Abstract
Childhood obesity has become a global pandemic in developed countries, leading to a host of medical conditions that contribute to increased morbidity and premature death. The causes of obesity in childhood and adolescence are complex and multifaceted, presenting researchers and clinicians with myriad challenges in preventing and managing the problem. This chapter reviews the state-of-the-science for understanding the etiology of childhood obesity, the preventive interventions and treatment options for overweight and obesity, and the medical complications and co-occurring psychological conditions that result from excess adiposity, such as hypertension, non-alcoholic fatty liver disease, and depression. Interventions across the developmental span, varying risk levels, and service contexts (e.g., community, school, home, and healthcare systems) are reviewed. Future directions for research are offered with an emphasis on translational issues for taking evidence-based interventions to scale in a manner that reduce the public health burden of the childhood obesity pandemic.
Keywords: adiposity, childhood obesity, health psychology, prevention, research translation
1.0. INTRODUCTION
Influenced by genetics, biology, psychosocial factors, and health behaviors, overweight and obesity (OW/OB) in childhood is a complex public health problem affecting the majority of developed countries worldwide. Additionally, the key contributors to obesity—poor diet and physical inactivity—are among the leading causes of preventable youth deaths, chronic disease, and economic health burden (Friedemann et al 2012, Hamilton et al 2018). Despite the remarkable need to prevent childhood obesity and to intervene earlier to prevent excess weight gain in later developmental periods, few interventions have demonstrated long-lasting effects or been implemented at such a scale to have an appreciable public health impact (Hales et al 2018).
In this review, we describe the extent and nature of the childhood obesity pandemic, present conceptual and theoretical models for understanding its etiology, and take a translational-developmental perspective in reviewing intervention approaches within and across developmental stages and in the various contexts in which childhood OW/OB interventions are delivered. We pay particular attention to co-occurring psychological conditions intertwined with OW/OB for children, adolescents, and their families as they relate to both development/etiology and to intervention. For this reason, our review begins with interventions aimed at prevention and moves to management and treatment options for obesity and its psychological and medical comorbidities. Then, we discuss the state-of-the-science and expert recommendations for interventions to prevent and manage childhood OW/OB and what it would take to implement current evidence-based programs at scale. Last, we end by discussing identified gaps in the literature to inform future directions for research and the translation of research findings to real-world practice that can curb the pandemic. For readability, we use the term “interventions for the prevention and management of childhood OW/OB” to capture an array of approaches referred to by a variety of monikers in the literature, including primary prevention, prevention of excess weight gain, weight loss intervention, weight management, and treatment of obesity. More specific labels are used when needed.
2.0. EPIDEMIOLOGY OF CHILDHOOD OBESITY
Childhood OW/OB is determined by the child’s height and weight to calculate body mass index (BMI), which is adjusted according to norms based on the child’s age and gender. BMI between the 85th and 94th percentile is in the “overweight” range, whereas BMI ≥ 95th percentile for age and gender is in the “obese” range (Centers for Disease Control and Prevention [CDC] 2018). Rates of obesity among children and adolescents in developed countries worldwide, collected in 2013, were 12.9% for boys and 13.4% for girls (Ng et al 2014). In the United States (US) from 1999–2016, 18.4% of children ages 2–19 years had obesity, and 5.2% had severe obesity, defined as BMI ≥120% of the 95th percentile for age and gender (Skinner et al 2018). The prevalence of obesity has increased between 2011–2012 and 2015–2016 in children ages 2–5 and 16–19 years (Hales et al 2018). Being in the obese range during childhood or adolescence makes the youth five times more likely to be obese in adulthood compared to peers who maintain a healthy weight (Simmonds et al 2016). Compared to obesity, severe obesity is strongly linked with greater cardiometabolic risk, adult obesity, and premature death (Skinner et al 2015).
OW/OB and its health consequences are disproportionately distributed across the US, with a higher prevalence among children of disadvantaged racial and socioeconomic backgrounds. Rates of OW/OB are significantly higher among Non-Hispanic black and Hispanic children compared to Non-Hispanic White children (e.g., Hales et al 2018). Such disparities are particularly pronounced among severe obesity, where 12.8% of African American children, and 12.4% of Hispanic children have severe obesity compared to 5.0% of Non-Hispanic White children (Hales et al 2018). Youth in low socioeconomic households are more likely to develop OW/OB compared to their counterparts in high socioeconomic households. In 2011–2014, 18.9% of children ages 2–19 living in the lowest income group (≤130% of Federal Poverty Line) had obesity, whereas 10.9% of children in the highest income group (>350% Federal Poverty Line) had obesity (Ogden et al 2018). Influences on multiple socioecological levels put racially diverse children of low socioeconomic status (SES) at higher risk of developing OW/OB, which is further exacerbated by limited access to health services that can prevent excess weight gain and its sequelae.
3.0. ETIOLOGY OF CHILDHOOD OBESITY
At the most basic level, childhood OW/OB emerges from consuming more calories than expended, resulting in excess weight gain and an excess body fat. Caloric imbalance is the result of, and can be further exacerbated by, a range of obesogenic behaviors. That is, behaviors that are highly correlated with excess weight gain. The most common obesogenic behaviors are high consumption of sugar sweetened beverages and low-nutrient, high saturated fat foods, low levels of physical activity and high levels of sedentary behaviors, and shortened sleep duration (e.g., Sisson et al 2016). Diet, physical activity, screen time, and sleep patterns are influenced by a myriad of factors and interactions involving genetics, interpersonal relationships, environment, and community (e.g., Russell & Russell 2019, Smith et al 2018d). Children living in the United States commonly consume the “Western Diet,” known as a diet high in calories, rich in sugars, trans and saturated fats, salt and food additives, and low in complex carbohydrates, and vitamins. Poor sleep patterns, defined as short duration and late timing, can contribute to obesity through changing levels of appetite-regulating hormones, and irregular eating patterns including late night snacking and eating (Miller et al 2015). Children who experience shortened night time sleep from infancy to school age are at increased risk of developing OW/OB compared to same-aged children sleeping average, age-specific hours (e.g., Taveras et al 2014). Research indicates that children with higher rates of screen time also consume high levels of energy-dense snacks, beverages, and fast food, and fewer fruits and vegetables, and screen time is hypothesized to affect food and beverage consumption through distracted eating, reducing feelings of satiety or fullness, and exposure to advertisements for junk food (sweet and salty, calorically-dense foods) (Robinson et al 2017). Screen time can also negatively affect children’s sleeping patterns, and is correlated with sedentary behaviors (e.g., watching television, playing video games) (Hale & Guan 2015).
3.1. Conceptual Models for Understanding and Addressing Childhood OW/OB
Conceptualizing development of childhood OW/OB requires consideration of interplay of genetic, biological, psychological, behavioral, interpersonal, and environment factors (Kumar & Kelly 2017). OW/OB interventions are typically designed to account for these multilevel factors to assist children in achieving expert recommendations for physical activity and fruit and vegetable consumption, while limiting sugar sweetened beverages intake and screen time, and regulating sleep patterns (Kakinami et al 2019). Creating behavioral change requires understanding of the multi-level interactions to identify opportunities for intervention to prevent excess weight gain long-term. A variety of conceptual models exist to explain potential interactions and individual influences leading to obesogenic behaviors and development of childhood OW/OB, and targets for improving health behaviors and routines. Importantly, basic science and conceptual models can be translated to develop effective, targeted intervention programs for prevention of excess weight gain.
3.1.1. Biopsychosocial model
The biopsychosocial model combines biological foundations in child development with environmental and psychosocial influences to identify and address mechanisms and processes to prevent and manage development of childhood OW/OB (Russell & Russell 2019). This model features biological factors, such as genetics, alongside environmental, psychosocial, and behavioral risk factors (e.g., family disorganization, parenting skills, feeding practices, child appetite, temperament), and the development of self-regulation. Such an approach can illustrate developmental processes interacting with biological underpinnings that can be targeted in prevention and management interventions for OW/OB. Intervening from a biopsychosocial model involves cognitive behavioral and behavioral therapy to reframe thoughts and replace unhealthy eating behaviors with new habits.
3.1.2. Ecological systems theory (EST)
EST embeds individual development and change within multiple proximal and distal contexts and emphasizes the need to understand how an “ecological niche” can contribute to the development of specific characteristics, and how such niches are embedded in more distal contexts (Davison & Birch 2001). For example, a child’s ecological niche can be the family or school, which are embedded in larger social contexts, such as the community and society. Individual child characteristics, such as gender and age, interact within and between the family and community context levels, which all influence development of OW/OB. The EST model presents various predictors of childhood OW/OB through identifying risk factors moderated by intraindividual child characteristics. The structure of the EST is present in various studies examining influences of community exposures and children’s individual attributes on weight outcomes.
3.1.3. The Six C’s Model
The Six-C’s is a developmental ecological model that includes environmental (family, community, country, societal), personal, behavioral, and hereditary influences, and a system for categorizing environmental influences, all of which can be adapted to each stage of child development from infancy to adolescence (Harrison et al 2011). The Six C’s stand for: cell, child, clan, community, country, and culture, which represent biology/genetics, personal behaviors, family characteristics, factors outside of the home including peers and school, state and national-level institutions, and culture-specific norms, respectively. Each C includes factors that contribute to child obesity that occur and interact simultaneously throughout child development. For example, among preschool age children, obesity-predisposing genes (cell), excessive media exposure (child), parent dietary intake (clan), unhealthful peer food choices (community), national economic recession, (country) and oversized portions (culture), are all factors associated with obesity that can occur simultaneously and interact during this developmental stage.
3.1.3. The developmental cascade model of pediatric obesity
The model described in the Smith et al. (2018b) article offers a longitudinal framework to elucidate the way cumulative consequences and spreading effects of multiple risk and protective factors, across and within biopsychosocial spheres and phases of development, can propel children towards OW/OB outcomes. The cascade model of pediatric obesity (Figure 1) was developed using a theory-driven model-building approach and a search of the literature to identify paths and relationships in the model that were empirically based. The model allows for different pathways and interactions between different combinations of variables and constructs that contribute to pediatric obesity (equifinality), identifying multi-level risk and protective factors spanning from the prenatal stage to adolescence stage. The complete model can, but has yet to, be tested. The model focuses on intra- and inter-individual child processes and mechanisms (e.g., parenting practices), while acknowledging that individuals are embedded within the broader ecological systems. St. George et al (in press) then conducted a systematic review of the intervention literature to elucidate the ways in which the developmental cascade model of childhood obesity can inform and is informed by intervention approaches for childhood OW/OB.
Figure 1. Developmental cascade model of pediatric obesity.
