Abstract
Objective
The objective is to formulate clinical practice guidelines for the treatment of diabetes in older adults.
Conclusions
Diabetes, particularly type 2, is becoming more prevalent in the general population, especially in individuals over the age of 65 years. The underlying pathophysiology of the disease in these patients is exacerbated by the direct effects of aging on metabolic regulation. Similarly, aging effects interact with diabetes to accelerate the progression of many common diabetes complications. Each section in this guideline covers all aspects of the etiology and available evidence, primarily from controlled trials, on therapeutic options and outcomes in this population. The goal is to give guidance to practicing health care providers that will benefit patients with diabetes (both type 1 and type 2), paying particular attention to avoiding unnecessary and/or harmful adverse effects.
Screening, treatment, and management of diabetes mellitus and complications in older patients.
List of Recommendations
Role of the endocrinologist and diabetes care specialist
1.1 In patients aged 65 years and older with newly diagnosed diabetes, we advise that an endocrinologist or diabetes care specialist should work with the primary care provider, a multidisciplinary team, and the patient in the development of individualized diabetes treatment goals. (Ungraded Good Practice Statement)
1.2 In patients aged 65 years and older with diabetes, an endocrinologist or diabetes care specialist should be primarily responsible for diabetes care if the patient has type 1 diabetes, or requires complex hyperglycemia treatment to achieve treatment goals, or has recurrent severe hypoglycemia, or has multiple diabetes complications. (Ungraded Good Practice Statement)
Screening for diabetes and prediabetes, and diabetes prevention
2.1 In patients aged 65 years and older without known diabetes, we recommend fasting plasma glucose and/or HbA1c screening to diagnose diabetes or prediabetes. (1|⊕⊕⊕⊕)
Technical remark: The measurement of HbA1c may be inaccurate in some people in this age group because of comorbidities that can affect the lifespan of red blood cells in the circulation. Although the optimal screening frequency for patients whose initial screening test is normal remains unclear, the writing committee advocates repeat screening every 2 years thereafter. As with any health screening, the decision about diabetes and prediabetes screening for an individual patient depends on whether some action will be taken as a result and the likelihood of benefit. For example, such screening may not be appropriate for an older patient with end-stage cancer or organ system failure. In these situations, shared decision-making with the patient is recommended.
2.2 In patients aged 65 years and older without known diabetes who meet the criteria for prediabetes by fasting plasma glucose or HbA1c, we suggest obtaining a 2-hour glucose post–oral glucose tolerance test measurement. (2|⊕⊕⊕O)
Technical remark: This recommendation is most applicable to high-risk patients with any of the following characteristics: overweight or obese, first-degree relative with diabetes, high-risk race/ethnicity (e.g., African American, Latino, Native American, Asian American, Pacific Islander), history of cardiovascular disease, hypertension (≥140/90 mm Hg or on therapy for hypertension), high-density lipoprotein cholesterol level <35 mg/dL (0.90 mmol/L) and/or a triglyceride level >250 mg/dL (2.82 mmol/L), sleep apnea, or physical inactivity. Shared decision-making is advised for performing this procedure in frail older people or in those for whom it may be overly burdensome. Standard dietary preparation for an oral glucose tolerance test is advised.
2.3 In patients aged 65 years and older who have prediabetes, we recommend a lifestyle program similar to the Diabetes Prevention Program to delay progression to diabetes. (1|⊕⊕⊕⊕)
Technical remark: Metformin is not recommended for diabetes prevention at this time, as it is not approved by the Food and Drug Administration for this indication. As of 2018, a Diabetes Prevention Program–like lifestyle intervention is a covered benefit for Medicare beneficiaries in the United States who meet the criteria for prediabetes.
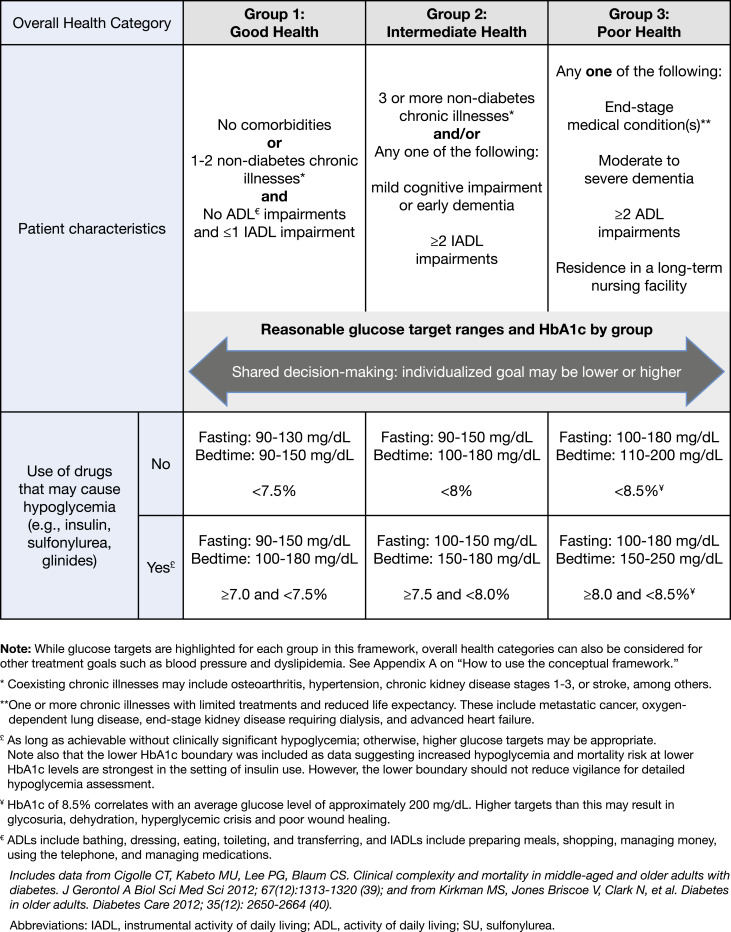
Assessment of older patients with diabetes
3.1 In patients aged 65 years and older with diabetes, we advise assessing the patient’s overall health (see Table 2) and personal values prior to the determination of treatment goals and strategies (see Table 3). (Ungraded Good Practice Statement)
3.2 In patients aged 65 years and older with diabetes, we suggest that periodic cognitive screening should be performed to identify undiagnosed cognitive impairment. (2|⊕⊕OO)
Technical remark: Use of validated self-administered tests is an efficient and cost-effective way to implement screening (see text). Alternative screening test options, such as the Mini-Mental State Examination or Montreal Cognitive Assessment, are widely used. An initial screening should be performed at the time of diagnosis or when a patient enters a care program. Screening should be repeated every 2 to 3 years after a normal screening test result for patients without cognitive complaints or repeated 1 year after a borderline normal test result. Always evaluate cognitive complaints and assess cognition in patients with complaints.
3.3 In patients aged 65 years and older with diabetes and a diagnosis of cognitive impairment (i.e., mild cognitive impairment or dementia), we suggest that medication regimens should be simplified (see recommendation 3.1) and glycemic targets tailored (i.e., be more lenient; see recommendation 4.1) to improve compliance and prevent treatment-related complications. (2|⊕⊕OO)
Technical remark: Medical and nonmedical treatment and care for cognitive symptoms in people with diabetes and cognitive impairment are no different from those in people without diabetes and cognitive impairment. Depending on the situation and preferences of the patient, a primary caregiver can be involved in decision-making and management of medication.
Table 2.
Clinical Care of Older People
| General Health Assessmenta | General Health Testsb | Diabetes-Specific Healthc |
|---|---|---|
| Functional status (ADLs/IADLsd) | ECG | Retinopathy |
| Depression | Lipid panel | Nephropathy |
| Cognition | Bone mineral density | Neuropathy |
| Fall risk | AAA ultrasound | Medical nutrition therapy |
| Weight (kg)/height (m)2 = BMI | Diabetes screening (for nondiabetic persons) | Diabetes management |
| Blood pressure | Diabetes self-management training | |
| Tobacco use | ||
| Alcohol use | ||
| Medication review | ||
| Cancer screening | ||
| Hearing | ||
| Comorbid conditions | ||
| Visual acuity | ||
| Frailty/physical performance |
Abbreviations: AAA, abdominal aortic aneurysm; ADL, activity of daily living; BMI, body mass index; IADL, instrumental activity of daily living.
All items are required services to qualify for Medicare coverage of annual wellness examinations for people in the United States >65 y of age, except for frailty/physical performance (33). These are generally conducted by primary care providers.
All items are services covered by Medicare for people in the United State >65 y of age as part of annual wellness examinations at intervals varying from annually to once per lifetime (33).
All items are services covered by Medicare for people in the United States >65 y of age as part of standard diabetes care (33). These are covered annually except for diabetes management visits, which are covered as recommended by the diabetes care team.
Functional status is based on assessment of independence or dependency (having difficulty and receiving assistance) of five ADLs (bathing, dressing, eating, toileting, and transferring) and five IADLs (preparing meals, shopping, managing money, using the telephone, and managing medications) (34).
Table 3.
Conceptual Framework for Considering Overall Health and Patient Values in Determining Clinical Targets in Adults Aged 65 y and Older
|
Treatment of hyperglycemia
Setting glycemic targets and goals
4.1 In patients aged 65 years and older with diabetes, we recommend that outpatient diabetes regimens be designed specifically to minimize hypoglycemia. (1|⊕⊕⊕O)
Technical remark: Although evidence for specific targets is lacking, glycemic targets should be tailored to overall health and management strategies (e.g., whether a medication that can cause hypoglycemia is used) (see Table 3).
Assessing glycemia in older adults with diabetes
4.2 In patients aged 65 years and older with diabetes who are treated with insulin, we recommend frequent fingerstick glucose monitoring and/or continuous glucose monitoring (to assess glycemia) in addition to HbA1c. (1|⊕⊕OO)
Lifestyle interventions for older adults with diabetes
Lifestyle modifications
4.3 In patients aged 65 years and older with diabetes who are ambulatory, we recommend lifestyle modification as the first-line treatment of hyperglycemia. (1|⊕⊕⊕⊕)
Nutrition
4.4 In patients aged 65 years and older with diabetes, we recommend assessing nutritional status to detect and manage malnutrition. (1|⊕⊕⊕⊕)
Technical remark: Nutritional status can be assessed using validated tools such as the Mini Nutritional Assessment and Short Nutritional Assessment Questionnaire.
4.5 In patients aged 65 years and older with diabetes and frailty, we suggest the use of diets rich in protein and energy to prevent malnutrition and weight loss. (2|⊕⊕OO)
4.6 In patients aged 65 years and older with diabetes who cannot achieve glycemic targets with lifestyle modification, we suggest avoiding the use of restrictive diets and instead limiting consumption of simple sugars if patients are at risk for malnutrition. (2|⊕OOO)
Technical remark: Patients’ glycemic responses to changes in diet should be monitored closely. This recommendation applies to both older adults living in the community and those in nursing homes.
Drug therapy for hyperglycemia
Glycemic management of diabetes in older adults with diabetes
4.7 In patients aged 65 years and older with diabetes, we recommend metformin as the initial oral medication chosen for glycemic management in addition to lifestyle management. (1|⊕⊕⊕O)
Technical remark: This recommendation should not be implemented in patients who have significantly impaired kidney function (estimated glomerular filtration rate <30 mL/min/1.73 m2) or have a gastrointestinal intolerance.
4.8 In patients aged 65 years and older with diabetes who have not achieved glycemic targets with metformin and lifestyle, we recommend that other oral or injectable agents and/or insulin should be added to metformin. (1|⊕⊕⊕⊕)
Technical remark: To reduce the risk of hypoglycemia, avoid using sulfonylureas and glinides, and use insulin sparingly. Glycemic treatment regimens should be kept as simple as possible.
Treating complications of diabetes
Management of hypertension in older adults with diabetes
5.1 In patients aged 65 to 85 years with diabetes, we recommend a target blood pressure of 140/90 mm Hg to decrease the risk of cardiovascular disease outcomes, stroke, and progressive chronic kidney disease. (1|⊕⊕⊕O)
Technical remark: Patients in certain high-risk groups could be considered for lower blood pressure targets (130/80 mm Hg), such as those with previous stroke or progressing chronic kidney disease (estimated glomerular filtration rate <60 mL/min/1.73 m2 and/or albuminuria). If lower blood pressure targets are selected, careful monitoring of such patients is needed to avoid orthostatic hypotension. Patients with high disease complexity (group 3, poor health, Table 3) could be considered for higher blood pressure targets (145 to 160/90 mm Hg). Choosing a blood pressure target involves shared decision-making between the clinician and patient, with full discussion of the benefits and risks of each target.
5.2 In patients aged 65 years and older with diabetes and hypertension, we recommend that an angiotensin-converting enzyme inhibitor or an angiotensin receptor blocker should be the first-line therapy. (1|⊕⊕⊕O)
Technical remark: If one class is not tolerated, the other should be substituted.
Management of hyperlipidemia in older adults with diabetes
5.3 In patients aged 65 years and older with diabetes, we recommend an annual lipid profile. (1|⊕⊕OO)
5.4 In patients aged 65 years and older with diabetes, we recommend statin therapy and the use of an annual lipid profile to achieve the recommended levels for reducing absolute cardiovascular disease events and all-cause mortality. (1|⊕⊕⊕⊕)
Technical remark: The Writing Committee did not rigorously evaluate the evidence for specific low-density lipoprotein cholesterol targets in this population, so we refrained from endorsing specific low-density lipoprotein cholesterol targets in this guideline. For patients aged 80 years old and older or with short life expectancy, we advocate that low-density lipoprotein cholesterol goal levels should not be so strict.
5.5 In patients aged 65 years and older with diabetes, we suggest that if statin therapy is inadequate for reaching the low-density lipoprotein cholesterol reduction goal, either because of side effects or because the low-density lipoprotein cholesterol target is elusive, then alternative or additional approaches (such as including ezetimibe or proprotein convertase subtilisin/kexin type 9 inhibitors) should be initiated. (2|⊕OOO)
5.6 In patients aged 65 years and older with diabetes and fasting triglycerides >500 mg/dL, we recommend the use of fish oil and/or fenofibrate to reduce the risk of pancreatitis. (1|⊕⊕OO)
Management of congestive heart failure in older adults with diabetes
5.7 In patients aged 65 years and older who have diabetes and congestive heart failure, we advise treatment in accordance with published clinical practice guidelines on congestive heart failure. (Ungraded Good Practice Statement)
5.8 In patients aged 65 years and older who have diabetes and congestive heart failure, the following oral hypoglycemic agents should be prescribed with caution to prevent worsening of heart failure: glinides, rosiglitazone, pioglitazone, and dipeptidyl peptidase-4 inhibitors. (Ungraded Good Practice Statement)
Management of atherosclerosis in older adults with diabetes
5.9 In patients aged 65 years and older with diabetes and a history of atherosclerotic cardiovascular disease, we recommend low-dosage aspirin (75 to 162 mg/d) for secondary prevention of cardiovascular disease after careful assessment of bleeding risk and collaborative decision-making with the patient, family, and other caregivers. (1|⊕⊕OO)
Eye complications in older adults with diabetes
5.10 In patients aged 65 years and older with diabetes, we recommend annual comprehensive eye examinations to detect retinal disease (1|⊕⊕⊕⊕).
Technical remark: Screening and treatment should be conducted by an ophthalmologist or optometrist in line with present-day standards.
Neuropathy, falls, and lower extremity problems in older adults with diabetes
5.11 In patients aged 65 years and older with diabetes and advanced chronic sensorimotor distal polyneuropathy, we suggest treatment regimens that minimize fall risk, such as the minimized use of sedative drugs or drugs that promote orthostatic hypotension and/or hypoglycemia. (2|⊕OOO)
5.12 In patients aged 65 years and older with diabetes and peripheral neuropathy with balance and gait problems, we suggest referral to physical therapy or a fall management program to reduce the risk of fractures and fracture-related complications. (2|⊕OOO)
5.13 In patients aged 65 years and older with diabetes and peripheral neuropathy and/or peripheral vascular disease, we suggest referral to a podiatrist, orthopedist, or vascular specialist for preventive care to reduce the risk of foot ulceration and/or lower extremity amputation. (2|⊕⊕OO)
Chronic kidney disease in older adults with diabetes
5.14 In patients aged 65 years and older with diabetes who are not on dialysis, we recommend annual screening for chronic kidney disease with an estimated glomerular filtration rate and urine albumin-to-creatinine ratio. (1|⊕⊕⊕⊕)
5.15 In patients aged 65 years and older with diabetes who are in group 3 (poor health, see Table 3) of the framework and have a previous albumin-to-creatinine ratio of <30 mg/g, we suggest against additional annual albumin-to-creatinine ratio measurements. (2|⊕⊕OO)
5.16 In patients aged 65 years and older with diabetes and decreased estimated glomerular filtration rate, we recommend limiting the use or dosage of many classes of diabetes medications to minimize the side effects and complications associated with chronic kidney disease. (1|⊕⊕OO)
Technical remark: Specific use/dosing guidance on each class of diabetes medication is provided in Table 7.
Table 7.
Medications Used to Treat Hyperglycemia and Special Concerns With Use in Older Patients With CKD and CVD
| Medication Class | Use in Older Patients | Use in Patients With CKD (Stages 3 to 5) | Use in Patients With CVD |
|---|---|---|---|
| Insulin | Can cause hypoglycemia | Decreased clearance. Increased risk of hypoglycemia. Dosages may need adjusting. Consider giving rapid-acting insulin postprandially because of gastroparesis. | May worsen fluid retention when used with thiazolidinediones. Hypoglycemia to be avoided because of potential arrhythmias and stroke |
| Metformin | Can cause gastrointestinal intolerance | Reduce dosage to 1000 mg/d if eGFR <45a; do not start if eGFR <45a | May be beneficial in patients with coronary artery disease. Avoid use in patients with severe CHF to avoid lactic acidosis |
| Does not cause hypoglycemia | Stop if eGFR <30a | ||
| May cause vitamin B12 deficiency | Stop if increased risk of acute kidney injury (radiocontrast dye, hypotension, sepsis, shock, hypoxia). | ||
| SUs | Can cause hypoglycemia | Glyburide: avoid if eGFR <60a | Can cause hypoglycemia, which is to be avoided because of potential arrhythmias and stroke |
| Can cause weight gain | Glimepiride: avoid if eGFR <30a | ||
| Avoid glyburide | Glipizide: use with caution if eGFR < 30a | ||
| Glinides | Can cause hypoglycemia | Nateglinide: stop if eGFR <60a but can use if patient is on dialysis | Can cause hypoglycemia, which is to be avoided because of potential arrhythmias and stroke |
| May be useful for individuals who skip meals | Repaglinide: use with caution if eGFR <30a | ||
| Thiazolidinediones | Does not cause hypoglycemia | No dosage adjustment needed. Can cause fluid retention. Can increase fractures. | Pioglitazone has been shown to reduce CVD mortality. Can cause fluid retention with potential to worsen heart failure |
| Can increase fracture risk | |||
| Can cause fluid retention | |||
| Can cause weight gain | |||
| α-Glucosidase inhibitors | Does not cause hypoglycemia | Avoid if serum creatinine >2.0 mg/dL because of lack of studies in such patients | |
| Gastrointestinal side effects may cause nonadherence | |||
| DPP-4 inhibitors | Does not cause hypoglycemia | Sitagliptin: | Saxagliptin has been shown to increase the risk of heart failure |
| eGFR >50a: 100 mg/d | |||
| eGFR 30–50a: 50 mg/d | |||
| eGFR <30a: 25 mg/d | |||
| Saxagliptin: | |||
| eGFR >50a: 2.5 or 5 mg daily | |||
| eGFR ≤50a: 2.5 mg daily | |||
| Alogliptin: | |||
| eGFR >60a: 25 mg daily | |||
| eGFR 30–60a: 12.5 mg daily | |||
| eGFR <30a: 6.25 mg daily | |||
| Linagliptin: | |||
| No dosage adjustment needed | |||
| SGLT2 inhibitors | Does not cause hypoglycemia | Canagliflozin: eGFR 45–60a: 100 mg/d; eGFR <45a: avoid use | Empagliflozin and canagliflozin have been demonstrated to reduce major adverse cardiovascular events and CHF |
| Empagliflozin can reduce cardiovascular events and progression of CKD | Dapagliflozin: eGFR <60a: avoid use | ||
| Volume depletion adverse effects more common in older patients | Empagliflozin: eGFR <45a: avoid use | ||
| Ertugliflozin: eGFR <60a: avoid use | |||
| Canagliflozin may increase fracture risk; has also been associated with an increased risk of toe and foot amputations | Canagliflozin and dapagliflozin have been associated with acute kidney injury | ||
| May rarely cause ketoacidosis | Empagliflozin and canagliflozin can reduce progression of CKD | ||
| GLP-1 receptor agonists | Does not cause hypoglycemia | Exenatide: eGFR <30a: avoid use | Liraglutide and semaglutide have been demonstrated to reduce major adverse CVD events |
| May cause gastrointestinal side effects | Liraglutide, dulaglutide, semaglutide: no dosage adjustment needed | ||
| Lixisenatide: avoid if eGFR <15a | |||
| Bromocriptine | May cause nausea | Use with caution. Not studied in CKD. | |
| Does not cause hypoglycemia | |||
| Colesevelam | May cause gastrointestinal side effects | No dosage adjustment needed, but limited data are available | |
| Does not cause hypoglycemia |
eGFR levels are all in mL/min/1.73 m2.
Special settings and populations
Management of diabetes away from home—in hospitals and long-term care facilities—and transitions of care
6.1 In patients aged 65 years and over with diabetes in hospitals or nursing homes, we recommend establishing clear targets for glycemia at 100 to 140 mg/dL (5.55 to 7.77 mmol/L) fasting and 140 to 180 mg/dL (7.77 to 10 mmol/L) postprandial while avoiding hypoglycemia. (1|⊕⊕OO)
Technical remark: An explicit discharge plan should be developed to reestablish long-term glycemic treatment targets and glucose-lowering medications as the patient transitions to posthospital care.
6.2 In patients aged 65 years and older with diabetes and a terminal illness or severe comorbidities, we recommend simplifying diabetes management strategies. (1|⊕OOO)
6.3 In patients aged 65 years and older without diagnosed diabetes, we suggest routine screening for HbA1c during admission to the hospital to ensure detection and treatment where needed (see the technical remark in recommendation 2.1). (2|⊕⊕OO)
Introduction
Scope of guideline
In recognition of the broad nature of the topic, the Writing Committee has identified topics deemed to have the greatest impact on the overall health and quality of life of older individuals (defined here as age 65 years or older) with diabetes. The Writing Committee has chosen to use the American Diabetes Association (ADA) definitions for diabetes and prediabetes (see section 2 on “Screening for Diabetes and Prediabetes, and Diabetes Prevention”). We discuss pathophysiology and epidemiology unique to older adults, evidenced-based treatment strategies, such as lifestyle management and drug therapy, and the identification and management of common comorbidities and diabetes-related complications, such as hypertension, hyperlipidemia, congestive heart failure (CHF), retinopathy, neuropathy, and chronic kidney disease (CKD). We also discuss special settings and type 1 diabetes (T1D). Some topics, such as a detailed discussion on the use of devices and technology, are identified as being important for the care of patients with diabetes but are beyond the scope of the guideline. Furthermore, we emphasize the heterogeneity of the older adult population with diabetes and provide guidance for individualization of treatment plans by creating a conceptual framework that suggests three categories of overall health (see “Assessment of Older Patients With Diabetes”). This framework is discussed in detail in section 3 and referenced in specific recommendations wherever relevant. Lastly, members of the Writing Committee sought to incorporate the patient’s voice into this guideline by developing and administering a brief survey in collaboration with patient advocacy organizations/community organizers who helped us identify individuals with diabetes for participation. The results of this survey are reported in a designated section in Appendix B.
Epidemiology
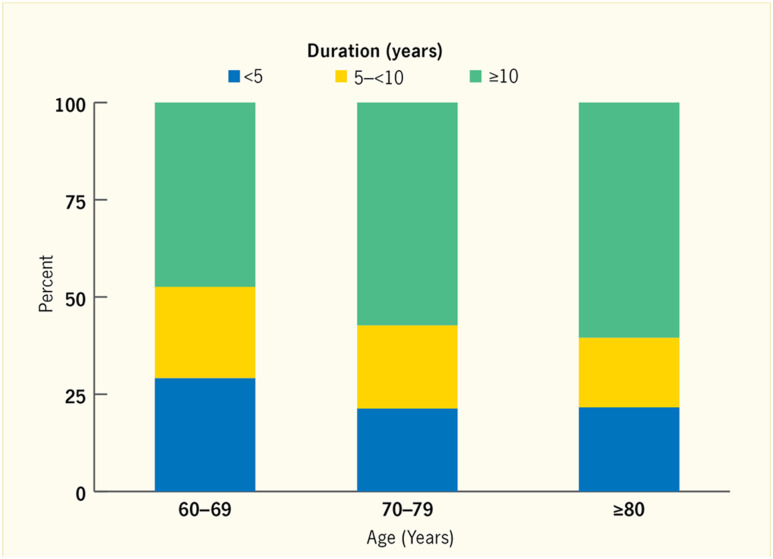
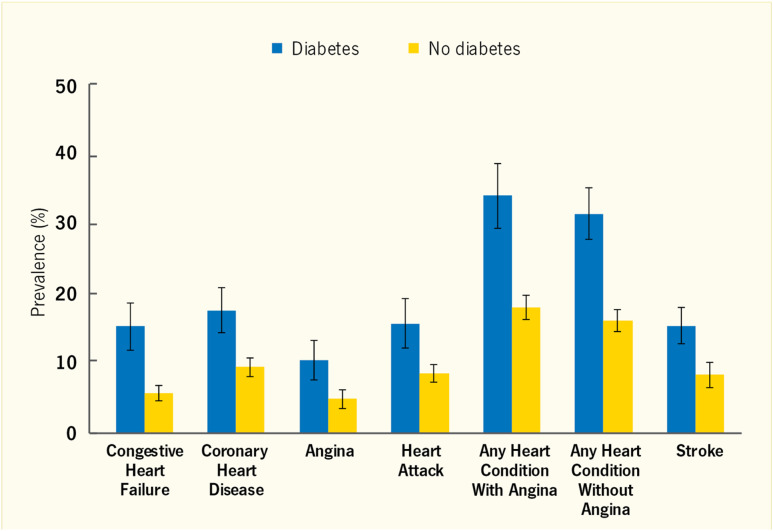
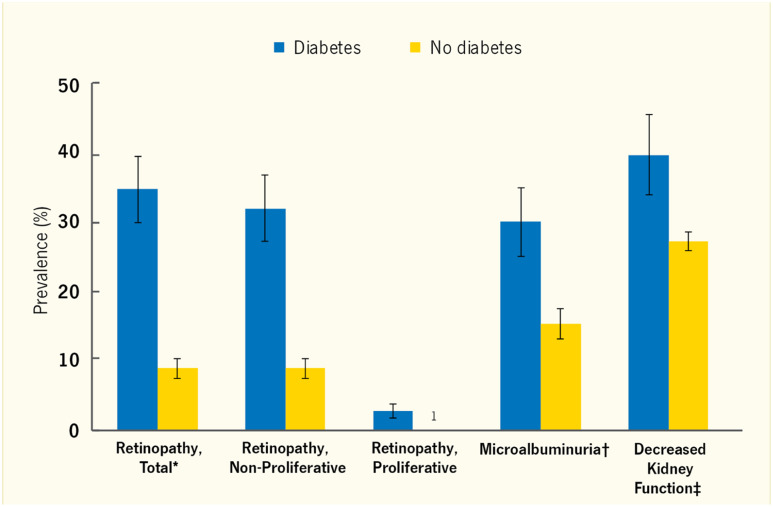
Among older adults with diabetes, >90% have type 2 diabetes (T2D), and in one study, this value was 96% (1). T2D is an age-related disease with a prevalence of 33% in the US population aged 65 years or older, and nearly 50% of older people meet the criteria for prediabetes (2). The incidence of newly diagnosed diabetes is highest among those aged 65 to 79 years. The reported duration of T2D among older people is illustrated in Fig. 1 (3). Although nearly half of those with diabetes aged 60 to 69 years report having had the disease for >10 years, ∼20% of individuals over the age 80 years report a duration of <5 years. However, the duration of T2D may be underestimated unless individuals are screened regularly. The prevalence of diabetes in the United States is projected to increase dramatically during the next 3 decades; as the population ages, the numbers of higher-risk minority groups increase, and people with diabetes live longer because of decreasing rates of cardiovascular deaths (4). Moreover, older adults are susceptible to all of the usual complications of diabetes [reviewed in Refs. (3) and (5)]. The prevalence rates of end-stage renal disease, loss of vision, myocardial infarction, stroke, peripheral vascular disease, and peripheral neuropathy are increased by the presence of diabetes, as illustrated in Fig. 2 for cardiovascular diseases (CVDs) and in Fig. 3 for microvascular complications (3).
Figure 1.
Duration of diabetes among adults aged ≥60 y, by age, United States, 2009–2010 (3). [Reproduced from Laiteerapong N, Huang ES. Chapter 16: Diabetes in older adults. In Cowie CC, Casagrande SS, Menke A, et al., eds. Diabetes in America, 3rd ed. Bethesda, MD: National Institutes of Health, NIH Pub No. 17-1468, 2017; pp 16-1 to 16-26.]
Figure 2.
Cardiovascular complications among adults age ≥65 y, by diabetes status, United States, 2007–2010. Data are self-reported. Error bards represent 95% CIs. [Reproduced from Laiteerapong N, Huang ES. Chapter 16: Diabetes in older adults. In Cowie CC, Casagrande SS, Menke A, et al., eds. Diabetes in America, 3rd ed. Bethesda, MD: National Institutes of Health, NIH Pub No. 17-1468, 2017; pp 16-1 to 16-26.]
Figure 3.
Microvascular complications among adults age ≥65 y, by diabetes status, United States, 2005–2010. Diabetes status is self-reported. Error bars represent 95% CIs. *Retinopathy detected by nonmydriatic digital fundus photography. Based on 2005–2008 data. †Microalbuminuria defined as an albumin-to-creatinine ratio of 30 to 300 mg/g. Based on 2007–2010 data. ‡Decreased kidney function based on eGFR <60 mL/min/1.73 m2 determined using the CKD-EPI equation and serum creatinine. 1Estimate is too unreliable to present; one case (or no cases) or relative SE >50%. [Reproduced from Laiteerapong N, Huang ES. Chapter 16: Diabetes in older adults. In Cowie CC, Casagrande SS, Menke A, et al., eds. Diabetes in America, 3rd ed. Bethesda, MD: National Institutes of Health, NIH Pub No. 17-1468, 2017; pp 16-1 to 16-26.]
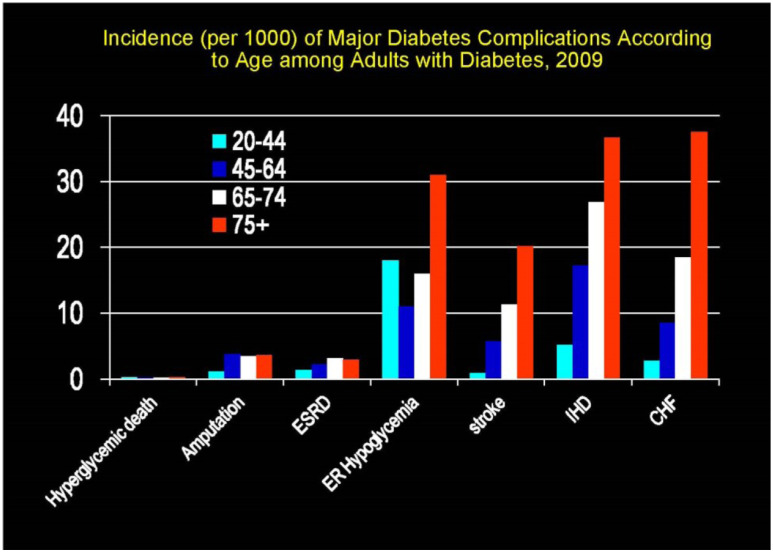
The dramatic effect of age on the incidence of major diabetes complications is illustrated in Fig. 4 (6). As summarized in Halter et al. (7), ∼50% of individuals over age 65 years with diabetes have diabetic nephropathy, which manifests as albuminuria, impaired glomerular filtration rate (GFR), or both. Diabetic kidney disease accounts for nearly half of all cases of end-stage renal disease in the United States, and the rate is highest among those aged ≥75 years. The risk for lower extremity amputation is 10-fold greater in older people with diabetes than in those without diabetes.
Figure 4.
Incidence (per 1000) of major diabetes complications according to age among adults with diabetes, 2009 (6). ER, emergency room; ESRD, end-stage renal disease; IHD, ischemic heart disease. [Reproduced from the National Diabetes Surveillance System at http://www.cdc.gov/diabetes]
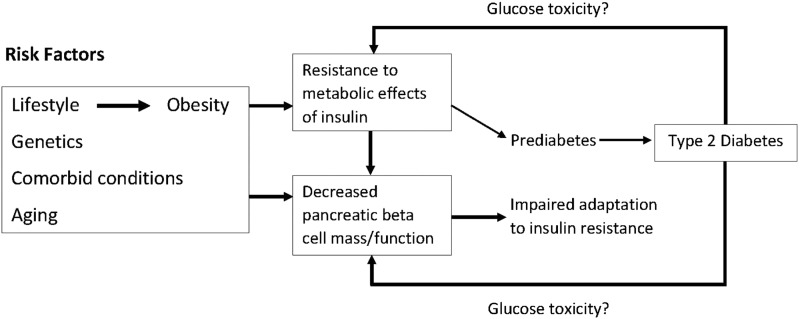
Pathophysiology of hyperglycemia
A detailed discussion of the pathophysiology of T2D and its relationship to aging is beyond the scope of this report. As summarized recently (8), T2D occurs in the older population as a result of a complex interaction among genetic, lifestyle, and aging influences [see Fig. 5 (9)]. This complexity means that there is substantial heterogeneity in the pathophysiology, clinical features, and rate of progression of the disease among older people. A recent review summarizes the effects of aging on glucose tolerance and insulin secretion (8). Notably, consistent declines in β cell function and insulin secretion are hallmarks of aging in rodents and humans (10–18). These impairments limit the response to lifestyle-induced insulin resistance, resulting in progression to prediabetes and T2D. Glucose toxicity from chronic exposure to hyperglycemia can worsen insulin resistance and further impair pancreatic β cell function (19). Thus, hyperglycemia in diabetes may drive further worsening of age-related impairments of both β cell function and proliferation. Lipotoxicity from exposure to products of fat cell lipolysis may also contribute to this vicious cycle (20), as do visceral obesity and intramyocellular fat. The heterogeneity of T2D likely reflects the varying contributions of multiple factors to the development of hyperglycemia in a given individual or family. Understanding these factors for an individual patient may provide a basis for the selection of glucose-lowering interventions (8).
Figure 5.
Model for age-related hyperglycemia (9). [Adapted with permission from Chang AM, Halter JB. Aging and insulin secretion. Am J Physiol Endocrinol Metab 2003;284:E7–E12.]
Systematic Review and Meta-Analyses
The Writing Committee commissioned two systematic reviews to support this guideline. Both reviews focused on individuals aged 65 years and older. Although the target population of this guideline is individuals with diabetes, concerns about not identifying sufficient evidence necessitated that the two systematic reviews summarize evidence on individuals with and without diabetes (presented separately).
The first review attempted to answer the following question: In older individuals, does treatment with antihypertensive pharmacologic therapy lead to improvement in patient-important outcomes? The review identified 19 randomized trials. Antihypertensive therapy was associated with a reduction in all-cause mortality, cardiovascular mortality, myocardial infarction, heart failure, stroke, and CKD. Older patients with diabetes treated with antihypertensive therapy had lower risk of CKD without a significant reduction in other outcomes; however, there was no significant difference in estimates of beneficial effects between those with and without diabetes.
The second review attempted to answer the following question: In older individuals, does treatment with lipid-lowering pharmacologic therapy lead to improvement in patient-important outcomes? The review identified 23 randomized trials. For primary prevention, statins reduced the risk of coronary artery disease and myocardial infarction, but not all-cause or cardiovascular mortality or stroke. These effects were imprecise in patients with diabetes, but there was no significant interaction between diabetes status and the intervention effect. For secondary prevention, statins reduced all-cause mortality, cardiovascular mortality, coronary artery disease, myocardial infarction, and revascularization. Intensive (vs less intensive) statin therapy reduced the risk of coronary artery disease and heart failure.
