Abstract
Background:
While a primary goal of anterior cruciate ligament (ACL) reconstruction is to reduce pathologically increased anterior and rotational knee laxity, the relationship between knee laxity after ACL reconstruction and patient-reported knee function remains unclear.
Hypothesis/Purpose:
We hypothesized there would be no significant correlation between the degree of residual anterior and rotational knee laxity and patient-reported outcomes 2 years following primary ACL reconstruction.
Study Design:
Cross-Sectional Study
Methods:
From a prospective multicenter nested cohort of patients, 433 patients under age 36 years injured in sports with no history of concomitant ligament surgery, revision ACL surgery, or surgery of the contralateral knee were identified and evaluated at a minimum 2 years following primary ACL reconstruction. Each patient underwent Lachman and pivot-shift evaluation as well as a KT-1000 assessment along with KOOS and subjective IKDC scores. A proportional odds logistic regression model was used to predict each 2-year patient-reported outcome (PRO) score, controlling for preop score, age, sex, BMI, smoking, Marx activity score, education, subsequent surgery, meniscus and cartilage status, graft type, and range of motion asymmetry. Measures of knee laxity were independently added to each model to determine correlation with PROs.
Results:
Side-to-side manual Lachman differences were IKDC A in 246 (57%) patients, IKDC B in 183 (42%) patients, and IKDC C in 4 (<1%) patients. Pivot-shift was classified as IKDC A in 209 (48%) patients, IKDC B in 183 (42%) patients, and IKDC C in 11 (2.5%) patients. The mean side-to-side KT-1000 difference was 2.0±2.6mm. No significant correlations were noted between pivot-shift or anterior tibial translation as assessed by Lachman or KT-1000 and any PRO. All predicted differences in PROs based on IKDC A versus B pivot-shift and anterior tibial translation were less than 4 points.
Conclusion:
Neither the presence of IKDC A versus B pivot-shift nor increased anterior tibial translation of up to 6 mm are associated with clinically relevant decreases in PROs 2 years following ACL reconstruction.
Key Terms: ACL reconstruction, knee laxity, patient-reported outcomes
Introduction
Anterior cruciate ligament (ACL) tears are a frequent and debilitating injury in a young athletic patient population. Rupture of the ACL results in pathologically increased tibial anterior translation and internal rotation relative to the femur.2 Many patients with ACL tears report feelings of instability in the knee, particularly during cutting and pivoting activities. These abnormal movement patterns also increase the stress borne by other intra-articular structures,3,4 potentially increasing the risk of subsequent meniscus tears, articular cartilage damage, and osteoarthritis.
A primary goal of ACL reconstruction is to reduce pathologically increased anterior and rotational laxity of the knee. Knee laxity in the setting of ACL injury is frequently assessed through the use of physical examination including manual examination (Lachman, anterior drawer, and pivot-shift tests) as well as through more quantitative measures such as the KT-1000. The International Knee Documentation Committee (IKDC) objective evaluation of knee laxity describes knee laxity according to differences in anterior translation relative to the contralateral side: IKDC A (0–2 mm difference), IKDC B (3–5mm difference), IKDC C (6–10mm difference), and IKDC D (greater than 10 mm difference). Rotational laxity is assessed through the pivot-shift as IKDC A (negative), IKDC B (Pivot glide), IKDC C (clunk), and IKDC D (gross). Finally, side to side anterior translation as assessed with the KT-1000 athrometer is classified as IKDC A (−1 to 2 mm difference), IKDC B (3 −5 mm or −3 to −1 mm difference), IKDC C (6–10 mm of less than −3 mm difference), or IKDC D (greater than 10 mm difference).5
In additional to knee laxity, patient-reported outcomes are frequently utilized to assess results of ACL reconstruction. The IKDC subjective score8 and Knee Injury and Osteoarthritis Outcome Score (KOOS)17 are validated, patient-reported outcome tools often used in the ACL-injured population. The IKDC subjective score is a single score, while the KOOS includes five distinct subscales(pain, function in activities of daily living, knee symptoms, sport and recreation function, and knee-related quality of life).
