Abstract
Aims
To translate evidence-based programs (EBP) for a new setting, attention must be given to the characteristics of the intervention and the local setting, as well as evidence that is compelling to decision makers. This paper describes the history of a partnership and stakeholder recommendations to inform the adaptation of an EBP for primary care.
Methods
We established a community advisory board (CAB) consisting of stakeholders with expertise in primary care delivery. A thematic analysis was conducted with fieldnotes and transcriptions from CAB meetings and regular meetings with participating clinics.
Results
We found that 1) parenting programs with a focus on behavioral and physical health are appropriate for this setting, 2) variability in the structure of primary care means implementation must be tailorable, and 3) financial and organizational outcomes are compelling for decision makers.
Conclusion
Factors related to the content and structure of evidence-based programs are uniquely related to distinct implementation outcomes of interest to key stakeholders.
Keywords: Implementation Science, Primary Health Care, Parenting, Pediatric Obesity, Organizational Decision Making, Health Services Research, Integrated Delivery of Health Care
Introduction
Decades of research support the efficacy of parenting programs in preventing a wide array of child behavioral health problems (O’Connell, Boat, & Warner, 2009; Sandler, Ingram, Wolchik, & Winslow, 2015; Van Ryzin, 2016). In the formative years of prevention science, however, programs were designed to maximize potential efficacy, and little attention was given to whether they could be implemented by regular service delivery settings (Institute of Medicine & National Research Council, 2014). Consequently, uptake by providers, access for families, and public health impact have all been limited (Spoth et al., 2013). There is growing interest in primary care as a service delivery system in which to embed evidence-based parenting programs (Leslie et al., 2016; Perrin, Leslie, & Boat, 2016). Leslie and colleagues identified three barriers to the implementation of parenting programs, which may be solved by primary care. First, stigma currently associated with parenting programs may be reduced by including services as part of regular well-checks. Second, there is no universally recognized service home for family-based prevention; primary pediatric care might fulfill this role. Third, there is no current funding system in place for family-based prevention; however, given the potential effects on a range of health issues, it is possible that Medicaid or private healthplans would be willing to provide a sustainable funding stream. The reach of primary care is also advantageous: 98% of US children ages 5–11 have a primary care provider and 93% have had a visit in the past year (Bloom, Jones, & Freeman, 2013). Other relative advantages of primary care over other potential delivery settings (e.g., schools) include routine caregiver involvement in primary care visits, the trust for pediatricians, and longitudinal contact with the same pediatrician or pediatric practice over time.
While primary care has tremendous potential, Leslie and colleagues’ (2016) review shows that the effects of evidence-based programs delivered in primary care (e.g., Incredible Years, Triple P, PCIT) have been mixed and that sustainability has been limited. Moreover, a recent review of research on parenting programs in primary care showed scant attention to implementation process and outcomes in favor of an almost exclusive focus on effectiveness (Smith et al., 2019).
Glasgow and Emmons (2007) created a typology of factors that must be addressed by translational research to improve the uptake of evidence-based programs. This model focuses on interactions between characteristics of the setting (e.g., needs of the clients, competing demands on the staff, financial and organizational stability), the intervention (e.g., cost, customizability, manualization), and its research evidence (e.g., whether it can be delivered and works in this setting, with this population, when delivered by this type of provider). Because it focuses not just on characteristics of each of these domains (i.e., setting, intervention, and evidence), but the intersection of these characteristics, the Glasgow and Emmons’ framework was helpful in our planning process as we attempted to adapt the program to fit within this setting and design the evaluation to provide useful information to local decision makers.
In the sections that follow, we describe a community-academic research partnership to understand these factors within the context of a hybrid effectiveness-implementation trial (Curran, Bauer, Mittman, Pyne, & Stetler, 2012) of the Family Check-Up 4 Health (FCU4Health) within pediatric primary care (Smith, Berkel, Jordan, et al., 2018). Because understanding the self-interests of relevant stakeholders is a critical element of forming and sustaining partnerships (Carney, Maltby, Mackin, & Maksym, 2011; Kellam, 2012), we begin by explaining the history of our collaborations with primary care clinics with a focus on our partners’ motivation for collaboration. Next, we present lessons learned from engaging our partners in this project with respect to Glasgow and Emmons’ framework for translational research. Finally, we highlight the implications for our findings with respect to the potential impact on distinct implementation outcomes as defined by Proctor and colleagues (2011).
History of the Partnership and Partner Motivation
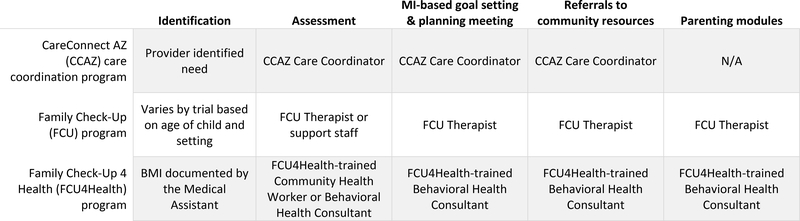
Three main factors played an important role in the development of the partnership: 1) a service gap identified by a large care coordination program; 2) collateral effects of an evidence-based behavioral health program on physical health outcomes, and 3) the movement toward the integration of behavioral health and primary care. This section describes these dynamics with respect to the motivation of our partners. In 2010, Phoenix Children’s Hospital’s (PCH) General Pediatrics (GenPeds) clinic, had a care coordination program supported by state tobacco tax funding (Beaumont, Berkel, Tovar-Huffman, & Shaw, 2011; Berkel et al., 2015). The program, called CareConnect AZ, was adapted from the Bridges for Newborns program (Rose, Coombs, Schwartz, & Clark, 2007). It included a comprehensive assessment to guide services and made use of Motivational Interviewing (Miller & Rollnick, 2002) to connect families with community resources (see Figure 1). Families were identified at PCH or partnering clinics and consisted primarily of ethnic minority (two-thirds Latino), low-income families with multiple health and social concerns. Care coordinators in the program noted that parenting challenges frequently interfered with child health, and they struggled with the lack of availability of evidence-based parenting programs in the community. Pediatricians in GenPeds echoed this frustration. We conducted an anonymous survey with 20 pediatricians who cited parenting and behavioral health as their second highest concerns for their patient population (each endorsed by 95%), after obesity/nutrition (endorsed by 100%) (Berkel et al., 2016). All of the respondents endorsed the need to embed evidence-based parenting programs into the clinic, as supported by this comment:
I feel that we often don’t have enough time during sick visits or even well checks to fully address these issues and it could be so beneficial to have a parenting program to ensure that we are fully meeting the needs of our patients.
