Summary
Ultrasound imaging of the lung and associated tissues may play an important role in the management of patients with COVID‐19–associated lung injury. Compared with other monitoring modalities, such as auscultation or radiographic imaging, we argue lung ultrasound has high diagnostic accuracy, is ergonomically favourable and has fewer infection control implications. By informing the initiation, escalation, titration and weaning of respiratory support, lung ultrasound can be integrated into COVID‐19 care pathways for patients with respiratory failure. Given the unprecedented pressure on healthcare services currently, supporting and educating clinicians is a key enabler of the wider implementation of lung ultrasound. This narrative review provides a summary of evidence and clinical guidance for the use and interpretation of lung ultrasound for patients with moderate, severe and critical COVID‐19–associated lung injury. Mechanisms by which the potential lung ultrasound workforce can be deployed are explored, including a pragmatic approach to training, governance, imaging, interpretation of images and implementation of lung ultrasound into routine clinical practice.
Keywords: COVID‐19, lung ultrasound, point‐of‐care ultrasound, training, workforce
요약
폐와 주변 조직의 초음파 영상은 COVID‐19와 관련된 폐 손상 환자 관리에 중요한 역할을 할 수 있다. 폐 초음파는 청 진 또는 방사선 촬영과 같은 다른 모니터링 방식과 비교하였 을 때 진단의 정확도가 높고, 인체공학적으로 유리하며, 감염 관리 문제점이 적다. 환기 보조의 시작, 증가, 감소 및 이탈 시 점을 알려줌으 로써 폐 초음파는 호흡 부전 환자 를 위한 COVID‐19 관리에 통합될 수 있다. 현재 의료 서비스에 가해 지는 전례 없는 압력을 감안할 때, 임상 의사에 대한 지원 및 교육은 폐 초음파를 보다 폭넓게 구현하기 위하여 꼭 필요하 다. 본 담화적 리뷰는 중등증, 중증 및 치명적인 COVID‐19 관 련 폐 손상 환자에서 폐 초음파 사용 및 해석을 위한 증거와 임상 지침의 요약을 제공하였다. 훈련, 거버넌스, 이미징, 영상 해석 및 임상에서 폐 초음파의 구현을 위한 실용적인 접근법 을 포함하여 폐 초음파를 다룰 수 있는 잠재적인 인력인이 배 치될 수 있는 메커니즘을 탐구하였다.
Introduction
Ultrasound imaging of the lung and associated tissues may help inform clinical decision‐making for patients with coronavirus disease 2019 (COVID‐19) and management of their associated respiratory failure and lung injury. This is facilitated in part by the typical sonographic characteristics of COVID‐19–associated lung injury during disease progression and recovery 1. Although there exists much evidence to support the clinical value of lung ultrasound 2, practice is underpinned through education, competency and associated governance procedures 3. As with other point‐of‐care ultrasound areas, examinations should be conducted to answer a focused clinical question and procedures should be aligned with agreed national and local standards 4, 5.
The COVID‐19 pandemic has led to unprecedented pressure on healthcare services, particularly care pathways for all critically ill patients 6. The existing lung ultrasound workforce can easily be upscaled and upskilled through education on the principles of lung ultrasound in patients with COVID‐19. This narrative review provides a summary of these principles and how lung ultrasound more generally can be integrated into the COVID‐19 care pathway. We present possible mechanisms for pragmatic training in the use of lung ultrasound which may be achievable, despite the unprecedented demand on clinical services.
Methods
We searched the CENTRAL, EMBASE and Web of Science databases for all articles published between 1 November 2019 and 1 April 2020. The following MeSH key words were used: ‘lung’; ‘chest’; ‘pulmonary’; ‘pulmo*’; ‘thorax’; ‘thora*’; ‘ultrasound’; ‘sonography’; ‘ultraso*’; ‘sonog*’; ‘COVID*’; and ‘SAR‐CoV‐2’. This yielded 11 full‐text papers (Table 1).
Table 1.