The relationship between degree of knee laxity after ACL reconstruction and patient-reported knee function is not completely clear. Previous work has generally noted poor correlation between residual anterior laxity following ACL reconstruction and patient-reported outcomes,6,7,9,15,20 but none of these studies control for other factors known to influence patient-reported outcomes following ACL reconstruction.21 The relationship between residual rotational knee laxity and patient-reported outcomes following ACL reconstruction may be more significant,10 but has been studied less frequently.
The goal of this study was to evaluate the relationship between the degree of knee laxity (instrumented and physical exam) and patient-reported outcomes (IKDC and KOOS) in a prospective nested cohort of young patients a minimum of 2 years after primary ACL reconstruction. The hypothesis tested was that there would be no significant correlation between the degree of anterior or rotational knee laxity and patient-reported outcomes.
Methods
Patients
From a prospective multicenter cohort of patients who underwent primary ACL reconstruction between 2005 and 2012, a subset of patients (nested cohort) under age 33 years at the time of surgery (under age 36 at follow-up) who were injured in sports with no history of concomitant ligament surgery, subsequent ipsilateral revision ACL surgery, or surgery of the contralateral knee were identified at a minimum 2 years after their ACL reconstruction. From this cohort of 869 eligible patients, 433 patients were recruited to return to their enrolling center between 2 and 3 years after surgery. Reconstruction was performed by one of six experienced surgeons at four institutions. Each institution’s institutional review board approved the study.
Baseline Data Collection
All participants completed questionnaires at enrollment and at the 2-year follow-up to capture demographic variables and patient-reported outcomes including the KOOS,17 IKDC Subjective score,8 and Marx activity score.13 Surgeon-completed questionnaires at the time of surgery documented physical examination, arthroscopic findings, and surgical technique that included graft type and meniscus and cartilage pathology and treatment. Meniscus status was classified as normal, stable meniscus tear without treatment, meniscal repair, or partial meniscectomy. Articular cartilage status was dichotomized according to the modified Outerbridge scale as normal/grade 1 or grade 2, 3, or 4.12,16
Follow-up Data Collection
All 433 patients underwent a physical examination by one of nine independent examiners that included Lachman and pivot-shift evaluation as well as a KT-1000 assessment of anterior knee laxity and measurement of knee range of motion with a goniometer. Examiners were board certified orthopaedic surgeons for evaluation of the Lachman, anterior drawer, and pivot-shift and certified physical therapists for range of motion measurements and KT-1000 testing. The examiners were blinded as to which was the operative knee through the use of a knee sleeve during the examination. Patients also completed patient-reported outcome assessments with KOOS and IKDC subjective scores. Any subsequent ipsilateral knee surgery other than revision ACL reconstruction (which was a study exclusion criterion) was noted.
Statistics
The relationship between laxity measures (KT1000, Lachman, and pivot- shift) and patient-reported outcomes at 2 years postoperative was assessed by utilizing multiple regression modeling. For each of the five KOOS subscales (symptoms, pain, activities of daily living [ADL], sports and recreation, quality of life [QOL]) and the subjective IKDC scores at 2 years, a model was built that included the baseline score, age, sex, BMI, education level, smoking status (never, quit, current), Marx activity scale, graft type (autograft bone-patellar tendon-bone, autograft hamstring, allograft, hybrid autograft + allograft), medial and lateral meniscus treatment (normal, stable untreated tear, repair, resection), articular cartilage grade in the patellofemoral, medial and lateral compartments (normal/grade 1, grades 2/3/4), subsequent surgery (yes/no), side-to-side knee extension difference measured at the 2-year exam (degrees), and age by education interaction. Attempted linear regression on the patient-reported outcome scores resulted in a violation of the normality of residuals; therefore, proportional-odds logistic regression was used.
For each outcome, side-to-side differences in KT-1000, Lachman, and pivot-shift measures were individually added to the baseline model due to the anticipated collinearity between them. Odds ratios, 95% confidence intervals, and p-values were obtained for each physical examination measure. To compensate for multiple comparisons, p-values less than 0.002 were considered statistically significant.
