Abstract
Purpose:
This study evaluated the flexural strength of polymethyl methacrylate (PMMA) reinforced with various concentrations of zinc oxide (Zn O) nanoparticles.
Materials and methods:
Nano ZnO was added in 0, 0.4, 0.6, 0.8, 1.2 and 1.4 percentage to PMMA denture base material. 60 specimens of heat cure polymerizing acrylic resin of dimensions 10mm x 4mm x 80mm were fabricated in accordance to ISO 20795-1-2013. The specimens were divided into 6 groups. Acrylic specimens were processed according to manufacturer’s instruction. Three-point bending test was performed to evaluate the flexural strength. Surface analysis was performed with scanning electron microscopy (SEM) to observe the fracture surfaces of specimens. ANOVA and Tukey tests were used for the statistical analysis (p < 0.05).
Results:
Statistical analysis revealed significant differences in strength between groups. The flexural strength improved with the addition ZnO nanoparticles. Highest mean value was observed in Group nZn -14 (91.31 MPa) and lowest in control Group nZn-0 (61.36 MPa). ANOVA and Tukey’s honestly significance test found statistical significant differences among the groups ( p<0.001).
Conclusion:
The addition of ZnO nanoparticles in all concentrations increased the flexural strength of acrylic resin when compared to the control group.
Keywords: Flexural strength, heat cure acrylic, nano particles, poly methyl metha acrylate, zinc oxide
Introduction
Polymethyl methacrylate (PMMA) is the commonly used denture base material. It possesses a combination of favorable characteristics such as easy laboratory manipulation, light weight, inexpensive fabrication, stability in the oral environment, lack of toxicity and appropriate aesthetic and color matching ability (1,2). Limitations inherent in the resin are poor fatigue failure, high coefficient of thermal expansion, low thermal conductivity, dimensional inaccuracy, denture fracture and wear of the denture teeth (3,4). Clinicians encounter fracture of denture to low resistance to impact, flexural, or fatigue stresses (5). In order to prevent fracture of the dentures, the thickness of acrylic resin in susceptible regions was increased or reinforced (6). Copolymerization by rubber (7), reinforcement by incorporation of different forms like metallic wire (8), fibers (9, 10,11) and the use of metallic oxides (12) were attempted to improve the properties of PMMA denture base resins.
Nanoparticles have been increasingly used in material science for its wear and tear resistance and anti-corrosion abilities. The alteration of filler size improves the properties of the material (13). The earlier studies conducted showed a marginal improvement of flexural strength but had several shortcomings in fatigue life, fatigue crack, propagation resistance and long term wear that restricted immediate clinical application (14,15,16,17). The search exists with more ideal reinforcement. The nano materials and technology provides wider opportunity in identifying the better reinforcement material.
Nano zinc oxide (ZnO) has excellent antibacterial, antifungal properties. ZnO in blending with denture base resins can improve the properties of denture base resins, significantly the biological properties of acrylic resins. This study was done with the objective to evaluate the flexural strength of PMMA with various concentrations of Zn O nanoparticles.
Materials and methods
A total of 60 heat cure acrylic denture base specimens (DPI Heat Cure, India) with dimension of 65mm x 40mm x 5mm were fabricated according to manufacturer’s recommendations. The specimens were divided into six groups for flexural strength evaluation (n=10). Sample distribution and composition of material listed in Table 1.
Table 1.
Sample distribution.