In both of the systematic reviews, the quality of evidence, or certainty in the estimates, was high for most outcomes when evaluated in all older patients. When the evaluation was restricted to those with diabetes, the estimates of beneficial effects were generally similar to those observed in all older patients, but the CIs were relatively wide, indicating imprecision. Accordingly, the corresponding quality of evidence was considered to be moderate for older patients with diabetes. There was also no significant difference in estimates (interaction) between those with and without diabetes, suggesting that extrapolation of data from the older population at large to older individuals with diabetes is reasonable.
1. Role of the Endocrinologist and Diabetes Care Specialist
1.1 In patients aged 65 years and older with newly diagnosed diabetes, we advise that an endocrinologist or diabetes care specialist should work with the primary care provider, a multidisciplinary team, and the patient in the development of individualized diabetes treatment goals. (Ungraded Good Practice Statement)
1.2 In patients aged 65 years and older with diabetes, an endocrinologist or diabetes care specialist should be primarily responsible for diabetes care if the patient has T1D, or requires complex hyperglycemia treatment to achieve treatment goals, or has recurrent severe hypoglycemia, or has multiple diabetes complications. (Ungraded Good Practice Statement)
Evidence
Given the heterogeneity of the population of older adults with diabetes, the role of the endocrinologist or the diabetes care specialist in the care of an individual patient may vary considerably during the course of the disease. Decision-making about this role requires active participation and good lines of communication among the endocrinologist or diabetes care specialist, the primary care physician, and the patient. Because of the high burden of diabetes and its complications on overall health status (21, 22), many older patients benefit from care by an interdisciplinary team. The endocrinologist or diabetes care specialist functions as the leader of the diabetes care team, which includes a nurse educator, dietician, and others (e.g., pharmacist, psychologist, social worker). The endocrinologist or diabetes care specialist may also serve the medical community by providing up-to-date training in the care of older patients with diabetes. Possible roles of the endocrinologist or diabetes care specialist include the following.
No role.
Diabetes care is provided by the patient’s primary care team, which has received up-to-date training in the care of older patients with diabetes. An endocrinologist or diabetes care specialist may not be needed for patients whose hyperglycemia and CVD prevention treatment goals are easily achieved with lifestyle alone or with simple oral agent therapy (one or two medications). Application of the Chronic Disease Model can facilitate diabetes quality care in the primary care setting (23).
Consultant-only collaborative care.
Overall diabetes care is provided by the patient’s primary care team. The endocrinologist or diabetes care specialist assists in assessing the patient’s diabetes status and related complications and setting treatment goals with recommendations for specific interventions. Consultation may occur at the time of original diabetes diagnosis or when there is a change in the patient’s diabetes status (e.g., treatment goals no longer being achieved, recurrent hypoglycemia, development of one or more diabetes complications). Consultation may involve only a member (not all) of the diabetes care team (e.g., nurse educator or dietician). The endocrinologist or diabetes care specialist may be asked to initiate insulin therapy for a patient and then send the patient back to the primary care provider once stable, or they may consult to assist with glycemic management when a patient is hospitalized.
Overall diabetes management.
For selected patients, the endocrinologist or diabetes care specialist and the diabetes care team are primarily responsible for diabetes care and collaborate with providers who manage the patient’s other health problems and comorbidities. This situation may occur by default if the patient has no primary care provider or if the patient is already under the care of the endocrinologist or diabetes care specialist for long-standing T1D or other endocrine conditions. Specific indications for the endocrinologist or diabetes care specialist to assume control of overall diabetes management for an older patient include complex hyperglycemia treatment (use of three or more glucose-lowering agents; the addition of insulin, especially multiple types or injections), recurrent severe hypoglycemia, multiple diabetes complications, and a long history of diabetes.
2. Screening for Diabetes and Prediabetes, and Diabetes Prevention
2.1 In patients aged 65 years and older without known diabetes, we recommend fasting plasma glucose and/or HbA1c screening to diagnose diabetes or prediabetes. (1|⊕⊕⊕⊕)
Technical remark: The measurement of HbA1c may be inaccurate in some people in this age group because of comorbidities that can affect the lifespan of red blood cells in the circulation. Although the optimal screening frequency for patients whose initial screening test is normal remains unclear, the writing committee advocates repeat screening every 2 years thereafter. As with any health screening, the decision about diabetes and prediabetes screening for an individual patient depends on whether some action will be taken as a result and the likelihood of benefit. For example, such screening may not be appropriate for an older patient with end-stage cancer or organ system failure. In these situations, shared decision-making with the patient is recommended.
2.2 In patients aged 65 years and older without known diabetes who meet the criteria for prediabetes by fasting plasma glucose or HbA1c, we suggest obtaining a 2-hour glucose post–oral glucose tolerance test measurement. (2|⊕⊕⊕O)
Technical remark: This recommendation is most applicable to high-risk patients with any of the following characteristics: overweight or obese, first-degree relative with diabetes, high-risk race/ethnicity (e.g., African American, Latino, Native American, Asian American, Pacific Islander), history of CVD, hypertension (≥140/90 mm Hg or on therapy for hypertension), high-density lipoprotein cholesterol level <35 mg/dL (0.90 mmol/L) and/or a triglyceride level >250 mg/dL (2.82 mmol/L), sleep apnea, or physical inactivity. Shared decision-making is advised for performing this procedure in frail older people or in those for whom it may be overly burdensome. Standard dietary preparation for an oral glucose tolerance test is advised.
2.3 In patients aged 65 years and older who have prediabetes, we recommend a lifestyle program similar to the Diabetes Prevention Program to delay progression to diabetes. (1|⊕⊕⊕⊕)
Technical remark: Metformin is not recommended for diabetes prevention at this time, as it is not approved by the Food and Drug Administration for this indication. As of 2018, a Diabetes Prevention Program–like lifestyle intervention is a covered benefit for Medicare beneficiaries in the United States who meet the criteria for prediabetes.
Evidence
The ADA defines diabetes and prediabetes based on glucose measures (24). Importantly, individuals with prediabetes are at increased risk for progression to diabetes and development of CVDs; Table 1 (24) lists the ADA criteria for prediabetes and diabetes. The fasting plasma glucose and HbA1c categories allow easy identification of both diabetes and prediabetes. However, many people over the age of 60 years affected with diabetes and prediabetes are not diagnosed unless an oral glucose tolerance test is performed (2). Importantly, individuals with prediabetes are at increased risk for progression to diabetes and development of CVDs. Population screening demonstrates a high rate of detection of newly diagnosed diabetes. Additionally, modeling such studies suggests that early detection and treatment of diabetes can reduce long-term complications (25). Furthermore, diabetes and prediabetes criteria predict risk for subsequent diabetes and CVD similarly in both older and younger people. The prevalence of disorders of sleep increases with age, and such disorders have been associated with the development or exacerbation of diabetes and risks of cardiovascular events. Therefore, assessment for sleep disorders and their treatment should be considered in older patients at risk for and with diabetes (26).
Table 1.
ADA Criteria for Prediabetes and Diabetes
| Prediabetesa | Diabetesb |
|---|---|
| FPG 100 mg/dL (5.6 mmol/L) to 125 mg/dL (6.9 mmol/L) = IFG | FPG ≥126 mg/dL (7.0 mmol/L) |
| OR | OR |
| 2-h PG during 75-g OGTT 140 mg/dL (7.8 mmol/L) to 199 mg/dL (11.0 mmol/L) = IGT | 2-h PG ≥200 mg/dL (11.1 mmol/L) during OGTTc |
| OR | OR |
| A1C 5.7%–6.4% (39–47 mmol/mol)d | A1C ≥6.5% (48 mmol/mol)d |
| OR | |
| In a patient with classic symptoms of hyperglycemia or hyperglycemic crisis, a random PG ≥200 mg/dL (11.1 mmol/L). |
[Data from American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2019. Diabetes Care. 2019;42:S13–s28].
Abbreviations: FPG, fasting PG; IFG, impaired fasting glucose; IGT, impaired glucose tolerance; OGTT, oral glucose tolerance test; PG, plasma glucose.
For all three tests, risk is continuous, extending below the lower limit of the range and becoming disproportionately greater at the higher end of the range.
In the absence of unequivocal hyperglycemia, diagnosis requires two abnormal test results from the same sample or in two separate test samples.
The test should be performed as described by the World Health Organization, using a glucose load containing the equivalent of 75-g anhydrous glucose dissolved in water.
The test should be performed in a laboratory using a method that is National Glycohemoglobin Standardization Program certified and standardized to the Diabetes Control and Complications Trial assay.
Progression from prediabetes to diabetes can be slowed substantially (27–30). Evidence supporting this observation includes recent meta-analyses involving nearly 50,000 subjects (31, 32). In people over the age of 60 years in the Diabetes Prevention Program, lifestyle intervention to reduce body weight and increase physical activity reduced the rate of progression to diabetes by 71% during 4 years (estimated number needed to treat to prevent one person progressing to diabetes, 5.6). The reduced rate of progression to diabetes was maintained during 15 years of follow-up, although the lifestyle intervention was much less intense during the last 10 years (28, 29). Notably, the impact of this intervention is cost-effective (27). Additionally, metformin was less effective in people over the age of 60 years (estimated number needed to treat, 39.2) in the Diabetes Prevention Program, and the meta-analyses suggest that drug treatment tends to have transitory effects on diabetes prevention.
3. Assessment of Older Patients With Diabetes
Overall health framework
3.1 In patients aged 65 years and older with diabetes, we advise assessing the patient’s overall health (see Table 2) and personal values prior to the determination of treatment goals and strategies (see Table 3). (Ungraded Good Practice Statement)
Evidence
The treatment strategies and goals developed for older adults depend on overall patient health, including medical complexity and functional status. Table 2 (33, 34) provides a guide for the comprehensive assessment of the older adult, including the general medical assessment and diabetes-focused evaluations. Functional status refers to a person’s ability to perform normal daily activities required to meet basic needs, fulfill usual roles, and maintain health and well-being (35). Both aging and diabetes are independent risk factors for impaired functional status, and the interaction of these two factors is highly complex and unique for each patient. For this reason, recent diabetes guidelines have generally concluded that care of the aging patient with diabetes requires an individualized, rather than purely algorithmic, approach (36–38). However, there is no standard tool recommended for the assessment and documentation of how effectively older adults function in their lives. Functional status is most often documented using subsets of specific activities that are necessary for living independently. They include activities of daily living (ADLs), that is, bathing, dressing, eating, toileting, and transferring, as well as instrumental ADLs (IADLs), that is, preparing meals, shopping, managing money, using the telephone, and managing medications (Table 2) (34). In patients with diabetes, deficits in IADLs identified during routine evaluation should trigger a more in-depth evaluation of the patient, including a detailed assessment of hypoglycemia and hyperglycemia, microvascular and macrovascular complications, and cognition, as discussed in depth in this guideline.
Overall health in older adults has been described in terms of frameworks or categories that guide the clinician to consider multiple factors when assessing the health of an adult over the age of 65 years. One such framework was developed by Blaum et al. (35) and was incorporated into the 2012 ADA consensus report on the care of older adults with diabetes. The Blaum framework suggests considering chronic diseases (fewer than three vs three or more), cognitive or visual impairment (none, mild, moderate to severe), and IADL dependencies (none vs two or more) to define functional status. This framework was used to identify three classes of patients corresponding to increasing levels of mortality risk and was thus validated as a tool for determining the likelihood of benefit of a treatment strategy based on life expectancy (39). Using this evidence, the Blaum categories and the 2012 ADA consensus report as guides, we developed a conceptual framework for overall health that categorizes patients into good health (group 1), intermediate health (group 2), and poor health (group 3) groups [Table 3 (39, 40) and “Setting glycemic targets and goals” under section 4 on “Treatment of Hyperglycemia”].
Frailty
Frailty can be defined as a state of increased vulnerability to physical or psychological stressors because of decreased physiological reserves in multiple organ systems that cause a limited capacity to maintain homeostasis. Moreover, it represents a predisability condition that can be responsive to intervention (41).
Screening for geriatric syndromes, including frailty, should be part of a stepped-care approach in older people with diabetes, particularly in primary and community care settings. Where there is evidence of moderate to severe physical or cognitive impairment or functional loss, referral to geriatricians or other skilled clinicians for a comprehensive assessment is needed. The importance of detecting frailty lies in the opportunity to consider targeted interventions that reduce functional decline and risk of disability.
Any report of a change in mobility, presence of falls, noticeable decrease in IADLs after recent discharge from a hospital, or presence of continuing fatigue should prompt the clinician to screen for functional loss and/or frailty [Table 4 (42–45)]. An initial screen for physical impairment can be obtained by using the following commonly employed measures in geriatric practice (46) [Table 5 (47–51)].
Table 4.
Tools to Detect Frailty
| Assessment Tool | Comments |
|---|---|
| Fried score | Well-established physical frailty tool based on data from the Cardiovascular Health Study; often seen as a reference frame for studies of frailty in community-dwelling older adults; requires two procedures/measures (gait speed and grip strength) and answers to three questions (relating to weight loss, level of exhaustion, and amount of physical activity); can identify “prefrail” individuals (42). |
| Clinical Frailty Scale (Note: A larger 70-item assessment tool called the Frailty Index is also available.) | Based on data from the Canadian Study of Health and Aging; seven-point scale; predictive of future events including mortality; easy to employ in routine clinical practice (43). |
| FRAIL score | Well-validated in multiple population groups; sensitivity and specificity similar to that of the Fried scale. Comprises only five questions (no procedures) covering fatigue, climbing stairs, walking, number of illnesses, and weight loss (44). |
[Reproduced with permission from Sinclair AJ, Abdelhafiz A, Dunning T, Izquierdo M, Rodriguez Manas L, Bourdel-Marchasson I, Morley JE, Munshi M, Woo J, Vellas B. An international position statement on the management of frailty in diabetes mellitus: summary of recommendations 2017. J Frailty Aging 2018;7:10–20.] (45)
Table 5.
Commonly Employed Measures to Screen for Physical Impairment
| Measure | Comments |
|---|---|
| Timed “get-up and go” test | Most adults can complete this test. Good correlation with gait speed, Barthel Index, and measures of balance (47, 48). |
| 4-m Gait speed | Robust, clinically friendly measure. Easy to perform. Can be used to measure functional status in older adults and to predict future health and well-being. Population norms available (49, 50). |
| Grip strength | Requires a dynamometer for objective measurement; normative ranges in older people available. Predictive of increased future functional limitations and disability, increased fracture risk, and increased all-cause mortality (51). |
Screening for sarcopenia
Sarcopenia is an age-related loss of muscle mass that has now been linked to progressive loss of muscle strength and reduced physical performance (52). Sarcopenia is accelerated in the presence of diabetes. Clinicians can refer patients with possible sarcopenia for a dual-energy X-ray absorptiometry scan, but this procedure is expensive and may not be convenient. Bioelectrical impedance analysis is an alternative method for the assessment of lean muscle mass and may be considered in place of dual-energy X-ray absorptiometry scanning. Alternatively, a rapid screening test for sarcopenia in a clinical setting can be obtained using a simple five-question instrument called the Sarc-F, which looks at fall history, ability to lift objects, and difficulties with mobility. This scale has been validated extensively and has been shown to be highly predictive of future disability and hospitalization (53).
Cognitive impairment in older adults with diabetes
In the general population, the prevalence of dementia increases from 1% to 2% at ages 60 to 64 years to 6% to 9% at ages 75 to 79 years to well above 35% in those who are 90 years and older (54). The population burden of cognitive impairment in older individuals is even larger if predementia stages of cognitive dysfunction, such as mild cognitive impairment (MCI), are also considered.
Epidemiological studies have found clear associations between diabetes and dementia risk (55). A meta-analysis including over 1 million individuals presented a pooled overall relative risk (RR) for dementia in people with diabetes of 1.73 (95% CI, 1.65 to 1.82) compared to people without diabetes (56). This increased risk was present in both Alzheimer’s disease (RR, 1.56; 95% CI, 1.41 to 1.73) and vascular dementia (RR, 2.27; 95% CI, 1.94 to 2.66) (56); notably, however, Alzheimer’s disease generally was not diagnosed with biomarker support in these epidemiological studies. Neuropathological studies indicate that diabetes is primarily associated with an increase in the burden of vascular pathologies rather than plaques and tangles, the neuropathological hallmarks of Alzheimer’s disease (57). Moreover, diabetes is associated with an increased risk of MCI (RR, 1.21; 95% CI, 1.02 to 1.45) (58) and an increased rate of conversion from MCI to dementia (OR, 1.65; 95% CI, 1.12 to 2.43) (59). Of note, these numbers primarily apply to patients with T2D because data on older individuals with T1D are still scarce.
With the aging of the population and trends in diabetes prevalence, the combination of cognitive impairment and diabetes is likely to become more common, having implications for diabetes care. Clearly, cognitive impairment in patients with diabetes is associated with poorer diabetes self-management and glycemic control (60, 61), an increased frequency of hospital admissions and occurrence of severe hypoglycemic episodes (62, 63), and an increased occurrence of major cardiovascular events and death (64). Early identification of individuals with cognitive impairment may avoid some of these poor outcomes (65–67). Of note, the relationship between some of these “outcomes” and cognitive impairment may be bidirectional: there are clear indications that CVD, but also occurrence of hypoglycemic episodes (68), increase the risk of developing cognitive impairment in older patients with diabetes.
Detection and diagnosis
3.2 In patients aged 65 years and older with diabetes, we suggest that periodic cognitive screening should be performed to identify undiagnosed cognitive impairment. (2|⊕⊕OO)
Technical remark: Use of validated self-administered tests is an efficient and cost-effective way to implement screening (see text). Alternative screening test options, such as the Mini-Mental State Examination or Montreal Cognitive Assessment, are widely used. An initial screening should be performed at the time of diagnosis or when a patient enters a care program. Screening should be repeated every 2 to 3 years after a normal screening test result for patients without cognitive complaints or repeated 1 year after a borderline normal test result. Always evaluate cognitive complaints and assess cognition in patients with complaints.
Evidence
In the general population, screening for cognitive impairment and dementia is currently not recommended because of insufficient evidence on the balance of benefits and harms of screening (69). This ratio may be different in people with diabetes because the harm of unrecognized cognitive impairment (e.g., risks related to diabetes treatment) might be larger than that in people without diabetes. The benefit of screening is that this harm might be at least partially avoided (67). Therefore, an active approach to the detection of cognitive impairment (i.e., screening) has been advocated for older adults with diabetes (65, 67). However, the evidence base upon which screening procedures can be operationalized (i.e., which target groups, type of test, frequency of testing) is limited. With regard to the target group, the chance of encountering cognitive impairment should be sufficiently high to warrant screening. At this stage, we therefore suggest that screening should be limited to those over the age of 65 years; in younger patients, actively responding to cognitive complaints should be sufficient.
The purpose of screening is to identify marked clinically relevant stages of cognitive impairment (i.e., MCI or dementia) likely to interfere with diabetes management. A positive screening test should be complemented by an appropriate diagnostic evaluation, starting with history taking, to formally diagnose or rule out these conditions. With regard to the choice of screening test, brief widely used tests such as the Mini-Mental State Examination or Montreal Cognitive Assessment may be suitable, although administering these tests still requires ∼10 minutes, and currently no strong evidence supports the choice of one particular test over another (70, 71). Notably, self-administered cognitive screening tools are becoming available and might offer an efficient alternative (72), greatly facilitating widespread implementation.
With regard to the timing and frequency of screening, performing an initial assessment at the time of diabetes diagnosis or when a patient enters a care program would be appropriate. Screening could then be repeated annually, or even less frequently, depending on the perceived risk. In patients without cognitive complaints, screening should be repeated 2 to 3 years after an initial normal screening test result or 1 year after a borderline normal test result. Cognitive complaints should always be evaluated.
Thus far, no evidence supports a benefit of intensive glycemic treatment to preserve cognitive function in patients with diabetes (68). However, further trials are underway, and cognition is increasingly considered an (secondary) outcome measure in drug trials in diabetes.
Management and treatment
3.3 In patients aged 65 years and older with diabetes and a diagnosis of cognitive impairment (i.e., MCI or dementia), we suggest that medication regimens should be simplified (see recommendation 3.1) and glycemic targets tailored (i.e., be more lenient; see recommendation 4.1) to improve compliance and prevent treatment-related complications. (2|⊕⊕OO)
Technical remark: Medical and nonmedical treatment and care for cognitive symptoms in people with diabetes and cognitive impairment is no different from those in people without diabetes and cognitive impairment. Depending on the situation and preferences of the patient, a primary caregiver can be involved in decision-making and management of medication.
Evidence
No randomized controlled trials (RCTs) have shown that simplified glucose-lowering treatment regimens improve adherence in patients with diabetes and cognitive impairment or that tailored glycemic targets reduce the risk of treatment-related adverse events, particularly hypoglycemic episodes. However, patients with impaired cognition are known to have lower adherence and an increased risk of adverse events (60, 61, 63). Furthermore, more stringent control increases the risk of hypoglycemia (see “Balancing risks and benefits of lower glycemic targets” under section 4 on “Treatment of Hyperglycemia”). Therefore, the assumption that simplifying treatments and tailoring targets improve compliance and prevent treatment-related complications in patients with impaired cognition is reasonable. HbA1c levels <8.0% (64 mmol/mol) have been proposed for mild-to-moderate cognitive impairment, and those below 8.5% (69 mmol/mol) for moderate to severe cognitive impairment (66).
With regard to patient care and management in those with cognitive impairment, regular review of the patient’s ability to self-manage diabetes and the need for appropriate support is essential. Providing support for caregivers and involving them in all aspects of care are also important.
4. Treatment of Hyperglycemia
Setting glycemic targets and goals
4.1 In patients aged 65 years and older with diabetes, we recommend that outpatient diabetes regimens be designed specifically to minimize hypoglycemia. (1|⊕⊕⊕O)
Technical remark: Although evidence for specific targets is lacking, glycemic targets should be tailored to overall health and management strategies (e.g., whether a medication that can cause hypoglycemia is used) (see Table 3).
Evidence
Hypoglycemia has both acute and chronic negative effects on individuals with diabetes in both outpatient and inpatient settings, although this section pertains to outpatient practice only (see “Special Settings and Populations” for evidence relevant to inpatient care). In the adult population aged 65 years and older, hypoglycemia appears to increase the risk of traumatic falls (73–75) and has a bidirectional relationship with cognitive dysfunction (see “Cognitive impairment in older adults with diabetes” under section 3 on “Assessment of Older Patients with Diabetes”). Hypoglycemia has also been associated with morbidity and mortality in post hoc analyses of data from large clinical trials that included older adults. In one study that analyzed data from the Action in Diabetes and Vascular Disease: Preterax and Dimicron Modified Release Controlled Evaluation (ADVANCE) trial, 231 patients had at least one severe hypoglycemic episode. Of these patients, most (65%) had been randomized to the intensive control arm of the trial (goal HbA1c <6.5%). The authors reported that severe hypoglycemia was associated with an approximate doubling of the adjusted risks of major macrovascular and microvascular events, death from a cardiovascular cause and death from any cause (P < 0.001). Severe hypoglycemia was also associated with other conditions such as respiratory and gastrointestinal conditions (76).
Although avoidance of hypoglycemia is a critical treatment strategy, overall glucose control remains an important goal. Blood glucose levels consistently over the renal threshold for glycosuria (>200 in chronic hyperglycemia, although variable) routinely increases the risk of dehydration, electrolyte abnormalities, urinary infections, dizziness, and falls. Hyperglycemic crises, including diabetic ketoacidosis, hyperglycemic hyperosmolar syndrome, and the combination of the two (hyperosmolar ketoacidosis), are severe complications of unrecognized or undertreated hyperglycemia in older adults. Older adults with these conditions have higher mortality rates than do younger individuals (77). Relaxing glycemic targets for older patients with a high burden of comorbidities and limited life expectancy may be appropriate, yet goals that minimize hyperglycemia are indicated for all patients.
Balancing risks and benefits of lower glycemic targets
As first noted in the Diabetes Control Complications Trial (DCCT), achieving a lower mean glucose to reduce complications may come at the cost of increased hypoglycemia risk (78). Because prevention of both microvascular and macrovascular disease via glycemic control may take years to realize, the health value of strict glycemic targets later in life has been controversial. National and international guidelines that address glycemic targets generally agree on individualizing care based on overall health status and weighing the expected timing of benefits against life expectancy (37, 79, 80).
Several studies have illustrated the clinical challenge of selecting glycemic targets by associating HbA1c achieved with mortality. One large retrospective analysis from the United Kingdom associated survival with HbA1c in a cohort of >40,000 individuals with T2D aged 50 years or older whose treatment had been intensified beyond oral monotherapy. The results showed a U-shaped association; the adjusted hazard ratios (HRs) of all-cause mortality were 1.52 (95% CI, 1.32 to 1.76) and 1.79 (95% CI, 1.56 to 2.06) in the groups with the lowest (median, 6.4%) and highest HbA1c (median, 10.5%) levels, respectively, compared with the group with a median HbA1c of 7.5% (81).
A secondary analysis of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) randomized trial further highlighted the complexity of targets by addressing setting vs achieving HbA1c targets. This trial compared the outcomes of achieving a relatively low glycemic target of HbA1c <6.5% with those of achieving an HbA1c of 7% to 7.9%. Multiple treatment options were available to providers to achieve glucose goals. After ∼5 years, the intensive treatment group had a 20% higher rate of mortality, which was significant, and subsequent analysis of 10,251 subjects enrolled in ACCORD indicated that the group of subjects who were unable to reach the intensive HbA1c target accounted for the excess mortality (82). This analysis also demonstrated that a higher average on-treatment HbA1c was a stronger predictor of mortality than was a lower HbA1c and that the risk of death with the intensive strategy increased linearly from 6% to 9% HbA1c (82). Of note, the progression of retinopathy was reduced by 30% with intensive control, although no measurements of functional status were reported for judging the impact on overall health (83). However, this finding was not reproduced in the recently published long-term results of the Veterans Affairs Diabetes Trial (VADT) (84).
Importantly, older individuals enrolled in diabetes clinical trials are more likely to have better overall health than are older individuals in the general population. Numerous studies successfully achieved standard glycemic targets without increased hypoglycemia in older adults with good or intermediate health (85, 86). Because these trials exclude older adults with poor health, they support the concept that intensive strategies for selected individuals can be effective and safe. The compendium of results from these and other published analyses suggests that although some patients may benefit from tighter targets, many are unable to reach these targets, and aggressive therapy may be harmful to some patients without the benefit of reducing complications.
Assessing glycemia in older adults with diabetes
4.2 In patients aged 65 years and older with diabetes who are treated with insulin, we recommend frequent fingerstick glucose monitoring and/or continuous glucose monitoring (to assess glycemia) in addition to HbA1c. (1|⊕⊕OO)
Evidence
Although measurement of HbA1c is a convenient and validated method for determining overall glycemic status, it does not assist in identifying hypoglycemia. In one study, 40 patients aged 69 years or older with HbA1c values ≥8% were evaluated with blinded continuous glucose monitoring (CGM) for 3 days. Most (70%) had T2D, and nearly all (93%) were treated with insulin. Nearly 75% of subjects experienced a glucose level <60 mg/dL despite an elevated HbA1c. Importantly, of the 102 hypoglycemic episodes recorded, 93% were unrecognized by symptoms or by fingerstick glucose measurements performed four times a day (87). Detailed assessment of glycemia in older adults may also indicate glycemic variability, which is directly calculated by CGM systems and predicts hypoglycemia in older adults with T1D (88).
Older adults with T2D also tend to display unique glucose patterns, with relatively more postprandial hyperglycemia than fasting hyperglycemia (89). Knowledge of such patterns should lead to more tailored and potentially safer medication regimens, for example, adding premeal insulin to one large meal per day instead of progressive titration of long-acting basal insulin.
When available, CGM is an important tool for safely addressing high-risk glycemic patterns. CGM use in older adults is limited and is variable across populations, including patients with T1D, those with T2D, those using insulin pump therapy, and those using multiple daily injections of insulin. Clinicians who prescribe CGM for older adults need to consider many factors, including use of personal vs intermittent diagnostic CGM, patient selection and individualized goals of CGM, patient access and affordability, and involvement of family and/or caregivers in sharing of glucose data. For those older adults who have been enrolled in clinical trials, CGM used intermittently or continuously appears to be a useful tool for guiding therapy to allow improved glycemic control without increased hypoglycemia. In a clinical trial by Vigersky et al. (90), individuals with T2D, including older adults, were randomized to intermittent real-time CGM to test the impact on glycemic control. The population included individuals using various antihyperglycemic agents, including basal insulin but excluding prandial insulin. Interestingly, the results indicated that intermittent CGM can assist both patients and providers in adjusting diabetes regimens to achieve lower targets without increasing hypoglycemia risk (90). In the older adult cohort of the DIAMOND study, 116 individuals ≥60 years of age with both T1D and T2D on multiple daily injections of insulin were randomized to either personal real-time CGM or to continuation of self-monitored blood glucose. At the end of 6 months, the CGM group demonstrated high use (97% of participants used CGM at least 6 days per week), greater HbA1c reduction, and less glycemic variability (91).
In addition to its limitations in identifying glucose patterns, the HbA1c test must be interpreted with caution, which is particularly significant in older adults given the increased likelihood of relevant conditions that may alter red blood cell turnover (e.g., advanced kidney disease, gastrointestinal bleeding, valvular heart disease). This topic has been explored in detail by others (92, 93).
Lifestyle interventions for older adults with diabetes
Lifestyle modifications
4.3 In patients aged 65 years and older with diabetes who are ambulatory, we recommend lifestyle modification as the first-line treatment of hyperglycemia. (1|⊕⊕⊕⊕)
Evidence
In overweight patients, lifestyle modifications resulting in as little as 5% weight loss can improve glycemic control and the need for medications to control glucose levels (94, 95). Nonetheless, older patients face a number of issues related to nutrition and exercise capacity. Weight loss should be approached with caution in older adults, as both intentional and unintentional weight loss may lead to severe nutritional deficiencies (40). The recommendation of a combination of physical activity and nutritional therapy, including the recommended intake of calcium, vitamin D, and other nutrients, is an appropriate strategy for this population. An increase in physical activity in older adults should reduce sedentary behavior, and moderate-intensity aerobic activity should be emphasized. Moreover, the activity plan must consider the older adult’s abilities and aerobic fitness after careful medical evaluation, including exercise testing and heart rate/blood pressure (BP) monitoring as needed. Activities aimed at increasing flexibility, muscle strength, and balance are also recommended (96).
Intensive education regarding carbohydrate and calorie counting and meal planning can be useful for individuals with an active lifestyle to effectively modify insulin dosing and improve glycemic control (97, 98). A simpler diabetes meal planning approach emphasizing portion control and healthful food choices may be more suitable for older individuals with cognitive impairment or learning difficulties (99, 100). In the case of sarcopenia, nutritional therapy coupled with exercise training is thought to be beneficial.
Nutrition
Nutrition is an integral component of diabetes self-care for all people with diabetes regardless of age (79, 101). Notably, nutritional guidelines do not differ for older adults with or without diabetes. However, older adults may experience unique challenges that impact their ability to follow a healthy diet (i.e., finances, buying food, preparing meals) or have a higher risk of malnutrition due to taste and smell alteration, dysphagia, deficient dentition, gastrointestinal dysfunction, anorexia, cognitive dysfunction, and/or depression (40, 102).
4.4 In patients aged 65 years and older with diabetes, we recommend assessing nutritional status to detect and manage malnutrition. (1|⊕⊕⊕⊕)
Technical remark: Nutritional status can be assessed using validated tools such as the Mini Nutritional Assessment and Short Nutritional Assessment Questionnaire.
Evidence
Many studies support early screening for malnutrition in older patients, especially those at high risk for malnutrition (acute care-admitted patients and home-care residents) (103, 104). Malnutrition is an important problem in the older adult population and has potentially serious consequences, such as prolonged hospitalization, increased costs, and a higher number of readmissions (105, 106). Therefore, early detection and management of malnutrition are crucial for preventing future complications. Moreover, a number of screening tools are already available to assess nutritional status, and certain assessments, such as the Mini Nutritional Assessment and Short Nutritional Assessment Questionnaire, can be easily administered to older individuals.
4.5 In patients aged 65 years and older with diabetes and frailty, we suggest the use of diets rich in protein and energy to prevent malnutrition and weight loss. (2|⊕⊕OO)
Evidence
Low-quality studies suggest that consuming energy-dense and protein-rich food could improve food consumption and prevent weight loss and malnutrition risk. Approximately 40% of older adults do not meet the recommended 0.8 g/kg protein intake requirement. The PROT-AGE study group has recently recommended an average daily intake in the range of 1.0 to 1.2 g/kg body weight/d for healthy older people and even 1.2 to 1.5 g/kg body weight/d in older patients with acute or chronic diseases. Furthermore, experts have proposed a protein intake of at least 1.5 g/kg/d (15% to 20% of the total caloric intake) in sarcopenic or cachectic older individuals (107). Studies on specific nutrients (protein supplements, branched-chain amino acids, creatine) have not shown consistent benefits (108), although the Society for Sarcopenia, Cachexia, and Wasting Diseases recommends measuring 25-hydroxyvitamin D levels and replacing them if low in all sarcopenic patients (109).
Nutrition plans for patients with diabetes are generally individualized healthy diets based on preferences, abilities, and treatment goals. We must emphasize healthful eating patterns consisting of nutrient-dense, high-quality foods rather than specific nutrients to improve overall health regarding body weight; glycemic, BP, and lipid targets; and reductions in the risk of diabetes complications (101). The Mediterranean (110), Dietary Approaches to Stop Hypertension (DASH) (111, 112), and plant-based (113) diets are all examples of healthful eating patterns.
Dietary guidelines recommend an increase in fiber intake of 25 to 35 g/d (114). Choosing vegetables, legumes, whole grains, and high-fiber breakfast cereals is the best way to increase fiber consumption, although increasing fiber should be avoided in cases of delayed gastric emptying (gastroparesis). Additionally, meeting fluid intake recommendations is important for preventing constipation and fecal impaction in older adults (115).
People with diabetes should limit their sodium consumption to <2300 mg/d. Palatability, availability, affordability, and the difficulty of achieving low-sodium recommendations in a nutritionally adequate diet are all important considerations (116). Additionally, older adults are much more likely to suffer the adverse effects of alcohol due to changes in their ability to metabolize alcohol, particularly those taking multiple medications and those who are at increased risk of adverse events (117, 118).
4.6 In patients aged 65 years and older with diabetes who cannot achieve glycemic targets with lifestyle modification, we suggest avoiding the use of restrictive diets and instead limiting consumption of simple sugars if patients are at risk for malnutrition. (2|⊕OOO)
Technical remark: Patients’ glycemic responses to changes in diet should be monitored closely. This recommendation applies to both older adults living in the community and those in nursing homes.
Evidence
For nursing home residents, some studies (119–121) suggest that it is better to use regular diets for nursing home residents with diabetes. Diets tailored to a patient’s culture, preferences, and personal goals might increase quality of life, satisfaction with meals, and nutritional status (119, 120). Moreover, short-term substitution of controlled diets with “diabetic diets” was not found to modify the level of glycemic control (122).
As the most common fluid and electrolyte disturbance in older adults, dehydration needs to be prevented and managed in people living in long-term care facilities (123). Many interventions can reduce its prevalence (124, 125) in this population and, notably, diuretics and antihypertensives should be carefully managed after admission to avoid contributing to fluid and electrolyte depletion.
For community-dwelling older adults, maintaining a nutrient-dense diet is essential for promoting health and preventing nutrition-related complications (126). Evidence indicates that restrictive diets impose significant risks of sarcopenia and malnutrition in community-dwelling older adults (127).
Drug therapy for hyperglycemia
Glycemic management of diabetes in older individuals
Glycemic management strategies must be adjusted to the individual needs of older patients. Specific factors regarding certain drug classes are particularly important for older people with diabetes, especially those with CKD and heart disease.
