Abstract
Polluted air poses a significant threat to human health. Exposure to particulate matter (PM) and harmful gases contributes to cardiovascular and respiratory diseases, including allergies and obstructive lung disease. Air pollution may also be linked to cancer and reduced life expectancy. Uptake of PM has been shown to cause pathological changes in the intestinal microbiota in mice and humans. Less is known about the effects of pollution-associated microbiota on human health. Several recent studies described the microbiomes of urban and rural air samples, of the stratosphere and sand particles, which can be transported over long distances, as well as the air of indoor environments. Here, we summarize the current knowledge on airborne bacterial, viral, and fungal communities and discuss their potential consequences on human health. The current data suggest that bacterial pathogens are typically too sparse and short-lived in air to pose a significant risk for infecting healthy people. However, airborne fungal spores may exacerbate allergies and asthma. Little information is available on viruses including phages, and future studies are likely to detect known and novel viruses with a yet unknown impact on human health. Furthermore, varying experimental protocols have been employed in the recent microbiome and virome studies. Therefore, standardized methodologies will be required to allow for better comparisons between studies. Air pollution has been linked to more severe outcomes of SARS (severe acute respiratory syndrome) coronavirus (SARS-CoV) infections. This may have contributed to severe SARS-CoV-2 outbreaks, especially those in China, Northern Italy, Iran, and New York City.
1. Introduction
1.1. Definition, Guidelines, and Sources of Air Pollution
Air quality is commonly described by the concentrations of PM (ranging in diameter from 10 μm or smaller (PM10) to below 0.1 μm (PM0.1)) and of the gaseous pollutants, ozone (O3), nitrogen dioxide (NO2), and sulfur dioxide (SO2) [1–5]. Current recommendations for PM2.5 and PM10 by the World Health Organization (WHO) are 10 and 20 μg/m3 on average per year, respectively, while upper limits for NO2, O3, and SO2 are 40, 100 (at ground levels), and 20 μg/m3, respectively (Table 1). Other agencies including the European Union (EU), the Chinese Ministry of Environmental Protection, and the United States Environmental Protection Agency (EPA) also publish guidelines (Table 1). Alarmingly, approximately 92% of the world's population lives in regions where WHO guidelines are not met [6].
Table 1.
Recommendations and thresholds.
| WHO recommendations | EU thresholds | Chinese Ministry of Environmental Protection∗ | United States EPA | |
|---|---|---|---|---|
| PM2.5 | 10 μg/m3 annual average | 25 μg/m3 annual average | 35 μg/m3 annual average | 35 μg/m3 averaged over 24 hours |
| 25 μg/m3 24-hour maximum | 75 μg/m3 daily average | |||
|
| ||||
| PM10 | 20 μg/m3 annual average | 40 μg/m3 annual average | 70 μg/m3 annual average | 150 μg/m3 averaged over 24 hours |
| 50 μg/m3 daily average | 50 μg/m3 daily average | 150 μg/m3 daily average | ||
|
| ||||
| NO2 | 40 μg/m3 annual average | 40 μg/m3 annual average | 40 μg/m3 annual average | 53 parts per billion (ppb) annual mean |
| 200 μg/m3 1-hour maximum | 200 μg/m3 1-hour maximum | 80 μg/m3 daily average 200 μg/m3 1-hour average |
||
|
| ||||
| O3 | 100 μg/m3 8-hour maximum | 120 μg/m3 8-hour average | 160 μg/m3 8-hour average 200 μg/m3 1-hour average |
0.070 parts per million (ppm) averaged over 8 hours |
|
| ||||
| SO2 | 20 μg/m3 daily average | 125 μg/m3 daily average | 60 μg/m3 annual average 150 μg/m3 daily average |
0.5 ppm averaged over 3 hours |
| 500 μg/m3 10-minute maximum | 350 μg/m3 1-hour maximum | 500 μg/m3 1-hour average | ||
Numbers in parentheses are the maximal numbers of allowed exceedances per year. ∗Values applying for urban areas are shown. Stricter standards are required for special regions such as national parks. Numbers are according to the WHO [1], the EU [2], the Chinese Ministry of Environmental Protection [5], and the United States Environmental Protection Agency (EPA, values retrieved from https://www.epa.gov/criteria-air-pollutants/naaqs-table).
Major emitters of air pollution are fossil fuel power plants, industry, agriculture, mobile sources (cars and other vehicles), wildfires, and natural processes occurring in various ecosystems [7–9]. In the US, mobile sources are the major emitters of nitrogen oxides (NOX), while stationary sources contribute mainly to emissions of SO2, PM2.5, and PM10 (Figure 1(a)) [7]. PM10 consists of particles produced by diesel fuel combustion, burning of wood, or biomass. PM2.5 emissions can result directly from exhaust of cars or other combustion processes and comprise soot particles. In addition, gases such as NOX, sulfur oxides (SOX), or ammonia (NH3) can form PM2.5, termed secondary fine dust, in a gas-to-particle conversion process [8]. Agriculture is the leading source of PM2.5 secondary fine dust in many parts of the world including Europe, which partially originates from NH3 of fertilizers (Figure 1(b)) [9].
Figure 1.
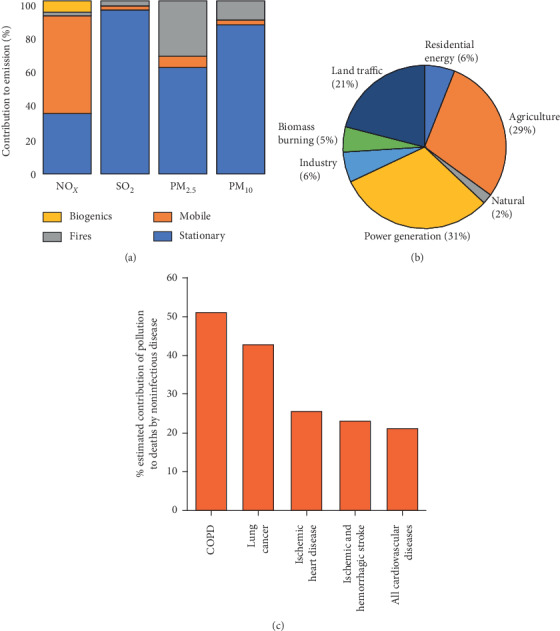
Origins of air pollution and contribution to deaths. (a) Relative contribution of different sources to the emission of NOX, SO2, PM2.5, and PM10 in the US for the year 2014 [7]. (b) Relative contribution of outdoor air pollution sources to premature death in the US for the year 2010 [9]. (c) Estimated contributions of global air pollution risk factors to deaths caused by noncommunicable disease for the years 1990–2015 [10].
2. Pollution-Related Diseases
The major health problems described for exposure to air pollution are likely caused by PM and mainly affect the airways and the cardiovascular system [10–16]. Both PM10 and PM2.5 can cause eye irritations, allergies, and rhinitis [10–12]. Globally, air pollution contributes to most deaths by chronic obstructive pulmonary disease (COPD) and to large proportions of fatalities caused by lung cancer, ischaemic heart disease, stroke, and cardiovascular diseases (Figure 1(c)). PM can also carry heavy metals that are associated with cancer and other diseases [17, 18]. The “Beijing Cough” is caused by polluting particles from inhaled smog [19]. A recent study described a correlation between PM10 and hospital admissions for respiratory diseases [20].
PM2.5 can reach deeper into the lung tissue than larger particles [21]. Long-time exposure has been correlated with increased risks of chronic diseases, including COPD that can develop into lung cancer (Table 2) [10–12, 19]. Cardiovascular diseases linked to PM2.5 include ischaemic heart disease and stroke [22].
Table 2.
| Particle size | Short-term exposure | Long-term exposure |
|---|---|---|
| PM10 | Allergies, asthma, bronchitis, COPD, coughing, eye irritations, hay fever, increased respiratory infections, and rhinitis | COPD |
| PM2.5 | Asthma, cardiovascular disease, COPD, coronary heart disease, heart insufficiencies, hypertonia, and increased respiratory infections | Allergies, asthma, atherosclerosis, COPD, increased risk for cancer, and shortened life expectancy |
| PM0.1 | Asthma and coronary heart disease | Unknown |
Emerging evidence suggests causal associations between PM2.5 and type 2 diabetes, decreased cognitive functions, attention-deficit/hyperactivity disorder, autism, and neurodegenerative diseases [10]. PM2.5 may also be linked to premature birth, low birth weight, and sudden infant death syndrome [23]. However, these potential effects of air pollution remain to be better established and quantified.
