The outbreak of the novel coronavirus disease 2019 (COVID‐19) pandemic has overtaken the world at an unprecedented magnitude that not only leads to an uncontrollable surge in the number of patients and deaths but also compromises the safety and health of medical workers, including surgeons. While mitigation measures have been adopted by numerous hard‐hit countries in hopes of “flattening the curve” of infection, safety management approaches are required to provide surgical intervention to patients during the pandemic. As there are currently no uniform best‐practice recommendations on the management of the surgical patient amidst this ongoing pandemic, it is crucial to address the management of head and neck cancer (HNC) as significant aerosolization of respiratory pathogens is associated with diagnostic and therapeutic procedures (Saadi et al., 2020), including head and neck surgeries and open tracheostomy (Chee, Lee, Lai, & Chin, 2004). Strict guidelines are yet to be established for managing HNC as an indefinite delay may exacerbate treatment outcomes and result in cancer upstaging to the point of irreversibility. The mean doubling time of HNC has been reported to range from 94 to 99 days (Forster, Douglass, Harriss‐Phillips, & Bezak, 2017; Murphy et al., 2015; Waaijer, 2003). A clear clinical pathway must be provided, beginning with an initial survey, cancer ablation, and free flap reconstruction till postoperative care. Based on a single‐institution experience, we propose a formal and comprehensive algorithm for the inpatient management of advanced head and neck malignancies.
After the outbreak of COVID‐19, an institution‐wide protocol for managing advanced HNC was established at Kaohsiung Medical University Hospital in Kaohsiung, Taiwan. During the 3‐month period between January 2020 and March 2020, a total of 55 advanced HNC patients who underwent cancer ablation and free flap reconstruction were identified. All of the patients were diagnosed with either a stage T3 or T4 HNC. Out of the need to maintain a high level of suspicion for COVID‐19, we have established a stringent flowchart guideline from the initial phase of prehospital admission to postoperative care. This algorithm for managing patients of advanced HNC can be applied for different stages of COVID‐19 severity in any location based on a spectrum divided into four levels of outbreak severity: limited local transmission, containment, delay, and mitigation.
When community spread is absent as COVID‐19 remains limited to local transmission or under containment, surgeries can still be arranged using the undermentioned protocol. Prior to the admission of the HNC patient for inpatient treatment, a preliminary COVID‐19 risk survey consisting of a chest radiograph and history of travel, occupation, contact, and cluster (TOCC), as outlined by the Taiwanese Center of Disease Control, are obtained to rule out any potential carrier of COVID‐19 (Figure 1). As part of the risk survey, if a patient is suspected to have the virus, reverse‐transcription polymerase chain reaction (RT‐PCR) testing for COVID‐19 from nasopharyngeal swabs and chest computed tomography are arranged. Positive signs and symptoms include fever (body temperature exceeding 37.5°C), loss of smell and taste, diarrhea, cough, or other upper respiratory symptoms. In addition, laboratory tests consisting of C‐reactive protein and procalcitonin levels are ordered as these blood tests have been incorporated into the active surveillance of suspected inpatient cases of COVID‐19 using information technology at our institution with tremendous success and effectiveness (Lin et al., 2020).
FIGURE 1.
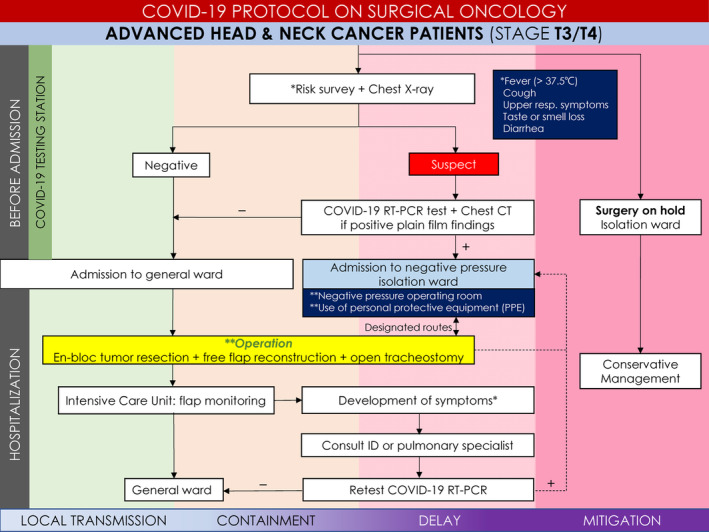
Covid‐19 guidance algorithm for advanced head and neck cancer reconstruction
If infection status is negative after the initial survey, the patient is directly admitted for surgery. During surgery, open tracheostomy could be safely performed wearing only regular surgical mask and personal protective equipment (PPE) in contrast to the highly inconvenient yet necessary enhanced PPE for confirmed cases. After surgery, the patient enters postoperative care at the intensive care unit (ICU). As the patients are transferred out of the ICU, they must return to the previous bed at the general ward so as to prevent cross‐infection. In the same light, all patients only received care from the same medical team of physicians and nurses.
