Abstract
The aging-associated decline of biological functions represents an important contributor to the increase in morbidity and mortality of human beings. Of these biological functions deterioration; there is a significant decline in the heart function, impairments in the lungs gas exchange, and impairments in the immune function. Many alterations in the body humeral and cellular immune response were observed with ageing process: The circulating pro-inflammatory cytokines are increased, the naive lymphocytes are decreased, the numbers of the antigen-presenting cells areelevated and the overall response is impaired.
In addition, ageing is associated with a progressive restriction in the telomere length. Telomeres are located at chromosomes ends and play an essential role in preserving chromosome stability. Also, telomere length is very important to the immune system, because of the high sensitivity of the immune cells to the shortening of telomeres. Telomeres shortening adversely affect the immune cells’ function and developments. These adverse changes increased the susceptibility for severe infection, risk of hospitalization, and even death.
Elderly COVID-19 patients are at a real risk of complications due to impaired immune function, cytokine storm and defective respiratory function. Administration of anti-ageing immunomodulation factors like Nicotinamide Adenine Dinucleotide NAD+ can minimize these changes through its potent immunomodulation and longevity effects. NAD+ has a direct inhibitory effect on PARP-1 and can prevent pro-inflammatory cytokines over-activation. Increasing the NAD+ level will also result in stabilizing telomeres and this has a positive impact on immune cells function.
Keywords: COVID-19, NAD+, Telomeres, Cytokine storm, Ageing
Introduction
COVID-19 is a viral infection with an outbreak started in China at end of December 2019, and then declared a pandemic in March 2020 by world health Organization (WHO). It is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. Coronaviruses are a large family of viruses that can cause infections with a wide range of severity. The severe types may often associate with immune-inflammatory injury, in which the level of oxidative stress increases significantly [2].
SARS-CoV-2 is the seventh coronavirus known to infect humans; severe acute respiratory syndrome coronavirus (SARS-CoV), Middle East respiratory syndrome coronavirus (MERS-CoV), and SARS-CoV-2 can result into severe or even fatal illnesses, whereas HKU1, NL63, OC43 and 229E are frequently associated with mild symptoms [2]. SARS-CoV-2 is primarily transmitted through respiratory droplets. But a person can additionally be affected by contact with objects that affected person (not necessarily symptomatic) have touched. Moreover, COVID-19 infection may lead to intestinal infection and be present in faeces [3,4].
The present virus, SARS-CoV-2, is highly infectious and caused a pandemic infection within three months from its primary outbreak. In the majority of cases, patients present with typical respiratory symptoms (fever, cough, and myalgia or fatigue) [5]. However, diarrhea may be a presenting feature in some patients which often linked to delay diagnosis and a fatal outcome [6]. In severe cases of COVID 19, the patient develops severe respiratory distress (respiratory rate >30 breaths/min), RNAaemia, secondary bacterial infection, and/or acute cardiac injury [5]. Individuals at extreme risk for severe illness include people aged over 60 years and those with chronic health problems like diabetes, chronic respiratory disease, hypertension, and cancer [7].
The COVID-19 immune response
SARS-CoV-2 likewise SARS-CoV, uses the envelope spike (S) glycoprotein binding to the angiotensin-converting enzyme 2 (ACE2) as a receptor to enter the cells [8,9]. The S protein of SARS-CoV-2 binds weakly to ACE2 compare to SARS-CoV, this weak binds of SARS-CoV-2 results in less severe diseases than SARS-CoV [10]. ACE2 represents a type I transmembranemetallocarboxypeptidase with homology to ACE, a key enzyme in the Renin-Angiotensin system RAS [11]. These receptors are expressed in vascular endothelial cells [12], lung [13], kidney, and gastrointestinal tract [14]. SARS-CoV2 can induce the production of double-membrane vesicles. These vesicles lack pathogen-associated molecular patterns and then replicate in these vesicles, thereby avoiding the host detection of their dsRNA [1].
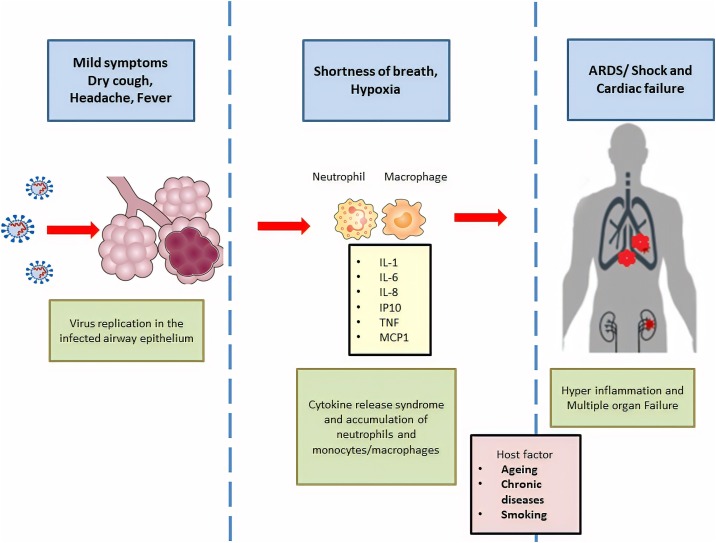
When the virus enters the cells, its antigen will be presented to the antigen-presenting cells (APCs), with successive activation of the body’s humoral and cellular immunity [1]. Patients affected by COVID-19 virus showed higher leukocyte count but lymphocytopenia. The number of CD4+ and CD8+ T cells significantly is reduced [15]. Despite their excessive activation, as evidenced by substantial proportions of HLA-DR (CD4 3.47%) and CD38 (CD8 39.4%) double-positive fractions [15]. Moreover, viral replication activates interferon regulatory factors (IRFs) and TLR-3-induced NF‐κB pathway; which increases the production of proinflammatory cytokines and cytokine storm. The abnormal immune response caused by the SARS-CoV-2 virus has to be mediated by leukocytes other than T cells [16]. The excessive release of cytokines like IFN-α and IFN-γ and chemokines results in a cytokine storm with a deadly inflammatory response [[17], [18], [19]]. The cytokine storm will trigger an intense systemic immune reaction, causes acute respiratory distress syndrome ARDS, acute cardiac injury, and multiple organ failure, which lead to death in severe cases of SARS-CoV-2 infection, similar to what occurs in SARS-CoV and MERS-CoV infection [15,17] (Fig. 1 ).