To quantify the magnitude of the relationship between each physical exam measure on patient-reported outcome score (as opposed to the odds-ratio), the linear predictors from the proportional-odds models were transformed back to the scale of the patient-reported outcome. For a given outcome score, each unique value observed in the sample was multiplied by the predicted probability that the patient’s score equals that value, which produced a weighted average. These transformed scores were evaluated by cross-validation.
For each model, 10-fold cross validation was carried out to obtain out-of-sample predictions for every patient. This methodology randomly splits the data into 10 non-overlapping sets, and, then, for each of the 10 sets, fits a model on 9 of the 10 sets and gets predicted values on the set that was left out. This method was repeated for all 10 partitions, so each patient got a prediction based on a model that it was not used to create. Scatter plots were then made of the observed KT-1000 value versus cross-validated predicted patient-reported outcome scores, and box plots were made of the predicted scores for each Lachman and pivot-shift value.
Results
The 433 study participants included 210 males (48.5%) and 223 females (51.5%) with a mean age at follow-up of 22.7 ± 4.9 years (range: 15 to 35 years). Meniscus and cartilage status at the time of ACL reconstruction and other demographic data are reported in Table 1. ACL reconstruction with hamstring autograft was performed in 149 patients (34.4%), patellar tendon autograft in 262 patients (60.5%), allograft in 9 patients (2.1%) and hybrid allograft + autograft in 13 patients (3.0%). Fifty-four patients (12.5%) underwent additional surgery on the index knee prior to follow-up.
Table 1:
Baseline Patient and Injury Data
| Age (Mean ± St Dev) | 22.7 ± 4.9 years |
| Sex | |
| Male | 210 (48.5%) |
| Female | 223 (51.5%) |
| Body Mass Index (Mean ± St Dev) | 25.5 ± 4.6 kg/m2 |
| Smoking Status | |
| Current | 26 (6.0%) |
| Quit | 40 (9.2%) |
| Never smoked | 366 (84.5 %) |
| Unknown | 1 (0.2%) |
| Years of Education (Mean ± St Dev) | 12.3 ± 3.2 |
| Marx activity level (Median and IQR) | 12 (8–16) |
| Medial meniscus | |
| Normal | 267 (61.7%) |
| Stable Untreated tear | 39 (9.0%) |
| Repair | 88 (20.3%) |
| Partial Meniscectomy | 39 (9.0%) |
| Lateral meniscus | |
| Normal | 198 (45.7%) |
| Stable Untreated tear | 66 (15.2%) |
| Repair | 32 (7.4%) |
| Partial Meniscectomy | 137 (31.6%) |
| Patellofemoral Compartment Cartilage | |
| Normal / Grade 1 | 416 (96.1%) |
| Grade 2, 3, or 4 | 17 (3.9%) |
| Lateral Compartment Cartilage | |
| Normal / Grade 1 | 381 (88.0%) |
| Grade 2, 3, or 4 | 52 (12.0%) |
| Medial Compartment Cartilage | |
| Normal / Grade 1 | 395 (91.2%) |
| Grade 2, 3, or 4 | 38 (8.8%) |
| Graft Type | |
| Patellar tendon autograft | 262 (60.5%) |
| Hamstring tendon autograft | 149 (34.4%) |
| Allograft | 22 (5.1%) |
Side-to-side manual Lachman differences were IKDC A (0–2 mm) in 246 (57%) patients, IKDC B (3–5 mm) in 183 (42%) patients, and IKDC C (6–10 mm) in 4 (<1%) patients. Pivot-shift was classified as IKDC A in 209 (48%) patients, IKDC B in 183 (42%) patients, IKDC C in 11 (2.5%) patients, and could not be obtained due to guarding in 30 (7%) patients. The mean side-to-side KT-1000 difference was 2.0 ± 2.6 mm. The side-to-side KT-1000 difference was classified as IKDC A (−1 to 2mm) in 178 patients, (41.1%), IKDC B (2 to 6mm or −3 to −1mm) in 214 patients (49.4%), IKDC C (6 to 10 mm or < −3mm) in 37 patients (8.5%), and IKDC D (>10mm) in 2 patients (0.5%). The mean side-to-side knee extension difference was 0.7 ± 2.6 degrees.
