Short abstract
Objective
This systematic review and meta-analysis was performed to evaluate the efficacy of using a helmet for oxygen therapy in critically ill patients with respiratory failure.
Methods
The Cochrane Library, Embase, and PubMed databases were searched for all randomized controlled trials (RCTs) examining the efficacy of a helmet versus standard oxygen therapy or a mask in critically ill patients with respiratory failure. The quality of all included studies was evaluated by the method recommended by The Cochrane Collaboration. The systematic review and meta-analysis was conducted using Review Manager software, version 5.3 (Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark).
Results
Ten RCTs involving 708 patients were included in the present meta-analysis. The results of the meta-analysis showed that the oxygenation index, partial pressure of carbon dioxide, and complications were not significantly different between the helmet group and the standard oxygen therapy or mask group. The incidence of intubation and the mortality rate were significantly lower in the helmet group than in the standard oxygen therapy or mask group.
Conclusion
Delivering oxygen via a helmet can decrease the incidence of required intubation and improve the mortality rate, resulting in beneficial outcomes in critically ill patients with respiratory failure.
Keywords: Helmet, oxygen therapy, mask, critically ill patients, respiratory failure, noninvasive ventilation
Introduction
The clinical value of noninvasive ventilation (NIV) in the form of continuous positive airway pressure (CPAP) for patients with acute respiratory failure has been increasingly affirmed, especially for patients with acute respiratory distress syndrome, pulmonary interstitial fibrosis, immune dysfunction, and similar disorders.1–3 Because of its unique structure, a helmet device is associated with a lower incidence of noninvasive positive-pressure ventilation (NIPPV)-related complications than is a normal mask, providing significant advantages.4–7 However, noninvasive mechanical ventilation with a helmet may lead to carbon dioxide (CO2) retention and hypercarbia.8 Because of the limitations of studies performed by different research groups and the small sample size of single-centre studies, the present review and meta-analysis was performed to analyse the results of using a helmet for critically ill patients with respiratory failure. In terms of conventional oxygen therapy, ordinary mask NIPPV and routine nasal catheters are commonly used in patients with severe hypoxaemia. To improve the statistical efficiency of the analysis and reduce the heterogeneity among the study population, this investigation was conducted as a systematic review and meta-analysis of randomized controlled trials (RCTs) comparing a helmet and conventional oxygen therapy to objectively evaluate the clinical efficacy of a helmet for critically ill patients with respiratory failure.
Materials and methods
Search strategy
Two investigators independently searched PubMed, Elsevier and Cochrane (Central) for clinical RCTs of critically ill patients receiving helmet oxygen therapy and conventional oxygen therapy. A literature search from 1 January 1995 to 31 December 2018 was carried out using the following search keywords and terms: (“respiratory failure” or “hypoxemic respiratory failure” or “hypoxemic respiratory distress” or “ARF” or “AHRF”) and (“nippv” or “bipap” or “cpap” or “niv” or “nipsv” or “noninvasive positive pressure ventilation” or “non invasive positive pressure ventilation” or “noninvasive ventilation” or “non invasive ventilation” or “bilevel positive airway pressure” or “continuous positive airway pressure” or “noninvasive pressure support ventilation” or “non invasive pressure support ventilation” or “mask ventilation” or “helmet ventilation” or “oxygen therapy”). The search was limited to published studies and, with reference to the literature, was based on the authors’ request for the full text and the original data.
Data screening and extraction
Citation titles and abstracts were independently screened by two reviewers (T.Y. and T.W.). All potentially eligible papers were retrieved in full. The references of all retrieved articles were examined to identify additional potentially eligible studies. The trial characteristics and outcomes were independently recorded by the two reviewers using a predesigned data abstraction form. In cases of disagreement, all the authors jointly reviewed the article in question until a consensus was reached. Any duplicate papers were identified and excluded from the meta-analysis. The literature inclusion criteria were as follows: (1) study type: group design RCT; (2) study population: severely ill patients being treated in the intensive care unit; (3) intervention measures: the experimental group used helmet-based ventilation and the control group used mask ventilation or conventional oxygen therapy, and a clear description of the specific oxygen therapy was provided; and (4) outcome measures: oxygenation index, partial pressure of CO2 (PaCO2), rate of requirement of tracheal intubation, incidence of complications, and mortality rate. If the information provided in the article was not complete, contact with the original author was made to supplement the data; if the necessary amount of original data could not be obtained, the study was excluded.
