Abstract
Objectives:
Although inadequate health literacy has been shown to impact health outcomes in other cancers, little is known about its impact in head and neck cancer (HNC). This study aimed to determine the prevalence and predictors of inadequate health literacy and evaluate the association between health literacy and quality of life (QOL) in HNC survivors.
Methods:
We conducted a retrospective analysis of HNC survivors evaluated in a multidisciplinary HNC survivorship clinic. Survivors had to be ≥1-year postcompletion of treatment to be included in the analysis. Health literacy was assessed via self-report with the Brief Health Literacy Screen (score <10 indicating inadequate health literacy), and QOL was measured using the University of Washington QOL questionnaire. Linear regression with robust standard errors was utilized to evaluate the association between health literacy and QOL.
Results:
Of the 218 survivors evaluated, 13.8% (n = 30) demonstrated inadequate health literacy. After adjusting for age, marital status, site, stage, treatment modality, and years since treatment completion, social-emotional QOL scores for survivors with adequate health literacy were estimated to be 10.67 points higher than those with inadequate health literacy (P = .013). Health literacy was not significantly associated with physical QOL after adjusting for covariates (P = .130).
Conclusion:
Inadequate health literacy is associated with a lower social QOL in HNC survivors, and among those with inadequate health literacy, interventions to ameliorate the impact on QOL are needed.
Keywords: Head and neck cancer, health literacy, survivorship, quality of life
INTRODUCTION
The majority of patients with head and neck cancer (HNC) present with regionally advanced disease,1,2 which necessitates multimodal therapy.3 Consequently, patients are presented with complex treatment options and must understand and appreciate the potential treatment sequelae fully in order to participate in shared decision making and informed consent. Although aggressive treatment regimens have resulted in improved survival,2,4 especially for those with human papillomavirus (HPV)-associated HNC,5 this increased survival comes at a cost to the survivors’ functional capacity and physical health. As the intensity of standard therapy amplifies, survivors experience a substantial increase in acute and late treatment-related toxicities.6,7 HNC survivors not only suffer the physical burden of cancer and its treatment (e.g., impaired swallowing, speech, and musculoskeletal function) but also experience significant psychological (e.g., depression) and social (e.g., unemployment) burdens.8–10
Health literacy is defined as an individual’s ability to obtain, process, and understand basic health information and services needed in order to make appropriate health decisions.11
Patients need to know when and from whom to seek care, as well as to understand health forms and consents and implement written and verbal instructions to manage their healthcare effectively. In the United States, it is estimated that only 12% of adults have proficient health literacy, whereas 14% of the population have below basic health literacy.12 To date, two studies have evaluated the prevalence of inadequate health literacy in HNC patients. One study evaluated 60 HNC and 30 lung cancer patients and found the prevalence of inadequate and marginal health literacy was approximately 12%, with no difference observed in the mean literacy scores between the two cancer types.13 The other study, which was of eight laryngology patients, reported that one-third of subjects had inadequate literacy.14
Adults with low health literacy demonstrate limited ability to interpret health information and to adhere to prescribed medications and treatment regimes.15 Furthermore, literacy level can impact hospital utilization and healthcare costs.16 Previous studies have demonstrated that patients with inadequate health literacy are more likely to utilize emergency and inpatient care services than those with adequate health literacy.17–20 Consequentially, patients with inadequate health literacy also bear an increased burden of healthcare cost. A study of 92,739 veterans found the average cost per patient for those with inadequate or marginal health literacy was significantly higher than for those with adequate literacy. The study estimated that the 3-year cost of care for these patients was $143 million more than for their counterparts.21 Health status has also been linked to literacy levels. Among elderly Medicare patients, health literacy was directly associated with perceived health status, and lower literacy was related to worse self-rated health status.19 Most significantly, inadequate health literacy can contribute to higher mortality.17,22 A prospective cohort study of 3,260 adults enrolled in Medicare found that inadequate health literacy independently predicted all-cause mortality.
