Abstract
Background
Despite continuing vaccine controversies, little is known about the trajectory of change in vaccine confidence over time. The current study examined whether there are subpopulations among the New Zealand public with diverging trajectories of confidence in the safety of childhood vaccinations from 2013 to 2017.
Methods
Using longitudinal survey data from the New Zealand Attitudes and Values Study, latent class growth models identified subpopulations with distinct rates and directions of change in vaccine confidence from 2013 to 2017 (N= 12,423; 11,912; 12,009; 10,254). The demographic profiles of these subpopulations were examined.
Findings
Most New Zealanders’ (60%) maintained strong vaccine confidence throughout the years (i.e. vaccine believers), but 30% expressed decreasing confidence over time (i.e. vaccine skeptics). Around 10% were former skeptics who had low vaccine confidence in 2013 but showed increasing confidence thereafter. Men, Europeans/Others, those more educated and living in more affluent regions were more likely to be vaccine believers. Relative to former skeptics, women, older individuals and those with lower education were more likely to be vaccine skeptics.
Interpretation
Attitudes toward the safety of childhood vaccinations are becoming increasingly polarized in New Zealand. Roughly 30% of the population are becoming more concerned about vaccine safety over time, 10% are becoming more confident, whereas 60% show consistent high vaccine confidence. It is vital to further investigate the key contributors to decreasing confidence among vaccine skeptics and implement target interventions.
Funding
Templeton Religion Trust Grant (TRT0196) for data collection; Corresponding author supported by University of Auckland Doctoral Scholarship.
Keywords: Vaccine confidence, Childhood vaccination safety, New Zealand, Longitudinal data
Research in Context.
Evidence before this study
Google scholar was used as the main search database. Peer-reviewed papers published between 2010 and 2019 were primarily searched for but some papers published at an earlier date were derived from reference lists. Key search terms included: vaccine confidence; vaccine hesitancy; childhood immunisations; New Zealand; vaccine safety concerns; parental vaccine attitudes; vaccine hesitant parents. We examined comprehensive review papers on vaccination attitudes, and studies on contributors to immunisation uptake, timeliness or vaccination attitudes conducted both within and outside of New Zealand. Referenced papers were chosen based on relevance of content, study method, sample characteristics and implication of findings. Resources published or commissioned by the New Zealand Ministry of Health and World Health Organization (surveys, immunisation handbook, vaccination coverage data) were also reviewed and referenced.
Added value of this study
Previous studies have not yet examined the trajectory of change in New Zealanders’ perceptions of childhood vaccine safety over time. The present study addresses this gap in research by using a large longitudinal sample of New Zealand adults to identify distinct subpopulations with diverging trajectories of vaccine confidence from 2013 to 2017. The demographic profiles of these distinct subpopulations are also examined.
Implications of all the available evidence
Although the majority of New Zealanders consistently exhibit strong vaccine confidence, a considerable proportion continue to show decreasing confidence over time. It is imperative to develop tailored interventions for groups at higher risk of low vaccine confidence. This includes improving healthcare access for low socio-economic groups, and implementing educational campaigns on vaccine safety and interpreting vaccine information for those with low education. Health professionals also need to be sufficiently trained to effectively address vaccine safety concerns among diverse groups.
Alt-text: Unlabelled box
Childhood vaccinations are a crucial public health intervention that protects people against harmful infections [1,2]. However, vaccine hesitancy has been highlighted as a major threat to global health by the World Health Organization in 2019 [3]. The refusal or delay in vaccinations can be linked to a diverse range of factors, including limited healthcare access, distrust in health professionals, complacency and vaccine safety concerns [4,5]. Standard vaccinations undergo rigorous safety testing before approval and are constantly monitored thereafter [1]. Nonetheless, with the recent increase in anti-vaccination movements and dissemination of anti-vaccine information, public concern about vaccine safety seem to be on the rise [4,[41]. Many express concerns that vaccines contain harmful substances and may cause various illnesses [1,4]. Specific fears about the Mumps, Measles and Rubella (MMR) vaccine can be traced back to Wakefield's (1998) fraudulent study on the link between MMR and autism [4]. Despite the retraction of this study and multiple epidemiological studies disproving its proposed association, MMR-autism myths continue to circulate and cause fear among parents [1,4,7]. Such doubts about vaccine safety challenge vaccination uptake and have contributed to the resurgence of measles outbreaks in multiple countries [4], including New Zealand [8].
In New Zealand, the National Immunisation Schedule offers a series of free standard vaccinations for New Zealanders from six weeks to 65 years of age (see Appendix for full Immunisation Schedule) [1]. To achieve herd immunity and prevent disease transmission, it is important to ensure that 92-94% of the population have been immunised [1]. Yet, during the 12-month period ending 31st December 2019, children who were fully immunised for their age at the six milestone ages (6, 8, 12, 18, and 24 months, and 5 years) were 79%, 90%, 92%, 84%, 91% and 88% respectively [9]. The proportion of fully immunised children was particularly low among Māori; the indigenous peoples of New Zealand (63.3% to 87.8%), and children living in highly deprived areas (69.6% to 89.7%). At each of the milestone ages, 4.3 to 5.4% of parents declined any one vaccination during the year 2019 [9]. Although reasons for declines are complex and cannot be explained by a single factor, they are often linked to concern about vaccine safety [4,10].
Among parents who delayed or missed immunisations, concerns about the risk or side effects of vaccinations are frequently cited as one of the main reasons for incomplete immunisations [10,11]. Some parents hold misconceptions that vaccines can cause illnesses such as autism or cot death [1], while others undermine vaccine necessity or desire more vaccine information [10,11]. As for the general population, the 2013 New Zealand Attitudes and Values Study (NZAVS) found that 68·5% of New Zealanders expressed strong confidence in the safety of the New Zealand childhood immunisation schedule but 26% showed moderate and 5·5% showed low confidence [12]. Māori individuals, women, parents, those less educated and living in more deprived areas reported decreased levels of vaccine confidence [12]. Among Māori and those with high deprivation, increased healthcare barriers and negative experiences with health professionals [13,14] may be contributing to their low vaccine confidence. Given that belief in vaccine safety is an important determinant of vaccination uptake [15,16], it is essential to track changes in and constantly monitor public vaccine confidence. However, due to the scarcity of large-scale panel data, little is currently known about the trajectory of change in New Zealanders’ vaccine confidence over time.
The present study addresses this gap in research by assessing New Zealanders’ confidence in the safety of standard childhood vaccinations during a period of heightened anti-vaccine controversies. With increased accessibility to anti-vaccine information online [4], vaccine confidence among those who previously held vaccine safety concerns may have further decreased throughout the years. As the New Zealand public tends to express varying levels of confidence in vaccine safety [12], this raises the potential that there may be multiple subpopulations showing differing rates and directions of change in vaccine confidence over time. Using survey data across four waves of the NZAVS (2013 and 2015-17), we examine whether the New Zealand public collectively exhibits decreasing or steady vaccine confidence over time, or whether there are distinct subpopulations with diverging trajectories of confidence. In the occasion that multiple subpopulations are identified, we aim to assess key demographic differences between these distinct groups. Our findings provide novel insight into the trajectory of New Zealanders’ confidence in the safety of childhood vaccinations over time and help dictate interventions that aim to improve public vaccine confidence.
