Abstract
Arthropod-borne viruses (arboviruses) belonging to the Flavivirus genus of the Flaviviridae family, are a major public health threat in tropical and subtropical regions, and have recently become a medical concern in temperate zones. Most flaviviruses are classified as zoonotic viruses. Human flavivirus infections can be asymptomatic, responsible for unspecific symptoms in the first few days following infection, or responsible for severe complications potentially resulting in death. During the first days following symptom onset, laboratory diagnosis of acute human flavivirus infection is mainly based on molecular detection of the viral genome by RT-PCR methods, followed by the capture of specific antibodies using serological tests after the first week of infection. The detection of antibodies that have virus neutralizing activity can be used to confirm flavivirus infection. However, human flavivirus infections induce the production of cross-reactive antibodies, often making serology inconclusive. Indeed, serological diagnosis of flavivirus infection can be hampered by a patient’s history of flavivirus exposure, particularly in regions where multiple antigenically related flaviviruses co-circulate. We focus our mini review on conventional immunoassays that allow the diagnosis of major flavivirus-associated human infections in basic, routine and high-profile central health centers; and the interpretation of diagnostic serology tests for patients living within different epidemiological situations.
Keywords: antigenic cross-reactivity, arbovirus, diagnosis, Flavivirus, immunoassay, infection, serology
1. Introduction
More than five hundred arthropod-borne viruses (arboviruses) are registered in the International Catalog of Arboviruses (https://wwwn.cdc.gov/Arbocat/), 25% of them are confirmed human pathogens [1]. Most arboviruses of public health importance are members of the Flaviviridae, Togaviridae and Bunyaviridae families [2]. Within the Flaviviridae family, members of the Flavivirus genus have become an increased global health problem over the past decades due to the extension of their global distribution such as dengue virus (DENV) [3,4], West Nile virus (WNV) [5,6], or Zika virus (ZIKV) [7,8]. Reemergence in areas where circulation was previously thought to be contained has been observed, as for yellow fever virus (YFV) [4]. Other medically-important flaviviruses such as Japanese encephalitis virus (JEV), which circulates mainly in Southern and Southeastern Asia [9], or tick borne encephalitis virus (TBEV), which is endemic in parts of Eurasia [10], have not yet expanded their global distribution but they have the potential for spread because their vectors are widely distributed. To date we are still not able to predict emergence or re-emergence of flaviviruses in areas where competent arthropod vectors are established. Indeed, all areas with competent vectors should be prepared for the emergence or reemergence of flaviviruses and arboviruses in general [11]. Medically-important flaviviruses are an increasing concern in tropical and subtropical regions but also now in temperate zones. Travelers returning from areas of endemic flavivirus circulation and the transport of infected animals increase the likelihood of introducing a new pathogen into temperate regions where competent arthropod vectors are increasingly present [12]. This was the case with the emergence of WNV in North America [13] and Europe [14] from the 2000s; DENV [15] in Mediterranean countries for the last ten years or more recently ZIKV in South America in 2015 [16] and recently Europe in 2019 [17]. To prevent local transmission of newly introduced flaviviruses, early diagnosis of autochthonous infections and imported infections from travelers and their rapid notification have therefore become a priority in non-endemic areas. Newly emerging viral infections can be associated with the description of new modes of transmission, as for ZIKV that has been shown to be transmissible in humans through sexual intercourse [7,18]. Flavivirus-related human diseases resulting from non-vector-borne transmission, mainly blood transfusion for ZIKV [19], WNV [20] or DENVs [21] as well as sexual and mother-to-child transmission for ZIKV [7], can complicate the individual diagnosis in flavivirus endemic areas.
Flavivirus-associated human disease diagnosis requires laboratory testing, either through direct detection of the infecting agent, or the detection of antibodies directed against the infecting virus. The detection of viral RNA using PCR-based techniques offers excellent detection performance of flaviviruses in biological fluids. Most of the time, viral RNA amplification techniques still require clinical laboratories with advanced technology. Antibody tests detect antibodies directed against flavivirus antigens, mainly the envelope E protein, and, depending on the serological assay, can detect different immunoglobulin classes including IgM, IgG, and IgA. Interpretation of serological results can be challenging, principally due to an extensive cross-antigenic reactivity between the members of the Flavivirus genus [6,10,22,23,24,25,26,27,28,29]. In this review we discuss the place of serology in laboratory diagnosis of flavivirus-related human diseases, and the advantages and limitations of the main serological assays, with a focus on interpretation of serological results in different epidemiological settings.
2. Laboratory Diagnosis of Flavivirus-Associated Human Diseases
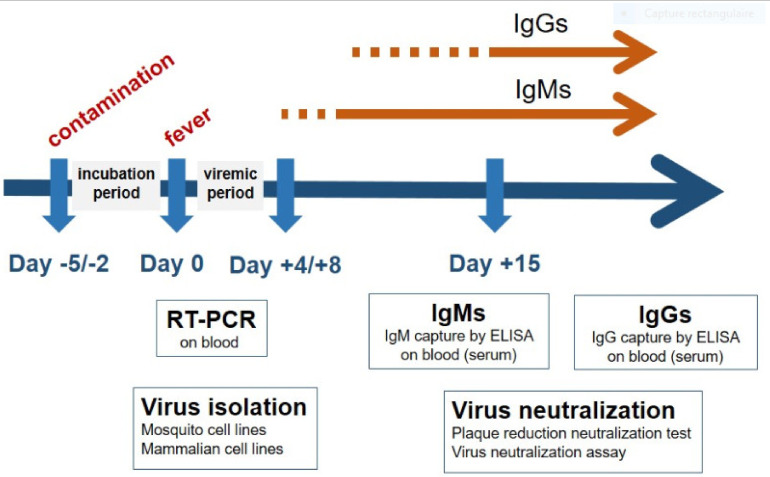
Routine diagnosis of flavivirus-associated human diseases relies on the detection of the pathogen, its nucleic acids or specific viral antigens during the acute phase of the disease followed by the capture of specific antibodies at least one week after the infection. Advantages and limitations of each method and the window of detection are detailed in Table 1 and Figure 1.
Table 1.
Current laboratory techniques for the diagnosis of acute human flavivirus infections.
| Methods | Advantages | Critical Evaluation |
|---|---|---|
| RT-PCR |
|
|
| Virus isolation |
|
|
| Viral antigen capture |
|
|
| Serology |
|
|
Figure 1.