The mean, unadjusted KOOS subscales and IKDC subjective scores were generally similar based on postoperative knee laxity as assessed by physical examination (Tables 2, 3, and 4), with the exception of the KOOS QOL subscale for IKDC C classified patients on the Lachman, which was notably lower. However, there were an insufficient number of patients with IKDC laxity (particularly Lachman) to perform a meaningful analysis of these patients. Evaluation of those patients with IKDC anterior laxity as assessed by KT-100 demonstrated no clinically relevant differences (Table 4). Distributions of the instrumented side-to-side anterior laxity measurements are shown in Figure 2.
Table 2 –
Lachman Examination at 2-year follow-up
| Side-to-side Lachman | |||
|---|---|---|---|
| 0–2 mm (IKDC A) n = 246 |
3–5 mm (IKDC B) n = 183 |
6–10mm (IKDC C) n = 4 |
|
| IKDC Subjective | 88.3 ± 10.8 | 89.1 ± 10.4 | 83.6 ± 8.4 |
| KOOS Symptoms | 87.8 ± 10.6 | 87.5 ± 10.5 | 85.7 ± 15.2 |
| KOOS Pain | 93.3 ± 8.5 | 93.7± 7.5 | 93.1± 10.5 |
| KOOS ADL | 97.7 ± 5.4 | 97.8 ± 4.2 | 100 ± 0 |
| KOOS Sport/Rec | 86.2 ± 15.0 | 89.6 ± 12.0 | 81.2 ± 12.5 |
| KOOS QOL | 78.7 ± 16.4 | 81.4 ± 16.5 | 56.2 ± 18.4 |
Table 3 –
Pivot-Shift Examination at 2-year follow-up
| Pivot-Shift Grade | |||
|---|---|---|---|
| None (IKDC A) n = 209 |
Glide (IKDC B) n = 183 |
Clunk (IKDC C) n = 11 |
|
| IKDC Subjective | 88.1 ± 10.4 | 89.0 ± 11.0 | 90.2 ± 10.6 |
| KOOS Symptoms | 87.9 ± 10.4 | 87.7 ± 11.0 | 83.8 ± 9.9 |
| KOOS Pain | 93.3 ± 7.9 | 93.8 ± 8.3 | 90.9 ± 10.3 |
| KOOS ADL | 97.6 ± 4.9 | 97.9 ± 5.1 | 97.0 ± 6.7 |
| KOOS Sport/Rec | 86.4 ± 15.0 | 88.9 ± 12.7 | 90.4 ± 10.8 |
| KOOS QOL | 79.0 ± 17.4 | 80.9 ± 15.6 | 80.7 ± 12.3 |
Table 4 –
KT-1000 at 2-year follow-up
| Side-to-side KT-1000 Difference | |||
|---|---|---|---|
| −1 to 2 mm (IKDC A) n = 178 |
3 to 5 mm or −3 to −1mm (IKDC B) n = 214 |
6 to 10mm or less than −3mm (IKDC C) n = 37 |
|
| IKDC Subjective | 88.8 ± 10.0 | 88.4 ± 12.1 | 85.9 ± 12.3 |
| KOOS Symptoms | 87.8 ± 10.9 | 87.2 ± 11.5 | 86.0 ± 10.7 |
| KOOS Pain | 93.8 ± 7.7 | 93.0± 9.9 | 91.6 ± 10.0 |
| KOOS ADL | 97.7 ± 4.9 | 97.4 ± 7.9 | 97.1 ± 5.3 |
| KOOS Sport/Rec | 86.8 ± 14.2 | 87.7 ± 14.9 | 88.9 ± 12.0 |
| KOOS QOL | 80.6 ± 16.4 | 78.9 ± 17.3 | 76.9 ± 16.8 |
Figure 2:

KT Histogram
When patient demographic and surgical variables controlled for in the proportional odds logistic regression models, the presence of an IKDC B pivot-shift did not correlate with significantly increased odds of having lower patient-reported outcomes scores relative to patients with IKDC A pivot-shift. Similarly, increased anterior tibial translation with Lachman or KT-1000 testing did not correlate with significantly increased odds of lower patient-reported outcomes scores.