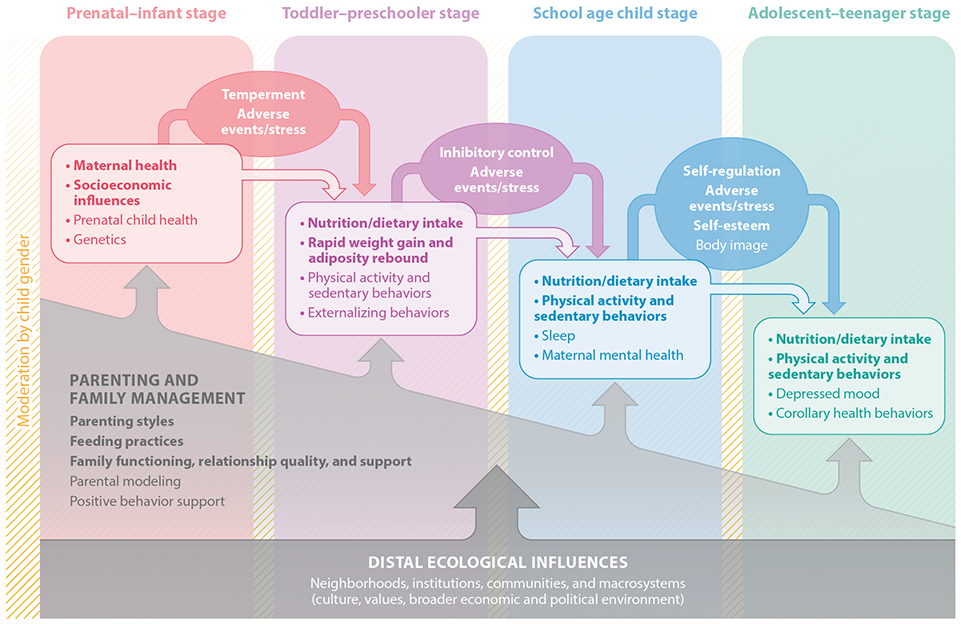
Note. Bold text indicates strongest support based on our review of the literature. Reprinted with permission from Taylor and Francis Group: Originally published in Smith JD, Egan KN, Montaño Z, Dawson-McClure S, Jake-Schoffman DE, et al. 2018. A developmental cascade perspective of paediatric obesity: Conceptual model and scoping review. Health Psychology Review 12: 271–293.
3.2. Psychosocial Contributors
3.2.1. Maternal mental and physical health
An emerging body of literature has shown a significant relationship between higher levels of parental stress and youths’ higher weight status and unhealthy lifestyle behaviors (Tate et al 2015). In a prospective study, Stout et al (2015) found that fetal exposure to stress, as evidenced by elevated maternal cortisol and corticotropin-releasing hormone, was related to patterns of increasing BMI over the first 24 months of life. Children of mothers experiencing psychological distress and anxiety during pregnancy had higher fat mass, BMI, subcutaneous and visceral fat indices, liver fat fraction, and risk of obesity at age 10 years compared to those whose mothers did not (Vehmeijer et al 2019). Early stress can have long-lasting effects, and studies from a nationally-representative cohort study have shown that postnatal maternal stress during the first year has a positive longitudinal relationship with the child’s BMI up to age 5 (Leppert et al 2018), and psychological distress at age 5 was associated with risk of obesity at age 11 in another nationally-representative cohort (Hope et al 2019). Among Hispanic children and adolescents whose caregivers reported ≥ 3 chronic stressors, Isasi et al (2017) found an increased likelihood of childhood obesity when compared to those whose parents reported no chronic stressors. In a systematic review assessing the impact of maternal stress on children’s weight-related behaviors, O’Connor et al (2017) found mixed evidence for the relationship specific to dietary intake; however, researchers found consistent evidence for the detrimental impact on youths’ physical activity and sedentary behavior, which was often conceptualized as screen time. Understandably, highly stressed parents may have an increased reliance on convenient fast-food options versus grocery shopping and preparing fresh and healthy meals for their children and may not have the energy or wherewithal to support their youths’ physical activity, nor engage in limit-setting behaviors specific to their children’s screen time.
One of the few studies using a longitudinal design did not replicate the relationship between high parental stress and lower levels of youth physical activity, but the relationship held for high levels of parental stress and increased fast food consumption (Baskind et al 2019). Interestingly, this study observed an interaction effect on the relationship of high parental stress and childhood obesity by only low-income households and among ethnic minority children, specifically non-Hispanic black children—explaining one of the factors that contributes to healthy disparities for childhood obesity rates in the US. In another study using a large, prospective cohort, Shankardass et al (2014) found a significant effect of parental stress on BMI. The researchers also observed a significantly larger effect among Hispanics versus the total sample population, further noting that the relationship was weaker and not statistically significant among non-Hispanic children. Due to the salient role of caregiver stress on child health behaviors, it seems that interventions for childhood OW/OB should incorporate stress reduction strategies for parents while simultaneously focusing efforts on reaching racial/ethnic minority families and the economically disadvantaged.
Maternal mental health, most commonly operationalized as depressive symptoms and diagnosis, relate to children’s risk for OW/OB. The longitudinal effects of postnatal maternal depressive symptoms predicted obesity risk in preschool-age children, and unhealthier lifestyle behaviors, such as high TV viewing time and low levels of physical activity (Benton et al 2015). Children of mothers with severe depression were more likely to be obese compared to children of mothers with fewer symptoms (Marshall et al 2018). Maternal mental health could negatively affect child feeding behaviors such that elevated depressive symptoms in low-income mothers have been associated with increased use of feeding to soothe children (Savage & Birch 2017). Few interventions for childhood obesity to date specifically target caregiver depression, but some protocols provide guidance to engage caregivers in services to manage depression and related stressors (Smith et al 2018c).
3.2.2. Child mental health
Poor self-regulation and related constructs such as reactivity and impulsivity, are prospective obesogenic risk factors (Bergmeier et al 2014, Smith et al 2018d). A child’s temperament describes behavioral tendencies in reactivity and self-regulation. Negative reactivity is characterized by a quick response with intense negative affect, and is difficult to soothe. Infants and children with negative reactivity are at high risk of excess weight gain, and developing obesity later on and toddlers with low self-regulation and inability to control impulses or behavior are at increased risk for obesity and rapid weight over the subsequent nine years compared to toddlers with higher self-regulation abilities (Graziano et al 2013). Poorer emotional self-regulation at age 3 is an independent predictor of obesity at age 11 (Anderson et al 2017). On the other hand, the ability to delay gratification at age 4 is associated with lower BMI 30 years later (Schlam et al 2013). It is possible that parents of children with difficult temperament experience challenges effectively managing children’s behaviors and setting limits, leading to irregular health routines and increased obesity risk (Bergmeier et al 2014, Smith et al 2018d). Further, parents could overuse food and feeding to soothe children (Anzman-Frasca et al 2012). Throughout childhood, emotional regulation deficits and other mental health disorders continue to predict obesity and weight gain. Emotional regulation in conjunction with stress during childhood is highly linked to low physical activity, emotional eating, irregular and disrupted sleep, and later development of obesity (Aparicio et al 2016). A longitudinal study examining emotional psychopathology in preadolescence saw that boys diagnosed with a social phobia, panic disorder or dysthymia (persistent depressive disorder) had higher waist circumference and/or BMI, and girls diagnosed with dysthymia had increased waist circumference at the three-year follow-up (Aparicio et al 2013). In a prospective study, overweight children who reported binge eating at ages 6–12 years gained 15% more fat mass over a period of four years compared to overweight children with no binge eating (Tanofsky-Kraff et al 2006). The predictive role of mental health on physical health conditions and subsequent comorbidities can be costly and burdensome. Children with obesity-related health conditions (e.g., type 2 diabetes, metabolic syndrome) and a comorbid psychiatric diagnosis (e.g., depressive mood disorder, bipolar disorder, attachment disorder) have higher healthcare utilization and costs per year compared to children without a comorbid psychiatric diagnosis (Janicke et al 2009a)
There is an association between OW/OB and depression in childhood and adolescence, but there is mixed evidence of the directionality of this effect among children and adolescents. A review of high quality studies by Mühlig et al (2016) saw that among nine studies examining the influence of depression on weight status, six found no significant influence. Of the studies that reported significant associations, one study saw effects only among female adolescents, another only for male adolescents, and a third showed effects of adolescent depressive symptoms on adult obesity at age 53 years only in women. Conversely, OW/OB status can have significant influences on risk of low self-esteem and depressive symptoms/diagnosis in adolescence, as discussed later in this paper.
3.2.3. Stigma/bullying
Weight-related stigma, defined as subtly or overtly having discriminatory actions against individuals with obesity, toward children with obesity can impair quality of life, and contributes to unhealthy behaviors that can worsen obesity such as social isolation, decreased physical activity, and avoidance of health care services (Pont et al 2017). Unfortunately, stigma is widespread and tolerated in society, furthering the reach of negative harm. Children with obesity face explicit weight bias and stigma from multiple environments including from parents, obesity researchers, clinical settings, and school. Parents not only demonstrate implicit bias against childhood obesity, but also implicit and explicit biases against children with obesity (Lydecker et al 2018). Even among obesity researchers and health professionals, significant implicit and explicit anti-fat bias, and explicit anti-fat attitudes increased between 2001–2013 (Tomiyama et al 2015). Exposure to stigma and weight bias can have damaging psychosocial effects on children, such that stigma can mediate the relationship between BMI, depression, and body dissatisfaction (Stevens et al 2017).
Weight stigma can also initiate bullying and weight related teasing, which can have serious psychological consequences such as depression among children, further weight gain and lessen motivation to change. A nationally representative sample of children ages 10–17 years saw that OW/OB adolescents were at higher odds of being a victim of bullying, and also higher odds of perpetrating bullying and victimizing others (Rupp & McCoy 2019). The children at higher odds of engaging in bullying, or being bullied were also at significantly higher odds of having depression, difficulty making friends, and conduct problems compared to OW/OB adolescents who were not bullies or victims of bullying. The relationship between obesity and bullying needs to be addressed through bullying engagement, and coping skills for victimization to prevent and manage associated behavioral and depressive symptoms.
3.2.4. Family functioning and home environment
Evidence suggests a link between general family functioning, parent–child relationships, communication, and use of positive behavior support strategies and childhood OW/OB (see Smith et al 2017a). Influence of general parenting styles, as opposed to the more specific feeding styles, have been extensively studied and linked to children’s diet, physical activity, and weight (Shloim et al 2015). Children raised with an authoritative (warm and demanding) parenting style had healthier diet, higher physical activity levels, and lower BMI’s than those raised with the other styles (Sleddens et al 2011). Parents proactively structuring home environments to support and positively reinforce healthy dietary and physical activity behaviors also play a key role in children’s healthy lifestyles (Smith et al 2017b). Children exposed to less supportive environments consisting of family stress, father absence, maternal depression, confinement, and unclean home environments at 1 year of age has been associated with high BMI at age 21 (Bates et al 2018). Taken together, family participation and building parenting skills can play a salient role in the prevention of childhood OW/OB (Pratt & Skelton 2018, Wen et al 2011).
4.0. PREVENTION AND MANAGEMENT OF OVERWEIGHT AND OBESITY
This section discusses the state-of-the-science in childhood OW/OB prevention and management along with salient factors related to their implementation in varied healthcare delivery systems. The current climate is being shaped by the position of the American Medical Association. In 2013, the Board voted to classify obesity as a disease that requires medical attention. This classification aimed to emphasize health risks of obesity, remove individual blame, and create new implications and opportunities for intervention. This classification can help to further: 1) a broader public understanding of the obesity condition and associated stigma; 2) prevention efforts; 3) research for treatment and management; 4) insurance reimbursement for intervention; and 5) medical education (Kyle et al 2016). In primary healthcare settings specifically, the US Preventive Services Task Force (USPSTF) gave childhood obesity screening and family-based intervention a “B” grade for evidence of effectiveness (US Preventive Services Task Force 2017), which is sufficient to open insurance reimbursement streams for activities related to the prevention and management of childhood OW/OB that did not exist before. Reimbursement has been a significant barrier to uptake of effective interventions and the impact of the USPSTF in removing this impediment is not yet fully known.
A number of high-quality systematic reviews and meta-analyses have been published in recent years, which provide the most contemporary perspective of the effectiveness of interventions for prevention and management, as well as revealing wide variability and inconsistent findings. For example, Peirson et al (2015a) saw that prevention interventions were associated with slightly improved weight outcomes compared to control groups in mixed-weight children and adolescents. However, intervention effects were not consistent among each intervention strategy tested, suggesting that specific characteristics of the interventions, such as setting, participants, dose, and tailoring, should be examined to determine what is and is not effective in achieving desired outcomes.