Ultrafine nanoparticles (PM1 and PM0.1) can penetrate the skin, blood vessels, and the lymphatic system and are thereby distributed throughout the body; they can also act intracellularly [24]. Short-term exposure has been implicated in exacerbation of the abovementioned diseases, but long-term consequences are largely unknown [25]. However, nanoparticles have been found to induce oxidative stress, which is associated with neurodegenerative disorders, cancer, chronic fatigue syndrome, and cardiovascular and gastrointestinal diseases [26, 27]. Moreover, exposure to ultrafine nanoparticles has been linked to cardiovascular diseases in a recent cohort study [25].
Worldwide, about 3.3 million people die prematurely from outdoor air pollution each year [9], and additional about 3.8 million due to household pollution, mostly in developing countries where cooking with open fires is common practice [28]. Of these people, 27% die from pneumonia, 20% from COPD, 8% from lung cancer, and 45% due to cardiovascular diseases [10]. In Western countries, life expectancy is estimated to be reduced by an average of 8.3 months due to exposure to PM2.5 [29].
Globally, the effect of air pollution on life expectancy is estimated to be more than twice as strong as the effects of water, soil, and occupational pollution combined [10]. The estimated 9 million premature deaths annually due to indoor and outdoor air pollution exceed those estimated for smoking (about 7 million) and major infectious diseases (AIDS, tuberculosis, and malaria combined account for about 3 million premature deaths) [10].
2.1. Air Microbiome in Large Cities
Recently, the journal BMC Infectious Diseases published a special issue on the airborne microbiome, emphasizing on the spread of pathogens via human breath [30]. Here, we focus on pathogens potentially transported on the surface of airborne PM. The yet-unanswered question is whether and to what extent microbes carried by these particles contribute to diseases.
The airborne microbiota of several cities have been characterized—Beijing [31] and Urumqi [32] in China, Seoul in South Korea [33], and Milan in Italy [34]. Additional studies investigated the subway systems of New York City, USA [35], Oslo, Norway [36], and Hong Kong [37]. In these studies, air filters were used to collect PM; microbial nucleic acids were isolated, processed, and sequenced. However, experimental conditions varied which limits direct comparison of the results. In Beijing, PM2.5 and PM10 levels of a severe smog event were analyzed over seven days and the extracted DNA was sequenced on an Illumina HiSeq 2000 sequencing system to determine microbial compositions [31]. Sequencing library preparation included a PCR step since amounts of DNA extracted from the air samples were too small for direct sequencing, and generated reads were aligned to nonredundant NCBI complete genomes for taxonomic assignment [31]. The detected microbes included bacteria (86.1% and 80.8% of reads in PM2.5 and PM10, respectively), eukaryotes (13% and 18.3%), 0.8% archaea, and 0.1% viruses in both samples (Figure 2(a)). The most abundant bacteria belonged to the Proteobacteria phylum, followed by Actinobacteria, Firmicutes, Bacteroidetes, and Cyanobacteria. Most inhalable microorganisms were soil-associated and nonpathogenic. However, microbes known to cause allergies and respiratory diseases were detected, including the bacterium Streptococcus pneumoniae, the fungus Aspergillus fumigatus that can cause asthma and respiratory aspergillosis [40], and human adenovirus C that causes respiratory, gastrointestinal, and urinary tract infections [41]. RNA viruses such as influenza, coronaviruses, or rhinoviruses were undetectable by the employed method. The authors concluded that there was likely no risk for contracting infectious diseases from pollutant-associated microbes, but they recommended fixing soil by vegetation to reduce the amount of airborne microbes originating from fecal and terrestrial sources, including potential allergens [31]. In this context, it is noteworthy that in 2018, China announced to promote revegetation and to increase forestation levels from about 22% in 2016 to 30% by 2050 to tackle air pollution [42].
Figure 2.
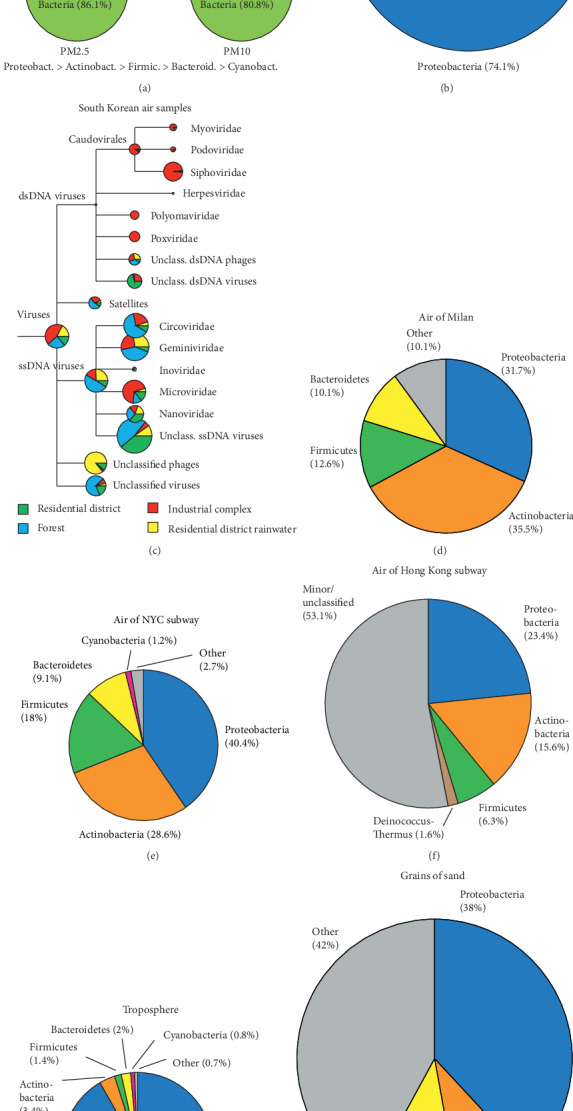
Compositions of air microbial communities in different locations. (a) Composition of the air microbes during a smog event in Beijing [31]. (b) Composition of the air bacterial communities during winter in the city of Urumqi [32]. (c) Virome of the air samples around Seoul, South Korea [33]. (d) Bacterial communities of air samples of the city of Milan during spring [34]. Bacterial communities of air samples obtained in the subway systems of New York City [35] (e) and Hong Kong [37] (f). Bacterial communities observed for the troposphere [38] (g) and on sand grains [39] (h).
Like in the air of Beijing, Proteobacteria and Actinobacteria were abundantly detected in the air of the city of Urumqi in northwest China (Figure 2(b)) [32]. This study also used DNA from filtered PM as the starting material, but taxonomic assignment was based on PCR-amplified 16S rRNA genes (prokaryotes) and 18S rRNA genes (eukaryotes) [32]. Several bacteria that may cause diseases in immunocompromised individuals but are typically harmless to the healthy population, such as Acinetobacter, Delftia, Serratia, and Chryseobacterium were detected. Some of the detected fungal spores are associated with allergies [43], such as Ascomycota, Basidiomycota, and Zygomycosis. Beijing is known for the “Beijing” cough, which affects many inhabitants independent of their age [19]. This condition may pose an increased risk for other lung diseases such as infection by SARS-CoV-2. Indeed, exposure to smog has been linked to an increased incidence of respiratory infections [44] and air pollution (such as PM and NO2) correlates with increased severity of diseases caused by infections with coronaviruses such as SARS-CoV-1 and SARS-CoV-2 [45–49]. SARS-CoV-2 may also be spread more efficiently in polluted air by attaching to PM [50].
A virome study from Seoul identified DNA viruses at different locations, industrial, residential, and a forest (Figure 2(c)) [33]. After removal of particles larger than 0.2 μm by filtration, samples were concentrated by tangential flow filtration and virus particles were purified by CsCl density centrifugation. DNA was extracted and, without PCR amplification, subjected to 454 pyrosequencing. Reads were assigned to viral sequences using the CAMERA databases and were taxonomically assigned with Megan [33]. The study was not designed to detect any RNA viruses. The authors identified predominantly plant-infecting single-stranded DNA (ssDNA) viruses of the Gemini-, Nano- and Circoviridae families. Nanoviridae are aphid-transmitted plant viruses with circular ssDNA segments [51]. Circoviridae also have circular genomes and infect plants, birds, pigs, fish, and insects [52]. Geminiviridae consist of two capsids, each containing a circular ssDNA of opposite polarities [53]; some members can significantly damage crops [54]. In addition, Microviridae, ssDNA phages infecting Enterobacteria, were identified. The authors also detected Caudovirales, tailed phages with double-stranded DNA genomes. Microviridae and Caudovirales comprise the most abundant phage populations in the human intestinal tract [55] and have also been identified in marine environments [56, 57]. No human pathogenic viruses were detected. However, previously unknown ssDNA viruses were identified. Further studies will be necessary to address potential risks of the airborne virome on human health and on crop productivity.
