Venovenous extracorporeal membrane oxygenation (ECMO) has been safely used as invasive mechanical respiratory support for almost 40 years.1 This therapy makes full use of cardiopulmonary bypass (CPB) technologies to take over the respiratory function of the lungs, providing oxygen transport and carbon dioxide removal.
Historically, several factors such as the high-risk profile target population, the complex technical management, and the generalized skepticism affected the widespread adoption of this therapy. Hence, ECMO for refractory respiratory failure became a niche resource limited to small numbers of patients.
Since then, extracorporeal technology has steadily improved: advanced biocompatibility, high-performance oxygenators, optimized circuit designs are all elements that increased the safety and the ease to use this therapy, boosting its reliability among clinicians.2
The spread of swine-origin influenza A (H1N1) virus in 2009 led to a pandemic associated with a large number of patients developing acute respiratory distress syndrome (ARDS), which resulted in an exceptionally increased ECMO case load. That promising experience, followed by studies such as the CESAR trial (efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure), enhanced the usage of ECMO.3,4
COVID-19 and Extracorporeal Oxygenation’s Membrane Lungs
The coronavirus disease 2019 (COVID-19) is an infectious disease caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The disease originated in Wuhan City, China, in December 2019 and has since spread worldwide causing a pandemic that, as of April 2, 2020, counts almost 1 million cases and 50,000 deaths.5
The COVID-19 pandemic ravaged Italy: a dramatic number of deaths have been registered (as of April 2, 2020, 12,550; case fatality rate 11.8%). Data on the characteristics of COVID-19 patients dying in Italy highlight ARDS as acute condition (reasonably leading to the exitus) observed in 96.5% of patients.6
Despite the lack of peremptory knowledge, venovenous ECMO is considered as standard of care for the management of eligible patients with severe COVID-19–related ARDS refractory to conventional treatment in expert centers following WHO/SCCM (Society of Critical Care Medicine) recommendations.7,8 Some studies reporting a few COVID-19 patients treated with ECMO have been published, but based on anecdotal reports, many others are receiving treatment.9–11 However, mortality rates are still high, and proofs of clear benefits are missing.12 On March 24, Extracorporeal Life Support Organization (ELSO) published a guidance document, which is meant to be a general consensus guideline on the use of ECMO in COVID-19 patients.13
Should Clinicians Be Concerned?
Although “ECMO is not a therapy to be rushed to the frontline when all resources are stretched in a pandemic,” as a matter of numbers, it is predictable to expect an important case load of ECMO support during this outbreak.14 Hence, it is essential to address some concerns about the virus-containment safety of the ECMO oxygenator’ membrane. In particular, there are two questions that must be answered: it is fundamental to ascertain whether trace of SARS-CoV-2 is present in blood or not and whether the virus can cross the membrane, get the gas phase, aerosolize, and concur to viral dissemination.
Is SARS-CoV-2 Present in Blood?
To the authors’ knowledge, just a few studies evaluated the biodistribution of SARS-CoV-2.15 Huang et al.16 prospectively collected data on 41 patients with laboratory-confirmed COVID-19. Real-time reverse transcription polymerase chain reaction (RT-PCR) analysis confirmed 6 cases (15%) of viral RNAemia. Zhang et al.17 assessed the presence of viral RNA in blood samples taken from 39 COVID-19 patients by means of quantitative PCR test. Six patients tested blood-positive, and among these, 3 were also serum-positive. Interestingly none of the blood-positive patients were also positive to the oral swab. Finally, Wang et al.18 analyzed 1070 specimens collected from 205 patients with COVID-19 throughout the progress of the illness. Viral RNA was determined in 307 blood specimens by real-time RT-PCR analysis, which resulted positive in 1% of cases. Hence, very limited and controversial data are available, and these suggest a possibility of systemic infection.
Can SARS-CoV-2 Cross the Membrane?
Extracorporeal science history has seen many breakthroughs in terms of oxygenation technology, but arguably one of the most important has been the development of membrane oxygenators, which addressed the huge biocompatibility issues of previous technologies (overcoming the direct blood–air contact) and allowing at the same time high gas-exchange performances. Nowadays, ECMO oxygenators are made of poly-4-methylpentene (PMP) asymmetric membranes with a sponge-like microporous wall and a 0.1-μm-thin dense outer skin that provides the complete separation of blood from gas phase. In contrast with polypropylene (PP), PMP has a 15-fold better oxygen and a 10-fold better carbon dioxide permeability coefficient.19 This close-to-ideal efficiency in terms of gas exchange, together with their homogenous membrane, makes PMP oxygenators reliable and durable devices.
Theoretically, there is no chance that SARS-CoV-2 can move from the bloodstream to the gas phase in a PMP oxygenator and disseminate through the exhaust port. PMP fibers’ physical characteristics should not allow the so-called “plasma leakage”, the presentation of a yellow-colored foam in the gas outlet of the oxygenator, followed by a loss of efficiency. This phenomenon was common with PP membranes, whereas it is rarely observed in modern times ECMO runs. However, rarely does not mean never: as a matter of fact, few reports of plasma leakage with PMP oxygenators have been published.