1. Method
1.1. Sampling procedure
The NZAVS is a longitudinal survey study of a national probability sample of New Zealand adults (See Appendix for response and retention rates). This study is reviewed by the University of Auckland Human Participants Ethics Committee every three years and has most recently been approved from 5-September-2017 until 3-June-2021 (Reference Number: 014889). In Time 1 (2009), the NZAVS recruited participants from the entire country by randomly selecting samples from the New Zealand electoral roll (response rate: 16·6%; see Sibley et al. 2019 for details on sampling procedure) [17]. A booster sample was later recruited at Time 3 (2011) through an unrelated survey posted on the website of a major New Zealand newspaper. Further booster samples were recruited from the 2012 and 2014 Electoral Roll in subsequent Time periods (See Sibley et al. 2014 for comparisons to New Zealand Census) [18]. The current study uses Time 5 (2013), Time 7 (2015), Time 8 (2016) and Time 9 (2017) data, which included the item on vaccine confidence. Time 6 (2014) data was excluded as the Time 6 survey did not include this item.
1.2. Participants
Each sample included a large probability sample of New Zealand adults; Time 5 (Total N = 18,261), Time 7 (Total N = 13,942), Time 8 (Total N = 21,937) and Time 9 (Total N = 17,072). Number of participants included in the final analysis are reported in the results section. Participants in each time point had a mean age of around 50 years (age range: 18–94, 19–96, 18–97, 18–98 respectively) and median household income of $90,000 (median household income was $63,800 in the 2013 New Zealand Census). Sixty three percent of each sample was female, with around 81% identifying as European, 12% as Māori, 3% as of Pacific and 4% as of Asian ethnicity (ethnic categories were not mutually exclusive). Roughly 77% of participants from each time point were employed, and 74% were parents.
1.3. Measures
1.3.1. Vaccination items
At all four time points, vaccine confidence was assessed using the likert item (1 = Strongly Disagree, 7 = Strongly Agree; only 1 and 7 were labelled); “It is safe to vaccinate children following the standard NZ immunisation schedule.” This item was developed for the NZAVS in consultation with medical professionals [12]. Vaccination status of participants’ children was measured using the item; “If you have children under 18, are their vaccinations up-to-date, as per the recommendations of your doctor/GP?” There were four response options; (1) Yes-fully, (2) No-partially, (3) No-none, (4) Don't know. This item was developed for the NZAVS and included in the Time 7, 8 and 9 survey. We only report vaccination status data from Time 9 as vaccine confidence is the focus of our study.
1.3.2. Demographics
Participants were asked to report their gender, date of birth, ethnicity, region of residence and education level. Ethnicity was measured using the standard New Zealand Census item, in which participants could indicate each ethnic group they identified with. Education was coded into an eleven-level ordinal variable (0 = No qualification, 1=level 1 Certificate [basic knowledge/skills for work] to 10 = doctoral degree) based on the ten tertiary qualification levels in New Zealand. Deprivation was measured using the 2013 New Zealand Deprivation Index, which uses census information to assign a decile-rank index from 1 (least deprived) to 10 (most deprived) to each meshblock unit (i.e. small geographical area) [19].
1.4. Analytic overview
Latent class growth models were conducted on Mplus version 8 to identify distinct latent classes (i.e. subpopulations) with similar trajectories of change in vaccine confidence over time. As some participants opted out while others opted in at different time points, we were unable to follow the same group of individuals throughout 2013 to 2017. Thus, we used a linked model that allowed for missing data and identified links between respondent's responses over the four survey years. Those who were constant responders contributed more to the model. This was the most appropriate method of analysis given the algorithm of the model and provides novel insight into longitudinal changes in vaccine confidence at a population level.
Guided by Asparouhov and Muthen's three-step approach to mixture modelling [20], we identified (1) the number of subpopulations based on the growth curve of vaccine confidence, (2) then participants were assigned to the subpopulation they most likely belonged to and (3) the demographic covariates characterizing the subpopulations were examined. Gender, age, ethnicity (European/Other as reference category), education and deprivation level were included as covariates. Participants’ reported education and deprivation level at Time 5 was prioritized and if missing, was overridden by that reported in Time 7, 8, and 9 consecutively (prioritizing Time 9 made trivial difference).
Osborne and Sibley [21] note several model criteria including the Akaike information criteria (AIC), Bayesian Information Criteria (BIC), sample-sized adjusted BIC (aBIC), entropy and class proportion. These criteria assess the suitability of a model with k profiles relative to k-1 profiles. Good fitting models have lower AIC, BIC and aBIC values, and higher entropy and likelihood of correct class membership [21]. An entropy of 0·8 or above is generally regarded as a good fitting model. According to Kim [22] and Tofighi and Enders [23], aBIC is the most recommended fit criteria for growth mixture models. The sample-size adjusted consistent AIC (ADCAIC) also performed quite well [22]. BIC, aBIC, ADCAIC and entropy values were used to determine our best fitting model. As a good model should be parsimonious (i.e. contain fewer classes as possible) and avoid extremely small class proportions, model parsimony and class proportions were also taken into account.
1.5. STROBE Checklist
This manuscript adheres to the STROBE checklist where applicable.
2. Results
2.1. Main Analyses
A total of 12,826 participants were included in our final analysis. The number of responses included from Time 5, 7, 8 and 9 were 12,423, 11,912, 12,009 and 10,254, respectively. We assessed the growth curve of vaccine confidence using one to six latent class solutions. Each model was estimated using 500 initial stage starts, 40 initial stage iterations and 80 final stage optimizations to ensure we obtained a global solution. As seen in Table 1, model fit indices substantially improved after adding a second latent class to the single class model. The BIC, aBIC and ADCAIC showed a sharp decrease but the entropy value was still slightly low (0·57). Adding a third class further improved model fit, with the aBIC and ADCAIC decreasing by 2205 and 2220, respectively. The entropy value increased to 0·73, indicating a reasonably good model fit.
Table 1.
Model indices and class proportions for solutions ranging from one to six classes.
| No. of Classes | BIC | aBIC | ADCAIC | Entropy | Class proportions |
|---|---|---|---|---|---|
| 1 | 138955 | 138927 | 138895 | ––– | 1·00 |
| 2 | 133194 | 133159 | 133120 | 0·57 | 0·57, 0·43 |
| 3 | 131001 | 130954 | 130901 | 0·73 | 0·60, 0·30, 0·10 |
| 4 | 129185 | 129124 | 129057 | 0·77 | 0·60, 0·26, 0·07, 0·06 |
| 5 | 128266 | 128192 | 128111 | 0·80 | 0·60, 0·22, 0·11, 0·06, 0·01 |
| 6 | 127374 | 127289 | 127193 | 0·80 | 0·56, 0·19, 0·10, 0·10, 0·03, 0·01 |
Due to the complexity of the model (i.e. latent class model with random effect on intercepts but not slopes), the model criteria continued to improve the more classes we added. However, considering model parsimony and class proportions, having more classes does not necessarily indicate a better model. In the four-class model, the fourth group was created by simply splitting the existing classes a little more and the class proportion of two groups were fairly small (6% and 7%; See Supplementary Material). The fifth and sixth-class model also extracted extremely small classes, with one class representing only 1% of the sample. Caution needs to be applied when interpreting such small classes as they are based on a minor proportion of the sample. Overall, the three-class model had a reasonably good model fit and relatively large class sizes. The three-class model was judged to be the most parsimonious model and thus chosen as our final model.