Intervention strategies for the prevention and management of child OW/OB occur in various contexts and within, and in coordination with, multiple service delivery systems. This is due in large part to the risk factors inherent to familial, school, and community/societal levels. Relatedly, for prevention in particular, there is some correspondence between the sample being targeted and the context, such that community and school-based interventions are far more likely to be universal (sample does not consider weight status) or selective (target sample is overweight or specifically targeted due to being at-risk for obesity; e.g., ethnic minority, low income) compared to the indicated (majority of target sample is in the obese range) models more commonly found in primary and specialty healthcare systems. Unsurprisingly, the specific intervention targets and behavior change strategies align with the context and approach (St. George et al in press).
4.1. Community Interventions
Community interventions are defined as incorporating policies and strategies aimed at reducing the population risk of obesity through legislation, modifications to the built environment, provision of accessible resources, and changes in economic/pricing/food subsidies (Bleich et al 2013). Community interventions can involve the use of media, businesses (e.g., restaurants), community health services, community gardens, community or recreational centers, city planning, and the local governments (Karacabeyli et al 2018). Interventions delivered in community settings have the ability to provide high degrees of access and exposure to strategies and programs to racially diverse, low-income children, who are at the highest risk of OW/OB. Interventions delivered in community settings can be effective, but the impact could be diminished through the lower likelihood of intervention completion due to living in lower socioeconomic circumstances and other obstacles (Fagg et al 2015).
In comparison to other settings, such as the school and family level, there were fewer studies conducted at the community level in a recent review (Bleich et al 2018). This may be due to the numerous challenges and complications involved in building community capacity and engaging community leaders, stakeholders, community agencies, and city organizations. Alternatively, it could reflect a greater focus to date on other contexts and intervention targets, which we discuss in the following sections. To address effectiveness and sustainability, a combined clinical and community intervention could hold promise, especially for racially diverse children living in a low-income community, who are most at-risk. A study by Hoffman et al (2018) showed that an integrated clinic-community model is feasible and improves physical activity and quality of life when compared to multidisciplinary treatment only in clinical care settings.
To summarize, there is promise in community-based interventions that involve either the health clinic and community partnerships or community and school partnerships. Interventions using a community-based participatory approach and a strong quasi-experimental design could achieve the long term goal of reducing both child BMI, the prevalence of OW/OB in childhood, and remission of obesity in children (Economos & Hammond 2017).
4.2. School-Based Interventions
School-based interventions are defined as taking place during school hours or after-school hours for children in kindergarten through high school, and being focused exclusively in the school or delivered primarily in the school setting with secondary settings of family/home, primary care, or community (Bleich et al 2018). Considering that the majority of children spend a significant amount of their day in school, many preventive interventions have leveraged schools as an entry point to improve the obesogenic environment by promoting more physical activity in physical education classes and recess, improving school playgrounds and nutritional options in school cafeterias, and providing healthy lifestyle education in classes or other school policies (Ickes et al 2014). Previous reviews recommend using multi-component interventions targeting two or more health behaviors (i.e., physical activity, dietary outcomes, sedentary behavior) to improve adiposity outcomes when compared to single-component interventions (e.g., Wang et al 2015). Interestingly, well-designed school-based studies are effective in improving dietary behavior, but typically do not see statistically significant differences in child BMI between intervention and control schools, except for among children who are already in the obese range (Bogart et al 2016). While increasing fruit, vegetable and water consumption are important, the health behavior modifications are not sufficient for significant long-term obesity management. A way this has been addressed is partnerships between schools and community-based interventions which also engage parents. In a review, Ickes et al (2014) found that less than half of childhood obesity interventions incorporated parents; of those studies involving parents, 75% demonstrated positive outcomes in reducing BMI or weight status. In a synthesis of systematic reviews and meta-analyses of school-based interventions, long-term interventions with a combination of diet and physical activity components and family or parental involvement significantly reduced weight among children (Khambalia et al 2012). Aligned with previous research, Bleich et al (2018) found that school-based interventions that used a multi-component approach of both physical activity and nutrition with some intervention with families in the home had the largest effects. A systematic review and meta-analysis by Wang et al (2015) observed that strength of evidence of obesity prevention programs for children ages 2–18 years was dependent on intervention type, and delivery setting(s). Strength of evidence was high for physical activity-only interventions delivered in school settings with home involvement, or combined diet and physical activity interventions delivered in school settings with home and community involvement. They also found moderately strong evidence when delivering combined interventions in school-based settings alone, in schools with home or community component, or in community with a school component.
Bleich et al (2018) also reviewed a smaller number of pre-school interventions and found some promise in both single component interventions—focusing solely on physical activity—and multi-component interventions. In two other reviews evaluating early child care center-based interventions, both found promising evidence for multi-component interventions and multiple levels influencing the child, parent, teachers/staff, and class (Sisson et al 2016, Ward et al 2017). An exemplar study, Natale et al (2017) conducted an early childhood multi-level obesity intervention, which included menu modifications at the child care center, a nutrition and physical activity educational curriculum for preschoolers, and a healthy meal preparation and role modeling curriculum for parents. At two-years follow-up, the researchers observed significantly less increase in BMI percentile among the intervention group versus controls. Overall, strong obesity prevention interventions in early care and education settings were associated with healthy eating and anthropometric outcomes, which was further improved by parental engagement. In sum, the preschool and school contexts hold promise for improving weight-related behaviors and adiposity outcomes; however, evidence is clear that parents should be engaged in the process of supporting and reinforcing their children’s health behaviors for these programs to be maximally effective (Ward et al 2017).
4.3. Family-Based Interventions
The home environment (e.g., family routines, limit setting, household chaos, crowding) has long been considered one of the most powerful influences on children’s healthy behaviors and OW/OB outcomes (Bates et al 2018). Playing an integral role in physical activity, diet, screen time, and sleep, parents can exhibit positive parenting practices (e.g., limit-setting, role modeling) and provide a healthy, supportive environment (e.g., provisions of fresh fruits and vegetables), thereby shaping their children’s lifelong habits and preventing the onset of childhood obesity (for a review see Smith et al 2018d). Family-based interventions are defined as involving either passive or active parental involvement, often with parents viewed as the primary or sole agents of change (Sung-Chan et al 2013). Active parental involvement entails repeated engagement, such as participation in workshops, counseling, or educational sessions; passive involvement does not integrally involve the parent or guardian (e.g., brochures, newsletters).
In a review evaluating family-based interventions for OW/OB prevention, Ash et al (2017) found a significant increase in the number of family-based interventions with just six studies published in 2008 compared to 35 studies in 2013. The majority of studies employed rigorous RCT study designs (73%), but almost two thirds of the studies were short-term and implemented for less than a year. A fraction of studies occurred in multiple settings and over half targeted multiple components beyond diet and physical activity, such as screen time or sleep. Many preventive studies targeting young children (pre-natal to five years old) tend to use home or primary-care based settings with parental involvement, whereas interventions targeting older children tended to take place in community- and school-based settings. These findings are commensurate with the review of St. George et al (in press), which showed a decrease in parental involvement and family-based intervention strategies with child age. This dovetails with the conclusions of Kothandan (2014) that family-based interventions demonstrated effectiveness for children younger than twelve, but for children twelve and up, school-based interventions were most effective in the short-term.
Regarding preventive interventions specifically, the majority of interventions have been tested among low SES families and predominantly white families (Ash et al 2017). Hispanics/Latinx have been well-represented in US intervention studies in comparison to other ethnic minorities (i.e., African Americans, Asians, and indigenous groups). Latinx are particularly well-suited to participate in family-based interventions given their cultural emphasis on familial values; however, a recent meta-analysis noted diminishing intervention effects with a higher proportion of Hispanic children (Ling et al 2016), which was attributed to a lack of culturally competent interventions to address language barriers and dietary preferences. In addition to incorporating other ethnic minorities and culturally appropriate interventions, Ash et al (2017) suggested that preventive family-based interventions should account for non-traditional families and their different needs and family dynamics.
In regard to family dynamics and interactions, poor family functioning has been linked with an increased risk of obesity, obesogenic behaviors, and adverse health outcomes (e.g., Pratt & Skelton 2018). Family-based care for childhood OW/OB involves targeting dietary and physical activity behaviors along with the rules of the family unit, family health routines, communication, and dynamics (Pratt & Skelton 2018). Existing protocols involve family counseling for diet and physical activity change in the home environment, with some approaches also targeting more general parenting and family management skills that have been found to impact OW/OB status of the child (Smith et al 2018a, Smith et al 2018b, Smith et al 2017b). Interventions including both parents and children have shown more positive short and long-term effects on child weight when compared to parent-only interventions and controls in some studies (Yackobovitch-Gavan et al 2018), whereas others have found comparable effects for parent-only and child-involved family-based approaches (Boutelle et al 2017). Further, parent-only interventions have been shown to be more cost-effective (Janicke et al 2009b). In a meta-analysis evaluating comprehensive behavioral family lifestyle interventions treating pediatric obesity, Janicke et al (2014) found an overall standardized effect size of 0.47, which indicates a small-to-moderate effect on BMI. The dose of treatment (i.e., number of intervention sessions, minutes spent in treatment) was positively related to the treatment effect, which provides support for the notion that more intense and longer interventions are associated with better outcomes, a conclusion also made by (Whitlock et al 2010). In addition, age was a significant moderator for weight outcomes indicating that older children had larger and more beneficial intervention effects than younger children.
Specifically, family-based interventions targeting positive behavior support have been used to address key mechanisms of change specific to promoting children’s healthy lifestyle behaviors (Smith et al 2017b). Positive behavior support has been identified as a way to reduce weight gain through improving the caregiver’s ability to support and work with the child toward a healthier diet and improved physical activity. Long-term prevention trials using family-based intervention to target positive behavior support found that children randomized to the intervention had lower BMI in the years following participation (Smith et al 2015). This finding was particularly promising given that these trials did not explicitly focus on child weight in any way; thus, prevention of childhood OW/OB was a spillover effect.
Given the various ways individual, interpersonal, and family health behaviors contribute to child obesity, a tailored family-based intervention could be effective in identifying specific family needs and providing appropriate resources. In a family-based tailored intervention, Taylor et al (2015) saw that the children of families randomized to the tailored treatment had significantly lower BMI compared to families in the usual care group. Additionally, children in the tailored treatment had better dietary behaviors and were more physically active than children in the treatment as usual group. Smith, Berkel et al. (2018b) adapted the highly effective and well-known individually-tailored family-based prevention program called the Family Check-Up® (Dishion et al 2008) to specifically target obesogenic behaviors with the aim of preventing obesity and excess weight gain in children ages 2 to 12 years. This adaptation is referred to as the Family Check-Up® 4 Health and is being tested in two large RCTs in coordination with pediatric primary care (Smith et al 2018a) and with community-based family resource centers and public schools (Berkel et al 2019) in low-income neighborhoods with racially/ethnically-diverse families at highest risk for childhood OW/OB.
4.4. Primary Healthcare
Primary care interventions are defined as health promotion or weight management programs conducted within or in close coordination with the primary healthcare system. Primary care is viewed as an ideal, real world environment for weight management interventions because of accessibility and frequency of visits (i.e., routine well-child visits) (Davis et al 2007). In a meta-analysis evaluating weight management interventions delivered in primary-care settings, Mitchell et al (2016) found an overall effect size of 0.26, indicating a small treatment effect, and a smaller effect than has been found in broader meta-analytic reviews (e.g., Janicke et al 2014, Whitlock et al 2010). The dose-response relationship was significant, where the number of treatment contacts, length of treatment in months, and the number of visits with the pediatrician was associated with larger treatment effects.
