al., 2013), disagreement exists in the field about whether mild bilateral hearing loss (MBHL; defined here as better-ear pure-tone average [BEPTA] greater than 15 dB and less than 45 dB) carries developmental risks. Researchers have proposed that MBHL represents an overdiagnosis of hearing loss (Carew et al., 2018), whereas other studies have shown MBHL can lead to cascading developmental deficits that affect communication outcomes in early elementary grades (Walker, Holte, et al., 2015). The primary purpose of the current study is to expand the evidence base regarding the developmental risk that may occur in cases of children with bilateral hearing loss who have substantial amounts of residual hearing. The secondary purpose is to examine how hearing aid (HA) dosage (i.e., the combined effect of HA use and aided and unaided hearing levels) impacts language and reading outcomes.
There is a fairly extensive literature examining outcomes of children with MBHL. Studies describing children with mild hearing loss relative to normative scores on standardized tests generally show mean language and literacy scores within the average range based on normative samples (Blair, Peterson, & Viehwig, 1985; Đoković et al., 2014; Tomblin, Oleson, Ambrose, Walker, & Moeller, 2018; Walker, Holte, et al., 2015), leading one to conclude that MBHL does not represent a disabling condition. As pointed out in multiple publications, however, reliance on norm-referenced scores may overestimate performance for children who are hard of hearing (Moeller, Tomblin, & OCHL Collaboration, 2015; Werfel & Douglas, 2017). Thus, many studies have included a hearing control group, matched on factors such as age, grade, and/or socioeconomic status (SES), to better characterize outcomes of children with MBHL relative to their achievement potential (Bess, Dodd-Murphy, & Parker, 1998; Blair et al., 1985; Carew et al., 2018; Đoković et al., 2014; Fitzpatrick, Durieux-Smith, Gaboury, Coyle, & Whittingham, 2015; Porter, Sladen, Ampah, Rothpletz, & Bess, 2013; Wake et al., 2006).
Findings comparing children with MBHL to hearing peers have been mixed. Several studies have found no differences between these groups on various outcome measures. Wake et al. (2006) compared 55 school-age children with slight or mild hearing loss to a group of age- and IQ-matched peers and found no significant differences in language or literacy. None of the children with MBHL used HAs at the time of testing. Based on these results, Wake et al. concluded that children with mild hearing loss and normal intelligence are not adversely affected by reduced auditory access. Fitzpatrick et al. (2015) examined 24 children with MBHL and 45 age- and SES-matched children with normal hearing (NH) at 12, 24, 36, and 48 months. Consistent with Wake et al., they did not find significant between-groups differences on parent report language measures. Fitzpatrick et al. noted that reduced hearing could have a negative impact on language outcomes, but early identification, intervention, and amplification may minimize or eliminate any achievement gaps early in development, allowing children with MBHL to be effectively caught up to peers by school entry. Fitzpatrick et al. acknowledged, however, that they lacked a group of children who were later identified and did not receive intervention, which precluded their ability to make definitive conclusions regarding the effects of clinical management on outcomes. Carew et al. (2018) did not find significant differences between 5- and 8-year-old children with MBHL who were early identified and hearing peers on standardized receptive and expressive language measures after adjusting for SES, English as a second language, sex, and nonverbal IQ, but their sample only included nine children with MBHL who were early identified.
In contrast to the nonsignificant findings by Wake et al. (2006), Fitzpatrick et al. (2015), and Carew et al. (2018), other studies have indicated that mild hearing loss can adversely affect developmental outcomes. Blair et al. (1985) found significantly lower scores on standardized academic tests for children with MBHL in first through fourth grade compared to hearing peers in their classes. Bess et al. (1998) reported that 37% of children with minimal hearing loss (MBHL and unilateral hearing loss combined) had failed at least one grade. In more recent reports, Porter et al. (2013) showed that children with minimal hearing loss (MBHL and unilateral hearing loss combined) scored more poorly on teacher report measures of attention, although there were no significant differences on vocabulary, auditory comprehension, or decoding and reading comprehension measures. Within the group of school-age children with minimal hearing loss, later identification of hearing loss and lower maternal education level were associated with larger psychoeducational difficulties. Đoković et al. (2014) compared one hundred forty-four 7- to 12-year-olds with MBHL to an age-matched group of 160 hearing peers. Children with MBHL were later identified (after school entry), had not received intervention for their hearing loss, and did not use HAs. The MBHL group performed significantly lower on standardized measures of morphosyntax and verbal reasoning but displayed no significant differences in vocabulary skills. Finally, Tomblin, Harrison, et al. (2015) reported that preschoolers with MBHL were approximately 0.5 SD lower on vocabulary (combined scores on the Wechsler Preschool and Primary Scale of Intelligence–Third Edition: Vocabulary subtest [Wechsler, 2002] and the Comprehensive Assessment of Spoken Language: Basic Concepts subtest [Carrow-Woolfolk, 1999]) and 1 SD lower on morphosyntax (experimental morphological elicitation task using probes of bound morphemes, described in Tomblin, Walker, et al., 2015) relative to an age- and SES-matched group of children with NH.
Only a few well-described, prospective cohorts of children with MBHL have been reported in the literature, which would allow for the exploration of the effects of HA use and aided audibility on language outcomes. The effects of amplification were specifically examined in a study by Walker, Holte, et al. (2015), which included thirty-eight 5- and 7-year-olds with MBHL. No hearing control group was included in the study, but participants were compared between groups based on consistency of HA use (i.e., full-time users, part-time users, nonusers). The three groups were matched on nonverbal IQ and SES. The full-time HA users achieved significantly higher scores on vocabulary, morphosyntax, and phonological awareness measures relative to the non-HA users, with the largest effect size in the morphosyntax domain. One limitation of this study is that it did not take into account how unaided hearing levels, aided hearing levels, and amount of HA use interact. Understanding the interactions of these variables is critical, if we are to understand how children's access to linguistic input impacts developmental outcomes.
In the Outcomes of Children With Hearing Loss (OCHL) study, we have proposed the cumulative linguistic experience hypothesis to conceptualize the effects of reduced auditory–linguistic access on language acquisition (Moeller & Tomblin, 2015). This hypothesis posits that children who have better unaided hearing and well-fit HAs and wear HAs during all waking hours should have greater access to linguistic input. We predict that this consistent access will lead to richer cumulative language experience, which in turn facilitates more efficient language learning and less risk of delay. Tomblin, Harrison, et al. (2015) provide empirical support for the cumulative linguistic experience hypothesis, in that they showed that aided audibility (after controlling for unaided hearing) and amount of daily HA use affect language growth trajectories in children with mild-to-severe hearing loss. One limitation of this research, however, is that it did not explore whether the benefits of wearing amplification diminish or asymptote as unaided hearing levels approach the normal range of hearing. It also did not examine the effects of HA dosage—the combined effects of unaided and aided hearing as well as the amount of HA use—on language outcomes and whether increased HA dosage helps to mitigate delays. Research in child language intervention suggests that high dosage levels in treatment may not be as effective for children who show high levels of engagement or attentiveness, compared to children who are less engaged or more inattentive (Warren, Fey, & Yoder, 2007). The same dosage–response principle may apply to children with hearing loss whose thresholds approach NH levels, but as of yet, we do not have any evidence to support this theory. Increased knowledge of the effects of HA dosage would guide implementation of optimally effective interventions for professionals who work with children with hearing loss.