A study in Milan, Northern Italy, evaluated forty air samples from ten days of sample collection during different seasons for bacterial and fungal communities (Figure 2(d)) [34]. The study relied on extracted bacterial DNA and PCR-amplified 16S rRNA genes that were sequenced on an Illumina Genome Analyzer IIx; taxonomic assignment was carried out with the RDP Bayesian Classifier [34]. Around 104, mainly soil and plant-associated, bacteria per cubic meter of air were detected, with Actinobacteria and Proteobacteria dominating [34]. Significant seasonal and temperature-dependent variations were observed, for instance, with more Actinobacteria on colder days. The authors did not address whether potentially pathogenic or allergy-inducing species were detected.
The air of the New York City subway system was found to contain microorganisms mainly originating from outdoor air with a minor proportion from human skin [35]. Here, DNA extracted from filtered air samples was subjected to PCR to amplify 16S and 18S rRNA genes, the amplicons were subsequently sequenced by 454 pyrosequencing, and taxonomic assignment was achieved using the SILVA database [35]. On average, samples contained 40.4% Proteobacteria, 28.6% Actinobacteria, 18% Firmicutes, 9.1% Bacteroidetes, 1.2% Cyanobacteria, and a complex mixture of fungal spores (Figure 2(e)). Surprisingly, no known human pathogens were detected, but some of the detected fungi may cause allergies. The severity of the outbreak of SARS-CoV-2 in New York City may have been partly due to the high population density, high mobility, pollution, and also preexisting conditions such as obesity, which affects about 40% of the US population and may be a factor contributing to more severe outcomes of COVID-19 [48, 58].
In Oslo, aerosols were found to contain bacterial populations comparable to those of New York, with 37 different genera in total, some of them of skin origin [36]. Concentrations were about 10-fold lower at night [36]. Similarly, the air of the Hong Kong subway system predominantly contained Proteobacteria and Actinobacteria (Figure 2(f)) [37]. This study relied on extracted DNA subjected to PCR amplification of 16S rRNA genes and Illumina MiSeq sequencing. Taxonomic assignment was achieved by aligning reads against the Greengenes rRNA gene sequence database using the UCLUST program [37]. As observed in the New York City subway, bacterial communities showed significant similarities with those of outdoor air samples, with some human skin-associated bacteria also being present. Again, known pathogenic bacteria were not detected in this study.
2.2. Rural Air Microbiome
Besides soil bacteria, the Beijing study identified fecal bacteria as a prominent component of air pollution, possibly originating from rural animal farms. In addition, human fecal bacteria from sewage are a possible origin [31]. A study of the air microbiome of the grain-growing region Vaud, Switzerland, found a strong correlation between aerosolized and grain dust-associated fungal communities [59]. The presence of allergenic and mycotoxigenic species in most samples suggests that these fungal species may contribute to work-related respiratory symptoms of grain workers who, however, are exposed to much higher concentrations than the general population [59]. A study comparing rural and urban areas of the US found that urbanization leads to homogenization of the airborne microbiota, with urban communities exhibiting less geographic variability than rural areas [60]. The rural air microbiome was found to contain large numbers of fungi that are known triggers of allergies, including Alternaria and Cladosporium [60]. Further studies are needed to assess to what extent diseases may result from exposure to the rural air microbiome and how they correlate with concentrations and exposure times.
2.3. Microbiomes of the Troposphere, Dust, and Sand
There is evidence that microbes can be transported across very long distances and to high altitudes [60]. Bacteria represented on average 20% of particles between 0.25 and 1 μm in diameter in either cloud-free or cloudy air obtained during the hurricanes Earl and Karl at 8–15 km altitude in the troposphere [38]. Numerous bacterial taxa were identified, including Acetobacteraceae, Burkholderiaceae, Streptomyces, and Pseudomonadaceae. Proteobacteria was the dominant phylum (Figure 2(g)). There were significant differences in microbial communities between samples from the two hurricanes. However, 17 bacterial and fungal species were common across all samples and may represent core members of the stratospheric microbiota [38]. Due to the poor resolution of the sequencing approach, the authors were unable to determine if any human pathogenic bacteria were present [38]. The vertical distribution of bacterial communities in the atmosphere above the Noto Peninsula, Japan, between 10- and 3,000-meter altitudes, has also been shown to vary substantially and mainly contained soil and marine bacteria [61]. The authors detected Bacilli and Proteobacteria, taxa that include known plant, animal, and human pathogens, which they speculated may be dispersed over large distances through high altitudes [61]. Whether these airborne pathogens can cause an infection after exposure to high altitude remains to be shown.
Sand grains can be transported over thousands of kilometers and transport bacteria, such that their populations may even be globally connected [62]. Sand grains of 200–600 μm in diameter from a German shore were shown to bind 104 to 105 bacteria composed of 3,000 to 6,000 different species, mostly of soil and marine origin [39]. A core bacterial community was determined, with 50% of the bacteria present on all sand grains, and the other half varied. Proteobacteria was the dominant phylum, followed by Bacteroidetes and Actinobacteria (Figure 2(h)). The identified bacteria were not discussed as potentially harmful for people.
Dust from desert soil was shown to transport diverse assemblages of bacteria to the Mediterranean [63]. The dust microbiome of the Gobi Desert was found to contain large amounts of Alphaproteobacteria [64]. Soil bacteria were more abundant during dust storm events, while the relative abundance of bacteria of anthropogenic origin decreased [65]. Anthropogenic bacteria included those carrying antibiotic resistance genes, suggesting that the air microbiome may contribute to the spread of antibiotic resistance over long distances, whereby these genes may get diluted. No human health risks have been described [65]. A concern, however, is the presence of antibiotic resistance genes in the sewage of livestock production that can be transported by water or through air [66].
2.4. Indoor Air Microbiome
Indoor pollution has been analyzed systematically using household air [67–69]. Here, Western households must be distinguished from those in developing countries where open fires used for cooking contribute to pollution, a major health concern and cause of premature mortality [70]. In Western households, major sources of microorganisms are humans, pets, plants, plumbing, heating, ventilation/air conditioning, mold, and dust from outdoors [68]. People typically stay most of the day indoors, and the air microbiomes differ significantly between environments such as schools, offices, households, and transportation and even between different rooms of the same household [67–69]. One cubic meter of indoor air typically contains 105 of both virus-like and bacteria-like particles, about a tenth of the concentrations found in outdoor air [68]. Fungal spores are less abundant and vary in numbers from around 80 up to 104 colony-forming units. Humans emit around 107 copies of bacterial and fungal genomes per hour [68]. Human stool can contain up to 109 particles per gram of fecal-transmitted pathogens such as norovirus, Shigella, or Salmonella [71]. It should be noted that humans carry 1012 microorganisms on their skin and 4 × 1013 in their digestive tract [72] and are the dominant sources of bioaerosols in indoor environments [73–75]. Key factors that determine the composition of the indoor fungal and bacterial microbiome appear to be moisture, age of the home, and dog ownership [76]. Potential effects on health may come from fungi as a significant source of allergens and mycotoxins [77], whereby indoor fungal communities are dominated by species originating from outdoors [78]. Fungal and bacterial spores can infect animals, plants, and humans [79], are highly stable, and can survive dormant for years. Fungi such as Cryptococcus spp. can cause fatal disease in immunocompromised populations, such as AIDS patients and transplant recipients [80]. However, most microorganisms are benign and protect against harmful microbes, assist in the digestion, train the immune system, and lower the risk of autoimmune diseases [81]. High doses of pathogens are, however, a risk under poor sanitary conditions and exposure to droplets and aerosols from infected people with high titers of pathogens.