Research evaluating literacy and health outcomes among cancer patients is limited. The majority of this research focuses on the utilization of preventive care and recommended screenings.23,24 There have been limited studies evaluating the effects of health literacy on quality of life (QOL) among cancer patients. Of the few studies published, the results have been mixed. In a study of adult cancer patients in an outpatient setting, limited literacy was not found to be a risk factor for poorer QOL.25 However, a study of adult patients newly diagnosed with lung, prostate, breast, or colorectal cancer demonstrated that health literacy was positively and independently associated with health-related QOL.26 To date, none of the studies have evaluated the association between health literacy and quality of life in HNC patients. The purpose of this study was to 1) determine the prevalence and predictors of inadequate health literacy, and 2) evaluate the association between health literacy and QOL in HNC survivors.
MATERIALS AND METHODS
We conducted a retrospective analysis of adult (≥18 years) survivors of HNC who completed questionnaires on health literacy and QOL as part of their clinical evaluation. Survivors evaluated in this analysis were seen in an outpatient, multidisciplinary HNC, survivorship clinic from August 2017 to November 2018. To be included in the analysis, survivors had to have completed primary treatment for squamous cell carcinoma of the oral cavity, oropharynx, or larynx/hypopharynx at least 1 year prior to their survivorship clinic visit. Survivors with a history of recurrence, second primaries, or distant metastasis were excluded. See Figure 1 for the Consolidated Standards of Reporting Trials diagram. This study was approved by the University of Pittsburgh Institutional Review Board.
Fig. 1.
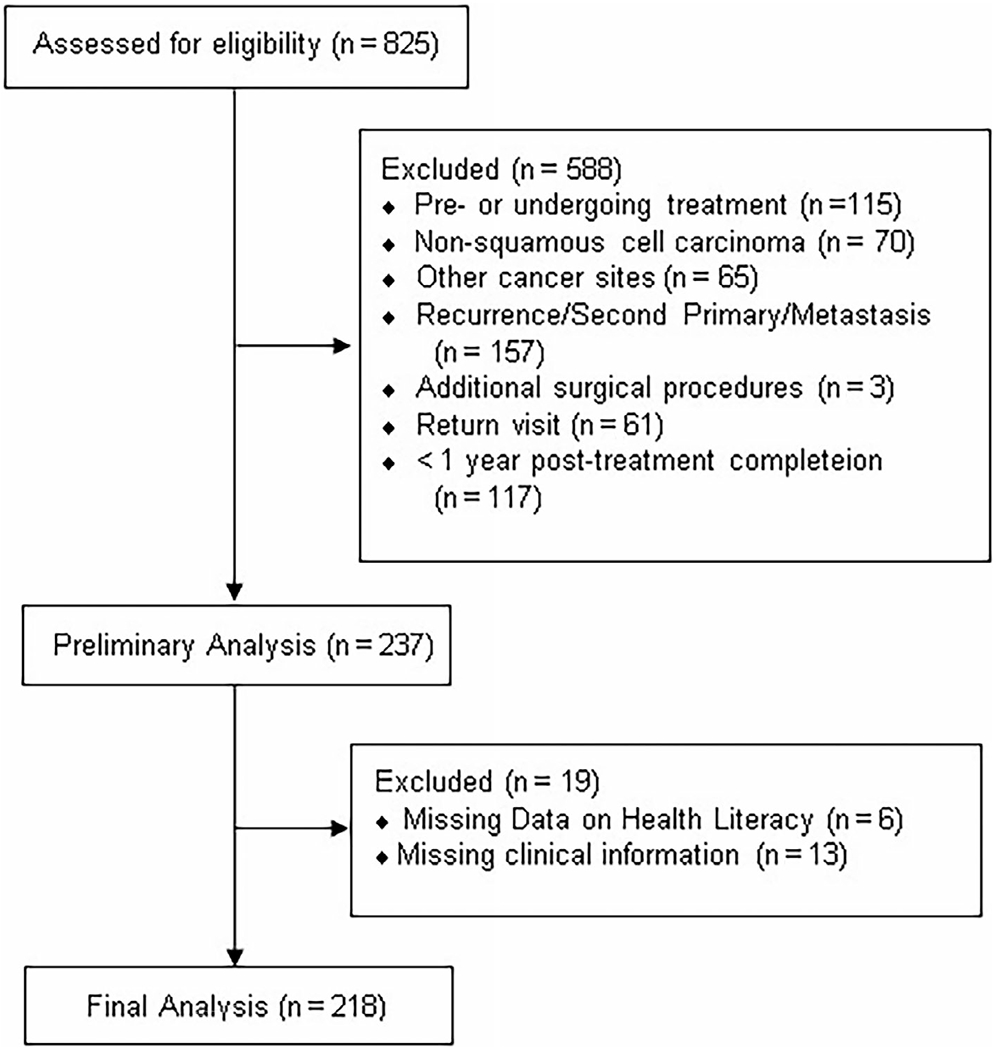
Consolidated Standards of Reporting Trials Flow diagram.