To summarize, reports on the risk of developmental delays in children with MBHL vary, but there is research to suggest that a legitimate cause for concern exists. The lack of significant differences across studies could be due to test selection: Global language assessments and parent report measures (Carew et al., 2018; Fitzpatrick et al., 2015; Wake et al., 2006) may be insensitive to differences between children with MBHL and children with NH. Results by Đoković et al. (2014) and Walker, Holte, et al. (2015) indicate that during the preschool and early elementary years, deficits may be specific to areas of language form (i.e., morphology), whereas there appears to be less vulnerability in language content (i.e., vocabulary). The surface hypothesis (Leonard, 1989) provides theoretical support for this pattern of increased risk in aspects of language form. The surface hypothesis, originally intended to describe deficits in children with developmental language disorders, proposes that the acoustic characteristics of English grammatical morphemes (e.g., short duration and relatively low phonetic substance) make it difficult for children to learn English morphology. Results from the longitudinal OCHL study support the application of the surface hypothesis to preschool-age children who are hard of hearing (Moeller & Tomblin, 2015; Tomblin, Harrison, et al., 2015), including children with MBHL (Walker, Holte, et al., 2015). It is unclear, however, whether delays in these vulnerable areas of language will persist over time or have cascading developmental consequences in the elementary years, particularly in terms of reading achievement.
Far less research has been conducted with respect to reading outcomes for children with MBHL compared to other developmental areas. Reading proficiency is of paramount concern, however, because of the implications for long-term academic and vocational success. Porter et al. (2013) did not find significant differences in decoding and reading comprehension, but that study combined children with MBHL and unilateral hearing loss together, resulting in only 12 children with bilateral HL. Wake et al. (2006) also did not find deficits in reading, but the majority of their sample had a slight (15–25 dB HL) hearing loss. Further research is needed to determine whether children with MBHL show deficits in areas of grammar, vocabulary, and reading in later grades or whether they are able to close the achievement gap after the preschool years (Tomblin, Harrison, et al., 2015). Another unanswered but related question is what underlying mechanisms support reading achievement in children with MBHL. If they are able to achieve reading levels that are commensurate with their hearing peers (as indicated by Porter et al., 2013 and Wake et al., 2006), are they relying on the same skills as children with NH, or do they show differences in how they achieve reading proficiency? Identifying fundamental skills that support reading abilities is important because it provides insight into how we might approach preliteracy and literacy intervention for different populations.
To understand the underlying factors that contribute to reading in children with MBHL, we have a large literature base to draw on that describes reading skills in typically developing children. Much of that literature is based around the “simple view” of reading (Gough & Tunmer, 1986), which conceptualizes reading comprehension as two interdependent aspects: decoding and language comprehension. During the early elementary years (first to third grade), reading ability is heavily dependent on decoding, which is directly influenced by code-based skills (i.e., phonological awareness, alphabet knowledge, and knowledge of print concepts). Starting around third grade, however, language comprehension becomes important for reading achievement. At this point, linguistic skills (vocabulary, listening comprehension) play a direct role in reading comprehension (Nation & Snowling, 1999; Storch & Whitehurst, 2002). Metalinguistic skills, such as morphological awareness, also contribute to reading abilities by mid-elementary grades (Apel, Wilson-Fowler, Brimo, & Perrin, 2012). Morphological awareness can be defined as the ability to recognize morphological structure in words (Apel, 2014; Carlisle, 2000). To date, however, there have been no investigations looking at the concurrent influence of vocabulary, listening comprehension, and morphological awareness skills on individual differences in reading for children with MBHL. Given past research that suggests that children who are hard of hearing show increased variability in morphological knowledge relative to vocabulary knowledge (Tomblin, Harrison, et al., 2015), it is possible that children with MBHL could demonstrate differences in the factors that account for variance in reading compared to children with NH, even if end-point reading outcomes are the same between groups. An alternative hypothesis is that children with hearing loss, including children with MBHL, will show delays in reading acquisition, but the underlying sources that account for variance in reading will be consistent with children with NH (qualitative similarity hypothesis; Paul & Lee, 2010). Regardless of the prediction, expanding our knowledge regarding the foundational skills that contribute to literacy will lead to a better understanding of reading development for children with MBHL and inform clinical and educational practices.
The goal of the current article is to advance the understanding of outcomes in the current generation of school-age children with MBHL to better inform clinical management practices. In doing so, we will address the following research questions:
Do children with NH outperform children with MBHL on language and reading measures in fourth grade?
What linguistic skills (vocabulary, language comprehension, morphological awareness) predict reading outcomes in children with MBHL and children with NH in fourth grade?
What factors are associated with individual differences in language and reading measures for children with MBHL?
Method
Participants
Participants included a subset of children who were enrolled in a multicenter, prospective, longitudinal study on outcomes of children who are hard of hearing (OCHL). Children were recruited from three primary sites: University of Iowa, Boys Town National Research Hospital, and University of North Carolina–Chapel Hill. All participants were required to meet the following criteria to enroll in the study: (a) spoken English as the primary communication mode, (b) vision within normal limits (with correction, if needed), (c) no significant motor or cognitive delays, and (d) between the ages of 6 months and 7 years at the first testing visit.
The current study focuses on outcomes of 60 children (33 girls, 27 boys) with MBHL (BEPTA greater than 15 dB HL and less than 45 dB HL) and 69 children (39 girls, 30 boys) with NH who received nonverbal IQ, language, and literacy tests. The average age of the children with MBHL was 10.38 years, and the average age of the children with NH was 10.37 years. Table 1 shows demographic information of the sample. For children with MBHL, the average BEPTA was 33.40 dB HL (SD = 7.38, range: 18.75–43.75). Fifty-one children wore bilateral HAs, four wore an HA unilaterally, and four children did not use HAs at all. One child only had HAs available for use at school, but not at home.
Table 1.
Demographic characteristics for children with mild bilateral hearing loss (MBHL) and children with normal hearing (NH).
| Variable | Children with MBHL (n = 60) |
Children with NH (n = 69) |
||||
|---|---|---|---|---|---|---|
| n | M (SD) | Range | n | M (SD) | Range | |
| Chronological age (years) | 60 | 10.38 (0.35) | 9.75–11.52 | 69 | 10.37 (0.37) | 8.96–11.08 |
| Maternal education level (years) | 60 | 15.65 (2.34) | 12–20 | 66 | 15.73 (2.97) | 8–20 |
| Better-ear PTA (dB HL) a | 60 | 33.40 (7.38) | 18.75–43.75 | 69 | < 20 | |
| Better-ear unaided SII | 58 | 0.64 (0.18) | 0.32–.098 | N/A | ||
| Better-ear aided SII b | 59 | 0.88 (0.08) | 0.56–0.99 | N/A | ||
| Age at confirmation (months) | 59 | 27.00 (23.70) | 1.00–64.00 | N/A | ||
| Age at HA fitting (months) | 56 | 32.42 (27.80) | 2.00–108.00 | N/A | ||
| Age at early intervention (months) | 36 | 11.28 (10.31) | 1.00–36.00 | N/A | ||
| Amount of daily HA use (hours) | 60 | 9.74 (4.42) | 0–16 | N/A | ||
Note. PTA = pure-tone average; SII = Speech Intelligibility Index; N/A = not applicable; HA = hearing aid.
The criteria for study enrollment for children who were hard of hearing was better-ear PTA of no better than 25 dB HL. Exceptions were made to include children with mild high-frequency HL (3-frequency PTA less than 25 dB HL in the better ear, but thresholds greater than 25 dB HL at 3, 4, or 6 kHz).