4.7 In patients aged 65 years and older with diabetes, we recommend metformin as the initial oral medication chosen for glycemic management in addition to lifestyle management. (1|⊕⊕⊕O)
Technical remark: This recommendation should not be implemented in patients who have significantly impaired kidney function [estimated GFR (eGFR) <30 mL/min/1.73 m2] or have a gastrointestinal intolerance.
Evidence
Metformin is highly effective, may reduce cardiovascular events and mortality, and does not cause hypoglycemia or weight gain (94, 95, 128, 129). As clinical events that may precipitate acute kidney injury, such as radiocontrast dye, nephrotoxic drugs, hypotension, heart failure, and surgery, may cause metformin accumulation, with a potential risk for lactic acidosis, metformin use is often stopped when patients are hospitalized. An additional concern is the development of vitamin B12 deficiency, and levels should be monitored yearly (130–133).
4.8 In patients aged 65 years and older with diabetes who have not achieved glycemic targets with metformin and lifestyle, we recommend that other oral or injectable agents and/or insulin should be added to metformin. (1|⊕⊕⊕⊕)
Technical remark: To reduce the risk of hypoglycemia, avoid using sulfonylureas (SUs) and glinides, and use insulin sparingly. Glycemic treatment regimens should be kept as simple as possible.
Evidence
SUs and glinides.
SUs, repaglinide, and nateglinide can cause hypoglycemia and weight gain. Glyburide should be avoided in older individuals because of a substantially increased risk of hypoglycemia compared with that of glimepiride and glipizide (130, 131, 134, 135).
Thiazolidinediones.
Pioglitazone and rosiglitazone can cause fluid retention and may precipitate or worsen heart failure; indeed, these drugs are contraindicated in patients with class III and IV heart failure (see “Management of congestive heart failure in older adults with diabetes” under section 5 on “Treating Complications of Diabetes”) (136–138). Furthermore, these medications are associated with increased fracture rates and bone loss in women (139, 140); thus, use in older women with underlying bone disease, such as osteoporosis, could potentially be problematic.
α-Glucosidase inhibitors.
α-Glucosidase inhibitors have only modest efficacy, and in older individuals, the gastrointestinal adverse effects of flatulence and diarrhea tend to cause a relatively high rate of nonadherence (141).
Dipeptidyl peptidase-4 inhibitors.
Dipeptidyl peptidase-4 (DPP-4) inhibitors are generally well tolerated. Importantly, early concerns regarding an increased risk of pancreatitis have not been borne out (142, 143), although some DPP-4 inhibitors have been associated with heart failure (see “Management of congestive heart failure in older adults with diabetes” under section 5 on “Treating Complications of Diabetes”).
Sodium-glucose cotransporter 2 inhibitors.
Sodium-glucose cotransporter 2 (SGLT2) inhibitors reduce HbA1c by ∼0.8%, can reduce weight, and do not cause hypoglycemia. Recently, both empagliflozin and canagliflozin have been shown to decrease major adverse cardiovascular events (MACE), heart failure, and the progression of CKD (144, 145). These compounds cause an obligate increase in urine volume and an increase in urogenital candida infections. Because adverse effects related to volume depletion were more frequent in older patients treated with canagliflozin, recommendations limit the dosage to 100 mg/d in such patients (146, 147). Canagliflozin has also been shown to be associated with a decrease in bone mineral density at the hip, but not the femoral neck, lumbar spine, or distal radius (148), with a significant increase in fractures of arms and legs but not the spine (149). Very rare cases of diabetic ketoacidosis have been reported in patients with T2D taking SGLT2 inhibitors, including patients over the age of 65 years (150, 151).
Glucagon-like peptide 1 receptor agonists.
Glucagon-like peptide 1 (GLP-1) receptor agonists increase insulin release, decrease glucagon secretion, delay gastric emptying, suppress appetite, and do not cause hypoglycemia; however, nausea is a common side effect (152). Initial concern about an increased risk for pancreatitis has not been proven (142, 143). Liraglutide and semaglutide have been found to improve cardiovascular outcomes (see “Congestive heart failure in older adults with diabetes” under section 5 on “Treating Complications of Diabetes”).
Insulin.
In patients with T2D, insulin therapy is usually initiated when oral agents do not provide sufficient glycemic control (153). Self-monitoring of blood glucose must be performed for insulin to be used safely and effectively.
Initially, a single long-acting insulin analog can be added as basal insulin therapy with dose adjustment to maintain fasting glucose in the desired range (79, 153, 154). Recently, insulin glargine U300 and insulin degludec, which are longer-acting basal insulins compared with insulin glargine U100, showed overall similar levels of glycemic control but with less variability and hypoglycemia (155, 156). If fasting glucose is near goal but the HbA1c remains above goal, rapid-acting insulin can be added first, prior to the largest meal and then prior to other meals, as necessary (79, 153, 154). Additionally, premixed insulins (neutral protamine hagedorn with regular or analog insulin) given twice daily may be a simpler approach (157), but the lack of flexibility, especially in patients who may skip or delay meals, may increase the risk of hypoglycemia (153).
Increasing from one to three or four injections per day means moving from a less complex to a more complex regimen, which may be limiting (79, 153, 154). The complexity of the treatment regimen must be balanced against the treatment goals and risks of hypoglycemia. For patients with arthritis of their hands, the use of insulin pens, or other assistive appliances, can be helpful.
Recently, fixed doses of GLP-1 receptor agonists and basal insulin, insulin degludec and liraglutide (IDegLira) and insulin glargine and lixisenatide (LixiLan), have become available in a single syringe, and thus only one injection is needed. A low dosage of the combination is started, and then the dosage is gradually titrated upward. Interestingly, studies have reported excellent reduction in HbA1c with less hypoglycemia and weight loss rather than weight gain compared with increased titration of basal insulin alone or intensification with basal/bolus insulin (158–160).
Values and preferences
Because T2D slowly worsens over time (161), increasing dosages and numbers of medications may be needed to control glucose levels. However, the sequence in which drugs should be added after metformin is not clear. Recent recommendations indicate that GLP-1 receptor agonists and SGLT2 inhibitors be prescribed early, given their beneficial cardiovascular outcomes (24, 162). In general, the more drugs that are prescribed, the poorer is adherence to a particular regimen (163). Of critical importance is the avoidance of hypoglycemia, which can have devastating outcomes in older patients. Thus, SUs and insulin should be avoided if at all possible.
5. Treating Complications of Diabetes
Macrovascular disease
Management of hypertension in older adults with diabetes
Hypertension is a well-known risk factor for cardiovascular and kidney disease. Lifestyle modification is generally advocated as the first treatment modality (see “Lifestyle interventions for older adults with diabetes” under section 4 on “Treatment of Hyperglycemia”), but one or more medications are usually needed for most patients. The goals of treatment and the specific medications used for treatment may differ between patients with diabetes and those without diabetes, particularly older adults.
5.1 In patients aged 65 to 85 years with diabetes, we recommend a target BP of 140/90 mm Hg to decrease the risk of CVD outcomes, stroke, and progressive CKD. (1|⊕⊕⊕O)
Technical remark: Patients in certain high-risk groups could be considered for lower BP targets (130/80 mm Hg), such as those with previous stroke or progressing CKD (eGFR <60 mL/min/1.73 m2 and/or albuminuria). If lower BP targets are selected, careful monitoring of such patients is needed to avoid orthostatic hypotension. Patients with high disease complexity (group 3, poor health, Table 3) could be considered for higher BP targets (145 to 160/90 mm Hg). Choosing a BP target involves shared decision-making between the clinician and patient, with full discussion of the benefits and risks of each target.
Evidence
In individuals who do not have diabetes (generally under the age of 65 years) many trials have shown that BP levels <140/90 mm Hg reduce mortality, MACE, and the progression of kidney disease. Thus, this level was recommended by the 2014 Eighth Joint National Committee evidence-based guideline for the management of high blood pressure in adults (164). In that guideline, the BP target for individuals >60 years of age is <150/90 mm Hg. However, the recent Systolic Blood Pressure Intervention Trial (SPRINT), which evaluated 9361 nondiabetic persons randomized to systolic BP (SBP) targets of <140 vs <120 mm Hg showed a 25% reduction in MACE and a 27% reduction in all-cause mortality with the more intensive treatment (165). The mean age of subjects entering SPRINT was 68.2 years, with 28% >75 years of age (165). Significant increases in rates of hypotension, syncope, electrolyte abnormalities, and acute kidney injury or failure were observed in the more intensively treated group, but these increases were not significantly greater in participants >75 years of age (165). The way in which BP was measured in SPRINT (unattended automated machine) was subsequently noted to yield a SBP 16 mm Hg lower than a standard office BP measurement (i.e., 136 vs 120 mm Hg) (166).
A systematic review and meta-analysis from the American College of Physicians and the American Academy of Family Physicians supported a level of <150/90 mm Hg for individuals aged 60 years or older with less consistent evidence for the SBP target of <120 mm Hg (167). The American College of Physicians and American Academy of Family Physicians guideline, titled “Pharmacologic treatment of hypertension in adults aged 60 years or older to higher versus lower BP targets,” contained a strong recommendation for an SBP <150 mm Hg in all patients, and a recommendation for a SBP <140 mm Hg for patients with a history of stroke or transient ischemic attacks and those at high cardiovascular risk (168). The 2017 Diabetes and Hypertension Position Statement from the ADA supported a target of <140/90 mm Hg for “fitter” older individuals but a higher SBP (145 to 160 mm Hg) for individuals with loss of autonomy or major functional limitations (169). However, the 2017 high BP guideline from the American College of Cardiology/American Heart Association redefined BP categories as normal (SBP <120 mm Hg, diastolic BP <80 mm Hg), elevated (SBP 120 to 129 mm Hg, diastolic BP 80 to 89 mm Hg), and hypertension (SBP ≥130 or diastolic BP ≥90 mm Hg) and recommended a target of <130/80 mm Hg for all adults, including those with diabetes, because of the increased cardiovascular risk in such patients. This recommendation was based primarily on the SPRINT data; however, the guideline acknowledged the lack of randomized trial data supporting this target in patients with diabetes (170).
Four large prospective randomized studies have been performed in patients with diabetes and targeted two different BP goals: the United Kingdom Prospective Diabetes Study (UKPDS) (171), the ACCORD study (172), the ADVANCE trial (173), and the Hypertension Optimal Treatment (HOT) trial (174). Overall, these studies generally support the goal of <140/90 mm Hg, although a post hoc report of SPRINT-eligible ACCORD-BP patients suggested that the SBP goal of 120 mm Hg also applied to patients with diabetes (175).
Similarly, the goal of <140/90 mm Hg rather than lower goals is supported by post hoc analyses of several other studies in patients with diabetes, including the Irbesartan Diabetic Nephropathy Trial (IDNT) (176), INVEST (177), the VADT (178), the Louisiana State University Hospital–Based Longitudinal Study (179, 180), and the Veterans Affairs Nephropathy in Diabetes Trial (181).
Moreover, several systematic reviews and meta-analyses have shown that an SBP treatment goal of 130 to 140 mm Hg is optimal and that a goal of <130 mm Hg is associated with a decrease in stroke risk. However, these reports show higher adverse effects [and even higher risk (J-curve) in some reviews] (182–188) and no further benefit to other CVD outcomes and mortality when SBP is <120 mm Hg.
Values and preferences
Although most studies and guidelines have recommended a BP target of <140/90 mm Hg, the 2017 American College of Cardiology/American Heart Association guideline recommends a target of <130/80 mm Hg, even in older patients with diabetes (170). Thus, treatment approaches and goals are controversial. Many clinicians may opt for this lower target in patients at high CVD risk after careful discussion of the pros and cons of such increased intensity of treatment with the patient.
Importantly, consideration should also be given to a higher BP target if the patient develops symptomatic orthostatic hypotension, and medications that tend to cause orthostatic hypotension should be avoided (189). Additionally, prescribing one or more hypertension medications to be taken at bedtime may have additional CVD benefits (190).
5.2 In patients aged 65 years and older with diabetes and hypertension, we recommend that an angiotensin-converting enzyme inhibitor or an angiotensin receptor blocker should be the first-line therapy. (1|⊕⊕⊕O)
Technical remark: If one class is not tolerated, the other should be substituted.
Evidence
Several studies have demonstrated a reduction in the progression of diabetic CKD with the use of angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) in patients with hypertension and advanced CKD (191–193). Subsequent head-to-head studies have shown that these two drug classes are essentially equivalent for diabetic CKD (194). Moreover, ACE inhibitors have been shown to significantly reduce the risk of all-cause and CVD mortality, MACE, and heart failure, whereas ARBs significantly reduce only the risk of heart failure. Neither drug class has been shown to significantly reduce the risk of stroke (195–197). ACE inhibitors also appear to reduce the progression of retinopathy (see “Eye complications in older adults with diabetes” under section 5 on “Treating Complications of Diabetes”). Therefore, ACE inhibitors and ARBs should be the first-line therapy used for the treatment of hypertension in older patients with diabetes and should be included when more than one medication is needed, especially if albuminuria is present (169). Nonetheless, these two drug classes should not be used together, especially in patients with CKD, due to increased risks of hyperkalemia and acute kidney injury (198).
Values and preferences
The need for more than one drug to treat hypertension is common in patients with T2D (199). Two drugs should be started together if the initial BP is ≥160/100 mm Hg (170, 200). The calcium channel blocker amlodipine has been shown to provide better cardiovascular outcomes than other agents by the Avoiding Cardiovascular Events Through Combination Therapy in Patients Living With Systolic Hypertension (ACCOMPLISH) study (201, 202) and is therefore commonly added as a secondary antihypertensive agent.
The question of the third or fourth drugs to be added after renin-angiotensin system blockers and calcium blockers has not been addressed in either controlled clinical trials or meta-analyses. Because hypertension involves a volume component in many patients with T2D, a thiazide diuretic is commonly recommended as the third drug unless the eGFR is <30 mL/min/1.73 m2, in which case a loop diuretic might be more appropriate (169, 202–204). If coronary artery disease is significant, a beta-blocker may be appropriate and can be added as a fourth drug to a prior three-drug regimen (205). If a beta-blocker is used, carvedilol has been shown to have fewer metabolic effects than metoprolol (206). Notably, when BP is not controlled with three or more medications, referral to a hypertension specialist is indicated (169).
Management of hyperlipidemia in older adults with diabetes
5.3 In patients aged 65 years and older with diabetes, we recommend an annual lipid profile. (1|⊕⊕OO)
5.4 In patients aged 65 years and older with diabetes, we recommend statin therapy and the use of an annual lipid profile to achieve the recommended levels for reducing absolute CVD events and all-cause mortality. (1|⊕⊕⊕⊕)
Technical remark: The Writing Committee did not rigorously evaluate the evidence for specific LDL-C targets in this population, so we refrained from endorsing specific LDL-C targets in this guideline. For patients aged 80 years old and older or with short life expectancy, we advocate that LDL-C goal levels should not be so strict.
Evidence
Epidemiological evidence documents that diabetes is an independent risk factor for CVD in both men and women. Furthermore, in patients with diabetes, all major cardiovascular risk factors, including cigarette smoking, hypertension, and high serum cholesterol (207–209), add to the degree of risk for CVD in older patients with diabetes. Individuals with diabetes have more than twice the risk for CVD than do those who do not have diabetes.
Cholesterol-lowering treatment with statins is equally efficacious in reducing RR and more effective in reducing absolute CVD events in older adults than in younger individuals because the older patients have a higher absolute risk for CVD. Most studies indicate that diabetic dyslipidemia in older adults is undertreated (210).
Numerous studies have confirmed the relationship between hypercholesterolemia and CVD, including myocardial infarction and stroke. Similarly, in large RCTs and multiple meta-analyses, statin use has been found to be effective in primary and secondary prevention when using myocardial infarction, revascularization and stroke as endpoints (211, 212).
Most patients aged 65 years and older with diabetes do not have marked elevations of LDL-C, because the method of measuring LDL-C underestimates the LDL particle number. However, these LDL-C levels are high enough to support the development of atherosclerosis (213). Because LDL-C may be normal but LDL particles may be small (213), risk stratification should be used to determine the level of LDL-C that should be achieved in older patients with diabetes using statins. Calculated non-HDL, which reflects all atherogenic particles, adds to the assessment of atherogenicity. Furthermore, risk stratification can be achieved by a number of CVD risk calculators, and, when indicated, coronary artery calcium may enhance risk stratification (214). Apolipoprotein B measurement can be useful in some patients to help refine their LDL treatment goal.
A role for LDL-C in hyperglycemic patients became apparent in several early large clinical trials [e.g., the 4S trial (215, 216), the Cholesterol and Recurrent Events (CARE) trial (217, 218), and the LIPID trial (219) using pravastatin]. In all of these trials, aggressive LDL-C–lowering therapy reduced recurrent CHD events in patients with diabetes, including those >65 years of age, by ∼25% to 35% (220, 221).
Additionally, the Treating to New Targets (TNT) study showed that patients with a high risk of CVD, including risk factors for diabetes and aging, should be treated with high doses of statins (atorvastatin at 80 mg vs atorvastatin at 10 mg) to reduce their LDL-C levels to <70 mg/dL and improve CVD outcomes (222). In contrast to statins, fibrates did not cause a significant reduction in stroke events compared with placebo in clinical trials.
The Prospective Study of Pravastatin in the Elderly at Risk (PROSPER) trial (223) included men and women, and the average age was 75 years. Approximately 8% of the participants had diabetes, and 3 years of pravastatin treatment reduced CVD during the subsequent 8 years. The average age in the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial (224) was 63 years, and ∼16% of the patients had diabetes. High-dose atorvastatin was shown to reduce recurrent stroke by almost 25% in this trial. Most studies have included men and women >65 years of age, and subgroup analyses have also shown beneficial results for patients with known diabetes. Overall, older patients with diabetes experienced a 35% decrease in CVD events from statin therapy, and side effects were minimal. In general, high-dose statin therapy is indicated for all patients with diabetes, irrespective of age, unless specifically contraindicated. Furthermore, although LDL-C levels are not necessarily elevated in patients with diabetes, statins still have a profound effect on the prevention of CVD, and thus all patients with T2D should be treated with statins. (Caveat: Most, but not all, studies support the value of statin use in the prevention of CVD in patients with diabetes.)
As described in the technical remark, the Writing Committee did not rigorously evaluate the evidence for specific LDL-C targets in older patients with diabetes. Therefore, we refrained from proposing specific LDL-C targets. The reader is referred to numerous guidelines and consensus statements that address this important topic (Table 6).
Table 6.
Related Guideline Content Table
| Rec. Number | Guideline Title | Publishing Organization | Publication Year |
|---|---|---|---|
| 2.3, 5.10, 5.13 | Standards of Medical Care in Diabetes 2019 | American Diabetes Association | 2019 |
| 3.2 | Standards of Medical Care in Diabetes 2019 | American Diabetes Association | 2019 |
| 4.1 | Management of Diabetes Mellitus in Primary Care (2017) | U.S. Department of Veterans Affairs and Department of Defense | 2017 |
| 4.7 | Oral Pharmacologic Treatment of Type 2 Diabetes Mellitus: A Clinical Practice Guideline Update from the American College of Physicians | American College of Physicians | 2017 |
| 5.1 | 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report from the Panel Members Appointed to the Eighth Joint National Committee (JNC 8) | Eighth Joint National Committee (JNC 8) | 2014 |
| 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines | American College of Cardiology/American Heart Association | 2017 | |
| Pharmacologic Treatment of Hypertension in Adults Aged 60 Years or Older to Higher vs Lower Blood Pressure Targets: A Clinical Practice Guideline from the American College of Physicians and the American Academy of Family Physicians | American College of Physicians/American Academy of Family Physicians | 2017 | |
| 5.3, 5.4 | American Association of Clinical Endocrinologists and American College of Endocrinology Guidelines for Management of Dyslipidemia and Prevention of Cardiovascular Disease | American Association of Clinical Endocrinologists | 2017 |
| 5.7 | Treatment of Diabetes in People With Heart Failure: Diabetes Canada Clinical Practice Guideline | Diabetes Canada | 2018 |
| 5.14 | Standards of Medical Care in Diabetes 2019 | American Diabetes Association | 2019 |
| 6.3 | Position Statement Executive Summary: Guidelines and Recommendations for Laboratory Analysis in the Diagnosis and Management of Diabetes Mellitus | National Academy of Clinical Biochemistry | 2011 |
5.5 In patients aged 65 years and older with diabetes, we suggest that if statin therapy is inadequate for reaching the LDL-C reduction goal, either because of side effects or because the LDL-C target is elusive, then alternative or additional approaches [such as including ezetimibe or proprotein convertase subtilisin/kexin type 9 inhibitors (PCSK9)] should be initiated. (2|⊕OOO)
Evidence
In statin-intolerant patients, ezetimibe may be administered to inhibit cholesterol absorption from the gastrointestinal tract (225). The Improved Reduction of Outcomes: Vytorin Efficacy International Trial (IMPROVE-IT) demonstrated that the addition of ezetimibe to statin therapy positively affected CVD in patients with acute coronary syndrome. The combination of these two agents decreased the LDL level to 53 mg/dL. In this trial, many of the patients were older than 65 years, and the CVD benefit was observed primarily in patients with diabetes (226, 227).
Additionally, PCSK9 inhibition has been shown to reduce LDL-C levels more than high-dose statins and to also reduce CVD outcomes. PCSK9 inhibitors have been approved for patients who are unable to reach the LDL goal with the maximally tolerated statin dose, those with clinical CVD on high-dose statins who have not reduced their LDL-C levels to target (228, 229), and those with familial hypercholesterolemia.
5.6 In patients aged 65 years and older with diabetes and fasting triglycerides >500 mg/dL, we recommend the use of fish oil and/or fenofibrate to reduce the risk of pancreatitis. (1|⊕⊕OO)
Evidence
The use of fibrates, as demonstrated in the Fenofibrate Intervention and Event Lowering in Diabetes (FIELD) study, resulted in no significant benefit regarding the primary endpoint or mortality, and it is therefore not recommended for CVD prevention in patients with diabetes. Importantly, fibrates in combination with statin therapy should be used together cautiously in view of an enhanced risk of myopathy, although this combination can be useful in treating patients with triglyceride levels >500 mg/mL and who are at risk for pancreatitis (230, 231). There is also evidence that fenofibrate may be valuable in preventing the progression of retinopathy (232, 233).
Management of congestive heart failure in older adults with diabetes
Epidemiology, morbidity, and mortality.
Aging and diabetes have a profound effect on the cardiovascular system structure and function that increases the risk of CHF. Aging increases vascular stiffness and reduces elasticity, leading to increased SBP, myocyte hypertrophy, and impaired diastolic function (234). Diabetes increases the risk of CHF due to associated comorbidities such as hypertension and complications such as macrovascular and microvascular disease and also directly affects the myocardium, causing cardiomyopathy (235–237). Therefore, the prevalence of CHF in older people with diabetes is high, reaching up to 30.6%, which is four times higher than expected in older adults without diabetes (238). Patients with both diabetes and CHF are at particular risk of adverse events. In the Reduction of Atherothrombosis for Continued Health (REACH) registry, which included 19,699 patients with diabetes and a mean age of 68.4 years, diabetes was associated with a 33% higher risk of hospitalization for CHF (9.4% vs 5.9%; adjusted OR, 1.33; 95% CI, 1.18 to 1.50). CHF at baseline was independently associated with cardiovascular mortality (HR, 2.45; 95% CI, 2.17 to 2.77; P < 0.001) and hospitalization (adjusted OR, 4.72; 95% CI, 4.22 to 5.29; P < 0.001), highlighting the need for adequate treatment of CHF in this population (239).
5.7 In patients aged 65 years and older who have diabetes and CHF, we advise treatment in accordance with published clinical practice guidelines on CHF. (Ungraded Good Practice Statement)
Evidence
CHF medications act in essentially the same way in those with and without diabetes. Nevertheless, the cardiovascular safety of the various classes of hypoglycemic medications is less well understood. Hyperglycemia increases the risk of CHF and hence should be controlled, although no direct evidence supports a reduction in the risk of CHF by treating hyperglycemia. Despite the common coexistence of diabetes and CHF in older people, optimal management is not fully evidence-based due to a lack of clinical trials in this age group. For this reason, treatment according to the recently published clinical practice guidelines is recommended (Table 6).
5.8 In patients aged 65 years and older who have diabetes and CHF, the following oral hypoglycemic agents should be prescribed with caution to prevent worsening of heart failure: glinides, rosiglitazone, pioglitazone, and DPP-4 inhibitors. (Ungraded Good Practice Statement)
Evidence
In a systematic review of observational studies including 34,000 patients with diabetes and CHF, metformin was associated with reduced mortality (23% vs 37%; adjusted risk estimate, 0.80; 95% CI, 0.74 to 0.87; P < 0.001), reduced all-cause hospitalizations (0.93, 95% CI, 0.89 to 0.98; P = 0.01), and low risk of lactic acidosis (240). No associations of SUs, insulin, acarbose, or glinides with CHF or mortality were found (241–243), but one study did suggest a possible link between glinides and heart failure (244). Moreover, rosiglitazone increased the risk of all-cause mortality (HR, 1.50; 95% CI, 0.49 to 4.59) and hospitalizations for CHF (RR, 1.30; 95% CI, 0.35 to 4.82) (245). A limited meta-analysis of seven RCTs reported that the risk for CHF was less with pioglitazone than with rosiglitazone (1.32, 1.04 to 1.68 vs 2.41, 1.61 to 3.61) and that the risk of cardiovascular death did not increase with either drug (0.93, 0.67 to 1.29, P = 0.68) (246). A more comprehensive meta-analysis of 94 RCTs demonstrated that pioglitazone was associated with reduced all-cause mortality (OR, 0.30; 95% CI, 0.14 to 0.63; P = 0.05) but with a nonsignificant increase in CHF (OR, 1.38; 95% CI, 0.90 to 2.12) (247).
Interestingly, the risk for hospitalization for CHF with DPP-4 inhibitors is inconsistent. The HR was significant for saxagliptin (HR, 1.27; 95% CI, 1.07 to 1.51) (248), marginally increased but not significant for alogliptin (HR, 1.19; 95% CI, 0.90 to 1.58) (249), and neutral for sitagliptin (HR, 1.00; 95% CI, 0.83 to 1.20) (250). Notably, the ability of these studies to detect CHF hospitalization risk with certainty may be limited, and further evidence is needed.
No increased risk of CHF hospitalization (HR, 0.96; 95% CI, 0.82 to 1.16) or mortality (HR, 0.94; 95% CI, 0.78 to 1.13) was found for the GLP-1 analog lixisenatide (251). In the recently published results of the LEADER trial, treatment with liraglutide compared with placebo was associated with significant cardiovascular benefits in high-risk T2D patients, although the mean age was ∼64 years. Furthermore, the SGLT2 inhibitor empagliflozin showed a decreased HR for hospitalization for heart failure (0.65; 95% CI, 0.50 to 0.85) and all-cause mortality (0.68; 95% CI, 0.57 to 0.82). Canagliflozin showed a similar benefit for heart failure in the CANVAS study (144). In advanced CHF, palliative care with a focus on symptom control is effective in improving quality of life as well as reducing hypoglycemic medications in frail older people, as they are often unnecessarily overtreated (252, 253).
The cardiovascular safety profile of the SGLT2 inhibitor dapagliflozin has also recently been studied in a large randomized, placebo-controlled study (median duration of 4.2 years) of adults with T2D. A key result was a lower rate of cardiovascular death or hospitalization for heart failure (4.9% vs 5.8%; HR, 0.83; 95% CI, 0.73 to 0.95; P = 0.005), which reflected a lower rate of hospitalization for heart failure (HR, 0.73; 95% CI, 0.61 to 0.88) (254). This appears to confirm a view held that these benefits are likely a class effect (255).
In contrast to the effects on the heart, an increase in lower extremity amputations was observed in patients taking canagliflozin in another long-term cardiovascular outcome study (CANVAS) (144), and the Food and Drug Administration (FDA) now requires a boxed warning regarding this effect of this medication (256).
Management of atherosclerosis in older adults with diabetes
Epidemiology, morbidity, and mortality.
Aging and diabetes have a synergistic effect on the structure and function of the vascular system that increases the risk of vascular disease. Increased arterial wall thickening and stiffening and reduced compliance occur with aging (257). With diabetes, endothelin (vasoconstrictor and procoagulant) production increases, and nitric oxide production (vasodilator) decreases, shifting the balance toward a vasoconstrictor, procoagulant, proliferative, and proinflammatory state that leads to the development of atherosclerosis (258). Contributors to progressive atherosclerosis include hyperglycemia, dyslipidemia, obesity, and hypertension (259). Moreover, diabetes increases the risk of ischemic stroke by twofold, independently of BP, as well as the RR of in-hospital or 30-day stroke-related mortality. Diabetes substantially increases the risk of peripheral arterial disease and its associated mortality by nearly twofold and increases peripheral arterial disease–related costs and length of hospital stay (260, 261). According to one recent study, there is little or no increase in risk of mortality, myocardial infarction, or stroke if the following five risk factors are within normal ranges in patients with T2D: HbA1c, LDL, albuminuria, smoking status, and BP (262). Although the available evidence suggests that large reductions in the classic complications of T2D, mainly myocardial infarction, stroke, amputations, and mortality, have occurred during the past 20 years (263), the burden of atherosclerosis in older patients with diabetes remains substantial, and multifactorial intervention in this age group is essential. Moreover, the ADA also notes that addressing multiple cardiovascular risk factors at the same time can lead to greater benefits (24).
Lifestyle interventions including exercise and weight loss in obese older patients reduce intrahepatic fat content, increase insulin sensitivity, and improve overall metabolic risk factors for atherosclerosis (11, 264). Clinical trials have shown that in older patients with diabetes, tight glycemic control with HbA1c no lower than 7.5% will have a cardiovascular benefit after at least 10 years of treatment (128, 265–267). Notably, patients >80 years old or those with multiple comorbidities were excluded from these trials. Furthermore, metformin treatment is associated with improved cardiovascular outcomes, regression of atherosclerosis, and low risk of lactic acidosis (268–270). In the EMPA-REG OUTCOME trial (271), the SGLT2 inhibitor empagliflozin showed lower rates of combined cardiovascular mortality, nonfatal myocardial infarction, and nonfatal stroke (HR, 0.86; 95% CI, 0.74 to 0.99; P = 0.04] and all-cause mortality (HR, 0.68; 95% CI, 0.57 to 0.82). In a recently completed randomized trial of canagliflozin vs placebo in T2D (mean age of 63.3 years) with high cardiovascular risk (CANVAS study), canagliflozin significantly reduced (P < 0.001 for noninferiority; P = 0.02 for superiority) the rate of the primary outcome (a composite of death from cardiovascular causes, nonfatal myocardial infarction, or nonfatal stroke) (144). Moreover, results from the LEADER trial demonstrated significant cardiovascular benefits from liraglutide in comparison with placebo (272).
The thiazolidinedione rosiglitazone was previously shown to increase the risk of myocardial infarction (OR, 1.43; 95% CI, 1.03 to 1.98; P = 0.03) and cardiovascular mortality (OR, 1.64; 95% CI, 0.98 to 2.74; P = 0.06) (273), but following extensive monitoring by the FDA, no new adverse safety data have been demonstrated. The FDA has now entirely lifted the risk evaluation and mitigation strategy for rosiglitazone. Pioglitazone has been shown to reduce the composite of all-cause mortality, nonfatal myocardial infarction, and stroke in patients with T2D who have a high risk of macrovascular events following a large randomized controlled trial >5,000 patients with T2D with evidence of macrovascular disease (PROactive Study) (274).
Other hypoglycemic agents seem to have a neutral effect on cardiovascular outcome (247–251, 275), although the addition of glinides or α-glucosidase inhibitors to metformin therapy showed a reduction in risk of acute myocardial infarction (HR, 0.39, 95% CI, 0.20 to 0.75; and HR, 0.54; 95% CI, 0.31 to 0.95; respectively) (243). A meta-analysis of clinical trials of hypertension treatment in T2D showed that cardiovascular outcomes reached a plateau after attaining an SBP of 140 mm Hg. More intensive SBP control to ≤130 mm Hg was associated with a greater reduction in stroke but a significant increase in serious adverse events (276). A more recent meta-analysis confirmed the cardiovascular benefits of lowering SBP to 140 mm Hg but demonstrated that further reduction is associated with an increased risk of cardiovascular death, with no stroke reduction benefit (187). In a population-based cohort study of patients ≥85 years old, there was a U-shaped curve with a SBP of 164.2 mm Hg (95% CI, 154.1 to 183.8 mm Hg) being associated with the lowest mortality (277). All antihypertensive medications can be used in the treatment of hypertension in older people with diabetes, as no difference in mortality was observed with one drug class over the others, and the benefit may be due to the reduction in BP rather than a class effect (278). The benefit of statins in reducing cardiovascular risk is established. However, the evidence in older people is largely extrapolated from trials in younger populations. The PROSPER trial was designed for older people aged 70 to 82 years and showed 15% lower cardiovascular endpoints in the statin group (279). Interestingly, the addition of fibrate or niacin to statin therapy has shown no extra cardiovascular benefit (280, 281). Older patients with diabetes have a high burden of atherosclerosis and are likely to benefit from aspirin therapy after assessment of their bleeding risk (282, 283). Overall, frail older individuals with diabetes are unnecessarily overtreated, and reducing polypharmacy in this group may improve their quality of life.
5.9 In patients aged 65 years and older with diabetes and a history of atherosclerotic CVD, we recommend low-dosage aspirin (75 to 162 mg/d) for secondary prevention of CVD after careful assessment of bleeding risk and collaborative decision-making with the patient, family, and other caregivers. (1|⊕⊕OO)
Evidence
The primary prevention of cardiovascular events in older patients with diabetes is challenging because of a general lack of evidence for safe and effective treatment in this age group. Older patients with diabetes have a higher baseline cardiovascular risk and therefore are likely to benefit more from risk reduction than are younger patients without diabetes. However, this group of patients is largely heterogeneous with various levels of functional ability and life expectancy, which should be considered, as the current evidence is not generalizable to patients with poor functional status or multiple comorbidities or those with limited life expectancy.
Aspirin use in secondary prevention of CVD is now well established and has been shown to be effective in reducing cardiovascular morbidity and mortality in patients with a history of CVD (282). The main adverse effect is an increased risk of gastrointestinal bleeding. The excess risk may be as high as 5 per 1000 per year in real-world settings (24).
The evidence for use of aspirin in primary prevention, however, has been conflicting and unclear. In a recent randomized trial of aspirin vs placebo in >15,000 adults with diabetes but no evidence of CVD with a follow-up of 7.4 years, the aspirin group had significantly fewer serious vascular events [658 participants [8.5%] vs 743 [9.6%]; rate ratio, 0.88; 95% CI, 0.79 to 0.97; P = 0.01] but a significant excess of major bleeding events (rate ratio, 1.29; 95% CI, 1.09 to 1.52; P = 0.003) (284). Currently, the use of aspirin for primary prevention must remain a decision by the clinician on an individualized basis.
Microvascular disease
Eye complications in older adults with diabetes
Responses to standardized questionnaires suggest that vision loss due to diabetic retinopathy may significantly reduce quality of life and that treatment satisfaction may be significantly affected by the severity of macular edema (285–289). Retinopathy and neuropathy may affect the ability of a person to safely operate a motor vehicle (290).
The duration of diabetes predicts the presence of retinopathy, and control of hyperglycemia profoundly affects the onset and progression of diabetic retinopathy in both T1D and T2D (78, 231, 291–295). The beneficial microvascular effects of intensive glycemic control persisted after closeout of the DCCT research group, UKPDS, and ACCORD trials (128, 233, 296). In addition to poor glycemic control, the presence of albuminuria, hypertension, and dyslipidemia predict retinopathy (297–301). Furthermore, the observed present-day decline in the prevalence and incidence of retinopathy and vision impairment is thought to be the result of improved management of hyperglycemia, hypertension, and dyslipidemia (299, 302). In a Medicare study comparing 119 pairs of patients who received guideline care vs the closest matched controls who did not, low vision/blindness was substantially reduced during a 3-year period among persons who received recommended levels of care (300, 303, 304).
The benefit of strict BP control with respect to retinopathy, which was suggested in the UKPDS study (305) but not confirmed in the ACCORD study (231, 306), has not been consistently demonstrated. The use of ACE inhibitors or ARBs may have beneficial effects on retinopathy (307–310).