| Group | Sample | ZnO nanoparticles Conc. |
|---|---|---|
| nZn0 | 10 | - |
| nZn4 | 10 | 0.4 |
| nZn6 | 10 | 0.6 |
| nZn8 | 10 | 0.8 |
| nZn12 | 10 | 1.2 |
| nZn14 | 10 | 1.4 |
The heat cure acrylic resin (DPI Heat Cure, India) with liquid monomer and polymer powder of 0.10mm particle was used for specimen fabrication. ZnO nanoparticles of 12 nm particles were procured from external source (Zigma Elhrich). Zinc oxide nanoparticles are incorporated into the heat cure polymer by twin screw extruder. Specimen groups were fabricated with 0.4 % (group nZn4 ), 0.6% (group nZn6), 0.8% (group nZn8), 1.2% (group nZn12) and 1.4% (group nZn14) nano ZnO by weight. The specimens were fabricated by mixing the nano ZnO with monomer in ratio of 25g/10ml. Initially a master die was prepared according to ISO 20795.1.2013 with dimension of 65mm x 40mm x 5mm. The master die was duplicated with addition silicone impression material and resin specimen were fabricated with the specified dimensions by compression molding technique, processed by long heat cure polymerization cycle, trimmed with acrylic stone and finished with 600 grit sandpaper [Fig 1]. Each prepared specimen was cut lengthways with milling machine into three equal strips, 64 mm long, (10,0 ± 0,2) mm wide, and (3,3 ± 0,2) mm in height. The samples were subjected to a three-point bending test in universal testing machine (Autograph universal testing machine, Shimadzu Corp, Japan). The flexural strength was tested by applying a load until fracture at the midpoint of specimen by means of a hardened steel cylinder with a cross head of 1mm/min. The flexural strength in MPa was calculated using the equation, M = 3WI/2bd² Where M = flexural strength (MPa), W = fracture load (N), I = test span (center to center) distance between support points (mm), B = width of specimen (mm) and d = thickness of the specimen (mm). The mean flexural strength of each group was calculated, tabulated and statistically analyzed with ANOVA and Tukey HSD test.
Results
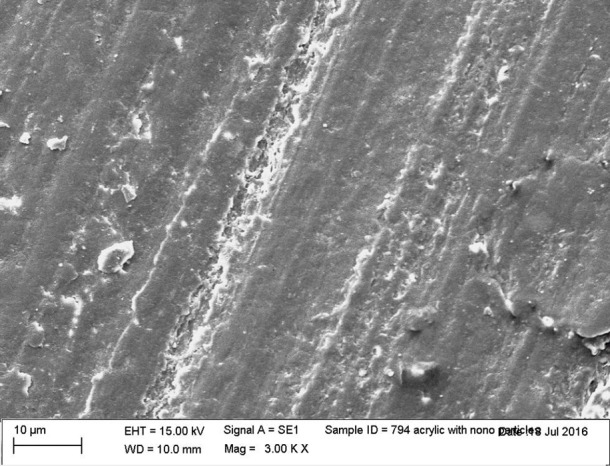
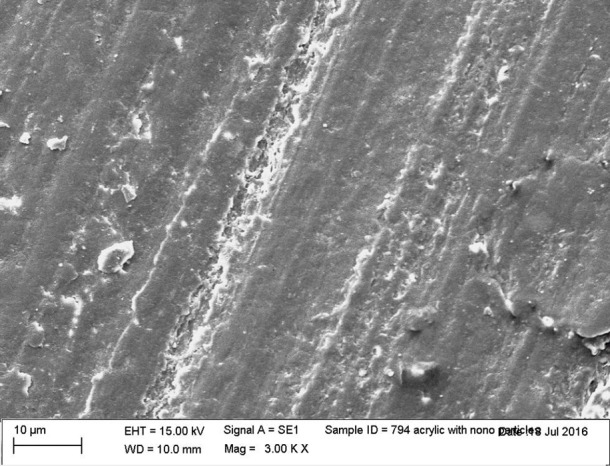
The mean flexural strength of specimen ispresented in Table 2. Group nZn0 control group showed lesser strength of 61.3 MPa and Group nZn14 – 91.31 MPa was the highest when compared to other groups. The flexural strength increased with the concentration of ZnO. Group nZn-4 to Group nZn-14 exhibited increase in strength of 71.73 MPa,77.05 MPa, 84.98 MPa, 86.92 MPa and 91.31 MPa. The data analysis was executed using statistical software SPSS Version 20.0 (SPSS Inc., Chicago, IL). ANOVA displayed statistically significant differences among the 6 groups (p<0.5). The Post hoc test multiple comparisons Tukey’s HSD revealed significant differences. The scanning electron microscope (SEM) revealed the distribution of the nanoparticles in PMMA and the fracture of the material occurred in the midst of the nano particles (Figure 1,Figure 2,Figure 3,Figure 4,Figure 5,Figure 6).