For children with MBHL who did not have hearing aids (n = 4), unaided SII is included. For children with hearing aids, aided SII is included.
Procedure
All study procedures were approved by the institutional review boards at The University of Iowa, Boys Town National Research Hospital, and University of North Carolina–Chapel Hill. Tomblin, Walker, et al. (2015) describe the experimental design and procedures for participants in the OCHL study. Data collection began in 2009. Nonverbal IQ testing took place during the first 5-year cycle at 4, 5, or 6 years of age. No participants were more than 1.5 SDs from the average range on nonverbal IQ testing. In 2013, children were enrolled in the second cycle of the longitudinal study, Outcomes of School-Age Children Who Are Hard of Hearing. All Outcomes of School-Age Children Who Are Hard of Hearing participants were tested as a single cohort in the summers after second and fourth grade.
Audiologic Assessment
A certified audiologist completed the hearing assessment at every test visit. Air- and bone-conduction thresholds were obtained for children with MBHL at 250, 500, 1000, 2000, 4000, 6000, and 8000 Hz. The four-frequency BEPTA was calculated for subsequent analyses. Children with NH passed a screening at 20 dB HL at 500, 1000, 2000, and 4000 Hz.
HA Verification and Audibility Measures
HA verification was completed with Audioscan Verifit speechmapping software (Cole, 2005) using simulated real-ear measures. Probe-microphone real-ear-to-coupler differences (Bagatto et al., 2005) were completed prior to HA verification in a 2-cc coupler. The Speech Intelligibility Index (SII; ANSI S3.5-1997), a weighted proportion of the amount of the long-term average speech spectrum audible above the listener's thresholds, was calculated using the standard male carrot passage speech signal (Cox & McDaniel, 1989) at an average input level (60 or 65 dB SPL). An SII value of 0 indicates that none of the long-term average speech spectrum is audible and 1 represents complete audibility. The better-ear SII at average speech levels was calculated for subsequent analyses.
HA Use Measures
During the test visit, the caregiver completed a questionnaire related to daily HA use (see Walker et al., 2013, for an example of the HA use questionnaire). Caregivers estimated average number of hours that the child wore HAs during the week and weekends, which was calculated as a weighted HA use measure (weekday use * 0.71 [5/7 days of the week] plus weekend use * 0.29 [2/7 days of the week]).
Language and Reading Measures
Test protocols were developed to be appropriate for children utilizing spoken English in fourth grade. The Woodcock-Johnson Tests of Achievement-III Picture Vocabulary subtest (WJTA-III; Woodcock, McGrew, Mather, & Schrank, 2001) measures expressive vocabulary via picture naming. The WJTA-III Understanding Directions subtest measures listening comprehension. It involves listening to sequential directions and maintaining the sequence of directions in response to the examiner's prompt. Overall reading abilities were assessed via the Gray Oral Reading Tests–Fifth Edition (GORT-5; Wiederholt & Bryant, 1992). The GORT is a timed reading task where the subject is given instructions to read a passage aloud as quickly and carefully as possible. After reading the passage, the participant answers several questions about the passage that are given orally by the examiner. The GORT yields an oral reading index that combines fluency and reading comprehension scores. The Test of Morphological Structure (TMS; Carlisle, 2000) assesses morphological awareness of the composition of inflected and derived words. We used the raw scores from the Word Derivation subtest, as it has been shown to be variable in typically developing children. In this cloze procedure task, the examiner says a target word aloud and then reads a sentence that is missing the final word. The participant is expected to change the target word into a different form that will complete the sentence (i.e., “Farm. My uncle is a _____. [farmer]). The TMS was administered orally, and participants' responses were oral. Items were scored as correct (1 point) or incorrect (0 points), with a total of 28 possible points.
Statistical Analyses
For Research Question 1, t tests were used to determine whether there were significant differences between groups (children with MBHL and children with NH) on the language and literacy measures. Significance levels were set at α = .05. Cohen's d was included to report effect sizes. To control for multiple independent variables and confirm findings from the t tests, multivariate analysis of variance (MANOVA) was also conducted. For Research Question 2, we used a hierarchical linear regression model to explore associations between predictor variables (i.e., vocabulary, listening comprehension, and morphological awareness) and an outcome variable (overall reading ability). For Research Question 3, we again used linear regression models to explore associations between predictor variables and language outcomes. Outcome variables included vocabulary, listening comprehension, morphological awareness, and reading. The predictors included maternal education level, unaided better-ear SII, and aided better-ear SII. We also included a variable that we termed HA dosage which was a combination of HA use and audibility levels (aided and unaided). This metric can be conceptualized as a measure of how much daily benefit a child was receiving from HAs. It was calculated as HA Dosage = Daily HA Use hoursAided Better-ear SII – (24 – Daily HA Use hours)Unaided Better-ear SII. In other words, number of hours of daily HA use is weighted to the power of aided SII (access to speech with HAs). If SII = 1, the child has full access to the speech spectrum for that number of hours. This value is subtracted from how often the child does not wear HAs during the day, weighted to the power of unaided SII (access to speech without HAs). Essentially, this equation combines the number of hours of daily HA use with aided and unaided hearing into one weighted measure of how much auditory access a child experiences throughout a 24-hr day. HA dosage was included in the regression model along with the other predictor variables.
Results
Outcome Comparisons Between Children With MBHL and Children With NH
Vocabulary
Children with MBHL (n = 60) demonstrated a mean standard score of 99.78 (SD = 10.76) on the WJTA Picture Vocabulary subtest, and children with NH (n = 69) demonstrated a mean standard score of 103.06 (SD = 10.11). The results of the independent-samples t test were not significant, t(127) = 1.78, p = .077, d = 0.31.
Listening Comprehension
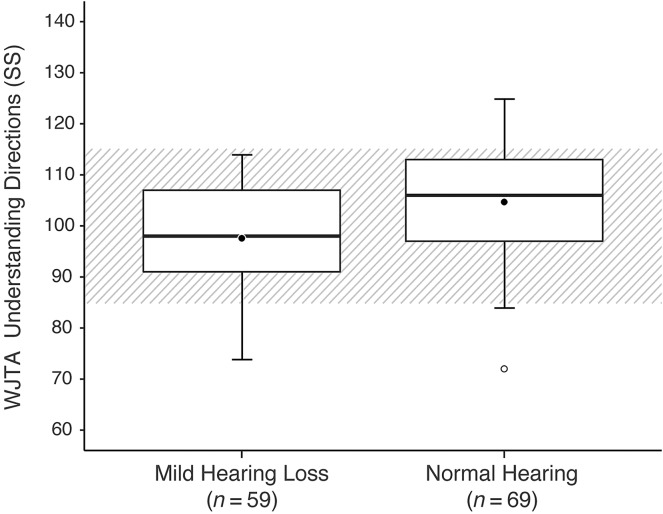
Children in the MBHL group (n = 59) demonstrated a mean standard score of 97.59 (SD = 12.64) on the WJTA Understanding Directions subtest, and children in the NH group (n = 69) demonstrated a mean standard score of 104.70 (SD = 12.59). The results of the independent-samples t test were significant, t(126) = 3.18, p = .002, d = 0.56. Figure 1 displays the distribution of the Understanding Directions standard scores for both groups.
Figure 1.
Box plots of Woodcock-Johnson Tests of Achievement (WJTA) Understanding Directions standard scores (SS) for children with mild hearing loss (left) and children with normal hearing (right). The central lines represent the median values, the filled circles represent the mean values, and the box limits are the 25th and 75th percentiles. The lower and upper fences are the 5th and 95th percentiles. Open circles represent outliers. The hatched area represents the average range for the normative sample.
