Abstract
Objectives
A previous meta-analysis reported high HIV incidence among pregnant and breastfeeding women in sub-Saharan Africa (SSA), but limited evidence of elevated risk of HIV acquisition during pregnancy or breastfeeding when compared to non-pregnant periods. The rapidly evolving HIV prevention and treatment landscape since publication of this review may have important implications for maternal HIV incidence.
Design
Systematic review and meta-analysis.
Methods
We searched four databases and abstracts from relevant conferences through December 1, 2018, for literature on maternal HIV incidence in SSA. We used random-effects meta-analysis to summarize incidence rates and ratios, and to estimate 95% prediction intervals (PI). We evaluated potential sources of heterogeneity with random-effects meta-regression.
Results
Thirty-seven publications contributed 100,758 person-years (PY) of follow-up. The estimated average HIV incidence rate among pregnant and breastfeeding women was 3.6 per 100PY (95%PI: 1.2, 11.1), while the estimated average associations between pregnancy and risk of HIV acquisition, and breastfeeding and risk of HIV acquisition, were close to the null. Wide 95% PIs around summary estimates, however, highlighted the variability of HIV incidence across populations of pregnant and breastfeeding women in SSA. Average HIV incidence appeared associated with age, partner HIV status, and calendar time. Average incidence was highest among studies conducted pre-2010 (4.1/100PY, 95%PI: 1.1, 12.2) and lowest among studies conducted post-2014 (2.1/100PY, 95%PI: 0.7, 6.5).
Conclusions
Substantial HIV incidence among pregnant and breastfeeding women in SSA, even in the current era of combination HIV prevention and treatment, underscores the need for prevention tailored to high-risk pregnant and breastfeeding women.
Keywords: HIV, incidence, pregnancy, breastfeeding, sub-Saharan Africa, adolescent, women
Introduction
HIV acquisition among pregnant and breastfeeding women increases risk of maternal morbidity and mortality, and accounts for a significant, and growing, proportion of pediatric HIV infections globally [1]. A meta-analysis of 19 studies conducted between 1980 and 2012 estimated an average HIV incidence rate of 3.8/100 person-years (PY, 95% CI: 3.0, 4.6) among pregnant and breastfeeding women in sub-Saharan Africa (SSA) [2]. While this estimate is above the World Health Organization’s (WHO) threshold for substantial risk of HIV acquisition [3], the rapidly evolving HIV prevention and treatment landscape since publication of this review may have important implications for maternal HIV incidence.
In 2013 the WHO updated HIV treatment guidelines, expanding antiretroviral therapy (ART) eligibility to CD4≤500 cells/mm3 [4], and in 2015 it recommended universal treatment for HIV [5]. These changes, together with increased uptake of HIV testing and counseling and medical male circumcision [6–8], coincided with a 30% decline in the estimated number of new adult HIV infections in SSA between 2010 and 2017 [9]. Similar temporal trends in incidence have been observed in three population-based cohort studies in SSA [10–12], with more gradual declines observed among women than among men [11, 12]. Although combination HIV prevention and treatment interventions may not directly target pregnant and breastfeeding women, these populations may experience downstream benefits in HIV prevention. In at least one study [13], maternal HIV incidence was considerably lower in a cohort of pregnant and breastfeeding women participating in a community-based HIV prevention program than estimates of maternal incidence from the previous review [2].
While the previous review observed evidence of heterogeneity among study-specific estimates of the incidence rate and the association between pregnancy and risk of HIV acquisition, their investigation into the underlying factors contributing to this variability was limited [2]. A better understanding of features contributing to variation in estimates is critical for guiding future research and policy, and for developing efficient strategies to reduce horizontal and vertical HIV transmission during pregnancy and breastfeeding.
In this updated review of literature from SSA between 1980 and 2018, we sought to summarize estimates of HIV incidence among pregnant and breastfeeding women; summarize estimates of the associations between pregnancy and risk of maternal HIV acquisition and between breastfeeding and risk of HIV acquisition; and identify population and methodological characteristics contributing to variation in study-specific estimates of incidence and association.
Methods
This review is registered with PROSPERO (CRD42017079577) and follows the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Guidelines [14].
Study selection and data abstraction
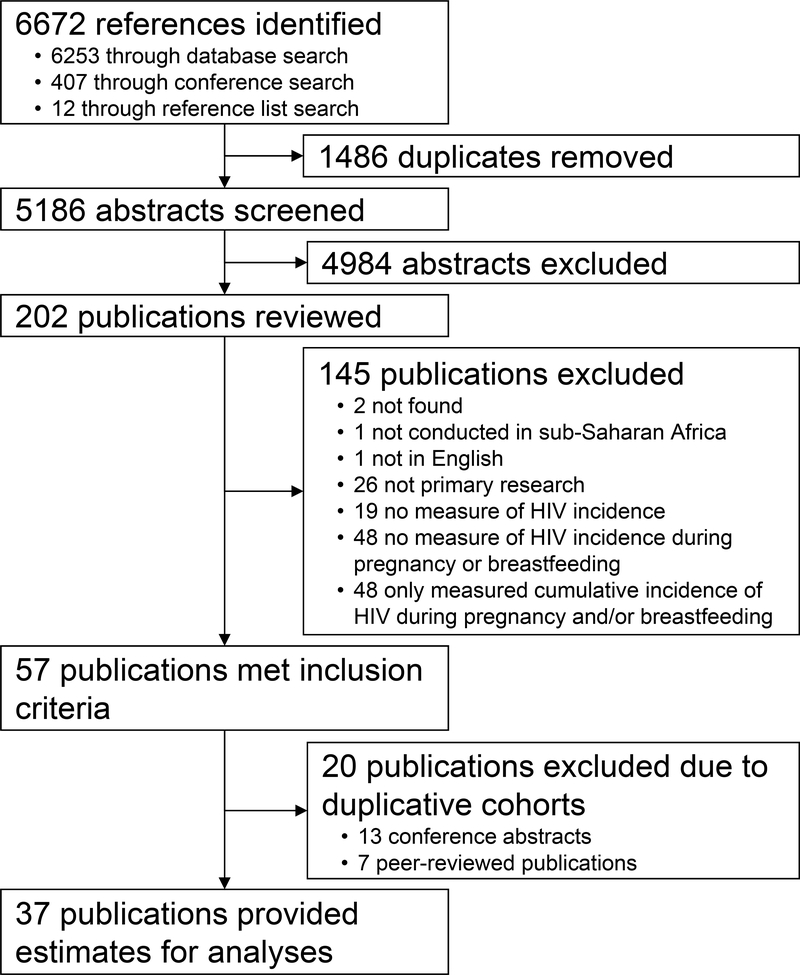
We searched PubMed, Embase, PsycInfo, and the Cochrane Library for relevant literature published between January 1, 1980 and December 1, 2018 (search strategy is available in Table S1). We also searched online abstract archives from HIV Research for Prevention Conference (2014–2018), Conference of Retroviruses and Opportunistic Infections (2014–2018), and International AIDS Society Conferences (2001–2018) using the terms (‘pregnant’, ‘pregnancy’, or ‘postpartum’) and (‘incident’, ‘incidence’, or ‘seroconvert’).
We screened resulting titles and abstracts to identify publications that referred to HIV incidence among women or to pregnancy/breastfeeding and HIV. We conducted a full text review of included publications to identify primary research reports with estimates of (or sufficient information to derive) the incidence rate of HIV among pregnant and breastfeeding women, the incidence rate ratio (IRR) or hazard ratio (HR) contrasting HIV incidence between pregnant and non-pregnant periods, and/or the IRR or HR contrasting HIV incidence between breastfeeding and non-breastfeeding periods. Included studies were restricted to those published in English and conducted in SSA. We requested additional information from authors when publications contained relevant but insufficient information, and reviewed the bibliographies of included publications for relevant references.
Two investigators reviewed each publication at screening and full-text review; disagreements were resolved by consensus. Data on outcomes and exposures of interest and key population and methodological features of each study were abstracted into standardized tables by one reviewer and checked by two others. When more than one publication reported the same outcome from the same study population over the same period, we included the report considered most complete.
Outcome and exposure definitions
HIV incidence, the primary outcome, was defined as the number of new HIV infections per 100 PY. Pregnancy and breastfeeding represented periods of interest in studies contributing incidence rate estimates, and represented exposures of interest in studies estimating the IRR or HR. We accepted all definitions in our primary analyses. In a sensitivity analysis, we excluded studies where the breastfeeding-period exceeded 24 months postpartum [15].
Statistical approach
We used inverse-variance-weighted random-effects meta-analysis to estimate natural log-transformed measures of the average HIV incidence rate among pregnant and breastfeeding women, the average association between pregnancy and risk of HIV acquisition, the average association between breastfeeding and risk of HIV acquisition, and 95% prediction intervals (PI) around summary estimates. 95% PIs convey the estimated spread of the random-effects distribution, and can be informally interpreted as 95% confidence interval (CI) for the true rate or association to be estimated in a randomly selected study population [16–18]. When zero seroconversions were reported, we applied a half-integer continuity correction to prevent the estimate from being omitted. Since IRRs roughly approximate HRs [19], we pooled these estimates for meta-analysis and assumed approximate collapsibility since HIV acquisition is rare [20]. Summary estimates and 95% PIs were exponentiated for interpretability.