Treatment with fenofibrate in trials intended for assessing cardiovascular protection has suggested that this drug may reduce the progression of diabetic retinopathy, but continued treatment beyond the closing of the clinical trials may be required to confer this benefit (231–233, 301, 311, 312). There is worldwide interest in developing evidence to support the use of fenofibrate for limiting the progression of diabetic retinopathy, but its safety and efficacy might best be justified by evidence from trials that are designed to examine visual and retinal findings as their primary outcome measures.
5.10 In patients aged 65 years and older with diabetes, we recommend annual comprehensive eye examinations to detect retinal disease (1|⊕⊕⊕⊕).
Technical remark: Screening and treatment should be conducted by an ophthalmologist or optometrist in line with present-day standards.
Evidence
Periodic screening is justified for detecting vision-threatening retinopathy at an early stage and for offering measures to reduce its progression (301). Panretinal photocoagulation is the mainstay of treatment of proliferative retinopathy but may produce an exacerbation of diabetic macular edema, a condition that affects a substantial number of older patients (313–316). A study of 76,127 patients with diabetes in a UK database reported that center-involving diabetic macular edema, potentially amenable to anti–vascular endothelial growth factor (VEGF) therapy, was present in the eyes of almost 10% of these patients (314). In an incident population of 64,983 patients with diabetes in a UK primary care setting, close to 28% of patients developed retinopathy, and close to 4% developed maculopathy (half were macular edema) within 9 years of diabetes diagnosis (315). Among persons ≥40 years of age in the United States with diabetes and retinal photographs, the prevalence of macular edema may be ∼3.8%, with no differences among age groups. Rather, the risk is associated with duration of diabetes and HbA1c (316). Such data, together with the impact of retinal edema on vision, suggest that a large number of older patients might experience improvements in vision and quality of life from anti-VEGF therapy. Intravitreal anti-VEGF therapy may be the most effective front-line modality for macular edema and may be an alternative to panretinal photocoagulation in the treatment of proliferative diabetic retinopathy (301, 317–324).
Notably, Medicare claims data suggest that diabetic retinopathy may be associated with an increased risk of age-related macular degeneration (325). Open-angle glaucoma and cataracts occur more commonly among persons with diabetes (326, 327). Moreover, the risk for glaucoma increases with the duration of diabetes and fasting hyperglycemia. Among older persons with T2D or T1D for 5 years, these additional risks lead us not only to endorse the recommendation of the ADA for an initial dilated and comprehensive eye examination by an ophthalmologist or optometrist but also to suggest screening thereafter at least annually (300, 301).
Neuropathy, falls, and lower extremity problems in older adults with diabetes
5.11 In patients aged 65 years and older with diabetes and advanced chronic sensorimotor distal polyneuropathy, we suggest treatment regimens that minimize fall risk, such as the minimized use of sedative drugs or drugs that promote orthostatic hypotension and/or hypoglycemia. (2|⊕OOO)
5.12 In patients aged 65 years and older with diabetes and peripheral neuropathy with balance and gait problems, we suggest referral to physical therapy or a fall management program to reduce the risk of fractures and fracture-related complications. (2|⊕OOO)
Evidence
The prevalence of diabetic neuropathy appears to be increasing and is correlated with increased age, duration of diabetes, higher HbA1c, and lifelong glycemic control (328–332). Manifestations of the most common form of diabetic neuropathy, chronic sensorimotor distal polyneuropathy, may include not only a history of pain but also advanced findings of proprioceptive deficit, motor strength loss, contractures, deformities, weakness of the extremities, and/or Charcot arthropathies. Persons treated with metformin and having neuropathic manifestations should be evaluated because metformin may cause vitamin B12 deficiency. The heterogeneity of peripheral and autonomic neuropathies in diabetes necessitates consideration of a differential diagnosis, especially if manifestations are lateralized or atypical (333–337).
Persons with diabetes are at increased risk of falls and hip fracture (338–343). Thus, inquiry about falls should occur at least annually (344). Evidence is inconclusive on whether specific glycemic targets or antihyperglycemic treatment regimens promote falls (345–348). Thiazolidinediones and SGLT-2 inhibitors might worsen fall-related outcomes by increasing fracture risk (140, 347, 349). Furthermore, hypoglycemia may be a risk factor for adverse outcomes of falls (73–75). Pharmacologic therapy for painful diabetic neuropathy requires caution in older adults, with special concern for polypharmacy, oversedation, and orthostasis (342, 350–354).
Neuropathy is associated with increased risk of falls in older individuals with diabetes (345, 346, 355–358), and exploratory studies have found associations between diabetic neuropathy and abnormalities in gait, posture, and balance (359–362). Physical therapy interventions for those with functional deficits may reduce risk factors for falls and possibly the actual rate of falls and fractures (363–366). In the presence of advanced manifestations of distal polyneuropathy, we suggest consultation with physical therapists for improvement in balance, gait, posture, and strength and/or suggested use of assistive devices. Referrals might specify imbalance, unsteadiness on feet, abnormality in gait, foot drop, history of falling, neuropathic foot ulcer, lack of coordination, or other functional deficits or consequences traceable to neuropathy.
5.13 In patients aged 65 years and older with diabetes and peripheral neuropathy and/or peripheral vascular disease, we suggest referral to a podiatrist, orthopedist, or vascular specialist for preventive care to reduce the risk of foot ulceration and/or lower extremity amputation. (2|⊕⊕OO)
Evidence
Lower extremity amputation for nontraumatic indications is performed relatively infrequently but with higher incidence among individuals with diabetes, and individuals in some populations and geographic areas are at disproportionate risk for this situation (367–370). Among the 60- to 69-year-old group in a large cohort study, the incidence of lower extremity amputation was 290% greater for those with a longer duration of diabetes (371). Evidence possibly linking amputation to canagliflozin therapy is preliminary (144). Variably reported individual patient risk factors for lower extremity amputation may include peripheral sensory neuropathy, autonomic neuropathy, gait abnormalities, peripheral vascular disease, foot ulcer, history of previous amputation, certain foot deformities, greater body mass, chronic renal failure, poor vision, older age, and higher HbA1c (372–379).
Foot ulcer increases amputation risk and utilization of medical care (380–383). However, further research is necessary to confirm trends in amputation rates and to establish whether a program of comprehensive foot care or specific management strategies for established foot complications may reduce the risk for amputation among older persons with diabetes (263, 330, 384–392). We endorse the standard of care concerning foot care as expressed by the ADA, which recommends patient self-care education, specifies the content and frequency of periodic comprehensive foot evaluations, recommends a multidisciplinary approach for foot ulcers and high-risk feet, and presents indications for referral for further vascular assessment, ongoing preventive care, and lifelong surveillance by foot care specialists (300). Examiners should identify any history of foot ulcer, poorly fitted footwear, loss of protective sensation, vascular insufficiency, foot deformity, or preulcerative lesion. For patients with altered gait due to neuropathy, local foot deformity, or unhealed ulcers, exercise programs may need to focus on non–weight-bearing activities (393). Furthermore, specialty care may be required to determine the appropriateness of off-loading devices, monitoring of foot skin temperature, use of therapeutic footwear, and need for vascular or podiatric surgical interventions (382, 394, 395).
Lower extremity amputation is associated with reduced survival and a reduction in physical health-related quality of life, as well as delayed recovery and impaired return to baseline function among nursing home residents (1, 396, 397).
The risk factor of vascular insufficiency must be considered among persons with diabetic foot ulcers (398, 399). The goals of lower extremity revascularization in older patients include maintenance of functional capacity and independent living status. Observational studies suggested similar limb salvage rates but less short-term mortality and morbidity after endovascular surgical revascularization (400, 401).
Chronic kidney disease in older adults with diabetes
GFR gradually decreases by ∼0.75 to 1 mL/min/1.73 m2 per year (402). The rate of GFR decline is accelerated in the 20% to 40% of older patients with diabetes and diabetic CKD (403). Notably, the decline in GFR reduces the clearance of insulin and many diabetes medications (404) and increases the risk of hypoglycemia (405, 406).
5.14 In patients aged 65 years and older with diabetes who are not on dialysis, we recommend annual screening for CKD with an eGFR and urine albumin-to-creatinine ratio. (1|⊕⊕⊕⊕)
5.15 In patients aged 65 years and older with diabetes who are in group 3 (poor health, see Table 3) of the framework and have a previous albumin-to-creatinine ratio of <30 mg/g, we suggest against additional annual albumin-to-creatinine ratio measurements. (2|⊕⊕OO)
Evidence
The general recommendation for annual measurement of urinary albumin-to-creatinine ratio and eGFR should also be carried out in older adults (300). However, progressive loss of GFR can occur in the absence of albuminuria (407).
In patients with an estimated limited lifespan who have normal urinary albumin excretion, the prognostic value of annual measurement of urinary albumin excretion over and above indicating an increased risk of CVD is likely minimal (408). Regardless, because a decrease in eGFR affects drug dosing and other aspects of care, at least annual testing should be performed, with more frequent testing if the eGFR is <60 mL/min/1.73 m2.
5.16 In patients aged 65 years and older with diabetes and decreased eGFR, we recommend limiting the use or dosage of many classes of diabetes medications to minimize the side effects and complications associated with CKD. (1|⊕⊕OO)
Technical remark: Specific use/dosing guidance on each class of diabetes medication is provided in Table 7.
Evidence
Insulin.
Reduced kidney function results in a prolongation of insulin half-life and a decrease in insulin requirements (409). All insulin preparations can be used in patients with CKD, and no specific reductions in dosing are necessary for patients. Patients with stages 4 to 5 CKD (eGFR <30 mL/min/1.73 m2) often have delayed gastric emptying; administering rapid-acting insulin after the meal may be helpful for matching the insulin peak with the time of the postprandial blood glucose peak. Postprandial rapid-acting insulin with a dose adjustment for the amount eaten may help patients with varying food intakes.
Metformin.
Because of drug accumulation with decreased clearance and therefore a potential risk for lactic acidosis, metformin can be used without dosage reduction down to an eGFR >45 mL/min/1.73 m2 and with a reduction to 1000 mg daily if the eGFR is ≥30 to 44 mL/min/1.73 m2. The drug should be stopped when the eGFR is <30 mL/min/1.73 m2 or in situations associated with hypoxia or an acute decline in kidney function such as sepsis/shock, hypotension, and use of radiographic contrast or other nephrotoxic agents (79, 410, 411) (see Table 7).
SUs and glinides.
SUs and their metabolites are renally cleared, leading to an increased risk of hypoglycemia as GFR declines. Glyburide should be avoided with an eGFR <60 mL/min/1.73 m2 (412). Glimepiride should be used with caution if the eGFR is <60 mL/min/1.73 m2 and should not be used with an eGFR <30 mL/min/1.73 m2. Less than 10% of glipizide is cleared renally, but it should still be used with caution with an eGFR <30 mL/min/1.73 m2 (413, 414).
The active metabolite of nateglinide accumulates in CKD and should not be used with an eGFR <60 mL/min/1.73 m2; however, the active metabolite is cleared by hemodialysis, and thus nateglinide can be used in patients on dialysis (415). Repaglinide appears safe for use in CKD but should be used with caution when the eGFR is <30 mL/min/1.73 m2 (416).
Thiazolidinediones.
Pioglitazone and rosiglitazone are hepatically metabolized and can be used in CKD without dosage adjustment (417, 418). However, fluid retention limits their use in CKD, and they are associated with increased fracture rates and bone loss (139). Thus, use in patients with underlying bone disease (such as renal osteodystrophy or osteoporosis) could potentially be problematic.
α-Glucosidase inhibitors.
Neither acarbose nor miglitol has been studied long-term in patients with a creatinine level >2 mg/dL, and their use should be avoided in these patients (419).
DPP-4 inhibitors.
The DPP-4 inhibitors sitagliptin, saxagliptin, and alogliptin undergo some renal clearance and require dosage adjustment in patients with reduced eGFR (420) (see Table 7). Only a small amount of linagliptin is cleared renally, and no dosage adjustment is indicated with a reduced GFR (420). In general, these drugs are very well tolerated.
SGLT2 inhibitors.
SGLT2 inhibitors generally become less effective as GFR decreases (146). Because of a small increase in adverse events related to intravascular volume contraction, no more than 100 mg once daily of canagliflozin should be used in patients with an eGFR of 45 to <60 mL/min/1.73 m2 (146, 421). Canagliflozin, empagliflozin, and ertugliflozin should be stopped if the eGFR is <45 mL/min/1.73 m2, and dapagliflozin should be stopped at 60 mL/min/1.73 m2, primarily because of a decrease in efficacy (146, 421). Interestingly, empagliflozin and canagliflozin have been shown to delay the progression of CKD (144, 145).
GLP-1 receptor agonists.
The clearance of exenatide decreases as the GFR declines (422). Cases of acute renal failure associated with exenatide use have been reported, and thus exenatide should not be used if the GFR is <30 mL/min/1.73 m2 (423). Lixisenatide should not be used if the GFR is <15 mL/min/1.73 m2, but no dosage changes are needed for liraglutide (424), semaglutide, or dulaglutide as renal function worsens. Nausea is a common side effect of these drugs and could potentially be problematic in older patients with compromised intake, especially those with progressing CKD.
Other oral medications.
Neither bromocriptine (dopamine receptor agonist) nor colesevelam (bile acid sequestrant) has been studied in patients with advanced CKD.
6. Special Settings and Populations
TID
Although it is clear that life expectancy for patients with T1D is improving (425), the number of people reaching 60 years and older is unknown. There appears to be two reasons for the increasing number of older adults with T1D. First, those diagnosed with childhood T1D have taken advantage of the improved therapies for glycemic management and nonglycemic measures for the prevention and treatment of long-term complications. Second, for reasons that are unclear, the number of cases of adult-onset T1D has increased. Given these factors, “geriatric T1D” is anticipated to become more common over the next decade. In one large American T1D registry of 22,697 participants of all ages (T1D Exchange), 3445 individuals (15%) are >50 years of age (426). This phenomenon provides opportunities for the study of a population that numerically was not common in the past.
Hypoglycemia
No RCTs have assessed outcomes for older individuals with T1D. In general, near normal glycemic targets are reserved for individuals with shorter durations of diabetes prior to the development of microvascular or macrovascular complications. Furthermore, the aggressiveness of glucose control needs to be balanced against the risks of hypoglycemia, which is generally a more dangerous side effect of insulin therapy in an older population. In one survey of 510 individuals with T1D >65 years of age, the yearly frequency of severe hypoglycemia (seizure or coma) was 16.1% (427). The same survey found that the duration of diabetes was an even greater risk factor for severe hypoglycemia: for those with at least a 40-year duration of diabetes (N = 758), the yearly rate was 18.6% (427). A subsequent study of 101 subjects with a recent prior history of severe hypoglycemia (mean age and duration of diabetes were 69 and 41 years, respectively) wearing blinded CGM revealed hypoglycemic exposure of an average of 99 min/d <70 mg/dL and 65 min/d <60 mg/dL (88). Certain cognitive test scores were worse in these individuals than in a control group matched for age and duration of T1D.
Cognitive dysfunction
Routine self-care of T1D requires sufficient cognitive capabilities due to the complexity of disease management. One report noted that in a group of patients with T1D (mean age and duration of diabetes 60 and 38 years, respectively) over a 4-year period, the decline in cognitive function was no different from that in an aged-matched control group (428). However, patients with a history of severe hypoglycemia or CVD were more susceptible to cognitive decline than were the control patients. Cognitive decline in older adults with T1D often requires simplification of insulin regimens (e.g., moving from carbohydrate and calorie counting to set meal-time dosing or moving from insulin pump to injections).
Functionality
The typical reduced physical function of older adults may be exacerbated by T1D. Neuropathy, visual impairment, and hypoglycemia unawareness may make driving an impossible task. In addition to these complications, arthritis, chronic pain, and other conditions are frequently observed in this population (diabetic cheiroarthropathy), presenting barriers to independent living. As functionality becomes more limited, the role of the caregiver becomes more critical. Due to to all of these concerns, less stringent glycemic targets are appropriate for older adults with T1D, particularly those with a >40-year duration of diabetes, when severe hypoglycemia becomes more common.
Hypertension and hypercholesterolemia
Even fewer data are available to guide clinicians for these common clinical problems. The presence of diabetic kidney disease generally results in lower BP targets, although the specific goals are controversial (429). BP targets with or without kidney disease have not been studied in older adults with T1D. Likewise, RCTs for the treatment of hypercholesterolemia have not been studied in patients with T1D, let alone in older patients with T1D. However, both proteinuria and obesity are accepted risk factors for CVD, and of the patients >50 years old in the T1D Exchange of 2014, 39% and 29% were overweight and obese, respectively (data for those >60 years old were not reported) (430). Because the duration of diabetes seems to be a risk factor for CVD, which is also the leading cause of mortality (431), it seems appropriate that most older adults with T1D should be treated similarly to those with T2D. Nevertheless, clinicians should evaluate each patient individually, especially those who are nonobese and diagnosed later in life where less aggressive treatment may be warranted.
Management of diabetes away from home—in hospitals and long-term care facilities—and transitions of care
More than 25% of people >65 years old have diabetes (120), and the prevalence of diabetes in the long-term care facility (LTCF) population has increased to 35% (432–434). Moreover, older patients with diabetes display various comorbid illnesses and functional impairments (435). Older patients with diabetes mellitus are frequently admitted to the hospital for non-diabetes–related problems such as cardiovascular and respiratory disorders and digestive, genitourinary, and infectious problems (436, 437).
Patients with diabetes may be admitted to general medical-surgical floors, straight to the intensive care unit, or to the operating room (438). Patients who are not eating or on steroids, pressors, tube feeding, total parenteral nutrition, special diets, hemotoneal or peritoneal dialysis, and/or other agents that modify glucose homeostasis and metabolic profiles. Frequently, hospitalized patients go from one condition or treatment to another in a very short time. Various specialists and teams may be involved in the treatment process, complicating communication and ordering processes. Thus, education of nursing and house staff as well as the contribution of so-called “Glucose Management Teams” cannot be overestimated (439). The benefits of glycemic control must be balanced with the adverse effects of glucose-lowering medications and a patient’s age, overall health status, and functional and intellectual capacity (40, 79).
6.1 In patients aged 65 years and over with diabetes in hospitals or nursing homes, we recommend establishing clear targets for glycemia at 100 to 140 mg/dL (5.55–7.77 mmol/L) fasting and 140 to 180 mg/dL (7.77–10 mmol/L) postprandial while avoiding hypoglycemia. (1|⊕⊕OO)
Technical remark: An explicit discharge plan should be developed to re-establish long-term glycemic treatment targets and glucose-lowering medications as the patient transitions to posthospital care.
Evidence
Glycemic targets for inpatient management of diabetes in older adults are established based on general guidelines while avoiding hypoglycemia (437). Best practice requires concrete strategies for transitions of care within the hospital and upon discharge (440–442).
The most common cause of glycemic variability in hospitalized patients with diabetes is a mismatch between caloric intake and insulin coverage. Alimentary intake is frequently a problem for hospitalized patients (443) and LTCF residents because of impaired appetite or inability to swallow or hold food down. Instead of a balanced meal, they might consume only fluids, frequently fruit juices, shakes, or dietary supplements that contain high concentrations of sugar and produce glycemic spikes. Using sliding scale regular insulin may lead to hypoglycemia and wide oscillations in blood glucose levels (444, 445). Nonetheless, holding insulin due to patients’ complaints of poor appetite results in hyperglycemia and may precipitate diabetic ketoacidosis.
Patients on enteral or parenteral nutrition and insulin develop hypoglycemia when feeding is stopped abruptly for various reasons (438). Thus, safety measures must be in place at every institution. Continuous enteral or parenteral nutrition produces a constant “postprandial” state with glycemic targets between 140 and 180 mg/dL (7.77 to 10 mmol/L). Aiming at glycemia targets below this range is dangerous.
Point-of-care glucose monitoring is helpful only when it is performed frequently and when a knowledgeable person reviews the data and makes appropriate adjustments (439, 446–448). Most hospitalized patients with diabetes are treated with insulin (449). Most missteps in diabetes management occur not at the selection of the initial doses of insulin but because of poor follow-up and lack of appropriate and timely adjustments.
Whereas glycemia of critically ill patients is usually managed in the intensive care unit with IV insulin administration, most noncritically ill patients are treated with basal-bolus regimens. In a randomized multicenter trial comparing the efficacy of a basal-bolus insulin regimen with glargine once daily and glulisine before meals (n = 104) to sliding scale regular insulin four times daily (n = 107) in patients with T2D undergoing general surgery, Umpierrez et al. (450) demonstrated that basal-bolus insulin not only improved glycemic control but also significantly reduced hospital complications.
Moderate (41 to 70 mg/dL) and severe (<40 mg/dL) hypoglycemia is common in hospitalized patients with diabetes, including older patients (432, 451–455). Hypoglycemia increases length of hospital stay and mortality (456–459). The presence of renal failure, poor nutrition, and sepsis is highly predictive of a high risk of hypoglycemia in older individuals. Although a causal relationship between hypoglycemia and mortality has not been established, a strong association between hypoglycemia and more severe illness is likely (455, 460, 461).
An RCT comparing treatment with oral agents and basal insulin in older patients with T2D in LTCFs demonstrated that treatment within both arms resulted in a similar frequency of hypoglycemia (462), suggesting that a low daily dose of basal insulin is sufficient to achieve reasonable and safe glycemia in older patients. Clearly, patients with T1D in institutional settings should never be left without insulin.
6.2 In patients aged 65 years and older with diabetes and a terminal illness or severe comorbidities, we recommend simplifying diabetes management strategies. (1|⊕OOO)
Evidence
Patients with late-stage cancer, organ failure, or pre–solid organ or post–solid organ or bone marrow transplant, patients on dialysis, and those in the intensive care unit present unique challenges. Higher glycemic targets may be acceptable in patients with severe comorbidities and in terminally ill individuals. A simplified management approach is fully justified in these patients.
6.3 In patients aged 65 years and older without diagnosed diabetes, we suggest routine screening for HbA1c during admission to the hospital to ensure detection and treatment where needed (see the technical remark in recommendation 2.1). (2|⊕⊕OO)
Evidence
Although measurements of HbA1c have earned their recognition in the diagnosis of diabetes mellitus (463) and in the process of monitoring glycemic control in patients with diabetes (464), they can also help to assess the chronicity of hyperglycemia in patients admitted to the hospital who do not have a previous diagnosis of diabetes (465).
Admission HbA1c levels have been shown to correlate with greater morbidity and mortality in patients with acute myocardial infarction (466, 467), heart failure (468), and poor functional outcome after acute ischemic stroke (465). The exact mechanism of these associations is not well understood, but one may surmise that chronic hyperglycemia has an adverse influence on the cardiovascular system in patients with undiagnosed diabetes or prediabetes.
Transitions of care
Transition of care from hospital to home or to an LTCF rightfully represents a critical element in the treatment of older patients with diabetes. The most important aspect of successful transition is effective, detailed, and thorough bidirectional communication between the discharging and receiving teams of health care providers. Excellent communication between the discharging team and patient as well as the patient’s family or caregiver is also of paramount importance. Older patients newly diagnosed with diabetes during their hospital stay may present additional obstacles during transitions of care. These patients deal with the shock of a new chronic disease and may not have a clear ability to understand and integrate complicated medical regimens, changes in lifestyle, home glucose monitoring, and other challenges of diabetes. Finally, the number of comorbidities as well as patients’ cognitive and functional status will dictate the appropriate steps in the transition of care offered to older patients with diabetes.
Methodology
Participants
The Writing Committee consisted of 10 content experts representing the following specialties: endocrinology, neurology, and geriatrics. Two of the committee members brought an international perspective to this guideline topic. The Writing Committee also included a clinical practice guideline methodologist who led the team of comparative effectiveness researchers that conducted the systematic reviews and meta-analyses.
Guideline development process
The Endocrine Society’s guideline development process combines elements of the GRADE framework (469) with an approach that was thought to be more appropriate for the rare endocrine disease space where scientific evidence is limited or nonexistent. The Society applies the steps in the GRADE framework to research questions for which there is an ample body of knowledge of low-to-moderate quality or higher (Table 8 for descriptions of low- and moderate-quality evidence). In these situations, GRADE provides the methodological and statistical rigor that results in robust recommendations that are classified using quality of evidence and strength of recommendation as described in by Guyatt et al. (470) and represented graphically in Table 8.
Table 8.
GRADE Classification of Guideline Recommendations
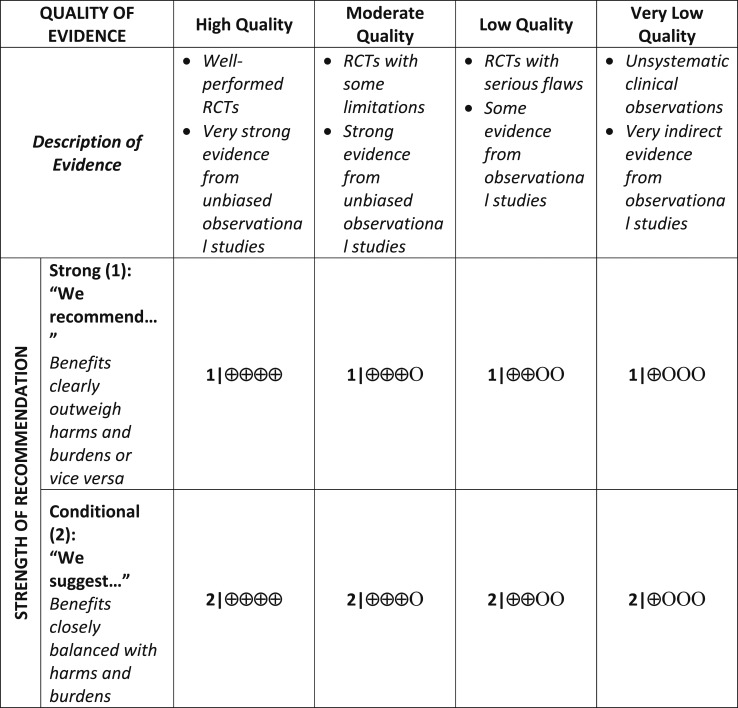
|
Where evidence is extremely limited and/or not systematically analyzed, we provide recommendations based on an expert review of the limited data. This process is less systematic than the GRADE methodological framework; however, these recommendations are also clearly classified using the GRADE classification system.
Some of the Society’s clinical practice guidelines also include Ungraded Good Practice Statements (471). This unclassified clinical guidance can include expert opinion statements on good practice, references to recommendations made in other guidelines, and observations on preventive care and shared decision-making.
Guideline recommendations include the relevant population, intervention, comparator, and outcome. When further clarification on implementation is needed, we include technical remarks. These provide supplemental information such as timing, setting, dosing regimens, and necessary expertise. All recommendations are followed by a synopsis of the evidence on which they are based. Authors may also include short statements on patients’ values and preferences, the balance of benefits and harms, and minority opinions, where relevant.
Note that the Society’s guideline development process is currently under review, and new approaches and processes are likely to be instituted in the coming months.
Conflicts of interest
To be considered for membership of a Writing Committee, nominees are required to disclose all relationships with industry for the 12-month period prior to guideline writing committee initiation. This is consistent with the reporting time frame for the National Institutes of Health and the FDA.
Conflicting relationships that should be declared include commercial, noncommercial, intellectual, institutional, and patient/public activities pertinent to the scope of the guideline.
The Chair of the Clinical Guidelines Subcommittee reviews these disclosed relationships and determines whether they are relevant to the topic of the guideline and present a relevant conflict of interest (COI).
The Chair of the Clinical Guidelines Subcommittee selects Co-Chairs and members based on the COI information received and the individuals’ expertise and other skills. The Endocrine Society Council then reviews and endorses the nominees or makes appropriate changes.
The chair of the Writing Committee must be free of any COI or other biases that could undermine the integrity or credibility of the work.
At least half (≥ 50%) of the Writing Committee members must be free of relevant COI.
Following initiation of the committee, members are asked to disclose any new relationships with industry at every in-person meeting and on most conference calls.
The authors who comprise the 50% or more without COIs must refrain from adding new relevant industry relationships throughout the guideline development process to ensure that the appropriate COI balance is preserved.
The authors who comprise the ≤50% with relevant COIs are required to declare the situation and recuse themselves from any relevant discussions, votes, and from drafting recommendations.
If a member is aware of another person who might have a conflict and has not declared it for some reason, they are obliged to bring this to the Chair’s attention.
Staff, Writing Committee Chairs, and members must be alert for situations that might present a potential or perceived conflict of interest.
Acknowledgments
The guideline writing committee thanks the participating organizations and individuals with diabetes for their invaluable contribution to the patient voice in this guideline. We particularly thank the Reverend Albert Whitaker from the ADA’s Senior Signature program, Ronald H. Lammy from the Total Wellness for Elders Program at the Elder HealthCare Disparities Coalition (Roxbury, MA), and Sarah Mart from Diabetes Sisters. The writing committee thanks the cosponsors of this guideline for their contribution to the development effort. The Endocrine Society acknowledges that the American Geriatrics Society (AGS) affirms the value of this document. (Affirmation of value means that AGS supports the general principles in this document and believes it is of general benefit to its membership.)
Financial Support: This guideline was supported by the Endocrine Society. No other entity provided financial support.
Disclosure Summary:
See Appendix C.
Disclaimer: The Endocrine Society’s clinical practice guidelines are developed to be of assistance to endocrinologists by providing guidance and recommendations for particular areas of practice. The guidelines should not be considered inclusive of all proper approaches or methods, or exclusive of others. The guidelines cannot guarantee any specific outcome, nor do they establish a standard of care. The guidelines are not intended to dictate the treatment of a particular patient. Treatment decisions must be made based on the independent judgement of healthcare providers and each patient’s individual circumstances. The Endocrine Society makes no warranty, express or implied, regarding the guidelines and specifically excludes any warranties of merchantability and fitness for a particular use or purpose. The Society shall not be liable for direct, indirect, special, incidental, or consequential damages related to the use of the information contained herein.
Glossary
Abbreviations:
- ACE
angiotensin-converting enzyme
- ACCORD
Action to Control Cardiovascular Risk in Diabetes
- ADA
American Diabetes Association
- ADL
activity of daily living
- ARB
angiotensin receptor blocker
- BP
blood pressure
- CGM
continuous glucose monitoring
- CHF
congestive heart failure
- CKD
chronic kidney disease
- CVD
cardiovascular disease
- DPP-4
dipeptidyl peptidase-4
- eGFR
estimated glomerular filtration rate
- FDA
Food and Drug Administration
- GLP-1
glucagon-like-peptide 1
- GFR
glomerular filtration rate
- HR
hazard ratio
- IADL
instrumental ADL
- LDL-C
low-density lipoprotein cholesterol
- LTCF
long-term care facility
- MACE
major adverse cardiovascular event
- MCI
mild cognitive impairment
- PCSK9
proprotein convertase subtilisin/kexin type 9
- RCT
randomized control trial
- RR
relative risk
- SGLT2
sodium-glucose cotransporter 2
- SBP
systolic blood pressure
- SDM
shared decision-making
- SPRINT
Systolic Blood Pressure Intervention Trial
- SU
sulfonylurea
- T1D
type 1 diabetes
- T2D
type 2 diabetes
- UKPDS
UK Prospective Diabetes Study
- VEGF
vascular endothelial growth factor
Appendixes
Appendix A. How to Use the Conceptual Framework
The guideline Writing Committee designed the framework (Table 3) to serve as a guide that encourages the diabetes clinician to consider available evidence and a patient’s overall health, likelihood to benefit from interventions, and personal values when considering treatment goals such as glucose, BP, and dyslipidemia. Consideration that the patient categories are general concepts and that individual patients may not fall clearly in one category is important. However, considering most patients in group 2 as prefrail and most in group 3 as frail with one or more disabilities may be helpful. Nevertheless, we recognize that neither the category nor patient values are necessarily static and may change over time with disease progression or may shift in either direction, for example, because of temporary disability.
Glucose targets
The framework prioritizes blood glucose targets over HbA1c, recognizing that both are important in clinical practice. However, owing to accuracy concerns of HbA1c as well as the failure of HbA1c to identify those at risk for hypoglycemia (see evidence statement in section 3 on “Assessment of Older Patients with Diabetes”), the framework intentionally places glucose values above HbA1c in the glucose target section.
Shared decision-making
Shared decision-making (SDM) is a collaborative, patient-directed decision-making process that helps the patient set goals and priorities with input from their health care team, family, and other caregivers. The objective is for the patient to make choices that meet his/her needs while honoring personal values and preferences. In the conceptual framework, the SDM arrow indicates that after consideration of these factors, some patients may have lower or higher targets.
SDM example
Mrs. Jones is a 72-year-old woman with T1D and rheumatoid arthritis who presents for the first time for ongoing management of her diabetes, which she has had for 40 years. She has retinopathy without impaired vision, peripheral polyneuropathy that has just become painful this past year, and stage 3 CKD with a GFR of 42. She has hypertension on two agents with SBP between 132 and 140 on recent checks. Owing to her rheumatoid arthritis, she uses a walker in the home and a wheelchair or scooter outdoors but is able to manage insulin and glucose monitoring independently, although some days her dexterity is so poor that she manages to only check twice. Her son pays her bills for her because she can no longer manage her online accounts due to MCI; otherwise, she is very involved in the local church and has evening activities three times a week.
Her HbA1c has been between 6.2 and 6.9 for the last 10 years, as you can see in the records, and she reports being pleased with her control. She uses long-acting basal insulin and rapid-acting insulin up to five times daily according to a carbohydrate ratio and correction factor, which, with further inquiry, you find that she applies very accurately; she declined an insulin pump and CGM in the past. From her glucose meter, her lowest glucose is 62 mg/dL, as measured in the fasting state, and she reports losing hypoglycemia awareness in the last 2 to 3 years; otherwise, her fasting mean glucose is 128 mg/dL.
You begin to discuss glucose goals, and she reports “Please don’t tell me my HbA1c should be higher; that is what my previous doctor said.” She reports feeling “fuzzy” and “clumsy” when her glucose is >200 mg/dL and attempts to loosen control have been difficult for her. You discuss the concerns around hypoglycemia, and she agrees that it is concerning. Together, you agree for her to wear a continuous glucose monitor for up to 10 days to evaluate her glucose patterns, and you place this device in the office. You agree on a glucose range of fasting, 100 to 150 mg/dL, and bedtime, 150 to 180 mg/dL (group 2 in framework), and she agrees to adjust as needed for safety while avoiding glucose levels >200 mg/dL as much as possible. You both agree to focus on the glucose ranges rather than HbA1c. You suggest that her son come with her to the next visit to discuss options for safe glucose monitoring going forward, as her rheumatoid arthritis is affecting her ability to self-monitor blood glucose.
Appendix B. Patient Voice Assessment
To include the patient’s perspective in this guideline and to place the recommendations into the context of patient experience, we sought the collaboration of both organized groups and individuals with diabetes who were age 65 years or older. An anonymous, unvalidated survey was developed by members of the writing committee and administered electronically (via E-mail) and in person to 80 adults. The survey was designed to address specific aspects of the guideline, namely, the perception of how diabetes and treatment of diabetes impact overall health. As a group, the respondents represented the target population of the guideline, with most having T2D and reporting complex disease management (55% reported daily insulin use) and a significant prevalence of complications (41% with disease-specific microvascular complications and 51% with macrovascular complications). Based on the preponderance of responses, the committee identified four common themes: (i) many older adults do not anticipate changing their various treatment targets with advancing age; (ii) diabetes is often not listed as the top health condition by older patients with diabetes, as other conditions are often considered more serious or important to them; (iii) most older patients with diabetes express significant fear of complications (microvascular and macrovascular) and primarily consider glucose control to be the most important factor for prevention; and (iv) lipid-lowering medications may be underused among older adults, which may be due to a lack of perceived benefit by themselves or their clinicians.
Methods
To include the patient’s perspective in this guideline, we sought the collaboration of both organized groups and individual patients with diabetes who were age 65 years or older. The Writing Committee developed a 20-question anonymous survey that included demographics, diabetes-specific characteristics, and perspectives on the health problems addressed in the guideline. The survey was tested internally but was not formally validated. The participating organizations included the ADA’s Senior Signature program (www.diabetes.org/in-my-community/awareness-programs/older-adults/) and the Diabetes Sisters (diabetessisters.org/). Individual patients were identified through a clinical database and were asked to submit the survey online. The survey was also administered in person to a focus group of older adults participating in a community program. All data collected directly from individuals did not include personal health information or identifiers.