Flow chart of molecular and serological diagnosis tests in the course of human flavivirus infections.
3. Early Diagnosis of Flavivirus-Associated Human Diseases
Flavivirus-associated human diseases can be reliably confirmed by the detection of viral nucleic acids using conventional reverse transcription (RT)-PCR or real-time RT-qPCR. The molecular diagnosis of flavivirus infection is dependent on the presence of viral nucleic acids in the sampled biological material. The RT-PCR assay, which is used routinely on blood specimens, can also be used on urine samples for ZIKV [30,31] and WNV [32], and less frequently on other biological samples such as cerebrospinal fluids (CSF). The window for ZIKV detection differs between body fluid samples with virus being detectable in semen specimens for long period of time (up several months) [33]. Notably, the molecular tests required for flavivirus detection in blood donations differs from those that are effective in clinical testing due to sensitivity requirements.
Although RT-PCR is a sensitive and specific method that allows rapid and reliable diagnosis of acute phase flavivirus in human diseases, its efficacy is mainly limited to the acute phase of infection (a few days post infection), and can be impacted by briefness of the viremic period or a low viral load in the blood in patients infected with flaviviruses such as WNV [20] or ZIKV [34]. However, the rate of detection in blood can be increased by testing whole blood instead of serum from patients infected by flaviviruses, especially for WNV [35] and ZIKV [36]. Indeed, laboratory testing standards need to adapt for “suspected flavivirus”.
The early diagnosis of dengue can also be performed using immunocapture of viral protein NS1 in the bloodstream using commercially available kits [37]. Unfortunately, other NS1-based tests are not yet available for other flavivirus infections.
In addition, virus isolation methods in cell lines such as African green monkey Vero cells and Aedes mosquito C6/36 cells are well-recognized methods for the confirmation of flavivirus infections, but their use is usually restricted to reference laboratories [38].
4. Detection of Flaviviruses Antibodies in Clinical Specimens
4.1. First Line Serological Assays
Table 2 details those immunological assays that are used in routine practice and those that are commercially available for flavivirus serology. Various techniques can be used to detect specific antibodies directed against flaviviruses. For serum specimens, hemagglutination inhibition assay and complement fixation techniques have been progressively replaced by commercial immunochromatographic lateral flow strip tests, immunofluorescence assays and enzyme-linked immunosorbent assay (ELISA) (including Mac and Gag-ELISA for the capture of IgM and IgG, respectively) [39,40,41,42,43]. Development of “in-house” ELISA tests by high profile central health centers is required to verify unvalidated serological data or when no licensed kits for detection of a particular flavivirus are yet available. However, such methods are uncommonly standardized. Advantages and limitations of each method are also detailed in Table 2.
Table 2.
Serological methods for detecting flavivirus-specific antibodies.
| Serological Diagnostic Methods | Virus-Specific Antibody Detection | Licensed Test Systems | Automation | General Remarks on the Method |
|---|---|---|---|---|
| Immuno-fluorescence tests (IFT) | Yes | Yes | Available IFT automation | IFT are referred as a conventional serological method |
| Enzyme-linked immunosorbent assays (ELISA) | Yes | Yes | Available ELISA automation | Conventional ELISA assays detect and measure a single analyte per plate |
| Virus neutralization tests (VNT) | Yes | No | No | VNT are performed to confirm the results of conventional serological methods |
| Lateral-flow immunoassays | Yes | Yes (only for DENV) | No | Rapid diagnostic tests but sensitivity and specificity are usually lower than for other methods. |
| Multiplex immunoassay (MIA) | Yes | No | Yes (MIA is based on the flow-cytometry technology) | MIA permits the multiplexing of many different assays within a single sample |
Specific immunoglobulin class M antibodies are usually detectable from the first week to 3 months post infection, and immunoglobulin class G antibodies are usually detectable from 2 weeks to several months or years. However, important variations can take place in the kinetics of antibody response depending on the biological assay used, viral antigens targeted for the antibody capture, immunological status in relation to a previous flavivirus exposure either by natural infection or vaccination, primary and secondary flavivirus-related human diseases, and individual immunological backgrounds.
Specific antibodies can be detected in CSF for flaviviruses responsible for severe neurological complications, especially tick-borne encephalitis virus (TBEV) [10], WNV [6,25] or JEV [26], and are usually detectable from the second week post infection when neurological disorders are diagnosed (from the first week for JEV [26]). The CSF-serum antibody index can be used to discriminate between blood-derived and brain-derived specific antibody fractions [10].
The main limitation of flavivirus serological assays is antibody cross-reactivity [6,10,22,23,24,25,26,27,28,29]. Unfortunately, the exact extent of cross-reactions between different flavivirus members is unknown, additionally it depends on the biological assay used for diagnosis and on the level of exposure to other co-circulating flaviviruses. Flavivirus-induced antibody cross-reactivity can also depend on the route of infection, as it has been reported for YFV with different cross reaction patterns among individuals previously exposed by vaccination or natural infection [27,44,45]. Amongst arboviruses, serological cross-reactions are not restricted to flaviviruses but are also reported for alphaviruses [46,47]. Cross-reaction between flaviviruses and alphaviruses, if any, should be very uncommon. However cross-reaction has been reported between flaviviruses and unrelated viruses, and between DENV and the novel betacoronavirus SARS-CoV-2 [48].
External quality assessment for WNV [49], DENV [50] or TBEV [51] diagnostics has demonstrated a large heterogeneity in laboratory performance, suggesting that all laboratories have not adopted rigorous control standards in order to provide comparable standardized flavivirus diagnosis results.
For ZIKV serology, cross reactions using first line serological assays are so promiscuous that official guidelines recommend the confirmation of all positive and inconclusive results by confirmatory serological assays [24]. Indeed, IgM and IgG antibody detection methods commonly suffer from false-positive and false-negative detection rates, meaning that most serological results are presumptive but not confirmatory.
DENV-1 to DENV-4 infections display similar symptoms, and antibody cross-reactivity makes simple antigen-based discrimination difficult between these four serotypes [52]. Differentiation of DENV serotypes can be achieved at the acute phase of the disease using serotype specific RT-PCR [37]. Therefore, serological differentiation of infection with the different DENV serotypes is generally achieved by neutralization tests, as greater specificity is shown in antibody neutralization than in antibody recognition. Notably, individuals experiencing a secondary DENV infection are characterized by the presence of high titers of production of anti-DENV IgGs during the acute phase of infection due to an anamnestic response, whereas IgGs are usually detected 10–15 days after a primary DENV infection [52].