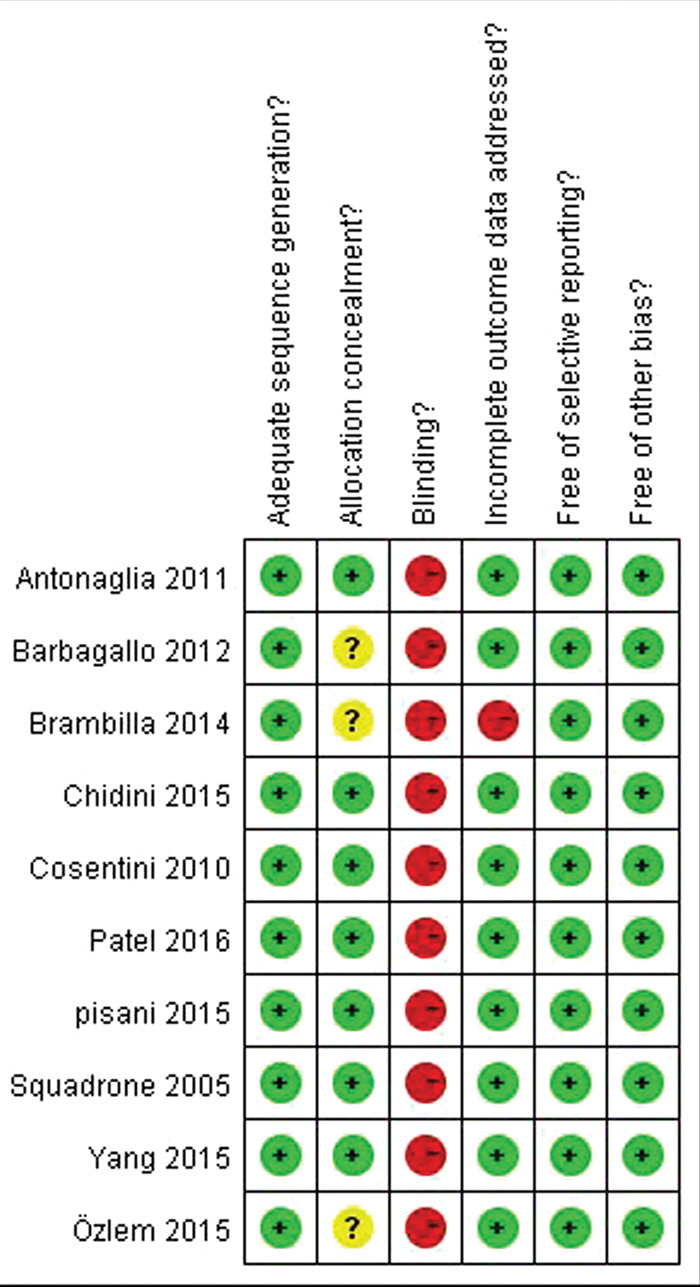
Grading the evidence
We evaluated the quality of the trials by applying the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) (GRADEpro GDT 2016; https://gradepro.org/).9 This system grades the quality of studies as high, moderate, low, or very low based on the quality of design, limitations, inconsistencies, indirectness, imprecision, and possible publication bias. Two investigators (T.Y. and T.W.) independently evaluated the studies, abstracted the data on methods and outcomes, and assessed the risk of bias.
Endpoints
The primary endpoint was to determine the potentially beneficial role of noninvasive mechanical ventilation with a helmet in terms of mortality in critically ill patients with respiratory failure; the cut-off points for mortality as defined within each study were used in the meta-analysis. The secondary endpoints were whether the helmet improved the oxygenation index, PaCO2, and the need for tracheal intubation in patients with respiratory failure. We also examined whether differences in complications existed among patients with a helmet versus standard oxygen therapy or a mask.
Statistical analyses
Data related to the oxygenation index, PaCO2, need for tracheal intubation, incidence of complications, and mortality rate in the overall population as well as in the in-hospital and pre-hospital subgroups were extracted, and a consecutive analysis for subgroups was performed (filtered according to the analysed variable). For dichotomous outcomes, risk ratios (RRs) with 95% confidence intervals (CIs) were used to represent the effects of helmet use on different outcomes. An RR of <1 favoured the use of a therapeutic helmet. Data were pooled only when adequate clinical and methodological similarities were present between the studies. The homogeneity assumption was assessed using the I2 value, which describes the percentage of total variation across studies that is due to heterogeneity rather than chance. I2 was computed as I2 = 100% × (Q − df)/Q, where Q is the Cochrane heterogeneity statistic and df represents the degrees of freedom. A value of 0% indicated no observed heterogeneity, and larger values were indicative of increasing heterogeneity. Between-study heterogeneity was assessed with the I2 test using P < 0.1 as the threshold for statistical significance.10 Publication bias was estimated using a funnel plot. Parametric variables are presented as mean ± standard deviation, and nonparametric variables are presented as median and interquartile range. Statistical analyses were conducted using Review Manager software, version 5.3 (Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark). A P-value of <0.05 was considered to indicate statistical significance.
Results
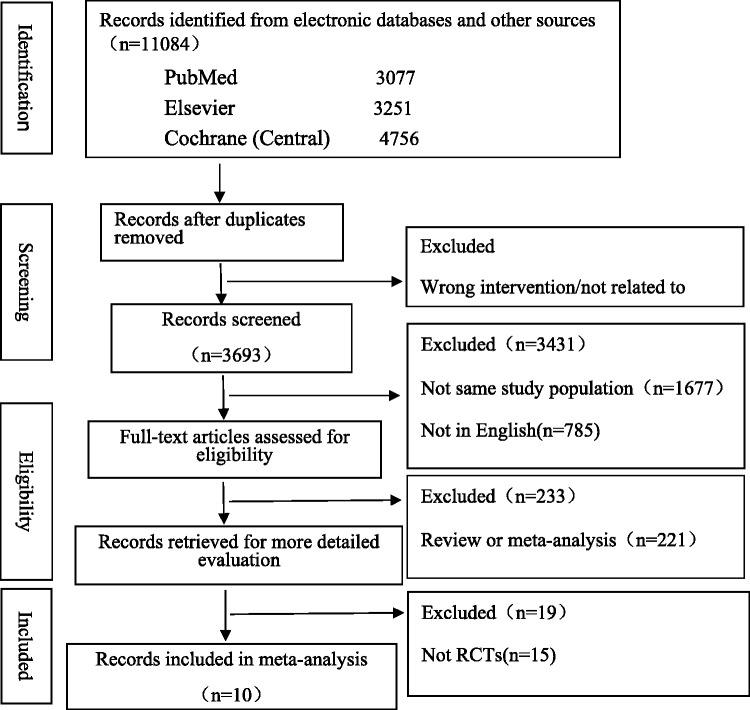
A flowchart of the study selection process is shown in Figure 1. Ten studies met the conditions for inclusion in the meta-analysis.8,11–19 These studies were published from 2005 to 2016 and included 708 patients (355 in the helmet group and 353 in the control group). The characteristics of the studies are shown in Figure 2.
