Abstract
Background:
The novel human coronavirus disease 2019 (COVID-19) pandemic has claimed more than 240,000 lives worldwide, causing tremendous public health, social, and economic damages. While the risk factors of COVID-19 are still under investigation, environmental factors, such as urban air pollution, may play an important role in increasing population susceptibility to COVID-19 pathogenesis.
Methods:
We conducted a cross-sectional nationwide study using zero-inflated negative binomial models to estimate the association between long-term (2010–2016) county-level exposures to NO2, PM2.5 and O3 and county-level COVID-19 case-fatality and mortality rates in the US. We used both single and multipollutant models and controlled for spatial trends and a comprehensive set of potential confounders, including state-level test positive rate, county-level healthcare capacity, phase-of-epidemic, population mobility, sociodemographic, socioeconomic status, behavior risk factors, and meteorological factors.
Results:
1,027,799 COVID-19 cases and 58,489 deaths were reported in 3,122 US counties from January 22, 2020 to April 29, 2020, with an overall observed case-fatality rate of 5.8%. Spatial variations were observed for both COVID-19 death outcomes and long-term ambient air pollutant levels. County-level average NO2 concentrations were positively associated with both COVID-19 case-fatality rate and mortality rate in single-, bi-, and tri-pollutant models (p-values<0.05). Per inter-quartile range (IQR) increase in NO2 (4.6 ppb), COVID-19 case-fatality rate and mortality rate were associated with an increase of 7.1% (95% CI 1.2% to 13.4%) and 11.2% (95% CI 3.4% to 19.5%), respectively. We did not observe significant associations between long-term exposures to PM2.5 or O3 and COVID-19 death outcomes (p-values>0.05), although per IQR increase in PM2.5 (3.4 ug/m3) was marginally associated with 10.8% (95% CI: −1.1% to 24.1%) increase in COVID-19 mortality rate.
Discussions and Conclusions:
Long-term exposure to NO2, which largely arises from urban combustion sources such as traffic, may enhance susceptibility to severe COVID-19 outcomes, independent of long-term PM2.5 and O3 exposure. The results support targeted public health actions to protect residents from COVID-19 in heavily polluted regions with historically high NO2 levels. Moreover, continuation of current efforts to lower traffic emissions and ambient air pollution levels may be an important component of reducing population-level risk of COVID-19 deaths.
Keywords: Air pollution, Nitrogen dioxide, COVID-19, Case-fatality rate, Mortality
Introduction
The novel human coronavirus disease 2019 (COVID-19) is an emerging infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)1. First identified in 2019 in Wuhan, the capital of Hubei Province, China, the COVID-19 pandemic has since rapidly spread globally. As of April 29, 2020, there have been 1,027,799 cases and 58,489 deaths confirmed in the United States2. Despite substantial public health efforts, the observed COVID-19 case-fatality rate (i.e. the ratio of the number of COVID-19 deaths over the number of cases) in the US is estimated to be 5.8%3. Although knowledge concerning the etiology of COVID-19-related disease has grown since the outbreak was first identified, there is still considerable uncertainty concerning its pathogenesis, as well as factors contributing to heterogeneity in disease severity around the globe. Environmental factors, such as urban air pollution, may play an important role in increasing susceptibility to severe outcomes of COVID-19. The impact of ambient air pollution on excess morbidity and mortality has been well-established over several decades4–8. In particular, major ubiquitous ambient air pollutants, including fine particulate matter (PM2.5), nitrogen dioxide (NO2), and ozone (O3), may have both direct and indirect systemic impact on the human body by enhancing oxidative stress and inflammation, eventually leading to respiratory, cardiovascular, and immune system dysfunction and deterioration9–13.
While the epidemiologic evidence is limited, previous findings on the outbreak of severe acute respiratory syndrome (SARS), the most closely related human coronavirus disease to COVID-19, revealed positive associations between air pollution and SARS case-fatality rate in the Chinese population14. An analysis of 213 cities in China recently demonstrated that temporal increases in COVID-19 cases was associated with short-term variations in ambient air pollution15. Hence, it is plausible that prolonged exposure to air pollution may have a detrimental effect on the prognosis of patients affected by COVID-1916. As is usual in the early literature on emerging hazards, questions remain concerning the generalizability and reproducibility of these finding, due to the lack of control for the epidemic stage-of-disease, population mobility, residual spatial correlation, and potential confounding by co-pollutants.
To address these analytical gaps and contribute towards a more complete understanding of the impact of long-term exposures to ambient air pollution on COVID-19-related health consequences, we conducted a nationwide study in the USA (3,122 counties) examining associations between multiple key ambient air pollutants, NO2, PM2.5, and O3, and COVID-19 case-fatality and mortality rates in both single and multi-pollutant models, with comprehensive covariate adjustment. We hypothesized that residents living in areas with higher long-term ambient air pollution levels may be more susceptible to COVID-19 severe outcomes, thus resulting in higher COVID-19 case-fatality rates and mortality rates among more heavily polluted counties.
Methods
We obtained the number of daily county-level COVID-19 confirmed cases and deaths that occurred from January 22, 2020, the day of first confirmed case in the US, through April 29, 2020 in the US from three databases: the New York Times17, USAFACTS18, and 1Point3Acres.com19. In this analysis, the main COVID-19 death outcomes included two measures, the county-level COVID-19 case-fatality rate and mortality rate. The COVID-19 case-fatality rate was calculated by dividing the number of deaths over the number of people diagnosed for each US county with at least 1 or more confirmed case, which can imply the biological susceptibility towards server COVID-19 outcomes (i.e. death). The COVID-19 mortality rate was the number of COVID-19 deaths per million population, and it can reflect the severity of the COVID-19 deaths in the general population.
Three major criteria ambient air pollutants were included in the analysis, including NO2, a traffic-related air pollutant and a major component of urban smog, PM2.5, a heterogeneous mixture of fine particles in the air, and O3, a common secondary air pollutant20. We recently estimated daily ambient NO2, PM2.5, and O3 levels at 1 km2 spatial resolution across the Contiguous US using an ensemble machine learning model21,22. We calculated the daily average for each county based on all covered 1 km2 grid cells, and then further calculated the annual mean (2010–2016) for NO2 and PM2.5, and the warm-season mean (2010–2016) for O3, defined as May 1 to October 31. Although more recent exposure data were not available, county-specific mean concentrations of air pollutants across years are highly correlated23.
