Abstract
Background:
Alcohol expectancies and externalizing behaviors, that is, aggression and rule-breaking behaviors, are associated with underage alcohol use. The interactive influence of these risk factors on problem alcohol use among minority adolescents is investigated in the present study.
Objectives:
This study examined the unique and interactive influences of alcohol expectancies and externalizing problems on specific measures of adolescents’ (a) past three-month binge drinking episodes and (b) negative consequences of alcohol use.
Methods:
Cross-sectional self-report data were collected in 2014 via tablet-based computerized assessments from a predominantly minority sample of 762 (404 females, Mage = 13.73 years, SDage =1.59) 6th, 8th, and 10th grade students recruited from public middle and high schools in Miami-Dade County, FL and Prince George’s County, MD. Students completed surveys on tablets in school settings regarding alcohol expectancies, expectancy valuations, externalizing problem behaviors, past 3-month binge drinking episodes, and experiences of alcohol-related negative consequences.
Results:
Zero-inflated negative binomial regressions indicated: (1) older adolescents were more likely to report binge drinking; and (2) a significant main effect for externalizing problem behaviors on binge use. Logistic regressions indicated (1) older adolescents were more likely to endorse an alcohol-related negative consequence and (2) the interaction between positive alcohol expectancies and externalizing behaviors was associated with endorsing an alcohol-related negative consequence.
Conclusions:
Engaging adolescents who exhibit serious externalizing behaviors and report positive alcohol expectancies via developmentally appropriate, tailored interventions is one feasible strategy to address escalation of binge alcohol use and related negative consequences among minority youth.
Keywords: adolescent health
Excessive underage alcohol use is a pervasive public health problem in the United States. Of particular concern is binge drinking, defined as five or more drinks for men or four or more drinks for women within a two-hour period. In 2018, prevalence rates for 8th, 10th, and 12th graders reporting binge drinking within the previous two weeks were 3.7%, 8.7%, and 13.8%, respectively.1 Adolescents reporting binge alcohol use are at higher risk for a number of negative consequences, including altered brain development,2 physical and sexual assault experiences,3,4 HIV-risk behaviors,5 accidental injuries,6 driving while intoxicated,7 and premature mortality.8 Negative health outcomes associated with excessive underage alcohol use confer alarming social and economic costs, recently estimated at $27 billion,9 making this one of the greatest preventable risks to health and developmental outcomes among adolescents.
Earlier age of alcohol use onset is associated significantly with binge alcohol use and with the development of alcohol use disorders (AUDs). Longitudinal and cross-sectional studies have documented significant associations between earlier age of onset of regular alcohol use and earlier onset of alcohol-related problems and psychopathology,10 including greater likelihood of future alcohol dependence,11 rapid trajectories into alcohol dependence and multiple relapses between episodes of dependence.12 Binge alcohol use may serve as a marker of progression toward problem alcohol use, and as such, screening for binge alcohol use is a critical selected prevention strategy for use with young adolescents.
Screening adolescents for alcohol use and understanding associated risk factors provides opportunities to prevent or reduce risk for early-stage problem alcohol use and related negative consequences. Screening, Brief Intervention, and Referral to Treatment (SBIRT) is an evidence-based selected prevention paradigm promoting individual assessments to determine the presence and severity of alcohol use and linking clients to brief, developmentally-appropriate forms of intervention or referring them out for more intensive treatment services.13 Embedded within SBIRT is the implementation of specific behavior change strategies to increase clients’ insight and awareness regarding the negative impact of substance use and build their motivation for positive behavioral change. For adolescents reporting severe patterns of underage alcohol use, this can be paired with referrals to more intensive, structured treatment services.14 The specific type of intervention or referral could be tailored, depending on co-occurring psychological and/or behavioral risk.
It is estimated that only 7.6% of adolescents who need substance use treatment actually receive these services.14 The gap between service needs and service utilization provides a rationale for using SBIRT to increase access to intervention services by screening underserved adolescents for unhealthy underage alcohol use and facilitating their engagement in selected prevention programs.15 Reviews indicate that brief motivational interventions may promote long-term reductions in alcohol use16 and are suitable for use with adolescents in health care, school and community settings.17 SBIRT represents a promising strategy for the early identification of adolescents at greatest risk for developing problem alcohol use, and implementing interventions targeting specific risk factors when they are likeliest to have impact. Therefore, understanding how multiple risk factors predict risky alcohol use provides clinicians useful information about modifiable psychological or behavioral profiles that co-occur, providing a target for brief intervention or treatment referral in students who screen positive for problem drinking.
Alcohol expectancies, or one’s beliefs about probable outcomes of alcohol use, are a significant risk factor for unhealthy underage alcohol use. Expectancy theory posits that individuals are motivated by their expected probability of receiving a valued reward.18 This conceptual framework suggests that adolescents’ alcohol consumption is partly explained by their positive and negative expectations vis-à-vis probable alcohol use outcomes. In particular, positive expectancy factors, including perceptions of enhanced sociability, courageousness, improved sexual functioning, and relaxation, serve to motivate alcohol consumption.19 Research indicates that onset of alcohol use increases the development of positive social- and relaxation-related alcohol expectancies, which in turn predict alcohol-related problems.20 One study found that adolescents 13 to 16 years old with AUD symptoms reported the highest positive expectancy scores, compared to other age groups.21 Individuals reporting more severe patterns of alcohol use, including binge drinking also report more specific positive alcohol-related expectancies, like enhanced sexual performance and increased power and aggression.22,23
Expectancy valuations may also contribute to adolescents’ severe alcohol use, above and beyond the effect of outcome expectancies. Expectancy valuations differ from outcome expectancies, such that valuations determine whether an adolescent perceives an expected outcome as good or bad, while outcome expectancies focus on whether an anticipated outcome will occur. This distinction is relevant, as positive alcohol expectancies and positive valuations have been shown to predict different alcohol use behaviors.24,25 A full model of adolescent alcohol use, therefore, must consider the desirability of positive expectancies because of their ability to reinforce alcohol use,26 which in turn can promote increasingly severe patterns of use.