Figure 1.
A structural comparison of the CareConnect AZ care coordination program, the original Family Check-Up program, and the adapted Family Check-Up 4 Health program
The original Family Check-Up (FCU; Dishion & Stormshak, 2007) was identified by the CareConnect AZ team as a potential strategy to fill this gap. The FCU is an evidence-based parenting program that uses a tailored approach to address child behavior problems and adolescent substance use. Much like CareConnect AZ, FCU includes a comprehensive assessment to guide services, motivational approaches to engage families, and connections with community resources (see Figure 1). From the care coordinators’ perspective, the benefit of adopting the FCU was the accompanying parent training curriculum, Everyday Parenting (EDP; Dishion, Stormshak, & Kavanagh, 2011). EDP includes 12 modules addressing three domains of parenting—relationship quality, positive behavior support, and monitoring and limit setting—and uses a modularized approach that allows providers to offer only those modules of the curriculum that address a family’s specific needs. These domains map onto measures in the assessment, and the scores are then shared with families. If the families express interest in working on these domains, the program provider will offer the corresponding EDP sessions. Care coordinators found this individually-tailorable approach to be particularly appropriate for the clinic because it 1) quickly addresses the most pressing needs, 2) increases family satisfaction and engagement, and 3) may be more feasible and cost-efficient to deliver, because it is a brief and targeted intervention.
Although the FCU was originally designed to target behavior problems and substance use, collateral effects on health behaviors and pediatric obesity have been identified (Smith, Montano, Dishion, Shaw, & Wilson, 2015; Van Ryzin & Nowicka, 2013). The positive parent-child relationships and discipline strategies targeted by the FCU to influence child behavior problems are also associated with physical health behaviors (Smith, Egan, et al., 2018). Given the effects on both behavioral and physical health, GenPeds and PCH’s nonalcoholic fatty liver disease clinic agreed to participate in pilot trials of the FCU, and these trials provided preliminary evidence of acceptability, appropriateness, and potential feasibility with structural adaptations (Chiapa et al., 2014; Rudo-Stern et al., 2014).
We were subsequently awarded funding from the Centers for Disease Control & Prevention through the Childhood Obesity Research Demonstration (CORD) 2.0 program (2015) to adapt the FCU for primary care, test the impact of the adapted program on the prevention of excess weight gain among children with elevated BMI, and study factors related to the implementation in different primary care settings. Because we were interested in learning about how a tailored parenting program would fit into a variety of integrated primary care settings, we engaged four Federally Qualified Health Centers (FQHCs) in the local area to our ongoing partnership with GenPeds at PCH. FQHCs by nature have integrated behavioral health and primary care, but their level of integration can fall on a continuum from coordinated care, in which referrals are made between separate physical locations, to co-located care, in which primary care and behavioral health providers work within the same physical space but function independently, to fully integrated care, in which various types of providers work together as a team (Heath, Wise Romero, & Reynolds, 2013).
FQHC “A” began as a behavioral health organization and added primary care services. Their motivation to collaborate was driven by their interest in more fully integrating their pediatric primary care and behavioral health services. FQHC “B” had behavioral health consultants within their primary care clinic who worked closely with the pediatrician. Their interest was driven by the fact that they had no effective obesity prevention services to address the substantial rates of pediatric obesity experienced by their population. FQHCs A and B signed on to be clinic sites for the CORD 2.0 study and join our advisory board. FQHC “C” served primarily urban Native American families and was interested in increasing obesity services for this population. However, because of the research component, it was necessary to obtain IRB approval from the Indian Health Service, which proved to be infeasible given the short timeframe of the grant (just over two years). Finally, leadership at FQHC “D” was satisfied with its existing programs for children in the age range targeted by the grant (6–12 years) and elected not to participate. However, they partnered with us on a separate pilot of the program adapted for adolescents. Although FQHCs C and D did not participate as sites in the trial, representatives from both served on our advisory board for the duration of the study.
In the next section, we share lessons learned from our partnerships with members of our advisory board. These lessons pertain to 1) the adaptation of the FCU to promote child health behaviors in primary care and 2) the design of the study to ensure that the information garnered is useful for decision makers considering whether to support the adoption of the program. For context, we begin with a brief overview of the trial, then we describe the methods used to obtain input from our advisory board, and finally present lessons learned.
Methods
Trial Overview
In partnership with GenPeds and two FQHCs, we conducted a type 2 hybrid effectiveness-implementation trial (Curran, et al., 2012) to test the adapted FCU, named the Family Check-Up 4 Health (FCU4Health; Smith, Berkel, Jordan, et al., 2018; Smith, Berkel, Rudo-Stern, et al., 2018). Six- to 12-year-old patients with elevated body mass index (BMI) were identified in primary care. Participants were randomly assigned to the FCU4Health (N=141) or usual care (N=99). Services were provided in-clinic or through a referral model and included 1) an assessment at baseline, 3-months, and 6-months, 2) feedback sessions to set goals and plan follow-up services after each assessment, 3) parenting modules following the baseline and 3-month feedback tailored to family needs and interests, and 4) referrals to community resources as needed throughout the 6-month period. A follow-up assessment was completed at 12 months with no additional feedback session or other services.
Participants
The community advisory board (CAB) consisted of administrative and clinical staff from each study site and other interested FQHCs, a military wellness clinic, state government representatives from Medicaid and the Department of Health and Human Services, four healthplans, professional organizations including the Arizona chapter and the national office of the American Academy of Pediatrics, and researchers with expertise in pediatric obesity, health disparities, and family engagement. Caregivers were not included at this stage because the focus was on the primary care setting. However, their feedback was obtained during the two pilots at PCH prior to this study and we have since formed a caregiver advisory board consisting of caregivers who participated in the program.