We compiled county-level information for several covariates that may also contribute to heterogeneity in the observed COVID-19 rates and thus may confound associations with long-term air pollution exposure. Healthcare capacity was measured by the number of intensive care unit (ICU) beds, hospital beds, and active medical doctors per 1000 people24. Population travel mobility index, based on anonymized location data from smartphones, was used to account for changes in travel distance in reaction to the COVID-19 pandemic25,26. Socioeconomic status (SES) was measured by social deprivation index27, a commonly used measure of area-level SES, composed of income, education, employment, housing, household characteristics, transportation, and demographics28. Sociodemographic covariates included population density, percentage of elderly (age ≥ 60), and percentage of male24. We also obtained behavioral risk factors including population mean body mass index (BMI) and smoking rate24, and meteorological variables29 including air temperature and relative humidity. Additional information about these covariates, including data sources, are given in the Technical Appendix.
Statistical methods
We fit zero-inflated negative binomial mixed models (ZINB) to estimate the associations between long-term exposure to NO2, PM2.5, and O3 and COVID-19 case-fatality rates and mortality rates. The ZINB model comprises a negative binomial log-linear count model and a logit model for predicting excess zeros30,31. The former was used to describe the associations between air pollutants and COVID-19 case-fatality rate among counties with at least one reported COVID-19 case. The latter can account for excess zeros in counties that have not observed a COVID-19 death as of April 29, 2020. We fit single-pollutant, bi-pollutant, and tri-pollutant models, in order to estimate the effects of each pollutant without and with control for co-pollutants. All analyses were conducted at the county level. For the negative binomial count component, results are presented as percent change in case-fatality rate or mortality rate per interquartile range (IQR) increase in each air pollutant concentration. IQRs were calculated based on mean air pollutant levels across all 3,122 counties. Similar results are presented as odds ratios for the excess zero component. We included a random intercept for each state because observations within the same state tended to be correlated, potentially due to similar COVID-19 responses, quarantine and testing policies, healthcare capacity, sociodemographic, and meteorological conditions.
As different testing practices may bias outcome ascertainment, we adjusted for state-level COVID-19 test positive rate (i.e. a high positive rate might imply that the confirmed case numbers were limited by the ability of testing, thus upward-biasing the case-fatality). To model how different counties may be at different time points of the epidemic curve (i.e., phase-of-epidemic), we adjusted for days both since the first case and since the 100th case within a county through April 29. In addition, we adjusted for potential confounders including county-level healthcare capacity, population mobility, sociodemographic, SES, behavior risk factors, and meteorological factors, as described above.
To control for potential residual spatial trends and confounding, we included spatial smoothers within the model using natural cubic splines with 5 degrees freedom for both county centroid latitude and longitude. To examine the presence of spatial autocorrelation in the residuals, we calculated Moran’s I of the standardized residuals of tri-pollutant main models among counties within each state. Statistical tests were 2-sided and statistical significance and confidence intervals were calculated with an alpha of 0.05. All statistical analyses were conducted used R version 3.4.
Sensitivity analyses
We conducted a series of sensitivity analyses to test the robustness of our results to outliers, confounding adjustment, and epidemic timing (Supplementary Appendix Figures S1 and S2). Given that New York City has far higher COVID-19 cases and deaths than any other region, we excluded all five counties within New York City in one sensitivity analysis. In another, we restricted the study to the most recent 4 weeks (April 1 to April 29), when the case count and death count may be more reliable and accurate compared to earlier periods. We also conducted sensitivity analysis by using air pollution data averaged between 2000 to 2016. To assess the importance of individual confounder covariates, we fit models by omitting a different set of covariates for each model iteration and compared effect estimates.
Results
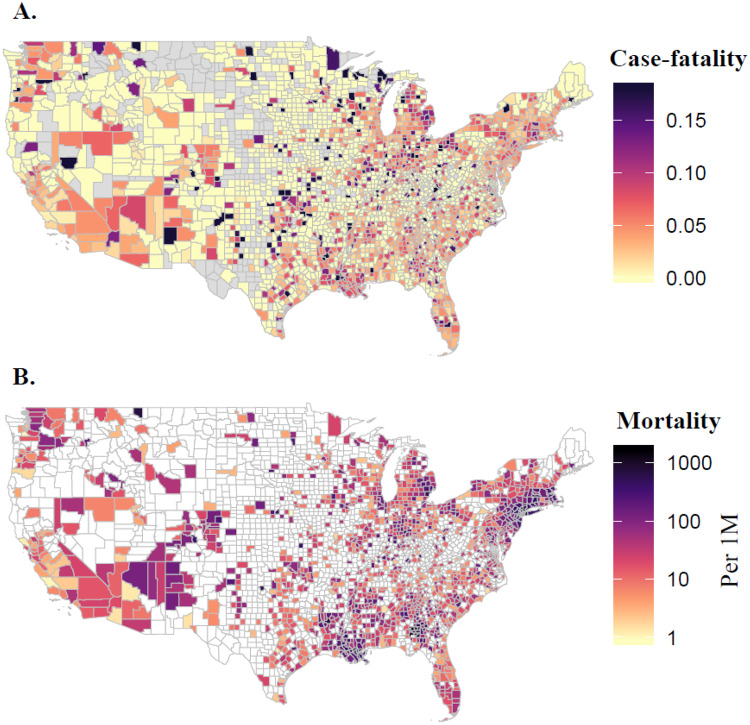
A total of 3,122 US counties were considered in the current analysis, with confirmed cases reported in 2,810 (90.0%) and deaths in 1,443 (46.2%). By April 29, 2020, 1,027,799 COVID-19 cases and 58,489 deaths were reported nationwide (Table 1). Among the counties with at least one reported COVID-19 case, the average county-level case-fatality rate was 3.7 ± 7.0% (mean ± standard deviation), and the average mortality rate was 69.4 ± 183.1 per 1 million people. Spatial variations were observed on COVID-19 case-fatality and mortality rates, where Michigan had the highest average county-level case-fatality rate of 8.2% and New York had the largest mortality rate of 1,117.2 deaths per 1 million people. The lowest case-fatality rate and mortality rate were observed in Wyoming (0.7%) and North Dakota (11.8 deaths per million people), respectively (Figure 1).
Table 1.