Table 2.
Descriptive Analysis on flexural strength.*Oneway p less than 0.001 (99.9 % sig), SD: Standard Deviation
| 95% Confidence Interval for Mean | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Groups | N | Mean | Std. Deviation | Std. Error | Lower Bound | Upper Bound | Minimum | Maximum | P value |
| nZn0 | 10 | 61.36 | 4.91 | 1.55 | 57.85 | 64.88 | 52.48 | 67.38 | .000* |
| nZn4 | 10 | 71.73 | 3.49 | 1.10 | 69.23 | 74.22 | 66.49 | 77.52 | .000* |
| nZn6 | 10 | 77.05 | 2.41 | .76 | 75.33 | 78.77 | 73.36 | 81.22 | .000* |
| nZn8 | 10 | 84.98 | 2.49 | .79 | 83.57 | 86.77 | 80.79 | 88.02 | .000* |
| nZn12 | 10 | 86.92 | 1.89 | .59 | 85.57 | 88.28 | 83.16 | 89.32 | .000* |
| nZn14 | 10 | 91.31 | 1.15 | .36 | 90.48 | 92.13 | 89.59 | 92.68 | .000* |
| Total | 60 | 78.89 | 10.62 | 1.37 | 76.15 | 81.64 | 52.48 | 92.68 | |
Figure 1.
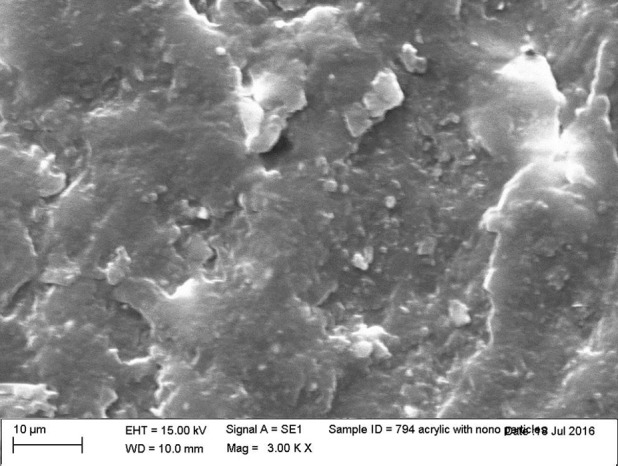
SEM of heat cure acrylic with no reinforcement.
Figure 2.
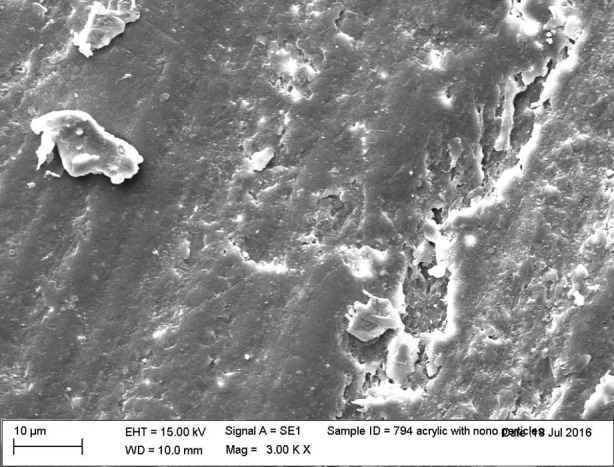
SEM of n Zn 4 nanoparticles reinforcement specimen.
Figure 3.
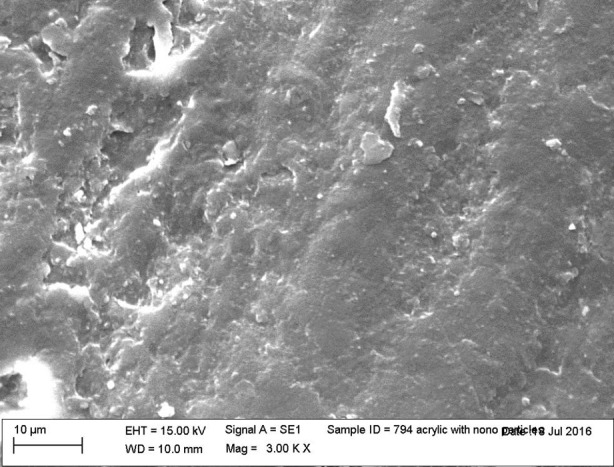
SEM of n Zn 6 nanoparticles reinforcement specimen.