A systematic review examining randomized control trials targeting obesity management in children ages 2–5 years saw five of six interventions, all in ambulatory healthcare settings, had significant decreases in child weight, with sustained intervention effects through follow-up (Ling et al 2016). The effective interventions actively involved parents in health education, group meetings, physical activity sessions, or behavioral therapy.
4.5. Interventions by Developmental Period
In a review of interventions of OW/OB from birth to age 18, St. George et al (in press) identified 74 distinct interventions reported across the 141 included articles. They were categorized based on the child’s age at entry into the intervention: prenatal/infancy (< 2 years; n = 4), early childhood (2–5 years; n = 11), childhood (6–11 years; n = 38), early adolescence (12–15 years; n = 18), and late adolescence (16–18 years; n = 3). Developmental stage of the child has also been found to align with the strategy, such that interventions in the prenatal and infancy periods are nearly all universal, whereas during childhood and adolescence, as compared to early childhood, the burden of disease is larger and intervention strategies more often target selected and indicated samples with greater intensity (St. George et al in press).
5.0. EXPERT RECOMMENDATIONS
5.1. Youth Health Behaviors
It is recommended that children and adolescents aged 6–17 years should achieve ≥ 60 minutes of physical activity each day (Piercy et al 2018). The 2015–2020 Dietary Guidelines for Americans recommend consuming a variety of fruits and vegetables, whole grains, proteins, low-fat dairy products, and limiting intake of sodium, solid fats and added sugars beginning at age 2 years (DeSalvo et al 2016). Unfortunately, only 21.6% of children 6–19 years reach the recommended 60 minutes of physical activity at least five days per week (Alliance 2016). Dietary quality impacts weight gain and OW/OB, and it is estimated that the obesity epidemic largely contributed to statistics showing a declining life expectancy, which occurred in 2015 for the first time in 30 years (Ludwig 2016).
The American Academy of Pediatrics (AAP) recommends that children under 18 months should have no screen time aside from video-chatting, and children ages 2–5 years engage in one hour of screen time per day of high-quality programs with parents. Children ages 6 and above should have limited media exposure, ≤ 2 hours per day, which should not interfere with sleep, physical activity, or other health behaviors. The AAP recommends that families should have “media-free” time together, and “media-free” locations such as in the dining room or bedroom to avoid interfering with meals and sleep duration (American Academy of Pediatrics Council on Communications and Media 2016). The World Health Organization asserts that screen time brings no benefit to children, and infants younger than one year should have no electronic screen exposure, and children age 2–4 years should not have more than one hour of daily “sedentary screen time.” In recent years, the portability of screen devices has led to an overall increase in screen time, with the majority of US youth exceeding screen time guidelines by a wide margin (averaging more than 7 hours daily) (Barnett Tracie et al 2018).
The most recent AAP guidelines recommend that children ages 1–2 years sleep 11–14 hours per 24 hours, children 3–5 sleep 10–13 hours, children 6–12 sleep 9–12 hours, and teenagers ages 13–18 should regularly sleep 8–10 hours (Paruthi et al 2016). Certain behaviors such as a regular routine, avoiding large meals close to bedtime, being physically active during the day time, and eliminating electronic devices in the bedroom are associated with better sleep (Irish et al 2015). According to the CDC, 60% of middle schoolers and 70% of high schoolers do not meet regular sleep recommendations.
5.2. Behavioral Intervention
Family-based intervention is recommended by The National Academy of Medicine, the American Academy of Pediatrics, and the Endocrine Society, among others, as the preferred approach for the management of OW/OB from infancy to adolescence. Based on a systematic review, the USPSTF concluded that lifestyle-based weight loss interventions (not necessarily family-based) consisting of 26 or more hours of intervention engagement are likely to assist children and adolescents in weight management (O’Connor et al 2017). Recommendations from a number of expert committees and task forces support targeting the following behaviors for prevention and management of childhood OW/OB: limiting consumption of sugar sweetened beverages, consuming daily recommended fruit and vegetables, limiting screen time, increasing physical activity, eating breakfast, limiting eating out at restaurants, encouraging family meals, and limiting portion sizes. The majority of existing interventions target multiple behaviors, but some have been designed for discrete behaviors.
5.3. Pharmacologic Intervention
Orlistat is the only FDA-approved medication for treating obesity for pediatric patients ages 12 years and older. Side effects in the gastrointestinal area are common in children, and further clinical trials are needed to evaluate medication risk and benefits among pediatric patients (Chao et al 2018). Expert opinion states that Orlistat, in conjunction to lifestyle changes, leads to modest weight loss and could benefit children in the indicated age range with obesity but tolerability limits its use (Kelly & Fox 2018). And results are not unequivocal. In a meta-analysis looking at primary-care based interventions, Peirson et al (2015b) found a medium effect (standardized effect size [ES] = −0.54) favoring behavioral interventions when compared to Orlistat plus behavioral intervention components (ES = −0.43). Additional research is needed on both effectiveness and tolerability in youth. Additionally, new pharmacologic options continue to be developed and tested and could reach the market in the next few years if approval is granted (Kelly & Fox 2018).
5.4. Surgical Intervention
The American Society for Metabolic and Bariatric Surgery Pediatric Committee’s best practice guidelines selection criteria are based on systematic reviews of co-morbidities, risks and outcomes, important team members, and patient selection. They recommend that adolescents being considered for a bariatric procedure should have a BMI of ≥35 kg/m2 with major co-morbidities such as type-2 diabetes mellitus, moderate to severe sleep apnea, or severe nonalcoholic steatohepatitis (Michalsky et al 2012). Data show that bariatric surgery in morbidly obese adolescents can greatly impact weight loss, and attenuate or resolve associated chronic disease. However, adolescents undergoing bariatric surgery should be assessed for capability to adhere to follow-up care regimens to ensure proper nutrition intake and care. The committee also recommends a multidisciplinary team for adolescents undergoing bariatric surgery, which could include an experienced bariatric surgeon, pediatric specialist, registered dietitian, mental health specialist, care coordinator, and exercise physiologist.
6.0. CLINICAL IMPLICATIONS OF CO-OCCURRING MEDICAL AND PSYCHOLOGICAL CONDITIONS
6.1. Co-Occurring Medical Conditions
The pro-inflammatory disease nature of obesity and contributing health behaviors affects normal physiology and metabolism, and can cause many associated diseases (Gonzalez-Muniesa et al 2017). If left untreated, obesity can lead to serious health conditions including type-2 diabetes, cardiovascular disease, asthma, obstructive sleep apnea, high blood pressure/hypertension, non-alcoholic fatty liver disease, hepatocellular carcinoma, and psychosocial problems (e.g., Nobili et al 2015). Recent research indicates increased risk of cardiovascular disease incidence, morbidity (ischemic heart disease, stroke), and mortality in adulthood associated with being in the obese BMI range in childhood or adolescence (Sommer & Twig 2018). Obesity prevention and management interventions in childhood are imperative for averting the burden of associated comorbidities.
6.1.1. Type-2 diabetes
Children with obesity are four times as likely to develop type-2 diabetes compared to children with a normal BMI (Abbasi et al 2017). Ethnic minority children of low income are at increased risk, and have limited maintenance and glycemic control, furthering the probability of developing additional health complications down the line (Pulgaron & Delamater 2014). Metformin is the main treatment of type-2 diabetes in youth and adults, though emerging evidence implicates a role in treating children with obesity and a family history of type-2 diabetes (e.g., Warnakulasuriya et al 2018). Exercise and lifestyle interventions have had significantly positive health effects in adults, however trials evaluating effects in youth with type-2 diabetes are limited. Given the data from adult trials, the American Diabetes Association recommends that youth with type-2 diabetes meet the 1-hour per day physical activity goal to manage symptoms and decrease health risks (Colberg et al 2016).
6.1.2. Obstructive sleep apnea
Pediatric obstructive sleep apnea (OSA) involves a child having disrupted breathing due to partially or completely blocked upper airways during sleep (Narang & Mathew 2012). Obesity confers the most significant risk for OSA. As many as 60% of children and adolescents with obesity have OSA, or some sort of disrupted breathing during sleep (Narang & Mathew 2012). Obesity and OSA have additional comorbidities and impairments including excessive daytime sleepiness, neurocognitive function, reduced physical activity, cardiovascular burden, and hypertension, further complicating quality life of children with obesity (Blechner & Williamson 2016). Obesity management such as increased physical activity and a healthy diet are recommended for OSA treatment, as well as surgical procedures, if appropriate.
6.1.3. Asthma
Asthma is one of the most common chronic diseases among children and adolescents: 10.1% of children ages 5–14 years had asthma in 2016 (National Center for Health Statistics 2019). Although both obesity and asthma rates have been increasing, it does not appear that obesity has been contributing to the increased asthma prevalence rate (Akinbami et al 2018). This does not discount the risks of obesity on asthma and its unique effects on asthma symptoms. OW/OB children have been observed to have higher prevalence of asthma, and exacerbation as early as preschool age compared to normal weight children (Lang et al 2018). Additionally, OW/OB children have reported distinct asthma symptoms, such as greater shortness of breath, reduced airway hyperresponsiveness, and loss of asthma control, compared to normal weight children (Lang et al 2015). The relationship between asthma and OW/OB should be further investigated.
6.1.4. Hypertension
Hypertension, like obesity, has been increasing among youth and is associated with increased cardiovascular disease risk throughout the lifetime (May et al 2012). The greatest risk factor for pediatric hypertension is elevated BMI (Falkner et al 2006). About 3% of children in the general population have hypertension, compared to about 25% of obese children (Shatat & Brady 2018). In a meta-analysis examining cardiovascular risk factors, compared with normal weight children, systolic blood pressure was higher by 4.54 mm Hg (n=12169, 8 studies) in overweight children, and by 7.49 mm Hg (n=8074, 15 studies) in obese children (Friedemann et al 2012). A study examining childhood hypertension and OW/OB in school children saw that 2.2% of the sample had hypertension, and 37% of those cases could be attributed to OW/OB status (Chiolero et al 2007). A review shows that children with obesity-related hypertension are at increased risk of cardiovascular morbidity and mortality (Wuhl 2019). About 3.8%–24.8% of children with OW/OB have hypertension, though these rates could be higher due to inconsistences and challenges with diagnoses (Flynn et al 2017). The risks of hypertension on children’s lifetime health emphasize the importance of preventing obesity early on.
6.1.5. Nonalcoholic fatty liver disease (NAFLD)
NAFLD is the leading cause of liver disease, leading to a shorter life expectancy due to associated comorbidities; one of which, non-alcoholic steatohepatitis, is projected to be the leading indication for pediatric liver transplant by 2025 (Charlton et al 2011). Epidemiological studies consistently show associations between NAFLD and adiposity, unhealthy diet, and sedentary behavior (Dunn & Schwimmer 2008). Prevalence of NAFLD is especially high in young people who have obesity such that 22.5%–52.8% of children with obesity have NAFLD compared to 2.6% of all children (Anderson et al 2015). Child obesity has the highest risk in the development of NAFLD during childhood (Hays & McGinnis 2018). A longitudinal study of participants ages 3–18 years were followed for 31 years, and saw that child OW/OB was associated with increased risk for adult NAFLD (Cuthbertson et al 2018). The associated risk was removed if participants obtained a normal range BMI by adulthood, emphasizing the salient role of weight management. The high prevalence of NAFLD among children with obesity, and effectiveness of weight change in treating this condition, emphasizes the need for prevention and management of obesity. Smith et al (2017a) found that among children who had NAFLD, poorer family functioning was significantly related to higher BMI, elevated levels of cholesterol, HbA1c, and glucose. Their study exposes the critical role of family functioning on child health, and the importance of using targeted intervention to prevent, and manage obesity and associated disease using a family-centered approach. Weight being the most modifiable factor, the mainstay of NAFLD treatment is lifestyle behavior modifications aimed at weight loss (Marchesini et al 2015).