2.5. Healthcare Facilities and Transportation
Not surprisingly, the indoor air microbiota of hospitals contain a larger percentage of potential bacterial pathogens than do outdoor samples [82]. Indeed, many healthcare facilities are affected by the spread of SARS-CoV-2 and the resulting infection of healthcare workers and other patients. Microbiome studies of hospitals may help to reduce exposure to pathogens; for example, rooms with higher airflow and humidity were associated with fewer airborne human pathogens [82]. Thus, architectural design may help to reduce transmission of pathogens in healthcare facilities. Ventilation systems of trains and airplanes typically recycle cabin air which is passed through filters that do not efficiently remove viruses. During the SARS-CoV-2 pandemic, this has resulted in almost complete shutdown of long-distance traffic and public transport in many countries. Spread of the virus may only be prevented if all passengers are confirmed negative for SARS-CoV-2 infections via antibody testing or real-time viral tests indicating a virus-free status. Such tests are available for influenza virus; they provide rapid results but are often less reliable than laboratory tests. Yet, that may be the only fast solution for long-distance travel in trains or airplanes. Keeping a safety distance and masks can only help to contain the spread of SARS-CoV-2 to a certain extent.
2.6. Airborne Viruses and Phages
Much less is known about airborne viruses than about bacterial and fungal communities. The International Committee on Taxonomy of Viruses (ICTV) lists approximately 6,000 known viruses, of which about 1,500 can cause diseases [83]. Patients acutely infected with influenza virus can harbor up to 109 virus particles per cubic centimeter in the blood stream and release approximately 10,000 aerosolized viruses by coughing or sneezing [75]. Indoors, influenza virus can reach concentrations of up to 2.6 × 105 particles per cubic meter [68]. Even more infectious by airborne transmission is measles virus, which leads to almost 100% infections upon contact with an infected person [84]. Measles virus causes severe disease during childhood and can also be dangerous for adults, especially for pregnant women [84].
Noroviruses are relatively stable and can persist in the environment for several weeks [84]. As few as 18 to 1,000 norovirus particles can cause an infection [85]. Noroviruses account for about 50% of infectious diarrhea in humans. There are at least 33 genotypes and acquired immunity is short-lived and not cross-protective, so that a person may encounter several norovirus infections per year. Norovirus is usually not seriously harmful to healthy adults, but to young children and the elderly [84]. Closed environments such as cruise ships are commonly affected by norovirus outbreaks.
3. Coronaviruses
Coronaviruses are single-stranded positive-sense RNA viruses, with seven known to infect humans, including SARS-CoV-1, MERS-CoV, and SARS-CoV-2 [86]. The four others contribute to about 10–15% of the seasonal acute respiratory infections [87]. Other seasonal viral infections are caused by influenza A and B viruses, respiratory syncytial virus, and rhinoviruses. Respiratory viruses such as influenza or coronaviruses, including SARS-CoV-2, are transmitted by respiratory droplets (larger drops emitted by coughing, sneezing, or talking) and aerosols (particles smaller than 1 micron in diameter) when they reach susceptible mucosal surfaces of the eyes, nose, or mouth. Indirect contact through smear infections from contaminated surfaces may occur but the amount of viable viruses may be small. The transmission of respiratory viruses can be limited by wearing face masks, which reduce the spread of droplets and aerosols between people. Outdoors, the viruses are normally too sparse to pose a significant risk for infecting healthy people if a safety distance from other people is maintained. Even though droplets may travel a distance of about 30 cm before they sink, a safety distance for up to 2 meters has been proposed to contain the spread of SARS-CoV-2. Face masks covering the nose and mouth can reduce droplet-based viral infections, while only surgical masks may protect against viral aerosols.
Air pollution as reviewed here can cause lung damage. This is a prominent problem mainly in large cities and manifests itself as “Beijing cough,” a dry cough highly prevalent in large and polluted cities [19]. There is evidence that people exposed to severe air pollution are more susceptible to infection with the present SARS-CoV-2 pandemic virus and experience stronger symptoms, not only in large cities of China but also in other parts of the world [46–51]. Pollution, including PM and NO2, likely contributed to the spread of SARS-CoV-2 and severity of disease in Northern Italy where pollution is severe [46, 47, 49, 50]. In addition to air pollution, preexisting conditions such as overweight may contribute to disease severity, which may especially be relevant for the US, where close to 40% are clinically obese [58].
SARS coronaviruses have a history as pollutant through plumbing [88]. For example, SARS-CoV-1 spread through the plumbing of the Amoy Gardens Building in Hong Kong, which was not aerosol-tight and thereby allowed the virus to spread from the 7th floor of the 33-story building with contaminated sewage [88]. Also, in the Hotel Metropole in Hong Kong, twelve people were infected within 24 hours, causing a chain of infection of up to 4,000 people [89]. SARS coronaviruses are extremely contagious [90]. Strict regimens for infected people in Singapore successfully contained the SARS-CoV-1 outbreak. However, the virus even escaped twice from researchers working under high safety laboratory conditions [91].
Phages, the viruses of bacteria, are abundant on our planet, in the oceans, air, soil, and other environments [92]. They can integrate into bacterial genomes but can also replicate by lysing the bacteria. About 10–20% of bacteria in the oceans are lysed daily by phages [93]. It is not trivial to characterize phages in an environmental sample; they typically require purification, concentration, and PCR amplification steps prior to sequencing and taxonomic assignment [94, 95]. The identification of phages in human samples has recently been discussed in detail [95]. Phages were identified in the air of Seoul and may therefore spread through the air [32]. Yet, they are not known to pose a risk for human health.
3.1. Effects of Inhaled and Ingested Pollution
An important question is whether air pollution influences the composition of the host microbiota. The gastrointestinal tract harbors the highest number of microbes and may be indirectly affected by high concentrations of pollutant PM [96]. In humans, inhaled PM is rapidly cleared from the lungs and transported into the intestine where it may cause alterations in bacterial community compositions [97]. In a mouse model of inflammatory bowel disease (IBD), orally administered environmental PM10 at a concentration representing a dose that could occur during periods of high levels of air pollution has been shown to significantly affect the gut microbiota [98]. The proportion of Firmicutes was increased, while Bacteroidetes decreased and inflammatory responses and gut permeability were promoted (Figure 3) [98]. Epidemiological evidence suggests that air pollutants are also linked to an increased risk for IBD in humans [99]. It has been suggested that air pollution, in general, and PM, specifically, may promote gastrointestinal diseases in humans [86]. Recently, it has been shown that PM inhalation may alter the intestinal microbiota in humans [100]. As observed experimentally in mice, an increase in Bacteroidetes and a decrease in Firmicutes were observed, with health consequences yet to be determined.
Figure 3.
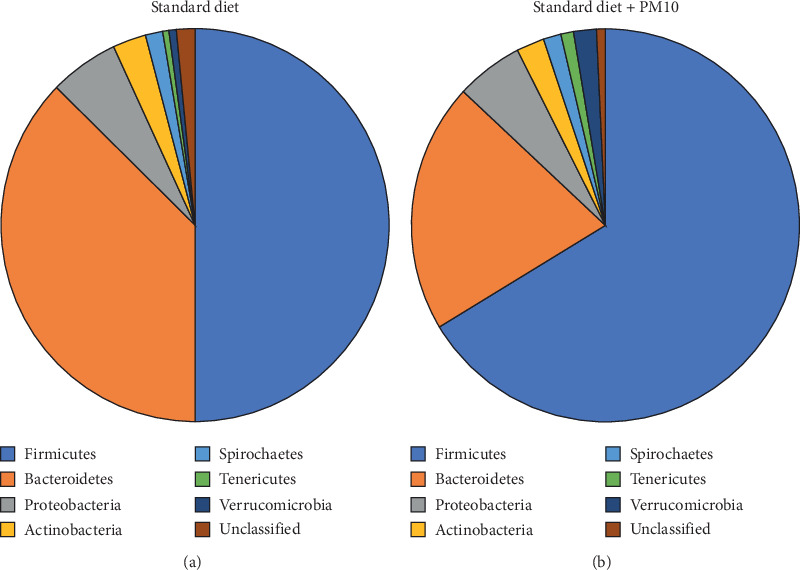
Changes in intestinal microbiota due to PM10 in a mouse model. IL-10 knockout mice, a model for inflammatory bowel disease, were fed with either standard mouse chow (left) or standard mouse chow supplemented with PM10 for 35 days [99]. Then, the bacterial composition in fecal samples of these mice was determined.