Predicted patient-reported outcome scores based anterior tibial translation assessed with KT-1000 (Figure 3) and Lachman testing (Figure 4) and rotational laxity as assessed with the pivot-shift (Figure 5) were calculated. All predicted differences in score based on IKDC A versus B pivot-shift and anterior tibial translation were less than 4 points (not clinically significant as the clinically relevant difference in these patient-reported outcome score is 10).22
Figure 3:

Predicted KT
Figure 4:
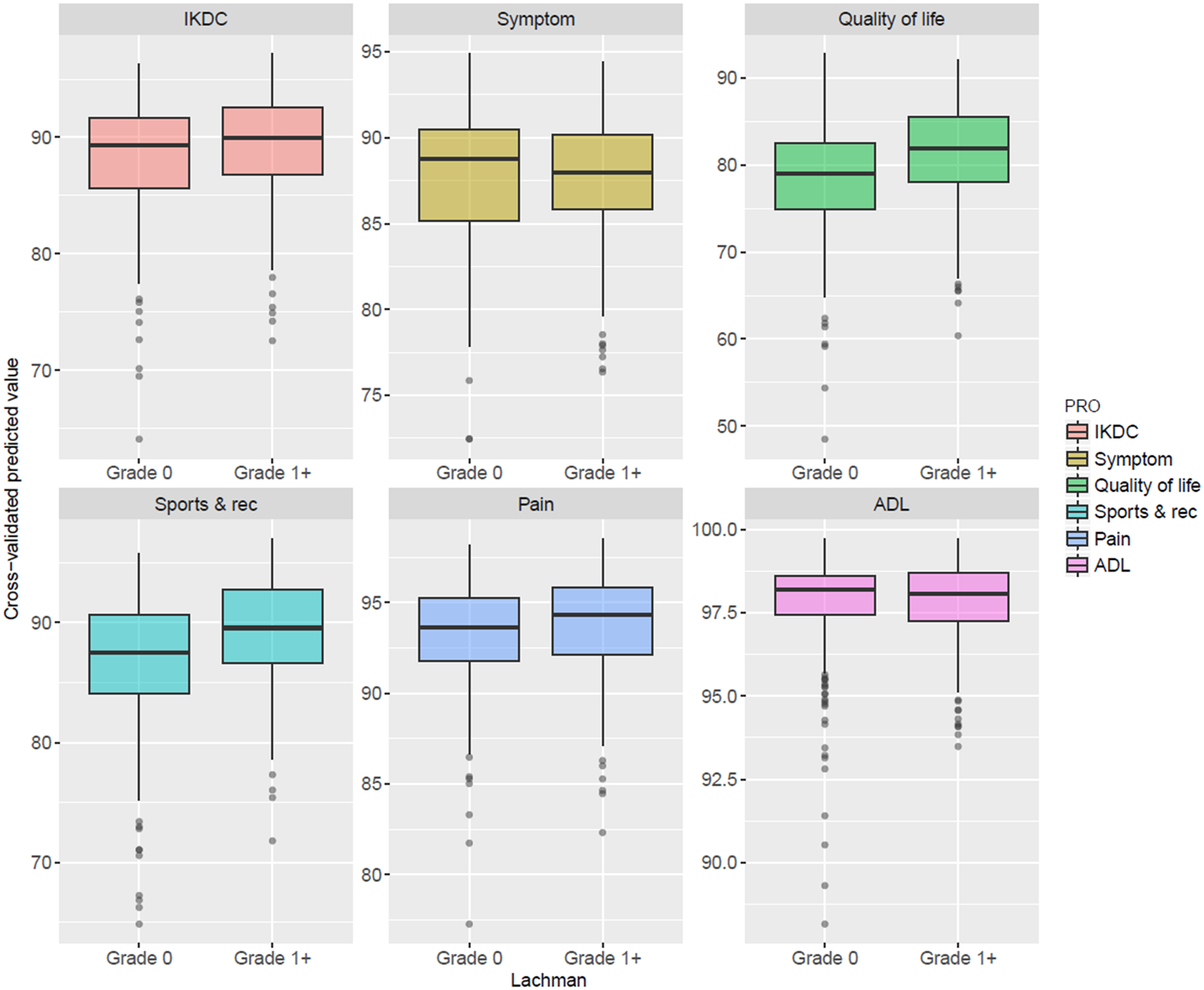
Lachman testing
Figure 5:

rotational laxity as assessed with the pivot-shift
Discussion
The most important findings of this study are that when controlling for patient and surgical factors, mildly increased anterior (KT1000) or rotational laxity (IKDC B versus IKDC A) are not associated with clinically relevant decreases in patient-reported outcome scores in young, active patients 2 years following ACL reconstruction.