Fig. 1.
COVID-19 caused by SARS-CoV-2 virus, leads to activation of innate immune cells, especially in patients developing severe disease and ARDS. levels of many pro-inflammatory effector cytokines, such as TNF, IL-1β, IL-6, and IL-8, as well as chemokines, such as MCP1, and IP10, are elevated, reflecting innate immune activation in patients with COVID-19, with higher levels in those who are critically ill.
Many elderly patients developed an uncontrolled immune response to COVID-19 [5]. The Ageing-associated disturbance in immune cells and increase in the proinflammatory cytokines (TNF‐α and IL‐6) makes elderly people more vulnerable to severe airway inflammation, with a following uncontrolled systemic inflammatory response [20].
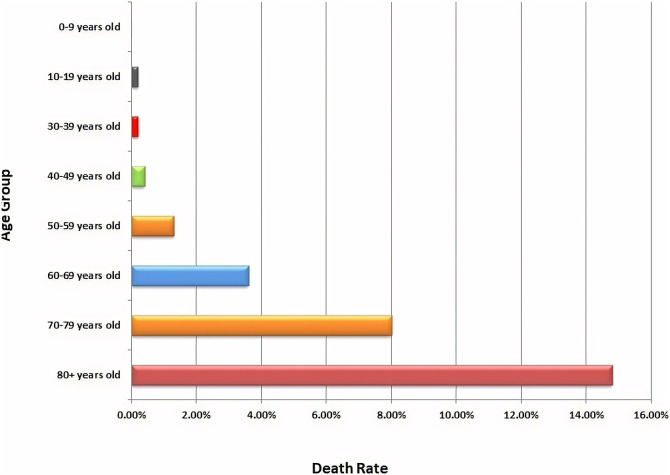
The disease burden in elderly
Despite the immaturity of children’s immune system, COVID-19 in children appears to be relatively rare and mild with approximately 2.4% of the total reported cases are among individuals aged less than 19 years. Of those less than 19 years, only (2.5%) developed severe disease, and (0.2%) suffered from the critical one [6]. Recent studies conducted in China [6], Italy [21], and USA [21] concluded that increased age of COVID-19 patients is associated with an increasing death rate and death rate of 80 years and above is passing 14% (Fig. 2 ).
Fig. 2.
Death rate by age for COVID 19 recorded cases.
Source: Worldmeter, 30 March 2020.
The variation in COVID-19 deaths among the different age groups, can suggest either immunosenescence or epigenetic factors. Immunosenescence is defined as “an age-related dysfunction of the immune system which leads to enhance the risk of infection” [22] because of Immunosenescence, elderly people are more susceptible to Viral infections whether they live in the community or long-term care facilities due to altering immune function [23].
The ageing effect on the immune response
Many physiological changes occur with ageing, such as the decline in the cardiac output, impairments in the lungs’ gas exchange, and impairments in the immune function [24,25]. These changes are often associated with progressive homeostatic instability and vulnerability to infections [[24], [25], [26]]. Ageing is also marked by many alterations in the innate and adaptive immune responses [27,28]. Two main changes are common with respect to T cell subpopulations: a decrease in naïve T cells that leads to the shrinking of the TCR repertoire and an increase in memory T cells that is primed by different aggressors [28,29]. Therefore, the ability of the human immune system to protect against infectious disease declines with age, and efficacy of vaccination reduces significantly in the elderly [28].
Immunopathology in elderly
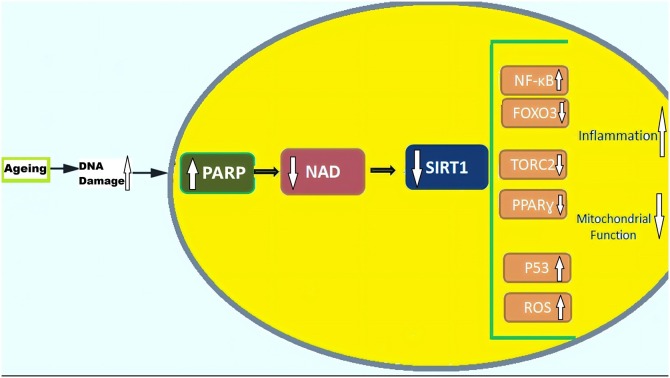
There is evidence that the NK cells are significantly increased in older adults while the percentages of type T of cells declined. In aged humans, APCs secretion of pro-inflammatory cytokines increased while they secrete decreased levels of anti-inflammatory and immune-regulatory cytokines. Increase Pro-inflammatory cytokines (e.g. Type I cytokines IFN-γ and TNF-α) and type II cytokines (IL-4)), and decreased FOXO3a activity play a significant role in the chronic pro-inflammatory state associated with the ageing process [30,31] (Fig. 3 ).