Results
Overall, 80 respondents completed the survey, and 77 of them reported having diabetes (three reported taking the survey on behalf of a family member). Most respondents were women (88%) between the ages of 60 and 80 years (93%), and 7% were between 81 and 100 years old. Most were white (68%) and black and/or African American (26%), with 2.5% and 1% Native American and other, respectively. Self-reported diabetes type indicated that more than half of the respondents had T2D, as expected, and 31% reported having T1D (see Appendix Table 1).
Diabetes self-management
Fifty-five percent of 75 respondents reported using insulin daily to manage diabetes, and ∼40% reported taking more than one medication to treat diabetes, with 15% reporting taking three or more. Most respondents disagreed that forgetting medications was a concern, although 29% did report this as a concern.
Glucose targets and hypoglycemia
Patients generally reported agreement between themselves and their care providers on what their glucose target should be, with only 4% reporting disagreement. One-third of respondents either agreed or strongly agreed that they fear having low blood glucose on most days. Interestingly, when asked if they would agree to relax or loosen glucose targets with age, most (62%) reported that they would not.
Blood pressure and lipid control
Nearly all agreed (96%) that controlling BP will reduce their risk of stroke, and 100% of 78 respondents agreed that having a BP in the “target range” is important for overall health. Of these participants, 36% reported taking no medications for BP, 28% reported taking one medication, and 36% reported taking more than one medication. In contrast, a smaller majority agreed that maintaining lipids in the target range is important (87%) and that taking a lipid-lowering medication will reduce the risk of heart attack (67%). Although the majority reported taking one medication for lipid lowering (68%), a large minority reported taking none (24%).
Complications
Most respondents (85%) reported that they worry about the future with respect to the possibility of serious complications of diabetes. Forty-one percent reported having a diabetes-specific complication, with most (72%) reporting nerve-related discomfort or pain (neuropathy). Just more than half reported having macrovascular disease: peripheral vascular disease (24%) and heart disease (27%). Nearly all respondents (96%) agreed that blood glucose control reduces the risk of vision loss. Most, although a lower percentage (85%), also agreed that blood glucose control is the “most important factor” that will reduce heart disease risk.
Overall health
When asked how many other health problems they had, approximately half of the respondents reported having two or three, 13% reported four or five, and 10% reported having six or more other health problems. When asked whether they think that diabetes takes up too much mental and physical energy on a daily basis, the responses were broadly distributed: 58% agreed, 20% were undecided, and 20% disagreed. When asked to rank all of their health conditions in order of importance, 40% of the 69 respondents ranked diabetes first. Other conditions common among older adults that are potentially related to diabetes were also ranked high (hypertension, heart disease, bladder control, depression, and overweight).
There are several limitations to employing a limited survey approach to illustrate the patient experience. First, the population was largely ambulatory and did not represent nonambulatory older adults or those living in LTCFs. Additionally, this limited survey mostly included black and white individuals living in urban or suburban areas, with no Latino/Hispanic and minimal Asian representation, and may not be generalizable to many areas of the global community.
In summary, there appeared to be significant heterogeneity in perceived health and cognitive function (measured by a question related to forgetting medications), supporting the guideline’s emphasis on tailoring treatment to the patient’s level of overall health and functional status. Diabetes did not predominate the participants’ perception of their overall health, possibly reflecting the accumulation of other conditions that impact health and quality of life with age. This finding may also suggest that some older adults may not be willing or able to invest the time and expense required to fulfill recommendations made in the guideline. Responses to the survey also highlight the potentially inconsistent messages heard by older patients regarding tailoring clinical targets (BP and glucose) and prevention of complications. Perhaps consistent with these results, most participants reported not being willing to relax glucose goals over time as they become older. Taken as a whole, the results highlight the importance of clear communication between clinicians and patients on the actual risks and benefits of different therapeutic strategies.
Appendix Table 1.
General Characteristics of the Survey Population
| Characteristic | Value | (%) |
|---|---|---|
| Age, y (N = 80) | 60–70 | 64 |
| 71–80 | 29 | |
| 81–90 | 3.75 | |
| 91–100 | 3.75 | |
| >100 | 0 | |
| Sex | Male | 12 |
| Female | 88 | |
| Race | Black and African American | 26 |
| White | 68 | |
| Asian | 1 | |
| Native American | 2.5 | |
| Mixed race | 0 | |
| Latino or Hispanic | 0 | |
| Other | 2.5 | |
| Self-reported diabetes type | T1D | 31 |
| T2D | 52 | |
| Familial or “MODY” | 0 | |
| Due to pancreatic disease or removal | 1.25 | |
| Other type | 9 | |
| I do not know | 6 |
Abbreviations: MODY, Maturity Onset Diabetes of Youth.
Appendix C.
Conflicts of Interest
| Writing Committee Member | Employment | Uncompensated Memberships | Uncompensated Leadership | Personal Financial | Organizational Financial | Spousal/ Family Info. |
|---|---|---|---|---|---|---|
| Derek LeRoith, Chair | Professor of Medicine, Endocrinology, Diabetes, and Bone Disease, Mount Sinai Medical Center | None | None | • Astrazeneca, consultant, Advisory Board • Merck Sharp & Dohme, faculty • MannKind, consultant | None | None |
| Geert-Jan Biessels | Professor of Neurology, University Medical Center Utrecht | None | None | None | • Boehringer Ingelheim, consultant and investigator | None |
| Susan Braithwaite | Emeritus Professor, Presence Saint Francis Hospital and Presence Saint Joseph Hospital | None | None | • ADA, book reviews • American Association of Clinical Endocrinologists and American College of Endocrinology, Associate Editor | None | None |
| Felipe Casanueva | Professor of Medicine, Santiago de Compostela University | None | • Pituitary Society, Board of Directors | • Pfizer, Advisory Board • Novo Nordisk, Advisory Board • Janssen Global Services, Advisory Board • Orexigen, speaker • Pronokal, speaker | None | None |
| Boris Draznin | Director, Adult Diabetes Program, School of Medicine, University of Colorado Denver | None | None | None | None | None |
| Jeffrey Halter | Professor of Internal Medicine and Director, Geriatrics Center, University of Michigan | None | None | None | None | None |
| Irl Hirsch | Professor of Medicine, University of Washington Medical Center–Roosevelt | None | None | • Abbott Laboratories, consultant • Roche Diabetes Care, consultant • BigFoot, consultant • Adocia, consultant | • Medtronic Diabetes, investigator | None |
| Marie McDonnell | Director, Brigham and Women's Diabetes Program, Brigham and Women’s Hospital and Harvard Medical School | None | None | • American Association of Clinical Endocrinologists, Associate Editor | None | None |
| Mark Molitch | Professor of Endocrinology, Northwestern University Feinberg Medical School | None | None | • Merck, member DSMB, consultant • Pfizer, member DSMB • Janssen Global Services, consultant • Chiasma, consultant • Novartis, consultant | • Bayer, investigator • Novo Nordisk, investigator • Calibra, investigator • Chiasma, investigator • Novartis, investigator | • Amgen, wife and daughter, stock ownership |
| M. Hassan Murad | Professor of Medicine, Mayo Clinic | None | None | None | None | None |
| Alan Sinclair | Director, Foundation for Diabetes Research in Older People, King’s College, United Kingdom | None | None | • Eli Lilly, Speaker • Merck Sharp & Dohme, Advisory Board | • Merck Sharp & Dohme/Merck, sponsorship | None |
Footnotes
Cosponsoring Associations: European Society of Endocrinology, The Gerontological Society of America, and The Obesity Society.
References
- 1. Laiteerapong N, Karter AJ, Liu JY, Moffet HH, Sudore R, Schillinger D, John PM, Huang ES. Correlates of quality of life in older adults with diabetes: the diabetes & aging study. Diabetes Care. 2011;34(8):1749–1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Menke A, Casagrande S, Geiss L, Cowie CC. Prevalence of and trends in diabetes among adults in the United States, 1988-2012. JAMA. 2015;314(10):1021–1029. [DOI] [PubMed] [Google Scholar]
- 3. Laiteerapong N, Huang ES. Diabetes in older adults. In: Cowie CC, Casagrande SS, Menke A, Cissell MA, Eberhardt MS, Meigs JB, Gregg EW, Knowler WC, Barrett-Connor E, Becker DJ, Brancati FL, Boyko EJ, Herman WH, Howard BV, Narayan KMV, Rewers M, Fradkin JE, eds. Diabetes in America. 3rd ed. Bethesda, MD: National Institutes of Health; 2018:16-1–16-26. [Google Scholar]
- 4. Narayan KM, Boyle JP, Geiss LS, Saaddine JB, Thompson TJ. Impact of recent increase in incidence on future diabetes burden: U.S., 2005–2050. Diabetes Care. 2006;29(9):2114–2116. [DOI] [PubMed] [Google Scholar]
- 5. Kirkman MS, Briscoe VJ, Clark N, Florez H, Haas LB, Halter JB, Huang ES, Korytkowski MT, Munshi MN, Odegard PS, Pratley RE, Swift CS; Consensus Development Conference on Diabetes and Older Adults . Diabetes in older adults: a consensus report. J Am Geriatr Soc. 2012;60(12):2342–2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Diabetes Surveillance System. Available at: www.cdc.gov/diabetes. Accessed 17 October 2017.
- 7. Halter JB, Musi N, McFarland Horne F, Crandall JP, Goldberg A, Harkless L, Hazzard WR, Huang ES, Kirkman MS, Plutzky J, Schmader KE, Zieman S, High KP. Diabetes and cardiovascular disease in older adults: current status and future directions. Diabetes. 2014;63(8):2578–2589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lee PG, Halter JB. The pathophysiology of hyperglycemia in older adults: clinical considerations. Diabetes Care. 2017;40(4):444–452. [DOI] [PubMed] [Google Scholar]
- 9. Chang AM, Halter JB. Aging and insulin secretion. Am J Physiol Endocrinol Metab. 2003;284(1):E7–E12. [DOI] [PubMed] [Google Scholar]
- 10. Halter JB. Aging and insulin secretion. In: Masoro EJ, Austad SN, eds. Handbook of the Biology of Aging. 7th ed. Waltham, MA: Elsevier; 2011:373–384. [Google Scholar]
- 11. Rankin MM, Kushner JA. Adaptive β-cell proliferation is severely restricted with advanced age. Diabetes. 2009;58(6):1365–1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Teta M, Long SY, Wartschow LM, Rankin MM, Kushner JA. Very slow turnover of β-cells in aged adult mice. Diabetes. 2005;54(9):2557–2567. [DOI] [PubMed] [Google Scholar]
- 13. Krishnamurthy J, Ramsey MR, Ligon KL, Torrice C, Koh A, Bonner-Weir S, Sharpless NE. p16INK4a induces an age-dependent decline in islet regenerative potential. Nature. 2006;443(7110):453–457. [DOI] [PubMed] [Google Scholar]
- 14. Tschen SI, Dhawan S, Gurlo T, Bhushan A. Age-dependent decline in β-cell proliferation restricts the capacity of β-cell regeneration in mice. Diabetes. 2009;58(6):1312–1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Basu R, Breda E, Oberg AL, Powell CC, Dalla Man C, Basu A, Vittone JL, Klee GG, Arora P, Jensen MD, Toffolo G, Cobelli C, Rizza RA. Mechanisms of the age-associated deterioration in glucose tolerance: contribution of alterations in insulin secretion, action, and clearance. Diabetes. 2003;52(7):1738–1748. [DOI] [PubMed] [Google Scholar]
- 16. Szoke E, Shrayyef MZ, Messing S, Woerle HJ, van Haeften TW, Meyer C, Mitrakou A, Pimenta W, Gerich JE. Effect of aging on glucose homeostasis: accelerated deterioration of β-cell function in individuals with impaired glucose tolerance. Diabetes Care. 2008;31(3):539–543. [DOI] [PubMed] [Google Scholar]
- 17. Utzschneider KM, Carr DB, Hull RL, Kodama K, Shofer JB, Retzlaff BM, Knopp RH, Kahn SE. Impact of intra-abdominal fat and age on insulin sensitivity and β-cell function. Diabetes. 2004;53(11):2867–2872. [DOI] [PubMed] [Google Scholar]
- 18. Chang AM, Smith MJ, Galecki AT, Bloem CJ, Halter JB. Impaired β-cell function in human aging: response to nicotinic acid-induced insulin resistance. J Clin Endocrinol Metab. 2006;91(9):3303–3309. [DOI] [PubMed] [Google Scholar]
- 19. Maedler K, Schumann DM, Schulthess F, Oberholzer J, Bosco D, Berney T, Donath MY. Aging correlates with decreased β-cell proliferative capacity and enhanced sensitivity to apoptosis: a potential role for Fas and pancreatic duodenal homeobox-1. Diabetes. 2006;55(9):2455–2462. [DOI] [PubMed] [Google Scholar]
- 20. DeFronzo RA. Insulin resistance, lipotoxicity, type 2 diabetes and atherosclerosis: the missing links. The Claude Bernard Lecture 2009. Diabetologia. 2010;53(7):1270–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Selvin E, Coresh J, Brancati FL. The burden and treatment of diabetes in elderly individuals in the U.S. Diabetes Care. 2006;29(11):2415–2419. [DOI] [PubMed] [Google Scholar]
- 22. Sudore RL, Karter AJ, Huang ES, Moffet HH, Laiteerapong N, Schenker Y, Adams A, Whitmer RA, Liu JY, Miao Y, John PM, Schillinger D. Symptom burden of adults with type 2 diabetes across the disease course: Diabetes & Aging Study. J Gen Intern Med. 2012;27(12):1674–1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Stellefson M, Dipnarine K, Stopka C. The chronic care model and diabetes management in US primary care settings: a systematic review. Prev Chronic Dis. 2013;10:120180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. American Diabetes Association. 2 Classification and diagnosis of diabetes: standards of medical care in diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S13–S28. [DOI] [PubMed] [Google Scholar]
- 25. Herman WH, Ye W, Griffin SJ, Simmons RK, Davies MJ, Khunti K, Rutten GE, Sandbaek A, Lauritzen T, Borch-Johnsen K, Brown MB, Wareham NJ. Early detection and treatment of type 2 diabetes reduce cardiovascular morbidity and mortality: a simulation of the results of the Anglo-Danish-Dutch study of intensive treatment in people with screen-detected diabetes in primary care (ADDITION-Europe). Diabetes Care. 2015;38(8):1449–1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jehan S, Myers AK, Zizi F, Pandi-Perumal SR, Jean-Louis G, McFarlane SI. Obesity, obstructive sleep apnea and type 2 diabetes mellitus: Epidemiology and pathophysiologic insights. Sleep Med Disord. 2018;2(3):52–58. [PMC free article] [PubMed] [Google Scholar]
- 27. Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM; Diabetes Prevention Program Research Group . Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Knowler WC, Fowler SE, Hamman RF, Christophi CA, Hoffman HJ, Brenneman AT, Brown-Friday JO, Goldberg R, Venditti E, Nathan DM; Diabetes Prevention Program Research Group . 10-Year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374(9702):1677–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Diabetes Prevention Program Research Group Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: the Diabetes Prevention Program Outcomes Study. Lancet Diabetes Endocrinol. 2015;3(11):866–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lindström J, Ilanne-Parikka P, Peltonen M, Aunola S, Eriksson JG, Hemiö K, Hämäläinen H, Härkönen P, Keinänen-Kiukaanniemi S, Laakso M, Louheranta A, Mannelin M, Paturi M, Sundvall J, Valle TT, Uusitupa M, Tuomilehto J; Finnish Diabetes Prevention Study Group . Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet. 2006;368(9548):1673–1679. [DOI] [PubMed] [Google Scholar]
- 31. Balk EM, Earley A, Raman G, Avendano EA, Pittas AG, Remington PL. Combined diet and physical activity promotion programs to prevent type 2 diabetes among persons at increased risk: a systematic review for the community preventive services task force. Ann Intern Med. 2015;163(6):437–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Haw JS, Galaviz KI, Straus AN, Kowalski AJ, Magee MJ, Weber MB, Wei J, Narayan KMV, Ali MK. Long-term sustainability of diabetes prevention approaches: a systematic review and meta-analysis of randomized clinical trials. JAMA Intern Med. 2017;177(12):1808–1817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Medicare Interactive Annual wellness visit. Available at: www.medicareinteractive.org/get-answers/medicare-covered-services/preventive-services/annual-wellness-visit. Accessed 16 October 2017.
- 34. Applegate WB, Blass JP, Williams TF. Instruments for the functional assessment of older patients. N Engl J Med. 1990;322(17):1207–1214. [DOI] [PubMed] [Google Scholar]
- 35. Blaum C, Cigolle CT, Boyd C, Wolff JL, Tian Z, Langa KM, Weir DR. Clinical complexity in middle-aged and older adults with diabetes: the Health and Retirement Study. Med Care. 2010;48(4):327–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Inzucchi SE, Matthews DR; Management of Hyperglycemia in Type 2 Diabetes American Diabetes Association and European Association for the Study of Diabetes Position Statement Writing Group. Response to comments on Inzucchi et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach. Update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2015;38:140–149 response. Diabetes Care. 2015;38:E128–E129. [DOI] [PubMed] [Google Scholar]
- 37. Garber AJ, Abrahamson MJ, Barzilay JI, Blonde L, Bloomgarden ZT, Bush MA, Dagogo-Jack S, DeFronzo RA, Einhorn D, Fonseca VA, Garber JR, Garvey WT, Grunberger G, Handelsman Y, Henry RR, Hirsch IB, Jellinger PS, McGill JB, Mechanick JI, Rosenblit PD, Umpierrez GE, American Association of Clinical Endocrinologists, American College of Endocrinology. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm—2016 executive summary. Endocr Pract. 2016;22(1):84–113. [DOI] [PubMed] [Google Scholar]
- 38. Davies MJ, D’Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, Rossing P, Tsapas A, Wexler DJ, Buse JB. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41(12):2669–2701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Cigolle CT, Kabeto MU, Lee PG, Blaum CS. Clinical complexity and mortality in middle-aged and older adults with diabetes. J Gerontol A Biol Sci Med Sci. 2012;67(12):1313–1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kirkman MS, Briscoe VJ, Clark N, Florez H, Haas LB, Halter JB, Huang ES, Korytkowski MT, Munshi MN, Odegard PS, Pratley RE, Swift CS. Diabetes in older adults. Diabetes Care. 2012;35(12):2650–2664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bergman H, Ferrucci L, Guralnik J, Hogan DB, Hummel S, Karunananthan S, Wolfson C. Frailty: an emerging research and clinical paradigm—issues and controversies. J Gerontol A Biol Sci Med Sci. 2007;62(7):731–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA; Cardiovascular Health Study Collaborative Research Group . Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M157. [DOI] [PubMed] [Google Scholar]
- 43. Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Abellan van Kan G, Rolland Y, Bergman H, Morley JE, Kritchevsky SB, Vellas B. The I.A.N.A Task Force on frailty assessment of older people in clinical practice. J Nutr Health Aging. 2008;12(1):29–37. [DOI] [PubMed] [Google Scholar]
- 45. Sinclair AJ, Abdelhafiz A, Dunning T, Izquierdo M, Rodriguez Manas L, Bourdel-Marchasson I, Morley JE, Munshi M, Woo J, Vellas B. An international position statement on the management of frailty in diabetes mellitus: summary of recommendations 2017. J Frailty Aging. 2018;7(1):10–20. [DOI] [PubMed] [Google Scholar]
- 46. Sinclair AJ, Abdelhafiz AH, Rodríguez-Mañas L. Frailty and sarcopenia—newly emerging and high impact complications of diabetes. J Diabetes Complications. 2017;31(9):1465–1473. [DOI] [PubMed] [Google Scholar]
- 47. Mathias S, Nayak USL, Isaacs B. Balance in elderly patients: the “get-up and go” test. Arch Phys Med Rehabil. 1986;67(6):387–389. [PubMed] [Google Scholar]
- 48. Bischoff HA, Stähelin HB, Monsch AU, Iversen MD, Weyh A, von Dechend M, Akos R, Conzelmann M, Dick W, Theiler R. Identifying a cut-off point for normal mobility: a comparison of the timed “up and go” test in community-dwelling and institutionalised elderly women. Age Ageing. 2003;32(3):315–320. [DOI] [PubMed] [Google Scholar]
- 49. Studenski S, Perera S, Wallace D, Chandler JM, Duncan PW, Rooney E, Fox M, Guralnik JM. Physical performance measures in the clinical setting. J Am Geriatr Soc. 2003;51(3):314–322. [DOI] [PubMed] [Google Scholar]
- 50. Cesari M. Role of gait speed in the assessment of older patients. JAMA. 2011;305(1):93–94. [DOI] [PubMed] [Google Scholar]
- 51. Roberts HC, Denison HJ, Martin HJ, Patel HP, Syddall H, Cooper C, Sayer AA. A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing. 2011;40(4):423–429. [DOI] [PubMed] [Google Scholar]
- 52. Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinková E, Vandewoude M, Zamboni M; European Working Group on Sarcopenia in Older People . Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on sarcopenia in older people. Age Ageing. 2010;39(4):412–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Morley JE, Cao L. Rapid screening for sarcopenia. J Cachexia Sarcopenia Muscle. 2015;6(4):312–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Prince M, Bryce R, Albanese E, Wimo A, Ribeiro W, Ferri CP. The global prevalence of dementia: a systematic review and metaanalysis. Alzheimers Dement. 2013;9(1):63–75.e2. [DOI] [PubMed] [Google Scholar]
- 55. Biessels GJ, Staekenborg S, Brunner E, Brayne C, Scheltens P. Risk of dementia in diabetes mellitus: a systematic review. Lancet Neurol. 2006;5(1):64–74. [DOI] [PubMed] [Google Scholar]
- 56. Gudala K, Bansal D, Schifano F, Bhansali A. Diabetes mellitus and risk of dementia: a meta-analysis of prospective observational studies. J Diabetes Investig. 2013;4(6):640–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Abner EL, Nelson PT, Kryscio RJ, Schmitt FA, Fardo DW, Woltjer RL, Cairns NJ, Yu L, Dodge HH, Xiong C, Masaki K, Tyas SL, Bennett DA, Schneider JA, Arvanitakis Z. Diabetes is associated with cerebrovascular but not Alzheimer’s disease neuropathology. Alzheimers Dement. 2016;12(8):882–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Cheng G, Huang C, Deng H, Wang H. Diabetes as a risk factor for dementia and mild cognitive impairment: a meta-analysis of longitudinal studies. Intern Med J. 2012;42(5):484–491. [DOI] [PubMed] [Google Scholar]
- 59. Cooper C, Sommerlad A, Lyketsos CG, Livingston G. Modifiable predictors of dementia in mild cognitive impairment: a systematic review and meta-analysis. Am J Psychiatry. 2015;172(4):323–334. [DOI] [PubMed] [Google Scholar]
- 60. Munshi M, Grande L, Hayes M, Ayres D, Suhl E, Capelson R, Lin S, Milberg W, Weinger K. Cognitive dysfunction is associated with poor diabetes control in older adults. Diabetes Care. 2006;29(8):1794–1799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Feil DG, Zhu CW, Sultzer DL. The relationship between cognitive impairment and diabetes self-management in a population-based community sample of older adults with type 2 diabetes. J Behav Med. 2012;35(2):190–199. [DOI] [PubMed] [Google Scholar]
- 62. Yaffe K, Falvey CM, Hamilton N, Harris TB, Simonsick EM, Strotmeyer ES, Shorr RI, Metti A, Schwartz AV; Health ABC Study . Association between hypoglycemia and dementia in a biracial cohort of older adults with diabetes mellitus. JAMA Intern Med. 2013;173(14):1300–1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Punthakee Z, Miller ME, Launer LJ, Williamson JD, Lazar RM, Cukierman-Yaffee T, Seaquist ER, Ismail-Beigi F, Sullivan MD, Lovato LC, Bergenstal RM, Gerstein HC; ACCORD Group of Investigators; ACCORD-MIND Investigators . Poor cognitive function and risk of severe hypoglycemia in type 2 diabetes: post hoc epidemiologic analysis of the ACCORD trial. Diabetes Care. 2012;35(4):787–793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. de Galan BE, Zoungas S, Chalmers J, Anderson C, Dufouil C, Pillai A, Cooper M, Grobbee DE, Hackett M, Hamet P, Heller SR, Lisheng L, MacMahon S, Mancia G, Neal B, Pan CY, Patel A, Poulter N, Travert F, Woodward M; ADVANCE Collaborative Group . Cognitive function and risks of cardiovascular disease and hypoglycaemia in patients with type 2 diabetes: the Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation (ADVANCE) trial. Diabetologia. 2009;52(11):2328–2336. [DOI] [PubMed] [Google Scholar]
- 65. American Diabetes Association. 4 Comprehensive medical evaluation and assessment of comorbidities: standards of medical care in diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S34–S45. [DOI] [PubMed] [Google Scholar]
- 66. American Diabetes Association. 12 Older adults: standards of medical care in diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S139–S147. [DOI] [PubMed] [Google Scholar]
- 67. Sinclair AJ, Hillson R, Bayer AJ; National Expert Working Group . Diabetes and dementia in older people: a best clinical practice statement by a multidisciplinary national expert working group. Diabet Med. 2014;31(9):1024–1031. [DOI] [PubMed] [Google Scholar]
- 68. Geijselaers SL, Sep SJ, Stehouwer CD, Biessels GJ. Glucose regulation, cognition, and brain MRI in type 2 diabetes: a systematic review. Lancet Diabetes Endocrinol. 2015;3(1):75–89. [DOI] [PubMed] [Google Scholar]
- 69. Moyer VA; U.S. Preventive Services Task Force . Screening for cognitive impairment in older adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160(11):791–797. [DOI] [PubMed] [Google Scholar]
- 70. Lin JS, O’Connor E, Rossom RC, Perdue LA, Eckstrom E. Screening for cognitive impairment in older adults: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2013;159(9):601–612. [DOI] [PubMed] [Google Scholar]
- 71. Dong Y, Kua ZJ, Khoo EY, Koo EH, Merchant RA. The utility of brief cognitive tests for patients with type 2 diabetes mellitus: a systematic review. J Am Med Dir Assoc. 2016;17(10):889–895. [DOI] [PubMed] [Google Scholar]
- 72. Koekkoek PS, Janssen J, Kooistra M, Biesbroek JM, Groeneveld O, van den Berg E, Kappelle LJ, Biessels GJ, Rutten GE. Case-finding for cognitive impairment among people with type 2 diabetes in primary care using the Test Your Memory and Self-Administered Gerocognitive Examination questionnaires: the Cog-ID study. Diabet Med. 2016;33(6):812–819. [DOI] [PubMed] [Google Scholar]
- 73. Johnston SS, Conner C, Aagren M, Ruiz K, Bouchard J. Association between hypoglycaemic events and fall-related fractures in Medicare-covered patients with type 2 diabetes. Diabetes Obes Metab. 2012;14(7):634–643. [DOI] [PubMed] [Google Scholar]
- 74. Signorovitch JE, Macaulay D, Diener M, Yan Y, Wu EQ, Gruenberger JB, Frier BM. Hypoglycaemia and accident risk in people with type 2 diabetes mellitus treated with non-insulin antidiabetes drugs. Diabetes Obes Metab. 2013;15(4):335–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Zhao Y, Kachroo S, Kawabata H, Colilla S, Mukherjee J, Fonseca V, Iloeje U, Shi L. Association between hypoglycemia and fall-related fractures and health care utilization in older veterans with type 2 diabetes. Endocr Pract. 2016;22(2):196–204. [DOI] [PubMed] [Google Scholar]
- 76. Zoungas S, Patel A, Chalmers J, de Galan BE, Li Q, Billot L, Woodward M, Ninomiya T, Neal B, MacMahon S, Grobbee DE, Kengne AP, Marre M, Heller S; ADVANCE Collaborative Group . Severe hypoglycemia and risks of vascular events and death. N Engl J Med. 2010;363(15):1410–1418. [DOI] [PubMed] [Google Scholar]
- 77. Benoit SR, Zhang Y, Geiss LS, Gregg EW, Albright A. Trends in diabetic ketoacidosis hospitalizations and in-hospital mortality—United States, 2000–2014. MMWR Morb Mortal Wkly Rep. 2018;67(12):362–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Nathan DM, Genuth S, Lachin J, Cleary P, Crofford O, Davis M, Rand L, Siebert C; Diabetes Control and Complications Trial Research Group . The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–986. [DOI] [PubMed] [Google Scholar]
- 79. Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, Peters AL, Tsapas A, Wender R, Matthews DR. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38(1):140–149. [DOI] [PubMed] [Google Scholar]
- 80. U.S. Department of Veterans Affairs, Department of Defense Management of diabetes mellitus in primary care (2017). Available at: www.healthquality.va.gov/guidelines/CD/diabetes/. Accessed 14 February 2019.