In contrast, during the delay phase, due to unsuccessful containment, if a patient is confirmed with infection after the initial risk survey, the patient is admitted to the negative‐pressure isolation ward. All patient transfers within the hospital must occur on a preplanned dedicated transport route to limit transmissibility of the coronavirus. Once the patient's surgery is arranged, surgical tracheostomy is still performed for its primary benefit of securing airway safety. For the entire duration of the surgery, all surgeons must wear enhanced PPE ranging from face shields to powered air‐purifying respirators as advocated in confirmed or highly suspicious cases (Chee et al., 2004; Tien, Jogeklar, Cooper, & Brenneman, 2005). Finally, the patient is returned to the negative‐pressure isolation ward for postoperative care. It is important to note that every member on the medical team assigned to care for the confirmed case must also be tested for COVID‐19 and quarantined for a minimum of 2 weeks. The team members can resume work only after a full clearance of infection status and completion of quarantine.
However, if outbreak severity requires mitigation strategies due to failed containment and delay efforts, a contingency plan must be readily available should any city or country be further overtaken by the pandemic. In this case, the government may declare a national emergency and place a ban on all diagnostic and therapeutic procedures. As the occupational risk of contracting COVID‐19 is heightened at this stage, all except emergent surgeries are postponed indefinitely. The rightmost portion of the algorithm indicates that, in the mitigation phase, indefinite deferral of all surgeries must be implemented. The advanced HNC patient enters negative‐pressure isolation and receives conservative treatment from infectionists and pulmonologists. Cancer ablation will not be performed until de‐escalation of outbreak severity.
In conclusion, given the complex nature of HNC and the vulnerability of healthcare providers, surgeons must constantly weigh the benefits of postponing surgery for less aggressive cancers to reduce COVID‐19 transmission against the risk of tumor progression. This algorithm shall serve as a timely guideline for the management of advanced HNC patients.
REFERENCES
- Chee, V. W. K. M. , Lee, S. F. , Lai, Y. C. , & Chin, N. M. (2004). Infection control measures for operative procedures in severe acute respiratory syndrome‐related patients. Anesthesiology, 100(6), 1394–1398. [DOI] [PubMed] [Google Scholar]
- Forster, J. C. , Douglass, M. J. J. , Harriss‐Phillips, W. M. , & Bezak, E. (2017). Simulation of head and neck cancer oxygenation and doubling time in a 4D cellular model with angiogenesis. Scientific Reports, 7, 11037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, C. Y. , Cheng, C. H., Lu, P. L. , Shih, D. C. , Hung, C. T. , Lo, H. H. , Tsai, M. J. , & Hung, J. Y. (2020). Active surveillance for suspected COVID‐19 cases in inpatients with information technology. Journal of Hospital Infection S0195‐6701(20):30126‐122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy, C. T. , Devarajan, K. , Wang, L. S. , Mehra, R. , Ridge, J. A. , Fundakowski, C. , & Galloway, T. J. (2015). Pre‐treatment tumor‐specific growth rate as a temporal biomarker that predicts treatment failure and improves risk stratification for oropharyngeal cancer. Oral Oncology, 51, 1034–1040. [DOI] [PubMed] [Google Scholar]
- Saadi, R. A. , Bann, D. V. , Patel, V. A. , Goldenberg, D. , May, J. , & Isildak, H. (2020). A commentary on safety precautions for otologic surgery during the COVID‐19 pandemic. Otolaryngology–Head and Neck Surger 019459982091974. https://doi.org/10.1177/0194599820919741 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Tien, H. C. C. T. , Jogeklar, A. , Cooper, A. B. , & Brenneman, F. (2005). Elective and emergency surgery in patients with severe acute respiratory syndrome (SARS). Canadian Journal of Surgery, 48(1), 71–74. [PMC free article] [PubMed] [Google Scholar]
- Waaijer, A. (2003). Waiting times for radiotherapy: Consequences of volume increase for the TCP in oropharyngeal carcinoma. Radiotherapy and Oncology, 66, 271–276. [DOI] [PubMed] [Google Scholar]