Demographics and Clinical Characteristics
Demographics assessed in this study included age, gender, marital status, and race. Clinical characteristics evaluated comprised primary tumor site (i.e., oral cavity, oropharynx, and laryngopharynx), HPV status for oropharyngeal cancer, tumor histology, American Joint Committee on Cancer (AJCC) 7th edition, treatment administered (i.e., nonsurgical treatment, surgery alone, or surgery with adjuvant treatment), and time since treatment completion.
Health Literacy
The Brief Health Literacy Screen (BHLS) is a three-item questionnaire designed to detect patients with suboptimal health literacy rapidly.27 The BHLS questions are as follows:
How confident are you filling out medical forms by yourself?
How often do you have someone help you read hospital materials?
How often do you have problems learning about your medical condition because of difficulty understanding written information?
Responses to each of the three questions are measured on a 5-point Likert scale. Scores from each question are summated, resulting in a total score ranging from 3 to 15. A cumulative score of 9 or less indicates an inadequate level of health literacy.27,28 Prior work demonstrated that the BHLS correlated with the Short Test of Functional Health Literacy in Adults (STOFHLA) and Rapid Estimate of Adult Literacy in Medicine.28 However, compared to these other questionnaires, the BHLS can be completed rapidly (<1 minute). The BHLS has also been utilized in a variety of research and clinical settings to measure health literacy.29–32
Quality of Life
QOL was measured using the University of Washington Quality of Life Scale (UWQOL) version 4. The UWQOL consists of 12 questions with response options ranging from 3 to 6 choices. Each set of response options is scaled evenly from 0 to 100. The domains are pain, appearance, activity, recreation, swallowing, chewing, speech, shoulder, taste, saliva, mood, and anxiety. The physical subscale score is computed as an average of six domain scores, which include chewing, swallowing, speech, taste, saliva, and appearance. The social–emotional subscale score is an average of anxiety, mood, pain, activity, recreation, and shoulder function. For both subscales, potential scores range from 0 to 100; with higher scores denoting better QOL.33,34
Statistical Analysis
All statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC). In the descriptive analysis, mean and standard deviation (SD) were calculated for continuous variables, whereas frequency and percentage were computed for categorical variables. Comparisons of demographics and clinical characteristics between literacy groups were examined using chi-square test (Fisher’s exact test if sample size was too small) for categorical variables, and two-sided t test (Kruskal-Wallis test if normality assumption was not satisfied) for continuous variables. Linear regression with robust standard errors was performed to analyze the association between QOL (physical and social–emotional subscales) and health literacy (inadequate or adequate), after adjusting for age (years), marital status (dichotomous), site, stage, treatment modality, and years since treatment completion.