- 81. Currie CJ, Peters JR, Tynan A, Evans M, Heine RJ, Bracco OL, Zagar T, Poole CD. Survival as a function of HbA1c in people with type 2 diabetes: a retrospective cohort study. Lancet. 2010;375(9713):481–489. [DOI] [PubMed] [Google Scholar]
- 82. Riddle MC, Ambrosius WT, Brillon DJ, Buse JB, Byington RP, Cohen RM, Goff DC Jr, Malozowski S, Margolis KL, Probstfield JL, Schnall A, Seaquist ER; Action to Control Cardiovascular Risk in Diabetes Investigators . Epidemiologic relationships between A1C and all-cause mortality during a median 3.4-year follow-up of glycemic treatment in the ACCORD trial. Diabetes Care. 2010;33(5):983–990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Gerstein HC, Beavers DP, Bertoni AG, Bigger JT, Buse JB, Craven TE, Cushman WC, Fonseca V, Geller NL, Giddings SJ, Grimm RH, Genuth S, Hramiak I, Ismail-Beigi F, Jimenez CRL, Kirby R, Probstfield J, Riddle MC, Seaquist ER, Friedewald WT; ACCORD Study Group . Nine-year effects of 3.7 years of intensive glycemic control on cardiovascular outcomes. Diabetes Care. 2016;39(5):701–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Agrawal L, Azad N, Bahn GD, Ge L, Reaven PD, Hayward RA, Reda DJ, Emanuele NV; VADT Study Group . Long-term follow-up of intensive glycaemic control on renal outcomes in the Veterans Affairs Diabetes Trial (VADT). Diabetologia. 2018;61(2):295–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Herman WH, Ilag LL, Johnson SL, Martin CL, Sinding J, Al Harthi A, Plunkett CD, LaPorte FB, Burke R, Brown MB, Halter JB, Raskin P. A clinical trial of continuous subcutaneous insulin infusion versus multiple daily injections in older adults with type 2 diabetes. Diabetes Care. 2005;28(7):1568–1573. [DOI] [PubMed] [Google Scholar]
- 86. Lee P, Chang A, Blaum C, Vlajnic A, Gao L, Halter J. Comparison of safety and efficacy of insulin glargine and neutral protamine hagedorn insulin in older adults with type 2 diabetes mellitus: results from a pooled analysis. J Am Geriatr Soc. 2012;60(1):51–59. [DOI] [PubMed] [Google Scholar]
- 87. Munshi MN, Segal AR, Suhl E, Staum E, Desrochers L, Sternthal A, Giusti J, McCartney R, Lee Y, Bonsignore P, Weinger K. Frequent hypoglycemia among elderly patients with poor glycemic control. Arch Intern Med. 2011;171(4):362–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Weinstock RS, DuBose SN, Bergenstal RM, Chaytor NS, Peterson C, Olson BA, Munshi MN, Perrin AJ, Miller KM, Beck RW, Liljenquist DR, Aleppo G, Buse JB, Kruger D, Bhargava A, Goland RS, Edelen RC, Pratley RE, Peters AL, Rodriguez H, Ahmann AJ, Lock JP, Garg SK, Rickels MR, Hirsch IB; T1D Exchange Severe Hypoglycemia in Older Adults With Type 1 Diabetes Study Group . Risk factors associated with severe hypoglycemia in older adults with type 1 diabetes. Diabetes Care. 2016;39(4):603–610. [DOI] [PubMed] [Google Scholar]
- 89. Munshi MN, Pandya N, Umpierrez GE, DiGenio A, Zhou R, Riddle MC. Contributions of basal and prandial hyperglycemia to total hyperglycemia in older and younger adults with type 2 diabetes mellitus. J Am Geriatr Soc. 2013;61(4):535–541. [DOI] [PubMed] [Google Scholar]
- 90. Vigersky RA, Fonda SJ, Chellappa M, Walker MS, Ehrhardt NM. Short- and long-term effects of real-time continuous glucose monitoring in patients with type 2 diabetes. Diabetes Care. 2012;35(1):32–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Ruedy KJ, Parkin CG, Riddlesworth TD, Graham C; DIAMOND Study Group . Continuous glucose monitoring in older adults with type 1 and type 2 diabetes using multiple daily injections of insulin: Results from the DIAMOND trial. J Diabetes Sci Technol. 2017;11(6):1138–1146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Sacks DB, John WG. Interpretation of hemoglobin A1c values. JAMA. 2014;311(22):2271–2272. [DOI] [PubMed] [Google Scholar]
- 93. World Health Organization Use of glycated haemoglobin (HbA1c) in the diagnosis of diabetes mellitus: abbreviated report of a WHO consultation. Geneva, Switzerland: World Health Organization; 2011. [PubMed]
- 94. Pastors JG, Warshaw H, Daly A, Franz M, Kulkarni K. The evidence for the effectiveness of medical nutrition therapy in diabetes management. Diabetes Care. 2002;25(3):608–613. [DOI] [PubMed] [Google Scholar]
- 95. Look AHEAD Research Group Eight-year weight losses with an intensive lifestyle intervention: the look AHEAD study. Obesity (Silver Spring). 2014;22(1):5–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Ali S, Garcia JM. Sarcopenia, cachexia and aging: diagnosis, mechanisms and therapeutic options—a mini-review. Gerontology. 2014;60(4):294–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Bell KJ, Barclay AW, Petocz P, Colagiuri S, Brand-Miller JC. Efficacy of carbohydrate counting in type 1 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2014;2(2):133–140. [DOI] [PubMed] [Google Scholar]
- 98. Rossi MC, Nicolucci A, Di Bartolo P, Bruttomesso D, Girelli A, Ampudia FJ, Kerr D, Ceriello A, Mayor CL, Pellegrini F, Horwitz D, Vespasiani G. Diabetes Interactive Diary: a new telemedicine system enabling flexible diet and insulin therapy while improving quality of life: an open-label, international, multicenter, randomized study. Diabetes Care. 2010;33(1):109–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Wheeler ML, Dunbar SA, Jaacks LM, Karmally W, Mayer-Davis EJ, Wylie-Rosett J, Yancy WS Jr. Macronutrients, food groups, and eating patterns in the management of diabetes: a systematic review of the literature, 2010. Diabetes Care. 2012;35(2):434–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Bowen ME, Cavanaugh KL, Wolff K, Davis D, Gregory RP, Shintani A, Eden S, Wallston K, Elasy T, Rothman RL. The diabetes nutrition education study randomized controlled trial: a comparative effectiveness study of approaches to nutrition in diabetes self-management education. Patient Educ Couns. 2016;99(8):1368–1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. American Diabetes Association. 5 Lifestyle management: standards of medical care in diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S46–S60. [DOI] [PubMed] [Google Scholar]
- 102. Weinger K, Beverly EA, Smaldone A. Diabetes self-care and the older adult. West J Nurs Res. 2014;36(9):1272–1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Abd Aziz NA, Teng NI, Abdul Hamid MR, Ismail NH. Assessing the nutritional status of hospitalized elderly. Clin Interv Aging. 2017;12:1615–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Cascio BL, Logomarsino JV. Evaluating the effectiveness of five screening tools used to identify malnutrition risk in hospitalized elderly: a systematic review. Geriatr Nurs. 2018;39(1):95–102. [DOI] [PubMed] [Google Scholar]
- 105. Gómez-Huelgas R, Giner-Galvañ V, Mostaza JM, Cuende JI, de Miguel-Yanes JM, Rovira E, Sánchez-Fuentes D, Suárez Fernández C, Román Sánchez P; SEMI Working Group . Unanswered clinical questions in the management of cardiometabolic risk in the elderly: a statement of the Spanish Society of Internal Medicine. BMC Cardiovasc Disord. 2014;14(1):193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. León-Sanz M, Brosa M, Planas M, García-de-Lorenzo A, Celaya-Pérez S, Hernández JA; PREDyCES Group Researchers . PREDyCES study: the cost of hospital malnutrition in Spain. Nutrition. 2015;31(9):1096–1102. [DOI] [PubMed] [Google Scholar]
- 107. Op den Kamp CM, Langen RC, Haegens A, Schols AM. Muscle atrophy in cachexia: can dietary protein tip the balance? Curr Opin Clin Nutr Metab Care. 2009;12(6):611–616. [DOI] [PubMed] [Google Scholar]
- 108. Baldwin C, Spiro A, Ahern R, Emery PW. Oral nutritional interventions in malnourished patients with cancer: a systematic review and meta-analysis. J Natl Cancer Inst. 2012;104(5):371–385. [DOI] [PubMed] [Google Scholar]
- 109. Morley JE, Argiles JM, Evans WJ, Bhasin S, Cella D, Deutz NE, Doehner W, Fearon KC, Ferrucci L, Hellerstein MK, Kalantar-Zadeh K, Lochs H, MacDonald N, Mulligan K, Muscaritoli M, Ponikowski P, Posthauer ME, Rossi Fanelli F, Schambelan M, Schols AM, Schuster MW, Anker SD; Society for Sarcopenia, Cachexia, and Wasting Disease . Nutritional recommendations for the management of sarcopenia. J Am Med Dir Assoc. 2010;11(6):391–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Esposito K, Maiorino MI, Ciotola M, Di Palo C, Scognamiglio P, Gicchino M, Petrizzo M, Saccomanno F, Beneduce F, Ceriello A, Giugliano D. Effects of a Mediterranean-style diet on the need for antihyperglycemic drug therapy in patients with newly diagnosed type 2 diabetes: a randomized trial. Ann Intern Med. 2009;151(5):306–314. [DOI] [PubMed] [Google Scholar]
- 111. Cespedes EM, Hu FB, Tinker L, Rosner B, Redline S, Garcia L, Hingle M, Van Horn L, Howard BV, Levitan EB, Li W, Manson JE, Phillips LS, Rhee JJ, Waring ME, Neuhouser ML. Multiple healthful dietary patterns and type 2 diabetes in the Women’s Health Initiative. Am J Epidemiol. 2016;183(7):622–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Ley SH, Hamdy O, Mohan V, Hu FB. Prevention and management of type 2 diabetes: dietary components and nutritional strategies. Lancet. 2014;383(9933):1999–2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Rinaldi S, Campbell EE, Fournier J, O’Connor C, Madill J. A comprehensive review of the literature supporting recommendations from the Canadian Diabetes Association for the use of a plant-based diet for management of type 2 diabetes. Can J Diabetes. 2016;40(5):471–477. [DOI] [PubMed] [Google Scholar]
- 114. Otten JJ, Pitzi Hellwig J, Meyers J, eds. Dietary Reference Intakes: The Essential Guide to Nutrient Requirements. Washington, DC: National Academies Press; 2006. [Google Scholar]
- 115. Hooper L, Bunn D, Jimoh FO, Fairweather-Tait SJ. Water-loss dehydration and aging. Mech Ageing Dev. 2014;136-137:50–58. [DOI] [PubMed] [Google Scholar]
- 116. Maillot M, Drewnowski A. A conflict between nutritionally adequate diets and meeting the 2010 dietary guidelines for sodium. Am J Prev Med. 2012;42(2):174–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Heuberger RA. Alcohol and the older adult: a comprehensive review. J Nutr Elder. 2009;28(3):203–235. [DOI] [PubMed] [Google Scholar]
- 118. Kuerbis A, Sacco P, Blazer DG, Moore AA. Substance abuse among older adults. Clin Geriatr Med. 2014;30(3):629–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Dorner B, Friedrich EK, Posthauer ME. Practice paper of the American Dietetic Association: individualized nutrition approaches for older adults in health care communities. J Am Diet Assoc. 2010;110(10):1554–1563. [DOI] [PubMed] [Google Scholar]
- 120. Munshi MN, Florez H, Huang ES, Kalyani RR, Mupanomunda M, Pandya N, Swift CS, Taveira TH, Haas LB. Management of diabetes in long-term care and skilled nursing facilities: a position statement of the American Diabetes Association. Diabetes Care. 2016;39(2):308–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Sami W, Ansari T, Butt NS, Hamid MRA. Effect of diet on type 2 diabetes mellitus: a review. Int J Health Sci (Qassim). 2017;11(2):65–71. [PMC free article] [PubMed] [Google Scholar]
- 122. Canadian Agency for Drugs and Technologies in Health Diabetic Diets for Frail Elderly Long-Term Care Residents With Type II Diabetes Mellitus: A Review of Guidelines. Ottawa (ON), Canada: Canadian Agency for Drugs and Technologies in Health; 2015. [PubMed] [Google Scholar]
- 123. Hooper L, Bunn DK, Downing A, Jimoh FO, Groves J, Free C, Cowap V, Potter JF, Hunter PR, Shepstone L. Which frail older people are dehydrated? J Gerontol A Biol Sci Med Sci. 2016;71(10):1341–1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Bunn D, Jimoh F, Wilsher SH, Hooper L. Increasing fluid intake and reducing dehydration risk in older people living in long-term care: a systematic review. J Am Med Dir Assoc. 2015;16(2):101–113. [DOI] [PubMed] [Google Scholar]
- 125. Keller H, Beck AM, Namasivayam A; International-Dining in Nursing Home Experts (I-DINE) Consortium . Improving food and fluid intake for older adults living in long-term care: a research agenda. J Am Med Dir Assoc. 2015;16(2):93–100. [DOI] [PubMed] [Google Scholar]
- 126. Bernstein M. Nutritional needs of the older adult. Phys Med Rehabil Clin N Am. 2017;28(4):747–766. [DOI] [PubMed] [Google Scholar]
- 127. Biolo G, Cederholm T, Muscaritoli M. Muscle contractile and metabolic dysfunction is a common feature of sarcopenia of aging and chronic diseases: from sarcopenic obesity to cachexia. Clin Nutr. 2014;33(5):737–748. [DOI] [PubMed] [Google Scholar]
- 128. Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-Year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577–1589. [DOI] [PubMed] [Google Scholar]
- 129. Claesen M, Gillard P, De Smet F, Callens M, De Moor B, Mathieu C. Mortality in individuals treated with glucose-lowering agents: a large, controlled cohort study. J Clin Endocrinol Metab. 2016;101(2):461–469. [DOI] [PubMed] [Google Scholar]
- 130. Chapman LE, Darling AL, Brown JE. Association between metformin and vitamin B12 deficiency in patients with type 2 diabetes: a systematic review and meta-analysis. Diabetes Metab. 2016;42(5):316–327. [DOI] [PubMed] [Google Scholar]
- 131. Aroda VR, Edelstein SL, Goldberg RB, Knowler WC, Marcovina SM, Orchard TJ, Bray GA, Schade DS, Temprosa MG, White NH, Crandall JP; Diabetes Prevention Program Research Group . Long-term metformin use and vitamin B12 deficiency in the diabetes prevention program outcomes study. J Clin Endocrinol Metab. 2016;101(4):1754–1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Germino FW. Noninsulin treatment of type 2 diabetes mellitus in geriatric patients: a review. Clin Ther. 2011;33(12):1868–1882. [DOI] [PubMed] [Google Scholar]
- 133. Qaseem A, Barry MJ, Humphrey LL, Forciea MA; Clinical Guidelines Committee of the American College of Physicians . Oral pharmacologic treatment of type 2 diabetes mellitus: a clinical practice guideline update from the American College of Physicians. Ann Intern Med. 2017;166(4):279–290. [DOI] [PubMed] [Google Scholar]
- 134. Dills DG, Schneider J, Aronoff SL, Azorr MA, Brunner D, Cefalu WT, Cohen AJ, Cyrus J, Freedman Z, Haag BL, Hamilton BP, Littlejohn TW, Lucas CP, Matlock JS, McGill JB, Miller SS, Nikolai T, Ogilvie JT, Podlecki DA, Ricaurte M, Roudebush CP, Singh SP, Smulovitz J, Soler NG, Stone J, Stonesifer LD, Tucker WS, Wallum BJ, White J, Whittier FC, Zieve FJ; Glimepiride/Glyburide Research Group . Clinical evaluation of glimepiride versus glyburide in NIDDM in a double-blind comparative study. Horm Metab Res. 1996;28(9):426–429. [DOI] [PubMed] [Google Scholar]
- 135. Shorr RI, Ray WA, Daugherty JR, Griffin MR. Individual sulfonylureas and serious hypoglycemia in older people. J Am Geriatr Soc. 1996;44(7):751–755. [DOI] [PubMed] [Google Scholar]
- 136. Nesto RW, Bell D, Bonow RO, Fonseca V, Grundy SM, Horton ES, Le Winter M, Porte D, Semenkovich CF, Smith S, Young LH, Kahn R. Thiazolidinedione use, fluid retention, and congestive heart failure: a consensus statement from the American Heart Association and American Diabetes Association. Diabetes Care. 2004;27(1):256–263. [DOI] [PubMed] [Google Scholar]
- 137. Udell JA, Cavender MA, Bhatt DL, Chatterjee S, Farkouh ME, Scirica BM. Glucose-lowering drugs or strategies and cardiovascular outcomes in patients with or at risk for type 2 diabetes: a meta-analysis of randomised controlled trials. Lancet Diabetes Endocrinol. 2015;3(5):356–366. [DOI] [PubMed] [Google Scholar]
- 138. Gilbert RE, Krum H. Heart failure in diabetes: effects of anti-hyperglycaemic drug therapy. Lancet. 2015;385(9982):2107–2117. [DOI] [PubMed] [Google Scholar]
- 139. Zhu ZN, Jiang YF, Ding T. Risk of fracture with thiazolidinediones: an updated meta-analysis of randomized clinical trials. Bone. 2014;68:115–123. [DOI] [PubMed] [Google Scholar]
- 140. Choi HJ, Park C, Lee YK, Ha YC, Jang S, Shin CS. Risk of fractures and diabetes medications: a nationwide cohort study. Osteoporos Int. 2016;27(9):2709–2715. [DOI] [PubMed] [Google Scholar]
- 141. Josse RG, Chiasson JL, Ryan EA, Lau DCW, Ross SA, Yale JF, Leiter LA, Maheux P, Tessier D, Wolever TMS, Gerstein H, Rodger NW, Dornan JM, Murphy LJ, Rabasa-Lhoret R, Meneilly GS. Acarbose in the treatment of elderly patients with type 2 diabetes. Diabetes Res Clin Pract. 2003;59(1):37–42. [DOI] [PubMed] [Google Scholar]
- 142. Li L, Shen JT, Bala MM, Busse JW, Ebrahim S, Vandvik PO, Rios LP, Malaga G, Wong E, Sohani Z, Guyatt GH, Sun X. Incretin treatment and risk of pancreatitis in patients with type 2 diabetes mellitus: systematic review and meta-analysis of randomised and non-randomised studies. BMJ. 2014;348:g2366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Thomsen RW, Pedersen L, Møller N, Kahlert J, Beck-Nielsen H, Sørensen HT. Incretin-based therapy and risk of acute pancreatitis: a nationwide population-based case-control study. Diabetes Care. 2015;38(6):1089–1098. [DOI] [PubMed] [Google Scholar]
- 144. Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, Shaw W, Law G, Desai M, Matthews DR; CANVAS Program Collaborative Group . Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–657. [DOI] [PubMed] [Google Scholar]
- 145. Wanner C, Inzucchi SE, Lachin JM, Fitchett D, von Eynatten M, Mattheus M, Johansen OE, Woerle HJ, Broedl UC, Zinman B; EMPA-REG OUTCOME Investigators . Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med. 2016;375(4):323–334. [DOI] [PubMed] [Google Scholar]
- 146. Gilbert RE, Weir MR, Fioretto P, Law G, Desai M, Kline I, Shaw W, Meininger G. Impact of age and estimated glomerular filtration rate on the glycemic efficacy and safety of canagliflozin: a pooled analysis of clinical studies. Can J Diabetes. 2016;40(3):247–257. [DOI] [PubMed] [Google Scholar]
- 147. Sinclair AJ, Bode B, Harris S, Vijapurkar U, Shaw W, Desai M, Meininger G. Efficacy and safety of canagliflozin in individuals aged 75 and older with type 2 diabetes mellitus: a pooled analysis. J Am Geriatr Soc. 2016;64(3):543–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Bilezikian JP, Watts NB, Usiskin K, Polidori D, Fung A, Sullivan D, Rosenthal N. Evaluation of bone mineral density and bone biomarkers in patients with type 2 diabetes treated with canagliflozin. J Clin Endocrinol Metab. 2016;101(1):44–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Watts NB, Bilezikian JP, Usiskin K, Edwards R, Desai M, Law G, Meininger G. Effects of canagliflozin on fracture risk in patients with type 2 diabetes mellitus. J Clin Endocrinol Metab. 2016;101(1):157–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Erondu N, Desai M, Ways K, Meininger G. Diabetic ketoacidosis and related events in the canagliflozin type 2 diabetes clinical program. Diabetes Care. 2015;38(9):1680–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Peters AL, Buschur EO, Buse JB, Cohan P, Diner JC, Hirsch IB. Euglycemic diabetic ketoacidosis: a potential complication of treatment with sodium-glucose cotransporter 2 inhibition. Diabetes Care. 2015;38(9):1687–1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Zaccardi F, Htike ZZ, Webb DR, Khunti K, Davies MJ. Benefits and harms of once-weekly glucagon-like peptide-1 receptor agonist treatments: a systematic review and network meta-analysis. Ann Intern Med. 2016;164(2):102–113. [DOI] [PubMed] [Google Scholar]
- 153. Wallia A, Molitch ME. Insulin therapy for type 2 diabetes mellitus. JAMA. 2014;311(22):2315–2325. [DOI] [PubMed] [Google Scholar]
- 154. Philis-Tsimikas A. Initiating basal insulin therapy in type 2 diabetes: practical steps to optimize glycemic control. Am J Med. 2013;126(9Suppl 1):S21–S27. [DOI] [PubMed] [Google Scholar]
- 155. Bergenstal RM, Bailey TS, Rodbard D, Ziemen M, Guo H, Muehlen-Bartmer I, Ahmann AJ. Comparison of insulin glargine 300 units/ml and 100 units/ml in adults with type 1 diabetes: continuous glucose monitoring profiles and variability using morning or evening injections. Diabetes Care. 2017;40(4):554–560. [DOI] [PubMed] [Google Scholar]
- 156. Marso SP, McGuire DK, Zinman B, Poulter NR, Emerson SS, Pieber TR, Pratley RE, Haahr PM, Lange M, Brown-Frandsen K, Moses A, Skibsted S, Kvist K, Buse JB; DEVOTE Study Group . Efficacy and safety of degludec versus glargine in type 2 diabetes. N Engl J Med. 2017;377(8):723–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Holman RR, Farmer AJ, Davies MJ, Levy JC, Darbyshire JL, Keenan JF, Paul SK; 4-T Study Group . Three-year efficacy of complex insulin regimens in type 2 diabetes. N Engl J Med. 2009;361(18):1736–1747. [DOI] [PubMed] [Google Scholar]
- 158. Rosenstock J, Diamant M, Aroda VR, Silvestre L, Souhami E, Zhou T, Perfetti R, Fonseca V; LixiLan PoC Study Group . Efficacy and safety of lixilan, a titratable fixed-ratio combination of lixisenatide and insulin glargine, versus insulin glargine in type 2 diabetes inadequately controlled on metformin monotherapy: the LixiLan proof-of-concept randomized trial. Diabetes Care. 2016;39(9):1579–1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Freemantle N, Mamdani M, Vilsbøll T, Kongsø JH, Kvist K, Bain SC. Ideglira versus alternative intensification strategies in patients with type 2 diabetes inadequately controlled on basal insulin therapy. Diabetes Ther. 2015;6(4):573–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Maiorino MI, Chiodini P, Bellastella G, Capuano A, Esposito K, Giugliano D. Insulin and glucagon-like peptide 1 receptor agonist combination therapy in type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Diabetes Care. 2017;40(4):614–624. [DOI] [PubMed] [Google Scholar]
- 161. Sinclair A, Dunning T, Rodriguez-Mañas L. Diabetes in older people: new insights and remaining challenges. Lancet Diabetes Endocrinol. 2015;3(4):275–285. [DOI] [PubMed] [Google Scholar]
- 162. Wilding JP, Rajeev SP, DeFronzo RA. Positioning SGLT2 inhibitors/incretin-based therapies in the treatment algorithm. Diabetes Care. 2016;39(Suppl 2):S154–S164. [DOI] [PubMed] [Google Scholar]
- 163. Gellad WF, Grenard JL, Marcum ZA. A systematic review of barriers to medication adherence in the elderly: looking beyond cost and regimen complexity. Am J Geriatr Pharmacother. 2011;9(1):11–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT Jr, Narva AS, Ortiz E. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–520. [DOI] [PubMed] [Google Scholar]
- 165. Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, Rocco MV, Reboussin DM, Rahman M, Oparil S, Lewis CE, Kimmel PL, Johnson KC, Goff DC Jr, Fine LJ, Cutler JA, Cushman WC, Cheung AK, Ambrosius WT; SPRINT Research Group . A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103–2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166. Kjeldsen SE, Lund-Johansen P, Nilsson PM, Mancia G. Unattended blood pressure measurements in the systolic blood pressure intervention trial: implications for entry and achieved blood pressure values compared with other trials. Hypertension. 2016;67(5):808–812. [DOI] [PubMed] [Google Scholar]
- 167. Weiss J, Freeman M, Low A, Fu R, Kerfoot A, Paynter R, Motu’apuaka M, Kondo K, Kansagara D. Benefits and harms of intensive blood pressure treatment in adults aged 60 years or older: a systematic review and meta-analysis. Ann Intern Med. 2017;166(6):419–429. [DOI] [PubMed] [Google Scholar]
- 168. Qaseem A, Wilt TJ, Rich R, Humphrey LL, Frost J, Forciea MA; Clinical Guidelines Committee of the American College of Physicians and the Commission on Health of the Public and Science of the American Academy of Family Physicians . Pharmacologic treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2017;166(6):430–437. [DOI] [PubMed] [Google Scholar]
- 169. de Boer IH, Bangalore S, Benetos A, Davis AM, Michos ED, Muntner P, Rossing P, Zoungas S, Bakris G. Diabetes and hypertension: a position statement by the American Diabetes Association. Diabetes Care. 2017;40(9):1273–1284. [DOI] [PubMed] [Google Scholar]
- 170. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, DePalma SM, Gidding S, Jamerson KA, Jones DW, MacLaughlin EJ, Muntner P, Ovbiagele B, Smith SC Jr, Spencer CC, Stafford RS, Taler SJ, Thomas RJ, Williams KA Sr, Williamson JD, Wright JT Jr. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APHA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):1269–1324. [DOI] [PubMed] [Google Scholar]
- 171. UK Prospective Diabetes Study Group Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998;317(7160):703–713. [PMC free article] [PubMed] [Google Scholar]
- 172. Cushman WC, Evans GW, Byington RP, Goff DC Jr, Grimm RH Jr, Cutler JA, Simons-Morton DG, Basile JN, Corson MA, Probstfield JL, Katz L, Peterson KA, Friedewald WT, Buse JB, Bigger JT, Gerstein HC, Ismail-Beigi F; ACCORD Study Group . Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1575–1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Patel A, MacMahon S, Chalmers J, Neal B, Woodward M, Billot L, Harrap S, Poulter N, Marre M, Cooper M, Glasziou P, Grobbee DE, Hamet P, Heller S, Liu LS, Mancia G, Mogensen CE, Pan CY, Rodgers A, Williams B; ADVANCE Collaborative Group . Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. Lancet. 2007;370(9590):829–840. [DOI] [PubMed] [Google Scholar]
- 174. Hansson L, Zanchetti A, Carruthers SG, Dahlöf B, Elmfeldt D, Julius S, Ménard J, Rahn KH, Wedel H, Westerling S; HOT Study Group . Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. Lancet. 1998;351(9118):1755–1762. [DOI] [PubMed] [Google Scholar]
- 175.175. Buckley LF, Dixon DL, Wohlford GF 4th, Wijesinghe DS, Baker WL, Van Tassell BW. Intensive versus standard blood pressure control in SPRINT-eligible participants of ACCORD-BP [published correction appears in Diabetes Care 2018;41(9):2048]. Diabetes Care. 2017;40:1733–1738. [DOI] [PubMed] [Google Scholar]
- 176. Pohl MA, Blumenthal S, Cordonnier DJ, De Alvaro F, Deferrari G, Eisner G, Esmatjes E, Gilbert RE, Hunsicker LG, de Faria JB, Mangili R, Moore J Jr, Reisin E, Ritz E, Schernthaner G, Spitalewitz S, Tindall H, Rodby RA, Lewis EJ. Independent and additive impact of blood pressure control and angiotensin II receptor blockade on renal outcomes in the Irbesartan Diabetic Nephropathy Trial: clinical implications and limitations. J Am Soc Nephrol. 2005;16(10):3027–3037. [DOI] [PubMed] [Google Scholar]
- 177. Cooper-DeHoff RM, Gong Y, Handberg EM, Bavry AA, Denardo SJ, Bakris GL, Pepine CJ. Tight blood pressure control and cardiovascular outcomes among hypertensive patients with diabetes and coronary artery disease. JAMA. 2010;304(1):61–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Anderson RJ, Bahn GD, Moritz TE, Kaufman D, Abraira C, Duckworth W; VADT Study Group . Blood pressure and cardiovascular disease risk in the Veterans Affairs Diabetes Trial. Diabetes Care. 2011;34(1):34–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179. Zhao W, Katzmarzyk PT, Horswell R, Wang Y, Li W, Johnson J, Heymsfield SB, Cefalu WT, Ryan DH, Hu G. Aggressive blood pressure control increases coronary heart disease risk among diabetic patients. Diabetes Care. 2013;36(10):3287–3296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Li W, Katzmarzyk PT, Horswell R, Wang Y, Johnson J, Hu G. Blood pressure and all-cause mortality among patients with type 2 diabetes. Int J Cardiol. 2016;206:116–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Leehey DJ, Zhang JH, Emanuele NV, Whaley-Connell A, Palevsky PM, Reilly RF, Guarino P, Fried LF; VA NEPHRON-D Study Group . BP and renal outcomes in diabetic kidney disease: the Veterans Affairs Nephropathy in Diabetes Trial. Clin J Am Soc Nephrol. 2015;10(12):2159–2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Bangalore S, Kumar S, Lobach I, Messerli FH. Blood pressure targets in subjects with type 2 diabetes mellitus/impaired fasting glucose: observations from traditional and Bayesian random-effects meta-analyses of randomized trials. Circulation. 2011;123(24):2799–2810. [DOI] [PubMed] [Google Scholar]
- 183. McBrien K, Rabi DM, Campbell N, Barnieh L, Clement F, Hemmelgarn BR, Tonelli M, Leiter LA, Klarenbach SW, Manns BJ. Intensive and standard blood pressure targets in patients with type 2 diabetes mellitus: systematic review and meta-analysis. Arch Intern Med. 2012;172(17):1296–1303. [DOI] [PubMed] [Google Scholar]
- 184. Reboldi G, Gentile G, Manfreda VM, Angeli F, Verdecchia P. Tight blood pressure control in diabetes: evidence-based review of treatment targets in patients with diabetes. Curr Cardiol Rep. 2012;14(1):89–96. [DOI] [PubMed] [Google Scholar]
- 185. Arguedas JA, Leiva V, Wright JM. Blood pressure targets for hypertension in people with diabetes mellitus. Cochrane Database Syst Rev. 2013; (10):CD008277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Emdin CA, Rahimi K, Neal B, Callender T, Perkovic V, Patel A. Blood pressure lowering in type 2 diabetes: a systematic review and meta-analysis. JAMA. 2015;313(6):603–615. [DOI] [PubMed] [Google Scholar]
- 187. Brunström M, Carlberg B. Effect of antihypertensive treatment at different blood pressure levels in patients with diabetes mellitus: systematic review and meta-analyses. BMJ. 2016;352:i717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. Xie X, Atkins E, Lv J, Bennett A, Neal B, Ninomiya T, Woodward M, MacMahon S, Turnbull F, Hillis GS, Chalmers J, Mant J, Salam A, Rahimi K, Perkovic V, Rodgers A. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016;387(10017):435–443. [DOI] [PubMed] [Google Scholar]
- 189. Solini A, Grossman E. What should be the target blood pressure in elderly patients with diabetes? Diabetes Care. 2016;39(Suppl 2):S234–S243. [DOI] [PubMed] [Google Scholar]
- 190. Hermida RC, Ayala DE, Mojón A, Fernández JR. Influence of time of day of blood pressure-lowering treatment on cardiovascular risk in hypertensive patients with type 2 diabetes. Diabetes Care. 2011;34(6):1270–1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Lewis EJ, Hunsicker LG, Bain RP, Rohde RD; The Collaborative Study Group . The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. N Engl J Med. 1993;329(20):1456–1462. [DOI] [PubMed] [Google Scholar]
- 192. Brenner BM, Cooper ME, de Zeeuw D, Keane WF, Mitch WE, Parving HH, Remuzzi G, Snapinn SM, Zhang Z, Shahinfar S; RENAAL Study Investigators . Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med. 2001;345(12):861–869. [DOI] [PubMed] [Google Scholar]
- 193. Lewis EJ, Hunsicker LG, Clarke WR, Berl T, Pohl MA, Lewis JB, Ritz E, Atkins RC, Rohde R, Raz I; Collaborative Study Group . Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med. 2001;345(12):851–860. [DOI] [PubMed] [Google Scholar]
- 194. Barnett AH, Bain SC, Bouter P, Karlberg B, Madsbad S, Jervell J, Mustonen J; Diabetics Exposed to Telmisartan and Enalapril Study Group . Angiotensin-receptor blockade versus converting-enzyme inhibition in type 2 diabetes and nephropathy. N Engl J Med. 2004;351(19):1952–1961. [DOI] [PubMed] [Google Scholar]
- 195. Cheng J, Zhang W, Zhang X, Han F, Li X, He X, Li Q, Chen J. Effect of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers on all-cause mortality, cardiovascular deaths, and cardiovascular events in patients with diabetes mellitus: a meta-analysis. JAMA Intern Med. 2014;174(5):773–785. [DOI] [PubMed] [Google Scholar]
- 196. Catalá-López F, Macías Saint-Gerons D, González-Bermejo D, Rosano GM, Davis BR, Ridao M, Zaragoza A, Montero-Corominas D, Tobías A, de la Fuente-Honrubia C, Tabarés-Seisdedos R, Hutton B. Cardiovascular and renal outcomes of renin-angiotensin system blockade in adult patients with diabetes mellitus: a systematic review with network meta-analyses [published correction appears in PLoS Med 2016;13(6):e1002064]. PLoS Med. 2016;13(3):e1001971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197. Wu HY, Huang JW, Lin HJ, Liao WC, Peng YS, Hung KY, Wu KD, Tu YK, Chien KL. Comparative effectiveness of renin-angiotensin system blockers and other antihypertensive drugs in patients with diabetes: systematic review and Bayesian network meta-analysis. BMJ. 2013;347:f6008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198. Fried LF, Emanuele N, Zhang JH, Brophy M, Conner TA, Duckworth W, Leehey DJ, McCullough PA, O’Connor T, Palevsky PM, Reilly RF, Seliger SL, Warren SR, Watnick S, Peduzzi P, Guarino P; VA NEPHRON-D Investigators . Combined angiotensin inhibition for the treatment of diabetic nephropathy. N Engl J Med. 2013;369(20):1892–1903. [DOI] [PubMed] [Google Scholar]
- 199. Bakris GL, Williams M, Dworkin L, Elliott WJ, Epstein M, Toto R, Tuttle K, Douglas J, Hsueh W, Sowers J; National Kidney Foundation Hypertension and Diabetes Executive Committees Working Group . Preserving renal function in adults with hypertension and diabetes: a consensus approach. Am J Kidney Dis. 2000;36(3):646–661. [DOI] [PubMed] [Google Scholar]
- 200. Lonn EM, Bosch J, López-Jaramillo P, Zhu J, Liu L, Pais P, Diaz R, Xavier D, Sliwa K, Dans A, Avezum A, Piegas LS, Keltai K, Keltai M, Chazova I, Peters RJ, Held C, Yusoff K, Lewis BS, Jansky P, Parkhomenko A, Khunti K, Toff WD, Reid CM, Varigos J, Leiter LA, Molina DI, McKelvie R, Pogue J, Wilkinson J, Jung H, Dagenais G, Yusuf S; HOPE-3 Investigators . Blood-pressure lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016;374(21):2009–2020. [DOI] [PubMed] [Google Scholar]
- 201. Jamerson K, Weber MA, Bakris GL, Dahlöf B, Pitt B, Shi V, Hester A, Gupte J, Gatlin M, Velazquez EJ; ACCOMPLISH Trial Investigators . Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med. 2008;359(23):2417–2428. [DOI] [PubMed] [Google Scholar]
- 202. Bakris GL, Sarafidis PA, Weir MR, Dahlöf B, Pitt B, Jamerson K, Velazquez EJ, Staikos-Byrne L, Kelly RY, Shi V, Chiang YT, Weber MA; ACCOMPLISH Trial Investigators . Renal outcomes with different fixed-dose combination therapies in patients with hypertension at high risk for cardiovascular events (ACCOMPLISH): a prespecified secondary analysis of a randomised controlled trial. Lancet. 2010;375(9721):1173–1181. [DOI] [PubMed] [Google Scholar]
- 203. Grossman E, Verdecchia P, Shamiss A, Angeli F, Reboldi G. Diuretic treatment of hypertension. Diabetes Care. 2011;34(Suppl 2):S313–S319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. Ernst ME, Moser M. Use of diuretics in patients with hypertension. N Engl J Med. 2009;361(22):2153–2164. [DOI] [PubMed] [Google Scholar]
- 205. Laffin LJ, Bakris GL. Update on blood pressure goals in diabetes mellitus. Curr Cardiol Rep. 2015;17(6):37. [DOI] [PubMed] [Google Scholar]
- 206. Bakris GL, Fonseca V, Katholi RE, McGill JB, Messerli FH, Phillips RA, Raskin P, Wright JT Jr, Oakes R, Lukas MA, Anderson KM, Bell DS; GEMINI Investigators . Metabolic effects of carvedilol vs metoprolol in patients with type 2 diabetes mellitus and hypertension: a randomized controlled trial. JAMA. 2004;292(18):2227–2236. [DOI] [PubMed] [Google Scholar]
- 207. Kreisberg RA, Kasim S. Cholesterol metabolism and aging. Am J Med. 1987;82(1B):54–60. [DOI] [PubMed] [Google Scholar]
- 208. Grundy SM, Benjamin IJ, Burke GL, Chait A, Eckel RH, Howard BV, Mitch W, Smith SC Jr, Sowers JR. Diabetes and cardiovascular disease: a statement for healthcare professionals from the American Heart Association. Circulation. 1999;100(10):1134–1146. [DOI] [PubMed] [Google Scholar]
- 209. Jellinger PS, Handelsman Y, Rosenblit PD, Bloomgarden ZT, Fonseca VA, Garber AJ, Grunberger G, Guerin CK, Bell DSH, Mechanick JI, Pessah-Pollack R, Wyne K, Smith D, Brinton EA, Fazio S, Davidson M. American Association of Clinical Endocrinologists and American College of Endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocr Pract. 2017;23(Suppl 2):1–87. [DOI] [PubMed] [Google Scholar]