Data Collection and Analysis
Data sources for the current study include transcriptions and field notes from CAB meetings and regular site meetings with participating clinics. Two CAB meetings (May and September 2016) were held prior to implementation launch (January 2017) to inform the adaptation and study design. Two additional meetings were held during implementation (September 2017, January 2019), and one was held immediately following the last data collection point (September 2019). Following recommendations from Kellam and colleagues (2012), our approach to CAB meetings encouraged participation based on mutual self-interests. Specifically, in each meeting, we presented our progress, asked for feedback, and then invited presentations by our partners about other related initiatives in the community. For the second CAB meeting, which occurred four months prior to our planned implementation launch, we held a full-day meeting with breakout groups to discuss issues related to characteristics of the intervention, the primary care setting, and the research design in accordance with Glasgow and Emmons’ (2007) framework. We also held regular meetings with the two FQHCs who would be delivering FCU4Health. They were held biweekly for the first six months of implementation (January – June 2017) and then monthly until the end of implementation. Meetings with the FQHCs included administrators (i.e., directors, supervisors, managers), as well as providers (i.e., behavioral health consultants, community health workers) as needed. Having both administrators and providers in attendance was useful to get multiple perspectives and achieve consensus. Finally, the study covered a portion of the salary of a GenPeds staff member to explain the study to residents and attending physicians and answer recruitment and eligibility questions as they arose. Field notes were taken in all meetings with study sites. In addition, all CAB meetings were recorded and transcribed. The first and second authors iteratively coded the data with thematic analysis using NVivo software. Elements of Glasgow and Emmons’ framework (i.e., intersections between the characteristics of the intervention and of the target setting, and types of evidence needed) were used as sensitizing concepts in the coding process (Bowen, 2006). Lower order codes were developed inductively and compiled into themes. Any disagreements were discussed until consensus was reached. To support the trustworthiness of the findings (Levitt, Motulsky, Wertz, Morrow, & Ponterotto, 2017), direct quotes are included as evidence of stakeholder perspectives and representatives of the advisory board are included as coauthors on the study.
Results
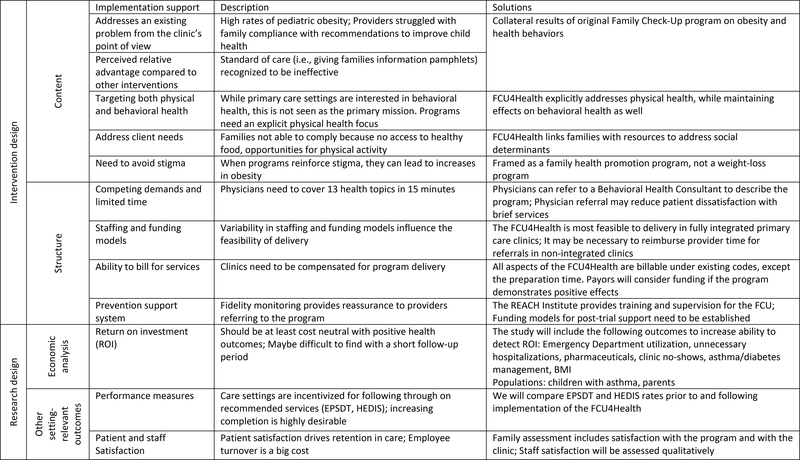
Findings from our stakeholders fit into two overarching themes: considerations for the intervention design and for the research design (see Figure 2). The intervention design theme was made up of two subthemes that address the intersection between the characteristics of the intervention and target setting. The first subtheme pertained to how the content of the intervention addresses unmet needs of the target setting. The second subtheme related to how well the structural components fit within the staffing and workflow of the target setting. The research design theme mapped squarely onto Glasgow and Emmons’ framework, and focused primarily on economic and organizational outcomes. In the following paragraphs, we share CAB insights and how we attempted to address them in the adaptation of the program and the design of the research. In addition, many CAB member suggestions linked factors related to the content, structure, and available evidence with distinct implementation outcomes. These are noted in the results and discussed further in the discussion.
Figure 2.
Key takeaways related to the intersections of setting, intervention, and research characteristics
Intervention Design: Addressing Content Needs
It was widely recognized among our CAB that prevailing approaches to address pediatric obesity have been ineffective. Prior to the submission of the grant proposal, GenPeds physicians described the cycle of typical interactions with families related to addressing BMI concerns. A patient is identified with elevated BMI during a well-check. The pediatrician provides the family with education and counseling related to established guidelines. The parent appears motivated and agrees to the recommended changes. Once at home, the parent realizes how difficult the changes are, due to issues like cost, time, and engrained habits. The family returns to the clinic for the next visit and the child’s BMI percentile has not changed, or perhaps it has increased. The pediatrician is frustrated with what is perceived as family non-compliance. The parent feels ashamed about not making the recommended changes and may not show up for the next appointment. The frustration with standard approaches was echoed in a conversation between two healthplan representatives and a clinic administrator during a CAB meeting:
1: “‘You are pre-diabetic, here take this booklet’ and you know that doesn’t help, and that is what is going on in many places. They don’t know how to do it; they don’t know what to do. They are not giving them that extra wrap-around service, like a dietician or a counselor, to find out where the barriers are. Don’t just give me a pill.”
2: “Or a pamphlet on how to eat better.”
1: “Yeah like, you need to exercise, and...”
3: “We do a lot of that, you know, education was dispensed, flyby outreach occurred and...”
1: “It was a copy of a copy of a copy.”
In a meeting with GenPeds residents about the program, we explained that the program was not meant to supplant the information that pediatricians give to patients, but to provide caregivers with the tools to implement pediatricians’ recommendations at home. In response, one GenPeds resident remarked, “every continuity clinic in the country would want something like that!”
CAB members emphasized the importance of addressing basic needs such as availability of nutritious food, spaces to play, and transportation to services. Community food banks often provide poor quality food, contributing to health disparities for low-income families.