Summary of retrieved evidence (alphabetical order by first author)
| Author [reference] | Article type | Peer reviewed | Number of patients | Clinical setting | Patient population | Scanning protocol | Transducer type | Sonographic elements/observations | Recommendations |
|---|---|---|---|---|---|---|---|---|---|
| Buonsenso et al. 7 | Letter | Yes | Not reported | Hospital | Children | Not reported | Linear wireless | Recommendations for lung ultrasound to reduce SARS‐CoV‐2 transmission. | Avoid the use of stethoscopes, chest radiographs and CT to reduce cross‐infection rates. |
| Buonsenso et al. 8 | Case report | Yes | 1 | Emergency Department | Adult | 12 areas | ConvexWireless | Bilateral involvement; irregular pleura; confluent B‐lines; small consolidations and spared areas. | Use of lung ultrasound to minimise number of clinicians that patient is exposed to and triage high/low‐risk patients. A portable device is easier to clean. |
| Corradi et al. 9 | Letter | Yes | Not applicable | Not reported | Not reported | Not reported | Not reported | Opinion on quantification of B‐lines relevant to patients with COVID‐19. | Visual estimation of B‐line number and frequency has high inter‐ and intra‐observer variability. |
| Huang et al. 1 | Case series | No | 20 | Emergency Department | Adults | 12 areas | Convex or linear | Bilateral involvement; posterior and inferior involvement; coalescent B‐lines; irregular pleura; small consolidations; air bronchograms; and small pleural effusions. | Lung characteristics of patients with COVID‐19 are ideal to image with ultrasound. |
| Moro et al. 10 | Clinical recommendation | Yes | Not reported | Not reported | Pregnant women | Not reported | Convex or linear | Thickened/irregular pleura; spared areas; small consolidations; lobar consolidations; and air bronchograms. | Tips include: set focus on pleural line; to view the pleura, reduce the gain; scan in sitting or side lying to avoid prone lying. |
| Peng et al. 11 | Letter | Yes | Not reported | Critical care | Critically unwell adults | 12 areas | Not reported | Thickened/irregular pleura; variety of B‐line patterns; non‐translobar and translobar consolidation; small consolidations; air bronchograms; and pleural effusions (rare). | Use of lung ultrasound to track disease evolution; monitor lung recruitment; response to prone position; management of extracorporeal membrane oxygenation; and guide weaning and liberation from mechanical ventilation. |
| Poggiali et al. 12 | Letter | Yes | 12 | Emergency Department | Adults | Not reported | Not reported | Bilateral involvement; B‐lines; spared areas; and small consolidations, mainly posteriorly. | Recommends the use of lung ultrasound in the Emergency Department for patients with COVID‐19. |
| Soldati et al. 13 | Letter | Yes | Not reported | Emergency Department, wards, and critical care | Not reported | 16 areas | Convex or linear | Bilateral involvement, confluent B‐lines; multiple areas of B‐lines; small consolidations; large consolidation in dependent areas; and air bronchograms. | Use of lung ultrasound to triage at home and pre‐hospital; diagnose COVID‐19; prognostic stratification; track evolution towards consolidation; guide mechanical ventilation and weaning; and monitor the effects of therapeutic interventions. |
| Soldati et al. 14 | Clinical recommendation | Yes | Not reported | Wards and critical care | Adults | 14 areas | Convex or linear | An expert consensus proposal for lung ultrasound scanning protocol in patients with COVID‐19. | Tips include: use a hand‐held device and set the focus on the pleural line. |
| Thomas et al. 15 | Case report | Yes | 1 | Ward and critical care | Adult | Not reported | Convex | Multifocal B‐lines; pleural thickening; and small consolidations. | Lung ultrasound may be useful to assess patients with COVID‐19. |
| Vetrugno et al. 16 | Clinical recommendation | Yes | Not reported | Critical care | Adults | 12 areaLUS score | Convex | Confluent B‐lines; pleural thickening/disruption; and small consolidations. | Use of lung ultrasound to diagnose and monitor; monitor patient trajectory; and reduce the need for radiographic imaging. |
Due in part to the rapid emergence of the COVID‐19 pandemic, evidence in the published literature to guide the use of lung ultrasound in COVID‐19 is sparse. Letters comprised the majority of publications (5/11), with two case reports and three clinical recommendation papers. The case series was a retrospective analysis of ultrasonic features of non‐critical patients with COVID‐19 and was published in a non‐peer–reviewed journal. Five publications 7, 8, 10, 13, 14 were written by the same authorship group and the emphasis of their observations is similar.
In the hierarchy of empirical evidence, all publications identified by our search were deemed to be weak 17. This lack of high‐quality evidence published in peer‐reviewed journals presents a challenge to the formulation of recommendations. Consequently, we also searched for publications from professional and healthcare organisations.