Because of the potential for publication bias, we drew funnel plots and analyzed them with the symmetry test of Egger et al. and with Duval and Tweedie’s trim-and-fill imputation method [21, 22]. We analyzed overall heterogeneity using 95% PIs and the p-value for Cochrane’s Q statistic. We used stratified analyses and univariate random-effects meta-regression to analyze heterogeneity further by comparing average rates and associations by population characteristics of included studies. Meta-regression was also used to explore associations between estimates and methodological aspects related to study quality [23, 24]. When a single study contributed information to more than one stratum of a variable, we used robust variances to account for correlation [25]. Given the large number studies contributing estimates of the incidence rate, we also constructed separate multivariable models for each for each potential source of heterogeneity of the incidence rate. Each model adjusted for region, years of study implementation, and calendar time to account for differences in HIV prevalence and ART coverage. All analyses were conducted using the Metafor package in R, version 3.5.1 (R Foundation for Statistical Computing, Vienna, Austria) [26].
Sources of heterogeneity
Characteristics related to underlying HIV risk – region, calendar time, age, membership of a high-risk population, and participant enrollment in an HIV-prevention clinical trial – may be associated with estimates of incidence and association. Because studies contributing estimates of the association had limited variability in calendar time, and did not provide age-stratified results, these features were only evaluated as sources of heterogeneity of the incidence rate.
We defined region using the World Bank’s classifications, and calendar time based on mid-year of study implementation. We examined calendar time continuously, as a quadratic function, and categorically with three periods: pre-combination HIV prevention (before 2010), early adoption (2010–2014), and program expansion (after 2014). These periods correspond to important updates to WHO HIV treatment and prevention recommendations [4, 5, 27, 28], and their implementation across SSA [6–8]. We defined age groups based on the most commonly reported categorization in the literature: <20, 20–24, 25–29, and ≥30. Other age group categorizations were considered in sensitivity analyses. We used a binary variable to distinguish between studies that enrolled a ‘high-risk’ cohort (e.g. HIV-discordant couples or female sex workers) and those that did not. We stratified by type of ‘high-risk’ group in sensitivity analyses. Studies were also classified according to whether participants were enrolled in a clinical trial evaluating an HIV prevention intervention.
The following features related to the measurement of incident infections and person-time may also be associated with estimates of incidence and association: study design, use of results from repeat HIV testing to identify seroconversions, reproductive periods observed over follow-up, use of HIV DNA/RNA polymerase chain reaction (PCR) in the HIV testing algorithm, and method for estimating date of HIV infection. As all studies contributing estimates of the association used repeat HIV testing and observed all reproductive periods over follow-up, these features were only evaluated as sources of heterogeneity of the incidence rate.
Finally, estimates of the IRR or HR may be related to the inclusion of breastfeeding-exposed periods in the reference group, adjustment for confounders, and adjustment for time-varying measures of condom use and intercourse frequency.
Results
Our search yielded 5,186 non-duplicate abstracts (Figure 1). Screening resulted in 202 publications for full-text review, of which 57 met inclusion criteria. After excluding 20 publications due to overlapping cohorts and outcomes, 37 publications remained (Table 1). Thirty-four contributed estimates of the HIV incidence rate [13, 29–61], and ten contributed estimates of either the IRR or HR [55–64]. Follow-up ranged from 45PY to 57,240PY. Most studies were conducted in southern Africa (n=20) [13, 29, 30, 32, 34, 35, 39–44, 48, 51, 52, 54, 55, 60, 61, 64]. The mid-point of follow-up occurred before 2010 in 26 studies [29, 32, 34–36, 38–44, 48, 50, 52–64], between 2010 and 2014 in eight [30, 31, 33, 37, 46, 47, 49, 55], and after 2014 in three [13, 45, 51]. Two studies reported results stratified by calendar time [55, 56]. In seven studies, participants were enrolled in an HIV prevention trial [32, 43, 54, 60–62, 64]. Four studies enrolled high-risk study populations [54, 57, 62, 63], and two studies reported results stratified by risk-group [58, 59]. Eight studies reported estimates of incidence stratified by age [13, 30, 38, 39, 44, 48, 55, 58].
Figure 1.
Study Selection Flowchart
Table 1.
Description of studies meeting inclusion criteria
| Publication | Region | Study design | Study years | Incident cases of HIV | PY | Definition of Pregnancy | Definition of Breastfeeding | Contrast estimated by IRR or HR | High-risk participant recruitment | Parent study was a clinical trial of an HIV prevention intervention | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Exposed Group | vs. | Unexposed Group | ||||||||||
| Studies that only contributed estimates of the incidence rate during pregnancy | ||||||||||||
| De Schacht (2014) [29] | Southern Africa | Prospective cohort | 2008–2011 | 14 | 328 |
Date of enrollment to date of delivery All participants enrolled during the index pregnancy. Median gestational age at enrollment was 24 weeks. |
- | - | - | No | No | |
| Egbe (2016) [31] | Western Africa | Cross-sectional | 2011 | 9 | 147 |
Date of first ANC visit to date of delivery Women were 16–20 weeks pregnant at their first ANC visit. |
- | - | - | No | No | |
| Imade (2013) [33] | Western Africa | Cross-sectional | 2010–2012 | 4 | 235 |
Date of first ANC visit to date of delivery Information on gestational age at first ANC is not provided. |
- | - | - | No | No | |
| Keating (2012) [34] | Southern Africa | Cross-sectional | 2009 | 11 | 275 |
Date of first ANC visit to date of delivery Average gestational age at first ANC was 25 weeks. |
- | - | - | No | No | |
| Kieffer (2011) [35] | Southern Africa | Cross-sectional | 2008–2008 | 58 | 388 |
Date of first ANC visit to date of delivery Information on gestational age at first ANC is not provided. |
- | - | - | No | No | |
| Moodley (2009) [41] | Southern Africa | Cross-sectional | 2006–2007 | 72 | 679 |
Date of first ANC visit to date of subsequent ANC visit Average of 24 weeks between first ANC visit and subsequent ANC visit. |
- | - | - | No | No | |
| Phiri (2016) [51] | Southern Africa | Cross-sectional | 2015 | 83 | 4888 |
Date of first ANC visit to date of delivery First ANC was assumed to have occurred approximately 4.5 months before delivery. |
- | - | - | No | No | |
| Rogers (2017) [46] | Eastern Africa | Cross-sectional | 2011–2014 | 2 | 45 |
Date of first ANC visit to date of subsequent ANC visit Average period between ANC visits is not provided. |
- | - | - | No | No | |
| Tabu (2013) [47] | Eastern Africa | Cross-sectional | 2012 | 5 | 311 | Not clearly defined, but the entire period between the first HIV test and the final HIV test occurred in pregnancy. | - | - | - | No | No | |
| Traore (2012) [49] | Western Africa | Prospective cohort | 2010–2011 | 0 | 126 |
First ANC visit to the end of pregnancy Average gestational age at first ANC was 14 weeks. Average length of follow-up was 22.8 weeks. |
- | - | - | No | No | |
| Studies that only contributed estimates of the incidence rate during breastfeeding | ||||||||||||
| De Schacht (2014) [30] | Southern Africa | Prospective cohort | 2008–2012 | 41 | 1278 | - |
Date of enrollment to 18 months postpartum Enrollment occurred 0–8 weeks postpartum, with the majority of women enrolling within four days of delivery. Median length of follow-up was 18.2 months. |
- | - | No | No | |
| Humphrey (2006) [32] | Southern Africa | Prospective cohort | 1997–2001 | 269 | 7763 | - |
Date of enrollment to 18 months postpartum Enrollment occurred between 0–96 hours after delivery. Women were analytically censored 12 months postpartum. |
- | - | No | NCT00198718 Evaluated the effect of maternal vitamin A supplementation soon after delivery on HIV incidence. | |
| Leroy (1994) [38] | Eastern Africa | Prospective cohort | 1988–1992 | 17 | 390 | - |
Date of delivery to 24 months postpartum Average length of follow-up was 32 months, but stratified analyses enabled the restriction of estimates to 24 months postpartum. |
- | - | No | No | |
| Miotti (1994) [40] | Southern Africa | Prospective cohort | 1989–1993 | 43 | 988 | - |
Date of delivery to 24 months postpartum Average length of follow-up was not provided. |
- | - | No | No | |
| Van de Perre (1992) [50] | Eastern Africa | Prospective cohort | 1998–1990 | 18 | 474 | - |
Date of delivery to 24 months postpartum Follow-up continued to 36 months postpartum, but stratified estimates enabled ascertainment of incidence between delivery and 24 months only. |
- | - | No | No | |
| Studies that only contributed estimates of the incidence rate during pregnancy and breastfeeding | ||||||||||||
| Fatti (2017) [13] | Southern Africa | Prospective cohort | 2013–2016 | 11 | 828 |
Date of first ANC visit to date of delivery Median gestational age at first ANC was 16 weeks. |
Date of delivery to 18 months postpartum Average length of follow-up was not provided. 11% of women were lost to follow-up by 12 months postpartum. |