RESULTS
Demographics and Clinical Characteristics
The majority of patients were white (92.7%, n = 202), married (72.0%, n = 157), and male (76.6%, n = 167), with a mean age of 64.8 years [range: 29–86 years; SD = 9.84]. The most common primary tumor site was oropharynx (46.8%, n = 102), followed by oral cavity (28.9%, n = 63) and larynx/hypopharynx (24.3%, n = 53). Most patients (75.7%, n = 165) had advanced stage (i.e., AJCC stage III–IV) cancer at the time of diagnosis. Of the 218 survivors, 54 (24.8%) underwent surgical intervention alone; 84 (38.5%) patients received nonoperative therapy; and 80 (36.7%) underwent surgical intervention and received adjuvant therapy. The mean time from treatment completion was 6.5 years (range 1 to 39 years, SD = 5.74) (see Table I).
TABLE I.
Demographics and Clinical Characteristics for the Whole Group and by Health Literacy Level
| Variables | Total (N = 218) | Inadequate Health Literacy (n = 30) | Adequate Health Literacy (n = 188) | P Value |
|---|---|---|---|---|
| Age (years), mean ± SD | 64.8 ± 9.8 | 64.8 ± 10.2 | 64.7 ± 9.8 | 0.961 |
| Gender | ||||
| Male, n (%) | 167 (76.6) | 23 (76.7) | 144 (76.6) | 0.993 |
| Female, n (%) | 51 (23.4) | 7 (23.3) | 44 (23.40 | |
| Marital status | ||||
| Married, n (%) | 157 (72.0) | 21 (70.0) | 136 (72.3) | 0.790 |
| Divorced/widowed/single, n (%) | 61 (28.0) | 9 (30.0) | 52 (27.7) | |
| Race | ||||
| White, n (%) | 202 (92.7) | 28 (93.3) | 174 (92.5) | >0.999* |
| Other, n (%) | 16(7.3) | 2 (6.7) | 14 (7.5) | |
| Tumor site | ||||
| Oral cavity, n (%) | 63 (28.9) | 9 (30.0) | 54 (28.7) | 0.913 |
| Oropharynx, n (%) | 102 (46.8) | 13 (43.3) | 89 (47.3) | |
| Larynx/hypopharynx, n (%) | 53 (24.3) | 8 (26.7) | 45 (23.9) | |
| AJCC stage | ||||
| Tis-II†, n (%) | 53 (24.3) | 5 (16.7) | 48 (25.5) | 0.364* |
| III-IV, n (%) | 165 (75.7) | 25 (83.3) | 140 (74.5) | |
| Treatment | ||||
| Nonoperative, n (%) | 84 (38.5) | 11 (36.7) | 73 (38.8) | |
| Surgery alone, n (%) | 54 (24.8) | 4 (13.3) | 50 (26.6) | 0.170 |
| Surgery + adjuvant, n (%) | 80 (36.7) | 15 (50.0) | 65 (34.6) | |
| Time since treatment completion (years) mean ± SD | 6.47 ± 5.7 | 5.03 ± 3.6 | 6.70 ± 6.0 | .218‡ |
For categorical variables, P value was calculated using chi-square test.
For continuous variables, P value was calculated using t test.
Fisher’s exact test.
Tis = 2.
Kruskal-Wallis test.
AJCC = American Joint Committee on Cancer; SD = standard deviation.
Health Literacy
The mean total health literacy score was 12.78 (SD = 2.65, range = 4–15). A total of 13.8% (n = 30) of patients scored a 9 or lower, indicating inadequate health literacy. The mean age of patients with inadequate health literacy (mean = 64.8 years) did not differ significantly from that of patients with adequate health literacy (mean = 64.7 years) (P = .961). Similarly, there was no significant difference in health literacy between racial groups (P = .880). No clinical characteristics were associated with health literacy.