6.2. Co-Occurring Psychological Conditions
6.2.1. Self-esteem/depression
Children with OW/OB are more likely to experience low self-esteem, and develop depressive symptoms during adolescence compared to normal weight peers (e.g., Mühlig et al 2016). This relationship can be attributed to multi-level factors including health behaviors, parenting styles, and family functioning. A review by Hoare et al (2014) suggests that obesogenic risk factors, such as infrequent physical activity, sedentary behavior, poor diet quality, and adiposity were associated with depressive symptoms in adolescents. Conversely, healthier eating patterns were associated with decreased depressive symptoms. Child eating disorder pathology, emotionally-manipulative parenting style, and lower child social status have been associated with depressive symptomatology among children with OW/OB (Sheinbein et al 2019). Children in poorly functioning families with low self-esteem participating in weight loss interventions have been observed to have poor 6-month outcomes, suggesting that multiple social-ecological factors need to be addressed when targeting depressive symptoms in children with OW/OB (Taylor et al 2017). Further, negative psychological experiences more generally, such as trauma and stigma, trigger emotional eating, leading to an ongoing obesity-depression cycle (Milaneschi et al 2019).
6.2.2. Eating disorders
Children with OW/OB have a high prevalence of disordered eating attitudes and behaviors, which can increase risk of developing eating disorders in adulthood. A high proportion of adolescents with restrictive eating disorders report a history of OW/OB (Lebow et al 2015). Additionally, it is estimated that over a quarter of youth with OW/OB have binge and loss of control eating (He et al 2017). Adolescent girls with OW/OB experiencing overvaluation of weight—so concerned with weight that self-evaluation is influenced—are at higher risk of starting to binge eat weekly 2 years later, have more severe depressive symptoms, and continuous overvaluation (Sonneville et al 2015). The bidirectional relationship of obesity and eating disorders, including eating disorder psychopathology, should be properly evaluated during treatment planning.
7.0. IMPLEMENTATION AND RESEARCH TRANSLATION CHALLENGES
One of the abundant challenges for the field is the translation and implementation of effective interventions to the real-world service delivery systems that can reach those most in need. This so-called research-practice gap is pronounced in obesity prevention and management given the preponderance of untested, usual care approaches currently in use; the persistence of debunked myths about causes and effective intervention approaches (e.g., fad diets); and the incongruence between what is being developed by experts and what is acceptable, feasible, and sustainable in existing systems given the constraints of the workforce, space, and funding. This says nothing about the consumer of evidence-based interventions, who historically have had only cursory involvement in the design and deployment of interventions. This has contributed to low engagement rates and high attrition from more intensive OW/OB interventions (Lydecker & Grilo 2016). Raising public and caregiver concern about the risks posed by OW/OB in childhood and adolescence would also facilitate engagement and retention. Currently, many parents with children with obesity underestimate their children’s weight (Lydecker & Grilo 2016) and are thus unlikely to seek intervention or to follow through with a referral for intervention. Add the stigma in society surrounding obesity and the shame parents experience concerning their child’s weight, and traditional approaches to care will continue to be underutilized.
While many of the aforementioned conceptual models encapsulate the multiple levels contributing to childhood obesity, researchers are trying to elucidate which combination of levels and service contexts have greatest effectiveness, and which implementation strategies best address the complexity at levels of the community, school, family, and primary care. Implementation strategies are defined as the methods or techniques used to enhance the adoption, implementation, and sustainability of a clinical program or practice (Proctor et al 2013). They are the actions taken on agents in the system of care itself, and rarely only on the patient or client that is the recipient of the clinical program or practice. The first iteration of the Childhood Obesity Research Demonstration Projects (CORD 1.0), a program of research administered by the CDC, examined multi-sector intervention implementation in schools, community centers, early care and health centers, and pediatric primary care practices. The three projects around the US, identified the facilitators and barriers of implementing multi-setting interventions targeting levels of the socioecologial model in racially diverse, lower-income communities (Dooyema et al 2017). CORD 1.0 projects identified common implementation barriers in schools, rural communities and community centers, including staff turnover, limited resources, and competing needs for existing requirements (such as standardized testing in schools) (Chuang et al 2016, Ganter et al 2017). Interventions in rural communities and multiple settings benefited from engaging parents and obtaining support from organization members and leadership (Chuang et al 2016, Ganter et al 2017). Facilitators of school interventions included using the principal as a champion and using students to engage other students (Blaine et al 2017). Low-income primary care settings showed that only about 27% of referred patients enrolled in the intervention (Barlow et al 2017). Such knowledge assists in the design of future studies to develop effective, accessible, and acceptable interventions for those needing it most.
These implementation challenges are not unique to childhood obesity but the complexity of the problem will require more rapid translation of discoveries in research with bidirectional input from successes and failures in practice back to researchers. Last, improving the packaging of evidence-based programs can provide potential implementers with a “ready off the shelf” product that requires less involvement by the intervention developers, which is a primary contributor to the high cost of adopting a new program (Jordan et al 2019), and can arguably aid implementers in delivering interventions with fidelity. This is the goal of the CDC’s Childhood Obesity Research Demonstration (CORD) 3.0 Project (https://www.cdc.gov/obesity/strategies/healthcare/cord3.html). However, the scale up penalty—reduced effects as interventions are widely disseminated and adopted—has been shown in the childhood obesity literature to be about 75% of efficacy studies (McCrabb et al 2019), but implementation scientists have argued for dynamic adaptation that retains effectiveness while also increasing sustainability (e.g., Chambers et al 2013). This is an area in need of attention as interventions are taken to scale.
8.0. RECOMMENDATIONS FOR FUTURE RESEARCH
Reviews of interventions for childhood OW/OB show variability in effectiveness, often changing health behaviors but not weight, thus exposing the difficulties of addressing and managing this public health crisis. There are a number of directions for future research to improve outcomes and address the challenges of wide-scale implementation.
1). Interventions need to be integrated across systems.
Given the multifaceted, multilevel, and interrelated nature of OW/OB development, if interventions are to be maximally effective there needs to be an integration of multiple service systems (primary care, schools, communities, child care, the home) for the delivery of multicomponent interventions that utilize behavioral, structural, environmental, policy, and biomedical approaches.
2). There is no “one size fits all.”
More complex, individual child and family interventions need to be tailored both in terms of content and implementation strategy to best align with the personal needs of those involved. This means flexible, adaptive, or modularized intervention protocols addressing the cadre of potential health behaviors and related individual and familial risk factors of OW/OB present, and getting the intervention to families in a manner that is engaging, accessible, and has wide reach.
3). Consider implementation earlier.
Researchers developing interventions for childhood OW/OB ought to consider their implementability from the beginning using the framework of “designing for dissemination and implementation” (Dearing et al 2013), which considers the capacities, needs, and preferences of the end users (service delivery systems, children/families, funding mechanisms) during design and testing. Another method for speeding translation is to adapt existing programs for new service contexts and new populations, rather than following the traditional pipeline of treating something different as “new” and having to establish efficacy and effectiveness before moving to implement. This concept has been referred to as “scaling out” (Aarons et al 2017) and it has been applied in childhood OW/OB prevention and management (Smith et al 2018b). Scaling out is a critical method for implementation research to address the health inequities and disparities of childhood obesity (McNulty et al 2019).
4). Engage the community to enhance scalability and sustainability.
Berkel et al (in press) engaged a diverse group of stakeholders, including payors, in the adaptation and delivery processes of a recent trial of the Family Check-Up® 4 Health as a means of increasing the likelihood of sustained adoption beyond the funded trial. Economos and Hammond (2017) suggest that community-level research should employ novel techniques of systems mapping and causal loop diagramming, which can help stakeholders to visualize the interrelated processes and elements that are relevant to the intervention. They also suggest using agent-based modeling and other simulation methods to help encapsulate the complex dynamics involved in implementing successful community-based interventions. Tailoring strategies to local communities and deepening engagement holds promise in enhancing sustainability and scalability of community-based interventions.
5). Research rigor—scale up balance.
Future directions should address the shortcomings of less rigorous study designs, which inherently increases the risk of confounding and presents challenges in attributing changes in the outcome to intervention effects, but as research translation moves toward scaling up after establishing effectiveness, this tradeoff is both expected and encouraged to increase external validity. Additionally, research is needed to determine the appropriate length and dosage of interventions, along with clear reporting of outcomes, consistency of measures, and long-term follow ups (Bleich et al 2018, Ickes et al 2014, St. George et al in press). Echoing Karacabeyli et al (2018), we also recommend collecting process evaluation and outcome data in order to understand the complex causal chain and to help bolster inferences in regard to the effectiveness and implementation of the intervention using hybrid designs .
6). Engagement and participation are critical challenges.
Large community trials in particular often suffer high attrition rates because of mobile populations who move to different residences, which can impact the ability to track and communicate with participants. And this relates to effectiveness. Children completing >75% of a community-based intervention program experienced beneficial change in BMI as well as associated health behaviors (physical activity, screen time, unhealthy food consumption) compared with children completing <75% of the program (Hardy et al 2015). A way to attenuate attrition in research on community-level interventions could be through adjusting study intervention design. The majority of community-based interventions used a quasi-experimental design, which is often attributed to practicality and sustainability (Bleich et al 2018, Karacabeyli et al 2018). Interestingly, less rigorous study designs (e.g., quasi-experimental vs. RCTs) demonstrated significant reductions in child weight (Karacabeyli et al 2018). By removing randomization, the authors reported that communities with the resources, engagement/buy-in, and capacity could be selected to participate, which optimized community support for the obesity intervention efforts through both sustainable partnerships and buy-in from the community and its champions. This participatory approach could potentially lead to lasting positive health changes that extend beyond the study period. In addition, Karacabeyli et al (2018) described the benefits of a quasi-experimental design which lends itself to selecting at-risk communities that could greatly benefit from intervention efforts. For example, using a stepped wedge or randomized rollout trial design where all at-risk communities selected would eventually receive the intervention at different time periods but none serve as “no intervention” controls (see Landsverk et al 2017).
9. CONCLUSIONS
There are signs that progress is being made in stemming the tide of childhood obesity and evidence-based interventions are available across development and for various contexts and systems that affected and at-risk children routinely encounter. Tremendous challenges remain in connecting the dots between etiology, development, and intervention targets, as well as when and where to intervene. There needs to be a push to scale up effective interventions as even small changes in weight can yield significant impact on multiple cardiometabolic indices (Lloyd-Jones et al 2010) that can improve quality and length of life. Clinical health psychologists are ideally suited to conduct research on this complex problem but transdisciplinary teams will be needed to increasingly move the dial.
SUMMARY POINTS.
Childhood obesity is a complex, multidetermined, preventable chronic disease that increases risk for premature death and psychological problems.
Evidence-based interventions for obesity are available for all stages of development from birth to 18 years.
Specific interventions can be delivered in community, school, home, and healthcare settings depending on the type of strategy and risk level of the targeted population.
Associated co-occurring medical and psychological conditions of childhood obesity present an opportunity for clinical and health psychology researchers and practitioners.
FUTURE ISSUES.
Future research ought to focus on translational considerations from the start and ways to scale up delivery of effective interventions.
Research is needed on interventions and their implementation to more effectively reach minority and underserved populations at greatest risk for obesity.