Current impact on healthcare provision
Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), which causes COVID‐19, was declared a ‘Public Health Emergency of International Concern’ on 30 January 2020 by the World Health Organization (WHO) 18. At the time of writing, global SARS‐CoV‐2 infections are in the hundreds of thousands and death rates are accelerating, placing enormous demands on healthcare provision 6. As such, healthcare provision needs to be responsive and adaptive. Examples of pragmatic approaches include a recent guide on methods for developing rapid guidelines on Covid‐19 19, a COVID‐19 critical care rapid guideline 20 and consensus guidelines for managing the airway in patients with COVID‐19 21.
The role of lung ultrasound
Common initial symptoms of COVID‐19 are fever, cough and dyspnoea, with a wide spectrum of severity 22. There are indications that 80% of patients have mild symptoms but approximately 14% experience moderate to severe disease with 5% becoming critically ill 23. Of the 19% of patients that contract COVID‐19 and require hospitalisation, almost all present with very distinctive clinical characteristics that progress in a similar way on computed tomography and ultrasound imaging 1, 24. However, many traditional tools used for clinical examination and decision‐making are of limited utility in a COVID‐19 patient care pathway.
Despite using dedicated stethoscopes for individual patients as per WHO guidance 25, auscultation presents a high risk of nosocomial transmission 26. The risk of transporting critically unwell patients for a computed tomography scan followed by the necessary decontamination procedures makes this form of imaging risky and time consuming 11. The use of portable chest radiographs also raises the issue of contamination, unless a dedicated machine is reserved for cohorted patients. In addition, chest radiographs correlate poorly with the clinical picture as compared with computed tomography and ultrasound imaging 27.
During COVID‐19 disease progression, changes in the lung parenchyma begin in the distal regions of the lung and progress proximally. There are ‘ground glass’ opacities and ‘crazy paving’ changes seen on computed tomography imaging in the early phases, and larger consolidations in the basal or dependent lung regions later in the disease course 24. The regions most frequently affected are the right middle and lower lobes followed by the left upper lobe 27. The histopathology of the COVID‐19 pneumonia progresses in the distal regions of the lung and is characterised by alveolar damage and oedema, interstitial thickening and gravitational consolidations 13. The pathological progression of COVID‐19 pneumonia is therefore well suited to a surface imaging technique such as lung ultrasound 1 (Fig. 1).
Figure 1.
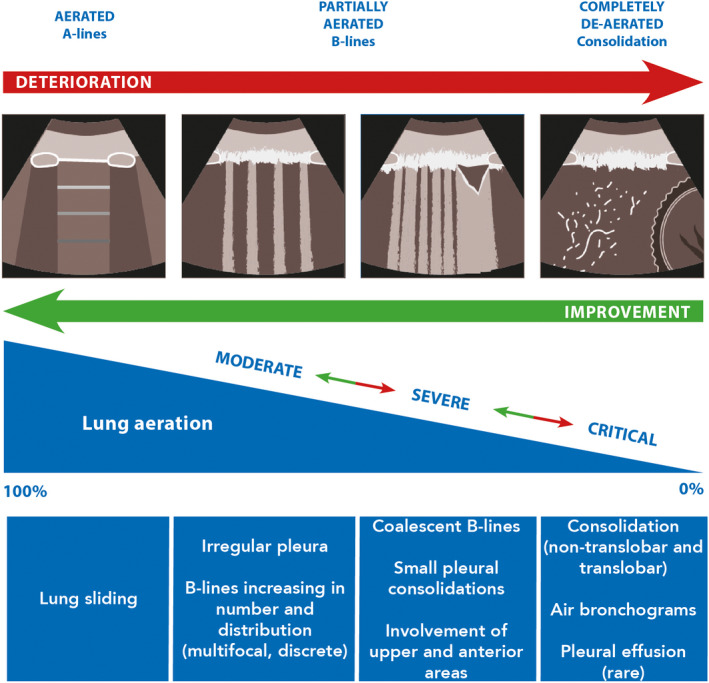
Sonographic characteristics of moderate, severe and critical pleural and parenchymal changes in patients with COVID‐19. [Colour figure can be viewed at wileyonlinelibrary.com]
To address contamination concerns, the UK Intensive Care Society has published guidance on the decontamination of ultrasound equipment for COVID‐19 patients 28. As the disease progresses and characteristics develop, COVID‐19 is associated with the sonographic appearances of pleural line irregularities and B‐line artefacts, which are caused by interstitial thickening and inflammation, and increase in number with severity. Small consolidations also increase in frequency and size 11. According to the WHO 28, patients with COVID‐19 requiring hospitalisation for moderate–severe disease will require supplementary oxygen and regular monitoring that facilitates early recognition and escalation of the deteriorating patient. Recommendations are that patients receiving respiratory support should be monitored closely for clinical deterioration 30 and serial lung ultrasound imaging may help inform this 31.