Quality of Life
For the survivors reporting inadequate health literacy, the mean physical QOL score was 69.6 (SD = 17.84), and the mean social QOL score was 65.9 (SD = 22.27). For survivors reporting high health literacy, the mean physical and social QOL scores were 77.9 (SD = 17.49) and 79.7 (SD = 17.60), respectively (Table II). The social QOL score for patients with adequate health literacy level is estimated to be 10.67 points (P = .013, 95% confidence interval, 2.25,19.09) higher than patients with inadequate health literacy level, while accounting for years since treatment, age, marital status, site, stage, and treatment modality. After adjusting for the covariates, health literacy was not significantly associated with physical QOL (P = .130 (Fig. 2).
TABLE II.
University of Washington Quality-of-Life Subscale Scores for the Whole Group and by Health Literacy Level (N = 218).
| Variables | Total (N = 218) | Inadequate Health Literacy (n = 30) | Adequate Health Literacy (n = 188) |
|---|---|---|---|
| Physical QOL, mean ± SD | 76.7 ± 17.7 | 69.6 ± 17.8 | 77.9 ± 17.5 |
| Social-emotional QOL, mean ± SD | 77.8 ± 18.9 | 65.9 ± 22.3 | 79.7 ± 17.6 |
SD = standard deviation; QOL = quality of life.
Fig. 2.

Association between health literacy (BHLS) and quality of life (QOL). (Left) Physical QOL. (Right) Social QOL. Hypothesis tests were performed after adjusting for age, marital status, site, stage, treatment modality, and years since treatment. BHLS = Brief Health Literacy Screen; QOL = quality of life.
DISCUSSION
The results of this study demonstrate that 14% of HNC survivors reported inadequate health literacy, which is slightly higher than the previously reported prevalence of 12%.13 Although research on this topic is sparse, the percent of patients with inadequate health literacy reported in our study was similar to those noted in other populations, including those with other cancer and chronic medical conditions.13,14,35,36 In a study of 1,463 colorectal cancer survivors, 14% demonstrated low subjective health literacy.35 Additionally, in a longitudinal study of newly diagnosed breast cancer patients, inadequate literacy rates varied from 16.5% to 18% across three time points.36 To our knowledge, this study was the first to describe the prevalence of health literacy in a large, diverse sample of HNC survivors.
Although not significant in our analysis, age, ethnicity, and education have consistently been associated with health literacy.37,38 Previous studies have demonstrated that middle-aged and older adult patients tend to report lower health literacy.15,39,40 In our analysis, the average age of survivors was similar between the two health literacy levels, which may be the result of limited younger adults in our sample. The majority of survivors were between the ages of 56 to 70 years of age, which is consistent with the general demographic of HNC.41 Due to the retrospective nature of our analysis, we could not obtain education level or income from survivors, but future studies on health literacy should include education and income as a variable of interest.
Health literacy has been shown in multiple disease settings, including cancer, to impact the QOL for patients. Our study demonstrated that inadequate health literacy was only significantly associated with lower social–emotional QOL. Prior studies have reported that a 7- to 10-point difference in UWQOL scores is considered a clinically meaningful difference.2,42,43 In our study, we noted a 10.67 point different in social–emotional QOL, representing a clinically meaningful difference. However, health literacy and physical QOL were not significantly associated. Patients with lower health literacy are more likely to be noncompliant with treatment and to report higher unmet informational needs and more mental distress, which may contribute to overall poorer QOL.35,36,44,45 Early intervention to improve patient understanding and health literacy, therefore, may improve patient QOL not only during but after treatment. Prior research has shown that interventions to improve health literacy resulted in a higher rate of patient adherence to treatment.15 Patient navigation programs that educate patients, address patient concerns, and facilitate coordination of care may lead to improved health literacy and understanding related to their disease.46 Further research is needed to determine the relationship between QOL and health literacy in order to develop and promote effective interventions to reduce literacy-related health disparities in HNC patients.