Serological assay alone cannot discriminate primary from secondary DENV infections known to cause more severe disease that could relate to antibody-dependent enhancement phenomena [52,53].
4.2. Confirmatory Serological Assays
The detection of neutralizing anti-flavivirus antibodies is correlated with the presence of the specific IgGs in blood specimens. Conventional plaque-reduction neutralization tests (PRNT) and virus neutralization assays (VNA) in microplates are considered the “gold standard” in discriminant flavivirus serology [54]. However, regional structural variation in flaviviruses means that PRNTs or VNAs should use local virus isolates, when possible, in order to achieve better specificity and sensitivity. This means that no standardized commercial materials can be used for the establishment of effective local diagnostic measures, and laboratory constraints mean that the large-scale application of such diagnostic measures is typically limited to centralized diagnostic services. Neutralization tests often necessitate manipulation of flaviviruses in a biosafety laboratory level (BSL) 2, 3 or 4 with respect to the biological risk classification, which differs among countries [55].
Although virus neutralization assays are the reference tests for serological diagnosis of flavivirus-associated human diseases, serological cross reactions between the flaviviruses are also reported with this assay [56] and variations in PRNT titers varied according to testing conditions [57]. Consequently, the development of new neutralizing assays is a priority for flavivirus-associated human disease diagnosis. Flow cytometry-based neutralization assays using GFP or Luc reporter gene virus are a promising method, taking a few days to complete and numerous clinical samples may be measured for neutralizing antibodies in the same run [58,59,60,61,62,63,64].
4.3. Innovative Serological Assays
One major advance in the diagnosis of flavivirus human-associated infections is the development of multiplex assays that can simultaneously detect antibodies directed against several flaviviruses in the same run. High-density microarrays containing peptides derived from various flaviviruses have been developed to improve the sensitive and specificity of flavivirus serodiagnosis [65]. Microsphere-based immunoassays (MIAs) for the measurement of IgM and IgG against a large variety of flaviviruses are now a technology of choice to provide a multiplex serological assay [66,67,68,69,70,71,72,73,74].
4.4. Serosurvey Studies
A wide range of methodological designs have been applied to serosurvey studies and the lack of standardization represents a major limitation in the interpretation of results, as demonstrated for DENV or ZIKV [75].
5. Challenges in the Serological Diagnosis of Human Flavivirus Infections
Diagnosis should take into account the access to laboratory tools, the epidemiology of arbovirus diseases in the region where the patient is supposed to have been infected, and the past exposure to flaviviruses.
5.1. Access to Laboratory Tools
Most countries that experience high levels of endemic flavivirus circulation have limited laboratory capabilities. It is not unusual that only rapid serological diagnosis test kits are available at the point of care testing [76,77]. Consequently, the number of licensed rapid test kits has been growing fast over recent years. For dengue disease, rapid tests offer a good specificity (usually up to 90%), but experience large limitations with a sensitivity ranging from 10 to 99% [78,79]. Combined immunocapture of soluble NS1 antigen with the capture of specific antibodies has been demonstrated to increase the effectiveness of rapid tests for dengue diagnosis [80].
In countries with limited laboratory capacities, ELISA assays are usually not available and there is no access to confirmatory virus neutralization assays. This is one of the main limitations of the implementation of international recommendations and guidelines that focus on gold standard assays but do not take test and facility availability into consideration.
In high income countries, even if tests are available and access to reference laboratory possible, the issue is that commercial serological assays have not been developed for each flavivirus of medical concern.
5.2. Co-Circulation of Flaviviruses
Multiple flaviviruses co-circulate in most areas of endemic diseases [81], and co-circulation patterns vary over time and space [82]. Indeed, local epidemiology and the timings of potential exposure should always be taken into consideration when interpreting results.
Another consequence of co-circulation is the high risk of co-infection and a positive result for a flavivirus does not preclude infection with another one [83].
In endemic areas of several flaviviruses, the rate of serologic positivity against such pathogens is so elevated that most serological assays are unreliable for the diagnosis of a flavivirus infection. This becomes even more intricate in regions where confirmatory serologic diagnosis tests are still lacking or when most people have been vaccinated for flavivirus-associated diseases such as dengue, yellow fever and Japanese encephalitis. Implementation of multiplex microsphere immunoassays (MIA) using native or recombinant viral antigens could be appropriate for resolving the complexity of flavivirus diagnostic serology in endemic areas [74,84,85,86].
5.3. Prevalence of Flaviviruses
Most serological assays against flaviviruses are evaluated in terms of specificity and sensitivity, but not in predictive value, which is the probability that the test gives the correct diagnosis [87,88,89]. Positive and negative predictive values (PPV and NPV) are subject to variations according to the prevalence of the disease in a population. If a test is 99% specific, and 10% of a population being tested have the disease, there will be only 1 false positive for 10 true positives. However, if only 1 out of 1000 people experiences the disease, there will be 10 false positives for 1 true positive. In other words; as the prevalence increases (e.g., epidemic situation), the PPV also increases but the NPV decreases, similarly, as the prevalence decreases (e.g., low endemic situation), the PPV decreases while the NPV increases. The evaluation of the test should use sample cohorts relevant for the local setting and only the test evaluated in this setting should be used.
As mentioned above, because the prevalence of flavivirus-associated human diseases is highly variable in time and space in endemic areas, interpretation of results requires detailed knowledge of the local epidemiology at the moment the patient has been exposed.
5.4. Determination of the Onset of Symptoms
As the window of detection of flavivirus RNA, of specific IgM and IgG antibodies, is determined relative to the onset of symptoms, determination of the exact timing of the symptoms is key to using the correct diagnostic test. Usually the onset of symptoms can be clearly identified in infections such as dengue because there is a rapid onset of high fever. However, in some flavivirus infections such as Zika, there is often no fever or a low grade fever without acute onset of symptoms [8]. If there are any doubts, both nucleic acid testing and serology should be performed.
5.5. Patient’s Past Exposure to Flaviviruses
As most flavivirus-associated human diseases are asymptomatic or responsible for mild symptoms, patients may have past unrecognized disease. Indeed, in endemic areas it should be considered that all residents may have cross-reactive antibodies.