Increasing engagement and retention in childhood obesity interventions is a promising focus for future research.
ACKNOWLEDGEMENTS
The authors wish to thank Sara St. George for feedback on an earlier version of this review and to acknowledge support of this work from the Centers for Disease Control and Prevention (grant U18DP006255) and the United States Department of Agriculture (grant 2018-68001-27550), awarded to Justin Smith and Cady Berkel; and the National Institute on Drug Abuse (grant P30 DA027828), to C. Hendricks Brown, in support of Justin Smith.
Footnotes
DISCLOSURE STATEMENT
Justin D. Smith is co-developer of the Family Check-Up® 4 Health intervention for childhood obesity. The authors are not aware of any other affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this review.
LITERATURE CITED
- Aarons GA, Sklar M, Mustanski B, Benbow N, Brown CH. 2017. “Scaling-out” evidence-based interventions to new populations or new health care delivery systems. Implementation Science 12: 111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abbasi A, Juszczyk D, van Jaarsveld CHM, Gulliford MC. 2017. Body Mass Index and Incident Type 1 and Type 2 Diabetes in Children and Young Adults: A Retrospective Cohort Study. Journal of the Endocrine Society 1: 524–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akinbami LJ, Rossen LM, Fakhouri THI, Fryar CD. 2018. Asthma prevalence trends by weight status among US children aged 2–19 years, 1988–2014. Pediatric Obesity 13: 393–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alliance NPAP. 2016. 2016 US report card on physical activity for children and youth
- American Academy of Pediatrics Council on Communications and Media. 2016. Media and Young Minds. Pediatrics 138: e20162591. [DOI] [PubMed] [Google Scholar]
- Anderson EL, Howe LD, Jones HE, Higgins JP, Lawlor DA, Fraser A. 2015. The Prevalence of Non-Alcoholic Fatty Liver Disease in Children and Adolescents: A Systematic Review and Meta-Analysis. PLoS One 10: e0140908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson SE, Sacker A, Whitaker RC, Kelly Y. 2017. Self-regulation and household routines at age three and obesity at age eleven: longitudinal analysis of the UK Millennium Cohort Study. International Journal Of Obesity 41: 1459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anzman-Frasca S, Stifter CA, Birch LL. 2012. Temperament and childhood obesity risk: A review of the literature. Journal of Developmental & Behavioral Pediatrics 33: 732–45 [DOI] [PubMed] [Google Scholar]
- Aparicio E, Canals J, Arija V, De Henauw S, Michels N. 2016. The role of emotion regulation in childhood obesity: implications for prevention and treatment. Nutrition Research Reviews 29: 17–29 [DOI] [PubMed] [Google Scholar]
- Aparicio E, Canals J, Voltas N, Hernandez-Martinez C, Arija V. 2013. Emotional psychopathology and increased adiposity: Follow-up study in adolescents. Journal of Adolescence 36: 319–30 [DOI] [PubMed] [Google Scholar]
- Ash T, Agaronov A, Young T, Aftosmes-Tobio A, Davison KK. 2017. Family-based childhood obesity prevention interventions: a systematic review and quantitative content analysis. The international journal of behavioral nutrition and physical activity 14: 113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow SE, Butte NF, Hoelscher DM, Salahuddin M, Pont SJ. 2017. Strategies to Recruit a Diverse Low-Income Population to Child Weight Management Programs From Primary Care Practices. Preventing chronic disease 14: E138–E38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett Tracie A, Kelly Aaron S, Young Deborah R, Perry Cynthia K, Pratt Charlotte A, et al. 2018. Sedentary Behaviors in Today’s Youth: Approaches to the Prevention and Management of Childhood Obesity: A Scientific Statement From the American Heart Association. Circulation 138: e142–e59 [DOI] [PubMed] [Google Scholar]
- Baskind MJ, Taveras EM, Gerber MW, Fiechtner L, Horan C, Sharifi M. 2019. Parent-Perceived Stress and Its Association With Children's Weight and Obesity-Related Behaviors. Prev Chronic Dis 16: E39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates CR, Buscemi J, Nicholson LM, Cory M, Jagpal A, Bohnert AM. 2018. Links between the organization of the family home environment and child obesity: A systematic review. Obesity Reviews 19: 716–27 [DOI] [PubMed] [Google Scholar]
- Benton PM, Skouteris H, Hayden M. 2015. Does maternal psychopathology increase the risk of pre-schooler obesity? A systematic review. Appetite 87: 259–82 [DOI] [PubMed] [Google Scholar]
- Bergmeier H, Skouteris H, Horwood S, Hooley M, Richardson B. 2014. Child temperament and maternal predictors of preschool children's eating and body mass index. A prospective study. Appetite 74: 125–32 [DOI] [PubMed] [Google Scholar]
- Berkel C, Rudo-Stern J, Villamar JA, Wilson C, Flanagan E, et al. in press. Recommendations from community partners to promote sustainable implementation of evidence-based programs in primary care. Journal of Community Psychology [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkel C, Smith JD, Bruening MM, Jordan N, Grimm K, et al. 2019. The Family Check-Up 4 Health: A Health Maintenance Approach to Improve Nutrition and Prevent Early Childhood Obesity. Presented at Society for Nutrition Education and Behavior Annual Conference Orlando, FL [Google Scholar]
- Blaine RE, Franckle RL, Ganter C, Falbe J, Giles C, et al. 2017. Using School Staff Members to Implement a Childhood Obesity Prevention Intervention in Low-Income School Districts: the Massachusetts Childhood Obesity Research Demonstration (MA-CORD Project), 2012-2014. Prev Chronic Dis 14: E03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blechner M, Williamson AA. 2016. Consequences of Obstructive Sleep Apnea in Children. Current Problems in Pediatric and Adolescent Health Care 46: 19–26 [DOI] [PubMed] [Google Scholar]
- Bleich SN, Segal J, Wu Y, Wilson R, Wang Y. 2013. Systematic Review of Community-Based Childhood Obesity Prevention Studies. Pediatrics 132: e201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleich SN, Vercammen KA, Zatz LY, Frelier JM, Ebbeling CB, Peeters A. 2018. Interventions to prevent global childhood overweight and obesity: a systematic review. The lancet. Diabetes & endocrinology 6: 332–46 [DOI] [PubMed] [Google Scholar]
- Bogart LM, Elliott MN, Cowgill BO, Klein DJ, Hawes-Dawson J, et al. 2016. Two-Year BMI Outcomes From a School-Based Intervention for Nutrition and Exercise: A Randomized Trial. Pediatrics 137: e20152493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boutelle KN, Rhee KE, Liang J, Braden A, Douglas J, et al. 2017. Effect of Attendance of the Child on Body Weight, Energy Intake, and Physical Activity in Childhood Obesity Treatment: A Randomized Clinical Trial. JAMA Pediatrics 171: 622–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. 2018. Defining Childhood Obesity. [Google Scholar]
- Chambers DA, Glasgow R, Stange K. 2013. The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change. Implement Sci 8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chao AM, Wadden TA, Berkowitz RI. 2018. The safety of pharmacologic treatment for pediatric obesity. Expert Opinion on Drug Safety 17: 379–85 [DOI] [PubMed] [Google Scholar]
- Charlton MR, Burns JM, Pedersen RA, Watt KD, Heimbach JK, Dierkhising RA. 2011. Frequency and outcomes of liver transplantation for nonalcoholic steatohepatitis in the United States. Gastroenterology 141: 1249–53 [DOI] [PubMed] [Google Scholar]
- Chiolero A, Cachat F, Burnier M, Paccaud F, Bovet P. 2007. Prevalence of hypertension in schoolchildren based on repeated measurements and association with overweight. Journal of Hypertension 25: 2209–17 [DOI] [PubMed] [Google Scholar]
- Chuang E, Brunner J, Moody J, Ibarra L, Hoyt H, et al. 2016. Factors Affecting Implementation of the California Childhood Obesity Research Demonstration (CA-CORD) Project, 2013. Prev Chronic Dis 13: E147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colberg SR, Sigal RJ, Yardley JE, Riddell MC, Dunstan DW, et al. 2016. Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care 39: 2065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuthbertson DJ, Brown E, Koskinen J, Magnussen CG, Hutri-Kähönen N, et al. 2018. Longitudinal analysis of risk of non-alcoholic fatty liver disease in adulthood. Liver International 0 [DOI] [PubMed] [Google Scholar]
- Davis MM, Gance-Cleveland B, Hassink S, Johnson R, Paradis G, Resnicow K. 2007. Recommendations for prevention of childhood obesity. Pediatrics 120: S229–S53 [DOI] [PubMed] [Google Scholar]
- Davison KK, Birch LL. 2001. Childhood overweight: A contextual model and recommendations for future research. Obesity Reviews 2: 159–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dearing JW, Smith DK, Larson RS, Estabrooks CA. 2013. Designing for Diffusion of a Biomedical Intervention. American Journal of Preventive Medicine 44: S70–S76 [DOI] [PubMed] [Google Scholar]
- DeSalvo KB, Olson R, Casavale KO. 2016. Dietary Guidelines for AmericansDietary Guidelines for AmericansDietary Guidelines for Americans. JAMA 315: 457–58 [DOI] [PubMed] [Google Scholar]
- Dishion TJ, Shaw DS, Connell A, Gardner FEM, Weaver C, Wilson M. 2008. The Family Check-Up with high-risk indigent families: Preventing problem behavior by increasing parents' positive behavior support in early childhood. Child Development 79: 1395–414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dooyema CA, Belay B, Blanck HM. 2017. Implementation of Multisetting Interventions to Address Childhood Obesity in Diverse, Lower-Income Communities: CDC's Childhood Obesity Research Demonstration Projects. Prev Chronic Dis 14: E140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn W, Schwimmer J. 2008. The obesity epidemic and nonalcoholic fatty liver disease in children. Curr Gastroenterol Rep 10: 67–72 [DOI] [PubMed] [Google Scholar]
- Economos CD, Hammond RA. 2017. Designing effective and sustainable multifaceted interventions for obesity prevention and healthy communities. Obesity 25: 1155–56 [DOI] [PubMed] [Google Scholar]
- Fagg J, Cole TJ, Cummins S, Goldstein H, Morris S, et al. 2015. After the RCT: who comes to a family-based intervention for childhood overweight or obesity when it is implemented at scale in the community? Journal of Epidemiology and Community Health 69: 142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falkner B, Gidding SS, Ramirez-Garnica G, Wiltrout SA, West D, Rappaport EB. 2006. The relationship of body mass index and blood pressure in primary care pediatric patients. J Pediatr 148: 195–200 [DOI] [PubMed] [Google Scholar]
- Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, et al. 2017. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics 140: e20171904. [DOI] [PubMed] [Google Scholar]
- Friedemann C, Heneghan C, Mahtani K, Thompson M, Perera R, Ward AM. 2012. Cardiovascular disease risk in healthy children and its association with body mass index: systematic review and meta-analysis. BMJ : British Medical Journal 345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganter C, Aftosmes-Tobio A, Chuang E, Kwass JA, Land T, Davison KK. 2017. Lessons Learned by Community Stakeholders in the Massachusetts Childhood Obesity Research Demonstration (MA-CORD) Project, 2013-2014. Prev Chronic Dis 14: E08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Muniesa P, Martinez-Gonzalez MA, Hu FB, Despres JP, Matsuzawa Y, et al. 2017. Obesity. Nature reviews. Disease primers 3: 17034. [DOI] [PubMed] [Google Scholar]