Fig. 3.
Ageing is associated with the accumulation of DNA damage, which leads to genotoxic stress, activation of PARP and decrease NAD with subsequent decline in SIRT1 activity in the nucleus and mitochondria, respectively. Decreased SIRT1 leads to NF-κB activation and decreased FOXO3a activity, together with increase p53 activity and ROS that lead to increased inflammation and decrease mitochondrial function.
The function of Dendritic cells in airway remodeling and inflammation is also compromised, leading to inevitably increase susceptibility to acute pneumonia and its complication [32]. Besides, older people produce significantly higher levels of monocyte chemoattractant protein‐1 (MCP‐1) and lower levels of the epidermal growth factor (EGF) [33]. Further, CD8+ and CD4+ T lymphocytes play an essential role in the developing cytokine network, resulting in higher production of pro-inflammatory mediators [34,35].
Age effect on telomeres
One of the crucial differences at the DNA level between old age individuals and children is their telomere length. Telomeres represent a region of repetitive nucleotide sequences at chromosome ends [36]. The immune system is extremely sensitive to the shortening of telomeres as its function depends strictly on cell renewal and clonal expansion of T and B types of cells. Immunosenescence is distinguished by telomere shortening with various kinetics of telomere debilitation in CD4+, CD8+ T lymphocytes, B lymphocytes, granulocytes, monocytes, and NK cell population [37].
There is a marked variation in leukocyte telomere length (LTL) between humans. This difference is typically attributed to the peculiar effect of gender, race/ethnicity, paternal age at conception, and environmental exposures [38].
In a cohort, prospective study included 75,309 reported that short LTL was associated with a high risk of hospitalization due to pneumonia and significant risk of death related to infections [39]. Another critical study on the immune response after flu vaccination documented that, individuals with long telomere length in B-lymphocytes produced a more robust antibody response when compared to individuals with short B-lymphocyte telomere length [39]. Epidemiological data on leukocyte telomere length (LTL) have concluded shorter LTL could be associated with increasing age [36,40], obesity, male gender [41,42], Caucasian race [43], alcoholism [44], atherosclerosis [45], diabetes [40,46] infection and cardiovascular disease [47,48] (Table 1 ).
Table 1.
Association of telomere length with age, gender, race, health risk factors, age-related chronic disease, and infection.
| First author, year (reference no.) | Study design | Factor | Telomere length |
|---|---|---|---|
| Cawthan, 2003 [47] | Cross- sectional | Heart diseases | Decrease |
| Benetos, 2004 [45] | Cross- sectional | Atherosclerosis in Hypertensive | Decrease |
| Gardner, 2005 [46] | Cohort | Diabetes mellitus | Decrease |
| Demissie, 2006 [42] | Cohort | Hypertension, increased insulin resistance and oxidative stress | Decrease |
| Fitzpatrick, 2007 [48] | Cross- sectional | Heart diseases | Decrease |
| Nordfjäll, 2008 [41] | Cohort | Obesity | Decrease |
| Halaschek-Wiener, 2008 [49] | Case-control | Caucasian race | Decrease |
| Sanders, 2013 [36] | Review | Ageing, male gender, Caucasian race, and atherosclerosis’ | Decrease |
| Fujishiro, 2018 [43] | Cohort | Caucasian race | Slow decline |
| Harpaz, 2018 [44] | Cross- sectional | Alcohol | Decrease |
LTL is also influenced by ethnicity [36]; two genome-wide association studies observed that the LTL was longer in African Americans than in European individuals. Moreover, the LTL was significantly longer in sub-Saharan Africans than in both Europeans and African Americans [49,50]. These critical findings suggest that differences in the LTL between Europeans and Africans are influenced by polygenic adaptation and ethnic differences in risks for diseases including viral infections [[51], [52], [53]]. These studies could explain why Africa has fewer cases of COVID-19 compared with most other parts of the world.
Furthermore, telomeres are shortened by cell division and oxidative stress and are lengthened by the enzyme telomerase and DNA exchange during mitosis. Telomere length is modulated by sirtuins, which area family of Nicotinamide adenine dinucleotide ((NAD+) dependent enzymes. Maintaining adequate NAD+ levels through NAD+ precursors would increase sirtuin activity and stabilizes telomeres [54]. Nicotinamide adenine dinucleotide (NAD+) is an essential pyridine nucleotide that participates in many metabolic reactions [55]. It is well-known for its critical role in redox reactions and as a signalling molecule. It serves as an essential cofactor and substrate for many critical cellular processes, including energy metabolism, mitochondrial function, biosynthesis, gene expression, calcium signaling, immunological functions, and ageing [56,57]. Decreases NAD+ level affect sirtuin activity and generally associated with short telomeres which subsequently induce cell ageing [36,40].