In flavivirus endemic regions where the populations are engaged in a vaccination program such as yellow fever in Africa and South America and Japanese encephalitis in South East Asia, or enrolled in a clinical trial of a candidate vaccine against a flavivirus of medical interest, interpretation of serological testing necessitates available information on the patient’s vaccination history.
5.6. Interpretation of Serological Results in Endemic Areas and in Travelers Returning from Endemic Areas
To illustrate the complexity in interpreting flavivirus serological results, we will consider the example of French Polynesia (South Pacific region), which suffers from high levels of flavivirus circulation, is a major tourist area, and has been identified as a hub for the spread of medically-important flaviviruses including Zika in 2013–2014 [70].
DENV was the only flavivirus circulating in French Polynesia until the emergence of ZIKV in 2013. DENV and ZIKV co-circulated from 2013 to 2014, and since mid-2014 DENV is the only circulating flavivirus [90].
Until the emergence of ZIKV in French Polynesia, the available serology tests for DENV provided reliable diagnosis for the disease among a large majority of residents. During the period of co-circulation of DENV and ZIKV, there was great difficulty in the serological diagnosis of both diseases due to a strong cross-antigenic reactivity between the two flaviviruses.
At the end of the ZIKV epidemic in French Polynesia, where at least one-half of the residents developed ZIKV antibodies [67], the serological diagnosis of DENV infection remained unreliable due to residual cross-reactive antibodies in individuals previously exposed to either flaviviruses [67].
For a traveler returning from French Polynesia, the situation is quite different. As has been observed with residents, a serology positive for DENV was specific prior to the emergence of ZIKV, whereas after the emergence, interpretation was confounded for the whole period of virus co-circulation due to the risk of cross-reactive antibodies. However, after the period of co-circulation, a positive serology could once again be considered specific for DENV (excepted if the traveler has a history of travel to another endemic area for flaviviruses or has been vaccinated against another flavivirus).
Indeed, the same serological test can have high or low predictive values, depending on the circulating rate of flaviviruses in the concerned area at the time of infection.
6. Conclusions
Flavivirus-associated human diseases are a growing cause of morbidity and mortality across the world and their area of distribution is expanding. Flaviviruses show a large amount of cross-reactivity in serological diagnostic tests, triggered by natural infection or vaccination. Cross-antigenic reactivity combined with a large overlap in clinical syndromes, co-circulation of different flaviviruses, and poor access to advanced laboratory diagnosis tools for serological confirmation make serological diagnosis of flavivirus-associated human diseases a great challenge. Most international guidelines and recommendations rely on gold standard assays, such as the virus neutralization assay, that unfortunately are not available in most areas with high endemic flavivirus circulation. We have identified an urgent need for more specific and sensitive serological methods allowing reliable standardized diagnosis for the timely management of flavivirus-associated human diseases.
Due to the frequent unreliability of current flavivirus serological tests, it is strongly encouraged to use molecular diagnosis in the first days following the onset of symptoms. However, we are convinced that implementation of multiplex serological assays based on the use of recombinant viral antigens will open avenues for the development of new specific and sensitive diagnostic tools for flavivirus detection in the near future [66,67,68,69,70,71,72,73,74].
Acknowledgments
We are grateful to David A. Wilkinson (UMR PIMIT) for the critical review of the manuscript and for the English spelling.
Funding
This work was supported by the POE FEDER 2014-20 of the Conseil Régional de La Reunion (ZIKAlert program, N° SYNERGIE RE00001902).
Conflicts of Interest
Author D.M. was employed by Eurofins Company. All other authors declare no competing interests.
References
- 1.Gubler D.J. The global emergence/resurgence of arboviral diseases as public health problems. Arch. Med. Rest. 2002;33:330–342. doi: 10.1016/S0188-4409(02)00378-8. [DOI] [PubMed] [Google Scholar]
- 2.Calisher C.H., Gould E.A. Taxonomy of the virus family Flaviviridae. Adv. Virus Res. 2003;59:1–19. doi: 10.1016/s0065-3527(03)59001-7. [DOI] [PubMed] [Google Scholar]
- 3.Gubbler D.J. Dengue and dengue hemorrhagic fever: Its history and resurgence as a global public health problem. In: Gubler D.J., Kuno G., editors. Dengue Dengue Hemorrhagic Fever. CAB; Wallingford, UK: 1997. pp. 1–22. [Google Scholar]
- 4.Gubler D.J. The changing epidemiology of yellow fever and dengue, 1900 to 2003: Full circle? Comp. Immunol. Microbiol. Infect. Dis. 2004;5:319–330. doi: 10.1016/j.cimid.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 5.Roehrig J.T. West nile virus in the United States-a historical perspective. Viruses. 2013;5:3088–3108. doi: 10.3390/v5123088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petersen L.R., Brault A.C., Nasci R.S. West Nile virus: Review of the literature. JAMA. 2013;310:308–315. doi: 10.1001/jama.2013.8042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Musso D., Ko A.I., Baud D. Zika Virus Infection: After the Pandemic. N Engl. J. Med. 2019;381:1444–1457. doi: 10.1056/NEJMra1808246. [DOI] [PubMed] [Google Scholar]
- 8.Musso D., Gubler D.J. Zika virus. Clin. Microbiol. Rev. 2016;29:487–524. doi: 10.1128/CMR.00072-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Misra U.K., Kalita J. Overview: Japanese encephalitis. Prog. Neurobiol. 2010;91:108–120. doi: 10.1016/j.pneurobio.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 10.Reusken C., Boonstra M., Rugebregt S., Scherbeijn S., Chandler F., Avšič-Županc T., Vapalahti O., Koopmans M., GeurtsvanKessel C.H. An evaluation of serological methods to diagnose tick-borne encephalitis from serum and cerebrospinal fluid. J. Clin. Virol. 2019;120:78–83. doi: 10.1016/j.jcv.2019.09.009. [DOI] [PubMed] [Google Scholar]
- 11.Musso D., Rodriguez-Morales A.J., Levi J.E., Cao-Lormeau V.-M., Gubler D.J. Unexpected outbreaks of arboviruses infections: Lessons learned from the Pacific and tropical America. Lancet Infect. Dis. 2018;18:e355–e361. doi: 10.1016/S1473-3099(18)30269-X. [DOI] [PubMed] [Google Scholar]
- 12.Charrel R.N. Diagnosis of arboviral infections–A quagmire of cross reactions and complexities. Travel Med. Infect. Dis. 2016;14:11–12. doi: 10.1016/j.tmaid.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 13.Nash D., Mostashari F., Fine A., Miller J., O’Leary D., Murray K., Huang A., Rosenberg A., Greenberg A., Sherman M., et al. The outbreak of West Nile virus infection in the New York City area in 1999. N. Engl. J. Med. 2001;344:1807–1814. doi: 10.1056/NEJM200106143442401. [DOI] [PubMed] [Google Scholar]
- 14.Tsai T.F., Popovici F., Cernescu C., Campbell G.L., Nedelcu N.I. West Nile encephalitis epidemic in southeastern Romania. Lancet. 1998;352:767–771. doi: 10.1016/S0140-6736(98)03538-7. [DOI] [PubMed] [Google Scholar]
- 15.European Centre for Disease Prevention and Control (ECDC) Local transmission of dengue fever in France and Spain. [(accessed on 7 May 2020)];2018 Available online: https://www.ecdc.europa.eu/en/publications-data/rapid-risk-assessment-local-transmission-dengue-fever-france-and-spain.