As with many areas of ultrasound imaging and interpretation, the identification, quantification and communication of the nature of B‐lines is subjective and may be open to interpretation 9, 14. The larger the number of regions scanned, the greater the likelihood of a representative picture of overall organ involvement. However, experience is required for the operator to generate high‐quality and reproducible images, and the imaging of many regions is time consuming. In this regard, we recommend a pragmatic approach depending on the level of operator experience and the requirements of the clinical team. The use of six‐zone scanning would provide a focused and rapid picture of involvement of key regions of the lung 32.
Where time allows, use of the 12‐zone lung ultrasound score 33 provides a potential mechanism to bring a degree of objectivity to quantifying the level of involvement, as a comprehensive whole‐organ assessment. In addition, it allows for communication of findings between serial scans, different operators and different care settings, so that changes can be better quantified and communicated. As such, these would be the realm of more experienced lung ultrasound practitioners, with minimal additional training 34; although only where time allows.
Supporting existing lung ultrasound practitioners
Existing lung ultrasound practitioners are those clinicians who have undertaken and formally demonstrated lung ultrasound competency in the care of patients with respiratory failure. Ideally, they would have successfully gained accreditation following training in lung ultrasound such as Focused Ultrasound in Intensive Care (FUSIC) accreditation. These clinicians would regularly use lung ultrasound to inform clinical decision‐making and the care of such patients within a structure that aligns with all relevant clinical and governance considerations. Clinicians include but are not limited to doctors, physiotherapists and advanced critical care practitioners.
Lung ultrasound may allow operators and clinicians to determine where a patient is on the clinical spectrum of COVID‐19–associated lung injury (Table 2) 35. Patients are grouped according to the severity of COVID‐19–associated respiratory failure: moderate, severe or critical 29. Although these groupings might broadly align with the clinical setting (e.g. ward, high dependency unit or intensive care unit), grouping according to the level of respiratory compromise allows for transferability of information regardless of the care pathway configuration or care setting. Inevitably, these patients may have comorbidities and/or other COVID‐19–related systemic involvement. Lung ultrasound in these patients is solely with respiratory function in mind. In all cases, correlation with clinical presentation is required and sonographic findings must never be the sole indicator for initiating, titrating, escalating and/or weaning treatment.
Table 2.
A simplified description of where in the COVID‐19 patient care pathway lung ultrasound is of most use
| Severity of COVID‐19–related lung injury | Typical sonographic characteristics | Typical clinical characteristics |
|---|---|---|
| Pre‐disease to moderate |
Development of B‐lines which begin to increase in number and distribution. The pleural line begins to become irregular. Areas with B‐lines are adjacent to normal areas of lung sliding and A‐lines. These are ‘skip lesions’ or ‘spared areas’. Small (~1 cm) consolidations. |
Respiratory rate > 30 min−1. Oxygen saturations ≤93% on room air. The need for supplemental oxygen. Lung tissue begins to lose aeration. |
| Severe |
B‐lines continue to increase in number and distribution, and begin to affect the upper and anterior areas of the lungs. B‐lines become coalescent/confluent. Small consolidations increase in number and size. |
Oxygen saturations ≤ 93% on supplementary oxygen. Clinical signs of respiratory distress. The need for additional supplemental oxygen or respiratory support. Lung tissue is becoming progressively de‐aerated. |
| Critical |
Extensive coalescent B‐lines affect the upper and anterior areas of the lungs. Significant small consolidations affect the upper and anterior areas of the lungs. Posterio‐basal sections of the lungs have significant bilateral alveolar interstitial syndrome progressing to consolidation with or without air bronchograms. Pleural effusions are small or rare unless the patient's fluid balance is high. |
Likely to be or require invasive mechanical ventilation. The need for a high fraction of inspired oxygen. Dependent areas of lung tissue have becoming non‐aerated. |
The lung ultrasound score is one potential mechanism to objectively grade COVID‐19–associated lung injury. The sonographic artefact patterns seen on lung ultrasound may also be used to monitor the degree of lung aeration at the bed‐side with effects seen from positive end expiratory pressure recruitment 33, 36 and spontaneous breathing trials during liberation from mechanical ventilation 37. Across 12 scanning zones, (six on each hemithorax) to a maximum score of 36, the four lung ultrasound aeration patterns (scored 0–3) are normal pattern (A‐lines or non‐significant B‐lines), generating zero points; significant B‐lines (≥3 per rib space), generating one point; coalescent B‐lines with or without small consolidations, generating two points; and consolidation, generating three points 31. Intra‐ and inter‐rater reliability has yet to be fully explored with the lung ultrasound scoring system 38, but this 0–36‐point scoring system may have the potential to monitor the deterioration or recovery of lung aeration in patients with COVID‐19 and to guide the administration of ventilation techniques, positive end expiratory pressure, prone positioning or any combination thereof.