- | - | No | No | |
| John (2006) [53] | Eastern Africa | Cross-sectional | - | 118 | 2565 |
First ANC to approximately 9 months postpartum Information on gestational age at first ANC is not provided. All women in this study had an HIV test at approximately 9 months postpartum. |
- | - | No | No | ||
| Kinuthia (2010) [36] | Eastern Africa | Cross-sectional | - | 53 | 779 |
First ANC to approximately 6 weeks postpartum Information on gestational age at first ANC is not provided. All women in this study had an HIV test approximately 6 weeks postpartum. |
- | - | No | No | ||
| Kinuthia (2015) [37] | Eastern Africa | Prospective cohort | 2011–2013 | 25 | 1278 |
Date of first ANC visit to date of delivery Median gestational at first ANC was 27 weeks. |
Date of delivery to 9 months postpartum Average length of follow-up was not provided. 98% of participants were retained through 9 months postpartum. |
- | - | No | No | |
| Mbizvo (2001) [39] | Southern Africa | Prospective cohort | 1991–1995 | 66 | 1375 |
Date of first ANC visit to date of delivery Information on gestational age at first ANC is not provided. |
Date of delivery to 24 months postpartum Average length of follow-up was not provided. |
- | - | No | No | |
| Mepham (2009) [52] | Southern Africa | Prospective cohort | 2001–2005 | 38 | 717 |
First ANC to approximately 6 months postpartum Median gestational age at first ANC was 25 weeks. All women in this study had an HIV test conducted at approximately 6 months postpartum. |
- | - | No | No | ||
| Moodley (2011) [42] | Southern Africa | Prospective cohort | 2005–2007 | 48 | 1946 |
First ANC to approximately 12 months postpartum Median gestational age at first ANC was 25 weeks. Average length of follow-up was not provided. 88% completed study follow-up. |
- | - | No | No | ||
| Moodley (2015) [43] | Southern Africa | Prospective cohort | 2008–2010 | 6 | 109 |
First ANC to approximately 14 weeks postpartum Median gestational age at first ANC was 24 weeks. Average length of follow-up was not provided. |
- | - | No | NCT01683461 Evaluated the efficacy of enhanced HIV counseling during antenatal and postnatal periods on incidence of STIs and risk-taking behavior. | ||
| Munjoma (2010) [44] | Southern Africa | Prospective cohort | 2002–2008 | 17 | 298 |
First ANC to approximately 9 months postpartum Information on gestational age at first ANC is not provided. Average length of follow-up was 38.2 months; stratified estimates enabled the ascertainment of incidence between first ANC and 9 months only. |
- | - | No | No | ||
| Nikuze (2017) [45] | Eastern Africa | Cross-sectional | 2016 | 33 | 805 | Not clearly defined, but the last HIV test occurred approximately 9 months postpartum | - | - | No | No | ||
| Taha (1998) [48] | Southern Africa | Prospective cohort | 1990–1995 | 97 | 2302 |
First ANC visit to 6 years postpartum Average length of follow-up was 30.2 months. Stratified results are not provided. |
- | - | No | No | ||
| Thomson (2018) [54]† | Southern Africa | Prospective cohort | 2004–2013 | 24 | 447 | LMP to end of pregnancy |
Variable based on pregnancy outcome Pregnancy loss at < 6 weeks gestation: N/A Pregnancy loss between 6–20 weeks gestation: First 28 days following pregnancy loss Pregnancy loss ≥ 20 weeks gestation or infant death before 6 months of age: First 42 days following pregnancy/infant loss. Live birth and no infant death before 6 months of age: Delivery to 6 months postpartum. |
- | - | Recruited HIV serodiscordant couples only |
NCT00194519 Evaluated the efficacy of twice daily acyclovir on HIV incidence NCT00557245 Evaluating the efficacy of PrEP for HIV prevention |
|
| Studies that contributed estimates of the incidence rate during pregnancy and/or breastfeeding, and estimates of the IRR or HR | ||||||||||||
| Braunstein (2011) [57] | Eastern Africa | Prospective cohort | 2006–2008 | 17 | 625 | Not clearly defined |
Not measured over follow-up Study ascertained breastfeeding status at baseline, but did not appear to measure changes to this status over follow-up. |
Incidence during Pregnant Period | vs. | Incidence during Non-Pregnant Periods | Recruited FSWs only | No |
| Chetty (2017) [55] | Southern Africa | Nested surveillance study | 2010–2015 | 66 | 1857 |
Variable based on pregnancy outcome Pregnancies ending in a still or live birth: The period between LMP and date of delivery Pregnancies ending in a miscarriage or termination: The period between LPM to date of expected delivery |
Delivery to 2 months postpartum | Incidence during Pregnant Period Incidence during Breastfeeding Period |
vs. vs. |
Incidence during Non-Pregnant, Non-Breastfeeding Periods Incidence during Non-Pregnant, Non-Breastfeeding Periods |
No | No |
| Gray (2005) [58]* | Eastern Africa | Prospective cohort | 1994–1999 | 63 | 4040 |
The period between pregnancy identification and the immediate postpartum period Average time between pregnancy identification and delivery was 4.6 months. |
Date of first HIV test in the postpartum period to date of repeat HIV test Average time between HIV tests during breastfeeding was 1.05 years |
Incidence among Pregnant Periods Incidence among Breastfeeding Periods |
vs. vs. |
Incidence among Non-Pregnant, Non-Breastfeeding Periods Incidence among Non-Pregnant, Non-Breastfeeding Periods |
This study ascertained information on male partner HIV status for some women and provided estimates of the incidence rate among women in HIV serodiscordant relationships | No |
| Marston (2013) [56]* | Southern and Eastern Africa | Nested surveillance study | 1994–2011 | 767 | 57240 | LMP to date of delivery | Date of delivery to 12 months postpartum | Incidence during Pregnant Period Incidence during Breastfeeding Period |
vs. vs. |
Incidence during Non-Pregnant, Non-Breastfeeding Periods Incidence during Non-Pregnant, Non-Breastfeeding Periods |
No | No |
| Morrison (2007) [59] | Southern and Eastern Africa | Prospective cohort | 1999–2004 | 63 | 3056 |
Not clearly defined Pregnancy status was ascertained at each study visit. It is not clear if the pregnancy status at a current visit defined the exposure status of person-time in the segment before the current visit or the segment after the current visit, or both. |
Not clearly defined Lactation status was ascertained at each study visit. It is not clear if lactation at a current visit defined the exposure status of person-time in the segment before the current visit or the segment after the current visit, or both. |
Incidence during Pregnant Period Incidence during Breastfeeding Period |
vs. vs. |
Incidence during Non-Pregnant, Non-Breastfeeding Periods (without use of hormonal contraception) Incidence during Non-Pregnant, Non-Breastfeeding Periods (without use of hormonal contraception) |
This study recruited a small sub-cohort of high-risk women from STI clinics, sex worker networks, and military bases, and reported incidence rates stratified by risk-group. | No |
| Reid (2010) [60] | Southern Africa | Prospective cohort | 2003–2007 | 72 | 1758 |
Date of first positive pregnancy test to six weeks after first negative pregnancy test In analytical models, “being pregnant” was turned on in the quarter of the first positive pregnancy test and remained on through the quarter of the last positive test. |
Not measured | Incidence during Pregnant Period | vs. | Incidence during Non-Pregnant Periods | No | NCT00076232 Evaluated the efficacy of twice daily acyclovir on HIV incidence |
| Teasdale (2018) [61]‡ | Southern Africa | Prospective cohort | 2003–2006 | 16 | 417 |
Variable based on pregnancy outcome When a live birth was reported <6 weeks from next study visit: Date of first positive pregnancy test to date of first negative test. When a live birth was reported ≥6 weeks from next study visit: Date of first positive pregnancy test to date of last positive test. |
Not measured | Incidence during Pregnant Period | vs. | Incidence during Non-Pregnant Periods (without use of hormonal contraception) | No | NCT00121459 Evaluated the effectiveness of the vaginal diaphragm for preventing HIV infections. |
| Studies that only contributed estimates of the IRR or HR | ||||||||||||
| Mugo (2011) [62]† | Southern and Eastern Africa | Prospective cohort | 2004–2007 | 17 | 231 | The period between LMP to 6 weeks postpartum | Not measured | Incidence during Pregnant Period | vs. | Incidence during Non-Pregnant Period | Recruited HIV serodiscordant couples only | NCT00194519 Description in Thomson (2018) |
| Vandepitte (2013) [63] | Eastern Africa | Prospective cohort | 2008–2011 | - | - |
Not clearly defined Pregnancy status was ascertained at each study visit. It is not clear if the pregnancy status at a current visit defined the exposure status of person-time in the segment before the current visit or the segment after the current visit, or both. |
Not measured | Incidence during Pregnant Period | vs. | Incidence during Non-Pregnant Period | 95% of cohort reported sex work at enrollment | No |
| Wand (2011) [64]‡ | Southern Africa | Prospective cohort | 2002–2005 | - | - | The period between the last negative pregnancy test and the last positive pregnancy test. | Not measured | Incidence during Pregnant Period | vs. | Incidence during Non-Pregnant Period | No | A portion of the study population was enrolled in an HIV prevention clinical trial. NCT00121459 Description in Teasdale (2018) |
Acronyms: ANC=antenatal care; FSW=female sex worker; HR=Hazard ratio; HTC=HIV testing and counseling; IRR=Incidence Rate Ratio; LMP=Last menstrual period; PrEP=pre-exposure prophylaxis; STI=sexually transmitted infection.