Descriptive Statistics* on County-Level COVID-19 Fatality Rate* and Long-Term Air Pollution Level in 3,122 US Counties
| State | # of County with Cases | Total Case # | Total Death # | COVID-19 Fatality Rate (%) | Mean NO2 Level (ppb) | Mean PM2.5 Level (ug/m3) | Mean Ozone Level (ppb) | # of ICU Beds per 1k ppl | # of Hospital Beds per 1k ppl | # of Medical Doctors per 1k ppl |
|---|---|---|---|---|---|---|---|---|---|---|
| Total | 2,810 | 1,027,799 | 58,489 | 3.7 ± 7.0 | 11.5 ± 4.5 | 39.8 ± 2.6 | 8.1 ± 1.9 | 0.15 ± 0.59 | 2.7 ± 3.5 | 1.3 ± 1.7 |
| Alabama | 67 | 6925 | 262 | 2.8 ± 2.8 | 8.8 ± 2.1 | 9.6 ± 0.5 | 41 ± 1.5 | 0.18 ± 0.18 | 2.8 ± 2.7 | 1 ± 1 |
| Alaska | 12 | 349 | 8 | 1.2 ± 2 | 11.7 ± 2.2 | 3.7 ± 1.9 | 51.7 ± 2.8 | 0.1 ± 0.12 | 2.4 ± 1.9 | 1.8 ± 1.1 |
| Arizona | 15 | 7202 | 302 | 3.2 ± 3.8 | 15.5 ± 5.3 | 4.5 ± 1.2 | 51.3 ± 1.7 | 0.14 ± 0.12 | 1.7 ± 0.9 | 1.3 ± 0.9 |
| Arkansas | 73 | 3040 | 59 | 2.3 ± 5.4 | 9.7 ± 2.7 | 9.2 ± 0.7 | 42.3 ± 1.2 | 0.12 ± 0.18 | 2.4 ± 2.5 | 0.9 ± 1 |
| California | 54 | 48792 | 1944 | 2.6 ± 2.7 | 12.9 ± 5.6 | 6.8 ± 2.6 | 46.2 ± 7 | 0.15 ± 0.09 | 2.1 ± 1.8 | 2.1 ± 1.3 |
| Colorado | 56 | 14613 | 763 | 4.8 ± 8.2 | 15.2 ± 9.6 | 4.3 ± 1.7 | 50.7 ± 1.5 | 0.58 ± 3.69 | 2.5 ± 4.2 | 1.5 ± 1.1 |
| Connecticut | 8 | 26260 | 2165 | 7.9 ± 3.5 | 17.2 ± 4.9 | 7.1 ± 0.7 | 42.3 ± 0.7 | 0.15 ± 0.06 | 2.3 ± 1.5 | 2.7 ± 1.6 |
| Delaware | 3 | 4629 | 144 | 3.2 ± 0.7 | 15.7 ± 5.6 | 9 ± 0.6 | 45.1 ± 0.7 | 0.18 ± 0.03 | 2.3 ± 1.2 | 2 ± 0.9 |
| District of Columbia | 1 | 4106 | 205 | 5 | 25.1 | 9.2 | 45.3 | 0.44 | 6.2 | 7.8 |
| Florida | 67 | 33186 | 1218 | 3.7 ± 4 | 10.9 ± 2.1 | 7.4 ± 0.8 | 35.8 ± 2.5 | 0.17 ± 0.16 | 2.3 ± 2.9 | 1.5 ± 1.4 |
| Georgia | 157 | 24127 | 1081 | 4.4 ± 4.3 | 10.2 ± 3.3 | 9.4 ± 1 | 41.5 ± 2.1 | 0.13 ± 0.22 | 2.7 ± 4.1 | 1 ± 1.1 |
| Hawaii | 4 | 605 | 16 | 1.8 ± 2.2 | 7.9 ± 1 | 5.3 ± 1.4 | 35.7 ± 0.8 | 0.13 ± 0.02 | 2.2 ± 0.5 | 2.4 ± 0.8 |
| Idaho | 33 | 1984 | 60 | 1.9 ± 5 | 11.4 ± 3.9 | 5.5 ± 1.3 | 46 ± 2.1 | 0.07 ± 0.11 | 1.7 ± 1.6 | 0.9 ± 0.8 |
| Illinois | 96 | 50001 | 2215 | 3.1 ± 4.7 | 14.4 ± 4.7 | 9.7 ± 0.3 | 43.1 ± 1.3 | 0.12 ± 0.16 | 2.3 ± 2.1 | 1.1 ± 1.1 |
| Indiana | 92 | 17391 | 964 | 5.4 ± 5.5 | 14.5 ± 3.8 | 10.3 ± 0.6 | 42.5 ± 1.4 | 0.15 ± 0.19 | 1.9 ± 2.2 | 1.1 ± 1.2 |
| Iowa | 86 | 6823 | 148 | 2.5 ± 11.1 | 11.4 ± 2.3 | 8.6 ± 0.6 | 41 ± 0.5 | 0.09 ± 0.16 | 2.8 ± 2.4 | 0.9 ± 1.5 |
| Kansas | 78 | 3739 | 128 | 2.3 ± 7.6 | 12 ± 3.2 | 7.6 ± 1 | 46 ± 1.8 | 0.12 ± 0.21 | 6.2 ± 6.8 | 1 ± 0.8 |
| Kentucky | 113 | 4484 | 235 | 2.8 ± 5.5 | 10 ± 2.7 | 9.6 ± 0.9 | 43.2 ± 1.2 | 0.15 ± 0.25 | 2.3 ± 2.7 | 1 ± 1.1 |
| Louisiana | 64 | 27599 | 1802 | 6.6 ± 4.9 | 11.2 ± 3.6 | 8.9 ± 0.6 | 40.8 ± 1.7 | 0.16 ± 0.19 | 3.4 ± 5.2 | 1.2 ± 1.5 |