2.2. Subpopulations
Three subpopulations with distinct rates and directions of change in vaccine confidence were identified. These groups were labelled ‘vaccine (safety) believers’, ‘vaccine (safety) skeptics’ and ‘former (safety) skeptics.’ The term ‘safety’ has been omitted from group labels hereafter for simplicity. Table 2 clarifies the definitions of key terms and groups labels used in this study. Table 3 reports the intercept (indicating group level of vaccine confidence in 2013) and slope (indicating the trend in confidence over time) for each group.
Table 2.
Definition of key terms and group labels as per used in this study.
| Key term | Definition |
|---|---|
| Vaccine confidence | Level of trust in the safety of childhood vaccinations measured by one's level of agreement to the statement that it is safe to vaccinate children following the NZ immunisation schedule. Having ‘strong vaccine confidence’ indicates that one has a high level of trust in and very minimal or no concerns about childhood vaccine safety. |
| Vaccine believers | Those that consistently expressed high levels of agreement to the statement that it is safe to vaccinate children following the NZ immunisation schedule during 2013 to 2017. Reasons for their ‘strong vaccine confidence’ may be diverse. This may include general trust in science or vaccinations specifically, better access to healthcare and/or positive perceptions of healthcare professionals or the government. |
| Vaccine skeptics | Those that showed decreasing levels of agreement to the statement that it is safe to vaccinate children following the NZ immunisation schedule from 2013 to 2017. Opposed to ‘vaccine believers’, reasons for decreasing ‘vaccine confidence’ may include increased exposure to anti-vaccine information, distrust in health professionals and/or limited access to healthcare or vaccine information. These individuals may be expressing diminishing belief in the safety of specific vaccines or vaccinations in general. |
| Former skeptics | Those that formerly showed the lowest level of agreement to the statement that it is safe to vaccinate children following the NZ immunisation schedule in 2013 but exhibited a steep increase in ‘vaccine confidence’ thereafter (until 2017). This increase could be due to multiple factors, including satisfactory follow-up vaccine conversations with doctors, corrected misconceptions about specific vaccines or vaccinations in general and/or improved access to healthcare. |
Table 3.
Model results for three latent class (subpopulation) solution.
| Latent class | Proportion | Mean estimate | SE | t-value | P-value | |
|---|---|---|---|---|---|---|
| 1. Vaccine believers | .607 | Intercept | 6.516 | 0.017 | 394.273 | <.000 |
| Slope | 0.022 | 0.003 | 7.313 | <.000 | ||
| 2. Vaccine skeptics | .295 | Intercept | 4.835 | 0.038 | 128.285 | <.000 |
| Slope | -0.137 | 0.015 | -9.223 | <.000 | ||
| 3, Former skeptics | .097 | Intercept | 3.472 | .074 | 47.112 | <.000 |
| Slope | .601 | .030 | 19.854 | <.000 |
2.2.1. Vaccine believers
The largest subpopulation (N = 7784, 60·7% of sample) was characterised by a high intercept (unstandardized mean intercept=6·52, p < 0·001) and small positive slope (unstandardized mean slope=0·02, p < 0·001). This subpopulation represents ‘vaccine believers’ who exhibited consistently high and subtly increasing belief in vaccine safety over time.
2.2.2. Vaccine skeptics
The second subpopulation contained 29·6% of the sample (N = 3792) and was characterised by a moderate intercept (unstandardized mean intercept=4·84, p < 0·001) and negative slope (unstandardized mean slope = -0·14, p < 0·001). This subpopulation represents ‘vaccine skeptics’ who are becoming increasingly concerned about vaccine safety over time.
2.2.3. Former skeptics
The third subpopulation (N = 1249, 9·7% of sample) was characterised by a low intercept (unstandardized mean intercept=3·43, p < 0·001) and steep positive slope (unstandardized mean slope = 60, p < 0·001). This subpopulation represents ‘former skeptics’ who initially had low vaccine confidence in 2013 (3·47) but are becoming increasingly confident over time. By 2017, their confidence rating reached 5·88.
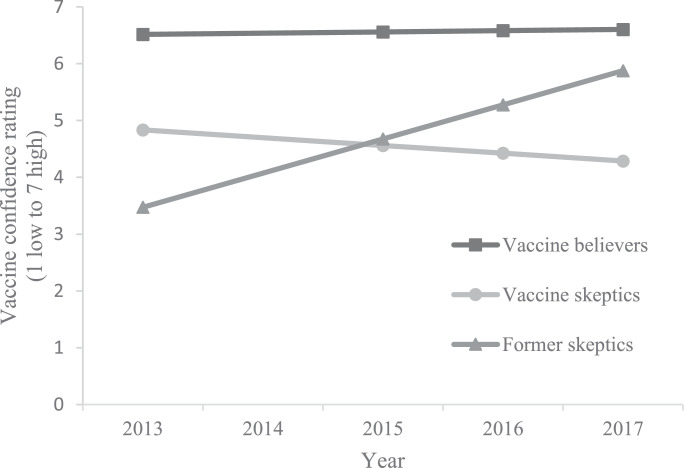
2.3. Differences between subpopulations
Vaccine believers persistently showed the highest level of vaccine confidence (see Figure 1). Former skeptics showed the steepest slope, with a particularly sharp increase in confidence between 2013 and 2015. Vaccine skeptics exhibited higher confidence than former skeptics in 2013, but their positions reversed across the years. In 2015, these two groups showed similar levels of confidence but in 2017, former skeptics showed notably higher confidence than vaccine skeptics (5·88 vs 4·29). With increasing confidence among former skeptics and decreasing confidence among vaccine skeptics, our findings indicate that vaccination attitudes are becoming increasingly polarized in New Zealand.
Figure 1.
Differences in trajectories of vaccine confidence between subpopulations from 2013 to 2017.
2.4. Demographic profiles of subpopulations
To identify key demographic differences between subpopulations, gender (reference category: women), age, ethnicity (reference category: European/Other), education (0=no qualification to 10= doctoral degree) and deprivation (1=lowest to 10=highest deprivation) level were included as auxiliary covariates to predict subpopulation membership. Each subpopulation was consecutively treated as the reference category and compared to the other two subpopulations. Tables in the Appendix present the 95% confidence intervals of odds ratios and the demographic breakdown of subpopulations based on most likely group membership (Note: caution needs to be taken when interpreting demographic breakdown as our analyses were based on probability of classification).
2.4.1. Vaccine believers
Compared to vaccine believers, former skeptics were more likely to be female relative to male (OR = 0·83), of Māori (OR = 1·70) or Pacific (OR = 1·97) compared to European ethnicity, live in more deprived as opposed to affluent regions (OR=1·05) and have lower education (OR=0·93). Similarly, vaccine skeptics were more likely to be women (OR = 0·66), of Māori (OR = 1·99), Pacific (OR = 1·58) or Asian (OR = 1·41) ethnicity, live in more deprived regions (OR = 1·06) and have lower education (OR = 0·89).
2.4.2. Vaccine skeptics
Compared to vaccine skeptics, former skeptics were more likely to be male relative to female (OR = 1·25), younger (OR = 0·99; age range: 18–94) and have higher education (OR = 1·05). Vaccine believers were less likely to be of Māori (OR = 0·50), Pacific (OR = 0·63) or Asian (OR = 0·71) compared to European ethnicity, and more likely to be men (OR = 1·51), live in more affluent regions (OR = 0·95) and have higher education (OR = 1·13).