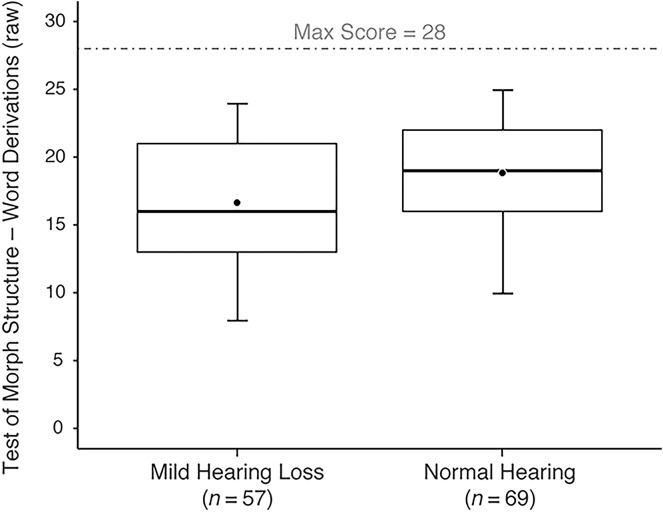
Morphological Awareness
Children with MBHL (n = 58) demonstrated a mean raw score of 16.64 (SD = 5.27) out of 28 possible on the TMS, and children with NH (n = 69) demonstrated a mean standard score of 18.84 (SD = 4.78). The results of the independent-samples t test were significant, t(125) = 2.47, p = .015, d = 0.44. Figure 2 displays the distribution of scores for both groups.
Figure 2.
Box plots of Test of Morphological Structure raw scores for children with mild hearing loss (left) and children with normal hearing (right). The central lines represent the median values, the filled circles represent the mean values, and the box limits are the 25th and 75th percentiles. The lower and upper fences are the 5th and 95th percentiles.
Reading
Children with MBHL (n = 59) demonstrated a mean standard score of 93.36 (SD = 13.58) on the GORT Oral Reading Index. Children with NH (n = 69) demonstrated a mean standard score of 94.91 (SD = 12.25). The results of the independent-samples t test were not significant, t(126) = 0.68, p = .497, d = 0.12.
Table 2 displays means, standard deviations, and results of t tests for the four outcome measures. We also conducted a MANOVA to adjust for multiple independent variables and correlations between variables. Results were consistent with the t tests. The overall MANOVA was significant, F(4, 120) = 4.02, p = .004, partial η2 = .118. Follow-up tests of between-subjects effects for individual measures indicated significant group differences for listening comprehension (p = .002) and morphological awareness (p = .016) and no significant differences in vocabulary and reading outcomes.
Table 2.
Summary statistics of outcome measures for children with mild bilateral hearing loss (MBHL) and children with normal hearing (NH).
| Outcome variable | MBHL |
NH |
Between groups |
|
|---|---|---|---|---|
| M (SD) | M (SD) | d | p | |
| WJTA Picture Vocabulary SS | 99.78 (10.76) | 103.06 (10.11) | 0.31 | .077 |
| WJTA Understanding Directions SS | 97.59 (12.64) | 104.70 (12.59) | 0.56 | .002* |
| Test of Morphological Awareness raw score | 16.64 (5.27) | 18.84 (4.78) | 0.44 | .015* |
| GORT Oral Reading Index SS | 93.36 (13.58) | 94.91 (12.25) | 0.12 | .497 |
Note. WJTA = Woodcock-Johnson Tests of Achievement; SS = standard score; GORT = Gray Oral Reading Tests.
Significance with α level = .05.
Linguistic Predictors of Reading Outcomes in Children With MBHL and Children With NH
Listening comprehension, vocabulary, and morphological awareness were entered as predictors, with overall reading skills as the dependent variable (see Table 3). The model for children with MBHL was significant, F(3, 52) = 25.04, p < .0001, R 2 = .59. Morphological awareness and vocabulary were both significant and accounted for unique variance. Morphological awareness accounted for the greatest amount of variance (β = 0.53, p < .001), followed by vocabulary (β = 0.29, p = .023). Listening comprehension was not a significant predictor in the model.
Table 3.
Summary of linear regression analysis for reading outcomes (Gray Oral Reading Tests Oral Reading Index standard score) with the mild bilateral hearing loss (MBHL) group and the normal hearing (NH) group.
| Predictor variables | MBHL |
NH |
||||||
|---|---|---|---|---|---|---|---|---|
| B | B (SE) | t | p | B | B (SE) | t | p | |
| WJTA Picture Vocabulary SS | 0.36 | 0.16 | 2.34 | .023* | 0.63 | 0.13 | 4.97 | < .001* |
| WJTA Understanding Directions SS | 0.03 | 0.13 | 0.23 | .823 | 0.37 | 0.09 | 4.17 | < .001* |
| TMS raw score | 1.36 | 0.33 | 4.11 | < .001* | 0.06 | 0.27 | 0.23 | .815 |
Note. B = unstandardized coefficient; B (SE) = unstandardized coefficient standard error; WJTA = Woodcock-Johnson Tests of Achievement; SS = standard score; TMS = Test of Morphological Awareness.
Significance with α level = .05.
The model for children with NH was also significant, F(3, 65) = 42.31, p < .0001, R 2 = .66. In contrast to the children with MBHL, vocabulary and listening comprehension were significant predictors. Vocabulary accounted for the greatest amount of variance (β = 0.52, p < .001), followed by listening comprehension (β = 0.38, p < .001). Morphological awareness was not a significant predictor in the model.
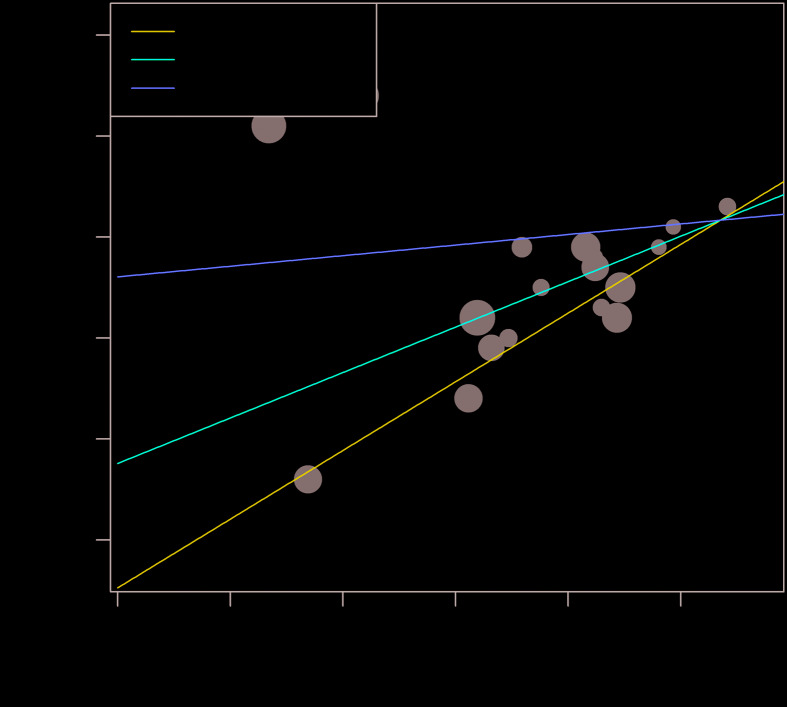
Child- and Family-Specific Predictors of Language Outcomes for Children With MBHL
Maternal education level, better-ear unaided SII, better-ear aided SII, HA dosage, and the interaction between HA dosage and better-ear unaided SII were entered into the model (see Table 4). We included the interaction to determine whether higher levels of unaided hearing resulted in less of an effect of HA dosage on outcomes. For vocabulary, better-ear unaided SII was the only variable that was significant after controlling for the other factors (β = 0.49, p = .031), indicating that better unaided hearing was associated with a larger vocabulary size. For listening comprehension, HA dosage and the interaction between HA dosage and unaided better-ear SII were both significant (β = 1.53, p = .044, and β = −1.39, p = .045, respectively). These results indicate that increased HA dosage resulted in higher listening comprehension scores. However, the interaction suggests that, as unaided hearing levels increase, there is less of an influence of HA dosage on listening comprehension. Figure 3 provides a visual display of this interaction. HA dosage is presented on the x-axis; a negative HA dosage indicates that the child is getting less benefit from HAs (either due to minimal use or lower SII), and a positive HA dosage indicates that the child is getting more benefit from HAs. In the figure, the circles represent unaided SII (larger circles = higher unaided SII). The three regression lines represent the 25th, 50th, and 75th percentiles of unaided SII. As unaided SII decreases, HAs have more of an impact on listening comprehension, as shown by the steeper regression line. With morphological awareness, none of the predictors was significant, but unaided SII approached significance (β = 0.41, p = .073). With reading, none of the predictors was significant, but HA dosage and the interaction of HA dosage and unaided hearing approached significance (β = 1.54, p = .078, and β = −1.36, p = .076, respectively).