Moreover, our work demonstrates the feasibility of utilizing the BHLS in the clinical setting. The BHLS was administered during a busy HNC clinic without leading to appointment delays. Although there is no established best method to assess health literacy, the BHLS has been noted by patients in other clinical settings to be easier to read and complete. Patients felt more comfortable responding to the BHLS survey compared to lengthier surveys such as the STOFHLA.47
This study has some limitations. The data obtained in this study was cross-sectional. Therefore, a causal association between health literacy and QOL cannot be inferred. The results of this study may also be subject to survival bias. Furthermore, the questionnaires utilized to measure health literacy and QOL relied on survivors’ self-report, which may be a source of bias. Further studies should consider evaluating additional measures of health literacy and health outcomes to validate the results noted in this analysis. Finally, our sample obtained from one specialty HNC practice, in a single institute, which resulted in a racially homogenous sample. Future studies should employ strategies to ensure a racially diverse sample to explore the influence of race on health literacy adequately.
CONCLUSION
Our study demonstrated that inadequate health literacy was significantly associated with lower social–emotional QOL. Given the results of our study and others demonstrating the impact health literacy has on patient-reported outcomes, a system-level adoption of health literacy as a baseline measure is warranted to improve quality of care and reduce disparities. Further prospective research is needed to confirm these findings and understand how health literacy influences HNC survivors’ behaviors, overall health, and survival. Finally, interventions to ameliorate the impact of health literacy on dimensions of QOL are needed to optimize the health of survivors.
ACKNOWLEDGMENTS
The authors thank Jennifer Seaman, PhD, RN, CHPN, and Sarah Dainauski, SN, for their editorial support.
Funding and Conflicts of Interest: The authors have no other funding, financial relationships, or conflicts of interest to disclose.
BIBLIOGRAPHY
- 1.Argiris A, Karamouzis MV, Raben D, Ferris RL. Head and neck cancer. Lancet 2008;371:1695–1709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pulte D, Brenner H. Changes in survival in head and neck cancers in the late 20th and early 21st century: a period analysis. Oncologist 2010;15: 994–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Comprehensive Care Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines) for Head and Neck Cancers, Version 2.2016. October 11, 2016; Available at: https://www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf. Accessed December 28, 2018.
- 4.Department of Veterans Affairs Laryngeal Cancer Study Group; Wolf GT, Fisher SG, Hong WK, et al. Induction chemotherapy plus radiation compared with surgery plus radiation in patients with advanced laryngeal cancer. N Engl J Med 1991;324:1685–1690. [DOI] [PubMed] [Google Scholar]
- 5.Ang KK, Harris J, Wheeler R, et al. Human papillomavirus and survival of patients with oropharyngeal cancer. N Engl J Med 2010;363:24–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Givens DJ, Karnell LH, Gupta AK, et al. Adverse events associated with concurrent chemoradiation therapy in patients with head and neck cancer. Arch Otolaryngol Head Neck Surg 2009;135:1209–1217. [DOI] [PubMed] [Google Scholar]
- 7.Trotti A, Pajak TF, Gwede CK, et al. TAME: development of a new method for summarising adverse events of cancer treatment by the Radiation Therapy Oncology Group. Lancet Oncol 2007;8:613–624. [DOI] [PubMed] [Google Scholar]
- 8.Martino R, Ringash J. Evaluation of quality of life and organ function in head and neck squamous cell carcinoma. Hematol Oncol Clin North Am 2008;22:1239–1256. [DOI] [PubMed] [Google Scholar]
- 9.Sehlen S, Lenk M, Herschbach P, et al. Depressive symptoms during and after radiotherapy for head and neck cancer. Head Neck 2003;25:1004–1018. [DOI] [PubMed] [Google Scholar]