Puis et al.20 described a case of a young woman who needed immediate oxygenator exchange because of the detection of plasma leakage followed by a fall in performances of two parallel-placed oxygenators. Gill et al.21 reported a case of a 16-month-old boy who required venoarterial ECMO support for acute myocarditis. Plasma leakage started to occur since day 1, and by day 6, it was mandatory to replace the oxygenator.21 Interestingly, in both cases, signs of recurring plasma leakage were detectable very quickly after oxygenator exchange. This particular aspect might rule out an oxygenator-dependent cause highlighting the hypothesis of a hyperacute reaction to the foreign materials of the ECMO system, leading to the deposition of fibrous/cellular deposits on the blood side of the hollow fibers (Central Figure).
Central Figure.
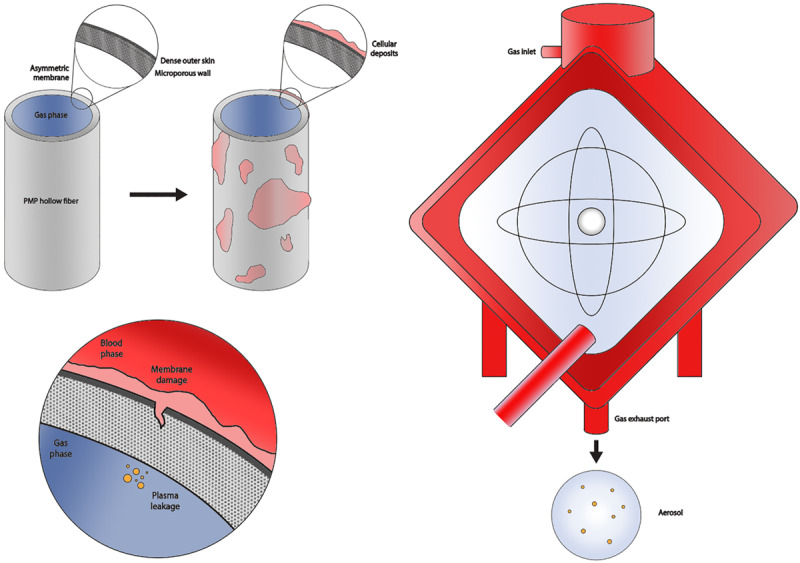
Intact poly-4-methylpentene (PMP) hollow fiber experiencing the deposition of cellular and fibrous remnants causing membrane damage, finally leading to plasma leakage and aerosolization of particles.
Further to this point, Lehle et al.22 demonstrated that deposition of debris during ECMO support is a major factor concurring to oxygenator’s failure: 31 patients with severe ARDS were treated with ECMO; among these, 3 patients required a replacement of the oxygenator after a mean support of 11 ± 7 days. Scanning electron microscopy analysis of the dismantled oxygenator showed abundant areas with “pseudomembrane” formations, which have been further characterized by means of phase-contrast microscopy, emphasizing a significant thickness of about 50% of the fiber itself. Moreover, information on the distribution of these adherent debris pointed out low-flow areas (such as contact zones between neighboring fibers and with the overlying fiber sheet) as more prone to cell deposition.22 It is important to underline that this phenomenon is not just microscopic: an ex vivo analysis of a PMP oxygenator through multidetector computed tomography (MDCT) followed by dissection and direct visualization showed microscopic fibrous-cellular deposits within the gas exchange surface of the membrane oxygenator.23
In addition, it is well known that ECMO breeds pharmacokinetic alterations, which make challenging to adequately administer drugs during the pump run.24 The reason for these alterations is the degradation and sequestration of circulating proteins and protein-bound drugs in the ECMO components, which happen over time in a not fully elucidated manner.25
CPB and COVID-19
As predictable, all scheduled heart surgeries have been postponed in the great majority of institutions because of the COVID-19 emergency. However, cardiac surgery is a practice in which postponing a procedure is not always an option. Thus, clinicians must be prepared to deal with possible infected patients who will need to undergo CPB-assisted heart surgery. CPB oxygenators are usually made of PP membrane that lacks the dense outer skin typical of PMP fibers.19 PP hollow fibers are microporous, and this configuration is historically renowned as vulnerable to plasma breakthroughs during long-term extracorporeal support. The average length of extracorporeal supports in a cardiac surgery setting is greatly shorter as compared with a typical respiratory ECMO, and this makes the occurrence of plasma leakage a hardly ever happening scenario. However, a word of caution is appropriate.
Conclusions
This dissertation seeks to address ECMO clinicians’ concerns regarding the risk of viral dissemination via the oxygenator’s exhaust port. We concluded that it is possible for SARS-CoV-2 to cross the membrane and aerosolize through the gas-exit port of the membrane lung. This phenomenon might be dependent on the presence of viral traces in the bloodstream and on the occurrence of fiber damage, which are both considered rare scenarios.
However, it is reasonable to minimize the risk of viral dissemination and cross contamination: evacuation of the exhaust port of the oxygenator and a strict control for the detection of plasma leakage signs (leading to early oxygenator exchange) are measures that should be taken to prevent spreading of aerosols from the membrane lung.