Another significant risk factor for adolescents’ unhealthy alcohol use is past history of externalizing behaviors, including antisocial behaviors (e.g., generalized delinquency, rule-breaking), aggressive behaviors (e.g., bullying, interpersonal violence) behaviors, and psychopathology directed at the external environment (e.g., aggression, hyperactivity). Developmental frameworks for externalizing behaviors suggest these behaviors in early adolescence may serve as risk factors which promote and accelerate adolescents’ substance use in later adolescence.27 One study found that delinquent behaviors at age 13 years were independently associated with increases in adolescents’ alcohol use at age 17 years, controlling for initial levels of alcohol consumption.28
Externalizing symptoms of disruptive behavior disorders appear to accelerate the progression of adolescents’ AUD symptoms.29 One longitudinal study found that diagnosis of any DSM-V externalizing domain disorder during early adolescence, defined as ADHD, ODD, CD, or non-alcohol-related Substance Use Disorders (SUDs), significantly predicted earlier time to AUD onset during late adolescence and early adulthood.30 Similarly, teachers’ reports of adolescents’ externalizing behaviors at age 9 differentiated males based on assignment of an AUD diagnosis status at age 28.31 These studies and others suggest that externalizing behaviors are a robust risk factor for acceleration of individuals’ alcohol consumption and subsequent onset of AUDs.
Adolescents’ alcohol expectancies, valuations and externalizing behaviors represent appropriate risk factors to consider when identifying adolescents at high risk for early-stage alcohol use problems and related negative consequences, as they may be likely to co-occur. SBIRT, implemented in a developmentally-informed manner in the context of public schools or other community settings, may provide prevention specialists with access to identify adolescents reporting binge drinking and early-stage alcohol problems.32 Previous school-based approaches to brief assessment and intervention have shown positive impacts on adolescents’ externalizing behaviors and substance use.33 Therefore, understanding the psychological and behavioral profiles that tend to co-occur with problem alcohol use in a school-based sample of minority youth would inform service providers with prevention and intervention targets for high-risk students.
It is important to note that structural disparities are likely to limit minority youths’ access to high-quality behavioral health services, compared to their White counterparts. African-American and Hispanic/Latino adolescents with SUDs are consistently less likely than White adolescents to receive substance use intervention services.34 At the same time, minority adolescents with SUDs are more likely to be tracked into criminal justice rather than mental health care systems. For example, African-American youth report lower levels of substance use compared to White youth, but they are more likely to be arrested for substance-related offenses, indicating inequities in current enforcement practices.35 Therefore, it is critical for service providers to meet the unique needs of underserved minority adolescents. Screening minority youth in schools or other community settings and identifying youth at elevated risk for problem trajectories of alcohol use represents an underutilized strategy to facilitate their engagement with targeted prevention tactics.
The “deviance proneness” model36 identifies both externalizing behaviors and positive alcohol expectancies, among other significant risk factors, as important variables that influence adolescents’ alcohol use outcomes, including binge alcohol use episodes and alcohol-related negative consequences. This model suggests co-exposure to risk factors are likely additive effects; however, unknown is whether high levels of both risk factors creates an interactive effect, especially among minority adolescents. For example, would the amount of positive alcohol expectancies endorsed more greatly predict the extent to which externalizing behaviors predict risky drinking in this population, compared to either risk factor alone? Determining whether these risk factors interact would elaborate upon the deviance proneness model via identification of risk factor combinations that predict high levels of problem alcohol use. Understanding the interconnection between risk factors and alcohol misuse in school-aged minority youth would improve targeted prevention initiatives, such as school-based SBIRT, by promoting tailored brief interventions or treatment referrals addressing both risk factors as high-risk students are screened and identified. This could serve minority adolescents more effectively and mitigate in part the structural factors preventing these youth from accessing intervention services. This supports a rationale for examining how interactions between alcohol expectancies/valuations and externalizing behaviors may predict outcomes such as adolescents’ (a) binge alcohol use and (b) negative alcohol-related consequences in an ethnically diverse, school-based sample of middle and high school students.
Hypotheses: Controlling for age and gender, interactions between externalizing behaviors and positive alcohol expectancies/valuations will be associated with adolescents’ (a) binge alcohol use and (b) alcohol-related negative consequences. Specifically, adolescents endorsing high levels of both risk factors will report higher scores for these unhealthful underage alcohol use outcomes.
Method
Participants
In 2014, a sample of 762 students ranging from 11 to 18 years old (53% female, Mage = 13.73 years, SD = 1.59) was recruited from a total of 14 public middle and high schools in Miami-Dade County, Florida (56.1% of the sample) and Prince George’s County, Maryland (43.9%). The sample consisted of 6th graders (25.2%), 8th graders (37.1%) and 10th graders (37.4%). The sample was predominately comprised of ethnic minority individuals, self-identified as Hispanic/Latino (41.4%), African-American (39.6%), White (8.7%), Asian (5.2%), or other/mixed ethnicity (5.2%). Seventy-five percent of participants were born in the US. One 18-year-old was an outlier in terms of age and was removed from the sample for our analyses.