- 16.Khawar W., Bromberg R., Moor M., Lyubynska N., Mahmoudi H. Seven Cases of Zika Virus Infection in South Florida. Cureus. 2017;9:e1099. doi: 10.7759/cureus.1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giron S., Franke F., Decoppet A., Cadiou B., Travaglini T., Thirion L., Durand G., Jeannin C., L’Ambert G., Grard G., et al. Vector-borne transmission of Zika virus in Europe, southern France, August 2019. Eurosurveillance. 2019;24:1900655. doi: 10.2807/1560-7917.ES.2019.24.45.1900655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moreira J., Peixoto T.M., Machado de Siqueira A., Lamas C.C. Sexually acquired Zika virus: A systematic review. Clin. Microbiol. Infect. 2017;23:296–305. doi: 10.1016/j.cmi.2016.12.027. [DOI] [PubMed] [Google Scholar]
- 19.Musso D., Stramer S.L. International Society of Blood Transfusion Working Party on Transfusion-Transmitted Infectious Diseases. Zika virus: A new challenge for blood transfusion. Lancet. 2016;387:1993–1994. doi: 10.1016/S0140-6736(16)30428-7. [DOI] [PubMed] [Google Scholar]
- 20.Busch M.P., Caglioti S., Robertson E.F., McAuley J.D., Tobler L.H., Kamel H., Linnen J.M., Shyamala V., Tomasulo P., Kleinman S.H. Screening the blood supply for West Nile virus RNA by nucleic acid amplification testing. N. Engl. J. Med. 2005;353:460–467. doi: 10.1056/NEJMoa044029. [DOI] [PubMed] [Google Scholar]
- 21.Levi J.E. Dengue Virus and Blood Transfusion. J. Infect. Dis. 2016;213:689–690. doi: 10.1093/infdis/jiv322. [DOI] [PubMed] [Google Scholar]
- 22.Center for disease control and prevention Updated Guidance for U.S. Laboratories Testing for Zika Virus Infection. Center for disease control and prevention 2016. [(accessed on 7 May 2020)]; Available online: https://www.cdc.gov/zika/pdfs/laboratory-guidance-zika.pdf.
- 23.Rathore A.P.S., St John A.L. Cross-Reactive Immunity Among Flaviviruses. Front. Immunol. 2020;11:334. doi: 10.3389/fimmu.2020.00334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rabe I.B., Staples J.E., Villanueva J., Hummel K.B., Johnson J.A., Rose L., Hills S., Wasley A., Fischer M., Powers A.M. Interim guidance for interpretation of Zika virus antibody test results. MMWR Morb. Mortal. Wkly. Rep. 2016;21:543–546. doi: 10.15585/mmwr.mm6521e1. [DOI] [PubMed] [Google Scholar]
- 25.Sambri V., Capobianchi M.R., Cavrini F., Charrel R., Donoso-Mantke O., Escadafal C., Franco L., Gaibani P., Gould E.A., Niedrig M., et al. Diagnosis of west nile virus human infections: Overview and proposal of diagnostic protocols considering the results of external quality assessment studies. Viruses. 2013;5:2329–2348. doi: 10.3390/v5102329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johnson B.W., Goodman C.H., Jee Y., Featherstone D.A. Differential Diagnosis of Japanese Encephalitis Virus Infections with the Inbios JE Detect TM and DEN Detect TM MAC-ELISA Kits. Am. J. Trop. Med. Hyg. 2016;94:820–828. doi: 10.4269/ajtmh.15-0631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Allwinn R., Doerr H.W., Emmerich P., Schmitz H., Preiser W. Cross-reactivity in flavivirus serology: New implications of an old finding? Med. Microbiol. Immunol. 2002;190:199–202. doi: 10.1007/s00430-001-0107-9. [DOI] [PubMed] [Google Scholar]
- 28.Mansfield K.L., Horton D.L., Johnson N., Li L., Barrett A.D., Smith D.J., Solomom T., Fooks A.R. Flavivirus-induced antibody cross-reactivity. J. Gen. Virol. 2011;92:2821–2829. doi: 10.1099/vir.0.031641-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Papa A., Karabaxoglou D., Kansouzidou A. Acute West Nile virus neuroinvasive infections: Cross-reactivity with dengue virus and tick-borne encephalitis virus. J. Med. Virol. 2011;83:1861–1865. doi: 10.1002/jmv.22180. [DOI] [PubMed] [Google Scholar]
- 30.De Campos M.R., Cirne-Santos C., Meira G.L.S., Santos L.L., de Meneses M.D., Friedrich J., Jansen S., Ribeiro M.S., da Cruz I.C., Schmidt-Chanasit J., et al. Prolonged detection of Zika virus RNA in urine samples during the ongoing Zika virus epidemic in Brazil. J. Clin. Virol. 2016;77:69–70. doi: 10.1016/j.jcv.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 31.Gourinat A.C., O’Connor O., Calvez E., Goarant C., Dupont-Rouzeyrol M. Detection of Zika virus in urine. Emerg. Infect. Dis. 2015;21:84–86. doi: 10.3201/eid2101.140894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barzon L., Pacenti M., Franchin E., Pagni S., Martello T., Cattai M., Cusinato R., Palu G. Excretion of West Nile virus in urine during acute infection. J. Infect. Dis. 2013;208:1086–1092. doi: 10.1093/infdis/jit290. [DOI] [PubMed] [Google Scholar]
- 33.Mead P.S., Duggal N.K., Hook S.A., Delorey M., Fischer M., Olzenak McGuire D., Becksted H., Max R.J., Anishchenko M., Schwartz A.M., et al. Zika Virus Shedding in Semen of Symptomatic Infected Men. N Engl. J. Med. 2018;378:1377–1385. doi: 10.1056/NEJMoa1711038. [DOI] [PubMed] [Google Scholar]
- 34.Musso D., Rouault E., Teissier A., Lanteri M., Zisou K., Broult J., Grange E., Nhan T.-X., Aubry M. Molecular detection of Zika virus in blood and RNA load determination during the French Polynesian outbreak. J. Med. Virol. 2016;89:1505–1510. doi: 10.1002/jmv.24735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lanteri M.C., Lee T.-H., Wen L., Kaidarova Z., Bravo M.D., Kiely N.E., Kamel H.T., Tobler L.H., Norris P.J., Busch M.P. West Nile virus nucleic acid persistence in whole blood months after clearance in plasma: Implication for transfusion and transplantation safety. Transfusion. 2014;54:3232–3241. doi: 10.1111/trf.12764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Murray K.O., Gorchakov R., Carlson A.R., Berry R., Lai L., Natrajan M., Garcia M.N., Correa A., Patel S.M., Aagaard K., et al. Prolonged Detection of Zika Virus in Vaginal Secretions and Whole Blood. Emerg. Infect. Dis. 2017;23:99–101. doi: 10.3201/eid2301.161394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.World Health Organization Dengue guidelines for diagnosis, treatment, prevention and control. World Heal Organization 2009. [(accessed on 7 May 2020)]; Available online: https://apps.who.int/iris/bitstream/handle/10665/44188/9789241547871_eng.pdf?sequence=1&isAllowed=y.