Upskilling the potential lung ultrasound workforce
Alongside the existing lung ultrasound workforce, the potential lung ultrasound workforce will likely prove vital in meeting the unprecedented demand on clinical services. These potential new operators include: those with previous lung ultrasound experience; those with alternate ultrasound imaging experience; and those with no previous ultrasound imaging experience. There should be a commitment to ensure that while point‐of‐care ultrasound may have a focused remit, the standards of education and demonstrable competency are identical to those in a traditional imaging setting. However, given the extraordinary pressures on clinical services and the highly valuable role that lung ultrasound may play in this pandemic, we present pragmatic considerations for upskilling the potential lung ultrasound workforce (Table 3). Nonetheless, in relation to all aspects of lung ultrasound, healthcare service providers and individual practitioners are reminded of their responsibility to provide the highest standards of clinical care. Key differences between the activities of existing lung ultrasound practitioners and potential lung ultrasound practitioners are proposed (Table 4).
Table 3.
Pragmatic considerations for the upskilling the potential lung ultrasound workforce
| Previous experience of lung ultrasound | Experienced in the use of other forms of ultrasound imaging | No previous ultrasound imaging experience | |
|---|---|---|---|
| Pre‐existing skills and knowledge |
Foundation physics Probe handling Image optimisation Familiarity with normal and pathological imaging Reporting of lung ultrasound findings Clinical application of lung ultrasound |
Foundation physics Probe handling Imaging optimisation Strategies to address suboptimal imaging Reporting of ultrasound imaging findings |
Familiarity with clinical management of critically ill patient |
| Skills and experience required |
Strategies to address suboptimal imaging, for example, high BMI, poor differentiation of tissues and patient positioning The key principles of imaging in patients with COVID‐19 |
Familiarisation with key elements of lung imaging Familiarity with normal and pathological imaging Strategies to address suboptimal imaging, for example , high BMI, poor differentiation of tissues and patient positioning Reporting of lung ultrasound findings Awareness of clinical application of lung ultrasound The key principles of imaging in patients with COVID‐19 |
Foundation physics Probe handling Imaging optimisation Familiarisation with key elements of lung imaging Familiarity with normal and pathological imaging Strategies to address suboptimal imaging, for example, high BMI, poor differentiation of tissues and patient positioning Reporting of lung ultrasound findings Clinical application of lung ultrasound imaging findings The key principles of imaging in patients with COVID‐19 |
| Support required | Existing lung ultrasound practitioner for directly supervised scanning experience. Subsequently as option for second opinion |
Existing lung ultrasound practitioner or generic sonography educator to teach lung ultrasound technique. Existing lung ultrasound practitioner for directly supervised scanning experience. Subsequently as option for second opinion. |
Generic sonography educator for foundations of ultrasound, including ?hands‐on’ support. Existing lung ultrasound practitioner or generic sonography educator to teach lung ultrasound technique. Existing lung ultrasound practitioner for directly supervised scanning experience. Subsequently as option for second opinion |
| Priority for training | High – the limited input required supports rapid progression to the frontline of COVID‐19 imaging |
Medium – will progress more quickly than those with no previous ultrasound imaging experience. The moderate input required supports progression to the frontline of COVID‐19 imaging |
Low – more extensive training required as compared with other workforce groups. Clinical knowledge means these individuals could become extremely valuable in the medium to long term. |
Table 4.
