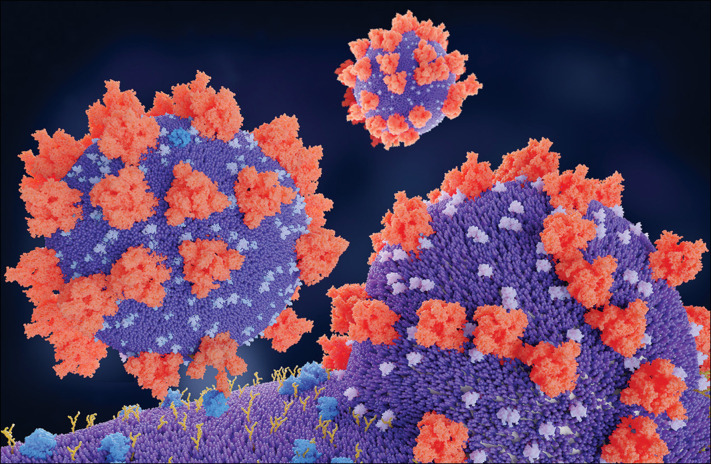
Few could have imagined that hypertension and its treatment with inhibitors of the renin–angiotensin–aldosterone system (RAAS) would become a hot topic during the global COVID-19 pandemic. Two factors have contributed to this: first, the observation that hypertension is one of the most common comorbidities associated with severe cases of COVID-19 in patients who have been admitted to hospital and their risk of death;1 and second, that like the severe acute respiratory syndrome coronavirus (SARS-CoV), SARS-CoV-2 infects cells via specific binding to angiotensin-converting enzyme 2 (ACE2), which is ubiquitously expressed in the lung and other tissues.2 These factors have fuelled speculation that use of RAAS inhibitors, particularly ACE inhibitors or angiotensin-receptor blockers, could lead to increased expression of ACE2 in the respiratory tract, thereby increasing the risk of both becoming infected and developing severe life-threatening complications due to COVID-19. The fact that no evidence supports any aspect of this speculation mattered little as the hypothesis gained traction, initially via social media and subsequently via the medical press.3 Anxiety among patients and physicians has been profound because ACE inhibitors and angiotensin-receptor blockers are the foundation of drug treatment for hypertension, heart disease, and chronic kidney disease, and are among the most widely prescribed drugs globally. Patients have subsequently been withdrawing and substituting these treatments, prompting international cardiovascular and hypertension specialist societies to issue statements of reassurance, while acknowledging the lack of high-quality data to refute the increasing alarm.
This debate, fuelled by speculation, has at last become enriched by data, with the publication of several observational cohort studies.4, 5, 6, 7, 8, 9, 10 In The Lancet, Francisco de Abajo and colleagues4 present data from a case-population pharmacoepidemiological study of 1139 adult patients (cases) who had been admitted to hospital in Madrid, Spain, due to COVID-19 during March, 2020, who were each carefully matched with ten population controls with data from 2018, to give a total of 11 390 matched controls. 444 (39%) cases were female and the mean age was 69·1 years (SD 15·4). The main outcome measure was admission to hospital of patients with PCR-confirmed COVID-19, comparing the current use of RAAS inhibitors with other antihypertensive drugs. The RAAS inhibitors were predominantly ACE inhibitors and angiotensin-receptor blockers, with few individuals currently using aldosterone antagonists or renin inhibitors. Compared with the use of other antihypertensive drugs, current use of RAAS inhibitors was not associated with increased risk of COVID-19 requiring admission to hospital (odds ratio [OR] 0·94, 95% CI 0·77–1·15, adjusted for potential confounding factors), or increased risk of severe complications from COVID-19 needing intensive care or leading to a fatal outcome (1·08, 0·80–1·47). These findings were uninfluenced by age, sex, or background cardiovascular risk. Moreover, excluding aldosterone antagonists and renin inhibitors and focusing only on ACE inhibitors or angiotensin-receptor blockers made no difference to these conclusions.
Potential differences exist between ACE inhibitors and angiotensin-receptor blockers in the context of risk associated with COVID-19. In the study by de Abajo and colleagues, no difference was found between ACE inhibitors and angiotensin-receptor blockers for the main outcome, which was most notable when comparing monotherapy with these drugs (adjusted OR for ACE inhibitor monotherapy was 0·83 [95% CI 0·62–1·12] and for angiotensin-receptor blocker monotherapy was 0·87 [0·60–1·28]).4 This finding is also consistent with most other recent observational studies.5, 6, 7 The exception among these studies was one study8 using observational data from 169 hospitals in Asia, Europe, and North America that reported possible enhanced benefit of ACE inhibitors compared with angiotensin-receptor blockers on mortality, but the authors rightly cautioned against overinterpretation of these data because of potential unmeasured confounding.