Table 4.
Summary of linear regression analysis for vocabulary, listening comprehension, morphological awareness, and reading outcomes for the mild bilateral hearing loss (MBHL) group.
| WJTA Picture Vocabulary standard score | ||||
|---|---|---|---|---|
| Predictors | B | B (SE) | t | p |
| HA dosage | 1.83 | 1.27 | 1.45 | .15 |
| Better-ear unaided SII | 29.15 | 13.09 | 2.23 | .03* |
| Better-ear aided SII | −14.81 | 23.78 | −0.62 | .53 |
| Maternal education level: high school or less | 3.08 | 4.79 | 0.64 | .52 |
| Maternal education level: vocational/some college | −5.69 | 3.77 | −1.51 | .14 |
| Maternal education level: college | 0.76 | 3.75 | 0.20 | .84 |
| HA dosage × Better-ear unaided SII | −1.69 | 1.53 | −1.11 | .27 |
|
WJTA Understanding Directions standard score | ||||
|
B
|
B (SE)
|
t
|
p
|
|
| HA dosage | 3.20 | 1.55 | 2.07 | .04* |
| Better-ear unaided SII | 25.94 | 16.14 | 1.61 | .11 |
| Better-ear aided SII | −23.85 | 28.98 | −0.82 | .41 |
| Maternal education level: high school or less | 1.07 | 5.95 | 0.18 | .86 |
| Maternal education level: vocational/some college | −1.82 | 4.69 | −0.39 | .70 |
| Maternal education level: college | 0.26 | 4.68 | 0.06 | .96 |
| HA dosage × Better-ear unaided SII | −3.84 | 1.87 | −2.06 | .05* |
|
Test of Morphological Structure raw score | ||||
|
B
|
B (SE)
|
t
|
p
|
|
| HA dosage | 1.00 | 0.64 | 1.57 | .13 |
| Better-ear unaided SII | 12.11 | 6.61 | 1.83 | .07 |
| Better-ear aided SII | −6.44 | 11.97 | −0.54 | .59 |
| Maternal education level: high school or less | 0.20 | 2.42 | 0.08 | .93 |
| Maternal education level: vocational/some college | −3.58 | 1.97 | −1.82 | .08 |
| Maternal education level: college | −0.54 | 1.90 | −0.28 | .78 |
| HA dosage × Better-ear unaided SII | −0.99 | 0.77 | −1.28 | .21 |
|
Gray Oral Reading Tests Oral Reading Index | ||||
|
B
|
B (SE)
|
t
|
p
|
|
| HA dosage | 2.54 | 1.41 | −1.80 | .08 |
| Better-ear unaided SII | 21.48 | 17.44 | 1.23 | .22 |
| Better-ear aided SII | −39.15 | 38.09 | −1.03 | .31 |
| Maternal education level: high school or less | −2.81 | 5.06 | −0.56 | .58 |
| Maternal education level: vocational/some college | −5.89 | 4.26 | −1.38 | .17 |
| Maternal education level: college | −4.76 | 4.08 | −1.17 | .25 |
| HA dosage × Better-ear unaided SII | −2.81 | 1.55 | −1.82 | .08 |
Note. WJTA = Woodcock-Johnson Tests of Achievement; B = unstandardized coefficient; B(SE) = unstandardized coefficient standard error; SII = Speech Intelligibility Index.
Significance with α level = .05.
Figure 3.
Standard scores on the Woodcock-Johnson Tests of Achievement (WJTA) Understanding Directions subtest as a function of the HA dosage with different levels of unaided Speech Intelligibility Index (SII).
Discussion
The primary goal of the current study was to determine whether children with MBHL demonstrate deficits in language and reading outcomes by the mid-elementary grades. We also explored key linguistic and metalinguistic factors that account for individual differences in reading abilities in children with MBHL compared to children with NH. Finally, we sought to establish whether HA dosage affects functional outcomes in a sample of children with significant residual hearing. The results are consistent with the notion that children with MBHL show delays in specific aspects of language. Further, higher HA dosage (measured via a weighted metric of aided and unaided SII and hours of daily HA use) appears to support listening comprehension for children with MBHL.
Language and Reading Outcomes
All participants were tested the summer after fourth grade. Although this is past the period in which primary language skills are being established, the mid-elementary years are still critical to academic and vocational success (Nippold, 2016). Research shows that language acquisition continues during this time, although changes in vocabulary and grammar skills may be more subtle (Nippold, 1993, 1995). Importantly, fourth grade is the point at which children transition from learning how to read to reading to learn (i.e., using their reading skills to acquire new vocabulary, advanced morphosyntax, and derivational morphology). In conjunction with this transition, academic instruction begins to shift toward decontextualized language in the classroom, making it increasingly difficult for children with weak language skills to meet the demands of academic settings. Most of the studies examining outcomes of children with MBHL have examined earlier stages of language development (Carew et al., 2018; Fitzpatrick et al., 2015; Porter et al., 2013; Tomblin, Harrison, et al., 2015; Walker, Holte, et al., 2015). Thus, we are limited in our understanding of later language and reading skills in the current generation of children with MBHL. A major contribution of the current article is that it helps to fill this gap in our knowledge.
Overall, between-groups data showed a profile of differential risk for children with MBHL. Between-groups differences in vocabulary size did not reach significance, suggesting that language content may be a relative strength, although variability in performance and deficits are still possible. In contrast to vocabulary, the MBHL group demonstrated significant delays in listening comprehension (which taps into working memory, receptive grammar, and vocabulary) and specific aspects of language form, with lower scores on a measure of morphological awareness. This trend toward vulnerability in morphosyntax is consistent with the cumulative linguistic experience hypothesis described by Moeller and Tomblin (2015). This hypothesis proposes that development of specific language domains (morphosyntax, phonology) depends on good auditory access to the phonetic structure of the linguistic input. Hearing loss, even in the mild range, reduces the consistency of exposure to morphemes. This is especially true for perceptually subtle grammatical morphology (morphemes with /s/, /z/, or /t/) or in cases where learning is taking place in acoustically degraded situations (i.e., virtually all classroom settings). The results from the current study add to the growing literature base that suggests children who are hard of hearing are at risk for delays in morphological development (Hansson, Sahlén, & Mäki-Torkko, 2007; Koehlinger, Van Horne, & Moeller, 2013; McGuckian & Henry, 2007).