The Rakai Community Cohort Study was a study site for both Gray et al. (2005) [58] and Marston et al. (2013) [56]. Periods of follow-up are minimally overlapping, enabling both cohorts to contribute estimates to this meta-analysis.
The Partners in Prevention HSV/HIV Transmission study contributed data from the same time period to both Mugo et al. (2011) [62] and Thomson et al. (2018) [54]. To prevent double counting this cohort, we excluded the IR estimated by Mugo et al. in favor of the IR estimated by Thomson et al. as this estimate included additional follow-up time from the Partners PrEP study. As our inclusion criteria restricted estimates of effect to the IRR or HR, we excluded the risk ratio estimated by Thomson et al. in favor of the HR estimated by Mugo et al.
The Methods for Improving Reproductive Health in Africa (MIRA) study contributed data to both Wand et al. (2011) [64] and Teasdale et al. (2018) [61], however the data included in each publication did not completely overlap. Teasdale et al. included results from both the South African and Zimbabwean MIRA site from 2003–2006, while Wand et al. included results from the South African MIRA site from 2002–2005. We included both studies in our main analysis but conducted sensitivity analyses where we included only one of these studies at a time.
There was limited variability in how studies measured incidence after accounting for study design (Table S2). Prospective cohort studies (n=24) enrolled HIV-seronegative women and retested them over follow-up to identify changes in HIV serostatus. Twenty-one prospective cohort studies contributed estimates of the incidence rate among pregnant and breastfeeding women [13, 29, 30, 32, 37–40, 42–44, 48–50, 52, 54, 58–61], and eight contributed estimates of the IRR or HR [57–64]. Eleven cross-sectional studies contributed estimates of the incidence rate among pregnant and breastfeeding women [31, 33–36, 41, 45–47, 51, 53]. In these studies, HIV status at the time of the first antenatal visit was retrospectively assessed at the time of enrollment, which occurred in the third trimester [31, 41, 46, 47], at delivery [33–35, 51], or in the postpartum period [36, 45, 53]. Women classified as HIV-negative in pregnancy were enrolled and current HIV serostatus was assessed to identify new HIV infections. Finally, two studies nested within large population-based surveillance studies contributed estimates of both the incidence rate and the HR [55, 56]. These studies used prospectively collected data from HIV surveillance assessments to assess changes in serostatus over time.
HIV incidence during pregnancy and breastfeeding
Studies contributing estimates of incidence during pregnancy typically captured the period between the first antenatal visit and delivery, while studies contributing estimates of incidence during breastfeeding captured the period from delivery up to 24 months postpartum depending on length of follow-up (Table 1).
Thirty-four studies contributed 100,758PY of follow-up and generated 44 estimates of HIV incidence among pregnant and/or breastfeeding women. Ten studies reported stratified estimates of incidence during pregnancy and during breastfeeding [13, 37, 39, 44, 54–59]. Using all available estimates, we observed little difference in the average HIV incidence rate during pregnancy only (n=22, 3.4/100PY, 95% PI: 1.1, 10.4), breastfeeding only (n=17, 3.1/100PY, 95% PI: 1.0, 9.5), and pregnancy and breastfeeding combined (n=5, 4.6/100PY, 95% PI: 1.4, 15.4). We therefore combined estimates into a single HIV incidence rate during ‘pregnancy and breastfeeding’ for subsequent analyses. The estimated average of the HIV incidence rates during pregnancy and breastfeeding was 3.6 per 100PY (95% PI: 1.2, 11.1; Figure S1). Our results were unchanged after excluding one study with follow-up exceeding 24 months postpartum [48]. There was no visual or statistical evidence of funnel plot asymmetry (p=0.3). Cochrane’s Q statistic indicated evidence of heterogeneity (p<0.001), which was consistent with the wide 95% PI.
The average HIV incidence rate among pregnant and breastfeeding women was associated with age, calendar time, study design, and method of estimating the timing of HIV infection (Table 2). Average HIV incidence rates were lower among women ≥30 years old than among women <20 years old (ratio of average incidence rates: 0.5, 95% CI: 0.3, 0.7), and this inverse relationship was robust to different categorizations of age (Table S3). HIV incidence appeared to have an inverted u-shaped association with calendar time (Figure S2). After adjusting for region and length of study, the average incidence rate for studies conducted after 2014 was 0.4 times the average rate for studies conducted prior to 2010 (95% CI: 0.2, 0.7). Incidence was also associated with study design. Average rates were highest among cross-sectional studies (4.7/100PY, 95% PI: 1.6, 13.5), followed by prospective cohort studies (3.4/100PY, 95% PI: 1.2, 9.4) and surveillance studies (2.2/100PY, 95% PI: 0.6, 7.4). Studies that defined the date of seroconversion as the date of the first positive HIV test observed higher incidence rates than studies that used a date between the last negative and first positive HIV test (ratio of average incidence rates: 4.3, 95% CI: 1.4, 13.2).
Table 2.
Stratified analysis and meta-regression of the incidence rate of HIV during pregnancy and breastfeeding
| Stratum Specific Estimates | Univariate Meta-Regression | Multivariate Meta-Regression* | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Number of Estimates | Pooled incidence rate | (95% PI) | Ratio of the pooled incidence rate | (95% CI) | P-value | Omnibus p-value | Ratio of the pooled incidence rate | (95% CI) | P-value | Omnibus p-value |
| Region | |||||||||||
| Southern Africa | 18 | 4.2 | (1.4, 12.3) | 1.0 | - | - | - | 1.0 | - | - | - |
| Eastern Africa | 10 | 3.3 | (1.1, 9.9) | 0.8 | (0.5, 1.2) | 0.3 | - | 0.7 | (0.4, 1.1) | 0.1 | - |
| Southeastern Africa | 3 | 2.4 | (0.7, 8.1) | 0.6 | (0.3, 1.1) | 0.1 | - | 0.9 | (0.3, 2.3) | 0.8 | - |
| Western Africa | 3 | 2.9 | (0.7, 11.5) | 0.7 | (0.3, 1.8) | 0.4 | 0.3 | 0.7 | (0.3, 1.8) | 0.4 | 0.4 |
| Calendar time† | |||||||||||
| Pre-2010 | 23 | 4.1 | (1.4, 12.2) | 1.0 | - | - | - | 1.0 | - | - | - |
| 2010–2014 | 8 | 2.9 | (0.9, 8.8) | 0.7 | (0.4, 1.2) | 0.2 | - | 0.7 | (0.4, 1.2) | 0.2 | - |
| Post-2014 | 4 | 2.1 | (0.7, 6.5) | 0.5 | (0.3, 0.9) | 0.02 | 0.04 | 0.4 | (0.2, 0.7) | 0.002 | 0.007 |
| High risk cohort | |||||||||||
| No | 32 | 3.6 | (1.2, 11.3) | 1.0 | - | - | - | 1.0 | - | - | - |
| Yes | 4 | 4.3 | (1.2, 15.9) | 1.2 | (0.5, 1.8) | 0.8 | 0.8 | 1.2 | (0.6, 2.5) | 0.3 | 0.3 |
| Participants enrolled in an HIV-prevention clinical trial | |||||||||||
| No | 29 | 3.5 | (1.2, 10.5) | 1.0 | - | - | - | 1.0 | - | - | - |
| Yes | 5 | 4.3 | (1.3, 14.2) | 1.2 | (0.6–2.4) | 0.6 | 0.6 | 1.9 | (0.9–4.1) | 0.2 | 0.2 |
| Age group | |||||||||||
| < 20 years | 7 | 3.8 | (1.5, 10.1) | 1.0 | - | - | - | 1.0 | - | - | - |
| 20–24 years | 6 | 2.8 | (1.1, 7.4) | 0.7 | (0.6, 1.0) | 0.05 | - | 0.7 | (0.5, 1.0) | 0.05 | - |
| 25–29 years | 5 | 2.5 | (0.9, 6.6) | 0.6 | (0.5, 0.9) | 0.01 | - | 0.6 | (0.4, 0.9) | 0.01 | - |
| 30+ years | 6 | 1.8 | (0.7, 4.8) | 0.5 | (0.3, 0.7) | <0.001 | <0.001 | 0.5 | (0.3, 0.7) | <0.001 | <0.001 |
| Undefined | 16 | - | - | - | - | - | - | - | - | - | - |
| Study Design | |||||||||||
| Prospective cohort | 21 | 3.4 | (1.2, 9.4) | 1.0 | - | - | - | 1.0 | - | - | - |
| Cross-sectional retesting | 11 | 4.7 | (1.6, 13.5) | 1.4 | (0.9, 2.1) | 0.1 | - | 1.8 | (1.0, 3.4) | 0.06 | - |
| Surveillance study | 2 | 2.2 | (0.6, 7.4) | 0.6 | (0.3, 1.4) | 0.2 | 0.1 | 0.9 | (0.3, 2.8) | 0.8 | 0.1 |
| Use of results from repeat HIV testing to identify HIV seroconversions | |||||||||||
| Yes | 30 | 3.7 | (1.3, 11.1) | 1.0 | - | - | - | 1.0 | - | - | - |
| No | 4 | 2.8 | (0.8, 9.4) | 0.8 | (0.4, 1.4) | 0.4 | 0.4 | 0.6 | (0.2, 1.6) | 0.3 | 0.3 |
| Reproductive periods observed during study follow-up | |||||||||||
| Pregnancy only | 11 | 4.3 | (1.4, 13.0) | 1.0 | - | - | - | 1.0 | - | - | - |
| Breastfeeding only | 5 | 3.8 | (1.2, 11.9) | 0.9 | (0.5, 1.6) | 0.7 | - | 0.9 | (0.4, 1.7) | 0.6 | - |
| Pregnancy and Breastfeeding | 10 | 3.8 | (1.2, 11.6) | 0.9 | (0.5, 1.5) | 0.7 | - | 0.7 | (0.4, 1.3) | 0.2 | - |
| Pregnancy, Breastfeeding, Non-Pregnant/Non-Breastfeeding | 8 | 2.7 | (0.9, 8.3) | 0.6 | (0.4, 1.1) | 0.1 | 0.4 | 0.6 | (0.3, 1.3) | 0.2 | 0.6 |
| Estimated timing of HIV seroconversion | |||||||||||
| Date between last negative and first positive HIV test | 11 | 2.6 | (0.9, 7.3) | 1.0 | - | - | - | 1.0 | - | - | - |
| Date of the first positive HIV test | 4 | 5.3 | (1.8, 16.1) | 2.0 | (1.1, 3.7) | 0.02 | 0.02 | 4.3 | (1.4, 13.2) | 0.01 | 0.01 |
| Undefined | 19 | - | - | - | - | - | - | - | - | - | - |
| HIV RNA/DNA PCR used in HIV testing algorithm | |||||||||||
| No | 21 | 4.2 | (1.5, 12.0) | 1.0 | - | - | - | 1.0 | - | - | - |
| Yes | 5 | 3.1 | (1.0, 9.5) | 0.7 | (0.4, 1.3) | 0.3 | 0.3 | 0.9 | (0.4, 2.1) | 0.8 | 0.8 |
| Undefined | 8 | - | - | - | - | - | - | - | - | - | - |
Acronyms: CI=confidence interval; HR=hazard ratio; PI=prediction interval
Unless otherwise indicated, models were adjusted for region, length of study implementation, and calendar time.