2.4.3. Former skeptics
Compared to former skeptics, vaccine skeptics were more likely to be female relative to male (OR = 0·80), older (OR = 1·01) and have lower education (OR = 0·96). Vaccine believers were less likely to be of Māori (OR = 0·59) or Pacific (OR = 0·51) compared to European ethnicity, and more likely to live in more affluent regions (OR = 0·95) and have higher education (OR = 1·08).
2.5. Vaccination status in Time 9
We only report data on vaccination status from Time 9 (most recent Time point) to reduce the density of our results and maintain our focus on vaccine confidence. As shown in Table 4, most participants reported that their children were ‘fully vaccinated’ (87·6%), followed by ‘partially vaccinated’ (6·1%) and ‘unvaccinated’ (2·9%). Asian peoples reported the highest percentage of fully vaccinated children (92·2%), whereas Pacific (6·9%) and Europeans (6·9%) reported the highest percentage of partially and Māori reported the highest percentage of unvaccinated children (4·0%).
Table 4.
Response to item; “If you have children under 18, are their vaccinations up-to-date, as per the recommendations of your doctor/GP?” across ethnic groups in Time 9.
| European (N = 3232) |
Māori (N = 705) |
Pacific (N = 274) |
Asian (N = 599) |
Total (N = 4909) |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | N | % | N | % | N | % | N | % | N | |
| Yes-Fully | 87·3 | 2823 | 85·5 | 603 | 86·9 | 239 | 92·2 | 552 | 87·6 | 4302 |
| No-partially | 6·9 | 222 | 5·8 | 41 | 6·9 | 19 | 2·4 | 15 | 6·1 | 299 |
| No-none | 2·9 | 94 | 4·0 | 28 | 0·9 | 3 | 1·8 | 10 | 2·9 | 142 |
| Don't know | 1·2 | 37 | 2·0 | 14 | 0 | 0 | 0·5 | 3 | 1·1 | 55 |
| Unreported | 1·8 | 57 | 2·7 | 19 | 5·2 | 14 | 3·2 | 19 | 2·3 | 111 |
Note: Ethnic groups determined based on prioritized ethnicity (in order: Māori, Pacific, Asian, European). Sample weighting on gender, ethnicity and region of residence applied. Note the small cell sizes for Pacific and Asian peoples due to their low response rate.
Among those with ‘no qualification to Level 2 certificate’, 83.1% were fully vaccinated (see Table 5). This increased to 87.1%, 88.7%, and 89.3% for each higher education category respectively. The proportion of unvaccinated children slightly decreased as education level increased (3·5%, 3·3%, 2·7%, and 2·3% respectively). The rate of partially vaccinated children was similar across all education groups (5·9-6·4%). Compared to those with higher education, those with ‘no qualification to Level 2 certificate’ (2.9%) reported a higher rate of ‘don't know’ (1·3%, 0·5%, 0·6%, respectively).
Table 5.
Response to item; “If you have children under 18, are their vaccinations up-to-date, as per the recommendations of your doctor/GP?” across education level groups in Time 9.
| No qualification to Level 2 Cert (N = 712) |
Level 3 to 5 Cert (N = 1185) |
Graduate cert/Bachelor degree (N = 1690) |
Post-graduate degree (N = 1239) |
|||||
|---|---|---|---|---|---|---|---|---|
| % | N | % | N | % | N | % | N | |
| Yes-Fully | 83·1 | 591 | 87·1 | 1032 | 88·7 | 1500 | 89·3 | 1107 |
| No-partially | 6·4 | 46 | 6·3 | 75 | 5·9 | 100 | 6·1 | 75 |
| No-none | 3·5 | 25 | 3·3 | 39 | 2·7 | 46 | 2·3 | 29 |
| Don't know | 2·9 | 20 | 1·3 | 15 | 0·5 | 8 | 0·6 | 7 |
| Unreported | 4·1 | 29 | 1·9 | 23 | 2·2 | 37 | 1·7 | 21 |
Note: Education was coded based on the ten tertiary qualification levels in New Zealand (e.g. Level 1 Cert: basic knowledge/skills for work, Level 2 Cert: introductory knowledge/skills for field of work).
Group categorization: ‘No qualification to Level 2 Cert’ (No qualification, Level 1 and 2 Certificate), ‘Level 3 to 5 Cert’ (Level 3 to 5 diploma/Certificate), ‘Graduate Cert/Bachelor degree’ (Level 6 diploma/Certificate to Bachelor degree), ‘Post-graduate degree’ (Postgraduate diploma/Honours, Masters and Doctorate degree). Sample weighting on gender, ethnicity and region of residence applied.
3. Discussion
Our results indicate that confidence in the safety of childhood vaccinations are becoming increasingly polarized in New Zealand. Around 30% of the population show decreasing confidence over time (i.e. vaccine skeptics), 10% are becoming more confident (i.e. former skeptics) and the remaining 60% show consistent high vaccine confidence (i.e. vaccine believers). A wide range of factors are likely contributing to the maintenance of strong vaccine confidence among vaccine believers. Based on previous studies [24], [25], [26], vaccine believers may be those who have satisfactory access to vaccine information and strong trust in health professionals. Similar to Australian mothers with strong confidence [24], vaccine believers in New Zealand may also have better knowledge regarding the risk of vaccine-preventable diseases as well as the benefits and social responsibility associated with vaccinating. Oppositely, vaccine skeptics may represent those who lack access to adequate healthcare, have inaccurate or insufficient vaccine knowledge or negative perceptions of health professionals [24,25,27]. Due to limited access to trusted sources of vaccine information, their doubts about vaccine safety may not have been sufficiently addressed by health professionals and further exacerbated by exposure to anti-vaccine sentiments.
As health professionals have important influence on one's vaccination attitudes and uptake [4,24,27,28], they may have had a pivotal role in persuading and providing reassurance for former skeptics. Given their initially low confidence, parents who were former skeptics are more likely to have previously delayed or declined vaccinations. Among American parents who had previously declined the HPV vaccine, receiving higher quality recommendations from healthcare providers and greater satisfaction with provider communication were associated with greater secondary vaccine acceptance [15]. Likewise, satisfactory follow-up vaccine conversations with doctors may have led former skeptics in New Zealand to reconsider and gradually change their views of vaccine safety. The 2014 measles outbreak [8] may have been a key event that encouraged these individuals to seek further vaccine information and consult health professionals. In contrast, vaccine skeptics may have limited knowledge about the risk of measles and lack the opportunities or capability to reassess their vaccine beliefs. Such discrepancies can be linked back to potential differences in healthcare access and trust in health professionals between subpopulations.
Disparities in healthcare access, perceptions of health professionals or vaccine knowledge are closely tied to one's demographic characteristics. Thus, examining demographic differences between the three subpopulations not only allowed us to identify those more likely to be vaccine skeptics but provided important insight into the reasons why certain groups may be exhibiting strong or decreasing vaccine confidence. Our results revealed similar differences between vaccine believers and those who were either vaccine skeptics or former skeptics. Men, those of European/Other ethnicity, with lower deprivation and higher education were more likely to be vaccine believers. Conversely, women, Māori and Pacific peoples, those living in more deprived regions and with lower education were more likely to have previously held or continue to show increasing vaccine safety concerns. Relative to vaccine believers, Asian peoples were more likely to be vaccine skeptics but not any more likely to be former skeptics than European/Others.