“The Medicaid population in general has so many basic needs. Food being one of their highest needs, but it is difficult for them to be healthy when they are getting a food box full of bread or peanut butter.” (healthplan representative)
CAB members went on to note that when families are able to get fresh produce, it typically spoils because families do not know how to store and prepare it. The FCU4Health links families with community-based food distribution and preparation programs. However, as noted above, it was important to monitor the quality of the community-based programs. CAB members felt the resource system should include ratings of both the quality of the resource and their accessibility (e.g. cost, wait list) for families. One member suggested that if families were able to provide feedback on specific resources, it would promote their self-efficacy in using the system. It was acknowledged that a system like this would require substantial resources to build and maintain. There are also privacy and ethical issues to address. In the meantime, an online system was built so that FCU4Health coordinators could share information about resources, and families’ experiences with them, with each other.
A second concern noted by the CAB related to the content of the intervention was the need to avoid reinforcing weight-related stigma. Two members of the group had conducted research on the topic with 10- to 14-year-olds and found language that distances the condition from the individual was seen more positively. One shared:
“The usual sort of emotional laden words fat, heavy, huge, chubby those are really perceived negatively, so are obese and obesity. Things that are perceived more positively are BMI, unhealthy weight are a little more dispassionate, but also frame it in terms of overall health and pounds needed to be lost. If you say somebody is obese, is fat, is heavy, that’s a personal characteristic. But if you say they have weight they need to lose, it’s more distanced from the person. So, we’ve been really careful with what seems to track better, ‘Oh I need to lose some weight’ or ‘I could be more fit.’”
The FCU4Health is designed to focus on health, rather than weight loss. To avoid stigma, program content and materials never mentioned BMI or obesity. Instead, they focused on parenting and health behaviors, which have broad implications for all aspects of child physical and behavioral health. We made sure that referring providers understood this distinction to accurately explain the program to families. The comprehensive approach targeting both physical and behavioral health was perceived to be especially appropriate for integrated primary care:
“Now that you’ve added these health components, it’s not just another counseling intervention. Nothing against that, but this one is really focusing on health as well.” (behavioral health provider)
Due to its health focus and family-centered orientation, CAB members felt that the content of FCU4Health is appropriate for the primary care mission.
Intervention Design: Addressing Structural Needs
While primary care clinics have great potential for the delivery of evidence-based parenting programs, there are also challenges, particularly with respect to flow, staffing, and competing demands on time. Primary care pediatricians (PCPs) are expected to deliver screening and education on 13 domains of health in the span of a 15-minute visit (Hagan, Shaw, & Duncan, 2017). CAB members acknowledged that patients may be dissatisfied by this rapid pace. However, caregivers might attribute the positive experience of the FCU4Health to the PCP, which could redress possible patient dissatisfaction.
“I know patients get frustrated. The doctor has 26 patients to see that day so they are in and out and they might not feel like they can get close to the PCP. If the patient knew that PCP was recommending them, because they care about them, but even though the provider does not have the time to deliver all of this stuff, it is still initiated from their doctor so they might still feel that extra satisfaction with them.” (behavioral health supervisor)
The most dominant issue in this subtheme was the variability across clinic structures. Three types of clinics were represented among the CAB members: (1) small, private, free-standing primary care, (2) hospital-based outpatient primary care, and (3) FQHCs with integrated, co-located, or coordinated primary care and behavioral health. Each clinic type had different kinds and levels of support for implementing evidence-based parenting programs. The CAB agreed that providers in small, private clinics appear to have the most limited resources, with no access to behavioral health professionals, dietitians, or care coordinators. One private pediatrician stated that while she can bill for time, her clinic has been unsuccessful in getting reimbursed for specific behavioral health codes. Child and family team meetings may be reimbursable in private clinics; however, the requirement for the child to be present conflicts with most parent training models. It was also noted that care coordination codes, which should be available to cover one hour of service per month, per patient, are also inconsistently reimbursed. The complex, multipayer, fee-for-service reimbursement environment of a typical pediatric practice poses significant challenges to implementing a program like FCU4Health. Even referring to the program would overextend their resources given the amount of information they already need to squeeze into a 15- to 20-minute appointment.
Members of GenPeds, the hospital-based clinic, reported that residents and medical assistants could help with screening for eligibility and explain the program to families. However, since they had lost their service grant funding for care coordination, there is no role in the hospital-based clinic with time and the appropriate training to deliver FCU4Health. Consequently, we developed a model in which patients were identified and recruited in GenPeds, but referred to providers outside the hospital to receive services. One challenge in this approach is how to facilitate bidirectional communication between the FCU4Health provider and the pediatrician. We also found that pediatricians required reminders about the program. Three solutions were raised. First, they suggested an EHR-based trigger for referrals. Because of the short timeframe of the grant, the IT department was unable to program a trigger for this project. Second, they suggested including information about the study in the obesity toolkits housed in each exam room. The toolkit included handouts for parents about nutrition and physical activity (Rogers et al., 2013) and was given out when children were identified with elevated BMI. This strategy was feasible to implement, but because some families would be randomized to a control group, it was important not to overemphasize the program itself. Third, we found it was helpful to pre-screen the patients who might be eligible based on previous EHR data and notify providers at the morning huddle. Relatedly, providers asked that we reduce the eligibility criterion related to income. CORD 2.0 (Centers for Disease Control & Prevention, 2015) had an explicit goal that, if deemed effective, the program would become covered by Medicaid or Children’s Health Insurance Program (CHIP). For this reason, we initially set a requirement that families meet the income requirements for Medicaid or CHIP. The staff involved with recruitment found it awkward to ask about income in the clinic. Providers reported that if they have to remember eligibility requirements, they are less likely to refer. They also voiced frustration when families were just above the eligibility threshold. We were able to work with CDC first to relax the threshold, and then eliminate it altogether.
In contrast to the hospital-based clinic, FQHCs had many more resources for delivering a program like FCU4Health. They reported being able to bill for behavioral health, dietitians/nutritionists, and care coordination/case management. Multiple provider types (e.g., physicians, behavioral health coordinators, dietitians, psychology, social work) are able to meet and bill for an interdisciplinary meeting to support child health. Because each provider can be reimbursed for services, and the providers are co-located within the same organization, the clinic is highly incentivized to identify needs that may be addressed through internal referrals.