Figure 1.
Flow diagram of the selection of studies for the meta-analysis. RCT, randomized controlled trial.
Figure 2.
Characteristics of the included studies examining the efficacy of a helmet versus standard oxygen therapy or a mask in patients with respiratory failure.
Outcomes
Helmet and oxygenation index outcomes
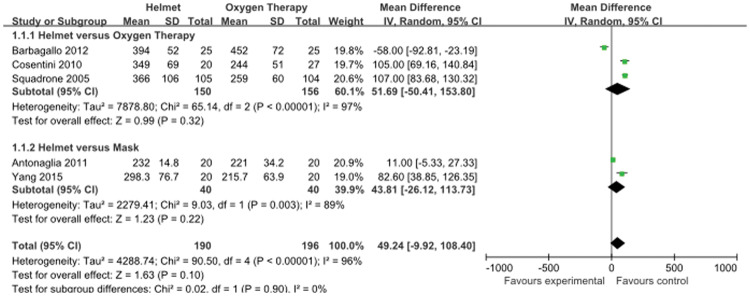
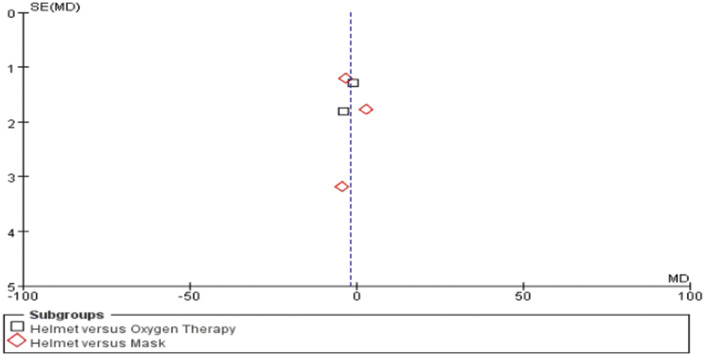
Five studies8,12,15,16,19 compared the effects of each therapy on the oxygenation index. Significant heterogeneity was present (I2 = 96%, P < 0.0001), and a random-effects model was used to analyse the results. As shown in Figure 3, use of a helmet did not have a significant effect on the oxygenation index [weighted mean difference (WMD), 49.24; 95% CI, −9.92 to 108.40] when the control group received standard oxygen therapy or mask ventilation. The effects of a helmet and standard oxygen therapy on the oxygenation index were compared in three studies.12,16,19 The results of this analysis showed that use of a helmet did not have a significant effect on the oxygenation index compared with use of standard oxygen therapy (WMD, 51.69; 95% CI, −50.41 to 153.80). The other two studies8,15 compared the effects of helmet and mask ventilation on the oxygenation index. The results showed that use of a helmet did not have a significant effect on the oxygenation index compared with use of the common mask (WMD, 43.81; 95% CI, −26.12 to 113.73). Publication bias was detected using a funnel plot assessment (Figure 4).
Figure 3.
Effects on the oxygenation index in patients with respiratory failure in the helmet and control subgroups using a random-effects analysis, with a forest plot showing mean differences between the helmet and control groups. Squares and horizontal lines indicate the mean difference and 95% CI for each trial; the size of each square is proportional to the statistical weight of the trial in the meta-analysis. Diamonds indicate the estimated effect derived from the meta-analysis, with the centre indicating the point estimate and the left and right points indicating 95% CIs. SD, standard deviation; CI, confidence interval.
Figure 4.
Funnel plot for publication bias regarding the effect of a helmet on the oxygenation index. Each point represents a separate study included in the meta-analysis. Squares indicate studies assessing the effects of a helmet compared with standard oxygen therapy. Diamonds indicate studies assessing the effects of a helmet compared with a mask. SE, standard error; MD, mean difference.