Further research is needed to better understand SARS-CoV-2 biodistribution over time during the illness, whereas current data appear to be inconsistent. It would also be relevant to investigate the predisposing factors of the acute-phase reaction leading to membrane lung damage. Resources must be optimized in a pandemic, and the dilemma between “doing” and “learning” loudly echoes without an answer. This work highlights that a combined approach is crucial.
Footnotes
Disclosure: The authors have no conflicts of interest to report.
References
- 1.Hill JD, O’Brien TG, Murray JJ, et al. Prolonged extracorporeal oxygenation for acute post-traumatic respiratory failure (shock-lung syndrome). Use of the Bramson membrane lung. N Engl J Med 1972286: 629–634 [DOI] [PubMed] [Google Scholar]
- 2.Kolla S, Awad SS, Rich PB, Schreiner RJ, Hirschl RB, Bartlett RH. Extracorporeal life support for 100 adult patients with severe respiratory failure. Ann Surg 1997226: 544–564; discussion 565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davies A, Jones D, Bailey M, et al. Extracorporeal membrane oxygenation for 2009 influenza A(H1N1) acute respiratory distress syndrome. JAMA 2009302: 1888–1895 [DOI] [PubMed] [Google Scholar]
- 4.Peek GJ, Mugford M, Tiruvoipati R, et al. CESAR trial collaboration: Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): A multicentre randomised controlled trial. Lancet 2009374: 1351–1363 [DOI] [PubMed] [Google Scholar]
- 5. European Centre for Disease Prevention and Control (ECDC) COVID-19 update 2 April 2020. https://
- 6.Characteristics of COVID-19 patients dying in Italy—Report based on data available on March 30, 2020: COVID-19 Surveillance Group, Istituto Superiore di Sanitá.
- 7.WHO: Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected: Interim guidance. 2020. https://apps.who.int/iris/bitstream/handle/10665/330854/WHO-nCoV-Clinical-2020.2-eng.pdf?sequence=1&isAllowed=yWHO/nCoV/Clinical/2020.2. Accessed February 11, 2020.
- 8.Alhazzani W, Hylander Møller M, Arabi YM, et al. Surviving sepsis campaign: Guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Intensive Care Med, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020395: 507–513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir Med 20208: 475–481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hong X, Xiong J, Feng Z, Shi Y. Extracorporeal membrane oxygenation (ECMO): Does it have a role in the treatment of severe COVID-19? Int J Infect Dis 202094: 78–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.ELSO Guidance Document: ECMO for COVID-19 Patients with Severe Cardiopulmonary Failure. https://elso.org.
- 14.MacLaren G, Fisher D, Brodie D. Preparing for the most critically ill patients with COVID-19: The potential role of extracorporeal membrane oxygenation. JAMA, 2020. [DOI] [PubMed] [Google Scholar]
- 15.Chang L, Yan Y, Wang L. Coronavirus Disease 2019: Coronaviruses and blood safety. Transfus Med Rev 2020pii: S0887–7963(20)30014-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020395: 497–506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang W, Du RH, Li B, et al. Molecular and serological investigation of 2019-nCoV infected patients: Implication of multiple shedding routes. Emerg Microbes Infect 20209: 386–389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang W, Xu Y, Gao R, et al. Detection of SARS-CoV-2 in different types of clinical specimens [published online ahead of print, 2020 Mar 11]. JAMA 2020. e203786, doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peinemann KV, Pereira Nunes S. Membranes for the Life Sciences. (2007). Weinheim, Germany, Wiley-VCH Verlag GmbH & Co; KgaA, 2007, Vol 1. [Google Scholar]
- 20.Puis L, Ampe L, Hertleer R. Case report: Plasma leakage in a polymethylpentene oxygenator during extracorporeal life support. Perfusion 200924: 51–52 [DOI] [PubMed] [Google Scholar]
- 21.Gill MC, O’Shaughnessy K, Dittmer J. A paediatric ECMO case of plasma leakage through a polymethylpentene oxygenator. Perfusion 201530: 600–603 [DOI] [PubMed] [Google Scholar]
- 22.Lehle K, Philipp A, Gleich O, et al. Efficiency in extracorporeal membrane oxygenation-cellular deposits on polymethylpentene membranes increase resistance to blood flow and reduce gas exchange capacity. ASAIO J 200854: 612–617 [DOI] [PubMed] [Google Scholar]
- 23.Dornia C, Philipp A, Bauer S, et al. Visualization of thrombotic deposits in extracorporeal membrane oxygenation devices using multidetector computed tomography: A feasibility study. ASAIO J 201359: 439–441 [DOI] [PubMed] [Google Scholar]
- 24.Shekar K, Fraser JF, Smith MT, Roberts JA. Pharmacokinetic changes in patients receiving extracorporeal membrane oxygenation. J Crit Care 201227: 741.e9–741.18 [DOI] [PubMed] [Google Scholar]
- 25.Shekar K, Roberts JA, Mcdonald CI, et al. Sequestration of drugs in the circuit may lead to therapeutic failure during extracorporeal membrane oxygenation. Crit Care 201216: R194. [DOI] [PMC free article] [PubMed] [Google Scholar]