| Maine | 16 | 1054 | 52 | 2.9 ± 5.8 | 10.4 ± 2.3 | 5 ± 0.6 | 35.2 ± 2.1 | 0.15 ± 0.13 | 2.5 ± 1.5 | 2.1 ± 1.2 |
| Maryland | 24 | 20849 | 911 | 4 ± 2.5 | 16.2 ± 5.1 | 8.8 ± 0.9 | 45.4 ± 0.6 | 0.15 ± 0.19 | 2.4 ± 2.2 | 2.5 ± 2.3 |
| Massachusetts | 14 | 59808 | 3400 | 6.3 ± 3.3 | 16 ± 4.6 | 6.4 ± 0.8 | 40.6 ± 1.1 | 0.15 ± 0.14 | 2.5 ± 1.6 | 3.7 ± 3.1 |
| Michigan | 78 | 39010 | 3631 | 8.2 ± 9.1 | 11.2 ± 4.9 | 7.7 ± 1.6 | 40.8 ± 1.3 | 0.16 ± 0.24 | 2.3 ± 2 | 1.3 ± 1.6 |
| Minnesota | 79 | 4637 | 319 | 3 ± 7.5 | 11.3 ± 2.2 | 6.7 ± 1.1 | 39.1 ± 1.6 | 0.1 ± 0.21 | 3.7 ± 5 | 1.4 ± 2.7 |
| Mississippi | 81 | 6569 | 250 | 4.2 ± 4 | 8.7 ± 2.2 | 9.4 ± 0.5 | 40.9 ± 1.8 | 0.14 ± 0.22 | 3.9 ± 3.3 | 1 ± 1.2 |
| Missouri | 96 | 7402 | 318 | 2.5 ± 5.4 | 10.3 ± 3.9 | 8.7 ± 0.6 | 43.3 ± 1 | 0.12 ± 0.19 | 2.2 ± 2.5 | 0.9 ± 1.5 |
| Montana | 30 | 454 | 16 | 2.4 ± 5.4 | 6.7 ± 1.7 | 4.9 ± 0.9 | 43.5 ± 2.2 | 0.07 ± 0.12 | 5.7 ± 6.9 | 1.4 ± 1 |
| Nebraska | 60 | 3759 | 72 | 2.9 ± 13.2 | 10.8 ± 2.6 | 7.5 ± 1.3 | 43.4 ± 2.5 | 0.08 ± 0.18 | 4 ± 3.8 | 0.9 ± 0.8 |
| Nevada | 12 | 4933 | 231 | 4.7 ± 9.4 | 14.1 ± 6 | 4.2 ± 1.2 | 50.3 ± 1.7 | 0.14 ± 0.22 | 2.5 ± 2.1 | 1.1 ± 0.9 |
| New Hampshire | 10 | 2050 | 66 | 1.9 ± 2.3 | 11.9 ± 0.8 | 5.4 ± 0.6 | 38.6 ± 1.1 | 0.19 ± 0.17 | 2.2 ± 1.4 | 3.2 ± 3.8 |
| New Jersey | 21 | 115647 | 6770 | 5.7 ± 2.2 | 22.9 ± 6.2 | 8.7 ± 0.7 | 43.2 ± 1.1 | 0.19 ± 0.09 | 2.7 ± 1.1 | 2.6 ± 1.4 |
| New Mexico | 30 | 3213 | 112 | 5.5 ± 18.5 | 11.4 ± 3.7 | 4.3 ± 1.1 | 50 ± 1.2 | 0.13 ± 0.12 | 2 ± 2.1 | 1.2 ± 1 |
| New York | 62 | 299691 | 21732 | 4.9 ± 5.8 | 15.1 ± 7.8 | 7.1 ± 1 | 41.2 ± 1.3 | 0.15 ± 0.11 | 3.2 ± 2.1 | 2.1 ± 2 |
| North Carolina | 98 | 9516 | 354 | 3.7 ± 6.1 | 10.6 ± 2.7 | 8.3 ± 1 | 42.2 ± 1.2 | 0.15 ± 0.17 | 1.8 ± 1.6 | 1.5 ± 1.9 |
| North Dakota | 35 | 1033 | 9 | 6.2 ± 23.5 | 7.1 ± 1.9 | 5.6 ± 0.5 | 40.3 ± 0.9 | 0.07 ± 0.18 | 6.5 ± 8.3 | 0.9 ± 1.1 |
| Ohio | 88 | 17303 | 937 | 5.6 ± 6.4 | 15.4 ± 3.7 | 10.2 ± 0.6 | 43.3 ± 1.1 | 0.17 ± 0.15 | 2.1 ± 1.7 | 1.2 ± 1.2 |
| Oklahoma | 70 | 3473 | 214 | 5.6 ± 8.7 | 10.5 ± 2.3 | 8.3 ± 0.9 | 46 ± 1.9 | 0.1 ± 0.16 | 2.8 ± 2.8 | 0.6 ± 0.6 |
| Oregon | 32 | 2446 | 101 | 2.4 ± 4.7 | 9.8 ± 2.6 | 4.8 ± 1.1 | 39.5 ± 3.8 | 0.12 ± 0.13 | 1.7 ± 1.5 | 1.7 ± 1.3 |
| Pennsylvania | 67 | 44366 | 2195 | 3.4 ± 3.4 | 13.9 ± 4.4 | 9.2 ± 1.2 | 43 ± 0.9 | 0.21 ± 0.29 | 3.3 ± 5.1 | 2.2 ± 4.6 |
| Rhode Island | 5 | 7182 | 146 | 1.2 ± 1.4 | 15.5 ± 3.5 | 6.3 ± 0.8 | 42.2 ± 0.2 | 0.14 ± 0.14 | 1.6 ± 1.2 | 3.7 ± 1.8 |
| South Carolina | 46 | 5881 | 232 | 4.1 ± 4.4 | 10.1 ± 2.2 | 8.7 ± 0.5 | 39.7 ± 2 | 0.17 ± 0.15 | 2.1 ± 2 | 1.3 ± 1.3 |
| South Dakota | 45 | 2372 | 13 | 1.3 ± 4.7 | 8.2 ± 2.2 | 6.3 ± 1.4 | 42.7 ± 1.2 | 0.08 ± 0.17 | 4.2 ± 4.8 | 1.1 ± 1.3 |
| Tennessee | 93 | 10090 | 191 | 1.9 ± 3.1 | 8.8 ± 3 | 9.1 ± 0.6 | 43 ± 1.1 | 0.13 ± 0.19 | 2.3 ± 2.5 | 1 ± 1.3 |