Helmet and PaCO2 outcomes
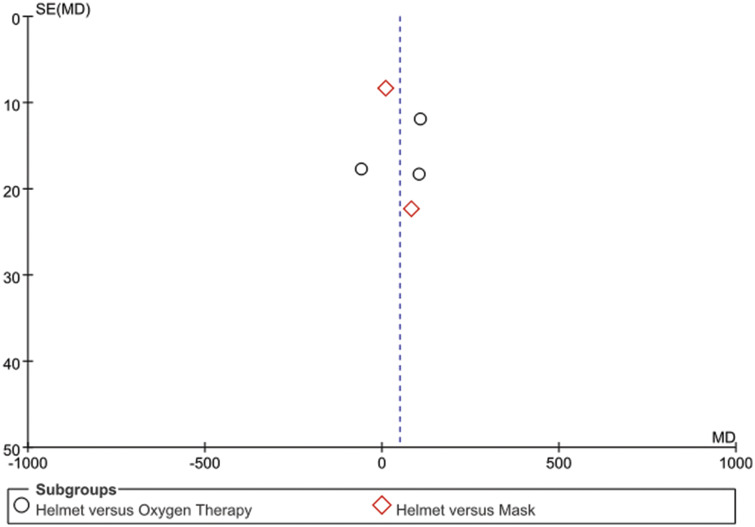
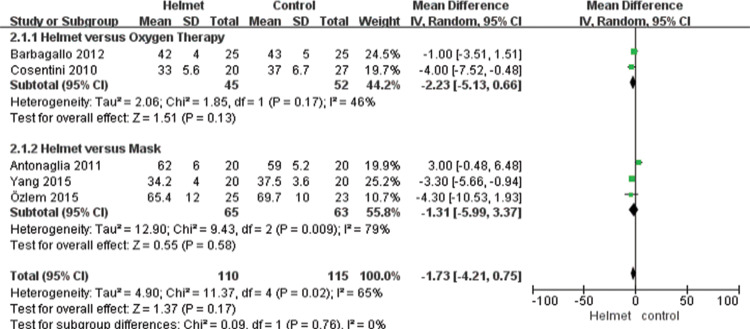
Five studies8,11,15,16,19 compared the effects of each therapy on PaCO2. Significant heterogeneity was present across the studies (I2 = 65%, P = 0.02), and a random-effects model was used for the analysis. The results showed that use of a helmet did not have significant effect on PaCO2 (WMD, −1.73; 95% CI, −4.21 to 0.75) when the control group received standard oxygen therapy or mask ventilation. The effect of a helmet and standard oxygen therapy on PaCO2 was compared in two studies.16,19 The results showed that compared with standard oxygen therapy, the helmet did not have a significant effect on PaCO2 (WMD, −2.23; 95% CI, −5.13 to 0.66). The other three studies8,11,15 compared the effect of helmet and mask ventilation on PaCO2. The results showed that use of a helmet did not have a significant effect on PaCO2 compared with the common mask (WMD, −1.31; 95% CI, −5.99 to 3.37) (Figure 5). Publication bias was detected using a funnel plot assessment (Figure 6).
Figure 5.
Effects on partial pressure of carbon dioxide (PaCO2) in patients with respiratory failure in the helmet and control subgroups using a random-effects analysis, with a forest plot showing mean differences between the helmet and control groups. Squares and horizontal lines indicate the mean difference and 95% CIs for each trial; the size of each square is proportional to the statistical weight of the trial in the meta-analysis. Diamonds indicate the estimated effect derived from the meta-analysis, with the centre indicating the point estimate and the left and right points indicating 95% CIs. SD, standard deviation; CI, confidence interval.
Figure 6.
Funnel plot for publication bias regarding the effect of a helmet on partial pressure of carbon dioxide (PaCO2). Each point represents a separate study included in the meta-analysis. Squares indicate studies assessing the effects of a helmet compared with standard oxygen therapy. Diamonds indicate studies assessing the effects of a helmet compared with a mask. SE, standard error; MD, mean difference.
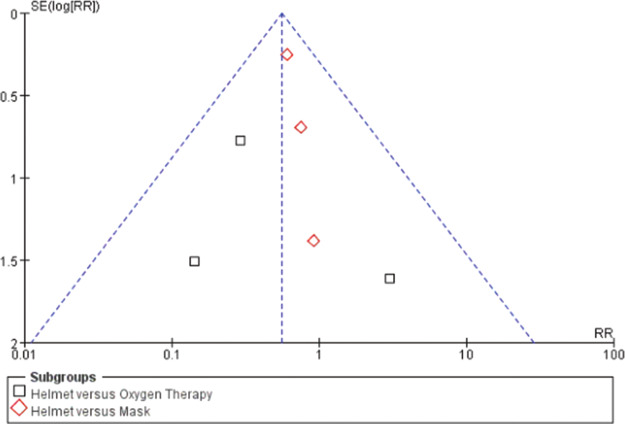
Helmet and tracheal intubation outcomes
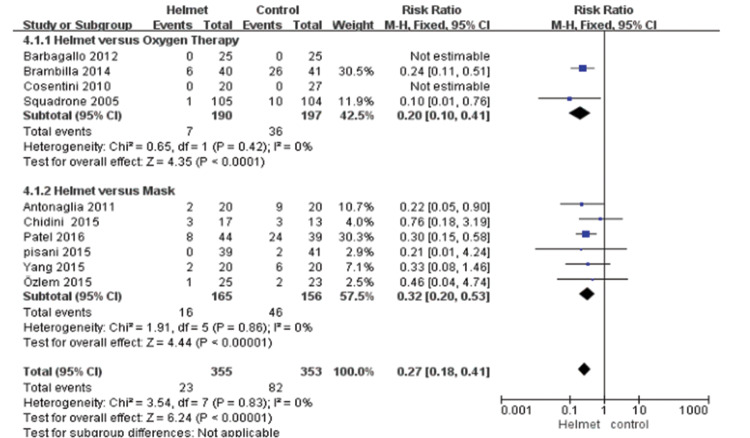
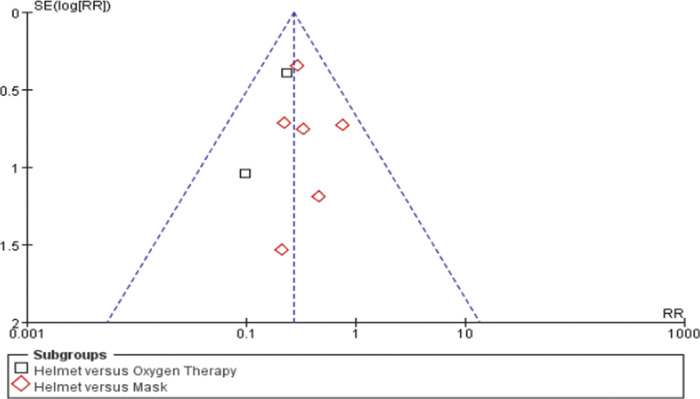
Ten studies8,11–19 compared the effects of each therapy on the incidence of the need for tracheal intubation. No heterogeneity was present (I2 = 0%), and a fixed-effects model was used for the analysis. The results showed that use of a helmet significantly reduced the incidence of endotracheal intubation (RR, 0.27; 95% CI, 0.18–0.41; P < 0.00001) when the control group received either standard oxygen therapy or mask ventilation. The incidence rate of tracheal intubation was compared between a helmet and standard oxygen therapy in four studies.12,16,17,19 The results showed that use of a helmet significantly reduced the incidence of tracheal intubation (RR, 0.20; 95% CI, 0.10–0.41; P < 0.00001). The other six studies8,11,13–15,18 compared the effect of helmet and mask ventilation on the incidence of tracheal intubation. The results showed that use of a helmet significantly reduced the incidence of tracheal intubation compared with the common mask (RR, 0.32; 95% CI, 0.20–0.53; P < 0.00001) (Figure 7). No publication bias was detected using a funnel plot assessment (Figure 8).