Measures
Alcohol Expectancies and Valuations were assessed using the Brief Comprehensive Effects of Alcohol (B-CEOA) Questionnaire.37 The B-CEOA contains 15 items to which respondents indicate their degree of agreement that a particular effect will occur as a result of alcohol use on a 0 to 3 scale, from 0 = disagree to 3 = agree. For example, positive expectancies include enhanced sociability (e.g., “It would be easier to talk to people”), courageousness (e.g., “I would feel bold and daring”), enhanced sexuality (e.g., I would enjoy sex more), and relaxation (e.g., “I would feel calm”). Respondents indicated their valuations of these expectancies by rating whether and to what degree that effect would be desirable or undesirable on an 0 to 4 scale, from 0 = bad to 4 = good. The B-CEOA has successfully measured alcohol expectancies and valuations in diverse samples of middle38 and high school39 students. In the present sample, the Cronbach’s alpha estimates were .80 for positive expectancies, .82 for negative expectancies, .88 for positive valuations, and .78 for negative valuations.
Externalizing Behaviors were assessed using the aggressive behavior and rule-breaking subscales from the Youth Self-Report (YSR;40). The aggressive behaviors subscale contains 17 items (e.g., “I get in many fights), and the rule-breaking subscale contains 15 items (e.g., “I break rules at home or elsewhere). For both scales, respondents indicate whether the item is not true (0), sometimes true (1), or often true (2) of them. These scales from the YSR have been implemented in previous studies with samples of middle41 and high school42 students, in which Hispanic/Latino youth were highly represented. In the present sample, Cronbach’s alpha estimates were .85 for the aggressive behavior and .75 for the rule-breaking subscales.
Binge Drinking was assessed using one item adapted from the Monitoring the Future Study (1): “How many occasions have you had four (for women)/five (for men) or more alcoholic drinks in a single day within the past three months (0-90 days)?” Items from the Monitoring the Future Study are regularly used to assess substance use and related factors in samples of middle and high school students,1 which are nationally-representative in terms of their racial/ethnic diversity.
Negative Alcohol-Related Consequences were assessed using the Short-Rutgers Alcohol Problem Index (S-RAPI;43). The S-RAPI contains 16 items assessing negative consequences of alcohol use in multiple domains of functioning (e.g., physical, school, legal, family, and social consequences). Respondents indicate how many times they have experienced an effect while they are drinking alcohol or as a result of their alcohol use (e.g., “Not able to do your homework or study for a test”) within the last year on a 0 to 3 scale (0 = never, 1 = 1-2 times, 2 = 3-5 times, 3 = more than 5 times). A previous study utilizing the present sample showed the S-RAPI demonstrates adequate validity in detecting alcohol-related problems for primarily African-American and Hispanic/Latino 6th, 8th, and 10th grade students.44 The Cronbach’s alpha estimate for the S-RAPI was .88 in the present sample.
Procedure
The data for the current study were derived from the baseline dataset of a larger, multi-site evaluation of a brief two-item screener for underage alcohol use developed by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) and the American Academy of Pediatrics (AAP). For this study, all 6th, 8th, and 10th graders attending participating middle schools and high schools in Miami-Dade County, FL (n = 8) and Prince George’s County, MD (n = 6) were eligible; however, only students whose parents completed a parental consent form were subsequently enrolled. Students completed assessments during school hours on individual computerized tablets. The assessment battery included measures of substance use, health risk behaviors, and parent-child relationships, among other constructs. The survey took approximately 45 minutes to complete and students received $25 gift cards to a national electronics retailer as compensation for their time involved in survey completion.
Data analytic strategy
Data were analyzed using R version 3.3.045 and SPSS version 22.046. Several variables (i.e., YSR subscales, S-RAPI scores, binge drinking counts) were missing < 2% of cases; missing cases from subscales of the B-CEOA ranged from 12.9% to 17.3%. Data missing from the B-CEOA were less likely, compared to the other variables included in this study, to be missing randomly, since adolescents who did not report alcohol use were less likely to complete the B-CEOA. Missing data were imputed using the package Amelia II version 1.6.4.47 Five values were imputed for each missing data point, resulting in five datasets with different imputations. Regressions were run on each dataset and results were combined using a maximum likelihood estimator. Next, regression diagnostics identified violations of normality assumptions for the distributions of outcome variables. Given the low frequency of negative alcohol-related consequences in the current sample, logistic regression was used to model this outcome assessed as a dichotomous variable; odds ratios (ORs) for this model are interpreted as the change in likelihood of negative alcohol consequences with a one-unit increase in the independent variable.
The binge drinking variable was characterized by positive skew and zero-inflation. Zero-Inflated Poisson (ZIP) and Negative Binomial (ZINB) regression models were explored in R using the MASS48 package. Both models account for excess zeros within the data (i.e., in this case, adolescents who have never consumed alcohol) and both are useful in cases in which counts for the dependent variable (i.e., amount of binge drinking for adolescents who have initiated alcohol use) are relatively rare events. The ZIP model proved to be a poor fit to the data, as the regression coefficients were highly distorted.