| Texas | 207 | 27054 | 732 | 2.9 ± 6 | 10.2 ± 3 | 8.5 ± 1.3 | 43.3 ± 4.7 | 0.1 ± 0.17 | 2.2 ± 4.1 | 0.9 ± 0.9 |
| Utah | 24 | 4500 | 45 | 0.9 ± 1.7 | 13.2 ± 6.7 | 4.6 ± 1.9 | 50.3 ± 1.1 | 0.08 ± 0.1 | 1.9 ± 1.4 | 1.2 ± 1.1 |
| Vermont | 14 | 859 | 47 | 2.8 ± 2.7 | 11.1 ± 1 | 5.3 ± 0.5 | 38.8 ± 0.8 | 0.1 ± 0.12 | 1.8 ± 1.5 | 2.6 ± 1.8 |
| Virginia | 119 | 14766 | 518 | 3.1 ± 4.6 | 12.2 ± 4 | 8.3 ± 0.6 | 42.9 ± 1.1 | 0.16 ± 0.29 | 2.9 ± 5.8 | 1.9 ± 3 |
| Washington | 38 | 13994 | 801 | 3.5 ± 4.4 | 10.6 ± 2.9 | 4.9 ± 1.2 | 38.5 ± 4.2 | 0.1 ± 0.11 | 2 ± 2.1 | 1.4 ± 1 |
| West Virginia | 50 | 1109 | 40 | 2.8 ± 8.1 | 9.4 ± 1.7 | 8 ± 1.3 | 42.5 ± 1.4 | 0.19 ± 0.28 | 3.4 ± 3.5 | 1.3 ± 1.8 |
| Wisconsin | 66 | 6520 | 308 | 5.8 ± 9.7 | 11.4 ± 3.9 | 7.6 ± 1.2 | 39.7 ± 1.6 | 0.13 ± 0.15 | 1.8 ± 1.2 | 1.5 ± 1.4 |
| Wyoming | 21 | 404 | 7 | 0.7 ± 2.1 | 6.8 ± 2.9 | 3.7 ± 0.7 | 46.4 ± 2.3 | 0.13 ± 0.14 | 4.5 ± 3.2 | 1.4 ± 0.9 |
Descriptive statistics was conducted on 3,122 US counties using data reported as of April 29, 2020
COVID-19 case fatality rate was calculated by the number of deaths divided by the number of cases, reported as of April 29, 2020
Figure 1.
County-level COVID-19 Case-fatality Rate (A) and Mortality Rate per 1 Million people (B) as of April 29, 2020.
Long-term (2010–2016) average concentrations across the contiguous US ranged from 5.8 to 19.3 parts per billion (ppb; 5th and 95th percentiles, respectively) NO2, 3.8 to 10.4 μg/m3 PM2.5, and 37.2 to 49.7 ppb for warm-season average ozone concentrations, respectively (Figure 2). The highest NO2 levels were in New York, New Jersey, and Colorado, and the lowest in Montana, Wyoming, and South Dakota. California and Pennsylvania had the highest PM2.5 concentrations, and the highest O3 levels were in Colorado, Utah, and California.
Figure 2.
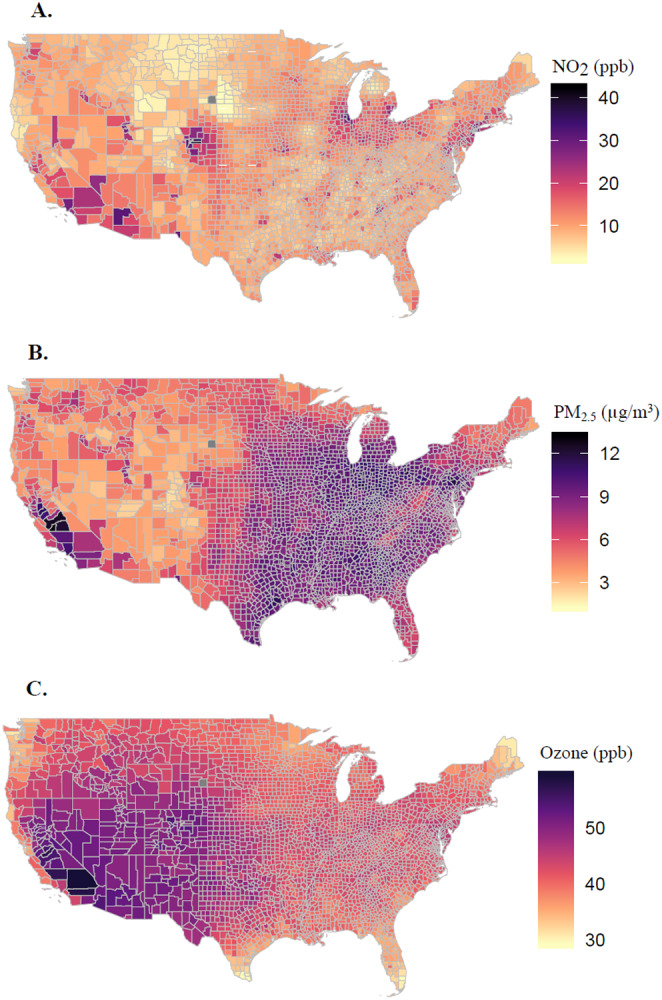
County-level Annual Average Concentrations of Nitrogen Dioxide (NO2, A), Fine Particulate Matter (PM2.5, B), and Ozone (C) for the period 2010–2016.
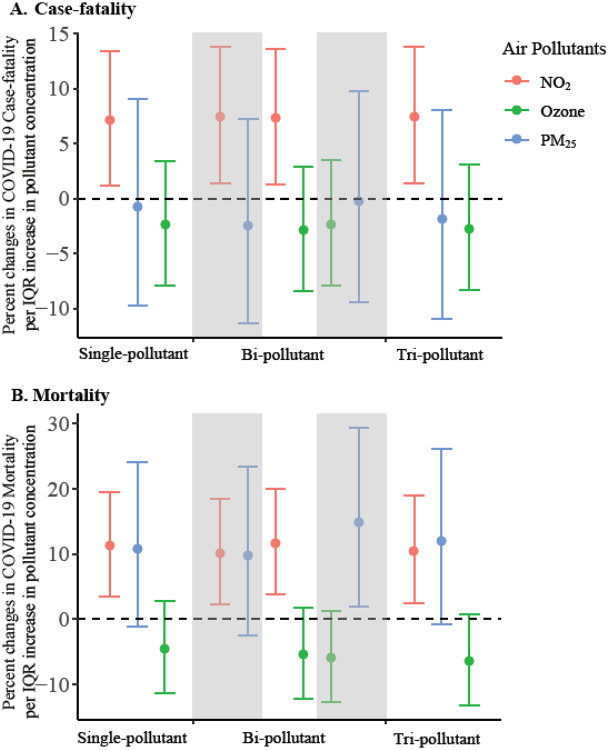
We observed significant positive associations between NO2 levels and both county-level COVID-19 case-fatality rate and mortality rate (p=0.02 and p<0.001, respectively, Table S1 and Figure 3), when controlling for covariates. In single pollutant models, COVID-19 case-fatality and mortality rates were associated with increases of 7.1% (95% CI: 1.2% to 13.4%) and 11.2% (95% CI: 3.4% to 19.5%), respectively, per IQR (~4.6 ppb) increases in NO2. These results imply that one IQR reduction in long-term exposure to NO2 level would have avoided 4,181 deaths (95% CI: 718 to 7,845) among those tested positive for the virus and 19.9 deaths (95% CI: 6.1 to 34.8) per million people in the general population, as of April 29, 2020.