“We are billable providers within our clinic. So, our psychologists and our dieticians are encompassed in the provider. It’s really in the organization’s benefit for the medical provider to call a dietician in to the room, and so the medical provider is getting reimbursed for their visit and then I’m a whole other consult. On the same day, we will get reimbursed for my time. And then I identify a behavioral reason and I get my psychologist in, and it’s another reimbursement. With this kind of program, it would be very simple, we already do some things like this. The medical provider sees the BMI or health risks, calls us, we go in ” (dietician)
However, not all FQHCs have achieved this level of integration, and different decisions about where the intervention would sit led to unique challenges. One FQHC in the study chose to locate the intervention in their primary care clinic. The pediatrician identified patients and provided a warm hand-off to the behavioral health consultant located within primary care to inform patients about the study. A community health worker then conducted the FCU4Health assessment in the family’s home. Home-based assessments were more feasible for families and reduced burden on the clinic where space was at a premium. The behavioral health consultants were unable to provide services in the home because of billing and structural constraints. The length of FCU4Health feedback sessions was also a challenge. Feedback sessions could go for 1–2 hours in English, and longer in Spanish due to the reliance on interpreters, whereas regular contacts with behavioral health in the primary care clinic were limited to 30 minutes. Clinic administration made allowances for the extra time by categorizing the visits as specialty care, instead of primary care, which was possible because of the patient’s obesity diagnosis. However, the pediatricians still depended on the behavioral health consultants to be available throughout the day and were frustrated when they were tied up for extended periods of time.
The second FQHC elected to identify patients in primary care and refer them to the behavioral health side of the clinic, where the FCU4Health would be housed. They faced a number of challenges as well. First, the majority of their patients either accessed primary care or behavioral health, but not both. Patients in primary care had to first complete a comprehensive assessment to enroll in behavioral health, in addition to the FCU4Health’s assessment. For those in behavioral health only, BMI, which is an eligibility requirement for the study, is not routinely collected. This clinic chose to have the behavioral health consultants, rather than community health workers, complete assessments with families. Because of their very full caseloads, scheduling was difficult. If a patient no-showed, which occurred frequently, it was not customary for clinic staff to follow up and the family was essentially lost from the study.
Preparation time was an issue for both clinics. In the FCU4Health, providers review the results of the assessment prior to meeting with families. As it stands, with back-to-back patients and extensive documentation requirements, healthcare professionals often need to spend time after business hours to complete their notes for the day. Consequently, there is little time available for reviewing the assessment and preparing to meet with families, particularly given that preparation is a non-billable expense.
A final structural issue was the perceived benefit of the program’s prevention implementation support system (Wandersman et al., 2008), which provides training, fidelity monitoring, and ongoing consultation (Mauricio, Rudo-Stern, Dishion, Letham, & Lopez, 2019). FCU4Health providers complete an online training on the theory and structure of the program, then an in-person training where they are able to roleplay program delivery and receive feedback from program consultants. Prior to a feedback session with a real family, they participate in a meeting with a consultant to plan a case conceptualization and a potential plan for follow-up services (e.g., which parenting modules and/or community resources to offer). They also participate in a post-feedback meeting to receive feedback on their delivery. Once they implement the model with fidelity with two families, they become certified in the model. After certification, consultation continues to be available upon request. A CAB member who was trained in the original FCU expressed her confidence due to the FCU’s evidence base and training and ongoing implementation monitoring procedures.
“The other thing too is, the FCU4Health is an approach that is to the point, very organized and all the motivational interviewing that it uses – it’s a pretty positive experience. Because when you refer someone to a therapist, I’m always crossing my fingers. It’s like buying a used car, there are these gems out there and sometimes you might run into a lemon. I don’t want them to give up on it when they do go to someone that they just didn’t connect with, but with this program, it’s been researched, there’s fidelity, there’s a way to deliver it, everyone is trained in making sure that they know the important aspects - the effective components of it. So, I know I would feel good referring someone to it because I know if they are doing this program, then they have to know how to do it.” (behavioral health supervisor)
Research Design: Addressing the Need for Research Evidence
CAB members gave us input on the research design to ensure that at end of the trial, decision makers would have access to the evidence they need for program adoption and sustainability. Economic outcomes were seen as particularly important given the economic demands associated with running a healthcare clinic. Return on investment (ROI) was identified as a primary outcome of interest. Healthplan and Medicaid representatives on the CAB stated that ROI calculations should include visits to the Emergency Department, unnecessary hospitalizations, pharmaceuticals, clinic no-shows, asthma and diabetes management, and BMI. CAB members felt ROI should be at least cost-neutral with positive health outcomes. Challenges to achieving ROI in this study would be limited by the restricted age range of participants (6–12 years) and the short follow-up period of the grant (1 year) because the high healthcare costs associated with elevated BMI typically do not manifest until adulthood. Moreover, they were concerned that healthcare costs to the practices may actually increase in the short-term because of expenses related to training and implementing the program. On the other hand, there was consensus that the FCU4Health is likely to be more effective than the standard practice of providing a brochure with health information. The CAB members suggested that focusing on the subset of children who have already developed a chronic disease, such as asthma, may increase the likelihood of a positive ROI. Based on this suggestion, we added a measure of asthma management (Childhood Asthma Control Test; Liu et al., 2007). Another suggestion was to consider assessing potential changes in parent BMI, which are more immediately linked with healthcare costs. Because the FCU4Health is family-centered, it is likely to have an impact on the entire family’s health behaviors. Thus, we decided to invite all family members to participate in anthropomorphic measurement.
A second outcome to consider was whether the program could increase utilization of preventive services among this patient population, especially with respect to closing the gap on Early and Periodic Screening, Diagnostic, and Treatment (EPSDT). EPSDT is a benefit for all Medicaid recipients under the age of 21 that covers screening, prevention, and treatment at age-appropriate intervals for physical, dental, developmental, and mental health services and carries performance incentives for providers (Frankenburg & North, 1974).
“For us closing gaps in health care is huge, it is very important especially in that age range. If we could look back and say two years prior to this program, the family was having a hard time, they were missing a lot of wellness checks, not getting their vaccinations on time, there is no dental visits that are on file, but once they participated in this program, the family is much better overall.” (healthplan representative)
The Healthcare Effectiveness Data and Information Set (HEDIS) performance measures, which include BMI documentation and counseling for children with elevated BMI, also carry incentives for completion. Physicians at Phoenix Children’s Hospital said they were reluctant to screen without an effective treatment. One of the partnering FQHCs was particularly interested in adopting the FCU4Health based on the hope that having an available treatment would increase BMI documentation and counseling.