Figure 4.
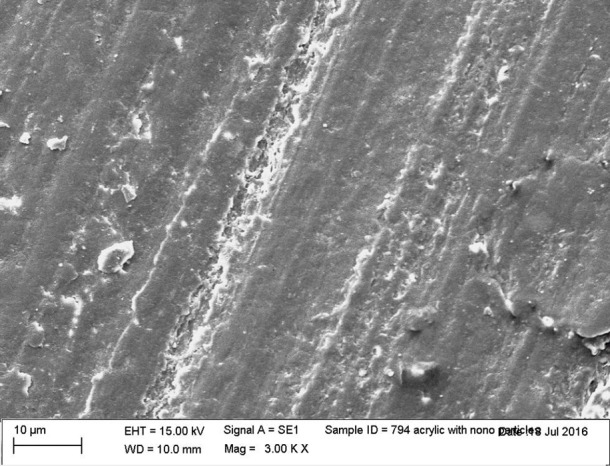
SEM of n Zn8 nanoparticles reinforcement specimen.
Figure 5.
SEM of nZn12 nanoparticles reinforcement specimen.
Figure 6.
SEM of nZn14 nanoparticles reinforcement specimen.
Discussion
The flexural strength of PMMA denture base resins improved with the concentrations of nano Zn0. Rahim et al (18) established that the addition of metal nanoparticles increases the surface hydrophobicity and reduce the agglomeration of biomolecules. The studies on aluminum dioxide (19), cobalt- chromium (20), silver (21), zinc oxide (22), zirconia (23), titanium dioxide (24) nano particles have improved the flexural strength and documented the theory of surface hydrophobicity and decreased molecular agglomeration (25).
Nano particles are considered over macroscopic materials for their higher surface to volume ratios and an increased percentage of atoms at the grain boundary. The nano particles reduces the filler size increases the compaction of materials improves the mechanical properties of materials (15,16,17). Various nanoscale fillers, including silica, calcium carbonate, and metal oxides when added to dental -polymer matrix improved the properties. Nano-sized ZnO fillers was considered because of the unique physical properties, low cost and extensive applications in diverse areas (26,27,28). Xie et al. (27) observed the antibacterial properties of ZnO nanoparticles. Studies have indicated that ZnO nanoparticles at a concentration of between 3 and 10mM caused 100% inhibition of bacterial growth. Additionally, ZnO has superior biocompatibility properties and less likely to alter esthetics of denture base. The percentages of ZnO nano particles analyzed had effective antibacterial effect, obtained from the studies of Xie et al (27), Raj et al. (29).
The polymerization reaction is significant in determining the mechanical properties of denture base resin. The availability and generation of free radicals, the control of temperature during polymerization are some of the significant factors that influence the properties of the material. The compression molding technique and long curing polymerization cycle enabled to obtain to optimize the procedure and aided in obtaining the superior flexural strength.
The nanoparticles where incorporated by twin stage extruder. It aided is better dispersion in polymer matrix and homogenous distribution of the particles. The addition of nano particles to resin matrix is significant in improving the properties. The technique adapted aided in better distribution and it is visualized in SEM (28).
The study followed stringent testing protocol. Fewer limitations were unavoidable in the testing set up. In future, different concentrations of particles, size of particles, custom made nano particles, other forms of nano rods, tubes, polymerization techniques, types of PMMA resins can be evaluated. More studies are required to evaluate thermal properties , impact strength, mechanical, physical, antifungal and antibacterial spectrum for better interpretation.
Conclusion
Within the limitation of this study it can be concluded that the flexural strength of PMMA denture base increased with the addition ZnO nano particle to the PMMA denture base.
Footnotes
Ethics committee approval: Not required.
Informed consent:Not required.
Peer review: Externally peer-reviewed.