In addition to IBD, exposure to air pollution has been linked to type 2 diabetes and obesity, possibly due to effects on the intestinal microbiota [101, 102]. Specific families of gut bacteria correlated with NOX exposure; Bacteroidaceae (phylum Bacteroidetes) increased, while Coriobacteriaceae (phylum Actinobacteria) decreased [101]. These changes were associated with increased fasting glucose levels characteristic of developing type 2 diabetes. In addition, polycyclic aromatic hydrocarbons and other organic pollutants present in PM can be metabolized by gastrointestinal bacteria and thereby alter the composition of the microbiota [103].
Alterations in the lung microbiome have been linked to various diseases such as cystic fibrosis, COPD, and asthma [104]. For example, patients with asthma and COPD have increased relative abundances of Proteobacteria compared to healthy individuals. Interestingly, it has been shown that individuals exposed to higher levels of PM from household air pollution in Malawi showed alterations of their lung microbiome, including higher relative abundances of potentially pathogenic bacteria of the genera Streptococcus and Neisseria [105]. Moreover, domestic biomass fuel use was associated with the presence of an environmental bacterium, Petrobacter, which is normally not present in the lung [105].
In summary, there is evidence that environmental pollution can affect the composition of both the gastrointestinal and the lung microbiota, with potential negative effects on human health. Thus, air pollutants, without directly transporting microbes, can indirectly affect the body's inherent microbiota.
4. Discussion
We are only beginning to understand the composition of aerial microbiomes and their potential impact on human health. However, from the current data, the following trends emerge for bacterial, viral, and fungal communities, despite the varying methodologies employed by the different studies.
4.1. Airborne Bacteria
The bacterial communities of urban air microbiomes appear to be mainly composed of the phyla Proteobacteria, Actinobacteria, and Firmicutes (Figure 3), while less abundant populations such as Bacteroidetes and Cyanobacteria are more variable among samples [31, 32, 34–37]. This is reminiscent of bacterial and viral microbiota of the oceans and the human intestinal tract that are composed of abundant core members and less-abundant variable populations [55, 106]. Potential human pathogens are typically below the detection limit in air samples even from closed environments such as subway systems, which means that there is not likely a significant risk for infection [31, 32, 34–37].
4.2. Airborne Viruses
Likewise, ambient air appears to not contain significant amounts of known viral pathogens [33]. However, only a small fraction of all viruses found in the environment are known, which makes it difficult to estimate potential effects of the air virome on human health [33]. A major constituent of the airborne virome is bacteriophages that are not known to pose a risk for humans but may affect bacterial populations contributing to the spread virulence and antibiotic resistance genes [33].
4.3. Coronaviruses
SARS-CoV-2 is the cause of the current COVID-19 pandemic of 2019/2020, which has led to outbreaks of varying severities. High infection and death rates were observed, for example, in Wuhan city and other parts of China, Lombardy in Northern Italy, Northern Iran, New York City, USA, Manaus, Brazil, and Johannesburg, South Africa. In some cases, the severity of the outbreaks may have been linked to air pollution in conjunction with a high population density. Other risk factors may comprise overweight/obesity, chronic cough, lung diseases such as COPD, and infectious diseases such as tuberculosis and HIV/AIDS [44–50, 58, 107, 108]. SARS-CoV-2 most efficiently spreads through contact with infected people in indoor environments [109]. This has prompted restrictions of public transport and long-distance travel in many countries worldwide. Outdoors, virus-containing droplets or aerosols typically do not travel through air beyond the proposed safety distance of one to two meters in amounts sufficient to cause an infection.
4.4. Airborne Fungi
A major risk for human health is airborne fungi that can exacerbate diseases including allergies and asthma [31, 32, 35]. Studies on fungal air microbiomes may help to identify measures to reduce the abundance of fungal species linked to allergies, asthma, and other diseases in outdoor and indoor ambient air. For indoor environments, it has been shown that the abundance of specific components of the airborne microbiota can be altered by architectural design, humidity, and the degree of air flow [82]. Thus, hypoallergenic architectural design can be envisioned. There is evidence that fungal spores are particularly abundant in rural air [59]. Interestingly, exposure to indoor dust-borne Alternaria spp. was found to be linked to a reduced occurrence of asthma, whereas indoor airborne Aspergillus fumigatus and Alternaria spp. were positively correlated with asthma [110]. Thus, exposure to fungi may have both positive and negative consequences for human health, depending on the species and the type of exposure (e.g., dust-borne vs. air-borne). In general, however, it is difficult to compare current studies, as they relied on varying protocols. In the future, standardized methodologies will be helpful to allow for better comparisons between studies.
On a larger scale, there is evidence that the microbiome is globally connected [62] and that microbes may be transported over thousands of kilometers by dust and fine sand [63, 111] and through high altitudes up to the troposphere [38, 61]. Whether potential pathogens can cause an infection after exposure to high altitude and the associated radiation, however, remains to be shown. While a direct effect of microbes transported over long distances on human health, such as infections, is unlikely, a potential concern is the dissemination of virulence factors and antibiotic resistance genes [65].
Exposure to PM, even without attached microorganisms, has been shown to alter the intestinal microbiota and may be linked to diseases such as IBD [98–100] and type 2 diabetes [101, 102]. Whether exposure to specific airborne microbes also influences these diseases remains to be determined.
Acknowledgments
The authors thank Prof. Dr. Peter Deuflhard, Zuse Institute Berlin, for the invitation to a meeting in Beijing in 2018, where this manuscript was initiated. The authors deeply regret that he passed away after an illness in 2019. The authors would like to thank Prof. Dr. Peter Palese (Icahn School of Medicine at Mount Sinai) for his generous support.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
Karin Moelling and Felix Broecker contributed equally to this work.
References
- 1.World Health Organization. Regional Office for Europe. Geneva, Switzerland: World Health Organization; 2005. http://www.euro.who.int/en/health-topics/environment-and-health/air-quality/publications/pre2009/air-quality-guidelines.-global-update-2005.-particulate-matter,-ozone,-nitrogen-dioxide-and-sulfur-dioxide. [Google Scholar]
- 2.Directive 2008/50/EC of the European Parliament and of the council of 21 may 2008 on ambient air quality and cleaner air for Europe. http://eur-lex.europa.eu/legal-content/en/ALL/?uri=CELEX:32008L0050.
- 3.United States Environmental Protection Agency. https://www.epa.gov/clean-air-act-overview/air-pollution-current-and-future-challenges.