- 38.White L.A. Susceptibility of Aedes albopictus C6/36 cells to viral infection. J. Clin. Microbiol. 1987;25:1221–1224. doi: 10.1128/JCM.25.7.1221-1224.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lukman N., Salim G., Kosasih H., Susanto N.H., Parwati I., Fitri S., Alisjahbana B., Widjaja S., Williams M. Comparison of the Hemagglutination Inhibition Test and IgG ELISA in Categorizing Primary and Secondary Dengue Infections Based on the Plaque Reduction Neutralization Test. Biomed Res. Int. 2016;2016:5253842. doi: 10.1155/2016/5253842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pavri K.M., Ghosh S.N. Complement-fixation tests for simultaneous isolation and identification of Dengue viruses, using tissue cultures. Bull. World Health Organ. 1969;40:984–986. [PMC free article] [PubMed] [Google Scholar]
- 41.Buonora S.N., Passos S.R.L., do Carmo C.N., Quintela F.M., de Oliveira D.N.R., dos Santos F.B., Hokerberg Y.H.M., Nogueira R.M.R., Daumas R.P. Accuracy of clinical criteria and an immunochromatographic strip test for dengue diagnosis in a DENV-4 epidemic. BMC Infect. Dis. 2016;16:37. doi: 10.1186/s12879-016-1368-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Niedrig M., Kursteiner O., Herzog C., Sonnenberg K. Evaluation of an Indirect Immunofluorescence Assay for Detection of Immunoglobulin M (IgM) and IgG Antibodies against Yellow Fever Virus. Clin. Vaccine Immunol. 2008;15:177–181. doi: 10.1128/CVI.00078-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Welch R.J., Chang G.-J.J., Litwin C.M. Comparison of a commercial dengue IgM capture ELISA with dengue antigen focus reduction microneutralization test and the centers for disease control dengue IgM capture-ELISA. J. Virol. Methods. 2014;195:247–249. doi: 10.1016/j.jviromet.2013.10.019. [DOI] [PubMed] [Google Scholar]
- 44.Houghton-Triviño N., Montaña D., Castellanos J. Dengue-yellow fever sera cross-reactivity; challenges for diagnosis. Rev. Salud. Publica. (Bogota) 2018;10:299–307. doi: 10.1590/S0124-00642008000200010. [DOI] [PubMed] [Google Scholar]
- 45.Souza N.C.S., e Félix A.C., de Paula A.V., Levi J.E., Pannuti C.S., Romano C.M. Evaluation of serological cross-reactivity between yellow fever and other flaviviruses. Int. J. Infect. Dis. 2019;81:4–5. doi: 10.1016/j.ijid.2019.01.023. [DOI] [PubMed] [Google Scholar]
- 46.Henss L., Yue C., Kandler J., Faddy H.M., Simmons G., Panning M., Lewis-Ximenez L.L., Baylis S.A., Schnierle B.S. Establishment of an Alphavirus-Specific Neutralization Assay to Distinguish Infections with Different Members of the Semliki Forest Complex. Viruses. 2019;11:82. doi: 10.3390/v11010082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hassing R.J., Leparc-Goffart I., Tolou H., van Doornum G., van Genderen P.J. Cross-reactivity of antibodies to viruses belonging to the Semliki forest serocomplex. Eurosurveillance. 2010;15:19588. [PubMed] [Google Scholar]
- 48.Yan G., Lee C.K., Lam L.T.M., Yan B., Chua Y.X., Lim A.Y.N., Phang K.F., Kew G.S., Teng H., Ngai C.H., et al. Covert COVID-19 and false-positive dengue serology in Singapore. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30158-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sanchini A., Donoso-Mantke O., Papa A., Sambri V., Teichmann A., Niedrig M. Second International Diagnostic Accuracy Study for the Serological Detection of West Nile Virus Infection. PLoS Negl. Trop. Dis. 2013;7:e2184. doi: 10.1371/journal.pntd.0002184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Domingo C., Alves M.J., de Ory F., Teichmann A., Schmita H., Muller R., Niedrig M. International external quality control assessment for the serological diagnosis of dengue infections. BMC Infect. Dis. 2015;15:167. doi: 10.1186/s12879-015-0877-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Niedrig M., Avšič T., Aberle S.W., Ferenczi E., Labuda M., Rozentale B., Mantke D. Quality control assessment for the serological diagnosis of tick borne encephalitis virus infections. J. Clin. Virol. 2007;38:260–264. doi: 10.1016/j.jcv.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 52.Gubler D.J. Dengue and dengue hemorrhagic fever. Clin. Microbiol. Rev. 1998;11:480–496. doi: 10.1128/CMR.11.3.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Halstead S.B., O’Rourke E.J. Antibody-enhanced dengue virus infection in primate leukocytes. Nature. 1977;265:739–741. doi: 10.1038/265739a0. [DOI] [PubMed] [Google Scholar]
- 54.Roehrig J.T., Hombach J., Barrett A.D.T. Guidelines for Plaque-Reduction Neutralization Testing of Human Antibodies to Dengue Viruses. Viral. Immunol. 2008;21:123–132. doi: 10.1089/vim.2008.0007. [DOI] [PubMed] [Google Scholar]
- 55.Change for Centers for Disease Control and Prevention National Institutes of Health. Biosafety in microbiological and biomedical laboratories, 5th ed. [(accessed on 7 May 2020)];2009 Available online: https://www.cdc.gov/labs/pdf/CDC-BiosafetyMicrobiologicalBiomedicalLaboratories-2009-P.PDF.