The ZINB model proved to be a better fit to the data in the present study. This model is less restrictive and allows the conditional variance of an outcome to be greater than the conditional mean of the outcome49; in our case where the mean for binge drinking days was 0.007 and the standard deviation was .59, this large difference supports the use of the ZINB model. A likelihood ratio test comparing the ZIP versus ZINB models goodness-of-fit (χ2 = 3.22, P < .01) supported the superiority of the ZINB model, as did Akaike Information Criterion which suggested the ZINB model’s quality was more parsimonious (231.39) when compared to the ZIP model (232.61). Incidence rate ratios (IRR) were calculated from the ZINB model coefficients and represent the multiplicative increase in the expected count with each one-unit increase in the independent variable, with other variables held constant. The odds ratio (OR) value for the zero-inflation component represents the predicted change in the odds of the model containing excess zeros (i.e., alcohol abstainers) with each one-unit increase in the independent variable. If the OR is greater than one, an increase in the independent variable increases the odds of a certain zero occurring (i.e., being an alcohol abstainer;50).
Given the large magnitude of correlation between positive alcohol expectancies and positive expectancy valuations, we examined these variables using separate models, in order to minimize the effects of multicollinearity.51 Our conceptual rationale for this decision is that alcohol expectancies and valuations are related, yet different constructs that contribute unique effects on adolescent drinking outcomes.24 Therefore, in lieu of dropping either predictor, we created different models for expectancies versus valuations to test our hypotheses.
Results
Self-reported alcohol use was low. Most adolescents reported zero past three-month binge drinking days (97%) and zero alcohol-related negative consequences (92%). Table 1 presents means, standard deviations, skewness, kurtosis, and Pearson bivariate correlations for each variable. All predictor variables were significantly correlated with one another, with the highest correlation between positive expectancies and positive expectancy valuations (r = 0.57). Binge drinking days and alcohol-related negative consequences were significantly correlated with one another (r = 0.40).
Table 1.
Means, standard deviations, skewness, kurtosis, and Pearson correlations among variables.
| VARIABLE | 1. | 2. | 3. | 4. | 5. | |
|---|---|---|---|---|---|---|
| 1. | Positive Expectancies | 0.57* | 0.32* | 0.13* | 0.25* | |
| 2. | Positive Valuations | 0.25* | 0.12* | 0.23* | ||
| 3. | Externalizing Problem Behaviors | 0.13* | 0.26* | |||
| 4. | Past 3-Month Binge Days | 0.40* | ||||
| 5. | S-RAPI Alcohol Problems | |||||
| Minimum | 0 | 0 | 0 | 0 | 0 | |
| Maximum | 3 | 4 | 1.33 | 5 | 1.8 | |
| Mean | 0.86 | 1.33 | 0.29 | 0.07 | 0.08 | |
| Standard Deviation | 0.74 | 1.00 | 0.23 | 0.59 | 0.27 | |
| Skew | 0.55 | 0.36 | 1.18 | 10.42 | 3.10 | |
| Kurtosis | −0.51 | −0.63 | 1.64 | 122.57 | 7.64 | |
Notes:
= p <01.
S-RAPI, Short-Rutgers Alcohol Problem Index.
Binge drinking
Results from the ZINB regression model conducted to test the interaction between positive expectancies and externalizing behaviors as a predictor of past 3-month binge drinking days are summarized in Table 2. Two significant main effects emerged in the zero-inflation portion of the model: older age (OR = 0.419, P < .05), and more externalizing problem behaviors (OR = 3.8e-7, P < .05) were both associated with decreased odds of belonging to the alcohol abstainer class. The hypothesized interaction was non-significant. For the count portion of the model, no significant main effects nor the hypothesized interaction were revealed.
Table 2.
ZINB model testing the interaction between positive expectancies and externalizing problem behaviors on adolescents’ past 3-month binge drinking days.
| ZERO-INFLATION MODEL | COUNT MODEL | |||||
|---|---|---|---|---|---|---|
| OR | SE | Z | IRR | SE | Z | |
| Gender | 0.985 | 0.95 | −0.02 | 3.665 | 0.90 | 1.44 |
| Age | 0.419 | 0.36 | −2.44* | 1.129 | .30 | .41 |
| Positive Expectancies | 0.047 | 1.89 | −1.62 | 0.376 | 1.92 | −.51 |
| EPBs | 3.8e−7 | 6.98 | −2.12* | 0.002 | 5.26 | −1.13 |
| PositiveExpectanciesXEPBs | 1171.67 | 4.12 | 1.72 | 63.865 | 3.62 | 1.15 |
Notes:
= P < .05.
= P < .01.
EPBs, Externalizing Problem Behaviors.
The interpretation indices for the ZINB model include both the Odds Ratio (OR) and the Incidence Rate Ratio (IRR) values. The OR is interpreted as the change in odds of belonging to the “alcohol abstainer” class, while the IRR is interpreted as the change in count for binge drinking days of those not in the “alcohol abstainer” class.
Results of the ZINB model testing the interaction between positive valuations and externalizing behaviors as a predictor of past three-month binge drinking days are summarized in Table 3. Age again emerged as a significant main effect in the zero-inflation portion of the model (OR = 0.350, P < .05). Older age was again associated with decreased odds of belonging to the alcohol abstainer class. The hypothesized interaction was non-significant. For the count portion of the model, no significant main effects nor the hypothesized interaction were revealed
Table 3.
ZINB model testing the interaction between positive valuations and externalizing problem behaviors on adolescents’ past three-month binge drinking days.
| ZERO-INFLATION MODEL | COUNT MODEL | |||||
|---|---|---|---|---|---|---|
| OR | SE | Z | IRR | SE | Z | |
| Gender | 0.285 | 0.95 | −.93 | 1.708 | .87 | .62 |
| Age | 0.350 | 0.36 | −2.37* | 1.154 | .36 | .40 |
| Positive Valuations | 0.756 | 1.89 | −.28 | 1.048 | .85 | .06 |
| EPBs | 0.163 | 6.98 | −.36 | .701 | 3.15 | −.11 |
| PositiveValuationsXEPBs | 0.176 | 4.12 | −.57 | 1.258 | 1.19 | .19 |
Notes:
= P < .05.