Key differences between the activities of existing lung ultrasound practitioners and potential lung ultrasound practitioners
| Existing lung ultrasound practitioner | Potential lung ultrasound workforce | |
|---|---|---|
| Core role in COVID‐19 imaging |
Identification of sonographic characteristics of COVID‐19 pathology Support clinical decision‐making. Support the ‘potential lung ultrasound workforce’ |
Identification of sonographic characteristics of COVID‐19 pathology Communicate findings to support clinical decision making. |
| Level of ‘sonographic autonomy’ | High – able to provide ‘stand‐alone’ sonographic interpretation |
Initially low – requires verification of imaging Progress to moderate – discussion of scan findings to inform clinical decision‐making. Progress to ability to provide ‘stand‐alone’ sonographic interpretation in non‐complex cases |
| Additional imaging mechanisms | Where time allows, use the 12‐zone lung ultrasound score (scale of 0–36) | None |
| Differential sonographic diagnosis |
Identification of sonographic characteristics of COVID‐19 as part of initial triage and diagnosis Differential sonographic diagnoses of pneumothorax or pleural effusion |
None |
In the context of a respiratory pandemic, we advocate for a balance of professional rigour and pragmatism 39. This includes taking account of local and national clinical governance considerations, although in all cases it is the operators’ responsibility to ensure these are addressed. Considerations of professional indemnity and registration must frame all decisions. For qualified medical doctors in the UK, professional indemnity and registration are unlikely to present barriers to lung ultrasound use. For physiotherapists in the UK with Professional and Public Liability through the Chartered Society of Physiotherapy, use of lung ultrasound (where professional expertise has been developed and maintained) as an adjunct to physiotherapy assessment and treatment is permissible. Other potential operators (e.g. respiratory nurses, radiographer sonographers, point‐of‐care sonographers, etc.) should consult their professional indemnity and registration bodies. Operators both within and outside of the UK should consult their professional indemnity and registration bodies in the first instance.
Other governance considerations include agreement with members of the care pathway (both upstream and downstream), their employer and local managers. Where professional indemnity and registration considerations have been addressed, it is hoped that ‘local’ elements could be readily negotiated. However, it is key to ensure that the individual or profession only operates within their defined and permissible scope of practice – and that the limitations of this are explicitly communicated 40. Lung ultrasound practitioners require: access to equipment of suitable quality to generate and store meaningful images 41; training with appropriate clinical support; clear lines of accountability; systems to report unexpected findings; and absolute clarity regarding decision‐making based upon imaging findings. Although we encourage pragmatism, a clinician who has received no training and does not have access to mentorship in the workplace clearly should not be attempting to use this imaging modality.
Conclusion
Amidst a global respiratory pandemic, lung ultrasound may have a key role to play in the clinical management of patients with COVID‐19–associated lung injury. Our clinical recommendations provide support for existing operators and describe how the current lung ultrasound workforce may be expanded. Future work should focus on adding to the very limited evidence base for these clinical recommendations and the integration of lung ultrasound into clinical care pathways. The pragmatic mechanisms outlined in this review may mobilise a whole new lung ultrasound workforce. One legacy of the current pandemic is likely to be the expansion of lung ultrasound use and expertise within the UK and beyond. Once the healthcare landscape returns to something approximating more normal circumstances, implementation of frameworks to support consolidation of lung ultrasound skills and competency are advocated.
Acknowledgments
We thank Mrs L. Hayward for her comments on a draft of the manuscript. No external funding or competing interests declared.
Contributor Information
M. J. Smith, Email: smithmj2@cf.ac.uk.
S. A. Hayward, @sonophysio.
S. M. Innes, @sminnes2.
A. S. C. Miller, @icmteaching.
References
- 1. Huang Y, Wang S, Liu Y, et al. A preliminary study on the ultrasonic manifestations of peripulmonary lesions of non‐critical novel coronavirus pneumonia (COVID‐19). SSRN 2020. Epub 28 February. doi.org/10.2139/ssrn.3544750 (accessed 06/04/2020). [Google Scholar]
- 2. Winkler M, Touw H, van de Ven P, et al. Diagnostic accuracy of chest radiograph, and when concomitantly studied lung ultrasound, in critically ill patients with respiratory symptoms: a systematic review and meta‐analysis. Critical Care Medicine 2018; 46: e707–14. [DOI] [PubMed] [Google Scholar]
- 3. Pietersen P, Madsen K, Graumann O, et al. Lung ultrasound training: a systematic review of published literature in clinical lung ultrasound training. Critical Ultrasound Journal 2018; 10: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dietrich C, Goudie A, Chiorean L, et al. Point of care ultrasound: a WFUMB position paper. Ultrasound in Medicine and Biology 2017; 43: 49–58. [DOI] [PubMed] [Google Scholar]
- 5. Cormack C, Wald A, Coombs R, et al. Time to establish pillars in point‐of‐care ultrasound. Australasian Journal of Ultrasound Medicine 2019; 22: 12–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization . Coronavirus disease 2019 (COVID‐19) situation report – 52. March 12 2020 https://www.who.int/docs/default-source/coronaviruse/20200312-sitrep-52-covid-19.pdf?sfvrsn=e2bfc9c0_2 (accessed 06/04/2020).