For those of Māori or Pacific ethnicity and from highly deprived regions, low healthcare access may be a key contributing factor to their higher likelihood of being a vaccine skeptic or former skeptic. These groups typically experience greater financial or transport related barriers to healthcare and difficulty communicating with health providers due to language or cultural differences [13,[29], [30], [31]]. They are thus less likely to have sufficient access to vaccine information, feel well-informed or have high-quality vaccine conversations with doctors. Among these groups, those who were able to have their initial vaccine concerns addressed by culturally competent health professionals may be showing increasing confidence, while those who lacked this opportunity or do not trust their health professional persistently express growing concern. As for Asian peoples, contrary to their high vaccination rates [9], they were more likely to be vaccine skeptics than vaccine believers. Perhaps Asian parents in New Zealand are more likely to be hesitant compliers—concerned but fully-vaccinating parents. Due to cultural or language barriers, Asian parents may find it difficult to communicate and/or health professionals may be unable to sufficiently address their vaccine concerns. Therefore, in addition to improving healthcare access for minority and low socio-economic groups, it is vital ensure that doctors acquire strong cultural competency and attend to the unique healthcare barriers of those with diverse backgrounds.
Interestingly, there were no significant differences in ethnicity or deprivation level between vaccine skeptics and former skeptics. Gender, age and education were key distinguishing factors between these two subpopulations. Compared to vaccine skeptics, former skeptics were more likely to be male, younger and have higher education. Women and those less educated were not only less likely to be vaccine believers, but more likely to exhibit decreasing as opposed to increasing confidence in vaccine safety over time. Age was only significant when comparing vaccine skeptics and former skeptics. Relative to older adults, younger adults with immunisation-age children may encounter more opportunities to re-evaluate their vaccine beliefs and strengthen their vaccine confidence. For instance, parents with young children may exhibit heightened fear for their child's health during measles outbreaks, leading them to seek further vaccine information from trusted sources of vaccine information. Health professionals may also exert particular effort to convince and promote vaccinations to younger parents as opposed to older adults. With their misconceptions less likely to be corrected by health professionals, older adults may exhibit growing distrust in vaccine safety amidst persistent vaccine controversies.
Many pregnant women and parents receive or seek information about childhood vaccinations through various sources such as health professionals, family and the internet [28,32,33]. With the abundance of anti-vaccine information online and on social media [4], this increases the chances they are exposed to anti-vaccine sentiments. As women typically make all decisions regarding their child's vaccination [11], they are more inclined to do additional vaccine research and feel anxious about making the right decision for their child. Consistent with findings from an American sample [28], perhaps New Zealand women are also more likely to trust non-professional sources of vaccine information than men. Given that health professionals are important sources of vaccine information that influence vaccination attitudes [10,26,27], they may have had a central role in alleviating safety concerns among women who are former skeptics. On the contrary, women who remain skeptical may be those that are swayed by anti-vaccine information and unsatisfied with their providers’ ability to address their concerns. To effectively convince these women, health professionals need to go beyond simply providing pro-vaccine information [32,34]. They need to take the time to understand the specific concerns and sources of misinformation among skeptical women, and use easily-understood language to communicate evidence-based data to correct any misconceptions they hold [34].
Our findings suggest that low education is an important contributor to decreasing confidence among vaccine skeptics. Despite somewhat mixed findings [6], numerous studies suggest that low education is associated with poor vaccine knowledge, decreased access to vaccine information and lower trust in health professionals [25,35,36]. Due to their reduced cognitive capability and increased feeling of powerlessness, people with low education are also more receptive to conspiracy theories [37]. Hence, vaccine skeptics, who tend to have lower education, may be more likely to endorse anti-vaccine conspiracy theories but lack access to trusted sources of vaccine information that can correct their misconceptions. On the other hand, higher education may be a key factor helping maintain strong vaccine confidence among vaccine believers. Through better education, these individuals may possess the cognitive ability to accurately interpret vaccination information and differentiate between false and evidence-based studies on vaccinations. Those more educated may also be better able to understand and communicate with their doctor, and thus more likely to trust in health professionals and the safety of vaccinations they recommended. Parents with higher education were found more likely to have fully vaccinated children (see Table 4), further highlighting that parental education is a crucial contributor to both vaccine confidence and uptake among New Zealanders.
In contrast to studies that assess vaccination attitudes at one given (static) point in time, our analyses provide novel information forecasting how New Zealanders’ perceptions of vaccine safety are changing over time, and how they are forecast to continue to change in the near future. Although the majority of New Zealanders consistently exhibit strong vaccine confidence, a considerable proportion show steadily decreasing confidence over time. Unless appropriate interventions are implemented in a timely manner, vaccine confidence among vaccine skeptics are likely to continue to decrease and lead to declines in vaccination uptake. It is imperative to develop tailored interventions for groups at higher risk of low vaccine confidence. This includes improving healthcare access for low socio-economic groups, and implementing educational campaigns on vaccine safety and interpreting vaccine information for those with low education. Moreover, health professionals need to be sufficiently trained to develop trusting relationships with and adequately address vaccine concerns among diverse groups, especially young mothers and ethnic minorities. To better identify specific strategies to effectively persuade vaccine skeptics, it is vital to further investigate the key facilitators of attitude change among former skeptics.
As there were limitations in the number and types of predictors we could include in our model, we were unable to assess how various other NZAVS items (e.g. satisfaction with healthcare access or family doctor, subjective health, personality traits) may influence subpopulation membership. We were also unable to assess non-linear trends or potential fluctuations in vaccine confidence among different subpopulations. Our study used a single 7-point likert item asking about safety perceptions of the New Zealand immunisation schedule to measure vaccine confidence. Although this item lends insight into general perceptions of childhood vaccine safety among the public, it could not accurately discern New Zealanders’ specific vaccine concerns or the main contributors to the differential trends of the three subpopulations. Future studies should employ more comprehensive measures of vaccine confidence that tap into people's beliefs about vaccine harm and benefits, and trust in healthcare professionals or the government (see scale used by Gilkey et al.) [16]. The influence of disparate access to healthcare and vaccine information, and susceptibility to anti-vaccine conspiracy theories should also be investigated. Subsequent studies should use risk ratios for more readily interpretable results and examine the clinical significance of demographic differences in vaccine confidence.
The present study did not examine the number of participants who had immunisation-age children nor potential differences in vaccination confidence between parents with different age groups of children. There may have been important differences in the way with those with young (<5 years) or school-aged children interpreted the vaccination item and viewed the safety of specific vaccinations (e.g. MMR or Human papillomavirus vaccine). Nevertheless, the aim of this study was to assess population level changes in general perceptions of vaccine safety in New Zealand and our findings still provide a valuable framework for future research on the key determinants of New Zealanders’ vaccine confidence. Examining the relationship between vaccine confidence and actual vaccination uptake is another important direction for future research. As the Time 7 to 9 NZAVS surveys ask about child vaccination status, our data will enable us to investigate the degree to which vaccine confidence and characteristics associated with the three subpopulations may influence vaccination uptake across time.