These findings are consistent with prior literature that has routinely failed to identify any clinically relevant or statistically significant correlations between patient-reported outcome scores and moderately increased anterior knee laxity. In the late 1990s and early 2000s, Hrubesch et el,6 Hyder et al,7 Muneta et al,15 Sernert et al,20 and Kocher et al10 published series of 44, 62, 97, 527, and 202 patients that identified no correlation between residual anterior knee laxity and patient-reported outcomes following ACL reconstruction. Muneta et al did identify several objective findings that did correlate with patient-reported outcome, most notably failure to regain full knee extension and persistent quadriceps weakness relative to the contralateral side.15 None of these studies specifically controlled for other patient and surgical factors in their analyses.
The influence of greater degrees of anterior knee laxity in outcome scores is less clear. In 2002 Sernert et al. noted poorer Lysholm scores in patients with residual anterior laxity greater than 6 mm on Lachman examination.19 In the current series, the ability to address this question is limited given that only 4 patients had an IKDC C Lachman and none had an IKDC D Lachman. A larger number of patients (39) did demonstrate IKDC grade C anterior laxity when utilizing KT-1000 testing. These patients did not demonstrate clinically relevant differences in PRO’s compared to the IKDC A and B groups (Table 4) and no statistically significant differences between side to side KT-1000 measurements and PRO’s were noted in the proportional odds logistic regression model. Many authors have defined the presence of a side-to-side difference in anterior translation of greater than 6 mm (IKDC C or D) as indicative of graft failure.18 The longer-term effects of persistent anterior laxity of this magnitude remain unknown, although it is likely that the resultant increased articular cartilage loads would increase risk of osteoarthritis with time.1,3,4
Fewer published studies evaluate the correlation between postoperative pivot-shift and patient-reported outcomes of ACL reconstruction. In a 2004 retrospective study, Kocher et al. noted a correlation between postoperative pivot-shift and Lysholm score.10 Patients with a pivot glide (IKDC B) demonstrated lower scores than those with no pivot shift (IKDC A), while those with a clunk (IKDC C) demonstrated poorer scores than the other 2 groups. It should be noted that this series also included relatively few patients (13 of 202, 2%) with an IKDC grade C pivot-shift. In the current series (in contrast), no differences in any patient-reported outcome scores were noted based on IKDC pivot-shift grade B versus A. The number of patients with IKDC grade C pivot-shifts was too low for meaningful conclusions. The reason for the different findings in these demographically similar cohorts is not completely clear, but may related to controlling for confounding variables.