- 7. Bounsenso D, Pata D, Chiaretti A. COVID‐19 outbreak: less stethoscope, more ultrasound. Lancet ‐ Respiratory Medicine 2020. Epub 20 March. doi.org/10.1016/S2213‐2600(20)30120‐X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Buonsenso D, Piano A, Raffaelli F, et al. Point‐of‐care lung ultrasound findings in novel coronavirus disease‐19 pnemoniae: a case report and potential applications during COVID‐19 outbreak. European Review For Medical And Pharmacological Sciences 2020; 24: 2776–80. [DOI] [PubMed] [Google Scholar]
- 9. Corradi F, Via G, Forfori F, et al. Lung ultrasound and B‐lines quantification inaccuracy: B sure to have the right solution. Intensive Care Medicine 2020. Epub 18 March. doi.org/10.1007/s00134‐020‐06005‐6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Moro F, Buonsenso D, Moruzzi M, et al. How to perform lung ultrasound in pregnant women with suspected COVID‐19 infection. Ultrasound in Obstetrics and Gynaecology 2020. Epub 24 March. doi.org/10.1002/uog.22028 [DOI] [PubMed] [Google Scholar]
- 11. Peng Q, Wang X, Zhang L. Findings of lung ultrasonography of novel corona virus pneumonia during the 2019–2020 epidemic. Intensive Care Medicine 2020. Epub 12 March. doi.org/10.1007/s00134‐020‐05996‐6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Poggiali E, Dacrema A, Bastoni D, et al. Can lung US help critical care clinicians in the early diagnosis of novel coronavirus (COVID‐19) pneumonia? Radiology 2020. Epub 13 March. doi.org/10.1148/radiol.2020200847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Soldati G, Smargiassi A, Inchingolo R, et al. Is there a role for lung ultrasound during the COVID‐19 pandemic? Journal of Ultrasound in Medicine 2020. Epub 20 March. doi.org/10.1002/jum.15284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Soldati G, Smargiassi A, Inchingolo R, et al. Proposal for international standardization of the use of lung ultrasound for COVID‐19 patients; a simple, quantitative, reproducible method. Journal of Ultrasound in Medicine 2020; 39: 1413–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Thomas A, Halijan G, Mitra G. Lung ultrasound findings in a 64‐year‐old woman with COVID‐19. Canadian Medical Association Journal 2020. Epub 31 March. doi.org/10.1503/cmaj.200414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Vetrugno L, Bove T, Orso D, et al. Our Italian experience of using lung ultrasound for identification, grading and serial follow‐up of severity of lung involvement for management of patients with COVID‐19. Echocardiography 2020. Epub 1 April. doi.org/10.1111/echo.14664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Djulbegovic B, Guyatt G. Progress in evidence‐based medicine: a quarter century on. Lancet 2017; 390: 415–23. [DOI] [PubMed] [Google Scholar]
- 18. World Health Organisation . WHO Director‐General's statement on IHR Emergency Committee on Novel Coronavirus (2019‐nCoV). 30 January 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov) (accessed 01/04/2020)
- 19. National Institute for Health and Care Excellence . Interim process and methods for developing rapid guidelines on COVID‐19. https://www.nice.org.uk/process/pmg35/chapter/scoping (accessed 29/03/2020).
- 20. National Institute for Health and Care Excellence . COVID‐19 rapid guideline: critical care in adults. https://www.nice.org.uk/guidance/ng159 (accessed 29/03/2020). [PubMed]
- 21. Cook T, El‐Boghdadly K, McGuire B, et al. Consensus guidelines for managing the airway in patients with COVID‐19. Anaesthesia 2020; 75: 785℃799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Public Health England, Guidance COVID‐19: epidemiology, virology and clinical features. Updated 27 March 2020 https://www.gov.uk/government/publications/wuhan-novel-coronavirus-background-information/wuhan-novel-coronavirus-epidemiology-virology-and-clinical-features (accessed 29/03/2020).