Survey response rates have been declining over the years. Telephone survey response rates at the Pew Research Centre have decreased from 36% to 15% between 1997 to 2009, and stabilized at 9% in 2012 [38]. Similarly, the NZAVS obtained a relatively low initial response rate of 16.6% in 2009 and the average response rate for booster samples remains at 9% (excluding Time 3 booster; See Appendix). As participants opted in and out of our study throughout the years, we were unable to follow the same group of individuals consistently over time. However, collecting booster samples helped us increase the national representativeness of our sample and maintain a large sample. Given that certain groups are more likely to respond to our surveys [39], booster samples purposely oversampled specific areas (e.g. areas with high deprivation, greater ethnically diversity) to compensate for this [17]. After applying sample weighting on gender, ethnicity and region, the NZAVS was able to accurately track changes in New Zealanders’ political attitudes over time [40]. Although this weighting procedure could not be used in our main analysis, our sample is still a reasonable reflection of the New Zealand adult population and provides scarce longitudinal data on population level changes in vaccine confidence.
In summary, our findings indicate that 30% of the New Zealand population are becoming more concerned about vaccine safety over time, 10% are becoming more confident, while the remaining 60% show consistent high vaccine confidence. Men, those of European/Other ethnicity, those living in more affluent regions and more educated were more likely to be vaccine believers. Compared to former skeptics, women, older individuals and those with lower education were more likely to be vaccine skeptics. Better healthcare access, stronger trust in health professionals and higher education may be key factors that help maintain high vaccine confidence among vaccine believers. Health professionals are likely to have had a pivotal role in alleviating vaccine safety concerns and boosting confidence among former skeptics. In contrast, vaccine skeptics may be those who lack access to trusted sources of vaccine information and are more susceptible to anti-vaccine theories. It is essential to further investigate the specific concerns and reasons for declining confidence among vaccine skeptics and implement target interventions accordingly.
Author Contributions
CHJL was the primary author of the manuscript who did the literature search, writing and data interpretation. CGS supervised the project and led the data analysis. CGS provided feedback on the draft report and both authors approved the final version.
Declaration of Competing Interest
CHJL and CGS report a grant from Templeton Religion Trust.
Acknowledgements
We thank all the NZAVS participants and research team. Collection of NZAVS data was supported by a grant from Templeton Religion Trust (TRT0196) awarded to CGS. CHJL was supported by a University of Auckland Doctoral Scholarship during manuscript preparation. The authors were not paid to write this article by any company or agency. The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Link to study website: www.nzavs.auckland.ac.nz
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.eclinm.2020.100387.
Appendix
Table A1.
New Zealand Immunisation Schedule (applied from 1 July 2019). Retrieved from Ministry of Health Website [9].
| Age | Diseases covered and vaccines |
|---|---|
| Pregnant women | Influenza 1 Injection annually, at any stage of pregnancy |
| Tetanus/Diphtheria/Pertussis (whooping cough) 1 injection, during the second or third trimester of pregnancy |
|
| 6 weeks | Rotavirus (start first dose before 15 weeks) 1 oral vaccine |
| Diphtheria/Tetanus/Pertussis/Polio/Hepatitis B/Haemophilus influenzae type b 1 injection |
|
| Pneumococcal 1 injection |
|
| 3 months | Rotavirus (second dose must be given before 25 weeks) 1 oral vaccine |
| Diphtheria/Tetanus/Pertussis/Polio/Hepatitis B/Haemophilus influenzae type b 1 injection |
|
| Pneumococcal 1 injection |
|
| 5 months | Diphtheria/Tetanus/Pertussis/Polio/Hepatitis B/Haemophilus influenzae type b 1 injection |
| Pneumococcal 1 injection |
|
| 15 months | Haemophilus influenzae type b 1 injection |
| Measles/Mumps/Rubella 1 injection |
|
| Pneumococcal 1 injection |
|
| Varicella (Chickenpox) 1 injection |
|
| 4 years | Diphtheria/Tetanus/Pertussis/Polio 1 injection |
| Measles/Mumps/Rubella 1 injection |
|
| 11 or 12 years | Tetanus/Diphtheria/Pertussis 1 injection |
| Human Papillomavirus (HPV) 2 injections given at least 6 months apart for those aged 14 and under 3 injections given over 6 months for those aged 15 and older |
|
| 45 years | Diphtheria/Tetanus 1 injection |
| 65 years | Diphtheria/Tetanus 1 injection |
| Zoster (shingles) 1 injection |
|
| Influenza 1 Injection annually |
Table A2.
Sample sizes, retention rates and response rates at each Time point of the New Zealand Attitudes and Values Study.
| Time 1 (2009) | Time 2 (2010) | Time 3 (2011) | Time 3.5 (2012) | Time 4 (2012) | Time 5 (2013) | Time 6 (2014) | Time 7 (2015) | Time 8 (2016) | Time 9 (2017) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Sample size (N) | 6,518 | 4,441 | 6,884 | 4,514 | 12,179 | 18,261 | 15,820 | 13,942 | 21,936 | 17,072 |
| N retained from at least one previous Time point | ––- | 4,423 | 3,918 | 4,090 | 6,807 | 10,502 | 15,740 | 13,941 | 13,779 | 16,931 |
| N retained from previous Time point only | ––- | 4,423 | 3,530 | ––- | 5,762 | 9,844 | 14,878 | 12,550 | 11,933 | 15,784 |
| Wave-to-Wave retention [Mortality Adjusted] | ––- | 68.15% | 79.88% | ––- | 84.13% | 81.00% | 81.65% | 79.58% | 85.99% | 72.05% |
| Time 1 Retention [Mortality Adjusted] | ––- | 68.15% | 60.74% | ––- | 63.26% | 61.84% | 58.96% | 53.32% | 54.24% | 44.95% |
| Number of Booster Samples | ––- | ––- | 1 | ––- | 5 | 2 | ––- | ––- | 1 | ––- |
| Additional N (including booster, occasional opt-in partners) | ––- | 16 | 2,966 | 424 | 5,374 | 7,759 | 82 | 2 | 8,157 | 141 |
| Response rate (average rate if more than 1 booster sample) | 16·6% | –– | 92·4% | ––- | 9·8% | 8·55% | ––- | ––- | 9·7% | ––- |
Note: Response rates for Time 2, 3.5, 6, 7 and 9 are not reported as these time points did not include booster samples (these samples included participants from previous time points and occasional opt-ins). Time 3 included a non-random booster recruited from unrelated online newspaper website. Time 4 included one weighted deprivation booster and four electoral boosters (one random and the other three oversampling based on region of residence or ethnicity). Time 5 included a random electoral and Māori electoral booster. Time 8 included a random electoral booster. Around 400-450 Pacific participants were recruited informally via Pacific networks in Time 3.5.
Table A3.