Patient and provider experience may also be compelling evidence to support ongoing implementation of FCU4Health in primary care. It was pointed out that most healthcare in the United States is delivered through a business model that is reliant upon patient satisfaction for retention in the clinic and word-of-mouth referrals to new patients. CAB members felt that the FCU4Health may increase satisfaction and, in turn, profit margins. Staff retention was also mentioned as a key issue affecting healthcare clinics. Turnover creates a tremendous burden in terms of hiring and training. If staff members have a sense of fulfillment in delivering the program and see the benefits for families, that will be key for sustainability via staff retention.
“Employee satisfaction and turnover rates - is this an onerous, difficult, tedious thing that the government’s making us do and nobody likes it? Or is this something that really returns my joy of why I am in health care.” (healthplan representative)
Finally, CAB members recognized potential collateral effects important for other systems. Schools, the justice system, and child welfare were identified as potential beneficiaries of the program.
“Schools definitely want a well child who is engaged and ready to learn. So you want to have that good- so they don’t drop out, so they don’t get into the criminal justice system and so on.” (Medicaid representative)
However, the legislative siloing of institutions, like education, health, and justice, is a barrier that would need to be overcome to justify delivering a program in one setting based on the benefits documented in another.
“Historically, there has been concern about scope-creep within one part of an agency to another. You know with Congress, here is housing, here is healthcare, don’t supplant what legislatively should be part of one agency in another.” (healthplan representative)
Discussion
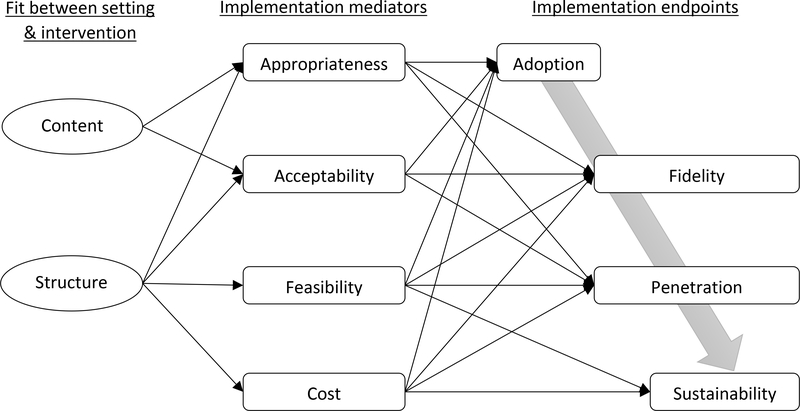
This first attempt to integrate the FCU4Health into three unique primary care clinics provided insights for practice and theory. First, we found Glasgow and Emmons’ (2007) translational research framework to be useful in guiding our discussions with stakeholders to adapt the FCU and test the adaptation (FCU4Health) in primary care. The overarching themes identified provided implications for the intervention and research design. Important considerations were 1) how well the content of the intervention addressed unmet needs of the clinic, 2) how well the structure of the intervention fit the clinic’s existing staffing and workflow, and 3) a focus on economic and organizational outcomes to inform decision making. In addition, these elements appeared to have differential links with various implementation outcomes identified in Proctor’s (2011) taxonomy. Combining these frameworks can help the field move toward more explanatory models in dissemination and implementation research (Estabrooks, Brownson, & Pronk, 2018). In the following paragraphs, we propose a theoretical model of how the intersections between interventions and clinics with respect to content and structure relate to implementation outcomes (see Figure 3).
Figure 3.
A theoretical model linking the intersections between setting and intervention characteristics and implementation outcomes
We focus on Proctor’s (2011) concepts of adoption, fidelity, penetration, and sustainability as endpoints in the model because they reflect behavioral outcomes—what actually gets delivered. Although not completely linear, they represent somewhat of a temporal process: first comes the decision to adopt, next the program is delivered with some degree of fidelity to a certain percentage of the population, and finally, the program may or may not be sustained (Glasgow et al., 2019). Fidelity and penetration remain relevant throughout the sustainment period (Aarons, Hurlburt, & Horwitz, 2011).
Fit between elements of both the content and the structure were associated with appropriateness and acceptability, which were in turn related to adoption. For example, appropriateness (Proctor, et al., 2011), or the perceived ability of an intervention to address a particular problem of interest to an organization, was initially driven by studies that demonstrated FCU’s effects on pediatric health behaviors and obesity, and then amplified by the adaptation to specifically focus on both behavioral and physical health outcomes, which aligns well with the move toward integrated primary care. With respect to acceptability, which refers to how agreeable or palatable an intervention is (Proctor, et al., 2011), CAB members felt it was important to frame the FCU4Health as a health promotion program rather than a weight loss program, which may reduce potential stigma. The sense of appropriateness and acceptability may not be uniform across members of an adopting organization. If leadership makes the decision to adopt when staff are not on board, there may be challenges to fidelity and penetration, which may have an impact on sustainability. In this particular example, however, leadership and staff were in agreement that the program was acceptable and appropriate for the setting.
Feasibility and cost were driven by fit related to the structure, rather than the content, and were thought to be the primary factors limiting adoption and sustained implementation. Variability in behavioral health integration appeared to be the most important factor. At the hospital-based clinic, the loss of care coordination resulted in adaptation to a referral model. For private, standalone clinics, the lack of integration was an insurmountable barrier to participation in the trial.
Cost was less of an issue driving adoption in this study because grant support was available to supplement non-billable services. However, having the grant support allowed us to figure out where potential challenges with billing would be while at the same time, providing confidence that clinics would be compensated for services while we solved any challenges. Our work with the FQHCs demonstrated that many of the individual components of the FCU4Health are already billable. One component of the FCU4Health that is not billable is reimbursement for preparation time. In between the assessment and feedback session, providers of the FCU4Health require time to review the assessment, develop a sound case conceptualization, and identify appropriate follow-up services. This preparation time is a core component of the program, but is not currently a billable service. The ability to bill for preparation activities (e.g., reviewing case notes or labs) would likely improve the quality of health services across disciplines. Once our economic analyses are complete, we will continue our discussions with Medicaid and healthplans about the potential for reimbursement for FCU4Health services. In future projects, we will continue to evaluate different models of delivery, which will evolve in tandem with ongoing changes to the healthcare system.