Author contributions:NGC designed the study. SV and NGC participated in generating the data for the study. SV and NGC participated in gathering the data for the study. SV participated in the analysis of the data. NGC wrote the majority of the original draft of the paper. NGC participated in writing the paper. All authors approved the final version of this paper.
Conflict of interest:The authors have no conflicts of interest to declare.
Financial disclosure:The authors declared that this study has received no financial support.
Acknowledgment:We thank Prof. Dr. B. Muthukumar, Head of Department for his support and guidance.
References
- 1.Salman, et al. . The influence of adding of modified ZrO2-TiO2 nanoparticles on certain physical and mechanical properties of heat polymerized acrylic resin. J Bagh College Dentistry. 2015;27(3):33–9. 10.12816/0015032 [DOI] [Google Scholar]
- 2.Zappini G, Kammann A, Wachter W. Comparison of fracture tests of denture base materials. J Prosthet Dent. 2003. December;90(6):578–85. 10.1016/j.prosdent.2003.09.008 [DOI] [PubMed] [Google Scholar]
- 3.McCabe JF, Walls AW. Applied Dental Materials. John Wiley & Sons; 2013. p. 591. [Google Scholar]
- 4.Jasim BS, Ismail IJ. The effect of silanized alumina nano-fillers addition on some physical and mechanical properties of heat cured polymethyl methacrylate denture base material. J Bagh College of Dentistry. 2014;26(2):18–23. 10.12816/0015190 [DOI] [Google Scholar]
- 5.Asar NV, Albayrak H, Korkmaz T, Turkyilmaz I. Influence of various metal oxides on mechanical and physical properties of heat-cured polymethyl methacrylate denture base resins. J Adv Prosthodont. 2013. August;5(3):241–7. 10.4047/jap.2013.5.3.241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aljafery AM, Hussain BM. Effect of addition ZrO2-Al2O3 nanoparticles mixture on some properties and denture base adaptation of heat cured acrylic resin denture base material. J Bagh College of Dentistry. 2015;27(3):15–21. 10.12816/0015028 [DOI] [Google Scholar]
- 7.Ochi M, Shimaoka S. Phase structure and toughness of siliconemodified epoxy resin with added silicone graft copolymer. Polymer (Guildf). 1999;40(5):1305–12. 10.1016/S0032-3861(98)00263-8 [DOI] [Google Scholar]
- 8.Vojdani M, Khaledi AA. Transverse strength of reinforced denture base resin with metal wire and E-glass fibers. JDT. 2006;3:159–66. [Google Scholar]
- 9.Kassab BT, Al-Nema LM. Evaluation of some mechanical properties of reinforced acrylic resin denture base material (An In vitro study). Al-Rafidain Dent J. 2009;9:57–65. [Google Scholar]
- 10.Raszewski Z, Nowakowska D. Mechanical properties of hot curing acrylic resin after reinforced with different kinds of fibers. Int J Biomedical Materials Res. 2013;1(1):9–13. 10.11648/j.ijbmr.20130101.12 [DOI] [Google Scholar]
- 11.Deepan N, Prakash A, Rao B, Sonthalia A. In vitro Evaluation and comparison of transverse and impact strength of heat polymerized acrylic resin reinforced with polyethylene fibers and polypropylene fibers. J Adv Med Dent Sci. 2014;2:46–56. [Google Scholar]
- 12.Jagger DC, Harrison A, Jandt KD. The reinforcement of dentures. J Oral Rehabil. 1999;26(3):185–94. 10.1046/j.1365-2842.1999.00375.x [DOI] [PubMed] [Google Scholar]
- 13.Sandhu JS, Kaur G. Nanodentistry: The Changing Trends in Dentistry. Int J Nanomedicine. 2011;6:2799–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khaled SM, Miron RJ, Hamilton DW, Charpentier PA, Rizkalla AS. Reinforcement of resin based cement with titania nanotubes. Dent Mater. 2010. February;26(2):169–78. 10.1016/j.dental.2009.09.011 [DOI] [PubMed] [Google Scholar]