Odds ratios for multinomial logistic regression with vaccine believers, vaccine skeptics and former skeptics as reference groups respectively.
|
Former skeptics |
Vaccine skeptics |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference Category: Vaccine believers | OR | Lower CI | Upper CI | SE | P-value | OR | Lower CI | Upper CI | SE | P-value | ||||||
| Gender | 0·827* | 0·704 | 0·972 | 0·068 | 0·011 | 0·660** | 0·591 | 0·738 | 0·037 | <0·001 | ||||||
| Māori | 1·699** | 1·372 | 2·104 | 0·185 | <0·001 | 1·988** | 1·707 | 2·315 | 0·155 | <0·001 | ||||||
| Pacific | 1·968** | 1·386 | 2·795 | 0·352 | 0·006 | 1·576* | 1·183 | 2·100 | 0·231 | 0·013 | ||||||
| Asian | 1·066 | 0·724 | 1·569 | 0·210 | 0·753 | 1·406* | 1·089 | 1·814 | 0·183 | 0·026 | ||||||
| Age | 0·996 | 0·991 | 1·002 | 0·003 | 0·195 | 1·003 | 0·999 | 1·007 | 0·002 | 0·115 | ||||||
| Deprivation | 1·054** | 1·025 | 1·083 | 0·015 | <0·001 | 1·056** | 1·035 | 1·077 | 0·011 | <0·001 | ||||||
| Education | 0·929** | 0·904 | 0·956 | 0·013 | <0·001 | 0·887 | 0·871 | 0·904 | 0·009 | <0·001 | ||||||
|
Former skeptics |
Vaccine believers |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference Category: Vaccine skeptics | OR | Lower CI | Upper CI | SE | P-value | OR | Lower CI | Upper CI | SE | P-value | ||||||
| Gender | 1·252* | 1·039 | 1·509 | 0·119 | 0·035 | 1·514** | 1·355 | 1·692 | 0·086 | <0·001 | ||||||
| Māori | 0·855 | 0·679 | 1·076 | 0·101 | 0·148 | 0·503** | 0·432 | 0·586 | 0·039 | <0·001 | ||||||
| Pacific | 1·249 | 0·856 | 1·821 | 0·240 | 0·301 | 0·634** | 0·476 | 0·845 | 0·093 | <0·001 | ||||||
| Asian | 0·758 | 0·493 | 1·167 | 0·167 | 0·148 | 0·711** | 0·551 | 0·918 | 0·093 | 0·002 | ||||||
| Age | 0·993* | 0·987 | 0·999 | 0·003 | 0·031 | 0·997 | 0·993 | 1·001 | 0·002 | 0·114 | ||||||
| Deprivation | 0·998 | 0·967 | 1·030 | 0·016 | 0·902 | 0·947** | 0·929 | 0·966 | 0·009 | <0·001 | ||||||
| Education | 1·047** | 1·014 | 1·081 | 0·017 | 0·005 | 1·127** | 1·106 | 1·148 | 0·011 | <0·001 | ||||||
|
Vaccine skeptics |
Vaccine believers |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference Category: Former skeptics | OR | Lower CI | Upper CI | SE | P-value | OR | Lower CI | Upper CI | SE | P-value | ||||||
| Gender | 0·799** | 0·663 | 0·963 | 0·076 | 0·008 | 1·210* | 1·029 | 1·421 | 0·100 | 0·035 | ||||||
| Māori | 1·170 | 0·929 | 1·473 | 0·138 | 0·216 | ·589** | 0·475 | 0·729 | 0·064 | <-0·001 | ||||||
| Pacific | 0·801 | 0·549 | 1·168 | 0·154 | 0·197 | ·508** | 0·358 | 0·722 | 0·091 | <0·001 | ||||||
| Asian | 1·318 | 0·857 | 2·029 | 0·290 | 0·272 | 0·938 | 0·637 | 1·381 | 0·185 | 0·737 | ||||||
| Age | 1·007* | 1·001 | 1·013 | 0·003 | 0·032 | 1·004 | 0·998 | 1·009 | 0·003 | 0·197 | ||||||
| Deprivation | 1·002 | 0·971 | 1·034 | 0·016 | 0·902 | 0·949** | 0·923 | 0·976 | 0·014 | <0·001 | ||||||
| Education | 0·955** | 0·925 | 0·986 | 0·016 | 0·004 | 1·076** | 1·046 | 1·107 | 0·016 | <0·001 | ||||||
Note: *p < 0·05, **p < 0·01, numbers in tables are rounded to 3 decimal points for greater accuracy.
Note: *p < 0·05, **p < 0·01, numbers in tables are rounded to 3 decimal points for greater accuracy.
Note: *p < 0·05, **p < 0·01, numbers in tables are rounded to 3 decimal points for greater accuracy.
Table A4.
Average latent class probabilities for most likely latent class membership (row) by latent class (column).
| 1 | 2 | 3 | |
|---|---|---|---|
| 1. Former skeptics | 0·843 | 0·101 | 0·056 |
| 2. Vaccine skeptics | 0·057 | 0·878 | 0·065 |
| 3. Vaccine believers | 0·014 | 0·085 | 0·901 |
Table A5.
Demographic characteristics of subpopulations based on most likely group membership.
| Gender |
Ethnicity |
Age (Time 5) |
Deprivation | Education | |||||
|---|---|---|---|---|---|---|---|---|---|
| Female (%) | Male (%) | Maori (%) | Pacific (%) | Asian (%) | Age range | Mean age (SD) | Mean level (SD) | Mean level (SD) | |
| Vaccine believers (N = 12826) | 60.81 | 39.19 | 10.55 | 2.69 | 4.30 | 17–94 | 49.72 (14.30) | 4.45 (2.70) | 5.36 (2.78) |
| Vaccine skeptics (N = 3388) | 67.89 | 32.11 | 19.45 | 4.90 | 4.78 | 18–94 | 50.03 (12.09) | 5.02 (2.78) | 4.53 (2.73) |
| Former skeptics (N = 1117) | 64.87 | 35.13 | 17.46 | 5.55 | 4.48 | 18–82 | 48.90 (13.66) | 4.96 (2.80) | 4.83 (2.82) |
Note: The current study initially aimed to make inferences about and look at population level trends in vaccine attitudes rather than identify the specific demographic breakdown of subpopulations. This is because our analyses were based on the probability of classification (not simple categorization) and thus, we need to be cautious about categorizing people into groups. Nevertheless, this data may inform the development of target vaccination interventions by helping identify groups of individuals most likely to fall into each subpopulation.
Ethnicity is not mutually exclusive (participants indicated all ethnic groups they identified with at each time point); Proportion for European is not included as it was used as reference category in the regression analysis that was used to obtain most likely class membership. Scale for deprivation (1=lowest, 10=highest) and education level (0=no qualification, 10=doctoral degree).
Appendix B. Supplementary materials
References
- 1.Ministry of Health . 2 ed. Ministry of Health; Wellington: 2018. Immunisation handbook 2017. [Google Scholar]
- 2.Strategic Advisory Group of Experts on Immunization . World Health Organization; Geneva: 2018. Assessment report of the Global Vaccine Action Plan. [Google Scholar]
- 3.World Health Organization. Ten threats to global health in 2019. Retrieved from https://www.who.int/emergencies/ten-threats-to-global-health-in-2019(Accessed 27 Feb 2020)
- 4.Dubé E, Vivion M, MacDonald NE. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: influence, impact and implications. Expert Re Vaccines. 2015;14:99–117. doi: 10.1586/14760584.2015.964212. [DOI] [PubMed] [Google Scholar]
- 5.MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 6.Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine. 2014;32:2150–2159. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 7.Hviid A, Hansen JV, Frisch M, Melbye M. Measles, mumps, rubella vaccination and autism: a nationwide cohort study. Ann Intern Med. 2019;170(8):513–520. doi: 10.7326/M18-2101. [DOI] [PubMed] [Google Scholar]
- 8.The Institute of Environmental Science and Research Ltd . 2015. Annual Summary of Outbreaks in New Zealand 2014. Wallaceville, New Zealand. [Google Scholar]
- 9.Ministry of Health. National and DHB immunisation data. 2019. Retrieved from http://www.health.govt.nz/our-work/preventative-healthwellness/immunisation/immunisation-coverage/national-and-dhbimmunisation-data (Accessed 27 Feb 2019).