Figure 3. Percent Change in County-level COVID-19 Case-fatality Rate (A) and Mortality Rate (B) Per Inter Quartile Range (IQR) increase in Long-Term Air Pollutant Concentrations.
Effect estimates and 95% confidence interval were calculated using county-level concentrations of nitrogen dioxide (NO2, red), ozone (green), and fine particulate matter (PM2.5, blue) averaged between 2010–2016, controlling for covariates including county-level number of case per 1000 people, social deprivation index, population density, percent of residents over 60 years old, percent of male, body mass index, smoking rate, number of regular hospital beds per 1000 people, number of intensive units beds per 1000 people, number of medical doctors per 1000 people, average mobility index assessed in March and April 2020, average temperature and humidity between January 22 to April 29, 2020, state-level COVID-19 test positive rate as of April 29, 2020, and spatial smoother with a degree freedom of 5 for both latitude and longitude. IQRs of NO2, PM2.5, and O3 averaged between 2010–2016 were 4.6 parts per billion (ppb), 3.4 ug/m3, and 2.8 ppb, respectively.
Results from the zero-component model agrees with the count model where higher NO2 concentrations were associated with a decrease in the probability of observing zero COVID-19 death (Appendix Table S1). The strength and magnitude of the associations between NO2 and both COVID-19 case-fatality rate and mortality rate persisted across single, bi-, and tri-pollutant models (Figure 3).
In contrast, PM2.5 was not associated with COVID-19 case-fatality rate (p=0.87) but was marginally associated with higher COVID-19 mortality rate (p=0.08), where one IQR (3.4 ug/m3) increase in PM2.5 was associated with 10.8% (95% CI: −1.1% to 24.1%) increase in COVID-19 mortality rate. Null associations were found between long-term exposure to O3 and both COVID-19 case-fatality and mortality rates (p=0.42 and p=0.22, respectively). The Moran’s I and p-values (Appendix Table S2) from these models suggested that most spatial correlation in the data has been accounted for.
Results remained robust and consistent across 30 sets of sensitivity analyses (Appendix Figures S1 and S2). When we restricted the analyses to data reported between April 1 to April 29, when COVID-19 tests were more readily available, significant associations remained between NO2 and COVID-19 case-fatality and mortality rates, and no associations were found with PM2.5 or O3. We also observed similar trends pointing to associations with NO2 when excluding the New York City. In addition, even though 679 counties (22%) had missing behavioral risk data, the analysis omitting behavioral risk factors yielded similar results.
Discussion
In this nationwide study, we used county-level information on long-term air pollution and corresponding health, behavioral, and demographic data to examine associations between long-term exposures to key ambient air pollutants and COVID-19 death outcomes in both single and multi-pollutant models. We observed significant positive associations between NO2 levels and both county-level COVID-19 case-fatality rate and mortality rate, while null associations were found for long-term PM2.5 and O3 exposures. These results provide additional initial support for the interpretation that long-term exposure to NO2, a component of urban air pollution related to traffic, may enhance susceptibility to severe COVID-19 outcomes. These findings may help identify susceptible and high-risk populations, especially those living in areas with historically high NO2 pollution, including the metropolitan areas in New York, New Jersey, Colorado, and Michigan. Given the rapid escalation of COVID-19 spread and associated mortality in the US, swift and coordinated public health actions, including strengthened enforcement on social distancing and expanding healthcare capacity, are needed to protect these and the other vulnerable populations. Although average NO2 concentrations have decreased gradually over the past decades, it is critical to continue enforcing air pollution regulations to protect public health, given that health effects occur even at very low concentrations8.
Among the sparse studies on the link between air pollution and COVID-19, our findings are consistent with a recent European study that reported 78% of the COVID-19 deaths across 66 administrative regions in Italy, Spain, France and Germany, occurred in the five most polluted regions with the highest NO2 levels32. Another recent paper reported correlations between high levels of air pollution and high death rates seen in northern Italy33. However, major questions remain concerning the robustness and generalizability of these early findings, due to the lack of control for population mobility, multipollutant exposures, and most importantly, potential residual spatial autocorrelation.
With the current analysis, we hopefully contribute to the questions involving the potential link between urban air pollution and COVID-19 risk in addressing these issues. We examined two major COVID-19 death outcomes, the county-level case-fatality rate and the mortality rate. The case-fatality rate can imply on the biological susceptibility towards server COVID-19 outcomes (i.e. death), while the mortality rate can offer information of the severity of the COVID-19 deaths in the general population. Looking at both case-fatality and mortality will contribute to a more comprehensive understanding on the impact of air pollution exposures on COVID-19 death outcomes. Our study included an assessment of three major air pollutants using high spatial resolution maps, the use of recent county-level data, consideration for both single and multi-pollutant models, and control of county-level mobility. Given that the stage of the COVID-19 epidemic might depend on the size and urbanicity of the county, we included the time of the first and 100th case for each county in the models as covariates to minimize the possibility that the observed associations are confounded by epidemic timing due to unmeasured location and population-level characteristics. Due to the cross-sectional design, we controlled for potential spatial trends by including flexible spatial trends in the main analysis, and evaluated residual autocorrelation using Moran’s I statistic. Our analyses indicated that the presence of spatial confounding was substantial, necessitating the use of spatial smoothing. We observed statistically significant PM2.5 and O3 associations with COVID-19 mortality in models without controlling for spatial smoothers (Appendix Figures S1 and S2). Finally, we conducted a total of 30 sets of sensitivity analyses and observed robust and consistent results.