= P < .01.
EPBs = Externalizing Problem Behaviors.
The interpretation indices for the ZINB model include both the Odds Ratio (OR) and the Incidence Rate Ratio (IRR) values. The OR is interpreted as the change in odds of belonging to the “alcohol abstainer” class, while the IRR is interpreted as the change in count for binge drinking days of those not in the “alcohol abstainer” class.
Negative alcohol-related consequences
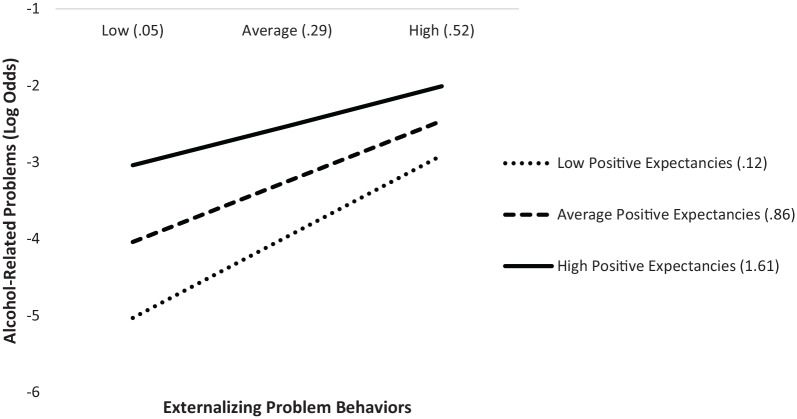
Results from the logistic regression model testing the interaction between positive expectancies and externalizing behaviors on alcohol-related negative consequences are presented in Table 4. Age emerged as a significant main effect (OR = 1.707, P < .001). The hypothesized interaction between positive expectancies and externalizing behaviors was significant (OR = 0.206, P < .05). Simple slope analysis revealed that students were at greatest risk for experiencing an alcohol-related problem when positive expectancies were high. However, the strength of the positive slope between externalizing behaviors and an alcohol-related problem decreased as expectancies grew. This effect was significant at low (i.e., 0.12, or one standard deviation below the mean expectancy score; β = 4.52, P < .001) levels of positive expectancies, and decreased in strength as expectancies reached average (i.e., 0.86; β = 3.35, P < .001) and high (i.e., 1.61, or one standard deviation above the mean expectancy score; β = 2.18, P < .001) levels. This two-way interaction is plotted in Figure 1.
Table 4.
Logistic regression model predicting adolescents’ negative alcohol-related consequences from the interaction between positive expectancies and externalizing problem behaviors.
| B | SE | Z | OR | |
|---|---|---|---|---|
| Age | 0.535 | 0.122 | 4.383** | 1.707 |
| Gender | 0.360 | 0.300 | 1.203 | 1.433 |
| Positive Expectancies | 1.437 | 0.396 | 3.632** | 4.208 |
| EPBs | 4.719 | 1.303 | 3.623** | 112.00 |
| PositiveExpectanciesXEPBs | −1.580 | 0.779 | −2.037* | 0.206 |
Notes:
= P < .05.
P < .001.
EPBs = Externalizing Problem Behaviors.
Figure 1.
Conditional effect of externalizing problem behaviors on adolescents’ negative alcohol-related consequences as moderated by positive expectancies.
Note: Log Odds range from -∞ to ∞.
Results of the logistic regression model testing the interaction between positive valuations and externalizing behaviors on negative alcohol-related consequences are presented in Table 5. Age (OR = 1.697, P < .001) and positive valuations (OR = 1.777, P < .05) emerged as significant main effects of negative alcohol-related consequences. The hypothesized interaction was non-significant for this model.
Table 5.
Logistic regression model predicting adolescents’ negative alcohol-related consequences from the interaction between positive valuations and externalizing problem behaviors.
| B | SE | Z | OR | |
|---|---|---|---|---|
| Age | 0.529 | 0.119 | 4.440** | 1.697 |
| Gender | 0.494 | 0.265 | 1.634 | 1.693 |
| Positive Valuations | 0.575 | 0.265 | 2.167* | 1.777 |
| EPBs | 2.169 | 1.280 | 1.694 | 8.754 |
| PositiveValuationsXEPBs | 0.176 | 0.563 | 0.312 | 1.192 |
Notes:
= P < .05.
= P < .001.
EPBs, Externalizing Problem Behaviors.
Discussion
The inflated IRR value (3.8e-7) for the externalizing problem behaviors variable in the ZINB model predicting binge alcohol use does not lend itself to practical interpretation regarding counts of binge alcohol use. This inflated coefficient is perhaps best understood by considering that the NB model includes a random component reflecting uncertainty about the true rates at which events occur for individual cases, which more accurately characterizes uncertainty in prediction when compared to Poisson models.51 Therefore, while revealing a statistically significant relationship, we present our data and conclusions as exploratory regarding adolescent binge drinking, given the inflated coefficient.
With this caveat noted, our study examined the interplay of alcohol expectancies and expectancy valuations with externalizing problems, vis-à-vis past 3-month binge drinking and negative alcohol-related consequences, in a sample of predominantly African-American and Hispanic/Latino adolescents from two major metropolitan areas. Our findings suggested significant predictive relations for positive alcohol expectancies and externalizing problem behaviors regarding the presence and frequency of adolescents’ early-stage alcohol use problem outcomes.