To the best of our knowledge, this is the first study to examine performance on a test of morphological awareness for children who are hard of hearing, although it has been studied in children with cochlear implants (Apel & Masterson, 2015). We focused specifically on derivational morphology skills (i.e., deriving a word such as farmer from farm) because these skills show rapid growth starting around fourth grade (Tyler & Nagy, 1989). These skills have also been shown to contribute unique variance to reading comprehension, spelling, and decoding (Carlisle, 2000; Wolter, Wood, & D'zatko, 2009). Based on the surface hypothesis (Leonard, 1989) and the cumulative linguistic experience hypothesis, we would predict that children with MBHL would have difficulty with derivational morphology, which could be a source of individual differences in reading scores. The current results support that prediction and highlight the possible need for clinical intervention for children with mild hearing loss who are struggling in the morphological domain. In educational and speech-language pathology settings, morphological awareness has received less attention than other metalinguistic skills such as phonemic awareness (Apel, 2014; Apel et al., 2012), but these findings show that children with MBHL may need additional assessment and support in this area.
A further prediction of the cumulative linguistic experience hypothesis is that language content will be less impacted by hearing loss than language form. The basis of this prediction stems from the rationale that vocabulary acquisition will not rely as heavily on fidelity of phonetic perception as morphology, and lexical cues are more redundant and salient than phonetic cues in the input. The results of the current study support this prediction, in that we did not see any significant delays in vocabulary for the fourth graders with MBHL. We acknowledge a limitation of the current study is that we only included a measure of vocabulary breadth and not vocabulary depth. The WJTA Picture Vocabulary task asks the child to name pictures as they are presented to him or her. Most standardized vocabulary tests only involve word recognition or naming (i.e., vocabulary breadth). These tasks measure surface-level knowledge but do not tap into how much children know about words (i.e., vocabulary depth). As children enter secondary grades, deeper vocabulary knowledge leads to better reading comprehension (Nation & Snowling, 1999; Ouellette, 2006; Paul & Gustafson, 1991). Recent research from the OCHL study suggests that, by the end of third grade, children with mild to severe hearing loss may be closing the gap with same-age hearing peers in terms of vocabulary breadth, but not vocabulary depth (Walker, Redfern, & Oleson, 2019). Unfortunately, we did not have any measures of vocabulary depth in the period analyzed in the current study, and vocabulary depth measures often tend to be overlooked in favor of vocabulary size measures in clinical and educational settings. Future research should explore whether children with MBHL have less in-depth knowledge of vocabulary, as seen in children whose hearing loss ranges from mild to severe, as opposed to only examining vocabulary breadth.
Linguistic Predictors of Reading Outcomes
On the global reading measure, the MBHL group showed commensurate performance to NH peers, suggesting that there were no quantitative differences on a composite measure of reading fluency and comprehension. On the other hand, the regression analysis showed differences between groups in the underlying factors that predict reading outcomes. Higher reading scores were associated with stronger vocabulary and listening comprehension skills for the children with NH, with morphological awareness not contributing to individual differences in reading. In contrast, morphological awareness accounted for the majority of the variance in reading scores for the children with MBHL. Thus, the two groups appeared to demonstrate unique pathways to achieving success in reading. This finding is in contrast to the prediction that children with hearing loss will use similar strategies in reading acquisition as CNH, but with a slower developmental trajectory (Paul & Lee, 2010). We speculate that, because the children with MBHL demonstrated great variability in morphological awareness, this factor may have weighed more heavily on reading outcomes for the group with hearing loss than the group with NH, over and above the influence of vocabulary and listening comprehension. The clinical implications of this finding are that educators and speech-language pathologists should be aware of the risk of morphological deficits in this population and the influence that it has on reading outcomes. It is also important to note that the apparent weaknesses in morphology for the children with MBHL were not enough to lead to significant global reading deficits on a group level; however, it could affect later reading achievement or writing. Examining writing skills is beyond the scope of the current study, but future directions should explore writing in children with mild hearing loss, including spelling and different genres of written expression (narratives, expository writing, and persuasive writing).
Clinical Predictors of Language Outcomes
An important finding from this study is that increased HA dosage appears to support listening comprehension. A persistent challenge when trying to measure the benefit of HA use in children with MBHL is that even when they receive well-fit amplification, they may not use them on a consistent basis (Walker, McCreery, et al., 2015; Walker et al., 2013). Furthermore, amount of HA use is confounded with unaided hearing levels, in that children with less access to speech wear HAs more often than children with more access. Here, we developed a metric that would combine hours of HA use with aided and unaided audibility levels, which we termed HA dosage. The purpose of this index was to consolidate how much auditory access children with HAs were getting with how often they were wearing the HAs throughout the day; in other words, a measure of “cumulative linguistic experience.” The results from a linear regression analysis indicated that higher amounts of HA dosage are significantly associated with better listening comprehension scores. We also saw a significant interaction between HA dosage and unaided SII, suggesting that the benefits of HAs may plateau for children with higher levels of unaided SII. The current data align with recent evidence from McCreery et al. (2020), which suggested that an unaided SII of greater than 0.80 may indicate resilience in language acquisition for children with hearing loss. Reading scores approached significance levels with HA dosage, as did the interaction between HA dosage and unaided SII. Vocabulary and morphological awareness were not significantly associated with HA dosage, although there was a positive correlation between vocabulary size and unaided hearing levels. We interpret these data as evidence that HAs, when worn consistently, are an effective intervention strategy for children with MBHL. However, the effectiveness of this form of treatment may decrease for children with very slight degrees of hearing loss.
Clinical Implications
HA candidacy protocols for children with MBHL historically have recommended amplification only after evidence of developmental delays has been documented. This “failure-based” approach (Winiger, Alexander, & Diefendorf, 2016) is the result of a lack of evidence-based HA candidacy criteria and the fact that commonly used speech and language assessments may lack sensitivity for the types of deficits experienced by children with MBHL. As described above, a critical finding from the current study is that children with MBHL are at risk for delays in language form, particularly morphology. Combined with the findings from our previous research (Walker, Holte, et al., 2015), these deficits appear to persist at least into mid-elementary grades. Thus, morphosyntax and morphological awareness should be carefully examined in children with MBHL, as this domain may be an early clinical indicator for identifying which children with MBHL would benefit from increased use of amplification and additional support services.
Another take-home message from this study is the importance of using aided and unaided audibility levels to determine whether children will benefit from HAs. Current HA candidacy criteria are typically based on audiometric thresholds or estimates of thresholds from auditory brainstem responses, which do not take into account the effects of ear canal acoustics on threshold measures. Although children with MBHL are to be considered candidates for HAs under the American Academy of Audiology (2013) Clinical Practice Guidelines for Pediatric Amplification, no discrete cutoff for candidacy is provided. Using unaided SII measures rather than the dB HL audiogram may help to standardize recommendations among audiologists and identify which children are at risk for language delays (McCreery et al., 2020). Additional work is needed to examine how the unaided SII could be employed as a clinical criterion for amplification in children with MBHL.