NAD+ metabolic pathways
There are five major precursors and intermediates to synthesize NAD+: 1-tryptophan, 2-nicotinamide (NAM), 3-nicotinic acid (NA), nicotinamideriboside (NR), and 5-nicotinamide mononucleotide (NMN.) The synthesis of NAD+ is usually carried out through two main pathways synthesis: de novo synthesis and salvage pathways. The de novo pathway converts tryptophan to quinolinic acid (QA) leading to the production of nicotinic acid mononucleotide (NaMN) via the kynurenine pathway. Altered kynurenine pathway activity is frequently linked to both ageing and some of the age-associated diseases [58].
To control NAD+ levels, most NAD+ is recycled via salvage pathways from NMN, NR, NAM, and NA. These substances are usually present in the extracellular spaces and are transported through the plasma membrane where they can be utilized [59]. NAD+ occupies a critical role as the substrate of NAD+-consuming enzymes like poly-ADP-ribose polymerases (PARPs), sirtuins and, CD38/157 ectoenzymes. Cellular NAD+ levels may be enhanced by activators of the salvage pathway or by inhibitors of enzymes that utilize NAD+ like CD38, PARPs, and SARM1 [60].
There is growing evidence from pharmacological studies that nicotinamide administration can result in alterations in nitric oxide production which reduces the DNA damage response, and improves mitochondrial activity [61,62]. NAD+ exerts potent preventive effects through the poly (ADP-ribose) polymerases, mono-ADP-ribosyltransferases, and sirtuin enzymes. These enzymes catalyze protein modifications, such as ADP-ribosylation and deacetylation, inevitably leading to changes in protein function. Sirtuins localize to telomeres and regulate telomere length [47]. As the organism gets older, NAD+ level decreases with a subsequent decreases in sirtuins activity, telomeres shorten and cells gradually deteriorate, stop dividing, and die [35,63]. This ageing-associated decline in NAD+ is believed to be a tremendous risk for diseases and/or disabilities, like hearing and vision loss, cognitive dysfunction, auto-immunity, dysregulation of the immune response [59]. A recent study showed that the administration of NAD+ associated with an increase in sirtuin activity. Increasing sirtuin activity stabilizes telomeres, reduced DNA damage, and improves telomere-dependent disease [64]. Stabilizing telomeres produces a beneficial impact on immune cell functions. Therefore, NAD+ involvement in DNA repair and immune response could be targeted in ageing therapeutic trials.
Role of NAD+ in infection and autoimmune diseases
In the last century, several studies have tested the relation between NAD+ and infection. Murray and his colleagues reported that in vitro HIV-1 infected human cells decreased the intracellular NAD+. Also, they suppressed NAD+ activity against the PARP enzyme. And this change could be reversed by using NAD+ [65]. A study published in clinical endocrinology explored the inhibitory effects of NAD+ on poly (ADP ribose) synthetase, and also its suppressing effect on interferon-gamma-induced HLA-DR antigen expression in cultured thyroid cells from patients with Graves’ disease [66]. Similarly, because of its specific immune modulatory change in HLA-DR expression, several scientists suggested using NAD+ in the treatment for tuberculosis [67,68].
Other potentially significant immunomodulatory effects of nicotinamide include modulation of cytokine action [69], and regulation of the intercellular adhesion molecules [70]. NAD+ also has been shown to block mast cell degranulation and inhibit protease release from leukocytes [71]. And if combined with tetracycline, they can regulate peculiar immune responses through suppression of complement activation, antibody production, leukocyte chemotaxis, prostaglandin synthesis, and the production of lipases and collagenases [71].
By targeting cellular antiviral agents, like virus-host interactome, can suggest a novel strategy for the development of effective treatments for COVID-19. Many host proteins are either involved in vital pathways of viral infection or the direct targets of the coronavirus. GSK3B, DPP4, SMAD3, PARP1, and IKBKB in common are among the targetable proteins [72].
Poly-ADP ribose polymerase-1 (PARP-1), is a DNA base repair enzyme that often activated by DNA breaks. On the other hand, PARP1 can also act as a mediator of inflammation due to its activation of nuclear factor- κB (NF-κB) and other transcription factors [73]. NF-κB is a protein complex that represents a key transcription factor that typically participates in cytokine production, ageing, and pro-survival responses in diverse cell types [73].
PARP-1 is a large protein composed of 1014 amino acids and has ADP-ribosyltransferase (monomer or polymer) activity [74]. It catalyzes the cleavage of NAD+ into nicotinamide and ADP-ribose. By this way, PARP-1 carries out a critical antiviral role through ADP-ribosylation of the viral genome (RNA or DNA) and inhibition of viral transcripts translation [74]. However, several viral families, including Togaviridae and Coronaviridae encode for a macrodomain protein that hydrolyzes ADP-ribose units from proteins and nucleic acids [75]. By this mechanism, these viruses inhibit the protective effect of PARP-1; and facilitate optimal replication and virulence [75]. Consequently, Excessive activation of PARP-1 occurs to compensate ADP-ribose hydrolyzation of PARP will be accompanied by increase pro-inflammatory cytokine production and excessive NAD+ consumption followed by glycolysis block, depletion of energy and cell death [76,77]. Moreover, NAD+ depletion mediated by uncontrolled PARP activity leads to decreased sirtuin 1 (SIRT1) activity indirectly. This process of PARP-1 overactivation can be reversed by exogenous NAD+ administration [75]. Further, NAD+ supplement with successive PARP-1 inhibition prevents NF-κB activation. By modulating NF-kB transcriptional activity, NAD+ has a vital role in controlling the ongoing inflammatory state, over activation of the immune system, and even the cytokine storm.