- 4.World Health Organization. Geneva, Switzerland: World Health Organization; 2018. Ambient (outdoor) air pollution. http://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health. [Google Scholar]
- 5.Ministry of Environmental Protection of the People’s Republic. 2017. http://www.stats.gov.cn/tjsj/ndsj/2017/indexeh.htm. [Google Scholar]
- 6.Kirby T. WHO: 92% of the world’s population breathe polluted air. Lancet Respiratory Medicine. 2016;4(11):p. 862. doi: 10.1016/s2213-2600(16)30330-7. [DOI] [PubMed] [Google Scholar]
- 7.Environmental Protection Agency. 2014. https://gispub.epa.gov/neireport/2014/
- 8.Baek B. H., Koziel J. A., Aneja V. P. A preliminary review of gas-to-particle conversion monitoring and modelling efforts in the USA. International Journal of Global Environmental Issues. 2006;6(2/3):204–230. doi: 10.1504/ijgenvi.2006.010155. [DOI] [Google Scholar]
- 9.Lelieveld J., Evans J. S., Fnais M., Giannadaki D., Pozzer A. The contribution of outdoor air pollution sources to premature mortality on a global scale. Nature. 2015;525(7569):367–371. doi: 10.1038/nature15371. [DOI] [PubMed] [Google Scholar]
- 10.Landrigan P. J., Fuller R., Acosta N. J. R., et al. The Lancet Commission on pollution and health. Lancet (London, England) 2018;391(391):462–512. doi: 10.1016/S0140-6736(17)32345-0. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. Regional Office for Europe. Geneva, Switzerland: World Health Organization; 2013. http://www.euro.who.int/__data/assets/pdf_file/0006/189051/Health-effects-of-particulate-matter-final-Eng.pdf. [Google Scholar]
- 12.Pihlava T., Uuppo M., Niemi S. Health Effects of Exhaust Particles. https://www.univaasa.fi/materiaali/pdf/isbn_978-952-476-479-7.pdf. [Google Scholar]
- 13.Momtazan M., Geravandi S., Rastegarimehr B., et al. An investigation of particulate matter and relevant cardiovascular risks in Abadan and Khorramshahr in 2014-2016. Toxin Reviews. 2019;38(4):290–297. doi: 10.1080/15569543.2018.1463266. [DOI] [Google Scholar]
- 14.Khaniabadi Y. O., Sicard P., Takdastan A., et al. Mortality and morbidity due to ambient air pollution in Iran. Clinical Epidemiology and Global Health. 2019;7(2) doi: 10.1016/j.cegh.2018.06.006. [DOI] [Google Scholar]
- 15.Goudarzi G., Geravandi S., Idani E., et al. An evaluation of hospital admission respiratory disease attributed to sulfur dioxide ambient concentration in Ahvaz from 2011 through 2013. Environmental Science and Pollution Research. 2016;23(21):22001–22007. doi: 10.1007/s11356-016-7447-x. [DOI] [PubMed] [Google Scholar]
- 16.Khaefi M., Goudarzi G., Yari A. R., et al. An association between ambient pollutants and hospital admitted respiratory cases in Ahvaz, Iran. Fresenius Environmental Bulletin. 2016;25(10):3955–3961. [Google Scholar]
- 17.Idani E., Geravandi S., Akhzari M., et al. Characteristics, sources, and health risks of atmospheric PM10-bound heavy metals in a populated middle eastern city. Toxin Reviews. 2018:1–9. doi: 10.1080/15569543.2018.1513034. [DOI] [Google Scholar]
- 18.Goudarzi G., Alavi N., Geravandi S., et al. Health risk assessment on human exposed to heavy metals in the ambient air PM10 in Ahvaz, southwest Iran. International Journal of Biometeorology. 2018;62(6):1075–1083. doi: 10.1007/s00484-018-1510-x. [DOI] [PubMed] [Google Scholar]
- 19.Ouyang Y. China wakes up to the crisis of air pollution. The Lancet Respiratory Medicine. 2013;1(1):p. 12. doi: 10.1016/s2213-2600(12)70065-6. [DOI] [PubMed] [Google Scholar]
- 20.Geravandi S., Sicard P., Khaniabadi Y. O., et al. A comparative study of hospital admissions for respiratory diseases during normal and dusty days in Iran. Environmental Science and Pollution Research. 2017;24(22):18152–18159. doi: 10.1007/s11356-017-9270-4. [DOI] [PubMed] [Google Scholar]
- 21.Churg A., Brauer M. Ambient atmospheric particles in the airways of human lungs. Ultrastructural Pathology. 2000;24(6):353–361. doi: 10.1080/019131200750060014. [DOI] [PubMed] [Google Scholar]
- 22.Hayes R. B., Lim C., Zhang Y., et al. PM2.5 air pollution and cause-specific cardiovascular disease mortality. International Journal of Epidemiology. 2020;49(1):25–35. doi: 10.1093/ije/dyz114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Litchfield I. J., Ayres J. G., Jaakkola J. J. K., et al. Is ambient air pollution associated with onset of suddent infant death syndrome: a case-crossover study in the UK. BMJ Open. 2018;8(4) doi: 10.1136/bmjopen-2017-018341.e018341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li N., Georas S., Alexis N., et al. A work group report on ultrafine particles (American Academy of Allergy, Asthma & Immunology): why ambient ultrafine and engineered nanoparticles should receive special attention for possible adverse health outcomes in human subjects. Journal of Allergy and Clinical Immunology. 2016;138(2):386–396. doi: 10.1016/j.jaci.2016.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Downward G. S., van Nunen E. J. H. M., Kerckhoffs J., et al. Long-term exposure to ultrafine particles and incidence of cardiovascular and cerebrovascular disease in a prospective study of a Dutch cohort. Environmental Health Perspectives. 2018;126(12) doi: 10.1289/ehp3047.127007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jin Y., Wu S., Zeng Z., Fu Z. Effects of environmental pollutants on gut microbiota. Environmental Pollution. 2017;222:1–9. doi: 10.1016/j.envpol.2016.11.045. [DOI] [PubMed] [Google Scholar]
- 27.Rao A. L., Bharani M., Pallavi V. Role of antioxidants and free radicals in health and disease. Advances in Pharmacology and Toxicology. 2006;7(3):29–38. [Google Scholar]
- 28.World Health Organization. Geneva, Switzerland: World Health Organization; 2018. Household air pollution and health. http://www.who.int/news-room/fact-sheets/detail/household-air-pollution-and-health. [Google Scholar]
- 29.International Institute for Applied Systems Analysis (IIASA) 2011. http://www.unece.org/fileadmin/DAM/env/documents/2011/eb/wg5/WGSR48/Informal%20docs/Info.doc.8_CIAM_report_on_Cost_effective_emission_reductions_to_improve_air_quality_in_Europe_in_2010.pdf. [Google Scholar]
- 30.Tang J. T., Li Y. Editorial: the airborne microbiome – implications for aerosol transmission and infection control–special issue. BMC Infectious Diseases. 2019;19(1):p. 755. doi: 10.1186/s12879-019-4399-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cao C., Jiang W., Wang B., et al. Inhalable microorganisms in beijing’s PM2.5and PM10Pollutants during a severe smog event. Environmental Science & Technology. 2014;48(3):1499–1507. doi: 10.1021/es4048472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gou H., Lu J., Li S., Tong Y., Xie C., Zheng X. Assessment of microbial communities in PM1 and PM10 of Urumqi during winter. Environmental Pollution. 2016;214:202–210. doi: 10.1016/j.envpol.2016.03.073. [DOI] [PubMed] [Google Scholar]
- 33.Whon T. W., Kim M.-S., Roh S. W., Shin N.-R., Lee H.-W., Bae J.-W. Metagenomic characterization of airborne viral DNA diversity in the near-surface atmosphere. Journal of Virology. 2012;86(15):8221–8231. doi: 10.1128/jvi.00293-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bertolini V., Gandolfi I., Ambrosini R., et al. Temporal variability and effect of environmental variables on airborne bacterial communities in an urban area of Northern Italy. Applied Microbiology and Biotechnology. 2013;97(14):6561–6570. doi: 10.1007/s00253-012-4450-0. [DOI] [PubMed] [Google Scholar]
- 35.Robertson C. E., Baumgartner L. K., Harris J. K., et al. Culture-independent analysis of aerosol microbiology in a metropolitan subway system. Applied and Environmental Microbiology. 2013;79(11):3485–3493. doi: 10.1128/aem.00331-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dybwad M., Granum P. E., Bruheim P., Blatny J. M. Characterization of airborne bacteria at an underground subway station. Applied and Environmental Microbiology. 2012;78(6):1917–1929. doi: 10.1128/aem.07212-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Leung M. H. Y., Wilkins D., Li E. K. T., Kong F. K. F., Lee P. K. H. Indoor-air microbiome in an urban subway network: diversity and dynamics. Applied and Environmental Microbiology. 2014;80(21):6760–6770. doi: 10.1128/aem.02244-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.DeLeon-Rodriguez N., Lathem T. L., Rodriguez-R L. M., et al. Microbiome and the upper troposphere: species composition and prevalence, effects of tropical storms, and atmospheric implications. Proceedings of the National Academy of Sciences of the United States of America. 2013;110(7):3575–3586. doi: 10.1073/pnas.1212089110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Probandt D., Eickhorst T., Ellrott A., Amann R., Knittel K. Microbial life on a sand grain: from bulk sediment to single grains. The ISME Journal. 2018;12(2):623–633. doi: 10.1038/ismej.2017.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Latgé J. P. Aspergillus fumigatus and aspergillosis. Clinical Microbiology Reviews. 1999;12(2):310–350. doi: 10.1128/cmr.12.2.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ghebremedhin B. Human adenovirus: viral pathogen with increasing importance. European Journal of Microbiology and Immunology. 2014;4(1):26–33. doi: 10.1556/eujmi.4.2014.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.GB Times. 2018. https://gbtimes.com/china-to-increase-forest-coverage-to-23-percent-by-2020.
- 43.Chew F. T., Lim S. H., Shang H. S., et al. Evaluation of the allergenicity of tropical pollen and airborne spores in Singapore. Allergy. 2000;55(4):340–347. doi: 10.1034/j.1398-9995.2000.00308.x. [DOI] [PubMed] [Google Scholar]
- 44.Grigg J. Air pollution and respiratory infection: an emerging and troubling association. American Journal of Respiratory and Critical Care Medicine. 2018;198(6):700–701. doi: 10.1164/rccm.201804-0614ed. [DOI] [PubMed] [Google Scholar]
- 45.Cui Y., Zhang Z. F., Froines J., et al. Air pollution and case fatality of SARS in the People’s Republic of China: an ecologic study. Environmental Health. 2003;2(1):p. 15. doi: 10.1186/1476-069X-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Carrington D. Air pollution likely to increase coronavirus death rate, warn experts. The Guardian, March 17. 2020. https://www.theguardian.com/environment/2020/mar/17/air-pollution-likely-to-increase-coronavirus-death-rate-warn-experts.