- 10.Koch R, Wittekindt C, Altendorf-Hofmann A, Singer S, Guntinas-Lichius O. Employment pathways and work-related issues in head and neck cancer survivors. Head Neck 2015;37:585–593. [DOI] [PubMed] [Google Scholar]
- 11.US Department of Health Human Services. Healthy People 2010. Washington, DC: US Government Printing Office; https://www.cdc.gov/nchs/data/hpdata2010/hp2010_final_review.pdf. Accessed November 20, 2018. [Google Scholar]
- 12.Kutner ME, Greenburg E, Jin Y, Paulsen C. The Health Literacy of America’s adults: results from the 2003 National Assessment of Adult Literacy. NCES 2006-483. Washington DC: National Center for Education Statistics; 2006. https://nces.ed.gov/pubs2006/2006483.pdf. Accessed November 20, 2018. [Google Scholar]
- 13.Koay K, Schofield P, Gough K, et al. Suboptimal health literacy in patients with lung cancer or head and neck cancer. Support Care Cancer 2013;21:2237–2245. [DOI] [PubMed] [Google Scholar]
- 14.Beitler JJ, Chen AY, Jacobson K, Owens A, Edwards M, Johnstone PA. Health literacy and health care in an inner-city, total laryngectomy population. Am J Otolaryngol 2010;31:29–31. [DOI] [PubMed] [Google Scholar]
- 15.Miller TA. Health literacy and adherence to medical treatment in chronic and acute illness: a meta-analysis. Patient Educ Couns 2016;99:1079–1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011;155:97–107. [DOI] [PubMed] [Google Scholar]
- 17.Baker DW, Gazmararian JA, Williams MV, et al. Health literacy and use of outpatient physician services by Medicare managed care enrollees. J Gen Intern Med. 2004;19:215–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murray MD, Tu W, Wu J, Morrow D, Smith F, Brater DC. Factors associated with exacerbation of heart failure include treatment adherence and health literacy skills. Clin Pharmacol Ther 2009;85:651–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cho YI, Lee SY, Arozullah AM, Crittenden KS. Effects of health literacy on health status and health service utilization amongst the elderly. Soc Sci Med 2008;66:1809–1816. [DOI] [PubMed] [Google Scholar]
- 20.Hope CJ, Wu J, Tu W, Young J, Murray MD. Association of medication adherence, knowledge, and skills with emergency department visits by adults 50 years or older with congestive heart failure. Am J Health Syst Pharm 2004;61:2043–2049. [DOI] [PubMed] [Google Scholar]
- 21.Haun JN, Patel NR, French DD, Campbell RR, Bradham DD, Lapcevic WA. Association between health literacy and medical care costs in an integrated healthcare system: a regional population based study. BMC Health Serv Res 2015;15:249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J. Health literacy and mortality among elderly persons. Arch Intern Med 2007;167:1503–1509. [DOI] [PubMed] [Google Scholar]
- 23.Oldach BR, Katz ML. Health literacy and cancer screening: a systematic review. Patient Educ Couns 2014;94:149–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morris NS, Field TS, Wagner JL, et al. The association between health literacy and cancer-related attitudes, behaviors, and knowledge. J Health Commun 2013;18(suppl 1):223–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hahn EA, Cella D, Dobrez DG, et al. The impact of literacy on health-related quality of life measurement and outcomes in cancer outpatients. Qual Life Res. 2007;16:495–507. [DOI] [PubMed] [Google Scholar]
- 26.Halverson JL, Martinez-Donate AP, Palta M, et al. Health literacy and health-related quality of life among a population-based sample of cancer patients. J Health Commun 2015;20:1320–1329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med 2004;36:588–594. [PubMed] [Google Scholar]