Conclusion
Older people and those with pre-existing conditions are greatly affected by COVID-19 and are more susceptible to poor clinical prognosis. The pathophysiological changes associated with ageing, declined immune function and comorbidity make them more likely to suffer from a severe type of COVID-19 disease and more serious complications. The ageing related decreases in NAD+ with the subsequent decline in telomeres length negatively influence the immune response, and COVID-19 outcome. We suggested the use of NAD+ as an immunomodulator for COVID-19 in older patients. Restoring normal NAD+ levels could decrease the severity of immune reaction in those patients and improve their clinical condition. We believe that a thorough understanding of the mechanism of the immune response against SARS-CoV-2-infection, immunosenescence, age-associated telomeres shortening will make the development of effective preventive and therapeutic strategy achievable.
Contributors
Huda Omran developed the idea, and both authors made a substantial contribution to the development and writing of this article. Huda Omran, acting as the corresponding author, accepted the ultimate responsibility for the decision to submit for publication.
Funding
No funding sources.
Competing interests
None declared.
Ethical approval
Not required.
References
- 1.Li X., Geng M., Peng Y., Meng L., Lu S. Molecular immune pathogenesis and diagnosis of COVID-19. J Pharm Anal. 2020;10(2):102–108. doi: 10.1016/j.jpha.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Corman V.M., Muth D., Niemeyer D., Drosten C. Hosts and sources of endemic human coronaviruses. Adv Virus Res. 2018;100:163–188. doi: 10.1016/bs.aivir.2018.01.001. Academic Press Inc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yuen K.S., Ye Z.W., Fung S.Y., Chan C.P., Jin D.Y. SARS-CoV-2 and COVID-19: the most important research questions. Cell Biosci. 2020;10 doi: 10.1186/s13578-020-00404-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lu J., Gu J., Li K., Xu C., Su W., Lai Z. COVID-19 outbreak associated with air conditioning in restaurant, Guangzhou, China, 2020. Emerg Infect Dis. 2020;26 doi: 10.3201/eid2607.200764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pan F., Ye T., Sun P., Gui S., Liang B., Li L. Time course of lung changes on chest CT during recovery from 2019 novel coronavirus (COVID-19) pneumonia. Radiology. 2020 doi: 10.1148/radiol.2020200370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet Publishing Group. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19).WHO; 2020.
- 8.Zhou P., Lou Yang X., Wang X.G., Hu B., Zhang L., Zhang W. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li W., Moore M.J., Vasllieva N., Sui J., Wong S.K., Berne M.A. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yi Y., Lagniton P.N.P., Ye S., Li E., Xu R.-H. COVID-19: what has been learned and to be learned about the novel coronavirus disease. Int J Biol Sci. 2020;16:1753–1766. doi: 10.7150/ijbs.45134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Riordan J.F. Angiotensin-I-converting enzyme and its relatives. Genome Biol. 2003;4:225. doi: 10.1186/gb-2003-4-8-225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jiang F., Yang J., Zhang Y., Dong M., Wang S., Zhang Q. Angiotensin-converting enzyme 2 and angiotensin 1-7: novel therapeutic targets. Nat Rev Cardiol. 2014;11:413–426. doi: 10.1038/nrcardio.2014.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harmer D., Gilbert M., Borman R., Clark K.L. Quantitative mRNA expression profiling of ACE 2, a novel homologue of angiotensin converting enzyme. FEBS Lett. 2002;532:107–110. doi: 10.1016/S0014-5793(02)03640-2. [DOI] [PubMed] [Google Scholar]
- 14.Leung W.K., To K.F., Chan P.K.S., Chan H.L.Y., Wu A.K.L., Lee N. Enteric involvement of severe acute respiratory syndrome - associated coronavirus infection. Gastroenterology. 2003;125:1011–1017. doi: 10.1016/j.gastro.2003.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xu Z., Shi L., Wang Y., Zhang J., Huang L., Zhang C. Case report pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. 2020;2600:19–21. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shi Y., Wang Y., Shao C., Huang J., Gan J., Huang X. COVID-19 infection: the perspectives on immune responses. Cell Death Differ. 2020:1–4. doi: 10.1038/s41418-020-0530-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Channappanavar R., Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol. 2017;39:529–539. doi: 10.1007/s00281-017-0629-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams A.E., Chambers R.C. The mercurial nature of neutrophils: still an enigma in ARDS? Am J Physiol - Lung Cell Mol Physiol. 2014;306:L217–L230. doi: 10.1152/ajplung.00311.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Michaud M., Balardy L., Moulis G., Gaudin C., Peyrot C., Vellas B. Proinflammatory cytokines, aging, and age-related diseases. J Am Med Dir Assoc. 2013;14:877–882. doi: 10.1016/j.jamda.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 21.Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020 doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 22.Gavazzi G., Krause K.H. Ageing and infection. Lancet Infect Dis. 2002;2:659–666. doi: 10.1016/S1473-3099(02)00437-1. [DOI] [PubMed] [Google Scholar]