- 47.Ogen Y. Assessing nitrogen dioxide (NO2) levels as a contributing factor to coronavirus (COVID-19) fatality. Science of The Total Environment. 2020;726 doi: 10.1016/j.scitotenv.2020.138605.138605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wu X., Nethery R. C., Sabath B. M., et al. Exposure to air pollution and COVID-19 mortality in the United States. medRxiv 2020. [DOI] [PMC free article] [PubMed]
- 49.Coccia M. Two mechanisms for accelerated diffusion of COVID-19 outbreaks in regions with high intensity of population and polluting industrialization: the air pollution-to-human and human-to-human transmission dynamics. medRxiv. 2020 doi: 10.1101/2020.04.06.20055657. [DOI] [Google Scholar]
- 50.Setti L., Passarini F., De Gennaro G., et al. The potential role of particulate matter in the spreading of COVID-19 in Northern Italy: first evidence-based research hypotheses. medRxiv. 2020 doi: 10.1101/2020.04.11.20061713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sicard A., Zeddam J.-L., Yvon M., Michalakis Y., Gutiérrez S., Blanc S. Circulative nonpropagative aphid transmission of nanoviruses: an oversimplified view. Journal of Virology. 2015;89(19):9719–9726. doi: 10.1128/jvi.00780-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rosario K., Breitbart M., Harrach B., et al. Revisiting the taxonomy of the family Circoviridae: establishment of the genus Cyclovirus and removal of the genus Gyrovirus. Archives of Virology. 2017;162(5):1447–1463. doi: 10.1007/s00705-017-3247-y. [DOI] [PubMed] [Google Scholar]
- 53.Zerbini F. M., Briddon R. W., Idris A., et al. ICTV virus taxonomy profile: Geminiviridae. Journal of General Virology. 2017;98(5):131–133. doi: 10.1099/jgv.0.000738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pande D., Madzokere E., Hartnady P., et al. The role of Kenya in the trans-African spread of maize streak virus strain A. Virus Research. 2017;232:69–76. doi: 10.1016/j.virusres.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 55.Broecker F., Russo G., Klumpp J., Moelling K. Stable core virome despite variable microbiome after fecal transfer. Gut Microbes. 2017;8(3):214–220. doi: 10.1080/19490976.2016.1265196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tucker K. P., Parsons R., Symonds E. M., Breitbart M. Diversity and distribution of single-stranded DNA phages in the north atlantic ocean. The ISME Journal. 2011;5(5):822–830. doi: 10.1038/ismej.2010.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mizuno C. M., Ghai R., Saghaï A., López-García P., Rodriguez-Valera F. Genomes of abundant and widespread viruses from the deep ocean. MBio. 2016;7(4):e00805–e00816. doi: 10.1128/mbio.00805-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Goyal P., Choi J. J., Pinheiro L. C., et al. Clinical characteristics of covid-19 in New York city. New England Journal of Medicine. 2020 doi: 10.1056/NEJMc2010419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pellissier L., Oppliger A., Hirzel A. H., et al. Airborne and grain dust fungal community compositions are shaped regionally by plant genotypes and farming practices. Applied and Environmental Microbiology. 2016;82(7):2121–2131. doi: 10.1128/aem.03336-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Barberán A., Ladau J., Leff J. W., et al. Continental-scale distributions of dust-associated bacteria and fungi. Proceedings of the National Academy of Sciences. 2015;112(18):5756–5761. doi: 10.1073/pnas.1420815112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Maki T., Hara K., Kobayashi F., et al. Vertical distribution of airborne bacterial communities in an Asian-dust downwind area, Noto Peninsula. Atmospheric Environment. 2015;119:282–293. doi: 10.1016/j.atmosenv.2015.08.052. [DOI] [Google Scholar]
- 62.Barberán A., Henley J., Fierer N., Casamayor E. O. Structure, inter-annual recurrence, and global-scale connectivity of airborne microbial communities. Science of The Total Environment. 2014;487:187–195. doi: 10.1016/j.scitotenv.2014.04.030. [DOI] [PubMed] [Google Scholar]
- 63.Itani G. N., Smith C. A. Dust rains deliver diverse assemblages of microorganisms to the eastern mediterranean. Scientific Reports. 2016;6 doi: 10.1038/srep22657.22657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Maki T., Kurosaki Y., Onishi K., et al. Variations in the structure of airborne bacterial communities in Tsogt-Ovoo of Gobi desert area during dust events. Air Quality, Atmosphere & Health. 2017;10(3):249–260. doi: 10.1007/s11869-016-0430-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mazar Y., Cytryn E., Erel Y., Rudich Y. Effect of dust storms on the atmospheric microbiome in the eastern mediterranean. Environmental Science & Technology. 2016;50(8):4194–4202. doi: 10.1021/acs.est.5b06348. [DOI] [PubMed] [Google Scholar]
- 66.Jia S., Zhang X.-X., Miao Y., et al. Fate of antibiotic resistance genes and their associations with bacterial community in livestock breeding wastewater and its receiving river water. Water Research. 2017;124:259–268. doi: 10.1016/j.watres.2017.07.061. [DOI] [PubMed] [Google Scholar]
- 67.Miletto M., Lindow S. E. Relative and contextual contribution of different sources to the composition and abundance of indoor air bacteria in residences. Microbiome. 2015;3:p. 61. doi: 10.1186/s40168-015-0128-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Prussin A. J., II, Marr L. C. Sources of airborne microorganisms in the built environment. Microbiome. 2015;3:p. 78. doi: 10.1186/s40168-015-0144-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Prussin A. J., II, Marr L. C., Bibby K. J. Challenges of studying viral aerosol metagenomics and communities in comparison with bacterial and fungal aerosols. FEMS Microbiology Letters. 2014;357(1):1–9. doi: 10.1111/1574-6968.12487. [DOI] [PubMed] [Google Scholar]
- 70.Abtahi M., Koolivand A., Dobaradaran S., et al. National and sub-national age-sex specific and cause-specific mortality and disability-adjusted life years (DALYs) attributable to household air pollution from solid cookfuel use (HAP) in Iran, 1990-2013. Environmental Research. 2017;156:87–96. doi: 10.1016/j.envres.2017.03.026. [DOI] [PubMed] [Google Scholar]
- 71.Johnson D. L., Mead K. R., Lynch R. A., Hirst D. V. L. Lifting the lid on toilet plume aerosol: a literature review with suggestions for future research. American Journal of Infection Control. 2013;41(3):254–258. doi: 10.1016/j.ajic.2012.04.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sender R., Fuchs S., Milo R. Revised estimates for the number of human and bacteria cells in the body. PLoS Biology. 2016;14(8) doi: 10.1371/journal.pbio.1002533.e1002533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Leung M. H., Lee P. K. The roles of the outdoors and occupants in contributing to a potential pan-microbiome of the built environment: a review. Microbiome. 2016;4:p. 21. doi: 10.1186/s40168-016-0165-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Adams R. I., Bhangar S., Pasut W., et al. Chamber bioaerosol study: outdoor air and human occupants as sources of indoor airborne microbes. PLoS One. 2015;10(7) doi: 10.1371/journal.pone.0128022.e0128022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yan J., Grantham M., Pantelic J., et al. Infectious virus in exhaled breath of symptomatic seasonal influenza cases from a college community. Proceedings of the National Academy of Sciences. 2018;115(5):1081–1086. doi: 10.1073/pnas.1716561115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kettleson E. M., Adhikari A., Vesper S., Coombs K., Indugula R., Reponen T. Key determinants of the fungal and bacterial microbiomes in homes. Environmental Research. 2015;138:130–135. doi: 10.1016/j.envres.2015.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Nevalainen A., Täubel M., Hyvärinen A. Indoor fungi: companions and contaminants. Indoor Air. 2015;25(2):125–156. doi: 10.1111/ina.12182. [DOI] [PubMed] [Google Scholar]