- Graziano PA, Kelleher R, Calkins SD, Keane SP, Brien MO. 2013. Predicting weight outcomes in preadolescence: the role of toddlers' self-regulation skills and the temperament dimension of pleasure. International journal of obesity (2005) 37: 937–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale L, Guan S. 2015. Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep medicine reviews 21: 50–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hales CM, Fryar CD, Carroll MD, Freedman DS, Ogden CL. 2018. Trends in obesity and severe obesity prevalence in us youth and adults by sex and age, 2007-2008 to 2015-2016. JAMA 319: 1723–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton D, Dee A, Perry IJ. 2018. The lifetime costs of overweight and obesity in childhood and adolescence: a systematic review. Obesity Reviews 19: 452–63 [DOI] [PubMed] [Google Scholar]
- Hardy LL, Mihrshahi S, Gale J, Nguyen B, Baur LA, O’Hara BJ. 2015. Translational research: are community-based child obesity treatment programs scalable? BMC Public Health 15: 652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison K, Bost KK, McBride BA, Donovan SM, Grigsby-Toussaint DS, et al. 2011. Toward a developmental conceptualization of contributors to overweight and obesity in childhood: The Six-Cs model. Child Development Perspectives 5: 50–58 [Google Scholar]
- Hays SM, McGinnis C. 2018. Nonalcoholic Fatty Liver Disease in Children: Beyond Metabolic Syndrome. The Journal for Nurse Practitioners 14: 725–31 [Google Scholar]
- He J, Cai Z, Fan X. 2017. Prevalence of binge and loss of control eating among children and adolescents with overweight and obesity: An exploratory meta-analysis. Int J Eat Disord 50: 91–103 [DOI] [PubMed] [Google Scholar]
- Hoare E, Skouteris H, Fuller-Tyszkiewicz M, Millar L, Allender S. 2014. Associations between obesogenic risk factors and depression among adolescents: a systematic review. Obesity Reviews 15: 40–51 [DOI] [PubMed] [Google Scholar]
- Hoffman J, Frerichs L, Story M, Jones J, Gaskin K, et al. 2018. An Integrated Clinic-Community Partnership for Child Obesity Treatment: A Randomized Pilot Trial. Pediatrics 141: e20171444. [DOI] [PubMed] [Google Scholar]
- Hope S, Micali N, Deighton J, Law C. 2019. Maternal mental health at 5 years and childhood overweight or obesity at 11 years: evidence from the UK Millennium Cohort Study. International Journal of Obesity 43: 43–52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ickes MJ, McMullen J, Haider T, Sharma M. 2014. Global school-based childhood obesity interventions: a review. Int J Environ Res Public Health 11: 8940–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irish LA, Kline CE, Gunn HE, Buysse DJ, Hall MH. 2015. The role of sleep hygiene in promoting public health: A review of empirical evidence. Sleep Medicine Reviews 22: 23–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isasi CR, Hua S, Jung M, Carnethon MR, Perreira K, et al. 2017. The Association of Parental/Caregiver Chronic Stress with Youth Obesity: Findings from the Study of Latino Youth and the Hispanic Community Health Study/Study of Latinos Sociocultural Ancillary Study. Childhood obesity (Print) 13: 251–58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janicke DM, Harman JS, Kelleher KJ, Zhang J. 2009a. The Association of Psychiatric Diagnoses, Health Service Use, and Expenditures in Children with Obesity-related Health Conditions. Journal of Pediatric Psychology 34: 79–88 [DOI] [PubMed] [Google Scholar]
- Janicke DM, Sallinen BJ, Perri MG, Lutes LD, Silverstein JH, Brumback B. 2009b. Comparison of Program Costs for Parent-Only and Family-Based Interventions for Pediatric Obesity in Medically Underserved Rural Settings. The Journal of Rural Health 25: 326–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janicke DM, Steele RG, Gayes LA, Lim CS, Clifford LM, et al. 2014. Systematic review and meta-analysis of comprehensive behavioral family lifestyle interventions addressing pediatric obesity. Journal of Pediatric Psychology [DOI] [PubMed] [Google Scholar]
- Jordan N, Graham AK, Berkel C, Smith JD. 2019. Budget impact analysis of preparing to implement the Family Check-Up 4 Health in primary care to reduce pediatric obesity. Prevention Science 20: 655–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kakinami L, Houle-Johnson SA, Demissie Z, Santosa S, Fulton JE. 2019. Meeting fruit and vegetable consumption and physical activity recommendations among adolescents intending to lose weight. Preventive Medicine Reports 13: 11–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karacabeyli D, Allender S, Pinkney S, Amed S. 2018. Evaluation of complex community-based childhood obesity prevention interventions. Obes Rev 19: 1080–92 [DOI] [PubMed] [Google Scholar]
- Kelly AS, Fox CK. 2018. Role of Pharmacotherapy in the Treatment of Pediatric Obesity and Its Comorbidities In Pediatric Obesity: Etiology, Pathogenesis and Treatment, ed. Freemark MS, pp. 613–27. Cham: Springer International Publishing [Google Scholar]
- Khambalia AZ, Dickinson S, Hardy LL, Gill T, Baur LA. 2012. A synthesis of existing systematic reviews and meta-analyses of school-based behavioural interventions for controlling and preventing obesity. Obes Rev 13: 214–33 [DOI] [PubMed] [Google Scholar]
- Kothandan SK. 2014. School based interventions versus family based interventions in the treatment of childhood obesity- a systematic review. Archives of public health = Archives belges de sante publique 72: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar S, Kelly AS. 2017. Review of Childhood Obesity: From Epidemiology, Etiology, and Comorbidities to Clinical Assessment and Treatment. Mayo Clinic Proceedings 92: 251–65 [DOI] [PubMed] [Google Scholar]
- Kyle TK, Dhurandhar EJ, Allison DB. 2016. Regarding Obesity as a Disease: Evolving Policies and Their Implications. Endocrinology and metabolism clinics of North America 45: 511–20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landsverk J, Brown CH, Smith JD, Chamberlain P, Palinkas LA, et al. 2017. Design and analysis in dissemination and implementation research In Dissemination and implementation research in health: Translating research to practice, ed. Brownson RC, Colditz GA, Proctor EK, pp. 201–27. New York: Oxford University Press [Google Scholar]
- Lang JE, Fitzpatrick AM, Mauger DT, Guilbert TW, Jackson DJ, et al. 2018. Overweight/obesity status in preschool children associates with worse asthma but robust improvement on inhaled corticosteroids. Journal of Allergy and Clinical Immunology 141: 1459–67.e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang JE, Hossain MJ, Lima JJ. 2015. Overweight children report qualitatively distinct asthma symptoms: analysis of validated symptom measures. The Journal of allergy and clinical immunology 135: 886–93.e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebow J, Sim LA, Kransdorf LN. 2015. Prevalence of a History of Overweight and Obesity in Adolescents With Restrictive Eating Disorders. Journal of Adolescent Health 56: 19–24 [DOI] [PubMed] [Google Scholar]
- Leppert B, Junge KM, Röder S, Borte M, Stangl GI, et al. 2018. Early maternal perceived stress and children’s BMI: longitudinal impact and influencing factors. BMC Public Health 18: 1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ling J, Robbins LB, Wen F. 2016. Interventions to prevent and manage overweight or obesity in preschool children: A systematic review. International Journal of Nursing Studies 53: 270–89 [DOI] [PubMed] [Google Scholar]
- Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, et al. 2010. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic impact goal through 2020 and beyond. Circulation 121: 586–613 [DOI] [PubMed] [Google Scholar]
- Ludwig DS. 2016. Lifespan Weighed Down by DietDiet and Decreasing LifespanDiet and Decreasing Lifespan. JAMA 315: 2269–70 [DOI] [PubMed] [Google Scholar]
- Lydecker JA, Grilo CM. 2016. The apple of their eye: Attitudinal and behavioral correlates of parents’ perceptions of child obesity. Obesity 24: 1124–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lydecker JA, O’Brien E, Grilo CM. 2018. Parents have both implicit and explicit biases against children with obesity. Journal of Behavioral Medicine 41: 784–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchesini G, Petta S, Dale Grave R. 2015. Diet, Weight Loss, and Liver Health in NAFLD: Pathophysiology, Evidence and Practice. Hepatology [DOI] [PubMed]
- Marshall SA, Ip EH, Suerken CK, Arcury TA, Saldana S, et al. 2018. Relationship between maternal depression symptoms and child weight outcomes in Latino farmworker families. Maternal & Child Nutrition 14: e12614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May AL, Kuklina EV, Yoon PW. 2012. Prevalence of cardiovascular disease risk factors among us adolescents, 1999–2008. Pediatrics 129: 1035–41 [DOI] [PubMed] [Google Scholar]
- McCrabb S, Lane C, Hall A, Milat A, Bauman A, et al. 2019. Scaling-up evidence-based obesity interventions: A systematic review assessing intervention adaptations and effectiveness and quantifying the scale-up penalty. Obesity Reviews 20: 964–82 [DOI] [PubMed] [Google Scholar]
- McNulty M, Smith JD, Villamar J, Burnett-Zeigler I, Vermeer W, et al. 2019. Implementation Research Methodologies for Achieving Scientific Equity and Health Equity. In Ethnicity & disease, pp. 83–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalsky M, Reichard K, Inge T, Pratt J, Lenders C. 2012. ASMBS pediatric committee best practice guidelines. Surgery for obesity and related diseases : official journal of the American Society for Bariatric Surgery 8: 1–7 [DOI] [PubMed] [Google Scholar]
- Milaneschi Y, Simmons WK, van Rossum EFC, Penninx BWJH. 2019. Depression and obesity: evidence of shared biological mechanisms. Molecular Psychiatry 24: 18–33 [DOI] [PubMed] [Google Scholar]
- Miller AL, Lumeng JC, LeBourgeois MK. 2015. Sleep patterns and obesity in childhood. Current Opinion in Endocrinology Diabetes and Obesity 22: 41–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell TB, Amaro CM, Steele RG. 2016. Pediatric Weight Management Interventions in Primary Care Settings: A Meta-Analysis. Health Psychol [DOI] [PubMed]
- Mühlig Y, Antel J, Föcker M, Hebebrand J. 2016. Are bidirectional associations of obesity and depression already apparent in childhood and adolescence as based on high-quality studies? A systematic review. Obesity Reviews 17: 235–49 [DOI] [PubMed] [Google Scholar]
- Narang I, Mathew JL. 2012. Childhood obesity and obstructive sleep apnea. J Nutr Metab 2012: 134202–02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Natale RA, Messiah SE, Asfour LS, Uhlhorn SB, Englebert NE, Arheart KL. 2017. Obesity Prevention Program in Childcare Centers: Two-Year Follow-Up. American journal of health promotion : AJHP 31: 502–10 [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. 2019. National Asthma Data (2017 National Health Interview Survey), Centers for Disease Control and Prevention [Google Scholar]
- Ng M, Fleming T, Robinson M, Thomson B, Graetz N, et al. 2014. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet 384: 766–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nobili V, Alkhouri N, Alisi A, Della Court C, Fitzpatrick E, et al. 2015. Nonalcoholic fatty liver disease: A challenge for pediatricians. JAMA Pediatrics 169: 170–76 [DOI] [PubMed] [Google Scholar]