- 23.Bader M.S., McKinsey D.S. Viral infections in the elderly: the challenges of managing herpes zoster, influenza, and RSV. Postgrad Med. 2005;118:45–54. doi: 10.3810/pgm.2005.11.1687. [DOI] [PubMed] [Google Scholar]
- 24.Heppner H.J., Cornel S., Peter W., Philipp B., Katrin S. Infections in the elderly. Crit Care Clin. 2013;29:757–774. doi: 10.1016/j.ccc.2013.03.016. [DOI] [PubMed] [Google Scholar]
- 25.National Academies Press (US); Washington (DC): 1992. Prevention, Institute of Medicine (US) Division of Health Promotion and Disease Risk factors for infection in the elderly, The Second Fifty Years: Promoting Health and Preventing Disability. [PubMed] [Google Scholar]
- 26.Fried L.P., Xue Q.L., Cappola A.R., Ferrucci L., Chaves P., Varadhan R. Nonlinear multisystem physiological dysregulation associated with frailty in older women: implications for etiology and treatment. J Gerontol - Ser A Biol Sci Med Sci. 2009;64(10):1049–1057. doi: 10.1093/gerona/glp076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fulop T., Dupuis G., Baehl S., Le Page A., Bourgade K., Frost E. From inflamm-aging to immune-paralysis: a slippery slope during aging for immune-adaptation. Biogerontology. 2016;17:147–157. doi: 10.1007/s10522-015-9615-7. [DOI] [PubMed] [Google Scholar]
- 28.Tu W., Rao S. Mechanisms underlying T cell immunosenescence: aging and cytomegalovirus infection. Front Microbiol. 2016;7:2111. doi: 10.3389/fmicb.2016.02111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yanes R.E., Gustafson C.E., Weyand C.M., Goronzy J.J. Lymphocyte generation and population homeostasis throughout life. Semin Hematol. 2017;54:33–38. doi: 10.1053/j.seminhematol.2016.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Salvioli S., Capri M., Valensin S., Tieri P., Monti D., Ottaviani E. Inflamm-aging, cytokines and aging: state of the art, new hypotheses on the role of mitochondria and new perspectives from systems biology. Curr Pharm Des. 2007;12:3161–3171. doi: 10.2174/138161206777947470. [DOI] [PubMed] [Google Scholar]
- 31.Alberti S., Cevenini E., Ostan R., Capri M., Salvioli S., Bucci L. Age-dependent modifications of type 1 and type 2 cytokines within virgin and memory CD4+ T cells in humans. Mech Ageing Dev. 2006;127:560–566. doi: 10.1016/j.mad.2006.01.014. [DOI] [PubMed] [Google Scholar]
- 32.Agrawal A., Agrawal S., Gupta S. Role of dendritic cells in inflammation and loss of tolerance in the elderly. Front Immunol. 2017;8:896. doi: 10.3389/fimmu.2017.00896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Franceschi C., Bonafè M., Valensin S., Olivieri F., De Luca M., Ottaviani E. Inflamm-aging: an evolutionary perspective on immunosenescence. Ann N Y Acad Sci. 2006;908:244–254. doi: 10.1111/j.1749-6632.2000.tb06651.x. [DOI] [PubMed] [Google Scholar]
- 34.Franceschi C., Valensin S., Bonafè M., Paolisso G., Yashin A.I., Monti D. The network and the remodeling theories of aging: historical background and new perspectives. Exp Gerontol. 2000;35(6–7):879–896. doi: 10.1016/S0531-5565(00)00172-8. Pergamon. [DOI] [PubMed] [Google Scholar]
- 35.Samani N.J., Boultby R., Butler R., Thompson J.R., Goodall A.H. Telomere shortening in atherosclerosis. Lancet. 2001;358:472–473. doi: 10.1016/S0140-6736(01)05633-1. [DOI] [PubMed] [Google Scholar]
- 36.Sanders J.L., Newman A.B. Telomere length in epidemiology: a biomarker of aging, age-related disease, both, or neither? Epidemiol Rev. 2013;35:112–131. doi: 10.1093/epirev/mxs008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kaszubowska L. Telomere shortening and ageing of the immune system - PubMed. J Physiol Pharmacol. 2008;59:169–186. [PubMed] [Google Scholar]
- 38.Aviv A. Genetics of leukocyte telomere length and its role in atherosclerosis. Mutat Res - Fundam Mol Mech Mutagen. 2012;730:68–74. doi: 10.1016/j.mrfmmm.2011.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Helby J., Nordestgaard B.G., Benfield T., Bojesen S.E. Shorter leukocyte telomere length is associated with higher risk of infections: a prospective study of 75,309 individuals from the general population. Haematologica. 2017;102:1457–1465. doi: 10.3324/haematol.2016.161943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Halaschek-Wiener J., Vulto I., Fornika D., Collins J., Connors J.M., Le N.D. Reduced telomere length variation in healthy oldest old. Mech Ageing Dev. 2008;129:638–641. doi: 10.1016/j.mad.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 41.Nordfjäll K., Eliasson M., Stegmayr B., Melander O., Nilsson P., Roos G. Telomere length is associated with obesity parameters but with a gender difference. Obesity. 2008;16:2682–2689. doi: 10.1038/oby.2008.413. [DOI] [PubMed] [Google Scholar]