- 210. Massing MW, Sueta CA, Chowdhury M, Biggs DP, Simpson RJ Jr. Lipid management among coronary artery disease patients with diabetes mellitus or advanced age. Am J Cardiol. 2001;87(5):646–649. [DOI] [PubMed] [Google Scholar]
- 211. Ma Y, Persuitte GM, Andrews C, Hovey KM, LaMonte MJ, Culver AL, Manson JE, Phillips LS, Liu S, Eaton C, Martin LW, Howard BV, Balasubramanian R, Bird CE, Ockene IS, Sturgeon SR, Ockene JK, Tinker L, Nassir R, Rossouw J. Impact of incident diabetes on atherosclerotic cardiovascular disease according to statin use history among postmenopausal women. Eur J Epidemiol. 2016;31(8):747–761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212. Wenger NK, Lewis SJ. Use of statin therapy to reduce cardiovascular risk in older patients. Curr Gerontol Geriatr Res. 2010:915296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213. Chahil TJ, Ginsberg HN. Diabetic dyslipidemia. Endocrinol Metab Clin North Am. 2006;35(3):491–510. [DOI] [PubMed] [Google Scholar]
- 214. Al Rifai M, Cainzos-Achirica M, Kianoush S, Mirbolouk M, Peng A, Comin-Colet J, Blaha MJ. Coronary artery calcium: recommendations for risk assessment in cardiovascular prevention guidelines [published correction appears in Curr Treat Options Cardiovasc Med 2018;20(11):92]. Curr Treat Options Cardiovasc Med. 2018;20(11):89.30255362 [Google Scholar]
- 215. Pyŏrälä K, Pedersen TR, Kjekshus J, Faergeman O, Olsson AG, Thorgeirsson G. Cholesterol lowering with simvastatin improves prognosis of diabetic patients with coronary heart disease. A subgroup analysis of the Scandinavian Simvastatin Survival Study (4S) [published correction appears in Diabetes Care. 1997;20(6):1048]. Diabetes Care. 1997;20(4):614–620. [DOI] [PubMed] [Google Scholar]
- 216. Scandinavian Simvastatin Survival Study Group Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet. 1994;344(8934):1383–1389. [PubMed] [Google Scholar]
- 217. Goldberg RB, Mellies MJ, Sacks FM, Moyé LA, Howard BV, Howard WJ, Davis BR, Cole TG, Pfeffer MA, Braunwald E; The CARE Investigators . Cardiovascular events and their reduction with pravastatin in diabetic and glucose-intolerant myocardial infarction survivors with average cholesterol levels: subgroup analyses in the Cholesterol and Recurrent Events (CARE) trial. Circulation. 1998;98(23):2513–2519. [DOI] [PubMed] [Google Scholar]
- 218. Sacks FM, Pfeffer MA, Moye LA, Rouleau JL, Rutherford JD, Cole TG, Brown L, Warnica JW, Arnold JM, Wun CC, Davis BR, Braunwald E. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med. 1996;335(14):1001–1009. [DOI] [PubMed] [Google Scholar]
- 219. Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998;339(19):1349–1357. [DOI] [PubMed] [Google Scholar]
- 220. Olafsdottir E, Aspelund T, Sigurdsson G, Thorsson B, Eiriksdottir G, Harris TB, Launer LJ, Benediktsson R, Gudnason V. Effects of statin medication on mortality risk associated with type 2 diabetes in older persons: the population-based AGES-Reykjavik Study. BMJ Open. 2011;1(1):e000132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221. Neil HA, DeMicco DA, Luo D, Betteridge DJ, Colhoun HM, Durrington PN, Livingstone SJ, Fuller JH, Hitman GA; CARDS Study Investigators . Analysis of efficacy and safety in patients aged 65–75 years at randomization: Collaborative Atorvastatin Diabetes Study (CARDS). Diabetes Care. 2006;29(11):2378–2384. [DOI] [PubMed] [Google Scholar]
- 222. Shepherd J, Barter P, Carmena R, Deedwania P, Fruchart JC, Haffner S, Hsia J, Breazna A, LaRosa J, Grundy S, Waters D. Effect of lowering LDL cholesterol substantially below currently recommended levels in patients with coronary heart disease and diabetes: the Treating to New Targets (TNT) study. Diabetes Care. 2006;29(6):1220–1226. [DOI] [PubMed] [Google Scholar]
- 223. Lloyd SM, Stott DJ, de Craen AJ, Kearney PM, Sattar N, Perry I, Packard CJ, Briggs A, Marchbank L, Comber H, Jukema JW, Westendorp RG, Trompet S, Buckley BM, Ford I. Long-term effects of statin treatment in elderly people: extended follow-up of the Prospective Study of Pravastatin in the Elderly at Risk (PROSPER). PLoS One. 2013;8(9):e72642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224. Amarenco P, Bogousslavsky J, Callahan A III, Goldstein LB, Hennerici M, Rudolph AE, Sillesen H, Simunovic L, Szarek M, Welch KM, Zivin JA; Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Investigators . High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006;355(6):549–559. [DOI] [PubMed] [Google Scholar]
- 225. Hammersley D, Signy M. Ezetimibe: an update on its clinical usefulness in specific patient groups. Ther Adv Chronic Dis. 2017;8(1):4–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226. Pokharel Y, Chinnakondepalli K, Vilain K, Wang K, Mark DB, Davies G, Blazing MA, Giugliano RP, Braunwald E, Cannon CP, Cohen DJ, Magnuson EA. Impact of ezetimibe on the rate of cardiovascular-related hospitalizations and associated costs among patients with a recent acute coronary syndrome: results from the IMPROVE-IT Trial (Improved Reduction of Outcomes: Vytorin Efficacy International Trial). Circ Cardiovasc Qual Outcomes. 2017;10(5):e003201. [DOI] [PubMed] [Google Scholar]
- 227. Fujisue K, Tsujita K. Current status of lipid management in acute coronary syndrome. J Cardiol. 2017;70(2):101–106. [DOI] [PubMed] [Google Scholar]
- 228. Robinson JG, Farnier M, Krempf M, Bergeron J, Luc G, Averna M, Stroes ES, Langslet G, Raal FJ, El Shahawy M, Koren MJ, Lepor NE, Lorenzato C, Pordy R, Chaudhari U, Kastelein JJ; ODYSSEY LONG TERM Investigators . Efficacy and safety of alirocumab in reducing lipids and cardiovascular events. N Engl J Med. 2015;372(16):1489–1499. [DOI] [PubMed] [Google Scholar]
- 229. Sabatine MS, Giugliano RP, Wiviott SD, Raal FJ, Blom DJ, Robinson J, Ballantyne CM, Somaratne R, Legg J, Wasserman SM, Scott R, Koren MJ, Stein EA; Open-Label Study of Long-Term Evaluation Against LDL Cholesterol (OSLER) Investigators . Efficacy and safety of evolocumab in reducing lipids and cardiovascular events. N Engl J Med. 2015;372(16):1500–1509. [DOI] [PubMed] [Google Scholar]
- 230. Chaudhary A, Iqbal U, Anwar H, Siddiqui HU, Alvi M. Acute pancreatitis secondary to severe hypertriglyceridemia: management of severe hypertriglyceridemia in emergency setting. Gastroenterol Res. 2017;10(3):190–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231. Chew EY, Ambrosius WT, Davis MD, Danis RP, Gangaputra S, Greven CM, Hubbard L, Esser BA, Lovato JF, Perdue LH, Goff DC Jr, Cushman WC, Ginsberg HN, Elam MB, Genuth S, Gerstein HC, Schubart U, Fine LJ; ACCORD Study Group; ACCORD Eye Study Group . Effects of medical therapies on retinopathy progression in type 2 diabetes. N Engl J Med. 2010;363(3):233–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232. Keech AC, Mitchell P, Summanen PA, O’Day J, Davis TM, Moffitt MS, Taskinen MR, Simes RJ, Tse D, Williamson E, Merrifield A, Laatikainen LT, d’Emden MC, Crimet DC, O’Connell RL, Colman PG; FIELD Study Investigators . Effect of fenofibrate on the need for laser treatment for diabetic retinopathy (FIELD study): a randomised controlled trial. Lancet. 2007;370(9600):1687–1697. [DOI] [PubMed] [Google Scholar]
- 233. Action to Control Cardiovascular Risk in Diabetes Follow-On (ACCORDION) Eye Study Group and the Action to Control Cardiovascular Risk in Diabetes Follow-On (ACCORDION) Study Group Persistent effects of intensive glycemic control on retinopathy in type 2 diabetes in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) follow-on study. Diabetes Care. 2016;39(7):1089–1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234. Lakatta EG. Changes in cardiovascular function with aging. Eur Heart J. 1990;11(Suppl C):22–29. [DOI] [PubMed]
- 235. Cameron JD, Bulpitt CJ, Pinto ES, Rajkumar C. The aging of elastic and muscular arteries: a comparison of diabetic and nondiabetic subjects. Diabetes Care. 2003;26(7):2133–2138. [DOI] [PubMed] [Google Scholar]
- 236. Pinto ES, Mensah R, Meeran K, Cameron JD, Murugaesu N, Bulpitt CJ, Rajkumar C. Peripheral arterial compliance differs between races: comparison among Asian, Afro-Caribbeans, and white Caucasians with type 2 diabetes. Diabetes Care. 2005;28(2):496. [DOI] [PubMed] [Google Scholar]
- 237. Henry RM, Paulus WJ, Kamp O, Kostense PJ, Spijkerman AM, Dekker JM, Nijpels G, Heine RJ, Bouter LM, Stehouwer CD. Deteriorating glucose tolerance status is associated with left ventricular dysfunction—the Hoorn Study. Neth J Med. 2008;66(3):110–117. [PubMed] [Google Scholar]
- 238. Boonman-de Winter LJM, Rutten FH, Cramer MJM, Landman MJ, Liem AH, Rutten GE, Hoes AW. High prevalence of previously unknown heart failure and left ventricular dysfunction in patients with type 2 diabetes. Diabetologia. 2012;55(8):2154–2162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239. Cavender MA, Steg PG, Smith SC Jr, Eagle K, Ohman EM, Goto S, Kuder J, Im K, Wilson PW, Bhatt DL; REACH Registry Investigators . Impact of diabetes mellitus on hospitalization for heart failure, cardiovascular events, and death: outcomes at 4 years from the Reduction of Atherothrombosis for Continued Health (REACH) registry. Circulation. 2015;132(10):923–931. [DOI] [PubMed] [Google Scholar]
- 240. Eurich DT, Weir DL, Majumdar SR, Tsuyuki RT, Johnson JA, Tjosvold L, Vanderloo SE, McAlister FA. Comparative safety and effectiveness of metformin in patients with diabetes mellitus and heart failure: systematic review of observational studies involving 34,000 patients. Circ Heart Fail. 2013;6(3):395–402. [DOI] [PubMed] [Google Scholar]
- 241. Masoudi FA, Inzucchi SE, Wang Y, Havranek EP, Foody JM, Krumholz HM. Thiazolidinediones, metformin, and outcomes in older patients with diabetes and heart failure: an observational study. Circulation. 2005;111(5):583–590. [DOI] [PubMed] [Google Scholar]
- 242. Chiasson JL, Josse RG, Gomis R, Hanefeld M, Karasik A, Laakso M; STOP-NIDDM Trial Research Group . Acarbose treatment and the risk of cardiovascular disease and hypertension in patients with impaired glucose tolerance: the STOP-NIDDM trial. JAMA. 2003;290(4):486–494. [DOI] [PubMed] [Google Scholar]
- 243. Chang YC, Chuang LM, Lin JW, Chen ST, Lai MS, Chang CH. Cardiovascular risks associated with second-line oral antidiabetic agents added to metformin in patients with type 2 diabetes: a nationwide cohort study. Diabet Med. 2015;32(11):1460–1469. [DOI] [PubMed] [Google Scholar]
- 244. Lee YC, Chang CH, Dong YH, Lin JW, Wu LC, Hwang JS, Chuang LM. Comparing the risks of hospitalized heart failure associated with glinide, sulfonylurea, and acarbose use in type 2 diabetes: a nationwide study. Int J Cardiol. 2017;228:1007–1014. [DOI] [PubMed] [Google Scholar]
- 245. Dargie HJ, Hildebrandt PR, Riegger GA, McMurray JJ, McMorn SO, Roberts JN, Zambanini A, Wilding JP. A randomized, placebo-controlled trial assessing the effects of rosiglitazone on echocardiographic function and cardiac status in type 2 diabetic patients with New York Heart Association functional class I or II heart failure. J Am Coll Cardiol. 2007;49(16):1696–1704. [DOI] [PubMed] [Google Scholar]
- 246. Lago RM, Singh PP, Nesto RW. Congestive heart failure and cardiovascular death in patients with prediabetes and type 2 diabetes given thiazolidinediones: a meta-analysis of randomised clinical trials. Lancet. 2007;370(9593):1129–1136. [DOI] [PubMed] [Google Scholar]
- 247. Mannucci E, Monami M, Lamanna C, Gensini GF, Marchionni N. Pioglitazone and cardiovascular risk. A comprehensive meta-analysis of randomized clinical trials. Diabetes Obes Metab. 2008;10(12):1221–1238. [DOI] [PubMed] [Google Scholar]
- 248. Scirica BM, Bhatt DL, Braunwald E, Steg PG, Davidson J, Hirshberg B, Ohman P, Frederich R, Wiviott SD, Hoffman EB, Cavender MA, Udell JA, Desai NR, Mosenzon O, McGuire DK, Ray KK, Leiter LA, Raz I; SAVOR-TIMI 53 Steering Committee and Investigators . Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med. 2013;369(14):1317–1326. [DOI] [PubMed] [Google Scholar]
- 249. White WB, Cannon CP, Heller SR, Nissen SE, Bergenstal RM, Bakris GL, Perez AT, Fleck PR, Mehta CR, Kupfer S, Wilson C, Cushman WC, Zannad F; EXAMINE Investigators . Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N Engl J Med. 2013;369(14):1327–1335. [DOI] [PubMed] [Google Scholar]
- 250. Green JB, Bethel MA, Armstrong PW, Buse JB, Engel SS, Garg J, Josse R, Kaufman KD, Koglin J, Korn S, Lachin JM, McGuire DK, Pencina MJ, Standl E, Stein PP, Suryawanshi S, Van de Werf F, Peterson ED, Holman RR; TECOS Study Group . Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015;373(3):232–242. [DOI] [PubMed] [Google Scholar]
- 251. Pfeffer MA, Claggett B, Diaz R, Dickstein K, Gerstein HC, Køber LV, Lawson FC, Ping L, Wei X, Lewis EF, Maggioni AP, McMurray JJ, Probstfield JL, Riddle MC, Solomon SD, Tardif JC; ELIXA Investigators . Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. N Engl J Med. 2015;373(23):2247–2257. [DOI] [PubMed] [Google Scholar]
- 252. Adler ED, Goldfinger JZ, Kalman J, Park ME, Meier DE. Palliative care in the treatment of advanced heart failure. Circulation. 2009;120(25):2597–2606. [DOI] [PubMed] [Google Scholar]
- 253. Lipska KJ, Ross JS, Miao Y, Shah ND, Lee SJ, Steinman MA. Potential overtreatment of diabetes mellitus in older adults with tight glycemic control. JAMA Intern Med. 2015;175(3):356–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254. Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Silverman MG, Zelniker TA, Kuder JF, Murphy SA, Bhatt DL, Leiter LA, McGuire DK, Wilding JP, Ruff CT, Gause-Nilsson IAM, Fredriksson M, Johansson PA, Langkilde AM, Sabatine MS. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347–357. [DOI] [PubMed] [Google Scholar]
- 255. Wu JH, Foote C, Blomster J, Toyama T, Perkovic V, Sundström J, Neal B. Effects of sodium-glucose cotransporter-2 inhibitors on cardiovascular events, death, and major safety outcomes in adults with type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2016;4(5):411–419. [DOI] [PubMed] [Google Scholar]
- 256. U.S. Food and Drug Administration FDA confirms increased risk of leg and foot amputations with the diabetes medicine canagliflozin (Invokana, Invokamet, Invokamet XR). Available at: www.fda.gov/downloads/Drugs/DrugSafety/UCM558427.pdf. Accessed 14 February 2019.
- 257. Lim MA, Townsend RR. Arterial compliance in the elderly: its effect on blood pressure measurement and cardiovascular outcomes. Clin Geriatr Med. 2009;25(2):191–205. [DOI] [PubMed] [Google Scholar]
- 258. McVeigh GE, Allen PB, Morgan DR, Hanratty CG, Silke B. Nitric oxide modulation of blood vessel tone identified by arterial waveform analysis. Clin Sci (Lond). 2001;100(4):387–393. [PubMed] [Google Scholar]
- 259. Carnethon MR, Biggs ML, Barzilay J, Kuller LH, Mozaffarian D, Mukamal K, Smith NL, Siscovick D. Diabetes and coronary heart disease as risk factors for mortality in older adults. Am J Med. 2010;123(6):556.e1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260. Mueller T, Hinterreiter F, Luft C, Poelz W, Haltmayer M, Dieplinger B. Mortality rates and mortality predictors in patients with symptomatic peripheral artery disease stratified according to age and diabetes. J Vasc Surg. 2014;59(5):1291–1299. [DOI] [PubMed] [Google Scholar]
- 261. Malone M, Lau NS, White J, Novak A, Xuan W, Iliopoulos J, Crozier J, Dickson HG. The effect of diabetes mellitus on costs and length of stay in patients with peripheral arterial disease undergoing vascular surgery. Eur J Vasc Endovasc Surg. 2014;48(4):447–451. [DOI] [PubMed] [Google Scholar]
- 262. Rawshani A, Rawshani A, Franzén S, Sattar N, Eliasson B, Svensson AM, Zethelius B, Miftaraj M, McGuire DK, Rosengren A, Gudbjörnsdottir S. Risk factors, mortality, and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2018;379(7):633–644. [DOI] [PubMed] [Google Scholar]
- 263. Gregg EW, Sattar N, Ali MK. The changing face of diabetes complications. Lancet Diabetes Endocrinol. 2016;4(6):537–547. [DOI] [PubMed] [Google Scholar]
- 264. Bouchonville M, Armamento-Villareal R, Shah K, Napoli N, Sinacore DR, Qualls C, Villareal DT. Weight loss, exercise or both and cardiometabolic risk factors in obese older adults: results of a randomized controlled trial. Int J Obes. 2014;38(3):423–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265. Lipska KJ, Krumholz H, Soones T, Lee SJ. Polypharmacy in the aging patient: a review of glycemic control in older adults with type 2 diabetes. JAMA. 2016;315(10):1034–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266. Gerstein HC, Miller ME, Ismail-Beigi F, Largay J, McDonald C, Lochnan HA, Booth GL; ACCORD Study Group . Effects of intensive glycaemic control on ischaemic heart disease: analysis of data from the randomised, controlled ACCORD trial. Lancet. 2014;384(9958):1936–1941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267. Hayward RA, Reaven PD, Wiitala WL, Bahn GD, Reda DJ, Ge L, McCarren M, Duckworth WC, Emanuele NV; VADT Investigators . Follow-up of glycemic control and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015;372(23):2197–2206. [DOI] [PubMed] [Google Scholar]
- 268. Lamanna C, Monami M, Marchionni N, Mannucci E. Effect of metformin on cardiovascular events and mortality: a meta-analysis of randomized clinical trials. Diabetes Obes Metab. 2011;13(3):221–228. [DOI] [PubMed] [Google Scholar]
- 269. Matsumoto K, Sera Y, Abe Y, Tominaga T, Yeki Y, Miyake S. Metformin attenuates progression of carotid arterial wall thickness in patients with type 2 diabetes. Diabetes Res Clin Pract. 2004;64(3):225–228. [DOI] [PubMed] [Google Scholar]
- 270. Inzucchi SE, Lipska KJ, Mayo H, Bailey CJ, McGuire DK. Metformin in patients with type 2 diabetes and kidney disease: a systematic review. JAMA. 2014;312(24):2668–2675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271. Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, Mattheus M, Devins T, Johansen OE, Woerle HJ, Broedl UC, Inzucchi SE; EMPA-REG OUTCOME Investigators . Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2117–2128. [DOI] [PubMed] [Google Scholar]
- 272. Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JFE, Nauck MA, Nissen SE, Pocock S, Poulter NR, Ravn LS, Steinberg WM, Stockner M, Zinman B, Bergenstal RM, Buse JB, Comm LS, Investigators LT; LEADER Steering Committee; LEADER Trial Investigators . Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375(4):311–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273. Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med. 2007;356(24):2457–2471. [DOI] [PubMed] [Google Scholar]
- 274. Dormandy JA, Charbonnel B, Eckland DJ, Erdmann E, Massi-Benedetti M, Moules IK, Skene AM, Tan MH, Lefèbvre PJ, Murray GD, Standl E, Wilcox RG, Wilhelmsen L, Betteridge J, Birkeland K, Golay A, Heine RJ, Korányi L, Laakso M, Mokán M, Norkus A, Pirags V, Podar T, Scheen A, Scherbaum W, Schernthaner G, Schmitz O, Skrha J, Smith U, Taton J; PROactive Investigators . Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet. 2005;366(9493):1279–1289. [DOI] [PubMed] [Google Scholar]
- 275. Gerstein HC, Bosch J, Dagenais GR, Díaz R, Jung H, Maggioni AP, Pogue J, Probstfield J, Ramachandran A, Riddle MC, Rydén LE, Yusuf S; ORIGIN Trial Investigators . Basal insulin and cardiovascular and other outcomes in dysglycemia. N Engl J Med. 2012;367(4):319–328. [DOI] [PubMed] [Google Scholar]
- 276. Jerums G, Panagiotopoulos S, Ekinci E, MacIsaac RJ. Cardiovascular outcomes with antihypertensive therapy in type 2 diabetes: an analysis of intervention trials. J Hum Hypertens. 2015;29(8):473–477. [DOI] [PubMed] [Google Scholar]
- 277. Molander L, Lövheim H, Norman T, Nordström P, Gustafson Y. Lower systolic blood pressure is associated with greater mortality in people aged 85 and older. J Am Geriatr Soc. 2008;56(10):1853–1859. [DOI] [PubMed] [Google Scholar]
- 278. Remonti LR, Dias S, Leitão CB, Kramer CK, Klassman LP, Welton NJ, Ades AE, Gross JL. Classes of antihypertensive agents and mortality in hypertensive patients with type 2 diabetes—network meta-analysis of randomized trials. J Diabetes Complications. 2016;30(6):1192–1200. [DOI] [PubMed] [Google Scholar]
- 279. Shepherd J, Blauw GJ, Murphy MB, Bollen EL, Buckley BM, Cobbe SM, Ford I, Gaw A, Hyland M, Jukema JW, Kamper AM, Macfarlane PW, Meinders AE, Norrie J, Packard CJ, Perry IJ, Stott DJ, Sweeney BJ, Twomey C, Westendorp RG; PROSPER study group. PROspective Study of Pravastatin in the Elderly at Risk . Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360(9346):1623–1630. [DOI] [PubMed] [Google Scholar]
- 280. Ginsberg HN, Elam MB, Lovato LC, Crouse JR III, Leiter LA, Linz P, Friedewald WT, Buse JB, Gerstein HC, Probstfield J, Grimm RH, Ismail-Beigi F, Bigger JT, Goff DC Jr, Cushman WC, Simons-Morton DG, Byington RP; ACCORD Study Group . Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1563–1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281. Boden WE, Probstfield JL, Anderson T, Chaitman BR, Desvignes-Nickens P, Koprowicz K, McBride R, Teo K, Weintraub W; AIM-HIGH Investigators . Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011;365(24):2255–2267. [DOI] [PubMed] [Google Scholar]
- 282. Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, Peto R, Buring J, Hennekens C, Kearney P, Meade T, Patrono C, Roncaglioni MC, Zanchetti A; Antithrombotic Trialists’ (ATT) Collaboration . Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet. 2009;373(9678):1849–1860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283. Pignone M, Alberts MJ, Colwell JA, Cushman M, Inzucchi SE, Mukherjee D, Rosenson RS, Williams CD, Wilson PW, Kirkman MS; American Diabetes Association; American Heart Association; American College of Cardiology Foundation . Aspirin for primary prevention of cardiovascular events in people with diabetes: a position statement of the American Diabetes Association, a scientific statement of the American Heart Association, and an expert consensus document of the American College of Cardiology Foundation [published corrections appear in Diabetes Care. 2010;33(9):2129–2131 and Diabetes Care. 2011;34(1):247–248]. Diabetes Care. 2010;33(6):1395–1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284. Bowman L, Mafham M, Wallendszus K, Stevens W, Buck G, Barton J, Murphy K, Aung T, Haynes R, Cox J, Murawska A, Young A, Lay M, Chen F, Sammons E, Waters E, Adler A, Bodansky J, Farmer A, McPherson R, Neil A, Simpson D, Peto R, Baigent C, Collins R, Parish S, Armitage J; ASCEND Study Collaborative Group . Effects of aspirin for primary prevention in persons with diabetes mellitus. N Engl J Med. 2018;379(16):1529–1539. [DOI] [PubMed] [Google Scholar]
- 285. Brown MM, Brown GC, Sharma S, Landy J, Bakal J. Quality of life with visual acuity loss from diabetic retinopathy and age-related macular degeneration. Arch Ophthalmol. 2002;120(4):481–484. [DOI] [PubMed] [Google Scholar]
- 286. Alcubierre N, Rubinat E, Traveset A, Martinez-Alonso M, Hernandez M, Jurjo C, Mauricio D. A prospective cross-sectional study on quality of life and treatment satisfaction in type 2 diabetic patients with retinopathy without other major late diabetic complications. Health Qual Life Outcomes. 2014;12(1):131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287. Fenwick EK, Pesudovs K, Khadka J, Dirani M, Rees G, Wong TY, Lamoureux EL. The impact of diabetic retinopathy on quality of life: qualitative findings from an item bank development project. Qual Life Res. 2012;21(10):1771–1782. [DOI] [PubMed] [Google Scholar]
- 288. Milne A, Johnson JA, Tennant M, Rudnisky C, Dryden DM. Measuring health-related quality of life for patients with diabetic retinopathy. Available at: www.ncbi.nlm.nih.gov/books/NBK248340/. Accessed 13 February 2019. [PubMed] [Google Scholar]
- 289. Gwathmey KG, Sadjadi R, Horton WB, Conaway MR, Barnett-Tapia C, Bril V, Russell JW, Shaibani A, Mauermann ML, Hehir MK, Kolb N, Guptill J, Hobson-Webb L, Gable K, Raja S, Silvestri N, Wolfe GI, Smith AG, Malik R, Traub R, Joshi A, Elliott MP, Jones S, Burns TM. Validation of a simple disease-specific, quality-of-life measure for diabetic polyneuropathy: CAPPRI. Neurology. 2018;90(23):e2034–e2041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290. Lorber D, Anderson J, Arent S, Cox DJ, Frier BM, Greene MA, Griffin J Jr, Gross G, Hathaway K, Hirsch I, Kohrman DB, Marrero DG, Songer TJ, Yatvin AL; American Diabetes Association . Diabetes and driving. Diabetes Care. 2014;37(Suppl 1):S97–S103. [DOI] [PubMed] [Google Scholar]
- 291. Diabetes Control and Complications Trial Research Group Progression of retinopathy with intensive versus conventional treatment in the Diabetes Control and Complications Trial. Ophthalmology. 1995;102(4):647–661. [DOI] [PubMed] [Google Scholar]
- 292. UK Prospective Diabetes Study (UKPDS) Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837–853. [PubMed] [Google Scholar]
- 293. Stratton IM, Kohner EM, Aldington SJ, Turner RC, Holman RR, Manley SE, Matthews DR. UKPDS 50: risk factors for incidence and progression of retinopathy in type II diabetes over 6 years from diagnosis. Diabetologia. 2001;44(2):156–163. [DOI] [PubMed] [Google Scholar]
- 294. Ismail-Beigi F, Craven T, Banerji MA, Basile J, Calles J, Cohen RM, Cuddihy R, Cushman WC, Genuth S, Grimm RH Jr, Hamilton BP, Hoogwerf B, Karl D, Katz L, Krikorian A, O’Connor P, Pop-Busui R, Schubart U, Simmons D, Taylor H, Thomas A, Weiss D, Hramiak I; ACCORD Trial Group . Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial. Lancet. 2010;376(9739):419–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295. Chew EY, Davis MD, Danis RP, Lovato JF, Perdue LH, Greven C, Genuth S, Goff DC, Leiter LA, Ismail-Beigi F, Ambrosius WT; Action to Control Cardiovascular Risk in Diabetes Eye Study Research Group . The effects of medical management on the progression of diabetic retinopathy in persons with type 2 diabetes: the Action to Control Cardiovascular Risk in Diabetes (ACCORD) Eye Study. Ophthalmology. 2014;121(12):2443–2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296. Aiello LP; DCCT/EDIC Research Group . Diabetic retinopathy and other ocular findings in the Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications Study. Diabetes Care. 2014;37(1):17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297. Klein R, Knudtson MD, Lee KE, Gangnon R, Klein BE. The Wisconsin Epidemiologic Study of Diabetic Retinopathy XXII: the twenty-five-year progression of retinopathy in persons with type 1 diabetes. Ophthalmology. 2008;115(11):1859–1868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298. Estacio RO, McFarling E, Biggerstaff S, Jeffers BW, Johnson D, Schrier RW. Overt albuminuria predicts diabetic retinopathy in Hispanics with NIDDM. Am J Kidney Dis. 1998;31(6):947–953. [DOI] [PubMed] [Google Scholar]
- 299. Antonetti DA, Klein R, Gardner TW. Diabetic retinopathy. N Engl J Med. 2012;366(13):1227–1239. [DOI] [PubMed] [Google Scholar]
- 300. American Diabetes Association. 11 Microvascular complications and foot care: standards of medical care in diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S124–S138. [DOI] [PubMed] [Google Scholar]
- 301. Solomon SD, Chew E, Duh EJ, Sobrin L, Sun JK, VanderBeek BL, Wykoff CC, Gardner TW. Diabetic retinopathy: a position statement by the American Diabetes Association [published correction appears in Diabetes Care 2017;40(9):1285]. Diabetes Care. 2017;40(3):412–418.28223445 [Google Scholar]
- 302. Klein R, Klein BE. Are individuals with diabetes seeing better?: a long-term epidemiological perspective. Diabetes. 2010;59(8):1853–1860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303. Sloan FA, Grossman DS, Lee PP. Effects of receipt of guideline-recommended care on onset of diabetic retinopathy and its progression. Ophthalmology. 2009;116(8):1515–1521.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304. Sloan FA, Belsky D, Ruiz D Jr, Lee P. Changes in incidence of diabetes mellitus-related eye disease among US elderly persons, 1994–2005. Arch Ophthalmol. 2008;126(11):1548–1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305. Matthews DR, Stratton IM, Aldington SJ, Holman RR, Kohner EM; UK Prospective Diabetes Study Group . Risks of progression of retinopathy and vision loss related to tight blood pressure control in type 2 diabetes mellitus: UKPDS 69. Arch Ophthalmol. 2004;122(11):1631–1640. [DOI] [PubMed] [Google Scholar]
- 306. Do DV, Wang X, Vedula SS, Marrone M, Sleilati G, Hawkins BS, Frank RN. Blood pressure control for diabetic retinopathy. Cochrane Database Syst Rev. 2015;1:CD006127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307. Chaturvedi N, Sjolie AK, Stephenson JM, Abrahamian H, Keipes M, Castellarin A, Rogulja-Pepeonik Z, Fuller JH; The EUCLID Study Group . Effect of lisinopril on progression of retinopathy in normotensive people with type 1 diabetes. Lancet. 1998;351(9095):28–31. [DOI] [PubMed] [Google Scholar]
- 308. Chaturvedi N, Porta M, Klein R, Orchard T, Fuller J, Parving HH, Bilous R, Sjølie AK; DIRECT Programme Study Group . Effect of candesartan on prevention (DIRECT-Prevent 1) and progression (DIRECT-Protect 1) of retinopathy in type 1 diabetes: randomised, placebo-controlled trials. Lancet. 2008;372(9647):1394–1402. [DOI] [PubMed] [Google Scholar]
- 309. Sjølie AK, Klein R, Porta M, Orchard T, Fuller J, Parving HH, Bilous R, Chaturvedi N; DIRECT Programme Study Group . Effect of candesartan on progression and regression of retinopathy in type 2 diabetes (DIRECT-Protect 2): a randomised placebo-controlled trial. Lancet. 2008;372(9647):1385–1393. [DOI] [PubMed] [Google Scholar]
- 310. Mauer M, Zinman B, Gardiner R, Suissa S, Sinaiko A, Strand T, Drummond K, Donnelly S, Goodyer P, Gubler MC, Klein R. Renal and retinal effects of enalapril and losartan in type 1 diabetes. N Engl J Med. 2009;361(1):40–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311. Wright AD, Dodson PM. Medical management of diabetic retinopathy: fenofibrate and ACCORD Eye studies. Eye (Lond). 2011;25(7):843–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312. Noonan JE, Jenkins AJ, Ma JX, Keech AC, Wang JJ, Lamoureux EL. An update on the molecular actions of fenofibrate and its clinical effects on diabetic retinopathy and other microvascular end points in patients with diabetes. Diabetes. 2013;62(12):3968–3975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 313. Bressler NM, Beck RW, Ferris FL III. Panretinal photocoagulation for proliferative diabetic retinopathy. N Engl J Med. 2011;365(16):1520–1526. [DOI] [PubMed] [Google Scholar]
- 314. Keenan TD, Johnston RL, Donachie PH, Sparrow JM, Stratton IM, Scanlon P. United Kingdom National Ophthalmology Database Study: Diabetic Retinopathy; Report 1: prevalence of centre-involving diabetic macular oedema and other grades of maculopathy and retinopathy in hospital eye services. Eye (Lond). 2013;27(12):1397–1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315. Martín-Merino E, Fortuny J, Rivero-Ferrer E, García-Rodríguez LA. Incidence of retinal complications in a cohort of newly diagnosed diabetic patients. PLoS One. 2014;9(6):e100283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316. Varma R, Bressler NM, Doan QV, Gleeson M, Danese M, Bower JK, Selvin E, Dolan C, Fine J, Colman S, Turpcu A. Prevalence of and risk factors for diabetic macular edema in the United States. JAMA Ophthalmol. 2014;132(11):1334–1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317. Elman MJ, Aiello LP, Beck RW, Bressler NM, Bressler SB, Edwards AR, Ferris FL 3rd, Friedman SM, Glassman AR, Miller KM, Scott IU, Stockdale CR, Sun JK; Diabetic Retinopathy Clinical Research Network . Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2010;117(6):1064–1077.e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318. Mitchell P, Bandello F, Schmidt-Erfurth U, Lang GE, Massin P, Schlingemann RO, Sutter F, Simader C, Burian G, Gerstner O, Weichselberger A; RESTORE Study Group . The RESTORE study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology. 2011;118(4):615–625. [DOI] [PubMed] [Google Scholar]
- 319. Elman MJ, Bressler NM, Qin H, Beck RW, Ferris FL III, Friedman SM, Glassman AR, Scott IU, Stockdale CR, Sun JK; Diabetic Retinopathy Clinical Research Network . Expanded 2-year follow-up of ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology. 2011;118(4):609–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320. Nguyen QD, Brown DM, Marcus DM, Boyer DS, Patel S, Feiner L, Gibson A, Sy J, Rundle AC, Hopkins JJ, Rubio RG, Ehrlich JS; RISE and RIDE Research Group . Ranibizumab for diabetic macular edema: results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology. 2012;119(4):789–801. [DOI] [PubMed] [Google Scholar]
- 321. Dugel PU, Layton A, Varma RB. Diabetic macular edema diagnosis and treatment in the real world: an analysis of medicare claims data (2008 to 2010). Ophthalmic Surg Lasers Imaging Retina. 2016;47(3):258–267. [DOI] [PubMed] [Google Scholar]
- 322. Stein JD, Newman-Casey PA, Kim DD, Nwanyanwu KH, Johnson MW, Hutton DW. Cost-effectiveness of various interventions for newly diagnosed diabetic macular edema. Ophthalmology. 2013;120(9):1835–1842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323. Wells JA, Glassman AR, Ayala AR, Jampol LM, Aiello LP, Antoszyk AN, Arnold-Bush B, Baker CW, Bressler NM, Browning DJ, Elman MJ, Ferris FL, Friedman SM, Melia M, Pieramici DJ, Sun JK, Beck RW; Diabetic Retinopathy Clinical Research Network . Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med. 2015;372(13):1193–1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324. Martin DF, Maguire MG. Treatment choice for diabetic macular edema. N Engl J Med. 2015;372(13):1260–1261. [DOI] [PubMed] [Google Scholar]
- 325. Hahn P, Acquah K, Cousins SW, Lee PP, Sloan FA. Ten-year incidence of age-related macular degeneration according to diabetic retinopathy classification among medicare beneficiaries. Retina. 2013;33(5):911–919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326. Zhao D, Cho J, Kim MH, Friedman DS, Guallar E. Diabetes, fasting glucose, and the risk of glaucoma: a meta-analysis. Ophthalmology. 2015;122(1):72–78. [DOI] [PubMed] [Google Scholar]
- 327. Li L, Wan XH, Zhao GH. Meta-analysis of the risk of cataract in type 2 diabetes. BMC Ophthalmol. 2014;14(1):94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328. Adler AI, Boyko EJ, Ahroni JH, Stensel V, Forsberg RC, Smith DG. Risk factors for diabetic peripheral sensory neuropathy. Results of the Seattle Prospective Diabetic Foot Study. Diabetes Care. 1997;20(7):1162–1167. [DOI] [PubMed] [Google Scholar]
- 329. Dyck PJ, Davies JL, Wilson DM, Service FJ, Melton LJ III, O’Brien PC. Risk factors for severity of diabetic polyneuropathy: intensive longitudinal assessment of the Rochester Diabetic Neuropathy Study cohort. Diabetes Care. 1999;22(9):1479–1486. [DOI] [PubMed] [Google Scholar]
- 330. Hyland KA, Greiner MA, Qualls LG, Califf RM, Hernandez AF, Curtis LH. Trends in the care and outcomes of medicare beneficiaries with type 2 diabetes, 2002–2011. Endocr Pract. 2016;22(8):920–934. [DOI] [PubMed] [Google Scholar]