Figure 7.
Effects on intubation in patients with respiratory failure in the helmet and control subgroups using a fixed-effects analysis, with a forest plot showing the risk ratio for helmet versus control. Squares and horizontal lines indicate the risk ratio and 95% CIs for each trial; the size of each square is proportional to the statistical weight of the trial in the meta-analysis. Diamonds indicate the estimated effect derived from the meta-analysis, with the centre indicating the point estimate and the left and right points indicating 95% CIs. SD, standard deviation; CI, confidence interval.
Figure 8.
Funnel plot for publication bias regarding the effect of a helmet on intubation. Each point represents a separate study included in the meta-analysis. Squares indicate studies assessing the effects of a helmet compared with standard oxygen therapy. Diamonds indicate studies assessing the effects of a helmet compared with a mask. RR, risk ratio; SE, standard error.
Helmet and complications outcomes
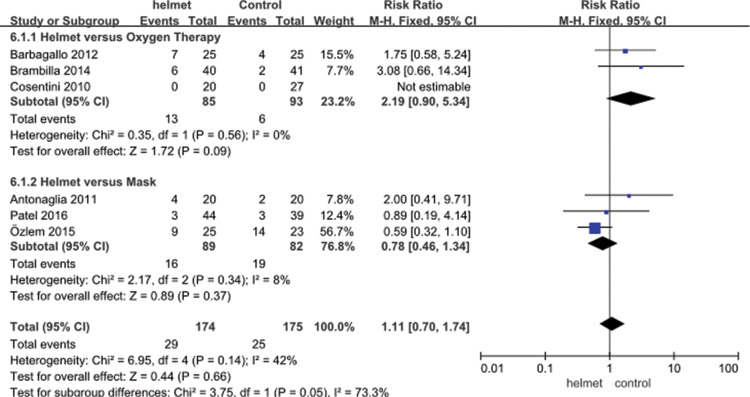
Six studies8,11,14,16,17,19 compared the effects of each therapy on the incidence of complications. No heterogeneity was present (I2 = 42%), and a fixed-effects model was used for the analysis. The results showed that use of a helmet did not have a significant effect on reducing complications (RR, 1.11; 95% CI, 0.70–1.74) when the control group received either standard oxygen therapy or mask ventilation. The effect of a helmet and standard oxygen therapy on the incidence of complications was compared in three studies.8,11,14 The results showed that compared with standard oxygen therapy, use of a helmet did not have a significant effect on the incidence of complications (RR, 2.19; 95% CI, 0.90–5.34). The other three studies16,17,19 compared the effect of helmet and mask ventilation on the incidence of complications. The results showed that use of a helmet did not have a significant effect on the incidence of complications compared with mask ventilation (RR, 0.78; 95% CI, 0.46–1.34) (Figure 9). No publication bias was detected using a funnel plot assessment (Figure 10).
Figure 9.
Effects on complications in patients with respiratory failure in the helmet and control subgroups using a fixed-effects analysis, with a forest plot showing the risk ratio for helmet versus control. Squares and horizontal lines indicate the risk ratio and 95% CIs for each trial; the size of each square is proportional to the statistical weight of the trial in the meta-analysis. Diamonds indicate the estimated effect derived from the meta-analysis, with the centre indicating the point estimate and the left and right points indicating 95% CIs. CI, confidence interval.
Figure 10.