- 28.Chew LD, Griffin JM, Partin MR, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008;23:561–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wallston KA, Cawthon C, McNaughton CD, Rothman RL, Osborn CY, Kripalani S. Psychometric properties of the brief health literacy screen in clinical practice. J Gen Intern Med 2014;29:119–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Willens DE, Kripalani S, Schildcrout JS, et al. Association of brief health literacy screening and blood pressure in primary care. J Health Commun 2013;18(suppl 1):129–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cawthon C, Mion LC, Willens DE, Roumie CL, Kripalani S. Implementing routine health literacy assessment in hospital and primary care patients. Jt Comm J Qual Patient Saf 2014;40:68–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cavanaugh KL, Osborn CY, Tentori F, Rothman RL, Ikizler TA, Wallston KA. Performance of a brief survey to assess health literacy in patients receiving hemodialysis. Clin Kidney J 2015;8: 462–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rogers SN, Gwanne S, Lowe D, Humphris G, Yueh B, Weymuller EA Jr. The addition of mood and anxiety domains to the University of Washington quality of life scale. Head Neck 2002;24:521–529. [DOI] [PubMed] [Google Scholar]
- 34.Rogers SN, Lowe D, Yueh B, Weymuller EA Jr. The physical function and social-emotional function subscales of the University of Washington Quality of Life Questionnaire. Arch Otolaryngol Head Neck Surg 2010;136: 352–357. [DOI] [PubMed] [Google Scholar]
- 35.Husson O, Mols F, Fransen MP, van de Poll-Franse LV, Ezendam NP. Low subjective health literacy is associated with adverse health behaviors and worse health-related quality of life among colorectal cancer survivors: results from the profiles registry. Psychooncology 2015;24: 478–486. [DOI] [PubMed] [Google Scholar]
- 36.Halbach SM, Ernstmann N, Kowalski C, et al. Unmet information needs and limited health literacy in newly diagnosed breast cancer patients over the course of cancer treatment. Patient Educ Couns 2016;99:1511–1518. [DOI] [PubMed] [Google Scholar]
- 37.Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR. The prevalence of limited health literacy. J Gen InternMed 2005;20: 175–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Amalraj S, Starkweather C, Nguyen C, Naeim A. Health literacy, communication, and treatment decision-making in older cancer patients. Oncology (Williston Park) 2009;23:369–375. [PubMed] [Google Scholar]
- 39.Berens EM, Vogt D, Messer M, Hurrelmann K, Schaeffer D. Health literacy among different age groups in Germany: results of a cross-sectional survey. BMC Public Health 2016;16:1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Barragan M, Hicks G, Williams MV, Franco-Paredes C, Duffus W, del Rio C. Low health literacy is associated with HIV test acceptance. J Gen Intern Med 2005;20:422–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sikora AG, Toniolo P, DeLacure MD. The changing demographics of head and neck squamous cell carcinoma in the United States. Laryngoscope 2004;114:1915–1923. [DOI] [PubMed] [Google Scholar]
- 42.El-Deiry MW, Futran ND, McDowell JA, Weymuller EA Jr, Yueh B. Influences and predictors of long-term quality of life in head and neck cancer survivors. Arch Otolaryngol Head Neck Surg 2009;135:380–384. [DOI] [PubMed] [Google Scholar]
- 43.Vartanian JG, Carvalho AL, Yueh B, et al. Long-term quality-of-life evaluation after head and neck cancer treatment in a developing country. Arch Otolaryngol Head Neck Surg 2004;130:1209–1213. [DOI] [PubMed] [Google Scholar]
- 44.Li BD, Brown WA, Ampil FL, Burton GV, Yu H, McDonald JC. Patient compliance is critical for equivalent clinical outcomes for breast cancer treated by breast-conservation therapy. Ann Surg 2000;231:883–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tormey LK, Reich J, Chen YS, et al. Limited health literacy is associated with worse patient-reported outcomes in inflammatory bowel disease. Inflamm Bowel Dis 2019;25:204–212. [DOI] [PubMed] [Google Scholar]
- 46.Martinez-Donate AP, Halverson J, Simon NJ, et al. Identifying health literacy and health system navigation needs among rural cancer patients: findings from the Rural Oncology Literacy Enhancement Study (ROLES). J Cancer Educ 2013;28:573–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sand-Jecklin K, Coyle S. Efficiently assessing patient health literacy: the BHLS instrument. Clin Nurs Res 2014;23:581–600. [DOI] [PubMed] [Google Scholar]