Our analyses revealed a main effect of age: older adolescents were more likely to report a past 3-month binge drinking day and report negative alcohol-related consequences. This finding may reflect age-related differences between young and older adolescents in cumulative experience with alcohol use.52 As reports of episodes of binge drinking tend to rise starting around age 16 years,53 our results reveal this alcohol use is likely not without negative consequences. As our sample contained 6th, 8th, and 10th graders, this finding suggests that adolescents perhaps begin to experience problem drinking around the 10th grade, as alcohol use in the 6th or 8th graders may be more exploratory or less harmful in nature (i.e., alcohol sipping, one serving per occasion).
Adolescents’ positive valuations did not emerge as a significant predictor of binge alcohol days. This does not align with prior research with early adolescents suggesting that positive valuations add explanatory power in predictive models of lifetime alcohol use.26 However, other research among samples of college students and alcohol-dependent inpatients, B-CEOA measurements of positive valuations did not significantly predict alcohol consumption.54 Positive valuations are perhaps more predictive of impairment related to alcohol use (compared to binge consumption), as they predicted S-RAPI measurements of negative alcohol-related consequences in our study. Therefore, valuations may not exhibit a differential effect on young minority adolescents’ binge alcohol use beyond expectancies, but rather may uniquely predict alcohol-related problems. More research is needed to determine the potential unique influences of positive valuations in comprehensive models of adolescent alcohol use.
In contrast, externalizing behaviors appeared to play a more central role in predicting early-stage alcohol use problems among adolescents in our sample. Externalizing behaviors exhibited consistent main effects across the logistic regression and the ZINB models, suggesting that increasing amounts of overt physical aggression, delinquent or antisocial behaviors, or bullying is associated with both recent binge-drinking and alcohol-related negative consequences. This finding aligns with prior research indicating that endorsement of such problem behaviors is associated with more severe alcohol-related outcomes that increase risk for the subsequent development of AUDs.22,23,55 Therefore, our findings suggest that minority students in public school settings who screen positive for problem alcohol use are concurrently at elevated risk for externalizing issues, perhaps likelier to violate zero tolerance policies in their middle and high schools.
Concerning our interaction finding between externalizing behaviors and alcohol expectancies, we found that high levels of both of these risk factors predicted the greatest odds of students endorsing an alcohol-related problem, confirming our hypothesis. These findings support a “deviance proneness” model of adolescent alcohol use. In this model, adolescents’ early-stage substance use problems are partially explained through interactions among conduct problems and alcohol expectancies, among other risk factors.36 Behavioral undercontrol, conceived as a construct consisting of aggression and delinquency, may influence adolescents’ alcohol involvement by increasing their positive alcohol expectancies.56 Corroborating research argues that the deviance proneness model may be extended to explain repeated episodes of binge use in later adolescence and subsequent progression into alcohol use problems during later adolescence.57 Our findings extend this model by suggesting that, among young minority adolescents with externalizing issues, those with higher levels of positive expectancies and/or aggressive and rule-breaking behaviors, are perhaps already experiencing alcohol-related problems as a result of their drinking, even if it is not reaching levels of binge consumption.
Regarding our interaction finding, we also note that, while high positive expectancies were associated with greatest risk at all levels of externalizing behaviors, the risk for alcohol-related problems increased more drastically for low expectancies as externalizing behaviors increased. In other words, while not reaching the same level of risk as those with high expectancies, the risk for an alcohol-related problem tended to increase rapidly as more externalizing behaviors were endorsed for those with lower expectancies. This finding may reflect the fact that positive expectancies tend to increase as adolescent’s experience with alcohol increases. For example, younger adolescents with externalizing issues, less experienced with alcohol’s psychological or behavioral effects, may have less expectations about what outcomes are likely to result from their drinking. This may put them at a more drastic likelihood to experience clinically-relevant consequences, like injuries, school, or family problems, as their externalizing issues increase. In contrast, adolescents with more experience with alcohol use perhaps have more expectations in general about potential drinking outcomes. As a result their rate of negative consequences may increase less drastically as externalizing issues increase, compared to those with low expectancies. Generally, however, higher scores for externalizing behaviors and positive expectancies were independently associated with S-RAPI scores in our study, and high levels of both risk factors was associated with the greatest predictive odds, suggesting, overall, our findings lend support to the deviance proneness model. Future work should look at adolescents with varying experience with alcohol use, as outcome expectations for alcohol change alongside drinking, meaning the relationships between expectancies and externalizing behaviors may change as well.
Our hypothesized interaction between alcohol expectancies/valuations and externalizing problem behaviors on adolescents’ binge alcohol use was not supported by our findings. Our non-significant findings are perhaps best understood with the caveat that this outcome variable was a rare event (3% of participants endorsed a binge drinking day and 1% endorsed more than one day). Although the conceptual framework of our hypotheses lends itself to testing interactions using a ZINB approach, significant statistical interactions may have emerged in a sample of adolescents with more extensive patterns of alcohol use.