- 42.Demissie S., Levy D., Benjamin E.J., Cupples L.A., Gardner J.P., Herbert A. Insulin resistance, oxidative stress, hypertension, and leukocyte telomere length in men from the Framingham Heart Study. Aging Cell. 2006;5:325–330. doi: 10.1111/j.1474-9726.2006.00224.x. [DOI] [PubMed] [Google Scholar]
- 43.Fujishiro K., Needham B.L., Landsbergis P.A., Seeman T., Jenny N.S., Roux A.V.D. Selected occupational characteristics and change in leukocyte telomere length over 10 years: the Multi-Ethnic Study of Atherosclerosis (MESA) PLoS One. 2018;13 doi: 10.1371/journal.pone.0204704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Harpaz T., Abumock H., Beery E., Edel Y., Lahav M., Rozovski U. The effect of ethanol on telomere dynamics and regulation in human cells. Cells. 2018;7:169. doi: 10.3390/cells7100169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Benetos A., Gardner J.P., Zureik M., Labat C., Xiaobin L., Adamopoulos C. Short telomeres are associated with increased carotid atherosclerosis in hypertensive subjects. Hypertension. 2004;43:182–185. doi: 10.1161/01.HYP.0000113081.42868.f4. [DOI] [PubMed] [Google Scholar]
- 46.Gardner J.P., Li S., Srinivasan S.R., Chen W., Kimura M., Lu X. Rise in insulin resistance is associated with escalated telomere attrition. Circulation. 2005;111:2171–2177. doi: 10.1161/01.CIR.0000163550.70487.0B. [DOI] [PubMed] [Google Scholar]
- 47.Cawthon R.M., Smith K.R., O’Brien E., Sivatchenko A., Kerber R.A. Association between telomere length in blood and mortality in people aged 60 years or older. Lancet. 2003;361:393–395. doi: 10.1016/S0140-6736(03)12384-7. [DOI] [PubMed] [Google Scholar]
- 48.Fitzpatrick Annette L., Kronmal Richard A., Gardner Jeffrey P., Psaty Bruce M., Jenny Nancy S., Tracy Russell P. Leukocyte telomere length and cardiovascular disease in the cardiovascular health study - PubMed. Am J Epidemiol. 2007;165:14–21. doi: 10.1093/aje/kwj346. [DOI] [PubMed] [Google Scholar]
- 49.Altshuler D.L., Durbin R.M., Abecasis G.R., Bentley D.R., Chakravarti A., Clark A.G. A map of human genome variation from population-scale sequencing. Nature. 2010;467:1061–1073. doi: 10.1038/nature09534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hunt S.C., Chen W., Gardner J.P., Kimura M., Srinivasan S.R., Eckfeldt J.H. Leukocyte telomeres are longer in AfricanAmericans than in whites: the National Heart, Lung, and Blood Institute Family Heart Study and the Bogalusa Heart Study. Aging Cell. 2008;7:451–458. doi: 10.1111/j.1474-9726.2008.00397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fitzpatrick Annette L., Kronmal Richard A., Gardner Jeffrey P., Psaty Bruce M., Jenny Nancy S., Tracy Russell P. Race/ethnicity and telomere length in the multi-ethnic study of atherosclerosis. Bone. 2012;23:1–7. doi: 10.1038/jid.2014.371. [DOI] [Google Scholar]
- 52.Tishkoff S.A., Reed F.A., Friedlaender F.R., Ehret C., Ranciaro A., Froment A. The genetic structure and history of Africans and African Americans. Science. 2009;324(5930):1035–1044. doi: 10.1126/science.1172257. (80-) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zeiger A.M., White M.J., Eng C., Oh S.S., Witonsky J., Goddard P.C. Genetic determinants of telomere length in african american youth. Sci Rep. 2018;8:1–9. doi: 10.1038/s41598-018-31238-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Amano H., Sahin E. Molecular & cellular oncology telomeres and sirtuins: at the end we meet again. Taylor and Francis. 2019;6 doi: 10.1080/23723556.2019.1632613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Braidy N., Berg J., Clement J., Khorshidi F., Poljak A., Jayasena T. Role of nicotinamide adenine dinucleotide and related precursors as therapeutic targets for age-related degenerative diseases: rationale, biochemistry, pharmacokinetics, and outcomes. Antioxidants Redox Signal. 2019;30:251–294. doi: 10.1089/ars.2017.7269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jung S.O., Ahn J.Y., Kim S., Yi S., Kim M.H., Jang H.H. Fluorescein derivative-based, selective and sensitive chemosensor for NADH. Tetrahedron Lett. 2010;51:3775–3778. doi: 10.1016/j.tetlet.2010.05.044. [DOI] [Google Scholar]
- 57.Lin S.J., Guarente L. Nicotinamide adenine dinucleotide, a metabolic regulator of transcription, longevity and disease. Curr Opin Cell Biol. 2003;15:241–246. doi: 10.1016/S0955-0674(03)00006-1. [DOI] [PubMed] [Google Scholar]