- 56.Ward M., Alger J., Berrueta M., Bock H., Buekens P., Cafferata M.L., Ciganda A., Garcia J., Garcia K., Lopez E., et al. Zika Virus and the World Health Organization Criteria for Determining Recent Infection Using Plaque Reduction Neutralization Testing. Am. J. Trop. Med. Hyg. 2018;99:780–782. doi: 10.4269/ajtmh.18-0237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Thomas S.J., Nisalak A., Anderson K.B., Libraty D.H., Kalayanarooj S., Vaughn D.W., Putnak R., Gibbons R.V., Jarman R., Endy T.P. Dengue plaque reduction neutralization test (PRNT) in primary and secondary dengue virus infections: How alterations in assay conditions impact performance. Am. J. Trop. Med. Hyg. 2009;81:825–833. doi: 10.4269/ajtmh.2009.08-0625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shan C., Xie X., Ren P., Loeffelholz M.J., Yang Y., Furuya A., Dupuis A.P., Kramer L.D., Wong S.J., Shi P.-Y. A Rapid Zika Diagnostic Assay to Measure Neutralizing Antibodies in Patients. EBioMedicine. 2017;17:157–162. doi: 10.1016/j.ebiom.2017.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Frumence E., Viranaicken W., Gadea G., Desprès P. A GFP Reporter MR766-Based Flow Cytometry Neutralization Test for Rapid Detection of Zika Virus-Neutralizing Antibodies in Serum Specimens. Vaccines. 2019;7:66. doi: 10.3390/vaccines7030066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Matsuda M., Yamanaka A., Yato K., Yoshii K., Watashi K., Aizaki H., Konishi E., Takasaki T., Kato T., Muramatsu M., et al. High-throughput neutralization assay for multiple flaviviruses based on single-round infectious particles using dengue virus type 1 reporter replicon. Sci. Rep. 2018;8:16624. doi: 10.1038/s41598-018-34865-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Koishi A.C., Suzukawa A.A., Zanluca C., Camacho D.E., Comach G., Duarte Dos Santos C.N. Development and evaluation of a novel high-throughput image-based fluorescent neutralization test for detection of Zika virus infection. Singh SK, editor. PLoS Negl. Trop. Dis. 2018;12:e0006342. doi: 10.1371/journal.pntd.0006342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kraus A.A., Messer W., Haymore L.B., de Silva A.M. Comparison of plaque- and flow cytometry-based methods for measuring dengue virus neutralization. J. Clin. Microbiol. 2007;45:3777–3780. doi: 10.1128/JCM.00827-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.De Alwis R., de Silva A.M. Measuring antibody neutralization of dengue virus (DENV) using a flow cytometry-based technique. Methods Mol. Biol. 2014;1138:27–39. doi: 10.1007/978-1-4939-0348-1_3. [DOI] [PubMed] [Google Scholar]
- 64.Lin R., Heeke D., Liu H., Rao E., Marshall J.D., Chio V., Cataniag F., Yu L., Zuo F., McCarthy M.P. Development of a robust, higher throughput green fluorescent protein (GFP)-based Epstein-Barr Virus (EBV) micro-neutralization assay. J. Virol. Methods. 2017;247:15–21. doi: 10.1016/j.jviromet.2017.04.012. [DOI] [PubMed] [Google Scholar]
- 65.Mishra N., Caciula A., Price A., Thakkar R., Ng J., Chauhan L.V., Jain K., Che X., Espinose D.A., Cruz M.M., et al. Diagnosis of Zika Virus Infection by Peptide Array and Enzyme-Linked Immunosorbent Assay. MBio. 2018;9:e00095. doi: 10.1128/mBio.00095-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Aubry M., Finke J., Teissier A., Roche C., Broult J., Paulous S., Despres P., Cao-Lormeau V.-M., Musso D. Seroprevalence of arboviruses among blood donors in French Polynesia, 2011–2013. Int. J. Infect. Dis. 2015;41:11–12. doi: 10.1016/j.ijid.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 67.Aubry M., Teissier A., Huart M., Merceron S., Vanhomwegen J., Roche C., Vial A.-L., Teururai S., Sicard S., Paulous S., et al. Zika virus seroprevalence, French Polynesia, 2014–2015. Emerg. Infect. Dis. 2017;23:669–672. doi: 10.3201/eid2304.161549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Aubry M., Teissier A., Huart M., Merceron S., Vanhomwegen J., Roche C., Vial A.-L., Teururai S., Sicard S., Paulous S., et al. Ross River virus Seroprevalence, French Polynesia, 2014–2015. Emerg. Infect. 2017;23:1751–1753. doi: 10.3201/eid2310.170583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lau C., Aubry M., Musso D., Teissier A., Paulous S., Desprès P., de-Lamballerie X., Pastorino B., Cao-Lormeau V.-M., Weinstein P. New evidence for endemic circulation of Ross River virus in the Pacific Islands and the potential for emergence. Int. J. Infect. Dis. 2017;57:73–76. doi: 10.1016/j.ijid.2017.01.041. [DOI] [PubMed] [Google Scholar]
- 70.Cao-Lormeau V.-M. Tropical Islands as New Hubs for Emerging Arboviruses. Emerg. Infect. Dis. 2016;22:913–915. doi: 10.3201/eid2205.150547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Venkateswaran K.N., Sarwar J., Parameswaran N., Krishnan K., Nelson W.M. Validation of a fluorescent microsphere multiplex serology assay for differential diagnosis of exposure to Zika virus and other closely related arboviruses. J. Immunol. 2018;200:25. [Google Scholar]
- 72.Venkateswaran N., Sarwar J., Parameswaran N., Fecteau T., O’Connor D., Nelson W.M., Venkateswaran K. Development and testing of a novel multiplex serodiagnostic assay for Zika and other arboviruses. J. Immunol. 2017;198:81.26. [Google Scholar]