Multivariate meta-regression adjusted for region and length of study implementation only.
After stratifying by type of high-risk population, we observed higher estimated incidence rates among pregnant and breastfeeding women with known HIV-positive partners (n=2, [54, 58]) than rates estimated in a more general study population (ratio of average incidence rates: 4.7 95% CI: 2.2, 10.2; Table S4).
Pregnancy and HIV acquisition
Ten studies contributed estimates of the association between pregnancy and HIV acquisition. In four, non-pregnant, non-breastfeeding periods served as the referent [55, 56, 58, 59]; in six, non-pregnant periods (which included breastfeeding) were defined as the referent [57, 60–64]. There was variability definitions of “non-pregnant” and “non-pregnant/non-breastfeeding” due to heterogeneous definitions of pregnancy and breastfeeding (Table 1). All studies used methods that allowed women to contribute person-time to both exposed and unexposed periods.
The average HR estimating the association between pregnancy and risk of HIV acquisition was 0.9 (95% PI: 0.2 to 3.8; Figure S3). Although we observed statistical evidence of funnel plot asymmetry (p=0.05), results were largely unchanged after using a trim-and-fill analysis to impute one possibly missing result (average HR: 1.0, 95% PI: 0.3, 3.3). We also observed evidence of heterogeneity among study-specific estimates of the association (p<0.001), which was consistent with the wide 95% PI spanning the null. Stratified analyses and meta-regression revealed limited evidence of associations between the average HRs and the measured characteristics of contributing studies (Table 3). Two estimates were generated by studies with partially overlapping cohorts [61, 64]; exclusion of either did not change these results substantially (Tables S5 and S6).
Table 3.
Stratified analysis and meta-regression of the association between pregnancy and risk of HIV acquisition
| Stratum Specific Estimates | Univariate Meta-Regression Results | ||||||
|---|---|---|---|---|---|---|---|
| Variable | Number of Estimates | Pooled HR | (95% PI) | Ratio of the pooled HR | (95% CI) | P-value | Omnibus p-value |
| Region of Africa | |||||||
| Southern Africa | 4 | 0.8 | (0.2, 3.9) | 1.0 | - | - | - |
| Eastern Africa | 3 | 0.9 | (0.2, 4.8) | 1.1 | (0.3, 3.7) | 0.9 | - |
| Southeastern Africa | 3 | 0.9 | (0.2, 4.5) | 1.1 | (0.4, 3.3) | 0.9 | 1.0 |
| High risk cohort | |||||||
| No | 7 | 0.9 | (0.2, 3.5) | 1.0 | - | - | - |
| Yes | 3 | 0.8 | (0.2, 3.8) | 0.9 | (0.3, 2.6) | 0.8 | 0.8 |
| Participants enrolled in an HIV-prevention clinical trial | |||||||
| No | 6 | 0.7 | (0.2, 2.5) | 1.0 | - | - | - |
| Yes | 4 | 1.2 | (0.3, 4.4) | 1.7 | (0.7, 3.9) | 0.2 | 0.2 |
| Study design | |||||||
| Prospective cohort | 8 | 1.1 | (0.3, 3.4) | 1.0 | - | - | - |
| Surveillance study | 2 | 0.6 | (0.2, 2.3) | 0.6 | (0.2, 1.5) | 0.2 | 0.2 |
| Use of HIV RNA/DNA PCR in HIV testing algorithm | |||||||
| No | 5 | 1.1 | (0.3, 4.4) | 1.0 | - | - | - |
| Yes | 3 | 0.9 | (0.2, 3.8) | 0.8 | (0.3, 2.3) | 0.7 | 0.7 |
| Undefined | 2 | - | - | - | - | - | - |
| Estimated timing of HIV seroconversion | |||||||
| Date between last negative and first positive HIV test | 5 | 1.0 | (0.3, 3.3) | 1.0 | - | - | - |
| Date of the first positive HIV test | 3 | 1.0 | (0.3, 3.7) | 1.1 | (0.4, 2.7) | 0.9 | 0.9 |
| Undefined | 2 | - | - | - | - | - | - |
| Referent group | |||||||
| Not Pregnant | 6 | 0.8 | (0.2, 3.3) | 1.0 | - | - | - |
| Not Pregnant or Breastfeeding | 4 | 1.0 | (0.2, 4.4) | 1.2 | (0.5, 3.1) | 0.7 | 0.7 |
| Adjustment for confounders | |||||||
| Yes | 8 | 0.8 | (0.2, 2.8) | 1.0 | - | - | - |
| No | 2 | 1.3 | (0.3, 5.8) | 1.6 | (0.6, 4.6) | 0.4 | 0.4 |
| Adjusted for time-varying measures of condom use and intercourse frequency* | |||||||
| No | 5 | 0.7 | (0.2, 2.8) | 1.0 | - | - | - |
| Yes | 3 | 1.0 | (0.2, 4.1) | 1.3 | (0.5, 3.7) | 0.6 | 0.6 |
Acronyms: CI=confidence interval; HR=hazard ratio; PI=prediction interval
Only among studies that used adjusted models.
Breastfeeding and HIV acquisition
Four studies compared the risk of HIV acquisition during breastfeeding to risk during non-pregnant and non-breastfeeding periods. The average HR estimating the association between breastfeeding and risk of HIV acquisition was 1.0 (95% PI: 0.6 to 1.6; Figure S4). We did not observe statistical evidence of funnel plot asymmetry (p=0.2). Compared to estimates of the association between pregnancy and risk of HIV acquisition, estimates of the association between breastfeeding and risk of HIV acquisition were more tightly clustered around the null. We observed little evidence of heterogeneity between the study-specific HR estimates (p=0.6), and our analyses revealed limited evidence of associations between the average HRs and the measured characteristics of contributing studies (Table 4).
Table 4.
Stratified analysis and meta-regression of the association between breastfeeding and risk of HIV acquisition
| Stratum Specific Estimates† | Univariate Meta-Regression Results‡ | ||||||
|---|---|---|---|---|---|---|---|
| Variable* | Number of Estimates | Pooled HR | (95% PI) | Ratio of the pooled HR | (95% CI) | P-value | Omnibus p-value |
| Region of Africa | |||||||
| Southeastern Africa | 2 | 0.9 | (0.8, 1.0) | - | - | - | - |
| Eastern Africa | 1 | 1.1 | NA | NA | NA | NA | NA |
| Southern Africa | 1 | 1.2 | NA | NA | NA | NA | NA |
| Study design | |||||||
| Prospective cohort | 2 | 1.1 | (0.9, 1.5) | - | - | - | - |
| Surveillance study | 2 | 0.9 | (0.8, 1.0) | 0.8 | (0.6, 1.1) | 0.2 | 0.2 |
| Estimated timing of HIV seroconversion | |||||||
| Date between last negative and first positive HIV test | 3 | 1.0 | (0.9, 1.1) | - | - | - | - |
| Date of the first positive HIV test | 1 | 1.1 | NA | NA | NA | NA | NA |
Acronyms: CI=confidence interval; HR=hazard ratio; PI=prediction interval
There was limited variability in the population and methodological features of included studies. All estimates were adjusted for confounders and generated by studies that used “not pregnant, not breastfeeding” as the referent group. No estimates were generated among a high-risk population or among a population enrolled in an HIV-prevention clinical trial. Only prospective cohort studies adjusted for time-varying sexual behaviors.