- 15.Gad MM, Fouda SM, Al-Harbi FA, Näpänkangas R, Raustia A. PMMA denture base material enhancement: a review of fiber, filler, and nanofiller addition. Int J Nanomedicine. 2017. May;12:3801–12. 10.2147/IJN.S130722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cevik P, Yildirim-Bicer AZ. The Effect of Silica and Prepolymer Nanoparticles on the Mechanical Properties of Denture Base Acrylic Resin. J Prosthodont. 2018. October;27(8):763–70. 10.1111/jopr.12573 [DOI] [PubMed] [Google Scholar]
- 17.Ladha K, Shah D. An in-vitro evaluation of the flexural strength of heat-polymerized poly (methyl methacrylate) denture resin reinforced with fibers. J Indian Prosthodont Soc. 2011. December;11(4):215–20. 10.1007/s13191-011-0086-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rahim, et al. . Incorporation of silica nanoparticles to increase the mechanical properties. J Physiol Sci. 2011;22:32–105. [Google Scholar]
- 19.Pfeiffer P, Rolleke C, Sherif L. Flexural strength and moduli of hypoallergenic denture base materials. J Prosthet Dent. 2005. April;93(4):372–7. 10.1016/j.prosdent.2005.01.011 [DOI] [PubMed] [Google Scholar]
- 20.Maruo Y, Nishigawa G, Oka M, Minagi S, Suzuki K, Irie M. Does plasma irradiation improve shear bond strength of acrylic resin to cobalt-chromium alloy?. Dent Mater. 2004. June;20(5):509–12. 10.1016/j.dental.2003.04.001 [DOI] [PubMed] [Google Scholar]
- 21.Yan Z, Liqin G, Xiuli Q, Lixia G.. Study on PET fiber modified by silver carrying zinc oxide nanoparticles. China Synthetic Fiber Industry 2005-04.
- 22.Ayad NM, Badawi MF, Fatah AA. Effect of reinforcement of high impact acrylic resin with zirconia on some physical and mechanical properties. Rev ClinPesqOdontol. 2008;4:145–51. [Google Scholar]
- 23.Harini P, Mohamed K, Padmanabhan TV. Effect of Titanium dioxide nanoparticles on the flexural strength of polymethylmethacrylate: an in vitro study. Indian J Dent Res. 2014. Jul-Aug;25(4):459–63. 10.4103/0970-9290.142531 [DOI] [PubMed] [Google Scholar]
- 24.Bhavikatti SK, Bhardwaj S, Prabhuji ML. Current applications of nanotechnology in dentistry: a review. Gen Dent. 2014. Jul-Aug;62(4):72–7. [PubMed] [Google Scholar]
- 25.Harishanand, et al. . Comparitive Study on Mechanical Properties of ZnO, ZrO2 and CeO2 Nanometal Oxides Reinforced Epoxy Composites, Advances in Polymer Science and Technology. Int J. 2013;3:7–13. [Google Scholar]
- 26.Alexandre M, Dubois P. Polymer-layered silicate nanocomposites: preparation, properties and uses of a new class of materials. Mater Sci Eng Rep. 2000;28(1-2):1–63. 10.1016/S0927-796X(00)00012-7 [DOI] [Google Scholar]
- 27.Xie Y, He Y, Irwin PL, Jin T, Shi X. Antibacterial activity and mechanism of action of zinc oxide nanoparticles against Campylobacter jejuni. Appl Environ Microbiol. 2011. April;77(7):2325–31. 10.1128/AEM.02149-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang XY, Wu WL, Bian YM, Zhu BS, Yu WQ. [The effect of different dispersive methods on flexural strength nano-ZrO(2) reinforced denture polymethyl methacrylate]. Shanghai Kou Qiang Yi Xue. 2009. June;18(3):313–6. [PubMed] [Google Scholar]
- 29.Raj I, Mozetic M, Jayachandran VP, Jose J, Thomas S, Kalarikkal N. Fracture resistant, antibiofilm adherent, self-assembled PMMA/ZnO nanoformulations for biomedical applications: physico-chemical and biological perspectives of nano reinforcement. Nanotechnology. 2018. July;29(30):305704. 10.1088/1361-6528/aac296 [DOI] [PubMed] [Google Scholar]