Implications for prevention
Adolescence is a critical period for identifying and addressing early-stage alcohol use problems. School and community settings are critical locations for delivery of evidence-based prevention programs that mitigate risks involved in unhealthy underage alcohol use. This is particularly relevant for minority adolescents with less routine access to preventive care or behavioral health services. Research studies of SBIRT initiatives in school settings to increase access have shown promising results. For example, one study which implemented SBIRT in two urban New York public schools showed that nearly all students who screened positive for substance use (42% of the sample) voluntarily accepted at least one brief intervention session.58
Adaptations of SBIRT methods to enhance their ability to address the unique needs of minority adolescents include: proactively identifying youths in need of intervention, consistently implementing and delivering intervention services in specific settings, and using family-focused approaches to assessment and intervention.59,60 The results of the present study suggest that externalizing behaviors and positive alcohol expectancies are risk factors that may be incorporated within strategies to tailor intervention strategies after screening for unhealthy alcohol use. Recent research with the present sample has indicated that adolescents’ alcohol use were associated with co-occurring delinquent and aggressive behaviors.61 This highlights opportunities for SBIRT approaches for underage alcohol use to generalize to minority adolescents’ co-occurring externalizing behaviors. For example, our results suggest that youth screening positive for alcohol misuse are likelier to manifest externalizing behaviors, suggesting these youth would benefit from strategies targeting a range of problem behaviors, not limited to alcohol use. In our study, externalizing behaviors predicted both of these clinically-severe outcomes.
Identifying minority youth displaying externalizing behaviors is important, given they tend to be disproportionally targeted for disciplinary sanctions in school settings.62 Incorporating brief intervention programming or offering referrals to clinicians specializing in family-based therapeutic services may best address the needs of at-risk minority youth, as these approaches are among the most effective for reducing problem substance use. A recent meta-analysis comparing outpatient SUD treatments indicated that adolescents receiving family therapy showed large and consistent reductions in substance use and generalized delinquency.16,63 Brief interventions promoting positive family relationships may be particularly well-suited for adolescents with co-occurring externalizing behaviors.64 In particular, culturally-sensitive family-based therapies, with bilingual and/or ethnic minority service providers that incorporate cultural norms, values, and beliefs into their modalities, have reported larger reductions in African-American and Hispanic/Latino adolescents’ substance use, relative to comparison conditions.65 The results of our study suggest minority adolescents who screen positive for binge use or report negative alcohol-use consequences may benefit from brief interventions or referrals to treatments focused on these intervention modalities.
Our results also suggest interventions simultaneously targeting distorted positive alcohol expectancies can potentially aid in preventing or treating minority youth’s alcohol problems. These adolescents can then be referred towards brief intervention or treatment programs focused on modifying alcohol expectancies and valuations. For example, AlcoholEdu is a computer-based universal prevention program which challenges positive alcohol expectancies by presenting information about alcohol’s pharmacological effects in a non-judgmental manner and promoting discussion about clients’ cognitive distortions and/or contradictions about arousal expectancies. AlcoholEdu implemented among college freshmen significantly reduced their scores for alcohol use and alcohol-related negative consequences at follow-up66 and reduced positive expectancies and increased negative expectancies.67 Another study showed that family-based cultural socialization, in which family members teach adolescents about the importance of their ethnic/cultural background, increased minority adolescents’ negative arousal expectancies about alcohol, which in turn was associated with reductions in their consumption.68 Our results suggest that minority youth with distorted alcohol expectancies and externalizing behaviors are at-risk for clinically severe alcohol use and may benefit from intervention programs designed to decrease both of these risk factors. Brief intervention programming incorporating challenges to distorted cognitions may be particularly efficacious.
This study’s results should be interpreted in light of its limitations. First, high-risk adolescents are likely underrepresented because they may have been less likely to turn in parental consent forms or be present in school on a recruitment or assessment day. Second, the study is limited by its reliance on self-report measures, although computerized data collection provided participants with enhanced privacy and confidentiality, with regard to underage alcohol use.69 Third, the distorted ZINB regression model coefficient, while revealing statistically significant relations between risk factors for adolescents’ substance use, do not lend themselves to practical interpretations. Last, the number of adolescents endorsing either binge-drinking or alcohol-related negative consequences was quite low. Although we modeled our predictions for these variables using strategies to account for excess zeros (i.e., abstainers), future research should examine these outcomes in an older, clinical sample of adolescents with diagnosed AUDs.
Despite these limitations, this study documented that 1) older age and externalizing problem behaviors independently predicted binge alcohol use and 2) these variables interacted to predict negative alcohol-related consequences in a large school-based sample of minority youth. Our results have implications for the application of SBIRT interventions to identify adolescents reporting patterns of unhealthful alcohol use and negative consequences, as well as to promote treatment referrals targeting distorted alcohol expectancies and externalizing behaviors.
Footnotes
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding:The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: *The study from which the data were derived for this article was funded by Grant R01 AA021888.
Author contribution: TR: conceptualization, formal analysis, investigation, writing–original draft, review, & editing of the final manuscript.
JGT: resources, writing–review & editing, supervision, project administration, funding acquisition.
SJS: resources, writing–review & editing, supervision, project administration, funding acquisition.