- 78.Adams R. I., Miletto M., Taylor J. W., Bruns T. D. Dispersal in microbes: fungi in indoor air are dominated by outdoor air and show dispersal limitation at short distances. The ISME Journal. 2013;7(7):1262–1273. doi: 10.1038/ismej.2013.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Brown J. K. M., Hovmøller M. S. Aerial dispersal of pathogens on the global and continental scales and its impact on plant disease. Science. 2002;297(5581):537–541. doi: 10.1126/science.1072678. [DOI] [PubMed] [Google Scholar]
- 80.Kwong-Chung K. J., Fraser J. A., Doering T. L., et al. Cryptococcus neoformans and Cryptococcus gattii, the etiologic agents of cryptococcosis. Cold Spring Harbor Perspectives in Medicine. 2014;4(7) doi: 10.1101/cshperspect.a019760.a019760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Flint H. J., Scott K. P., Louis P., Duncan S. H. The role of the gut microbiota in nutrition and health. Nature Reviews Gastroenterology & Hepatology. 2012;9(10):577–589. doi: 10.1038/nrgastro.2012.156. [DOI] [PubMed] [Google Scholar]
- 82.Kembel S. W., Jones E., Kline J., et al. Architectural design influences the diversity and structure of the built environment microbiome. The ISME Journal. 2012;6(8):1469–1479. doi: 10.1038/ismej.2011.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lefkowitz E. J., Dempsey D. M., Hendrickson R. C., Orton R. J., Siddell S. G., Smith D. B. Virus taxonomy: the database of the international committee on taxonomy of viruses (ICTV) Nucleic Acids Research. 2018;46(D1):D708–D717. doi: 10.1093/nar/gkx932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mahy B. W. J., Regenmortel M. H. V. Desk Encyclopedia of General Virology. Oxford, UK: Elsevier Ltd. and Academic Press; 2010. [Google Scholar]
- 85.Teunis P. F. M., Moe C. L., Liu P., et al. Norwalk virus: how infectious is it? Journal of Medical Virology. 2008;80(8):1468–1476. doi: 10.1002/jmv.21237. [DOI] [PubMed] [Google Scholar]
- 86.Cui J., Li F., Shi Z.-L. Origin and evolution of pathogenic coronaviruses. Nature Reviews Microbiology. 2019;17(3):181–192. doi: 10.1038/s41579-018-0118-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Monto Z. Z. A. S., DeJonge P., Callear A. P., et al. Coronavirus occurrence and transmission over 8 years in the HIVE cohort of households in Michigan. The Journal of Infectious Diseases. 2020 doi: 10.1093/infdis/jiaa161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.McKinney K. R., Gong Y. Y., Lewis T. G. Environmental transmission of SARS at Amoy Gardens. Journal of Environmental Health. 2006;68(9):26–30. [PubMed] [Google Scholar]
- 89.Chim S. S. C., Tong Y.-K., Hung E. C. W., Chiu R. W. K., Lo Y. M. D. Genomic sequencing of a SARS coronavirus isolate that predated the Metropole Hotel case cluster in Hong Kong. Clinical Chemistry. 2004;50(1):231–233. doi: 10.1373/clinchem.2003.025536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Chan P. K., Chan M. C. Tracing the SARS-coronavirus. Journal of Thoracic Disease. 2013;5(2):S118–S121. doi: 10.3978/j.issn.2072-1439.2013.06.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Ge X.-Y., Li J.-L., Yang X.-L., et al. Isolation and characterization of a bat SARS-like coronavirus that uses the ACE2 receptor. Nature. 2013;503(7477):535–538. doi: 10.1038/nature12711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Clokie M. R. J., Millard A. D., Letarov A. V., Heaphy S. Phages in nature. Bacteriophage. 2011;1(1):31–45. doi: 10.4161/bact.1.1.14942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Suttle C. A. The significance of viruses to mortality in aquatic microbial communities. Microbial Ecology. 1994;28(2):237–243. doi: 10.1007/bf00166813. [DOI] [PubMed] [Google Scholar]
- 94.Moelling K., Broecker F. Fecal microbiota transplantation to fight Clostridium difficile infections and other intestinal diseases. Bacteriophage. 2016;6(4) doi: 10.1080/21597081.2016.1251380.e1251380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Broecker F., Klumpp J., Schuppler M., et al. Long-term changes of bacterial and viral compositions in the intestine of a recovered Clostridium difficile patient after fecal microbiota transplantation. Cold Spring Harbor Molecular Case Studies. 2016;2(1) doi: 10.1101/mcs.a000448.a000448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Salim S. Y., Kaplan G. G., Madsen K. L. Air pollution effects on the gut microbiota. Gut Microbes. 2014;5(2):215–219. doi: 10.4161/gmic.27251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Möller W., Häußinger K., Winkler-Heil R., et al. Mucociliary and long-term particle clearance in the airways of healthy nonsmoker subjects. Journal of Applied Physiology. 2004;97(6):2200–2206. doi: 10.1152/japplphysiol.00970.2003. [DOI] [PubMed] [Google Scholar]
- 98.Kish L., Hotte N., Kaplan G. G., et al. Environmental particulate matter induces murine intestinal inflammatory responses and alters the gut microbiome. PLoS One. 2013;8(4) doi: 10.1371/journal.pone.0062220.e62220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ananthakrishnan A. N., McGinley E. L., Binion D. G., Saeian K. Ambient air pollution correlates with hospitalizations for inflammatory bowel disease. Inflammatory Bowel Diseases. 2011;17(5):1138–1145. doi: 10.1002/ibd.21455. [DOI] [PubMed] [Google Scholar]
- 100.Mutlu E. A., Comba I. Y., Cho T., et al. Inhalational exposure to particulate matter air pollution alters the composition of the gut microbiome. Environmental Pollution. 2018;240:817–830. doi: 10.1016/j.envpol.2018.04.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Alderete T. L., Jones R. B., Chen Z., et al. Exposure to traffic-related air pollution and the composition of the gut microbiota in overweight and obese adolescents. Environmental Research. 2018;161:472–478. doi: 10.1016/j.envres.2017.11.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Weinmayr G., Hennig F., Fuks K., et al. Long-term exposure to fine particulate matter and incidence of type 2 diabetes mellitus in a cohort study: effects of total and traffic-specific air pollution. Environmental Health. 2015;14:p. 53. doi: 10.1186/s12940-015-0031-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Claus S. P., Guillou H., Ellero-Simatos S. The gut microbiota: a major player in the toxicity of environmental pollutants? NPJ Biofilms and Microbiomes. 2016;2 doi: 10.1038/npjbiofilms.2016.3.16003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Adar S. D., Huffnagle G. B., Curtis J. L. The respiratory microbiome: an underappreciated player in the human response to inhaled pollutants? Annals of Epidemiology. 2016;26(5):355–359. doi: 10.1016/j.annepidem.2016.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Rylance J., Kankwatira A., Nelson D. E., et al. Household air pollution and the lung microbiome of healthy adults in Malawi: a cross-sectional study. BMC Microbiology. 2016;16(1):p. 182. doi: 10.1186/s12866-016-0803-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sunagawa S., Coelho L. P., Chaffron S., et al. Structure and function of the global ocean microbiome. Science. 2015;348:6237. doi: 10.1126/science.1261359.1261359 [DOI] [PubMed] [Google Scholar]
- 107.Maciel E. L. N., Gonçalves Júnior E., Dalcolmo M. M. P. Tuberculosis and coronavirus: what do we know? Epidemiologia e Serviços de Saúde. 2020;20(2) doi: 10.5123/S1679-49742020000200010.e2020128 [DOI] [PubMed] [Google Scholar]
- 108.Shiau S., Krause K. D., Valera P., et al. The burden of COVID-19 in people living with HIV: a syndemic perspective. AIDS and Behavior. 2020 doi: 10.1007/s10461-020-02871-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Qian H., Miao T., Liu L., et al. Indoor transmission of SARS-CoV-2. medRxiv. 2020 doi: 10.1101/2020.04.04.20053058. [DOI] [PubMed] [Google Scholar]
- 110.Shabankarefard E., Ostovar A., Farrokhi S., et al. Air- and dust-borne fungi in indoor and outdoor home of allergic patients in a dust-storm-affected area. Immunological Investigations. 2017;46(6):577–589. doi: 10.1080/08820139.2017.1322102. [DOI] [PubMed] [Google Scholar]
- 111.Goudarzi G., Alawi N., Geravandi S., et al. Ambient particulate matter concentration levels of Ahwaz, Iran. Environmental Geochemistry and Health. 2019;41(2):841–849. doi: 10.1007/s10653-018-0182-0. [DOI] [PubMed] [Google Scholar]