Limitations
Given the lack of evidence regarding the effects of mild degrees of hearing loss on communication development, this study has important clinical implications for service delivery in this population. At the same time, there are several limitations that should be acknowledged. As we have described in several articles (e.g., Tomblin, Walker, et al., 2015), the OCHL cohort consisted of a well-defined, tightly controlled sample of children with hearing loss. We excluded children with additional disabilities or children who were learning spoken English as a second language to isolate the effects of hearing loss on speech, language, and listening outcomes. As a result, findings from the current study may not apply to the general population of children with MBHL. In addition, the OCHL cohort was biased toward higher SES levels compared to the U.S. population as a whole, a trend that is common in longitudinal volunteer research (Holden, Rosenberg, Barker, Tuhrim, & Brenner, 1993). We attempted to control for this SES confound by including an age-matched sample of children with NH, who were recruited from the same zip codes as the children with hearing loss. Nevertheless, the participants with hearing loss in this study may represent a “best case” scenario, in that most of the children came from economically advantaged backgrounds with access to high-quality intervention and education.
Another limitation of this study is that our outcome measures consisted primarily of decontextualized, standardized language tests. Use of these end-state measures does not allow for examination of language processing in real time. Furthermore, these tests may not be sensitive to the unique vulnerabilities of children who are hard of hearing, especially with respect to high-frequency verb and noun morphology (Blaiser & Shannahan, 2018; Koehlinger et al., 2013; Koehlinger, Van Horne, Oleson, McCreery, & Moeller, 2015). The vocabulary measure, in particular, only assessed surface-level lexical knowledge. As children grow older, the ability to use vocabulary flexibly and efficiently plays a large role in reading comprehension and academic success. Future research should explore lexical–semantic organization and activation. An exception to standardized tests in the current test battery was the TMS, which is an experimental measure designed to assess metalinguistic awareness of derived morphological forms. Other metalinguistic skills, such as orthographic awareness, have also been shown to be associated with reading development in typically developing children (Apel et al., 2012), but these skills have received little to no attention in the literature on children who are hard of hearing. Future studies should include multiple measures of metalinguistic knowledge, as they may serve as important targets in intervention and educational instruction.
Conclusions
This study demonstrated that children with MBHL show persistent deficits in aspects of language form into the mid-elementary grades. Vocabulary size and reading skills appear to be age-appropriate by fourth grade; however, the factors that are associated with success in reading may be different between children with MBHL and children with NH. Consistent HA use appears to be an effective intervention approach for this population, although the benefits of this approach may diminish with higher unaided hearing levels. Finally, this study provides important evidence for professionals and parents that, although the needs of children with MBHL should not be underestimated, we can still expect them to achieve language and reading outcomes that are on par with their hearing peers.
Acknowledgments
This work was supported by National Institute on Deafness and Other Communication Disorders Grant 5R01DC009560 (co-principal investigators, J. Bruce Tomblin, University of Iowa, and Mary Pat Moeller, Boys Town National Research Hospital). The content of this project is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Deafness and Other Communication Disorders or the National Institutes of Health. Special thanks go to the families and children who participated in the research and to the examiners at the University of Iowa, Boys Town National Research Hospital, and University of North Carolina–Chapel Hill.
Funding Statement
This work was supported by National Institute on Deafness and Other Communication Disorders Grant 5R01DC009560 (co-principal investigators, J. Bruce Tomblin, University of Iowa, and Mary Pat Moeller, Boys Town National Research Hospital). The content of this project is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Deafness and Other Communication Disorders or the National Institutes of Health.
References
- American Academy of Audiology. (2013). Clinical practice guidelines: Pediatric amplification. Reston, VA: Author. [Google Scholar]
- American National Standards Institute. (1997). Methods for calculation of the speech intelligibility index (Technical Report S3.5-1997). New York, NY: Author. [Google Scholar]
- Apel K. (2014). A comprehensive definition of morphological awareness: Implications for assessment. Topics in Language Disorders, 34(3), 197–209. [Google Scholar]
- Apel K., & Masterson J. J. (2015). Comparing the spelling and reading abilities of students with cochlear implants and students with typical hearing. Journal of Deaf Studies and Deaf Education, 20(2), 125–135. [DOI] [PubMed] [Google Scholar]
- Apel K., Wilson-Fowler E. B., Brimo D., & Perrin N. A. (2012). Metalinguistic contributions to reading and spelling in second and third grade students. Reading and Writing, 25(6), 1283–1305. [Google Scholar]
- Bagatto M., Moodie S., Scollie S., Seewald R., Moodie S., Pumford J., & Liu K. P. (2005). Clinical protocols for hearing instrument fitting in the desired sensation level method. Trends in Amplification, 9(4), 199–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bess F. H., Dodd-Murphy J., & Parker R. A. (1998). Children with minimal sensorineural hearing loss: Prevalence, educational performance, and functional status. Ear and Hearing, 19(5), 339–354. [DOI] [PubMed] [Google Scholar]
- Blair J. C., Peterson M. E., & Viehwig S. H. (1985). The effects of mild sensorineural hearing loss on academic performance of young school-age children. The Volta Review, 87(2), 87–93. [Google Scholar]
- Blaiser K. M., & Shannahan M. A. (2018). Language sample practices with children who are deaf and hard of hearing. Language, Speech, and Hearing Services in Schools, 49(4), 950–964. [DOI] [PubMed] [Google Scholar]
- Carew P., Mensah F. K., Rance G., Flynn T., Poulakis Z., & Wake M. (2018). Mild–moderate congenital hearing loss: Secular trends in outcomes across four systems of detection. Child: Care, Health and Development, 44(1), 71–82. [DOI] [PubMed] [Google Scholar]
- Carlisle J. F. (2000). Awareness of the structure and meaning of morphologically complex words: Impact on reading. Reading and Writing, 12(3), 169–190. [Google Scholar]
- Carrow-Woolfolk E. (1999). Comprehensive Assessment of Spoken Language (CASL). Circle Pines, MN: AGS. [Google Scholar]
- Ching T. Y., Dillon H., Marnane V., Hou S., Day J., Seeto M., … Yeh A. (2013). Outcomes of early- and late-identified children at 3 years of age: Findings from a prospective population-based study. Ear and Hearing, 34(5), 535–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole B. (2005). Audionote2: Verifit test signals. Ontario, Canada: Audioscan. [Google Scholar]
- Cox R. M., & McDaniel D. M. (1989). Development of the Speech Intelligibility Rating (SIR) Test for hearing aid comparisons. Journal of Speech and Hearing Research, 32(2), 347–352. [DOI] [PubMed] [Google Scholar]
- Đoković S., Gligorović M., Ostojić S., Dimić N., Radić-Šestić M., & Slavnić S. (2014). Can mild bilateral sensorineural hearing loss affect developmental abilities in younger school-age children. Journal of Deaf Studies and Deaf Education, 19, 484–495. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick E. M., Durieux-Smith A., Gaboury I., Coyle D., & Whittingham J. (2015). Communication development in early-identified children with mild bilateral and unilateral hearing loss. American Journal of Audiology, 24(3), 349–353. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick E. M., Durieux-Smith A., & Whittingham J. (2010). Clinical practice for children with mild bilateral and unilateral hearing loss. Ear and Hearing, 31(3), 392–400. [DOI] [PubMed] [Google Scholar]