95% PI computed only when the number of estimates in the strata exceeds 1
Meta-regression computed only when the number of estimates exceeded 1 in the comparison group and in the referent stratum.
Discussion
In this meta-analysis update—which included 15 new studies and over 77,000 additional PY of follow-up—the estimated average HIV incidence rate among pregnant and breastfeeding women was above the “substantial risk” threshold described by the WHO [3], while the estimated average associations between pregnancy and risk of HIV acquisition, and breastfeeding and risk of HIV acquisition, were close to the null. Prediction intervals around each of our summary estimates were wide, highlighting the variability of HIV incidence across populations of pregnant and breastfeeding women in SSA.
Our results were consistent with findings from a previous meta-analysis that reported high average HIV incidence during pregnancy and breastfeeding [2]. Hormonal changes during pregnancy may increase susceptibility to HIV through changes in the vaginal epithelial thickness, microbiome, and CCR5 coreceptor expression [65, 66]. Pregnancy activates the innate immune system, increasing inflammation and concentration of dendritic cells in the female genital tract, while suppressing the adaptive immune response [67, 68]. Such immunologic changes may increase risk of HIV acquisition [69–71], and can last for several months postpartum [72, 73]. Behavioral changes occurring during pregnancy may also influence risk of HIV acquisition. Couples may be more likely to engage in unprotected sex during pregnancy [34, 58, 74], and male partners may be more likely to seek extra-partnership sexual liaisons during extended periods of pregnancy- or breastfeeding-related abstinence [34, 75–77].
Substantial heterogeneity of the incidence rates, however, cautions us from interpreting the average HIV incidence rate estimated in this study as the incidence rate among pregnant and breastfeeding women in SSA. Our results suggest maternal HIV incidence rates may lower among older compared to younger pregnant and breastfeeding women, and higher among women in HIV serodiscordant relationships. Additionally, we observed changes in average HIV incidence over calendar time that follow temporal trends observed in the region since the 1980s: a steady rise in HIV incidence until the early 2000s [78], largely driven by increasing HIV prevalence without viral suppression [79], followed by a slow decline that may be attributed to expanded HIV testing and counseling, medical male circumcision, and ART services. Inverted u-shaped trends in HIV incidence over time have been observed in large population-based cohorts in in SSA [10–12], with the latter two studies reporting associations between HIV incidence and community-level coverage of ART and medical male circumcision. Models predict that integrated behavioral and biomedical interventions will reduce HIV incidence generally [80, 81], and among pregnant women specifically [82], and cluster randomized trials of combination HIV prevention with universal ART demonstrated some reductions in community-wide HIV incidence [83, 84]. While we expect that HIV-negative pregnant and breastfeeding women may serve as beneficiaries of expanded combination HIV prevention, impact will likely across sub-groups.
Prediction intervals around overall, and stratum-specific, estimates of the average associations between pregnancy and risk of HIV acquisition and between breastfeeding and risk of HIV acquisition, were wide with lower and upper bounds on either side of the null. This variability is not unexpected; pregnancy and breastfeeding are periods marked by significant biological and behavioral changes that may have different effects on risk of HIV. For example, the potential increased risk of HIV arising from the pregnancy-induced physiological changes described earlier may be offset by a reduction in sexual intercourse that frequently occurs during late pregnancy and early breastfeeding [34, 54, 58, 74]. The direction of the observed association between pregnancy or breastfeeding and risk of HIV acquisition may therefore depend on both study context and analytical decisions regarding covariate measurement and adjustment [85]. Furthermore, as the physiological and behavioral changes that accompany pregnancy and breastfeeding are dynamic, decisions regarding how to define pregnancy, breastfeeding, and the referent state may influence the direction of the observed association. For example, the inclusion of breastfeeding in the referent group may produce estimates closer to the null since incidence rates during breastfeeding appear similar to those during pregnancy [2], while single categories for pregnancy and breastfeeding may obscure periods during pregnancy or breastfeeding when risk is truly elevated or suppressed. Work by Thomson et al. suggests that physiological changes during pregnancy increase susceptibility to HIV, particularly in late pregnancy and early breastfeeding [54]. However, additional work is needed to better understand the interaction between biological susceptibility and behavioral changes on risk of HIV acquisition among pregnant and breastfeeding women in different contexts around SSA.
Our results should be interpreted in light of possible limitations. It is unclear if contributing studies enrolled representative cohorts of women, so the extent to which our estimates generalize to all pregnant and breastfeeding women in SSA is unknown. It is possible that investigators targeted clinics in areas of elevated HIV incidence, which may bias estimates of incidence upwards. Few estimates of the incidence rate captured the first trimester of pregnancy and, given the variability of risk over the course of pregnancy [54, 58, 62], this may bias estimates of incidence. The directionality of this bias is unclear; two studies report higher incidence during early compared to late pregnancy [58, 62], while one reports the reverse [54]. For this reason, misclassification of early or late pregnancy-exposed periods as non-pregnant person-time may also bias estimates of the association in unknown directions. Finally, our analyses were restricted by the number of studies and the information provided by each study. The small number of estimates may have limited our power to detect associations between estimates and underlying sources of heterogeneity. Differences in populations and methodological features of contributing studies may not have been adequately captured by variables used in meta-regression models, and several important population features were unmeasured by contributing studies.
Although many countries in SSA have placed considerable focus on identifying and treating HIV-infected pregnant and breastfeeding women, HIV-uninfected women have received considerably less attention in antenatal and postnatal settings. Our results support the expansion of bio-behavioral HIV prevention interventions and repeat testing throughout pregnancy and breastfeeding to women at high risk of HIV acquisition. Further work is needed to identify risk factors for HIV acquisition during pregnancy and breastfeeding to facilitate targeted prevention interventions in antenatal and postnatal settings. Offering female-controlled strategies, such as tenofovir-based oral pre-exposure prophylaxis, and promoting couples-based prevention approaches in these settings, are important next steps that may reduce the risk of HIV-related maternal morbidity and mortality, and ensure continued progress towards the elimination of mother-to-child transmission of HIV.
Supplementary Material
Acknowledgements
This study was supported in part by the National Institutes of Health (R01 AI131060, R00 MH104154, K24 AI120796, P30 AI050410, D43 TW009340).
Abbreviations
- ART
antiretroviral therapy
- CI
confidence interval
- HIV
human immunodeficiency virus
- HR
hazard ratio
- IRR
incidence rate ratio
- PCR
polymerase chain reaction
- PI
prediction interval
- PY
person-years
- SSA
sub-Saharan Africa
- WHO
World Health Organization
Footnotes
Conflict of Interest Statement: We declare no competing interests.