Funnel plot for publication bias regarding the effect of a helmet on complications. Each point represents a separate study included in the meta-analysis. Squares indicate studies assessing the effects of a helmet compared with standard oxygen therapy. Diamonds indicate studies assessing the effects of a helmet compared with a mask. RR, risk ratio; SE, standard error.
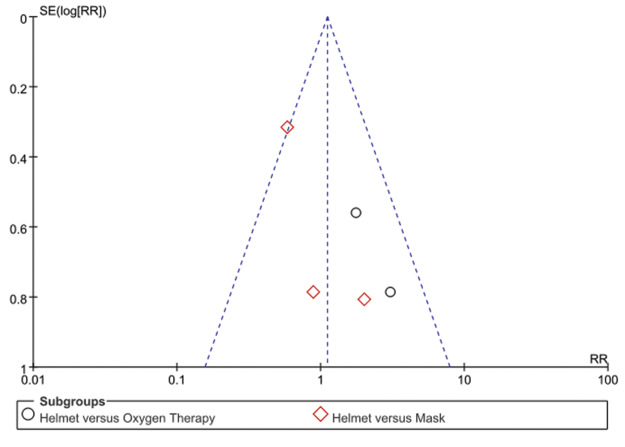
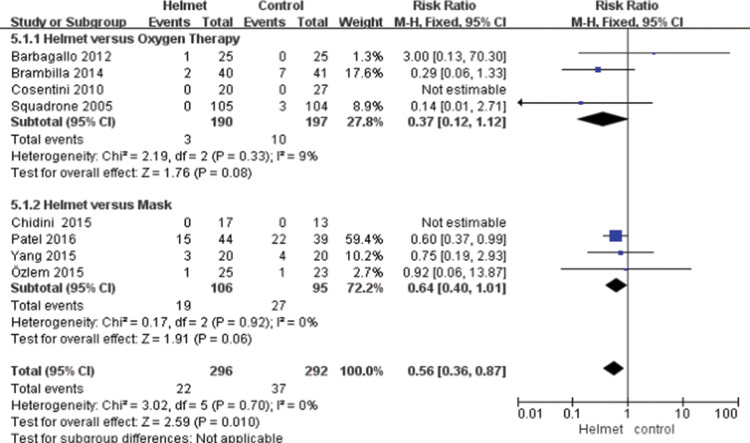
Helmet and mortality outcomes
Eight studies8,11,12,14–17,19 compared the effects of each therapy on the mortality rate. No heterogeneity was present across studies (I2 = 0%), and a fixed-effects model was used for the analysis. The results showed that use of a helmet significantly reduced the incidence of mortality (RR, 0.56; 95% CI, 0.36–0.87; P = 0.010) when the control group received either standard oxygen therapy or mask ventilation. The effect of a helmet and standard oxygen therapy on the mortality rate was compared in four studies.12,16,17,19 The results showed that compared with standard oxygen therapy, use of a helmet did not have a significant effect on the mortality rate (RR, 0.37; 95% CI, 0.12–1.12). The other four studies8,11,14,15 compared the effect of helmet and mask ventilation on the mortality rate. The results showed that use of a helmet did not have a significant effect on the mortality rate compared with a common mask (RR, 0.64; 95% CI, 0.40–1.01) (Figure 11). No publication bias was detected using a funnel plot assessment (Figure 12).
Figure 11.
Effects on mortality in patients with respiratory failure in the helmet and control subgroups using a fixed-effects analysis, with a forest plot showing the risk ratio for helmet versus control. Squares and horizontal lines indicate the risk ratio and 95% CIs for each trial; the size of each square is proportional to the statistical weight of the trial in the meta-analysis. Diamonds indicate the estimated effect derived from the meta-analysis, with the centre indicating the point estimate and the left and right points indicating 95% CIs. CI, confidence interval.
Figure 12.
Funnel plot for publication bias regarding the effect of a helmet on mortality. Each point represents a separate study included in the meta-analysis. Squares indicate studies assessing the effects of a helmet compared with standard oxygen therapy. Diamonds indicate studies assessing the effects of a helmet compared with a mask. RR, risk ratio; SE, standard error.
Discussion
To date, 10 RCTs have analysed the impact and efficacy of a helmet relative to conventional oxygen therapy in critically ill patients. The present meta-analysis was performed to clarify the role of a helmet in critically ill patients with respiratory failure compared with standard oxygen therapy or a common mask based on current published data. The main findings were that compared with the control therapy, use of a helmet significantly reduced the incidence of tracheal intubation and mortality but yielded no significant benefit with respect to the oxygenation index; moreover, the helmet did not increase PaCO2 or complications. Clearly, the results of this meta-analysis have important clinical value. Another systematic review showed that compared with standard oxygen therapy, NIV lowered both the short-term mortality rate and the tracheal intubation rate in patients presenting with acute respiratory failure.20 The present study not only compared NIV and standard oxygen therapy but also compared helmet and mask use in patients receiving NIV.