There are limitations of this study. First, the patient population included in the study is not representative of all patients undergoing ACL reconstructions. While the patient demographics and activity level are typical for ACL tears, this group only reflects those patients who have not suffered a subsequent ipsilateral or contralateral ACL reconstruction in the first 2 years postoperative. We therefore cannot comment as to any relationship between increased postoperative knee laxity and risk of re-injury or contralateral injury. In addition, we only performed on site evaluation in approximately one half of the patients who met inclusion criteria. This limitation is mitigated by the fact that the remaining patients who did not come back for did provide information regarding repeat surgery and patient-reported outcomes. No significant differences between this group and the patients who underwent on site evaluation were noted in regards to patient demographics or patient-reported outcomes, suggesting that the patients included in the study are representative of the entire eligible group. Further, the length of follow-up in the study is only 2 years. While important, these relatively short-term outcome data do not allow for analysis of any impact of postoperative laxity on the subsequent development of post-traumatic osteoarthritis or long-term declines in knee function or increases in pain. In a 2009 study, Möller et al. compared patient-reported outcomes of 2 groups of patients at 11.5 years following ACL reconstruction based whether their anterior laxity at two years post-operative was less than 3 mm (33 patients) or greater than 3 mm (23 patients).14 They noted no difference between the groups although it was not clear how many (if any) patients in the high laxity group exhibited laxity greater than 6 mm. These data indicate that relatively small degrees of increased anterior laxity does not lead to clinically important declines in function up to 10 years postoperative. While the presence of a high-grade pivot-shift postoperatively has been associated with an increased risk of the development of osteoarthritis 5–9 years following ACL reconstruction,9 no data are available regarding the impact of a persistent low-grade pivot-shift on long-term outcomes of ACL reconstruction.11 Finally, given that different examiners performed the independent evaluations at each institution, we were not able to definitively assess inter-rater reliability of the physical examination tests among different examiners. Although the IKDC classification system was utilized by all raters, the Lachman and pivot-shift grading represent subjective assessments by the examiners rather than quantitative measures.
This study’s strengths are in its large numbers (n=433), prospective nested cohort study design, and multivariable analysis that controls for potential confounding factors associated with or hypothesized to IKDC and/or KOOS such as increased anterior laxity including age, sex, graft type, and extension loss.
Conclusion
Neither the presence of IKDC A versus B pivot-shift nor increased anterior tibial translation of up to 6 mm compared to the contralateral side are not correlated with clinically relevant decreases in IKDC and KOOS 2 years following primary ACL reconstruction.
Figure 1:

STROBE Diagram
What is known about the subject?
The relationship between residual anterior and rotational knee laxity is not clear in the literature. While some studies have evaluated the relationship between anterior tibial translation and patient-reported outcomes and noted minimal correlation, these studies have not controlled for other factors known to affect patient-reported outcomes. Data describing the relationship between residual rotational laxity and patient-reported outcomes are sparse.
What this study adds to existing knowledge?
This study is the first to clearly demonstrate no detrimental effects of small degrees of residual anterior and rotational laxity (IKDC B) on patient-reported outcomes following ACL reconstruction utilizing prospective data collection and controlling for other factors that can influence PROs.
Contributor Information
MOON Knee Group:
Jack T. Andrish, Charles L. Cox, Warren R. Dunn, David C. Flanigan, Timothy Hewett, Morgan H. Jones, Christopher C. Kaeding, Dawn Lorring, Matthew J. Matava, Richard D. Parker, Angela Pedroza, Emily Preston, Brian Richardson, Bettina Schroeder, Matthew V. Smith, and Rick W. Wright
References