Although the various social distancing measures around the US have reduced vehicle traffic and urban air pollution, it is plausible that long-term exposure to urban air pollutants like NO2 may have direct and indirect effects within the human body, making people more biologically susceptible to severe COVID-19 outcomes. NO2 can be emitted directly from combustion sources or produced from the titration of NO with O3. NO2 and nitric oxide (NO) have relatively short atmospheric lifetime, thus having larger spatial heterogeneity compared to more regionally distributed pollutants such as PM2.5 and O3. As a result, the spatial distribution of NO2 represents the intensity of anthropogenic activity, especially emissions from traffic and power plants. As a reactive free radical, NO2 plays a key role in photochemical reactions that produce other secondary pollutants, including ozone and secondary particulate matter. In our analysis of three major air pollutants, however, NO2 showed strong and independent effects with COVID-19 case-fatality rate and mortality, meaning that the effects of NO2 may not be mediated by PM2.5 and O3. Even so, we cannot rule out the possibility that NO2 is serving as a proxy for other traffic-related air pollutants, such as soot, trace metals, or ultrafine particles. Long-term exposures to NO2 have been associated with acute and chronic respiratory diseases, including increased bronchial hyperresponsiveness, decreased lung function, and increased risk of respiratory infection and mortality34–36. In addition, as a highly reactive exogeneous oxidant, NO2 can induce inflammation and enhance oxidative stress, generating reactive oxygen and nitrogen species, which may eventually deteriorate the cardiovascular and immune systems37,38. The impact of long-term exposure to PM2.5 on excess morbidity and mortality has also been well-established4–5,8. An early unpublished report that explored the impacts of air pollution on mortality found that 1 μg/m3 PM2.5 was associated with 8% increase in COVID-19 mortality rates in the USA39. The study was conducted in a single pollutant model and did not investigate on COVID-19 case-fatality rates. In contrast, we found only marginally significant associations between COVID-19 mortality rates and PM2.5. Specifically, the magnitude and strength of this association observed in the current analysis were weaker, mainly due to our control of the spatial trends and residual autocorrelation, which may have confounded the previous study findings34. In addition, PM2.5 was not associated with COVID-19 case-fatality rate across all single and multipollutant models, indicating that it may have less impact on biological susceptibility to severe COVID-19 outcomes compared to NO2.
We acknowledge that our study is limited in several key areas. First, the cross-sectional study design reduced our ability to exploit temporal variation and trends in COVID-19 deaths, an important determinant in establishing causal inference. Towards this end, time-series analyses of air pollution and COVID-19 case-fatality rates and corresponding mortality rates will be important; these data will only be available in the future. Second, actual death counts are likely underestimated, particularly during the early stages of the outbreak, with highly dynamic reported fatality rates, increasing from 1.8% to 5.8% in the past two months. However, results using data from only the most recent four weeks were largely unchanged, suggesting that differential errors in reporting or testing for COVID-19 may not have exerted much influence on these findings. Third, although we controlled for many potential confounders such as population density, we cannot rule out the possibility that NO2 might be a proxy of urbanicity. The exclusion of climate meteorological variables and SES – two factors that have received substantial attention regarding the outbreak – did not alter the main results. In addition, testing data only came from state or federal agencies, while tests from private labs were not available. Due to the lack of county-level data, we could not account for the percentage of hospitalized cases or ICU use among cases or deaths, the number of available ventilators, and the underlying health conditions of cases likely to increase death risk (e.g., chronic obstructive pulmonary disease). Also, as a classic traffic related air pollutant, NO2 can exhibit spatial variation within a county, which may not be captured in our analysis. Identification of NO2 pollution hotspots within a county may be warranted.
Conclusions
We found statistically significant, positive associations between long-term exposure to NO2 and COVID-19 case-fatality rate and mortality rate, independent of PM2.5 and O3. Prolonged exposure to this urban traffic-related air pollutant may be an important risk factor of severe COVID-19 outcomes. The results support targeted public health actions to protect residents from COVID-19 in heavily polluted regions with historically high NO2 levels. Moreover, continuation of current efforts to lower traffic emissions and ambient air pollution levels may be an important component of reducing population-level risk of COVID-19 deaths.
Supplementary Material
Acknowledgement
This project was supported by Emory HERCULES exposome center through the National Institute of Environmental Health Sciences (grant number P30ES019776). S.G. acknowledges the funding support provided by the National Science Foundation (Award No. BCS-2027375). Any opinions, findings, and conclusions or recommendations expressed in this material are those of the author(s) and do not necessarily reflect the views of the National Institutes of Health and the National Science Foundation. The authors would like to thank Qian Di, Weeberb J. Requia, and Yagung Wei for contribution to the generation of air pollution data.
Footnotes
Potential Conflicts of Interest:
The authors have no conflicts of interest relevant to this article to disclose
Data Sharing Statement: Data will be made available when requested.
Reference
- 1.Onder G, Rezza G, Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. Jama. 2020. [DOI] [PubMed] [Google Scholar]
- 2.Johns Hopkins Coronavirus Resource Center; 2020. https://coronavirus.jhu.edu/map.html. Accessed April 29, 2020.