The results of the present meta-analysis show that compared with standard oxygen therapy or a mask, a helmet can reduce the incidence of tracheal intubation and mortality. Although comparatively fewer reports have focused on NIPPV with a helmet, non-human experiments have confirmed that helmet CPAP can maintain airway pressure and improve oxygenation without CO2 retention21 while providing the following advantages: no need for man-machine synchronization, a low incidence of pressure sores, less air leakage, no restrictions on drinking water and expectoration, maintenance of warmth and humidity in the upper airway and preservation of other physiological functions, and no direct blowing of gas. Clinical studies have confirmed that helmet CPAP can relieve hypoxia in patients with community-acquired pneumonia, can improve oxygenation and haemodynamics in patients with acute cardiogenic pulmonary oedema, can reduce the rate of tracheal intubation after abdominal surgery, and is safe and effective for prophylactic application in patients with lobectomy. People with hypoxaemia after cardiac surgery may also benefit.12,16,19,22 Another study confirmed that early extubation followed by immediate NIV application with a full-face mask or helmet can reduce the number of days spent on invasive ventilation without affecting the intensive care unit length of stay in highly selected patients with hypoxaemia.23
The results of this study show that use of a helmet does not have a significant benefit in terms of the oxygenation index and that compared with standard oxygen therapy or a mask, the helmet does not increase PaCO2. As when using the common mask, employing a helmet requires the patient to have effective independent breathing, clear respiratory secretions, and haemodynamic stability. Helmet use includes CPAP and pressure support ventilation modes. Notably, although the overall evaluation results show that a helmet does not increase CO2 retention in patients with severe illness, some reports have indicated that helmet use significantly increases CO2 retention in patients because of repeated CO2 inhalation within the helmet.24 Therefore, the initial clinical use of a helmet needs to be carefully considered, and the application of airway pressure release ventilation may be conducive to the effective discharge of CO2.
The results of this study showed that use of a helmet did not have a significant effect on complications. Ordinary facemask NIPPV has been widely used in clinical practice; however, few studies and reports on helmet NIV have been published. With the use of ordinary facemask NIPPV, especially with long-term noninvasive positive-pressure mechanical ventilation, ulcers or necrosis often appear at the bridge of the nose and on other facial skin, or eye irritation occurs; these complications become problematic when implementing mechanical ventilation for the treatment of clinical problems. To a certain extent, the design and use of the helmet avoid pressure on patients’ facial skin, reduce general mask ventilation-related complications, and improve the condition of patients with severe NIPPV intolerance. Studies have shown that the incidence of gastric flatulence and aspiration is lower with use of a helmet than with use of an ordinary mask, and a unique hood design is conducive to patients requiring extensive oral feeding.25,26 Another study confirmed that in patients with chronic obstructive pulmonary disease, neurally adjusted ventilator assist through a helmet improved comfort, performance, and patient–ventilator synchrony compared with pressure support through a face mask.27 Two recent studies showed that compared with a standard helmet, a new-generation helmet is equally effective in delivering nasal CPAP and more effective in delivering nasal pressure support ventilation, with improved comfort and patient–ventilator interaction.5,28 These findings clearly show that use of a helmet provides effective respiratory therapy in patients with severe respiratory failure.
This study had three main limitations. First, the study had language limitations because it only included literature reported in English. Second, the inclusion of literature examining the oxygenation index and complications and the inclusion of studies involving patients with differences in disease severity may have led to significant heterogeneity (i.e., the study population was not uniform along several dimensions).25 Third, few studies were included in the analysis. Therefore, the safety of a helmet in patients with severe clinical problems requires further clinical research.
In summary, use of a helmet reduced the incidence of tracheal intubation and mortality, and compared with standard oxygen therapy, the helmet had no significant beneficial effect on the oxygenation index and did not increase the PaCO2 and complications. These findings suggest that the use of a helmet in critically ill patients has important clinical value.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Ethics approval and consent to participate
Not applicable.
Funding
This work was supported by the Key Research and Development Program of Anhui province (201904a07020034) and Funding of “Peak” Training Program for Scientific Research of Yijishan Hospital, Wannan Medical College (GF2019G05).
References
- 1.Liston R, Deegan PC, McCreery C, et al. Haemodynamic effects of nasal continuous positive airway pressure in severe congestive heart failure. Eur Respir J 1995; 8: 430–435. [DOI] [PubMed] [Google Scholar]
- 2.Jaber S, Chanques G, Jung B. Postoperative noninvasive ventilation. Anesthesiology 2010; 112: 453–461. [DOI] [PubMed] [Google Scholar]
- 3.Zarbock A, Mueller E, Netzer S, et al. Prophylactic nasal continuous positive airway pressure following cardiac surgery protects from postoperative pulmonary complications: a prospective, randomized, controlled trial in 500 patients. Chest 2009; 135: 1252–1259. [DOI] [PubMed] [Google Scholar]