- 58.Castro-Portuguez R., Sutphin G.L. Kynurenine pathway, NAD+ synthesis, and mitochondrial function: targeting tryptophan metabolism to promote longevity and healthspan. Exp Gerontol. 2020;132 doi: 10.1016/j.exger.2020.110841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Rajman L., Chwalek K., Sinclair D.A. Therapeutic potential of NAD-Boosting molecules: the in vivo evidence. Cell Metab. 2018;27:529–547. doi: 10.1016/j.cmet.2018.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.ichiro Imai S., Johnson S. NAD+ biosynthesis, aging, and disease. F1000Research. 2018;7:132. doi: 10.12688/f1000research.12120.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Andrade J., Conde M., Ramfrez R., Monteseirfn J., Conde J., Sobrino F. 1996. Protection from nicotinamide inhibition of interleukin-lp-Induced RIN cell nitric oxide formation is associated with induction of MnSOD enzyme activity*. [DOI] [PubMed] [Google Scholar]
- 62.Sauve A.A. NAD+ and vitamin B3: from metabolism to therapies. J Pharmacol Exp Ther. 2008;324:883–893. doi: 10.1124/jpet.107.120758. [DOI] [PubMed] [Google Scholar]
- 63.Fossel M. The role of telomerase in age-related degenerative disease and cancer. Adv Cell Aging Gerontol. 2001;7:163–204. doi: 10.1016/S1566-3124(01)07019-5. [DOI] [Google Scholar]
- 64.Amano H., Chaudhury A., Rodriguez-Aguayo C., Lu L., Akhanov V., Catic A. Telomere dysfunction induces sirtuin repression that drives telomere-dependent disease. Cell Metab. 2019;29(6):1274–1290. doi: 10.1016/j.cmet.2019.03.001. 1274-1290.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Murray M.F., Nghiem M., Srinivasan A. HIV infection decreases intracellular nicotinamide adenine dinucleotide [NAD] Biochem Biophys Res Commun. 1995;212:126–131. doi: 10.1006/bbrc.1995.1945. [DOI] [PubMed] [Google Scholar]
- 66.Hiromatsu Y., Sato M., Yamada K., Nonaka K. Nicotinamide and 3‐aminobenzamide inhibit recombinant human interferon‐γ‐induced HLA‐DR antigen expression, but not HLA‐A, B, C antigen expression, on cultured human thyroid cells. Clin Endocrinol (Oxf) 1992;36:91–95. doi: 10.1111/j.1365-2265.1992.tb02907.x. [DOI] [PubMed] [Google Scholar]
- 67.Vanham G., Toossi Z., Hirsch C.S., Wallis R.S., Schwander S.K., Rich E.A. Examining a paradox in the pathogenesis of human pulmonary tuberculosis: immune activation and suppression/anergy. Tuber Lung Dis. 1997;78:145–158. doi: 10.1016/s0962-8479(97)90021-6. [DOI] [PubMed] [Google Scholar]
- 68.Rozwarski D.A., Grant G.A., Barton D.H.R., Jacobs W.R., Sacchettini J.C. Modification of the NADH of the isoniazid target (InhA) from mycobacterium tuberculosis. Science. 1998;279:98–102. doi: 10.1126/science.279.5347.98. (80) [DOI] [PubMed] [Google Scholar]
- 69.Hiromatsu Y., Yang D., Miyake I., Koga M., Kameo J., Sato M. Nicotinamide decreases cytokine-induced activation of orbital fibroblasts from patients with thyroid-associated ophthalmopathy. J Clin Endocrinol Metab. 1998;83:121–124. doi: 10.1210/jcem.83.1.4478. [DOI] [PubMed] [Google Scholar]
- 70.Hiromatsu Y., Sato M., Tanaka K., Ishisaka N., Kamachi J., Nonaka K. Inhibitory effects of nicotinamide on intercellular adhesion molecule-1 expression on cultured human thyroid cells. Immunology. 1993;80:330–332. [PMC free article] [PubMed] [Google Scholar]
- 71.Silwal P., Shin K., Choi S., Namgung U., Lee C.Y., Heo J.-Y.-Y. Tryptophan negatively regulates IgE-mediated mast cell activation. Korean J Phys Anthropol. 2017;30:53. doi: 10.11637/kjpa.2017.30.2.53. [DOI] [Google Scholar]
- 72.Zhou Y., Hou Y., Shen J., Huang Y., Martin W., Cheng F. Network-based drug repurposing for novel coronavirus 2019-nCoV/SARS-CoV-2. Cell Discov. 2020;6:1–18. doi: 10.1038/s41421-020-0153-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Mangerich A B.A. Pleiotropic cellular functions of PARP1 in longevity and aging: genome maintenance meets inflammation - PubMed. Oxid Med Cell Longev. 2012;2012 doi: 10.1155/2012/321653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Alemasova Elizaveta, Lavrik Olga. Poly(ADP-ribosyl)ation by PARP1: reaction mechanism and regulatory proteins. Nucleic Acids Res. 2019;47:3811–3827. doi: 10.1093/nar/gkz120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Grunewald M.E., Chen Y., Kuny C., Maejima T., Lease R., Ferraris D. The coronavirus macrodomain is required to prevent PARP-mediated inhibition of virus replication and enhancement of IFN expression. PLoS Pathog. 2019;15 doi: 10.1371/journal.ppat.1007756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Andrabi S.A., Umanah G.K.E., Chang C., Stevens D.A., Karuppagounder S.S., Gagné J.P. Poly(ADP-ribose) polymerase-dependent energy depletion occurs through inhibition of glycolysis. Proc Natl Acad Sci U S A. 2014;111:10209–10214. doi: 10.1073/pnas.1405158111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zhu Y., Zhao K.K., Tong Y., Zhou Y.L., Wang Y.X., Zhao P.Q. Exogenous NAD+ decreases oxidative stress and protects H2O2-treated RPE cells against necrotic death through the up-regulation of autophagy. Sci Rep. 2016;6 doi: 10.1038/srep26322. [DOI] [PMC free article] [PubMed] [Google Scholar]