- 10.Ministry of Health . Ministry of Health; Wellington: 2007. The National Childhood Immunisation Coverage Survey 2005. [Google Scholar]
- 11.Litmus . Litmus; Wellington: 2013. Audience research: delayers of infant immunisation. [Google Scholar]
- 12.Lee CH, Duck IM, Sibley CG. Personality and demographic correlates of New Zealanders’ confidence in the safety of childhood vaccinations. Vaccine. 2017;35:6089–6095. doi: 10.1016/j.vaccine.2017.09.061. [DOI] [PubMed] [Google Scholar]
- 13.Jansen P, Bacal K, Crengle S. Mauri Ora Associates; Auckland: 2008. He Ritenga Whakaaro: Māori experiences of health services. [Google Scholar]
- 14.Walker L, Ward E, Gambitsis D. Allen and Clarke; Wellington: 2019. Improving New Zealand's childhood immunisation rates. [Google Scholar]
- 15.Kornides ML, McRee AL, Gilkey MB. Parents who decline HPV vaccination: who later accepts and why? Acad Pediatr. 2018;18(2):S37–S43. doi: 10.1016/j.acap.2017.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gilkey MB, McRee AL, Magnus BE, Reiter PL, Dempsey AF, Brewer NT. Vaccination confidence and parental refusal/delay of early childhood vaccines. PLoS One. 2016;11(7) doi: 10.1371/journal.pone.0159087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sibley CG. Sampling procedure and sample details for the New Zealand Attitudes and Values Study. NZAVS Tech Doc. 2020 [Google Scholar]
- 18.Sibley CG. Comparison of demographics in the NZAVS and New Zealand census. NZAVS Tech Doc. 2014 [Google Scholar]
- 19.Salmond C, Crampton P. University of Otago; Dunedin: 2013. NZDep2013 Index of Deprivation. [Google Scholar]
- 20.Asparouhov T, Muthén B. Auxiliary variables in mixture modeling: three-step approaches using M plus. Struct Eq Model: Multidiscip J. 2014;21:329–341. [Google Scholar]
- 21.Osborne D, Sibley CG. Identifying “types” of ideologies and intergroup biases: advancing a person-centred approach to social psychology. Eur Rev Soc Psychology. 2017;28:288–332. [Google Scholar]
- 22.Kim SY. Determining the number of latent classes in single-and multiphase growth mixture models. Struct Eq Model: Multidiscip J. 2014;21:263–279. doi: 10.1080/10705511.2014.882690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tofighi D, Enders CK. Identifying the correct number of classes in growth mixture models. Adv Latent Var Mix Models. 2008;2007:317–341. [Google Scholar]
- 24.Leask J, Chapman S, Hawe P, Burgess M. What maintains parental support for vaccination when challenged by anti-vaccination messages? A qualitative study. Vaccine. 2006;24(49-50):7238–7245. doi: 10.1016/j.vaccine.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 25.Gust DA, Kennedy A, Shui I. Parent attitudes toward immunizations and healthcare providers: the role of information. Am J Prev Med. 2005;29:105–112. doi: 10.1016/j.amepre.2005.04.010. [DOI] [PubMed] [Google Scholar]
- 26.Pal M, Goodyear-Smith F, Exeter D. Factors contributing to high immunisation coverage among New Zealand Asians. J Primary Health Care. 2014;6(4):304–311. [PubMed] [Google Scholar]
- 27.Petousis-Harris H, Goodyear-Smith F, Godinet S, Turner N. Barriers to childhood immunisation among New Zealand mothers. N Z Family Physi. 2002;29(6):396–401. [Google Scholar]
- 28.Freed GL, Clark SJ, Butchart AT. Sources and perceived credibility of vaccine-safety information for parents. Pediatrics. 2011;127:S107–S112. doi: 10.1542/peds.2010-1722P. [DOI] [PubMed] [Google Scholar]
- 29.Ministry of Health . Ministry of Health; Wellington: 2013. Patient Experience 2011/12: Key findings of the New Zealand Health Survey. [Google Scholar]
- 30.Ministry of Health. Tier 1 statistics 2017/18: New Zealand Health Survey. 2019. Retrieved from https://www.health.govt.nz/publication/tier-1-statistics-2017-18-new-zealand-health-survey(Accessed 27 Feb 2020).
- 31.Ludeke M, Puni R, Cook L, Pasene M, Abel G, Sopoaga F. Access to general practice for Pacific peoples: a place for cultural competency. J Prim Health Care. 2012;4:123–130. [PubMed] [Google Scholar]
- 32.Veerasingam P, Grant CC, Chelimo C. Vaccine education during pregnancy and timeliness of infant immunization. Pediatrics. 2017;140 doi: 10.1542/peds.2016-3727. [DOI] [PubMed] [Google Scholar]
- 33.Charron J, Gautier A, Jestin C. Influence of information sources on vaccine hesitancy and practices. Médecine et Maladies Infectieuses. 2020 doi: 10.1016/j.medmal.2020.01.010. [DOI] [PubMed] [Google Scholar]
- 34.Healy CM, Pickering LK. How to communicate with vaccine-hesitant parents. Pediatrics. 2011;127:S127–S133. doi: 10.1542/peds.2010-1722S. [DOI] [PubMed] [Google Scholar]
- 35.Gust DA, Woodruff R, Kennedy A. Parental perceptions surrounding risks and benefits of immunization.. Proceedings of the seminars in pediatric infectious diseases; Philadelphia: WB Saunders; 2003. pp. 207–212. [DOI] [PubMed] [Google Scholar]
- 36.D'Alessandro A, Napolitano F, D'Ambrosio A. Vaccination knowledge and acceptability among pregnant women in Italy. Hum Vaccin Immunother. 2018;14:1573–1579. doi: 10.1080/21645515.2018.1483809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van Prooijen JW. Why education predicts decreased belief in conspiracy theories. Appl Cogn Psychol. 2017;31:50–58. doi: 10.1002/acp.3301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pew Research Center . Pew Research Centre; Washington: 2012. Assessing the Representativeness of Public Opinion Surveys. [Google Scholar]
- 39.Satherley N, Milojev P, Greaves LM, Huang Y, Osborne D, Bulbulia J, Sibley CG. Demographic and psychological predictors of panel attrition: Evidence from the New Zealand attitudes and values study. PLoS One. 2015;10(3) doi: 10.1371/journal.pone.0121950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sibley CG, Robertson A, Osborne D, Huang Y, Milojev P, Greaves LM, Houkamau CA, Bulbulia J, Barlow FK. Bias and tracking accuracy in voting projections using the New Zealand attitudes and values study. Polit Sci. 2017;69(1):16–34. [Google Scholar]
- 41.Larson HJ, Cooper LZ, Eskola J, Katz SL, Ratzan S. Addressing the vaccine confidence gap. The Lancet. 2011;378(9790):526–535. doi: 10.1016/S0140-6736(11)60678-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.