- 4.Ferrone G, Cipriani F, Spinazzola G, et al. A bench study of 2 ventilator circuits during helmet noninvasive ventilation. Respir Care 2013; 58: 1474–1481. [DOI] [PubMed] [Google Scholar]
- 5.Olivieri C, Costa R, Spinazzola G, et al. Bench comparative evaluation of a new generation and standard helmet for delivering non-invasive ventilation. Intensive Care Med 2013; 39: 734–738. [DOI] [PubMed] [Google Scholar]
- 6.Esquinas RA, Papadakos PJ, Carron M, et al. Clinical review: helmet and non-invasive mechanical ventilation in critically ill patients. Crit Care 2013; 17: 223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cammarota G, Olivieri C, Costa R, et al. Noninvasive ventilation through a helmet in postextubation hypoxemic patients: physiologic comparison between neurally adjusted ventilatory assist and pressure support ventilation. Intensive Care Med 2011; 37: 1943–1950. [DOI] [PubMed] [Google Scholar]
- 8.Antonaglia V, Ferluga M, Molino R, et al. Comparison of noninvasive ventilation by sequential use of mask and helmet versus mask in acute exacerbation of chronic obstructive pulmonary disease: a preliminary study. Respiration 2011; 82: 148–154. [DOI] [PubMed] [Google Scholar]
- 9.Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008; 336: 924–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ozlem CG, Ali A, Fatma U, et al. Comparison of helmet and facial mask during noninvasive ventilation in patients with acute exacerbation of chronic obstructive pulmonary disease: a randomized controlled study. Turk J Med Sci 2015; 45: 600–606. [DOI] [PubMed] [Google Scholar]
- 11.Squadrone V, Coha M, Cerutti E, et al. Continuous positive airway pressure for treatment of postoperative hypoxemia: a randomized controlled trial. JAMA 2005; 293: 589–595. [DOI] [PubMed] [Google Scholar]
- 12.Chidini G, Piastra M, Marchesi T, et al. Continuous positive airway pressure with helmet versus mask in infants with bronchiolitis: an RCT. Pediatrics 2015; 135: e868–e875. [DOI] [PubMed] [Google Scholar]
- 13.Patel BK, Wolfe KS, Pohlman AS, et al. Effect of noninvasive ventilation delivered by helmet vs face mask on the rate of endotracheal intubation in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA 2016; 315: 2435–2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang Y, Sun L, Liu N, et al. Effects of noninvasive positive-pressure ventilation with different interfaces in patients with hypoxemia after surgery for Stanford type a aortic dissection. Med Sci Monit 2015; 21: 2294–2304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cosentini R, Brambilla AM, Aliberti S, et al. Helmet continuous positive airway pressure vs oxygen therapy to improve oxygenation in community-acquired pneumonia: a randomized, controlled trial. Chest 2010; 138: 114–120. [DOI] [PubMed] [Google Scholar]
- 16.Brambilla AM, Aliberti S, Prina E, et al. Helmet CPAP vs. oxygen therapy in severe hypoxemic respiratory failure due to pneumonia. Intensive Care Med 2014; 40: 942–949. [DOI] [PubMed] [Google Scholar]
- 17.Pisani L, Mega C, Vaschetto R, et al. Oronasal mask versus helmet in acute hypercapnic respiratory failure. Eur Respir J 2015; 45: 691–699. [DOI] [PubMed] [Google Scholar]
- 18.Barbagallo M, Ortu A, Spadini E, et al. Prophylactic use of helmet CPAP after pulmonary lobectomy: a prospective randomized controlled study. Respir Care 2012; 57: 1418–1424. [DOI] [PubMed] [Google Scholar]
- 19.Milan M, Zanella A, Isgro S, et al. Performance of different continuous positive airway pressure helmets equipped with safety valves during failure of fresh gas supply. Intensive Care Med 2011; 37: 1031–1035. [DOI] [PubMed] [Google Scholar]
- 20.Kondo Y, Kumasawa J, Kawaguchi A, et al. Effects of non-invasive ventilation in patients with acute respiratory failure excluding post-extubation respiratory failure, cardiogenic pulmonary edema and exacerbation of COPD: a systematic review and meta-analysis. J Anesth 2017; 31: 714–725. [DOI] [PubMed] [Google Scholar]
- 21.Foti G, Sangalli F, Berra L, et al. Is helmet CPAP first line pre-hospital treatment of presumed severe acute pulmonary edema? Intensive Care Med 2009; 35: 656–662. [DOI] [PubMed] [Google Scholar]
- 22.Antonelli M, Pennisi MA, Pelosi P, et al. Noninvasive positive pressure ventilation using a helmet in patients with acute exacerbation of chronic obstructive pulmonary disease: a feasibility study. Anesthesiology 2004; 100: 16–24. [DOI] [PubMed] [Google Scholar]
- 23.Vaschetto R, Longhini F, Persona P, et al. Early extubation followed by immediate noninvasive ventilation vs. standard extubation in hypoxemic patients: a randomized clinical trial. Intensive Care Med 2019; 45: 62–71. [DOI] [PubMed] [Google Scholar]
- 24.Chiumello D, Coppola S, Froio S, et al. Noninvasive ventilation in chest trauma: systematic review and meta-analysis. Intensive Care Med 2013; 39: 1171–1180. [DOI] [PubMed] [Google Scholar]
- 25.Hernandez G, Fernandez R, Lopez-Reina P, et al. Noninvasive ventilation reduces intubation in chest trauma-related hypoxemia: a randomized clinical trial. Chest 2010; 137: 74–80. [DOI] [PubMed] [Google Scholar]
- 26.Ferrer M, Torres A. Noninvasive ventilation for acute respiratory failure. Curr Opin Crit Care 2015; 21: 1–6. [DOI] [PubMed] [Google Scholar]
- 27.Longhini F, Liu L, Pan C, et al. Neurally-adjusted ventilatory assist for noninvasive ventilation via a helmet in subjects with COPD exacerbation: a physiologic study. Respir Care 2019; 64: 582–589. [DOI] [PubMed] [Google Scholar]
- 28.Olivieri C, Longhini F, Cena T, et al. New versus conventional helmet for delivering noninvasive ventilation: a physiologic, crossover randomized study in critically Ill patients. Anesthesiology 2016; 124: 101–108. [DOI] [PubMed] [Google Scholar]