Finally, the structure of the FCU4Health includes the prevention support system, which is responsible for training and supervision to promote implementation fidelity (Wandersman, et al., 2008). Fidelity may be driven by the fit between setting and intervention in terms of both content and structure (Berkel, Mauricio, Schoenfelder, & Sandler, 2011). While fidelity as an implementation outcome was not brought up by our CAB, members did discuss that the prevention support system boosted their confidence and influenced their decision to adopt the program. The need to implement a program with fidelity has often been thought of as a barrier to the implementation of evidence-based programs. Alternatively, feedback from our CAB members support previous findings from Aarons and colleagues (2009) that a program’s evidence-base and fidelity monitoring procedures may increase providers’ confidence that their efforts will have a tangible effect on family outcomes. Future research should also examine whether a providers’ ability to implement a program with fidelity has an impact on the program’s sustainability.
Limitations
The current study obtained input from five primary care settings (three of which implemented the FCU4Health in the trial). Each clinic had a different constellation of resources that had implications for whether and how the program could be implemented. Given the substantial variability within a small sample size, it is certain that including additional clinics would uncover further unique structures and needs. However, the fact that we were able to include the perspectives of clinics that either chose not to or were not able to participate in the research serves to defuse potential bias.
Conclusion
Primary care is a promising setting for expanding the reach of evidence-based parenting programs. This study represented the first attempt to translate the Family Check-Up for delivery within primary care. The congruence between the focus of the FCU4Health and the mission of primary care promoted interest among our stakeholders. However, structural variability created implementation challenges that are still being addressed. The findings of this work have theoretical and practice implications for the translation of other evidence-based programs into primary care and other regular service delivery settings.
References
- Aarons GA, Hurlburt M, & Horwitz SM (2011). Advancing a conceptual model of evidence-based practice implementation in public service sectors. Administration and Policy in Mental Health and Mental Health Services Research, 38, 1, 4–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aarons GA, Sommerfeld DH, Hecht DB, Chaffin MJ, & Silovsky JF (2009). The impact of evidence-based practice implementation and fidelity monitoring on staff turnover: Evidence for a protective effect. Journal of Consulting & Clinical Psychology, 77, 2, 270–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaumont SW, Berkel C, Tovar-Huffman A, & Shaw T (2011). Advocacy and care coordination for young children and their families in Arizona. Paper presented at the annual meeting of the American Academy of Pediatrics, Chicago, IL. [Google Scholar]
- Berkel C, Araica E, Tovar-Huffman A, Beaumont S, Shaw T, & Christensen R (2015). Implementation and outcomes of a comprehensive care coordination program at Phoenix Children’s Hospital. Paper presented at the annual Phoenix Children’s Hospital Research Day, Phoenix , AZ. [Google Scholar]
- Berkel C, Beaumont S, Dishion TJ, Tovar-Huffman A, Araica E, & Smith JD (2016). Physician concerns about child health and the need for evidence-based parenting support. Paper presented at the annual Phoenix Children’s Hospital Research Day, Phoenix, AZ. [Google Scholar]
- Berkel C, Mauricio AM, Schoenfelder E, & Sandler IN (2011). Putting the pieces together: An integrated model of program implementation. Prevention Science, 12, 1, 23–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloom B, Jones LI, & Freeman G (2013). Summary health statistics for U.S. children: National Health Interview Survey, 2012 Vital Health Statistics (Vol. 10). Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Bowen GA (2006). Grounded theory and sensitizing concepts. International Journal of Qualitative Methods, 5, 3, 12–23. [Google Scholar]
- Carney JK, Maltby HJ, Mackin KA, & Maksym ME (2011). Community-academic partnerships: How can communities benefit? American Journal of Preventive Medicine, 41, 4, S206–S13. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control & Prevention. (2015). Childhood Obesity Research Demonstration 2.0; RFA-DP-16–004. Atlanta, GA: National Center for Chronic Disease Prevention. [Google Scholar]
- Chiapa A, Rudo-Stern J, Smith JD, Berkel C, Beaumont S, & Dishion TJ (2014). Implementing the Family Check-Up in a General Pediatrics Clinic for adolescent behavioral and mental health. Paper presented at the Phoenix Children’s Hospital Research Day, Phoenix, AZ. [Google Scholar]
- Curran GM, Bauer M, Mittman B, Pyne JM, & Stetler C (2012). Effectiveness- implementation hybrid designs: Combining elements of clinical effectiveness and implementation research to enhance public health impact. Medical Care, 50, 3, 217–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dishion TJ, & Stormshak EA (2007). Intervening in children’s lives: An ecological, family- centered approach to mental health care. Washington, DC: American Psychological Association. [Google Scholar]
- Dishion TJ, Stormshak EA, & Kavanagh K (2011). Everyday parenting: A professional’s guide to building family management skills. Champaign, IL: Research Press. [Google Scholar]
- Estabrooks PA, Brownson RC, & Pronk NP (2018). Dissemination and implementation science for public health professionals: An overview and call to action. Preventing Chronic Disease, 15, E162, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frankenburg WK, & North AF (1974). A guide to screening for the Early and Periodic Screening, Diagnosis and Treatment Program (EPSDT) under Medicaid. Evanston, IL: American Academy of Pediatrics. [Google Scholar]
- Glasgow RE, & Emmons KM (2007). How can we increase translation of research into practice? Types of evidence needed. Annual Review of Public Health, 28, 413–33. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Harden SM, Gaglio B, Rabin B, Smith ML, Porter GC, Ory MG, & Estabrooks PA (2019). RE-AIM Planning and Evaluation Framework: Adapting to New Science and Practice With a 20-Year Review. Frontiers in Public Health, 7, 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagan JF, Shaw JS, & Duncan PM (2017). Bright Futures guildelines for health supervision of infants, children, and adolescents (4th ed.). Elk Grove Village, IL: American Academy of Pediatrics. [Google Scholar]