© 2020 Juan Gaertner/Science Photo Library
Diabetes is a common comorbidity associated with poorer outcomes in patients with COVID-19 and these patients often have hypertension and are prescribed RAAS inhibitors. Thus, an interesting and potentially clinically important finding in the study by de Abajo and colleagues is that the use of RAAS inhibitors compared with other antihypertensive drugs almost halved the risk of adverse outcomes in patients with COVID-19 who had diabetes (adjusted OR 0·53, 95% CI 0·34–0·80).4 Other studies have also suggested that use of RAAS inhibitors might confer protective effects against complications and death in patients with COVID-19 versus other antihypertensive drugs, although these studies were not restricted to patients with diabetes.9, 10
A notable feature of the emerging data is the excess risk of admission to hospital, admission to intensive care units, and fatal outcomes in patients who are given any kind of antihypertensive drug versus non-users.4 Although this potential association of antihypertensive treatment and increased risk of severe COVID-19 has caused alarm, generally people are accepting that it most likely reflects the use of these drugs for patients who are older and who invariably have multiple comorbidities, and despite rigorous attempts to adjust for comorbidities in observational studies, fully adjusting for confounding by indication is not possible.
The limitations of the study by de Abajo and colleagues4 apply to all of the observational studies we have discussed here, which are not randomised controlled trials, and despite multiple statistical adjustments are invariably subject to confounding, either unmeasured or unknown. Controlling for whether patients were compliant with their RAAS inhibitor treatment, either before or after becoming infected with SARS-CoV-2, is also not possible. Nevertheless, the aforementioned studies,4, 5, 6, 7, 8, 9, 10 each with its own important nuances, all reached similar overarching conclusions from which a reasonable interpretation is that no evidence exists to support the speculation that RAAS inhibitors increase the risk of COVID-19. Nor does evidence exist to suggest that, once infected, the risk of admission to hospital due to COVID-19, progression to more severe complications, or death is increased with RAAS inhibitor use compared with treatment with other antihypertensive drugs. Findings from some studies even suggest that treatment with RAAS inhibitors might reduce risk of severe complications or death due to COVID-19,9, 10 but this potentially important finding needs confirmation in randomised controlled trials.
For the moment, we should applaud the remarkable achievement of investigators globally, in the face of considerable adversity, for rapidly generating scientific data that should diminish the speculation about the safety of RAAS inhibitors during this global COVID-19 pandemic and provide a degree of reassurance to patients and their doctors.
For the European Society of Cardiology Council's statement see https://www.escardio.org/Councils/Council-on-Hypertension-(CHT)/News/position-statement-of-the-esc-council-on-hypertension-on-ace-inhibitors-and-ang
For the European Society of Hypertension's statement see https://www.eshonline.org/spotlights/esh-statement-on-covid-19/
For the International Society of Hypertension's statement see https://ish-world.com/news/a/A-statement-from-the-International-Society-of-Hypertension-on-COVID-19/
Acknowledgments
BW reports honoraria from Daiichi Sankyo, Servier, Pfizer, Boehringer Ingelheim, and Menarini for lectures on hypertension outside the area of work commented on here. ZY declares no competing interests.
References
- 1.Huang C, Wang Y, Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen Y, Guo Y, Pan Y, Zhao ZJ. Structure analysis of the receptor binding of 2019-nCoV. Biochem Biophys Res Commun. 2020 doi: 10.1016/j.bbrc.2020.02.071. published online Feb 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020;8:e21. doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Abajo FJ, Rodríguez-Martín S, Lerma V. Use of renin-angiotensin-aldosterone system inhibitors and risk of COVID-19 requiring admission to hospital: a case-population study. Lancet. 2020 doi: 10.1016/S0140-6736(20)31030-8. published online May 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li J, Wang X, Chen J, Zhang H, Deng A. Association of renin-angiotensin system inhibitors with severity or risk of death in patients with hypertension hospitalized for coronavirus disease 2019 (COVID-19) infection in Wuhan, China. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1624. published online April 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mancia G, Rea F, Ludergnani M, Apolone G, Corrao G. Renin-angiotensin-aldosterone system blockers and the risk of Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMoa2006923. published online May 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reynolds HR, Adhikari S, Pulgarin C. Renin-angiotensin-aldosterone system inhibitors and risk of Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMoa2008975. published online May 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mehra MR, Desai SS, Kuy S, Henry TD, Patel AN. Cardiovascular disease, drug therapy, and mortality in Covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMoa2007621. published online May 1. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 9.Zhang P, Zhu L, Cai J. Association of inpatient use of angiotensin converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res. 2020 doi: 10.1161/CIRCRESAHA.120.317134. published online April 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bean DM, Kraljevic Z, Searle T. Treatment with ACE-inhibitors is associated with less severe disease with SARS-Covid-19 infection in a multi-site UK acute hospital trust. medRxiv. 2020 doi: 10.1101/2020.04.07.20056788. published online April 11. (preprint). [DOI] [PMC free article] [PubMed] [Google Scholar]