- Gough P. B., & Tunmer W. E. (1986). Decoding, reading, and reading disability. Remedial and Special Education, 7(1), 6–10. [Google Scholar]
- Hansson K., Sahlén B., & Mäki-Torkko E. (2007). Can a ‘single hit’ cause limitations in language development? A comparative study of Swedish children with hearing impairment and children with specific language impairment. International Journal of Language & Communication Disorders, 42(3), 307–323. [DOI] [PubMed] [Google Scholar]
- Holden G., Rosenberg G., Barker K., Tuhrim S., & Brenner B. (1993). The recruitment of research participants: A review. Social Work in Health Care, 19(2), 1–44. [DOI] [PubMed] [Google Scholar]
- Koehlinger K. M., Van Horne A. J. O., & Moeller M. P. (2013). Grammatical outcomes of 3- and 6-year-old children who are hard of hearing. Journal of Speech, Language, and Hearing Research, 56(5), 1701–1714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koehlinger K. M., Van Horne A. O., Oleson J., McCreery R., & Moeller M. P. (2015). The role of sentence position, allomorph, and morpheme type on accurate use of s-related morphemes by children who are hard of hearing. Journal of Speech, Language, and Hearing Research, 58(2), 396–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard L. B. (1989). Language learnability and specific language impairment in children. Applied Psycholinguistics, 10(2), 179–202. [Google Scholar]
- McCreery R. W., Walker E. A., Stiles D. J., Spratford M., Oleson J. J., & Lewis D. E. (2020). Audibility-based hearing aid fitting criteria for children with mild bilateral hearing loss. Language, Speech, and Hearing Services in Schools, 51, 55–67. https://doi.org/10.1044/2019_LSHSS-OCHL-19-0021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuckian M., & Henry A. (2007). The grammatical morpheme deficit in moderate hearing impairment. International Journal of Language & Communication Disorders, 42(Suppl. 1), 17–36. [DOI] [PubMed] [Google Scholar]
- Moeller M. P., & Tomblin J. B. (2015). An introduction to the Outcomes of Children With Hearing Loss study. Ear and Hearing, 36, 4S–13S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moeller M. P., Tomblin J. B., & OCHL Collaboration. (2015). Epilogue: Conclusions and implications for research and practice. Ear and Hearing, 36, 92S–98S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nation K., & Snowling M. J. (1999). Developmental differences in sensitivity to semantic relations among good and poor comprehenders: Evidence from semantic priming. Cognition, 70(1), B1–B13. [DOI] [PubMed] [Google Scholar]
- Nippold M. A. (1993). Developmental markers in adolescent language: Syntax, semantics, and pragmatics. Language, Speech, and Hearing Services in Schools, 24(1), 21–28. [Google Scholar]
- Nippold M. A. (1995). School-age children and adolescents: Norms for word definition. Language, Speech, and Hearing Services in Schools, 26(4), 320–325. [Google Scholar]
- Nippold M. A. (2016). Later language development: School-age children, adolescents, and young adults. Austin, TX: Pro-Ed. [Google Scholar]
- Ouellette G. P. (2006). What's meaning got to do with it: The role of vocabulary in word reading and reading comprehension. Journal of Educational Psychology, 98(3), 554–566. [Google Scholar]
- Paul P. V., & Gustafson G. (1991). Comprehension of high-frequency multimeaning words by students with hearing impairment. Remedial and Special Education, 12(4), 52–61. [Google Scholar]
- Paul P. V., & Lee C. (2010). The qualitative similarity hypothesis. American Annals of the Deaf, 154, 456–462. [DOI] [PubMed] [Google Scholar]
- Porter H., Sladen D. P., Ampah S. B., Rothpletz A., & Bess F. H. (2013). Developmental outcomes in early school-age children with minimal hearing loss. American Journal of Audiology, 22(2), 263–270. [DOI] [PubMed] [Google Scholar]
- Storch S. A., & Whitehurst G. J. (2002). Oral language and code-related precursors to reading: Evidence from a longitudinal structural model. Developmental Psychology, 38(6), 934–947. [PubMed] [Google Scholar]
- Tomblin J. B., Harrison M., Ambrose S. E., Walker E. A., Oleson J. J., & Moeller M. P. (2015). Language outcomes in young children with mild to severe hearing loss. Ear and Hearing, 36, 76S–91S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomblin J. B., Oleson J., Ambrose S. E., Walker E. A., & Moeller M. P. (2018). Early literacy predictors and second-grade outcomes in children who are hard of hearing. Child Development. Advance online publication. https://doi.org/10.1111/cdev.13158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomblin J. B., Walker E. A., McCreery R. W., Arenas R. M., Harrison M., & Moeller M. P. (2015). Outcomes of children with hearing loss: Data collection and methods. Ear and Hearing, 36, 14S–23S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyler A., & Nagy W. (1989). The acquisition of English derivational morphology. Journal of Memory and Language, 28(6), 649–667. [Google Scholar]
- Wake M., Tobin S., Cone-Wesson B., Dahl H.-H., Gillam L., McCormick L., … Williams J. (2006). Slight/mild sensorineural hearing loss in children. Pediatrics, 118(5), 1842–1851. [DOI] [PubMed] [Google Scholar]
- Walker E. A., Holte L., McCreery R. W., Spratford M., Page T., & Moeller M. P. (2015). The influence of hearing aid use on outcomes of children with mild hearing loss. Journal of Speech, Language, and Hearing Research, 58(5), 1611–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker E. A., McCreery R. W., Spratford M., Oleson J. J., Van Buren J., Bentler R., … Moeller M. P. (2015). Trends and predictors of longitudinal hearing aid use for children who are hard of hearing. Ear and Hearing, 36, 38S–47S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker E. A., Redfern A., & Oleson J. J. (2019). Linear mixed model analysis to examine longitudinal trajectories in vocabulary depth and breadth in children who are hard of hearing. Journal of Speech, Language, and Hearing Research, 62, 525–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker E. A., Spratford M., Moeller M. P., Oleson J., Ou H., Roush P., & Jacobs S. (2013). Predictors of hearing aid use time in children with mild-to-severe hearing loss. Language, Speech, and Hearing Services in Schools, 44(1), 73–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren S. F., Fey M. E., & Yoder P. J. (2007). Differential treatment intensity research: A missing link to creating optimally effective communication interventions. Mental Retardation and Developmental Disabilities Research Reviews, 13(1), 70–77. [DOI] [PubMed] [Google Scholar]
- Wechsler D. (2002). Wechsler Preschool and Primary Scale of Intelligence–Third Edition (WPPSI-III). San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Werfel K. L., & Douglas M. (2017). Are we slipping them through the cracks? The insufficiency of norm-referenced assessments for identifying language weaknesses in children with hearing loss. Perspectives of the ASHA Special Interest Groups, 2(9), 43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiederholt J. L., & Bryant B. R. (1992). Gray Oral Reading Tests–Fifth Edition (GORT-5). Austin, TX: Pro-Ed. [Google Scholar]
- Winiger A. M., Alexander J. M., & Diefendorf A. O. (2016). Minimal hearing loss: From a failure-based approach to evidence-based practice. American Journal of Audiology, 25, 232–245. [DOI] [PubMed] [Google Scholar]
- Wolter J. A., Wood A., & D'zatko K. W. (2009). The influence of morphological awareness on the literacy development of first-grade children. Language, Speech, and Hearing Services in Schools, 40, 286–298. [DOI] [PubMed] [Google Scholar]
- Woodcock R. W., McGrew K. S., Mather N., & Schrank F. A. (2001). Woodcock-Johnson III Normative Update Tests of Achievement (WJ III NU). Rolling Meadows, IL: Riverside Publishing. [Google Scholar]