- O'Connor SG, Maher JP, Belcher BR, Leventhal AM, Margolin G, et al. 2017. Associations of maternal stress with children's weight-related behaviours: a systematic literature review. Obesity Reviews 18: 514–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor EA, Evans CV, Burda BU, Walsh ES, Eder M, Lozano P. 2017. Screening for Obesity and Intervention for Weight Management in Children and Adolescents: Evidence Report and Systematic Review for the US Preventive Services Task ForceUSPSTF Evidence Report: Screening for Obesity in Children and YouthUSPSTF Evidence Report: Screening for Obesity in Children and Youth. JAMA 317: 2427–44 [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Fakhouri TH, Hales CM, Fryar CD, et al. 2018. Prevalence of obesity among youths by household income and education level of head of household—United States 2011–2014. Morbidity and Mortality Weekly Report 67: 186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paruthi S, Brooks LJ, D'Ambrosio C, Hall WA, Kotagal S, et al. 2016. Recommended Amount of Sleep for Pediatric Populations: A Consensus Statement of the American Academy of Sleep Medicine. J Clin Sleep Med 12: 785–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peirson L, Fitzpatrick-Lewis D, Morrison K, Ciliska D, Kenny M, et al. 2015a. Prevention of overweight and obesity in children and youth: a systematic review and meta-analysis. CMAJ open 3: E23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peirson L, Fitzpatrick-Lewis D, Morrison K, Warren R, Usman Ali M, Raina P. 2015b. Treatment of overweight and obesity in children and youth: a systematic review and meta-analysis. CMAJ open 3: E35–E46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, et al. 2018. The Physical Activity Guidelines for AmericansPhysical Activity Guidelines for AmericansPhysical Activity Guidelines for Americans. JAMA 320: 2020–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pont SJ, Puhl R, Cook SR, Slusser W. 2017. Stigma Experienced by Children and Adolescents With Obesity. Pediatrics 140: e20173034. [DOI] [PubMed] [Google Scholar]
- Pratt KJ, Skelton JA. 2018. Family Functioning and Childhood Obesity Treatment: a Family Systems Theory-Informed Approach. Academic Pediatrics [DOI] [PMC free article] [PubMed]
- Proctor E, Powell BJ, McMillen JC. 2013. Implementation strategies: recommendations for specifying and reporting. Implement Sci 8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulgaron ER, Delamater AM. 2014. Obesity and type 2 diabetes in children: epidemiology and treatment. Current diabetes reports 14: 508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson TN, Banda JA, Hale L, Lu AS, Fleming-Milici F, et al. 2017. Screen Media Exposure and Obesity in Children and Adolescents. Pediatrics 140: S97–S101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rupp K, McCoy SM. 2019. Bullying Perpetration and Victimization among Adolescents with Overweight and Obesity in a Nationally Representative Sample. Childhood Obesity [DOI] [PMC free article] [PubMed]
- Russell CG, Russell A. 2019. A biopsychosocial approach to processes and pathways in the development of overweight and obesity in childhood: Insights from developmental theory and research. Obesity Reviews 20: 725–49 [DOI] [PubMed] [Google Scholar]
- Savage JS, Birch LL. 2017. WIC mothers' depressive symptoms are associated with greater use of feeding to soothe, regardless of perceived child negativity. Pediatr Obes 12: 155–62 [DOI] [PubMed] [Google Scholar]
- Schlam TR, Wilson NL, Shoda Y, Mischel W, Ayduk O. 2013. Preschoolers' delay of gratification predicts their body mass 30 years later. J Pediatr 162: 90–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shankardass K, McConnell R, Jerrett M, Lam C, Wolch J, et al. 2014. Parental stress increases body mass index trajectory in pre-adolescents. Pediatr Obes 9: 435–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shatat IF, Brady TM. 2018. Editorial: Pediatric Hypertension: Update. Frontiers in Pediatrics 6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheinbein DH, Stein RI, Hayes JF, Brown ML, Balantekin KN, et al. 2019. Factors associated with depression and anxiety symptoms among children seeking treatment for obesity: A social-ecological approach. Pediatr Obes: e12518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shloim N, Edelson LR, Martin N, Hetherington MM. 2015. Parenting Styles, Feeding Styles, Feeding Practices, and Weight Status in 4-12 Year-Old Children: A Systematic Review of the Literature. Front Psychol 6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmonds M, Llewellyn A, Owen CG, Woolacott N. 2016. Predicting adult obesity from childhood obesity: a systematic review and meta-analysis. Obesity Reviews 17: 95–107 [DOI] [PubMed] [Google Scholar]
- Sisson SB, Krampe M, Anundson K, Castle S. 2016. Obesity prevention and obesogenic behavior interventions in child care: A systematic review. Preventive Medicine 87: 57–69 [DOI] [PubMed] [Google Scholar]
- Skinner AC, Perrin EM, Moss LA, Skelton JA. 2015. Cardiometabolic Risks and Severity of Obesity in Children and Young Adults. New England Journal of Medicine 373: 1307–17 [DOI] [PubMed] [Google Scholar]
- Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. 2018. Prevalence of Obesity and Severe Obesity in US Children, 1999–2016. Pediatrics 141: e20173459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sleddens EFC, Gerards SMPL, Thijs C, de Vries NK, Kremers SPJ. 2011. General parenting, childhood overweight and obesity-inducing behaviors: A review. International Journal of Pediatric Obesity 6: e12–e27 [DOI] [PubMed] [Google Scholar]
- Smith JD, Berkel C, Jordan N, Atkins DC, Narayanan SS, et al. 2018a. An individually tailored family-centered intervention for pediatric obesity in primary care: Study protocol of a randomized type II hybrid implementation-effectiveness trial (Raising Healthy Children study). Implementation Science 13: 1–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JD, Berkel C, Rudo-Stern J, Montaño Z, St George SM, et al. 2018b. The Family Check-Up 4 Health (FCU4Health): Applying implementation science frameworks to the process of adapting an evidence-based parenting program for prevention of pediatric obesity and excess weight gain in primary care. Frontiers in public health 6: 293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JD, Berkel C, Rudo-Stern J, Montaño Z, St. George SM, et al. 2018c. The Family Check-Up 4 Health (FCU4Health): Applying implementation science frameworks to the process of adapting an evidence-based parenting program for prevention of pediatric obesity and excess weight gain in primary care. Frontiers in Public Health [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JD, Egan KN, Montaño Z, Dawson-McClure S, Jake-Schoffman DE, et al. 2018d. A developmental cascade perspective of paediatric obesity: Conceptual model and scoping review. Health Psychology Review 12: 271–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JD, Montaño Z, Dishion TJ, Shaw DS, Wilson MN. 2015. Preventing weight gain and obesity: Indirect effects of a family-based intervention in early childhood. Prevention Science 16: 408–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JD, Montaño Z, Maynard A, Miloh T. 2017a. Family Functioning Predicts Body Mass Index and Biochemical Levels of Youths with Nonalcoholic Fatty Liver Disease. Journal of Developmental & Behavioral Pediatrics 38: 155–60 [DOI] [PubMed] [Google Scholar]
- Smith JD, St. George SM, Prado G. 2017b. Family-centered positive behavior support interventions in early childhood to prevent obesity. Child Development 88: 427–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommer A, Twig G. 2018. The Impact of Childhood and Adolescent Obesity on Cardiovascular Risk in Adulthood: a Systematic Review. Curr Diab Rep 18: 91. [DOI] [PubMed] [Google Scholar]
- Sonneville KR, Grilo CM, Richmond TK, Thurston IB, Jernigan M, et al. 2015. Prospective association between overvaluation of weight and binge eating among overweight adolescent girls. The Journal of adolescent health : official publication of the Society for Adolescent Medicine 56: 25–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- St. George SM, Agosto Y, Rojas L, Soares M, Bahamon M, et al. in press. A developmental cascade perspective of pediatric obesity: A systematic review of preventive interventions from infancy through late adolescence. Obesity Reviews [DOI] [PMC free article] [PubMed]
- Stevens SD, Herbozo S, Morrell HE, Schaefer LM, Thompson JK. 2017. Adult and childhood weight influence body image and depression through weight stigmatization. Journal of health psychology 22: 1084–93 [DOI] [PubMed] [Google Scholar]
- Stout SA, Espel EV, Sandman CA, Glynn LM, Davis EP. 2015. Fetal programming of children's obesity risk. Psychoneuroendocrinology 53: 29–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung-Chan P, Sung YW, Zhao X, Brownson RC. 2013. Family-based models for childhood-obesity intervention: A systematic review of randomized controlled trials. Obesity Reviews 14: 265–78 [DOI] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Cohen ML, Yanovski SZ, Cox C, Theim KR, et al. 2006. A Prospective Study of Psychological Predictors of Body Fat Gain Among Children at High Risk for Adult Obesity. Pediatrics 117: 1203–09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tate EB, Wood W, Liao Y, Dunton GF. 2015. Do stressed mothers have heavier children? A meta-analysis on the relationship between maternal stress and child body mass index. Obesity reviews : an official journal of the International Association for the Study of Obesity 16: 351–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taveras EM, Gillman MW, Peña M-M, Redline S, Rifas-Shiman SL. 2014. Chronic Sleep Curtailment and Adiposity. Pediatrics 133: 1013–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor JH, Xu Y, Li F, Shaw M, Dziura J, et al. 2017. Psychosocial predictors and moderators of weight management programme outcomes in ethnically diverse obese youth. Pediatric Obesity 12: 453–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor RW, Cox A, Knight L, Brown DA, Meredith-Jones K, et al. 2015. A Tailored Family-Based Obesity Intervention: A Randomized Trial. Pediatrics 136: 281. [DOI] [PubMed] [Google Scholar]
- Tomiyama AJ, Finch LE, Belsky ACI, Buss J, Finley C, et al. 2015. Weight bias in 2001 versus 2013: Contradictory attitudes among obesity researchers and health professionals. Obesity 23: 46–53 [DOI] [PubMed] [Google Scholar]
- US Preventive Services Task Force. 2017. Screening for Obesity in Children and Adolescents: US Preventive Services Task Force Recommendation Statement. JAMA 317: 2417–26 [DOI] [PubMed] [Google Scholar]
- Vehmeijer FOL CV Silva C, Derks IPM, El Marroun H, Oei EHG, et al. 2019. Associations of Maternal Psychological Distress during Pregnancy with Childhood General and Organ Fat Measures. Childhood Obesity [DOI] [PubMed] [Google Scholar]
- Wang Y, Cai L, Wu Y, Wilson RF, Weston C, et al. 2015. What childhood obesity prevention programmes work? A systematic review and meta-analysis. Obesity Reviews 16: 547–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward DS, Welker E, Choate A, Henderson KE, Lott M, et al. 2017. Strength of obesity prevention interventions in early care and education settings: A systematic review. Preventive Medicine 95: S37–S52 [DOI] [PubMed] [Google Scholar]
- Warnakulasuriya LS, Fernando MMA, Adikaram AVN, Thawfeek ARM, Anurasiri WL, et al. 2018. Metformin in the Management of Childhood Obesity: A Randomized Control Trial. Childhood obesity (Print) 14: 553–65 [DOI] [PubMed] [Google Scholar]
- Wen M, Simpson JM, Baur LA, Rissel C, Flood VM. 2011. Family functioning and obesity risk behaviors: Implications for early obesity intervention. Obesity 19: 1252–58 [DOI] [PubMed] [Google Scholar]
- Whitlock EP, O'Connor EA, Williams SB, Beil TL, Lutz KW. 2010. Effectiveness of weight management interventions in children: A targeted systematic review for the USPSTF. Pediatrics 125: e396–e418 [DOI] [PubMed] [Google Scholar]
- Wuhl E 2019. Hypertension in childhood obesity. Acta paediatrica (Oslo, Norway : 1992) 108: 37–43 [DOI] [PubMed] [Google Scholar]
- Yackobovitch-Gavan M, Wolf Linhard D, Nagelberg N, Poraz I, Shalitin S, et al. 2018. Intervention for childhood obesity based on parents only or parents and child compared with follow-up alone. Pediatric Obesity 13: 647–55 [DOI] [PubMed] [Google Scholar]