- Heath B, Wise Romero P, & Reynolds K (2013). A standard framework for levels of integrated healthcare. Washington, DC: SAMHSA-HRSA Center for Integrated Health Solutions. [Google Scholar]
- Institute of Medicine, & National Research Council. (2014). Strategies for scaling effective family-focused preventive interventions to promote children’s cognitive, affective, and behavioral health: Workshop summary. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Kellam SG (2012). Developing and maintaining partnerships as the foundation of implementation and implementation science: Reflections over a half century.Administration and Policy in Mental Health and Mental Health Services Research, 39, 4, 317–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leslie LK, Mehus CJ, Hawkins JD, Boat T, McCabe MA, Barkin S, Perrin EC, Metzler CW, Prado G, Tait VF, Brown R, & Beardslee W (2016). Primary health care: Potential home for family-focused preventive interventions. American Journal of Preventive Medicine, 51, 4, S106–S18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levitt HM, Motulsky SL, Wertz FJ, Morrow SL, & Ponterotto JG (2017). Recommendations for designing and reviewing qualitative research in psychology: Promoting methodological integrity. Qualitative Psychology, 4, 1, 2–22. [Google Scholar]
- Liu AH, Zeiger R, Sorkness C, Mahr T, Ostrom N, Burgess S, Rosenzweig JC, & Manjunath R (2007). Development and cross-sectional validation of the Childhood Asthma Control Test. Journal of Allergy and Clinical Immunology, 119, 4, 817–25. [DOI] [PubMed] [Google Scholar]
- Mauricio AM, Rudo-Stern J, Dishion TJ, Letham K, & Lopez M (2019). Provider readiness and adaptations of competency drivers during scale-up of the Family Check-Up. The Journal of Primary Prevention, 40, 1, 51–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, & Rollnick S (2002). Motivational interviewing: Preparing people for change (2nd ed.). New York: Guilford Press. [Google Scholar]
- O’Connell ME, Boat T, & Warner KE (Eds.). (2009). Preventing mental, emotional, and behavioral disorders among young people: Progress and possibilities. Washington, D.C.: National Academies Press. [PubMed] [Google Scholar]
- Perrin EC, Leslie LK, & Boat T (2016). Parenting as primary prevention. JAMA Pediatrics, 170, 7, 637–8. [DOI] [PubMed] [Google Scholar]
- Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, Griffey R, & Hensley M (2011). Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Administration and Policy in Mental Health and Mental Health Services Research, 38, 2, 65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers VW, Hart PH, Motyka E, Rines EN, Vine J, & Deatrick DA (2013). Impact of Let’s Go! 5–2-1–0: A community-based, multisetting childhood obesity prevention program. Journal of Pediatric Psychology, 38, 9, 1010–20. [DOI] [PubMed] [Google Scholar]
- Rose F, Coombs E, Schwartz S, & Clark J (2007). Bridges for Newborns: An Updated Evaluation. Burlingame, CA: The SPHERE Institute. [Google Scholar]
- Rudo-Stern J, Chiapa A, Smith JD, Berkel C, Beaumont SW, & Dishion TJ (2014). Implementing the Family Check-Up in a General Pediatrics Clinic. Paper presented at the Society of Pediatric Psychology Annual Conference, Philadelphia, PA. [Google Scholar]
- Sandler IN, Ingram A, Wolchik SA, & Winslow E (2015). Long-term effects of parenting-focused preventive interventions to promote resilience of children and adolescents. Child Development Perspectives, 9, 3, 164–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JD, Berkel C, Jordan N, Atkins DC, Narayanan SS, Gallo C, Grimm KJ, Dishion TJ, Mauricio AM, Rudo-Stern J, Meachum MK, Winslow E, & Bruening MM (2018). An individually tailored family-centered intervention for pediatric obesity in primary care: Study protocol of a randomized type II hybrid effectiveness-implementation trial (Raising Healthy Children study). Implementation Science, 13, 1, 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JD, Berkel C, Rudo-Stern J, Montano Z, St. George SM, Prado G, Mauricio AM, Chiapa A, Bruening MM, & Dishion TJ (2018). The Family Check-Up 4 Health (FCU4Health): Applying implementation science frameworks to the process of adapting an evidence-based parenting program for prevention of pediatric obesity and excess weight gain in primary care. Frontiers in Public Health, 6, 293, 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JD, Cruden G, Rojas L, Van Ryzin MJ, Fu E, Davis MM, Landsverk J, & Brown CH (2019). Implementation of parenting interventions in primary care for children’s mental and behavioral health: A scoping review. Submitted for publication. [Google Scholar]
- Smith JD, Egan KN, Montano Z, Dawson-McClure S, Jake-Schoffman DE, Larson M, & St. George SM (2018). A developmental cascade perspective of paediatric obesity: A conceptual model and scoping review. Health Psychology Review, 1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JD, Montano Z, Dishion TJ, Shaw DS, & Wilson MN (2015). Preventing weight gain and obesity: Indirect effects of a family-based intervention in early childhood. Prevention Science, 16, 408–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoth R, Rohrbach LA, Greenberg M, Leaf P, Brown CH, Fagan A, Catalano RF, Pentz MA, Sloboda Z, & Hawkins JD (2013). Addressing core challenges for the next generation of Type 2 translation research and systems: The translation science to population impact (TSci Impact) framework. Prevention Science, 14, 4, 319–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Ryzin MJ (2016). A component-centered meta-analysis of family-based prevention programs for adolescent substance use. Clinical Psychology Review, 45, 72–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Ryzin MJ, & Nowicka P (2013). Direct and indirect effects of a family-based intervention in early adolescence on parent–youth relationship quality, late adolescent health, and early adult obesity. Journal of Family Psychology, 27, 1, 106–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wandersman A, Duffy J, Flaspohler P, Noonan R, Lubell K, Stillman L, Blachman M, Dunville R, & Saul J (2008). Bridging the gap between prevention research and practice: The Interactive Systems Framework for Dissemination and Implementation. American Journal of Community Psychology, 41, 3–4, 171–81. [DOI] [PubMed] [Google Scholar]