Disclaimer: The funders of this study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
References
- 1.Johnson LF, Stinson K, Newell ML, Bland RM, Moultrie H, Davies MA, et al. The contribution of maternal HIV seroconversion during late pregnancy and breastfeeding to mother-to-child transmission of HIV. JAIDS 2012; 59(4):417–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Drake AL, Wagner A, Richardson B, John-Stewart G. Incident HIV during pregnancy and postpartum and risk of mother-to-child HIV transmission: a systematic review and meta-analysis. PLoS Med 2014; 11(2):e1001608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO). Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection: Recommendations for a public health approach. In. 2 ed. Geneva, Switzerland: WHO; 2016. [PubMed] [Google Scholar]
- 4.World Health Organization (WHO). Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. In. Geneva, Switzerland: WHO; 2013. [PubMed] [Google Scholar]
- 5.World Health Organization (WHO). Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV. In. Geneva, Switzerland: WHO; 2015. [PubMed] [Google Scholar]
- 6.World Health Organization (WHO). Global update on the health sector response to HIV, 2014. In. Geneva, Switzerland: WHO; 2014. [Google Scholar]
- 7.Joint United Nations Programme on HIV/AIDS (UNAIDS). Prevention Gap Report. In. Geneva, Switzerland: UNAIDS; 2016. [Google Scholar]
- 8.World Health Organization (WHO). Treat all: Policy adoption and implementation status in countries. In. Geneva, Switzerland: WHO; 2017. [Google Scholar]
- 9.Joint United Nations Programme on HIV/AIDS (UNAIDS). UNAIDS Data 2018. In. Geneva, Switzerland: UNAIDS; 2018. [Google Scholar]
- 10.Borgdorff MW, Kwaro D, Obor D, Otieno G, Kamire V, Odongo F, et al. HIV incidence in western Kenya during scale-up of antiretroviral therapy and voluntary medical male circumcision: a population-based cohort analysis. The lancet HIV 2018; 5(5):e241–e249. [DOI] [PubMed] [Google Scholar]
- 11.Vandormael A, Akullian A, Siedner M, de Oliveira T, Bärnighausen T, Tanser F. Declines in HIV incidence among men and women in a South African population-based cohort. Nat Commun 2019; 10(1):5482–5482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grabowski MK, Serwadda DM, Gray RH, Nakigozi G, Kigozi G, Kagaayi J, et al. HIV Prevention Efforts and Incidence of HIV in Uganda. N Engl J Med 2017; 377(22):2154–2166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fatti G, Grimwood A, Egbujie B, Mothibi E, Shaikh N, Jackson D, et al. Low HIV incidence in South African pregnant women receiving a prevention intervention. Topics in Antiviral Medicine 2017; 25(1):324s–325s. [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6(7):e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization (WHO). Infant and young child feeding. In. Geneva, Switzerland: WHO; 2018. [Google Scholar]
- 16.Higgins JPT, Thompson SG, Spiegelhalter DJ. A re-evaluation of random-effects meta-analysis. J R Stat Soc Ser A Stat Soc 2009; 172(1):137–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Riley RD, Higgins JPT, Deeks JJ. Interpretation of random effects meta-analyses. BMJ 2011; 342:d549. [DOI] [PubMed] [Google Scholar]
- 18.IntHout J, Ioannidis JPA, Rovers MM, Goeman JJ. Plea for routinely presenting prediction intervals in meta-analysis. BMJ open 2016; 6(7):e010247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hernan MA. The hazards of hazard ratios. Epidemiology 2010; 21(1):13–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.VanderWeele TJ. Unmeasured confounding and hazard scales: sensitivity analysis for total, direct, and indirect effects. Eur J Epidemiol 2013; 28(2):113–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000; 56(2):455–463. [DOI] [PubMed] [Google Scholar]
- 22.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997; 315(7109):629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Greenland S, O’Rourke K. On the bias produced by quality scores in meta-analysis, and a hierarchical view of proposed solutions. Biostatistics 2001; 2(4):463–471. [DOI] [PubMed] [Google Scholar]
- 24.Jüni P, Witschi A, Bloch R, Egger M. The Hazards of Scoring the Quality of Clinical Trials for Meta-analysis. JAMA 1999; 282(11):1054–1060. [DOI] [PubMed] [Google Scholar]
- 25.Tipton E Small sample adjustments for robust variance estimation with meta-regression. Psychol Methods 2015; 20(3):375–393. [DOI] [PubMed] [Google Scholar]
- 26.Viechtbauer W Conducting Meta-Analyses in R with the metafor Package. J Stat Softw 2010; 39(3):1–48. [Google Scholar]
- 27.World Health Organization (WHO). Antiretroviral therapy for HIV infection in adults and adolescents: recommendations for a public health approach - 2010 revision. In. Geneva, Switzerland: WHO; 2010. [PubMed] [Google Scholar]
- 28.World Health Organization (WHO). Guidance on couples HIV testing and counseling including antiretroviral therapy for treatment and prevention in serodiscordant couples: recommendations for a public health approach. In. Geneva, Switzerland: WHO; 2012. [PubMed] [Google Scholar]
- 29.De Schacht C, Hoffman HJ, Mabunda N, Lucas C, Alons CL, Madonela A, et al. High rates of HIV seroconversion in pregnant women and low reported levels of HIV testing among male partners in Southern Mozambique: results from a mixed methods study. PloS One 2014; 9(12):e115014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.De Schacht C, Mabunda N, Ferreira OC Jr, Ismael N, Calú N, Santos I, et al. High HIV incidence in the postpartum period sustains vertical transmission in settings with generalized epidemics: A cohort study in Southern Mozambique. J Int AIDS Soc 2014; 17:18808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Egbe TO, Tazinya RM, Halle-Ekane GE, Egbe EN, Achidi EA. Estimating HIV Incidence during Pregnancy and Knowledge of Prevention of Mother-to-Child Transmission with an Ad Hoc Analysis of Potential Cofactors. J Pregnancy 2016; 2016:7397695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Humphrey JH, Hargrove JW, Malaba LC, Iliff PJ, Moulton LH, Mutasa K, et al. HIV incidence among post-partum women in Zimbabwe: risk factors and the effect of vitamin A supplementation. AIDS 2006; 20(10):1437–1446. [DOI] [PubMed] [Google Scholar]
- 33.Imade GE, Sagay AS, Musa J, Ocheke AN, Adeniyi DS, Idighri M, et al. Declining rate of infection with maternal human immunodeficiency virus at delivery units in north-central Nigeria. Afr J Reprod Health 2013; 17(4):138–145. [PubMed] [Google Scholar]
- 34.Keating MA, Hamela G, Miller WC, Moses A, Hoffman IF, Hosseinipour MC. High HIV incidence and sexual behavior change among pregnant women in Lilongwe, Malawi: implications for the risk of HIV acquisition. PloS One 2012; 7(6):e39109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kieffer MP, Nhlabatsi B, Mahdi M, Hoffman HJ, Kudiabor K, Wilfert CM. Improved detection of incident HIV infection and uptake of PMTCT services in labor and delivery in a high HIV prevalence setting. J Acquir Immune Defic Syndr 2011; 57(4):e85–91. [DOI] [PubMed] [Google Scholar]
- 36.Kinuthia J, Kiarie JN, Farquhar C, Richardson B, Nduati R, Mbori-Ngacha D, et al. Cofactors for HIV-1 incidence during pregnancy and postpartum period. Curr HIV Res 2010; 8(7):510–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kinuthia J, Drake AL, Matemo D, Richardson BA, Zeh C, Osborn L, et al. HIV acquisition during pregnancy and postpartum is associated with genital infections and partnership characteristics. AIDS 2015; 29(15):2025–2033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leroy V, Van De Perre P, Lepage P, Saba J, Nsengumuremyi F, Simonon A, et al. Seroincidence of HIV-1 infection in African women of reproductive age: A prospective cohort study in Kigali, Rwanda, 1988–1992. AIDS 1994; 8(7):983–986. [DOI] [PubMed] [Google Scholar]
- 39.Mbizvo MT, Kasule J, Mahomed K, Nathoo K. HIV-1 seroconversion incidence following pregnancy and delivery among women seronegative at recruitment in Harare, Zimbabwe. Cent Afr J Med 2001; 47(5):115–118. [DOI] [PubMed] [Google Scholar]
- 40.Miotti P, Canner J, Chiphangwi J, Liomba G, Saah A, Dallabetta G. Preparations for AIDS vaccine evaluations. Rate of new HIV infection in a cohort of women of childbearing age in Malawi. AIDS Res Hum Retroviruses 1994; 10 Suppl 2:S239–241. [PubMed] [Google Scholar]
- 41.Moodley D, Esterhuizen TM, Pather T, Chetty V, Ngaleka L. High HIV incidence during pregnancy: compelling reason for repeat HIV testing. AIDS 2009; 23(10):1255–1259. [DOI] [PubMed] [Google Scholar]
- 42.Moodley D, Esterhuizen T, Reddy L, Moodley P, Singh B, Ngaleka L, et al. Incident HIV infection in pregnant and lactating women and its effect on mother-to-child transmission in South Africa. J Infect Dis 2011; 203(9):1231–1234. [DOI] [PubMed] [Google Scholar]
- 43.Moodley D, Moodley P, Sebitloane M, Soowamber D, McNaughton-Reyes HL, Groves AK, et al. High prevalence and incidence of asymptomatic sexually transmitted infections during pregnancy and postdelivery in KwaZulu Natal, South Africa. Sex Transm Dis 2015; 42(1):43–47. [DOI] [PubMed] [Google Scholar]
- 44.Munjoma MW, Mhlanga FG, Mapingure MP, Kurewa EN, Mashavave GV, Chirenje MZ, et al. The incidence of HIV among women recruited during late pregnancy and followed up for six years after childbirth in Zimbabwe. BMC Public Health 2010; 10:668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nikuze A, Wanjala S, Ben-Farhat J, Omwoyo W, Oyiengo L, Szumilin E, et al. HIV incidence, cascade, and testing among mothers in Western Kenya. In: 24th Conference on Retroviruses and Opportunistic Infections. Seattle, United States: CROI 2017; 2017. [Google Scholar]