- 331. Popescu S, Timar B, Baderca F, Simu M, Diaconu L, Velea I, Timar R. Age as an independent factor for the development of neuropathy in diabetic patients. Clin Interv Aging. 2016;11:313–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332. Van Acker K, Bouhassira D, De Bacquer D, Weiss S, Matthys K, Raemen H, Mathieu C, Colin IM. Prevalence and impact on quality of life of peripheral neuropathy with or without neuropathic pain in type 1 and type 2 diabetic patients attending hospital outpatients clinics. Diabetes Metab. 2009;35(3):206–213. [DOI] [PubMed] [Google Scholar]
- 333. Dyck PJ, Kratz KM, Karnes JL, Litchy WJ, Klein R, Pach JM, Wilson DM, O’Brien PC, Melton LJ III, Service FJ. The prevalence by staged severity of various types of diabetic neuropathy, retinopathy, and nephropathy in a population-based cohort: the Rochester Diabetic Neuropathy Study. Neurology. 1993;43(4):817–824. [DOI] [PubMed] [Google Scholar]
- 334. Thomas PK. Classification, differential diagnosis, and staging of diabetic peripheral neuropathy. Diabetes. 1997;46(Suppl 2):S54–S57. [DOI] [PubMed] [Google Scholar]
- 335. Vinik AI, Ziegler D. Diabetic cardiovascular autonomic neuropathy. Circulation. 2007;115(3):387–397. [DOI] [PubMed] [Google Scholar]
- 336. Tesfaye S, Boulton AJ, Dyck PJ, Freeman R, Horowitz M, Kempler P, Lauria G, Malik RA, Spallone V, Vinik A, Bernardi L, Valensi P; Toronto Diabetic Neuropathy Expert Group . Diabetic neuropathies: update on definitions, diagnostic criteria, estimation of severity, and treatments [published correction appears in Diabetes Care. 2010;33(12):2725]. Diabetes Care. 2010;33(10):2285–2293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337. Tesfaye S, Vileikyte L, Rayman G, Sindrup SH, Perkins BA, Baconja M, Vinik AI, Boulton AJ; Toronto Expert Panel on Diabetic Neuropathy . Painful diabetic peripheral neuropathy: consensus recommendations on diagnosis, assessment and management. Diabetes Metab Res Rev. 2011;27(7):629–638. [DOI] [PubMed] [Google Scholar]
- 338. Nicodemus KK, Folsom AR; Iowa Women’s Health Study . Type 1 and type 2 diabetes and incident hip fractures in postmenopausal women. Diabetes Care. 2001;24(7):1192–1197. [DOI] [PubMed] [Google Scholar]
- 339. Janghorbani M, Feskanich D, Willett WC, Hu F. Prospective study of diabetes and risk of hip fracture: the Nurses’ Health Study. Diabetes Care. 2006;29(7):1573–1578. [DOI] [PubMed] [Google Scholar]
- 340. Schwartz AV, Hillier TA, Sellmeyer DE, Resnick HE, Gregg E, Ensrud KE, Schreiner PJ, Margolis KL, Cauley JA, Nevitt MC, Black DM, Cummings SR. Older women with diabetes have a higher risk of falls: a prospective study. Diabetes Care. 2002;25(10):1749–1754. [DOI] [PubMed] [Google Scholar]
- 341. Maurer MS, Burcham J, Cheng H. Diabetes mellitus is associated with an increased risk of falls in elderly residents of a long-term care facility. J Gerontol A Biol Sci Med Sci. 2005;60(9):1157–1162. [DOI] [PubMed] [Google Scholar]
- 342. Mayne D, Stout NR, Aspray TJ. Diabetes, falls and fractures. Age Ageing. 2010;39(5):522–525. [DOI] [PubMed] [Google Scholar]
- 343. Pijpers E, Ferreira I, de Jongh RT, Deeg DJ, Lips P, Stehouwer CD, Nieuwenhuijzen Kruseman AC. Older individuals with diabetes have an increased risk of recurrent falls: analysis of potential mediating factors: the Longitudinal Ageing Study Amsterdam. Age Ageing. 2012;41(3):358–365. [DOI] [PubMed] [Google Scholar]
- 344. Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148–157. [DOI] [PubMed] [Google Scholar]
- 345. Nelson JM, Dufraux K, Cook PF. The relationship between glycemic control and falls in older adults. J Am Geriatr Soc. 2007;55(12):2041–2044. [DOI] [PubMed] [Google Scholar]
- 346. Schwartz AV, Vittinghoff E, Sellmeyer DE, Feingold KR, de Rekeneire N, Strotmeyer ES, Shorr RI, Vinik AI, Odden MC, Park SW, Faulkner KA, Harris TB; Health, Aging, and Body Composition Study . Diabetes-related complications, glycemic control, and falls in older adults [published correction appears in Diabetes Care. 2008;31(5):1089]. Diabetes Care. 2008;31(3):391–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347. Berlie HD, Garwood CL. Diabetes medications related to an increased risk of falls and fall-related morbidity in the elderly. Ann Pharmacother. 2010;44(4):712–717. [DOI] [PubMed] [Google Scholar]
- 348. Schwartz AV, Margolis KL, Sellmeyer DE, Vittinghoff E, Ambrosius WT, Bonds DE, Josse RG, Schnall AM, Simmons DL, Hue TF, Palermo L, Hamilton BP, Green JB, Atkinson HH, O’Connor PJ, Force RW, Bauer DC. Intensive glycemic control is not associated with fractures or falls in the ACCORD randomized trial. Diabetes Care. 2012;35(7):1525–1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349. Taylor SI, Blau JE, Rother KI. Possible adverse effects of SGLT2 inhibitors on bone. Lancet Diabetes Endocrinol. 2015;3(1):8–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350. Cohen K, Shinkazh N, Frank J, Israel I, Fellner C. Pharmacological treatment of diabetic peripheral neuropathy. P&T. 2015;40(6):372–388. [PMC free article] [PubMed] [Google Scholar]
- 351. Vinik AI, Strotmeyer ES, Nakave AA, Patel CV. Diabetic neuropathy in older adults. Clin Geriatr Med. 2008;24(3):407–435, v. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352. Crews RT, Yalla SV, Fleischer AE, Wu SC. A growing troubling triad: diabetes, aging, and falls. J Aging Res. 2013;2013:342650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353. Vinik AI. Clinical practice. Diabetic sensory and motor neuropathy. N Engl J Med. 2016;374(15):1455–1464. [DOI] [PubMed] [Google Scholar]
- 354. Huang ES, Karter AJ, Danielson KK, Warton EM, Ahmed AT. The association between the number of prescription medications and incident falls in a multi-ethnic population of adult type-2 diabetes patients: the diabetes and aging study. J Gen Intern Med. 2010;25(2):141–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355. Menz HB, Lord SR, St George R, Fitzpatrick RC. Walking stability and sensorimotor function in older people with diabetic peripheral neuropathy. Arch Phys Med Rehabil. 2004;85(2):245–252. [DOI] [PubMed] [Google Scholar]
- 356. Patel S, Hyer S, Tweed K, Kerry S, Allan K, Rodin A, Barron J. Risk factors for fractures and falls in older women with type 2 diabetes mellitus. Calcif Tissue Int. 2008;82(2):87–91. [DOI] [PubMed] [Google Scholar]
- 357. MacGilchrist C, Paul L, Ellis BM, Howe TE, Kennon B, Godwin J. Lower-limb risk factors for falls in people with diabetes mellitus. Diabet Med. 2010;27(2):162–168. [DOI] [PubMed] [Google Scholar]
- 358. Lee RH, Sloane R, Pieper C, Lyles KW, Adler RA, Van Houtven C, LaFleur J, Colón-Emeric C. Clinical fractures among older men with diabetes are mediated by diabetic complications. J Clin Endocrinol Metab. 2018;103(1):281–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 359. Cavanagh PR, Derr JA, Ulbrecht JS, Maser RE, Orchard TJ. Problems with gait and posture in neuropathic patients with insulin-dependent diabetes mellitus. Diabet Med. 1992;9(5):469–474. [DOI] [PubMed] [Google Scholar]
- 360. Corriveau H, Prince F, Hébert R, Raîche M, Tessier D, Maheux P, Ardilouze JL. Evaluation of postural stability in elderly with diabetic neuropathy. Diabetes Care. 2000;23(8):1187–1191. [DOI] [PubMed] [Google Scholar]
- 361. Allet L, Armand S, de Bie RA, Golay A, Pataky Z, Aminian K, de Bruin ED. Clinical factors associated with gait alterations in diabetic patients. Diabet Med. 2009;26(10):1003–1009. [DOI] [PubMed] [Google Scholar]
- 362. Brown SJ, Handsaker JC, Bowling FL, Boulton AJ, Reeves ND. Diabetic peripheral neuropathy compromises balance during daily activities. Diabetes Care. 2015;38(6):1116–1122. [DOI] [PubMed] [Google Scholar]
- 363. Allet L, Armand S, de Bie RA, Golay A, Monnin D, Aminian K, Staal JB, de Bruin ED. The gait and balance of patients with diabetes can be improved: a randomised controlled trial. Diabetologia. 2010;53(3):458–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 364. Morrison S, Colberg SR, Mariano M, Parson HK, Vinik AI. Balance training reduces falls risk in older individuals with type 2 diabetes. Diabetes Care. 2010;33(4):748–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365. Salsabili H, Bahrpeyma F, Forogh B, Rajabali S. Dynamic stability training improves standing balance control in neuropathic patients with type 2 diabetes. J Rehabil Res Dev. 2011;48(7):775–786. [DOI] [PubMed] [Google Scholar]
- 366. Gu Y, Dennis SM. Are falls prevention programs effective at reducing the risk factors for falls in people with type-2 diabetes mellitus and peripheral neuropathy: a systematic review with narrative synthesis. J Diabetes Complications. 2017;31(2):504–516. [DOI] [PubMed] [Google Scholar]
- 367. Holman KH, Henke PK, Dimick JB, Birkmeyer JD. Racial disparities in the use of revascularization before leg amputation in medicare patients. J Vasc Surg. 2011;54(2):420–426.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368. Johannesson A, Larsson GU, Ramstrand N, Turkiewicz A, Wiréhn AB, Atroshi I. Incidence of lower-limb amputation in the diabetic and nondiabetic general population: a 10-year population-based cohort study of initial unilateral and contralateral amputations and reamputations. Diabetes Care. 2009;32(2):275–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369. Hong MS, Beck AW, Nelson PR. Emerging national trends in the management and outcomes of lower extremity peripheral arterial disease. Ann Vasc Surg. 2011;25(1):44–54. [DOI] [PubMed] [Google Scholar]
- 370. Margolis DJ, Hoffstad O, Nafash J, Leonard CE, Freeman CP, Hennessy S, Wiebe DJ. Location, location, location: geographic clustering of lower-extremity amputation among Medicare beneficiaries with diabetes. Diabetes Care. 2011;34(11):2363–2367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371. Huang ES, Laiteerapong N, Liu JY, John PM, Moffet HH, Karter AJ. Rates of complications and mortality in older patients with diabetes mellitus: the diabetes and aging study. JAMA Intern Med. 2014;174(2):251–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372. Boyko EJ, Ahroni JH, Stensel V, Forsberg RC, Davignon DR, Smith DG. A prospective study of risk factors for diabetic foot ulcer. The Seattle Diabetic Foot Study. Diabetes Care. 1999;22(7):1036–1042. [DOI] [PubMed] [Google Scholar]
- 373. Adler AI, Boyko EJ, Ahroni JH, Smith DG. Lower-extremity amputation in diabetes. The independent effects of peripheral vascular disease, sensory neuropathy, and foot ulcers. Diabetes Care. 1999;22(7):1029–1035. [DOI] [PubMed] [Google Scholar]
- 374. Katoulis EC, Ebdon-Parry M, Lanshammar H, Vileikyte L, Kulkarni J, Boulton AJ. Gait abnormalities in diabetic neuropathy. Diabetes Care. 1997;20(12):1904–1907. [DOI] [PubMed] [Google Scholar]
- 375. Margolis DJ, Hofstad O, Feldman HI. Association between renal failure and foot ulcer or lower-extremity amputation in patients with diabetes. Diabetes Care. 2008;31(7):1331–1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376. Skoutas D, Papanas N, Georgiadis GS, Zervas V, Manes C, Maltezos E, Lazarides MK. Risk factors for ipsilateral reamputation in patients with diabetic foot lesions. Int J Low Extrem Wounds. 2009;8(2):69–74. [DOI] [PubMed] [Google Scholar]
- 377. Lipsky BA, Weigelt JA, Sun X, Johannes RS, Derby KG, Tabak YP. Developing and validating a risk score for lower-extremity amputation in patients hospitalized for a diabetic foot infection. Diabetes Care. 2011;34(8):1695–1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378. Zhao W, Katzmarzyk PT, Horswell R, Wang Y, Johnson J, Heymsfield SB, Cefalu WT, Ryan DH, Hu G. HbA1c and lower-extremity amputation risk in low-income patients with diabetes. Diabetes Care. 2013;36(11):3591–3598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379. Boyko EJ, Seelig AD, Ahroni JH. Limb- and person-level risk factors for lower-limb amputation in the prospective seattle diabetic foot study. Diabetes Care. 2018;41(4):891–898. [DOI] [PubMed] [Google Scholar]
- 380. Sohn MW, Stuck RM, Pinzur M, Lee TA, Budiman-Mak E. Lower-extremity amputation risk after charcot arthropathy and diabetic foot ulcer. Diabetes Care. 2010;33(1):98–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381. Rice JB, Desai U, Cummings AK, Birnbaum HG, Skornicki M, Parsons NB. Burden of diabetic foot ulcers for medicare and private insurers [published correction appears in Diabetes Care. 2014;37(9):2660]. Diabetes Care. 2014;37(3):651–658. [DOI] [PubMed] [Google Scholar]
- 382. Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017;376(24):2367–2375. [DOI] [PubMed] [Google Scholar]
- 383. Skrepnek GH, Mills JL Sr, Lavery LA, Armstrong DG. Health care service and outcomes among an estimated 6.7 million ambulatory care diabetic foot cases in the U.S. Diabetes Care. 2017;40(7):936–942. [DOI] [PubMed] [Google Scholar]
- 384. Patout CA Jr, Birke JA, Horswell R, Williams D, Cerise FP. Effectiveness of a comprehensive diabetes lower-extremity amputation prevention program in a predominantly low-income African-American population. Diabetes Care. 2000;23(9):1339–1342. [DOI] [PubMed] [Google Scholar]
- 385. Lavery LA, Wunderlich RP, Tredwell JL. Disease management for the diabetic foot: effectiveness of a diabetic foot prevention program to reduce amputations and hospitalizations. Diabetes Res Clin Pract. 2005;70(1):31–37. [DOI] [PubMed] [Google Scholar]
- 386. Buckley CM, Perry IJ, Bradley CP, Kearney PM. Does contact with a podiatrist prevent the occurrence of a lower extremity amputation in people with diabetes? A systematic review and meta-analysis. BMJ Open. 2013;3(5):e002331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387. Bonner T, Foster M, Spears-Lanoix E. Type 2 diabetes–related foot care knowledge and foot self-care practice interventions in the United States: a systematic review of the literature. Diabet Foot Ankle. 2016;7(1):29758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388. Wukich DK, Armstrong DG, Attinger CE, Boulton AJ, Burns PR, Frykberg RG, Hellman R, Kim PJ, Lipsky BA, Pile JC, Pinzur MS, Siminerio L. Inpatient management of diabetic foot disorders: a clinical guide. Diabetes Care. 2013;36(9):2862–2871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389. Humphries MD, Brunson A, Hedayati N, Romano P, Melnkow J. Amputation risk in patients with diabetes mellitus and peripheral artery disease using statewide data. Ann Vasc Surg. 2016;30:123–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 390. Tseng CL, Rajan M, Miller DR, Lafrance JP, Pogach L. Trends in initial lower extremity amputation rates among Veterans Health Administration health care system users from 2000 to 2004. Diabetes Care. 2011;34(5):1157–1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 391. Gregg EW, Li Y, Wang J, Burrows NR, Ali MK, Rolka D, Williams DE, Geiss L. Changes in diabetes-related complications in the United States, 1990–2010. N Engl J Med. 2014;370(16):1514–1523. [DOI] [PubMed] [Google Scholar]
- 392. Yashkin AP, Picone G, Sloan F. Causes of the change in the rates of mortality and severe complications of diabetes mellitus: 1992–2012. Med Care. 2015;53(3):268–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393. Colberg SR, Sigal RJ, Yardley JE, Riddell MC, Dunstan DW, Dempsey PC, Horton ES, Castorino K, Tate DF. Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2016;39(11):2065–2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 394. Crews RT, Shen BJ, Campbell L, Lamont PJ, Boulton AJ, Peyrot M, Kirsner RS, Vileikyte L. Role and determinants of adherence to off-loading in diabetic foot ulcer healing: a prospective investigation. Diabetes Care. 2016;39(8):1371–1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395. van Netten JJ, Price PE, Lavery LA, Monteiro-Soares M, Rasmussen A, Jubiz Y, Bus SA; International Working Group on the Diabetic Foot . Prevention of foot ulcers in the at-risk patient with diabetes: a systematic review. Diabetes Metab Res Rev. 2016;32(Suppl 1):84–98. [DOI] [PubMed] [Google Scholar]
- 396. Hoffstad O, Mitra N, Walsh J, Margolis DJ. Diabetes, lower-extremity amputation, and death. Diabetes Care. 2015;38(10):1852–1857. [DOI] [PubMed] [Google Scholar]
- 397. Vogel TR, Petroski GF, Kruse RL. Impact of amputation level and comorbidities on functional status of nursing home residents after lower extremity amputation. J Vasc Surg. 2014;59(5):1323–1330.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398. Moulik PK, Mtonga R, Gill GV. Amputation and mortality in new-onset diabetic foot ulcers stratified by etiology. Diabetes Care. 2003;26(2):491–494. [DOI] [PubMed] [Google Scholar]
- 399. Apelqvist J, Elgzyri T, Larsson J, Londahl M, Nyberg P, Thorne J. Factors related to outcome of neuroischemic/ischemic foot ulcer in diabetic patients. J Vasc Surg. 2011;53(6):1582–1588.e2. [DOI] [PubMed] [Google Scholar]
- 400. Brosi P, Dick F, Do DD, Schmidli J, Baumgartner I, Diehm N. Revascularization for chronic critical lower limb ischemia in octogenarians is worthwhile. J Vasc Surg. 2007;46(6):1198–1207. [DOI] [PubMed] [Google Scholar]
- 401. Dosluoglu HH, Lall P, Cherr GS, Harris LM, Dryjski ML. Superior limb salvage with endovascular therapy in octogenarians with critical limb ischemia. J Vasc Surg. 2009;50(2):305–316.e2. [DOI] [PubMed] [Google Scholar]
- 402. Lindeman RD. Changes in renal function with aging. Implications for treatment. Drugs Aging. 1992;2(5):423–431. [DOI] [PubMed] [Google Scholar]
- 403. de Boer IH, Rue TC, Hall YN, Heagerty PJ, Weiss NS, Himmelfarb J. Temporal trends in the prevalence of diabetic kidney disease in the United States. JAMA. 2011;305(24):2532–2539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 404. Hahr AJ, Molitch ME. Management of diabetes mellitus in patients with chronic kidney disease. Clin Diabetes Endocrinol. 2015;1(1):2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405. Moen MF, Zhan M, Hsu VD, Walker LD, Einhorn LM, Seliger SL, Fink JC. Frequency of hypoglycemia and its significance in chronic kidney disease. Clin J Am Soc Nephrol. 2009;4(6):1121–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 406. Miller ME, Bonds DE, Gerstein HC, Seaquist ER, Bergenstal RM, Calles-Escandon J, Childress RD, Craven TE, Cuddihy RM, Dailey G, Feinglos MN, Ismail-Beigi F, Largay JF, O’Connor PJ, Paul T, Savage PJ, Schubart UK, Sood A, Genuth S; ACCORD Investigators . The effects of baseline characteristics, glycaemia treatment approach, and glycated haemoglobin concentration on the risk of severe hypoglycaemia: post hoc epidemiological analysis of the ACCORD study. BMJ. 2010;340:b5444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 407. Kramer HJ, Nguyen QD, Curhan G, Hsu CY. Renal insufficiency in the absence of albuminuria and retinopathy among adults with type 2 diabetes mellitus. JAMA. 2003;289(24):3273–3277. [DOI] [PubMed] [Google Scholar]
- 408. Bakris GL, Molitch M. Microalbuminuria as a risk predictor in diabetes: the continuing saga. Diabetes Care. 2014;37(3):867–875. [DOI] [PubMed] [Google Scholar]
- 409. Rabkin R, Ryan MP, Duckworth WC. The renal metabolism of insulin. Diabetologia. 1984;27(3):351–357. [DOI] [PubMed] [Google Scholar]
- 410. Bakris GL, Molitch ME. Should restrictions be relaxed for metformin use in chronic kidney disease? Yes, they should be relaxed! What’s the fuss? Diabetes Care. 2016;39(7):1287–1291. [DOI] [PubMed] [Google Scholar]
- 411. U.S. Food and Drug Administration FDA drug safety communication: FDA revises warnings regarding use of the diabetes medicine metformin in certain patients with reduced kidney function. Available at: www.fda.gov/Drugs/DrugSafety/ucm493244.htm. Accessed 12 February 2019.
- 412. Holstein A, Beil W. Oral antidiabetic drug metabolism: pharmacogenomics and drug interactions. Expert Opin Drug Metab Toxicol. 2009;5(3):225–241. [DOI] [PubMed] [Google Scholar]
- 413. Balant L, Zahnd G, Gorgia A, Schwarz R, Fabre J. Pharmacokinetics of glipizide in man: influence of renal insufficiency. Diabetologia. 1973;9(S1):331–338. [DOI] [PubMed] [Google Scholar]
- 414. Arjona Ferreira JC, Marre M, Barzilai N, Guo H, Golm GT, Sisk CM, Kaufman KD, Goldstein BJ. Efficacy and safety of sitagliptin versus glipizide in patients with type 2 diabetes and moderate-to-severe chronic renal insufficiency. Diabetes Care. 2013;36(5):1067–1073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 415. Inoue T, Shibahara N, Miyagawa K, Itahana R, Izumi M, Nakanishi T, Takamitsu Y. Pharmacokinetics of nateglinide and its metabolites in subjects with type 2 diabetes mellitus and renal failure. Clin Nephrol. 2003;60(2):90–95. [DOI] [PubMed] [Google Scholar]
- 416. Hasslacher C; Multinational Repaglinide Renal Study Group . Safety and efficacy of repaglinide in type 2 diabetic patients with and without impaired renal function. Diabetes Care. 2003;26(3):886–891. [DOI] [PubMed] [Google Scholar]
- 417. Budde K, Neumayer HH, Fritsche L, Sulowicz W, Stompôr T, Eckland D. The pharmacokinetics of pioglitazone in patients with impaired renal function. Br J Clin Pharmacol. 2003;55(4):368–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 418. Chapelsky MC, Thompson-Culkin K, Miller AK, Sack M, Blum R, Freed MI. Pharmacokinetics of rosiglitazone in patients with varying degrees of renal insufficiency. J Clin Pharmacol. 2003;43(3):252–259. [DOI] [PubMed] [Google Scholar]
- 419. Reuser AJ, Wisselaar HA. An evaluation of the potential side-effects of α-glucosidase inhibitors used for the management of diabetes mellitus. Eur J Clin Invest. 1994;24(Suppl 3):19–24. [DOI] [PubMed] [Google Scholar]
- 420. Giorda CB, Nada E, Tartaglino B. Pharmacokinetics, safety, and efficacy of DPP-4 inhibitors and GLP-1 receptor agonists in patients with type 2 diabetes mellitus and renal or hepatic impairment. A systematic review of the literature [published correction appears in Endocrine. 2014;46(3):420–422]. Endocrine. 2014;46(3):406–419. [DOI] [PubMed] [Google Scholar]
- 421. Yamout H, Perkovic V, Davies M, Woo V, de Zeeuw D, Mayer C, Vijapurkar U, Kline I, Usiskin K, Meininger G, Bakris G. Efficacy and safety of canagliflozin in patients with type 2 diabetes and stage 3 nephropathy. Am J Nephrol. 2014;40(1):64–74. [DOI] [PubMed] [Google Scholar]
- 422. Linnebjerg H, Kothare PA, Park S, Mace K, Reddy S, Mitchell M, Lins R. Effect of renal impairment on the pharmacokinetics of exenatide. Br J Clin Pharmacol. 2007;64(3):317–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423. Johansen OE, Whitfield R. Exenatide may aggravate moderate diabetic renal impairment: a case report. Br J Clin Pharmacol. 2008;66(4):568–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 424. Davidson JA, Brett J, Falahati A, Scott D Mild renal impairment and the efficacy and safety of liraglutide. Endocr Pract 2011;17(3):345–355. [DOI] [PubMed] [Google Scholar]
- 425. Miller RG, Secrest AM, Sharma RK, Songer TJ, Orchard TJ. Improvements in the life expectancy of type 1 diabetes: the Pittsburgh Epidemiology of Diabetes Complications Study cohort. Diabetes. 2012;61(11):2987–2992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 426. Foster NC, Beck RW, Miller KM, Clements MA, Rickels MR, DiMeglio LA, Maahs DM, Tamborlane WV, Bergetstal R, Smith E, Olson BA, Garg SK. State of type 1 diabetes management and outcomes from teh T1D Exchange 2016–2018. Diabetes Technol Therap. 2019:21:66–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 427. Weinstock RS, Xing D, Maahs DM, Michels A, Rickels MR, Peters AL, Bergenstal RM, Harris B, Dubose SN, Miller KM, Beck RW; T1D Exchange Clinic Network . Severe hypoglycemia and diabetic ketoacidosis in adults with type 1 diabetes: results from the T1D Exchange Clinic registry. J Clin Endocrinol Metab. 2013;98:3411–3419. [DOI] [PubMed] [Google Scholar]
- 428. Duinkerken E, Brands AM, van den Berg E, Henselmans JM, Hoogma RP, Biessels GJ; Utrecht Diabetic Encephalopathy Study Group . Cognition in older patients with type 1 diabetes mellitus: a longitudinal study. J Am Geriatr Soc. 2011;59(3):563–565. [DOI] [PubMed] [Google Scholar]
- 429. Tuttle KR, Bakris GL, Bilous RW, Chiang JL, de Boer IH, Goldstein-Fuchs J, Hirsch IB, Kalantar-Zadeh K, Narva AS, Navaneethan SD, Neumiller JJ, Patel UD, Ratner RE, Whaley-Connell AT, Molitch ME. Diabetic kidney disease: a report from an ADA Consensus Conference. Diabetes Care. 2014;37(10):2864–2883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 430. Miller KM, Foster NC, Beck RW, Bergenstal RM, DuBose SN, DiMeglio LA, Maahs DM, Tamborlane WV; T1D Exchange Clinic Network . Current state of type 1 diabetes treatment in the U.S.: updated data from the T1D Exchange clinic registry. Diabetes Care. 2015;38(6):971–978. [DOI] [PubMed] [Google Scholar]
- 431. Orchard TJ, Nathan DM, Zinman B, Cleary P, Brillon D, Backlund JY, Lachin JM; Writing Group for the DCCT/EDIC Research Group . Association between 7 years of intensive treatment of type 1 diabetes and long-term mortality. JAMA. 2015;313(1):45–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 432. Newton CA, Adeel S, Sadeghi-Yarandi S, Powell W, Migdal A, Smiley D, Olson D, Chambria R, Pinzon I, Toyoshima M, Nagamia Z, Peng L, Johnson T, Umpierrez GE. Prevalence, quality of care, and complications in long term care residents with diabetes: a multicenter observational study. J Am Med Dir Assoc. 2013;14(11):842–846. [DOI] [PubMed] [Google Scholar]
- 433. Dybicz SB, Thompson S, Molotsky S, Stuart B. Prevalence of diabetes and the burden of comorbid conditions among elderly nursing home residents. Am J Geriatr Pharmacother. 2011;9(4):212–223. [DOI] [PubMed] [Google Scholar]
- 434. Resnick HE, Heineman J, Stone R, Shorr RI. Diabetes in U.S. nursing homes, 2004. Diabetes Care. 2008;31(2):287–288. [DOI] [PubMed] [Google Scholar]
- 435. Huang ES, Zhang Q, Gandra N, Chin MH, Meltzer DO. The effect of comorbid illness and functional status on the expected benefits of intensive glucose control in older patients with type 2 diabetes: a decision analysis. Ann Intern Med. 2008;149(1):11–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 436. Washington RE, Andrews RM, Mutter R. Emergency department visits for adults with diabetes, 2010. Available at: www.hcup-us.ahrq.gov/reports/statbriefs/sb167.jsp. Accessed 14 February 2019.
- 437. Umpierrez GE, Pasquel FJ. Management of inpatient hyperglycemia and diabetes in older adults. Diabetes Care. 2017;40(4):509–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 438. Low Wang CC, Draznin B. Practical approach to management of inpatient hyperglycemia in select patient populations. Hosp Pract (1995). 2013;41(2):45–53. [DOI] [PubMed] [Google Scholar]
- 439. Wang YJ, Seggelke S, Hawkins RM, Gibbs J, Lindsay M, Hazlett I, Low Wang CC, Rasouli N, Young KA, Draznin B. Impact of glucose management team on outcomes of hospitalizaron in patients with type 2 diabetes admitted to the medical service. Endocr Pract. 2016;22(12):1401–1405. [DOI] [PubMed] [Google Scholar]
- 440. Snow V, Beck D, Budnitz T, Miller DC, Potter J, Wears RL, Weiss KB, Williams MV. Transitions of care consensus policy statement: American College of Physicians, Society of General Internal Medicine, Society of Hospital Medicine, American Geriatrics Society, American College of Emergency Physicians, and Society for Academic Emergency Medicine. J Hosp Med. 2009;4(6):364–370. [DOI] [PubMed] [Google Scholar]
- 441. Coleman EA, Berenson RA. Lost in transition: challenges and opportunities for improving the quality of transitional care. Ann Intern Med. 2004;141(7):533–536. [DOI] [PubMed] [Google Scholar]
- 442. Umpierrez GE, Reyes D, Smiley D, Hermayer K, Khan A, Olson DE, Pasquel F, Jacobs S, Newton C, Peng L, Fonseca V. Hospital discharge algorithm based on admission HbA1c for the management of patients with type 2 diabetes. Diabetes Care. 2014;37(11):2934–2939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 443. Dorner B, Friedrich EK, Posthauer ME; American Dietetic Association . Position of the American Dietetic Association: individualized nutrition approaches for older adults in health care communities. J Am Diet Assoc. 2010;110(10):1549–1553. [DOI] [PubMed] [Google Scholar]
- 444. Pandya N, Thompson S, Sambamoorthi U. The prevalence and persistence of sliding scale insulin use among newly admitted elderly nursing home residents with diabetes mellitus. J Am Med Dir Assoc. 2008;9(9):663–669. [DOI] [PubMed] [Google Scholar]
- 445. Pandya N, Wei W, Meyers JL, Kilpatrick BS, Davis KL. Burden of sliding scale insulin use in elderly long-term care residents with type 2 diabetes mellitus. J Am Geriatr Soc. 2013;61(12):2103–2110. [DOI] [PubMed] [Google Scholar]
- 446. Swanson CM, Potter DJ, Kongable GL, Cook CB. Update on inpatient glycemic control in hospitals in the United States. Endocr Pract. 2011;17(6):853–861. [DOI] [PubMed] [Google Scholar]
- 447. Bersoux S, Cook CB, Kongable GL, Shu J. Trends in glycemic control over a 2-year period in 126 US hospitals. J Hosp Med. 2013;8(3):121–125. [DOI] [PubMed] [Google Scholar]
- 448. Klonoff DC, Draznin B, Drincic A, Dungan K, Gianchandani R, Inzucchi SE, Nichols JH, Rice MJ, Seley JJ. Pride statement on the need for a moratorium on the CMS plan to cite hospitals for performing point-of-care capillary blood glucose monitoring on critically ill patients. J Clin Endocrinol Metab. 2015;100(10):3607–3612. [DOI] [PubMed] [Google Scholar]
- 449. McDonnell ME, Umpierrez GE. Insulin therapy for the management of hyperglycemia in hospitalized patients. Endocrinol Metab Clin North Am. 2012;41(1):175–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 450. Umpierrez GE, Smiley D, Jacobs S, Peng L, Temponi A, Mulligan P, Umpierrez D, Newton C, Olson D, Rizzo M. Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes undergoing general surgery (RABBIT 2 surgery). Diabetes Care. 2011;34(2):256–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 451. Umpierrez GE, Smiley D, Zisman A, Prieto LM, Palacio A, Ceron M, Puig A, Mejia R. Randomized study of basal-bolus insulin therapy in the inpatient management of patients with type 2 diabetes (RABBIT 2 trial). Diabetes Care. 2007;30(9):2181–2186. [DOI] [PubMed] [Google Scholar]
- 452. Umpierrez GE, Smiley D, Hermayer K, Khan A, Olson DE, Newton C, Jacobs S, Rizzo M, Peng L, Reyes D, Pinzon I, Fereira ME, Hunt V, Gore A, Toyoshima MT, Fonseca VA. Randomized study comparing a basal-bolus with a basal plus correction insulin regimen for the hospital management of medical and surgical patients with type 2 diabetes: Basal Plus Trial. Diabetes Care. 2013;36(8):2169–2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 453. Wexler DJ, Meigs JB, Cagliero E, Nathan DM, Grant RW. Prevalence of hyper- and hypoglycemia among inpatients with diabetes: a national survey of 44 U.S. hospitals. Diabetes Care. 2007;30(2):367–369. [DOI] [PubMed] [Google Scholar]
- 454. Bueno E, Benitez A, Rufinelli JV, Figueredo R, Alsina S, Ojeda A, Samudio S, Cáceres M, Arguello R, Romero F, Echague G, Pasquel F, Umpierrez GE. Basal-bolus regimen with insulin analogues versus human insulin in medical patients with type 2 diabetes: a randomized controlled trial in Latin America. Endocr Pract. 2015;21(7):807–813. [DOI] [PubMed] [Google Scholar]
- 455. Boucai L, Southern WN, Zonszein J. Hypoglycemia-associated mortality is not drug-associated but linked to comorbidities. Am J Med. 2011;124(11):1028–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 456. Finfer S, Chittock DR, Su SY, Blair D, Foster D, Dhingra V, Bellomo R, Cook D, Dodek P, Henderson WR, Hébert PC, Heritier S, Heyland DK, McArthur C, McDonald E, Mitchell I, Myburgh JA, Norton R, Potter J, Robinson BG, Ronco JJ; NICE-SUGAR Study Investigators . Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360(13):1283–1297. [DOI] [PubMed] [Google Scholar]
- 457. Kagansky N, Levy S, Rimon E, Cojocaru L, Fridman A, Ozer Z, Knobler H. Hypoglycemia as a predictor of mortality in hospitalized elderly patients. Arch Intern Med. 2003;163(15):1825–1829. [DOI] [PubMed] [Google Scholar]
- 458. Shilo S, Berezovsky S, Friedlander Y, Sonnenblick M. Hypoglycemia in hospitalized nondiabetic older patients. J Am Geriatr Soc. 1998;46(8):978–982. [DOI] [PubMed] [Google Scholar]
- 459. Shorr RI, Ray WA, Daugherty JR, Griffin MR. Incidence and risk factors for serious hypoglycemia in older persons using insulin or sulfonylureas. Arch Intern Med. 1997;157(15):1681–1686. [PubMed] [Google Scholar]
- 460. Garg R, Hurwitz S, Turchin A, Trivedi A. Hypoglycemia, with or without insulin therapy, is associated with increased mortality among hospitalized patients. Diabetes Care. 2013;36(5):1107–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 461. Kosiborod M, Inzucchi SE, Goyal A, Krumholz HM, Masoudi FA, Xiao L, Spertus JA. Relationship between spontaneous and iatrogenic hypoglycemia and mortality in patients hospitalized with acute myocardial infarction. JAMA. 2009;301(15):1556–1564. [DOI] [PubMed] [Google Scholar]
- 462. Pasquel FJ, Powell W, Peng L, Johnson TM, Sadeghi-Yarandi S, Newton C, Smiley D, Toyoshima MT, Aram P, Umpierrez GE. A randomized controlled trial comparing treatment with oral agents and basal insulin in elderly patients with type 2 diabetes in long-term care facilities. BMJ Open Diabetes Res Care. 2015;3(1):e000104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 463. Sacks DB, Arnold M, Bakris GL, Bruns DE, Horvath AR, Kirkman MS, Lernmark A, Metzger BE, Nathan DM; National Academy of Clinical Biochemistry . Position statement executive summary: guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Diabetes Care. 2011;34(6):1419–1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 464. Huang ES, Liu JY, Moffet HH, John PM, Karter AJ. Glycemic control, complications, and death in older diabetic patients: the diabetes and aging study. Diabetes Care. 2011;34(6):1329–1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 465. Luitse MJ, Velthuis BK, Kappelle LJ, van der Graaf Y, Biessels GJ; DUST Study Group . Chronic hyperglycemia is related to poor functional outcome after acute ischemic stroke. Int J Stroke. 2017;12(2):180–186. [DOI] [PubMed] [Google Scholar]
- 466. Blasco ML, Sanjuan R, Palacios L, Huerta R, Carratala A, Nuñez J, Sanchis J. Prognostic value of admission glycated haemoglobin in unknown diabetic patients with acute myocardial infarction. Eur Heart J Acute Cardiovasc Care. 2014;3(4):347–353. [DOI] [PubMed] [Google Scholar]
- 467. Kim EJ, Jeong MH, Kim JH, Ahn TH, Seung KB, Oh DJ, Kim HS, Gwon HC, Seong IW, Hwang KK, Chae SC, Kim KB, Kim YJ, Cha KS, Oh SK, Chae JK; KAMIR-NIH Registry Investigators . Clinical impact of admission hyperglycemia on in-hospital mortality in acute myocardial infarction patients. Int J Cardiol. 2017;236:9–15. [DOI] [PubMed] [Google Scholar]
- 468. Matsushita K, Blecker S, Pazin-Filho A, Bertoni A, Chang PP, Coresh J, Selvin E. The association of hemoglobin A1c with incident heart failure among people without diabetes: the Atherosclerosis Risk in Communities Study. Diabetes. 2010;59(8):2020–2026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 469. Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, Jaeschke R, Rind D, Meerpohl J, Dahm P, Schünemann HJ. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–394. [DOI] [PubMed] [Google Scholar]
- 470. Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ; GRADE Working Group . GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 471. Guyatt GH, Schünemann HJ, Djulbegovic B, Akl EA. Guideline panels should not GRADE good practice statements. J Clin Epidemiol. 2015;68(5):597–600. [DOI] [PubMed] [Google Scholar]