- 1.Amano K, Pedoia V, Su F, Souza RB, Li X, Ma CB. Persistent Biomechanical Alterations After ACL Recontsruction Are Associated With Early Cartilage Matrix Changes Detected by Quantitative MR. Orthop J Sports Med. 2016. April 28;4(4):2325967116644421. doi: 10.1177/2325967116644421. eCollection 2016 Apr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amis AA. The functions of the fibre bundles of the anterior cruciate ligament in anterior drawer, rotational laxity and the pivot shift. Knee Surg Sports Traumatol Arthrosc. 2012;20(4):613–620. [DOI] [PubMed] [Google Scholar]
- 3.Arner JW, Irvine JN, Zheng L, et al. The Effects of Anterior Cruciate Ligament Deficiency on the Meniscus and Articular Cartilage: A Novel Dynamic In Vitro Pilot Study. Orthop J Sports Med. 2016;4(4):2325967116639895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Culvenor AG, Perraton L, Guermazi A, et al. Knee kinematics and kinetics are associated with early patellofemoral osteoarthritis following anterior cruciate ligament reconstruction. Osteoarthritis Cartilage. 2016;24(9):1548–1553. [DOI] [PubMed] [Google Scholar]
- 5.Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1(3–4):226–234. [DOI] [PubMed] [Google Scholar]
- 6.Hrubesch R, Rangger C, Reichkendler M, Sailer RF, Gloetzer W, Eibl G. Comparison of score evaluations and instrumented measurement after anterior cruciate ligament reconstruction. Am J Sports Med. 2000;28(6):850–856. [DOI] [PubMed] [Google Scholar]
- 7.Hyder N, Bollen SR, Sefton G, Swann AC. Correlation between Arthrometric evaluation of knees using KT 1000 and Telos stress radiography and functional outcome following ACL reconstruction. Knee. 1997;4(3):121–124. [Google Scholar]
- 8.Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29(5):600–613. [DOI] [PubMed] [Google Scholar]
- 9.Jonsson H, Riklund-Ahlstrom K, Lind J. Positive pivot shift after ACL reconstruction predicts later osteoarthrosis: 63 patients followed 5–9 years after surgery. Acta Orthop Scand. 2004;75(5):594–599. [DOI] [PubMed] [Google Scholar]
- 10.Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ. Relationships between objective assessment of ligament stability and subjective assessment of symptoms and function after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32(3):629–634. [DOI] [PubMed] [Google Scholar]
- 11.Lie DT, Bull AM, Amis AA. Persistence of the mini pivot shift after anatomically placed anterior cruciate ligament reconstruction. Clin Orthop Relat Res. 2007;457:203–209. [DOI] [PubMed] [Google Scholar]
- 12.Marx RG, Connor J, Lyman S, et al. Multirater agreement of arthroscopic grading of knee articular cartilage. Am J Sports Med. 2005;33(11):1654–1657. [DOI] [PubMed] [Google Scholar]
- 13.Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29(2):213–218. [DOI] [PubMed] [Google Scholar]
- 14.Möller E, Weidenhielm L, Werner S. Outcome and knee-related quality of life after anterior cruciate ligament reconstruction: a long-term follow-up. Knee Surgery Sports Traumatology Arthroscopy. 2009;17(7):786–794. [DOI] [PubMed] [Google Scholar]
- 15.Muneta T, Sekiya I, Ogiuchi T, Yagishita K, Yamamoto H, Shinomiya K. Objective factors affecting overall subjective evaluation of recovery after anterior cruciate ligament reconstruction. Scand J Med Sci Sports. 1998;8(5 Pt 1):283–289. [DOI] [PubMed] [Google Scholar]
- 16.Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43-B:752–757. [DOI] [PubMed] [Google Scholar]
- 17.Roos EM, Toksvig-Larsen S. Knee injury and Osteoarthritis Outcome Score (KOOS) - validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes. 2003;1:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Samitier G, Marcano AI, Alentorn-Geli E, Cugat R, Farmer KW, Moser MW. Failure of Anterior Cruciate Ligament Reconstruction. Arch Bone Jt Surg. 2015;3(4):220–240. [PMC free article] [PubMed] [Google Scholar]
- 19.Sernert N, Kartus J, Kohler K, Ejerhed L, Brandsson S, Karlsson J. Comparison of functional outcome after anterior cruciate ligament reconstruction resulting in low, normal and increased laxity. Scandinavian Journal of Medicine & Science in Sports. 2002;12(1):47–53. [DOI] [PubMed] [Google Scholar]
- 20.Sernert N, Kartus J, Kohler K, et al. Analysis of subjective, objective and functional examination tests after anterior cruciate ligament reconstruction. A follow-up of 527 patients. Knee Surg Sports Traumatol Arthrosc. 1999;7(3):160–165. [DOI] [PubMed] [Google Scholar]
- 21.Spindler KP, Huston LJ, Wright RW, et al. The prognosis and predictors of sports function and activity at minimum 6 years after anterior cruciate ligament reconstruction: a population cohort study. Am J Sports Med. 2011;39(2):348–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wright RW. Knee injury outcomes measures. J Am Acad Orthop Surg. 2009;17(1):31–39. [DOI] [PubMed] [Google Scholar]