- 23. World Health Organisation . Coronavirus disease 2019 (COVID‐19) Situation Report – 41. 1 March 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200301-sitrep-41-covid-19.pdf?sfvrsn=6768306d_2 (accessed 29/03/2020).
- 24. Pan F, Ye T, Sun P, et al. Time course of lung changes of chest CT during recovery from 2019 novel coronavirus (COVID‐19) pneumonia. Radiology 2020. Epub 13 February. doi.org/10.1148/radiol.2020200370 [Google Scholar]
- 25. World Health Organization . Infection prevention and control during health care when COVID‐19 is suspected Interim guidance. 19 March 2020. https://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125 (accessed 01/04/2020)
- 26. Ong SWX, Tan YK, Chia PY, et al. Air, surface, environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) from a symptomatic patient. Journal of the American Medical Association 2020; 323: 1610℃12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Yoon SH, Lee KH, Kim JY, et al. Chest radiographic and CT findings of the 2019 novel coronavirus disease (COVID‐19): analysis of nine patients treated in Korea. Korean Journal of Radiology. 2020; 21: 494–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Intensive Care Society . FUSIC COVID‐19 guidance and resources. 20 March 2020. https://www.ics.ac.uk/ICS/FUSIC/ICS/FUSIC/FUSIC_Accreditation.aspx?hkey=c88fa5cd-5c3f-4c22-b007-53e01a523ce8 (accessed 29/03/2020).
- 29. World Health Organization . Clinical management of severe acute respiratory infection (SARI) when COVID‐19 disease is suspected. Interim guidance, Version 1.2. 13 March 2020. https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected (accessed 06/04/2020).
- 30. NHS England and NHS Improvement . Specialty guides for patient management during the coronavirus pandemic Guidance for the role and use of non‐invasive respiratory support in adult patients with coronavirus (confirmed or suspected). Version 2. 26 March 2020. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/specialty-guide-NIV-respiratory-support-and-coronavirus-v3.pdf (accessed 06/04/2020)
- 31. Via G, Storti E, Gulati G, et al. Lung ultrasound in the ICU: from diagnostic instrument to respiratory monitoring tool. Minerva Anastesiologica 2012; 78: 1282–96. [PubMed] [Google Scholar]
- 32. Lichtenstein D, Mezière G. Relevance of lung ultrasound in the diagnosis of acute respiratory failure. Chest 2008; 134: 117–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bouhemad B, Brisson H, Le‐Guen M, et al. Bedside ultrasound assessment of positive end‐expiratory pressure‐induced lung recruitment. American Journal of Respiratory Critical Care Medicine 2011; 183: 341–7. [DOI] [PubMed] [Google Scholar]
- 34. Rouby J‐J, Arbelot C, Gao Y, et al. Training for lung ultrasound score measurement in critically ill patients. American Journal of Respiratory and Critical Care Medicine 2018; 198: 398–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Gargani L. Ultrasound of the lungs more than a room with a view. Heart Failure Clinics 2019; 15: 297–303. [DOI] [PubMed] [Google Scholar]
- 36. Tusman G, Acosta C, Costantini M. Ultrasonography for the assessment of lung recruitment maneuvers. Critical Ultrasound Journal 2016; 8: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Soummer A, Perbet S, Brisson H, et al. Ultrasound assessment of lung aeration loss during a successful weaning trial predicts post‐extubation distress. Critical Care Medicine 2012; 40: 2064–72. [DOI] [PubMed] [Google Scholar]
- 38. Anderson K, Fields J, Panebianco N, et al. Inter‐rater reliability of quantifying pleural B‐lines using multiple counting methods. Journal of Ultrasound Medicine 2013; 32: 115–20. [DOI] [PubMed] [Google Scholar]
- 39. Frogner B, Fraher E, Spetz J, et al. Modernizing scope‐of‐practice regulations — time to prioritize patients. New England Journal of Medicine 2020; 382: 591–3. [DOI] [PubMed] [Google Scholar]
- 40. Edwards H. Let's all jump on the ultrasound bandwagon: further debate on the use of ultrasound. Ultrasound 2010; 18: 4–7. [Google Scholar]
- 41. Thijssen J, Weijers G, de Korte C. Objective performance testing and quality assurance of medical ultrasound equipment. Ultrasound in Medicine and Biology 2007; 33: 460–71. [DOI] [PubMed] [Google Scholar]