- 3.COVID I, Murray CJ. Forecasting COVID-19 impact on hospital bed-days, ICU-days, ventilator-days and deaths by US state in the next 4 months. medRxiv. 2020. [Google Scholar]
- 4.Liu C, Chen R, Sera F, et al. Ambient particulate air pollution and daily mortality in 652 cities. New England Journal of Medicine. 2019;381(8):705–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shi L, Zanobetti A, Kloog I, et al. Low-concentration PM2. 5 and mortality: estimating acute and chronic effects in a population-based study. Environmental health perspectives. 2016;124(1):46–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anenberg SC, Henze DK, Tinney V, et al. Estimates of the global burden of ambient PM 2.5, ozone, and NO 2 on asthma incidence and emergency room visits. Environmental health perspectives. 2018;126(10):107004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alhanti BA, Chang HH, Winquist A, Mulholland JA, Darrow LA, Sarnat SE. Ambient air pollution and emergency department visits for asthma: a multi-city assessment of effect modification by age. Journal of exposure science & environmental epidemiology. 2016;26(2):180–188. [DOI] [PubMed] [Google Scholar]
- 8.Di Q, Wang Y, Zanobetti A, et al. Air pollution and mortality in the Medicare population. New England Journal of Medicine. 2017;376(26):2513–2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pino MV, Levin JR, Stovall MY, Hyde DM. Pulmonary inflammation and epithelial injury in response to acute ozone exposure in the rat. Toxicology and applied pharmacology. 1992;112(1):64–72. [DOI] [PubMed] [Google Scholar]
- 10.Ayyagari VN, Januszkiewicz A, Nath J. Pro-inflammatory responses of human bronchial epithelial cells to acute nitrogen dioxide exposure. Toxicology. 2004;197(2):148–163. [DOI] [PubMed] [Google Scholar]
- 11.Ayyagari VN, Januszkiewicz A, Nath J. Effects of nitrogen dioxide on the expression of intercellular adhesion molecule-1, neutrophil adhesion, and cytotoxicity: studies in human bronchial epithelial cells. Inhalation toxicology. 2007;19(2):181–194. [DOI] [PubMed] [Google Scholar]
- 12.Liang D, Moutinho JL, Golan R, et al. Use of high-resolution metabolomics for the identification of metabolic signals associated with traffic-related air pollution. Environment international. 2018;120:145–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liang D, Ladva CN, Golan R, et al. Perturbations of the arginine metabolome following exposures to traffic-related air pollution in a panel of commuters with and without asthma. Environment international. 2019;127:503–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cui Y, Zhang Z-F, Froines J, et al. Air pollution and case fatality of SARS in the People’s Republic of China: an ecologic study. Environmental Health. 2003;2(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yongjian Z, Jingu X, Fengming H, Liqing C. Association between short-term exposure to air pollution and COVID-19 infection: Evidence from China. Science of The Total Environment. 2020:138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Contini D, Costabile F. Does Air Pollution Influence COVID-19 Outbreaks? In: Multidisciplinary Digital Publishing Institute; 2020. [Google Scholar]
- 17.The New York Times; 2020. https://www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html. Accessed April 29, 2020.
- 18.USAFACTS; 2020. https://usafacts.org/visualizations/coronavirus-covid-19-spread-map/. Accessed April 29, 2020.
- 19.1Point3Acres.com; 2020. https://coronavirus.1point3acres.com/. Accessed April 29, 2020.
- 20.Pollution HEIPotHEoT-RA. Traffic-related air pollution: a critical review of the literature on emissions, exposure, and health effects. Health Effects Institute; 2010. [Google Scholar]
- 21.Di Q, Amini H, Shi L, et al. An ensemble-based model of PM2. 5 concentration across the contiguous United States with high spatiotemporal resolution. Environment international. 2019;130:104909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Di Q, Amini H, Shi L, et al. Assessing NO2 Concentration and Model Uncertainty with High Spatiotemporal Resolution across the Contiguous United States Using Ensemble Model Averaging. Environmental science & technology. 2019;54(3):1372–1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dai Yue-Hua, and Zhou Wei-Xing. “Temporal and spatial correlation patterns of air pollutants in Chinese cities.” PloS one 12, no. 8 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Area Health Resources Files; 2019. https://data.hrsa.gov/topics/health-workforce/ahrf. Accessed April 29, 2020.
- 25.Gao S, Rao J, Kang Y, Liang Y, Kruse J. Mapping county-level mobility pattern changes in the United States in response to COVID-19. Available at SSRN 3570145. 2020. [Google Scholar]
- 26.Warren MS, Skillman SW. Mobility Changes in Response to COVID-19. arXiv preprint arXiv:200314228. 2020. [Google Scholar]
- 27.Social Deprivation Index. Robert Graham Center; 2019. https://www.graham-center.org/rgc/maps-data-tools/sdi/social-deprivation-index.html. Accessed April 29, 2020. [Google Scholar]
- 28.Butler DC, Petterson S, Phillips RL, Bazemore AW. Measures of social deprivation that predict health care access and need within a rational area of primary care service delivery. Health services research. 2013;48(2pt1):539–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xia Y, Mitchell K, Ek M, et al. Continental scale water and energy flux analysis and validation for the North American Land Data Assimilation System project phase 2 (NLDAS 2): 1. Intercomparison and application of model products. Journal of Geophysical Research: Atmospheres. 2012;117(D3). [Google Scholar]
- 30.Garay AM, Hashimoto EM, Ortega EM, Lachos VH. On estimation and influence diagnostics for zero-inflated negative binomial regression models. Computational Statistics & Data Analysis. 2011;55(3):1304–1318. [Google Scholar]
- 31.Fang R. Zero-Inflated Negative Binomial (Zinb) Regression Model for over-dispersed count data with excess zeros and repeated measures, an application to human microbiota sequence data, University of Colorado Anschutz Medical Campus. Strauss Health Sciences Library; 2013. [Google Scholar]
- 32.Ogen Y. Assessing nitrogen dioxide (NO2) levels as a contributing factor to the coronavirus (COVID-19) fatality rate. Science of The Total Environment. 2020:138605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Conticini E, Frediani B, Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? 2020:114465 Environmental Pollution. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Abbey D, Colome S, Mills P, Burchette R, Beeson W, Tian Y. Chronic disease associated with long-term concentrations of nitrogen dioxide. Journal of exposure analysis and environmental epidemiology. 1993;3(2):181–202. [PubMed] [Google Scholar]
- 35.Faustini A, Rapp R, Forastiere F. Nitrogen dioxide and mortality: review and meta-analysis of long-term studies. European Respiratory Journal. 2014;44(3):744–753. [DOI] [PubMed] [Google Scholar]
- 36.Jammes Y, Delpierre S, Delvolgo MJ, Humbert-Tena C, Burnet H. Long-term exposure of adults to outdoor air pollution is associated with increased airway obstruction and higher prevalence of bronchial hyperresponsiveness. Archives of Environmental Health: An International Journal. 1998;53(6):372–377. [DOI] [PubMed] [Google Scholar]
- 37.Gan WQ, Davies HW, Koehoorn M, Brauer M. Association of long-term exposure to community noise and traffic-related air pollution with coronary heart disease mortality. American journal of epidemiology. 2012;175(9):898–906. [DOI] [PubMed] [Google Scholar]
- 38.Bevelander M, Mayette J, Whittaker LA, et al. Nitrogen dioxide promotes allergic sensitization to inhaled antigen. The Journal of Immunology. 2007;179(6):3680–3688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wu X, Nethery RC, Sabath BM, Braun D, Dominici F. Exposure to air pollution and COVID-19 mortality in the United States. medRxiv. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.