- 46.Rogers AJ, Akama E, Weke E, Blackburn J, Owino G, Bukusi EA, et al. Implementation of repeat HIV testing during pregnancy in southwestern Kenya: progress and missed opportunities. J Int AIDS Soc 2017; 20(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tabu F, Ngonzi J, Mugyenyi G, Bajunirwe F, Mayanja R, Morten S. Prevalence of HIV infection among parturients with a negative primary test during the antenatal period at Mbarara Regional Referral Hospital, Uganda. BJOG 2013; 120:13. [Google Scholar]
- 48.Taha TE, Dallabetta GA, Hoover DR, Chiphangwi JD, Mtimavalye LAR, Liomba GN, et al. Trends of HIV-1 and sexually transmitted diseases among pregnant and postpartum women in urban Malawi. AIDS 1998; 12(2):197–203. [DOI] [PubMed] [Google Scholar]
- 49.Traore C Evaluation of HIV incidence during pregnancy in Ouagadougou, Burkina Faso. In: 19th International AIDS Conference Washington DC, United States: International AIDS Society; 2012. [Google Scholar]
- 50.Van de Perre P, Hitimana DG, Simonon A, Dabis F, Msellati P, E. K, et al. Postnatal transmission of HIV-1 associated with breast abscess. Lancet 1992; 339:1490–1491. [DOI] [PubMed] [Google Scholar]
- 51.Phiri S, Manda E, Tweya H, Rosenberg N, Gugsa S, Chiwoko J, et al. Comparison of HIV testing yield rates for pregnant and lactating women towards zero new paediatric HIV infection: Experiences from Bwaila District Hospital, Lilongwe, Malawi. In: 21st International AIDS Conference Durban, South Africa: International AIDS Society; 2016. [Google Scholar]
- 52.Mepham S, Bland R, Ndirangu J, Newell ML. HIV incidence and associated socio-economic factors in a prospective cohort of pregnant women in rural, northern KwaZulu-Natal, South Africa. In: 5th International AIDS Society Conference on HIV Pathogenesis, Treatment, and Prevention Cape Town, South Africa: International AIDS Society; 2009. [Google Scholar]
- 53.John F, Chung M, Kinuthia J, Richardson B, Farquhar C, John-Stewart G, et al. HIV-1 incidence after antenatal counselling and testing. In: 16th International AIDS Conference Toronto, Canada: International AIDS Society; 2006. [Google Scholar]
- 54.Thomson KA, Hughes J, Baeten JM, John-Stewart G, Celum C, Cohen CR, et al. Increased Risk of HIV Acquisition Among Women Throughout Pregnancy and During the Postpartum Period: A Prospective Per-Coital-Act Analysis Among Women With HIV-Infected Partners. J Infect Dis 2018; 218(1):16–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chetty T, Vandormael A, Thorne C, Coutsoudis A. Incident HIV during pregnancy and early postpartum period: a population-based cohort study in a rural area in KwaZulu-Natal, South Africa. BMC Pregnancy Childbirth 2017; 17(1):248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Marston M, Newell ML, Crampin A, Lutalo T, Musoke R, Gregson S, et al. Is the risk of HIV acquisition increased during and immediately after pregnancy? A secondary analysis of pooled HIV community-based studies from the ALPHA network. PloS One 2013; 8(12):e82219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Braunstein SL, Ingabire CM, Kestelyn E, Uwizera AU, Mwamarangwe L, Ntirushwa J, et al. High human immunodeficiency virus incidence in a cohort of Rwandan female sex workers. Sex Transm Dis 2011; 38(5):385–394. [DOI] [PubMed] [Google Scholar]
- 58.Gray RH, Li X, Kigozi G, Serwadda D, Brahmbhatt H, Wabwire-Mangen F, et al. Increased risk of incident HIV during pregnancy in Rakai, Uganda: a prospective study. Lancet 2005; 366(9492):1182–1188. [DOI] [PubMed] [Google Scholar]
- 59.Morrison CS, Wang J, Van Der Pol B, Padian N, Salata RA, Richardson BA. Pregnancy and the risk of HIV-1 acquisition among women in Uganda and Zimbabwe. AIDS 2007; 21(8):1027–1034. [DOI] [PubMed] [Google Scholar]
- 60.Reid SE, Dai JY, Wang J, Sichalwe BN, Akpomiemie G, Cowan FM, et al. Pregnancy, contraceptive use, and HIV acquisition in HPTN 039: relevance for HIV prevention trials among African women. J Acquir Immune Defic Syndr 2010; 53(5):606–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Teasdale CA, Abrams EJ, Chiasson MA, Justman J, Blanchard K, Jones HE. Incidence of sexually transmitted infections during pregnancy. PloS One 2018; 13(5):e0197696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mugo NR, Heffron R, Donnell D, Wald A, Were EO, Rees H, et al. Increased risk of HIV-1 transmission in pregnancy: a prospective study among African HIV-1-serodiscordant couples. AIDS 2011; 25(15):1887–1895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vandepitte J, Weiss HA, Bukenya J, Nakubulwa S, Mayanja Y, Matovu G, et al. Alcohol use, mycoplasma genitalium, and other STIs associated With HIV incidence among women at high risk in Kampala, Uganda. J Acquir Immune Defic Syndr 2013; 62(1):119–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wand H, Ramjee G. Combined impact of sexual risk behaviors for HIV seroconversion among women in Durban, South Africa: implications for prevention policy and planning. AIDS Behav 2011; 15(2):479–486. [DOI] [PubMed] [Google Scholar]
- 65.Sheffield JS, Wendel GD Jr., McIntire DD, Norgard MV. The effect of progesterone levels and pregnancy on HIV-1 coreceptor expression. Reprod Sci 2009; 16(1):20–31. [DOI] [PubMed] [Google Scholar]
- 66.Hapgood JP, Kaushic C, Hel Z. Hormonal Contraception and HIV-1 Acquisition: Biological Mechanisms. Endocr Rev 2018; 39(1):36–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kourtis AP, Read JS, Jamieson DJ. Pregnancy and infection. N Engl J Med 2014; 370(23):2211–2218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Robinson DP, Klein SL. Pregnancy and pregnancy-associated hormones alter immune responses and disease pathogenesis. Horm Behav 2012; 62(3):263–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Asin SN, Eszterhas SK, Rollenhagen C, Heimberg AM, Howell AL. HIV type 1 infection in women: increased transcription of HIV type 1 in ectocervical tissue explants. J Infect Dis 2009; 200(6):965–972. [DOI] [PubMed] [Google Scholar]
- 70.Masson L, Passmore JA, Liebenberg LJ, Werner L, Baxter C, Arnold KB, et al. Genital inflammation and the risk of HIV acquisition in women. Clin Infect Dis 2015; 61(2):260–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kahle EM, Bolton M, Hughes JP, Donnell D, Celum C, Lingappa JR, et al. Plasma cytokine levels and risk of HIV type 1 (HIV-1) transmission and acquisition: a nested case-control study among HIV-1-serodiscordant couples. J Infect Dis 2015; 211(9):1451–1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Groer MW, El-Badri N, Djeu J, Williams SN, Kane B, Szekeres K. Suppression of natural killer cell cytotoxicity in postpartum women: time course and potential mechanisms. Biol Res Nurs 2014; 16(3):320–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Groer ME, Jevitt C, Ji M. Immune changes and dysphoric moods across the postpartum. Am J Reprod Immunol 2015; 73(3):193–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Teasdale CA, Abrams EJ, Chiasson MA, Justman J, Blanchard K, Jones HE. Sexual Risk and Intravaginal Practice Behavior Changes During Pregnancy. Arch Sex Behav 2017; 46(2):539–548. [DOI] [PubMed] [Google Scholar]
- 75.Onah HE, Iloabachie GC, Obi SN, Ezugwu FO, Eze JN. Nigerian male sexual activity during pregnancy. Int J Gynaecol Obstet 2002; 76(2):219–223. [DOI] [PubMed] [Google Scholar]
- 76.Lawoyin TO, Larsen U. Male sexual behaviour during wife’s pregnancy and postpartum abstinence period in Oyo State, Nigeria. J Biosoc Sci 2002; 34(1):51–63. [PubMed] [Google Scholar]
- 77.Awusabo-Asare K, Anarfi JK. Postpartum sexual abstinence in the era of AIDS in Ghana: prospects for change. Health Transit Rev 1997; 7 Suppl:257–270. [PubMed] [Google Scholar]
- 78.Collaborators GH. Estimates of global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2015: the Global Burden of Disease Study 2015. The lancet HIV 2016; 3(8):e361–e387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tanser F, Bärnighausen T, Grapsa E, Zaidi J, Newell M-L. High coverage of ART associated with decline in risk of HIV acquisition in rural KwaZulu-Natal, South Africa. Science 2013; 339(6122):966–971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Anderson SJ, Cherutich P, Kilonzo N, Cremin I, Fecht D, Kimanga D, et al. Maximising the effect of combination HIV prevention through prioritisation of the people and places in greatest need: a modelling study. Lancet 2014; 384(9939):249–256. [DOI] [PubMed] [Google Scholar]
- 81.Jones A, Cremin I, Abdullah F, Idoko J, Cherutich P, Kilonzo N, et al. Transformation of HIV from pandemic to low-endemic levels: a public health approach to combination prevention. Lancet 2014; 384(9939):272–279. [DOI] [PubMed] [Google Scholar]
- 82.Powers KA, Orroth K, Rosenberg NE, Graybill LA, Kumwenda A, Mtande T, et al. A mathematical modeling analysis of combination HIV prevention in antenatnal clinics. In: 26th Conference on Retroviruses and Opportunistic Infections Seattle, United States: CROI 2019; 2019. [Google Scholar]
- 83.Makhema MJ, Wirth K, Pretorius Holme M, Gaolathe T, Mmalane M, Kadima E, et al. Impact of prevention and treatment interventions on population HIV incidence: Primary results of the community-randomized Ya Tsie Botswana prevention project. J Int AIDS Soc 2018; 21(S6):e25148.30051631 [Google Scholar]
- 84.Hayes R, Donnell D, Floyd S, Mandla N, Bwalya J, Sabapathy K, et al. Effect of Universal Testing and Treatment on HIV Incidence - HPTN 071 (PopART). N Engl J Med 2019; 381(3):207–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Rothman K, Greenland S, Lash T. Modern Epidemiology, 3rd Edition. Philadelphia, PA: Lippincott Williams & Wilkins; 2008. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.