- 73.Basile A.J., Horiuchi K., Panella A.J., Laven J., Kosoy O., Lanciotti R.S., Venkateswaran N., Biggerstaff G.J. Multiplex Microsphere Immunoassays for the Detection of IgM and IgG to Arboviral Diseases. PLoS ONE. 2013;8:e75670. doi: 10.1371/journal.pone.0075670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tyson J., Tsai W.-Y., Tsai J.-J., Massgard L., Stramer S.L., Lehrer A.T., Nerurkar V.R., Wang W.-K. A high-throughput and multiplex microsphere immunoassay based on non-structural protein 1 can discriminate three flavivirus infections. PLoS Negl. Trop. Dis. 2019;13:e0007649. doi: 10.1371/journal.pntd.0007649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fritzell C., Rousset D., Adde A., Kazanji M., Van Kerkhove M.D., Flamand C. Current challenges and implications for dengue, chikungunya and Zika seroprevalence studies worldwide: A scoping review. PLoS Negl. Trop. Dis. 2018;12:e0006533. doi: 10.1371/journal.pntd.0006533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.The Academy of Medical Sciences Improving the development and deployment of rapid diagnostic tests in LMICs. Workshop report, 21 November 2016, London, United Kingdom. [(accessed on 7 May 2020)]; Available online: https://www.interacademies.org/sites/default/files/publication/improving_the_development_and_deployment_of_rapid_diagnostic_tests_in_lmics.pdf.
- 77.Pang J., Chia P.Y., Lye D.C., Leo Y.S. Progress and Challenges towards Point-of-Care Diagnostic Development for Dengue. Kraft CS, editor. J. Clin. Microbiol. 2017;55:3339–3349. doi: 10.1128/JCM.00707-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lim J.K., Alexander N., Di Tanna G.L. A systematic review of the economic impact of rapid diagnostic tests for dengue. BMC Health Serv. Res. 2017;17:850. doi: 10.1186/s12913-017-2789-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Blacksell S.D. Commercial Dengue Rapid Diagnostic Tests for Point-of-Care Application: Recent Evaluations and Future Needs? J. Biomed. Biotechnol. 2012;2012:151967. doi: 10.1155/2012/151967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fry S.R., Meyer M., Semple M.G., Simmons C.P., Sekaran S.D., Huang J.X., McElnea C., Huang C.-Y., Valks A., Yong P.R., et al. The diagnostic sensitivity of dengue rapid test assays is significantly enhanced by using a combined antigen and antibody testing approach. PLoS Negl. Trop. Dis. 2011;5:e1199. doi: 10.1371/journal.pntd.0001199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gubler D.J. Resurgent vector-borne diseases as a global health problem. Emerg. Infect. Dis. 1988;4:442–450. doi: 10.3201/eid0403.980326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.De Oliveira W.K., de França G.V.A., Carmo E.H., Duncan B.B., de Souza Kuchenbecker R., Schmidt M.I. Infection-related microcephaly after the 2015 and 2016 Zika virus outbreaks in Brazil: A surveillance-based analysis. Lancet. 2017;390:861–870. doi: 10.1016/S0140-6736(17)31368-5. [DOI] [PubMed] [Google Scholar]
- 83.Rodriguez-Morales A.J., Villamil-Gómez W.E., Franco-Paredes C. The arboviral burden of disease caused by co-circulation and co-infection of dengue, chikungunya and Zika in the Americas. Travel Med. Infect. Dis. 2016;14:177–179. doi: 10.1016/j.tmaid.2016.05.004. [DOI] [PubMed] [Google Scholar]
- 84.Wong S.J., Furuya A., Zou J., Xie X., Dupuis A.P., II, Kramer L.D., Shi P.-Y. A Multiplex Microsphere Immunoassay for Zika Virus Diagnosis. EBioMedicine. 2017;16:136–140. doi: 10.1016/j.ebiom.2017.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Cao-Lormeau V., Blake A., Mons S., Lastère S., Roche C., Vanhomwegen J., Dub T., Baudouin L., Teissier A., Larre P., et al. Guillain-Barré Syndrome outbreak associated with Zika virus infection in French Polynesia: A case control study. Lancet. 2016;387:1531–1539. doi: 10.1016/S0140-6736(16)00562-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Taylor C.T., Mackay I.M., McMahon J.L., Wheatley S.L., Moore P.R., Finger M.L.J., Hewitson G.R., Moore F.A. Detection of specific ZIKV IgM in travelers using a multiplexed flavivirus microsphere immunoassay. Viruses. 2018;10:253. doi: 10.3390/v10050253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Trevethan R. Commentary: Sensitivity, Specificity, and Predictive Values: Foundations, Pliabilities, and Pitfalls in Research and Practice. Front. Public Health. 2017:5. doi: 10.3389/fpubh.2019.00408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Altman D.G., Bland J.M. Statistics Notes: Diagnostic tests 1: Sensitivity and specificity. BMJ. 1994;308:1552–1552. doi: 10.1136/bmj.308.6943.1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Altman D.G., Bland J.M. Statistics Notes: Diagnostic tests 2: Predictive values. BMJ. 1994;309:102. doi: 10.1136/bmj.309.6947.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Musso D., Bossin H., Mallet H., Besnard M., Broult J., Baudouin L., Levi J.E., Sabino E.C., Ghawche F., Lanteri M.C., et al. Zika Virus in French Polynesia, 2013–2014: Anatomy of a completed outbreak. Lancet Infect. Dis. 2018;18:e172–e182. doi: 10.1016/S1473-3099(17)30446-2. [DOI] [PubMed] [Google Scholar]