ORCID iD: Timothy Regan  https://orcid.org/0000-0001-9886-8809
https://orcid.org/0000-0001-9886-8809
References
- 1. Miech RA, Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, Patrick ME. Monitoring the Future National Survey Results on Drug Use, 1975–2018: Volume I, Secondary School Students. Ann Arbor: Institute for Social Research, The University of Michigan; 2019:610. [Google Scholar]
- 2. Welch KA, Carson A, Lawrie SM. Brain structure in adolescents and young adults with alcohol problems: systematic review of imaging studies. Alcohol Alcohol. 2013;48(4):433–444. [DOI] [PubMed] [Google Scholar]
- 3. Reyes HLM, Foshee VA, Bauer DJ, Ennett ST. Proximal and time-varying effects of cigarette, alcohol, marijuana and other hard drug use on adolescent dating aggression. J Adolesc. 2014;37:281–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Charak R, Koot HM, Dvorak RD, Elklit A, Elhai JD. Unique versus cumulative effects of physical and sexual assault on patterns of adolescent substance use. Psychiatry Res. 2015;230(3):763–769. [DOI] [PubMed] [Google Scholar]
- 5. Stueve A, O’Donnell LN. Early alcohol initiation and subsequent sexual and alcohol risk behaviors among urban youths. Am J Public Health. 2005;95(5):887–893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lester L, Baker R, Coupland C, Orton E. Alcohol misuse and injury outcomes in young people aged 10-24. J Adolesc Health. 2018;62(4):450–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kann L, McManus T, Harris WA, et al. Youth risk behavior surveillance-United States, 2017. MMWR CDC Surveill Summ. 2018;67(8):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Marshall EJ. Adolescent alcohol use: risks and consequences. Alcohol Alcohol. 2014;49(2):160–164. [DOI] [PubMed] [Google Scholar]
- 9. Bouchery EE, Harwood HJ, Sacks JJ, Simon CJ, Brewer RD. Economic costs of excessive alcohol consumption in the US, 2006. Am J Prev Med. 2011;41:516–524. doi: 10.1016/j.amepre.2011.06.045 [DOI] [PubMed] [Google Scholar]
- 10. Johnson BA, Cloninger CR, Roache JD, Bordnick PS, Ruiz P. Age of onset as a discriminator between alcoholic subtypes in a treatment-seeking outpatient population. Am J Addict. 2000;9:17–27. [DOI] [PubMed] [Google Scholar]
- 11. Grant BF, Stinson FS, Harford TC. Age at onset of alcohol use and DSM-IV alcohol abuse and dependence: a 12-year follow-up. J Subst Abuse. 2001;13:493–504. [DOI] [PubMed] [Google Scholar]
- 12. Hingson RW, Heeren T, Winter MR. Age at drinking onset and alcohol dependence: age at onset, duration, and severity. Arch Pediatr Adolesc Med. 2006;160:739–746. [DOI] [PubMed] [Google Scholar]
- 13. Babor TF, Del Boca F, Bray JW. Screening, brief intervention and referral to treatment: Implications of SAMHSA’s SBIRT initiative for substance abuse policy and practice. Addiction. 2017;112(S2):110–117. [DOI] [PubMed] [Google Scholar]
- 14. Substance Abuse and Mental Health Services Administration. Results from the 2010 National Survey on Drug Use and Health: Mental Health Findings [Internet]. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2010. Available at: https://www.samhsa.gov/data/report/results-2010-national-survey-drug-use-and-health-mental-health-findings. Accessed September 5, 2018. [Google Scholar]
- 15. Becker SJ, Ozechowski T, Hogue A. Expanding the reach of brief interventions for adolescents: SBIRT-A. In: Monti PM, Colby SM, O’Leary TA. (eds) Adolescents, Alcohol, and Substance Abuse: Reaching Teens through Brief Interventions. New York, NY: Guilford Press; 2018:131–150. [Google Scholar]
- 16. Tanner-Smith EE, Lipsey MW. Brief alcohol interventions for adolescents and young adults: a systematic review and meta-analysis. J Subst Abuse Treat. 2015;51:1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mitchell SG, Gryczynski J, O’Grady KE, Schwartz RP. SBIRT for adolescent drug and alcohol use: current status and future directions. J Subst Abuse Treat. 2013;44:463–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sullivan LE. The SAGE Glossary of the Social and Behavioral Sciences. London: Sage Publications; 2009. [Google Scholar]
- 19. Jones BT, Corbin W, Fromme K. A review of expectancy theory and alcohol consumption. Addiction. 2001;96:57–72. [DOI] [PubMed] [Google Scholar]
- 20. Jester JM, Wong MM, Cranford JA, Buu A, Fitzgerald HE, Zucker RA. Alcohol expectancies in childhood: change with the onset of drinking and ability to predict adolescent drunkenness and binge drinking. Addiction. 2015;110:71–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Vilenne A, Quertemont E. Explicit and implicit positive alcohol expectancies in problem and non-problem drinkers: differences across age groups from young adolescence to adulthood. Front Psychol. 2015;6:1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. El-Guebaly N. Investigating the association between moderate drinking and mental health. Ann Epidemiol. 2007;17:S55–S62. [Google Scholar]
- 23. Reese FL, Chassin L, Molina BS. Alcohol expectancies in early adolescents: predicting drinking behavior from alcohol expectancies and parental alcoholism. J Stud Alcohol Drugs. 1994;55:276–284. [DOI] [PubMed] [Google Scholar]
- 24. Fromme K, D’Amico EJ. Measuring adolescent alcohol outcome expectancies. Psychol Addict Behav. 2000;14(2):206–212. [DOI] [PubMed] [Google Scholar]
- 25. Zamboanga BL, Zhang M, Olthuis JV, Kim SY. Understanding drinking game behaviors: a consideration of alcohol expectancies and motives to play and drink. Cognit Ther Res. 2018;42(3):302–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zamboanga BL, Schwartz SJ, Ham LS, Jarvis LH, Olthuis JV. Do alcohol expectancy outcomes and valuations mediate peer influences and lifetime alcohol use among early adolescents? J Genet Psychol. 2009;170(4):359–376. [DOI] [PubMed] [Google Scholar]
- 27. Sitnick SL, Shaw DS, Hyde LW. Precursors of adolescent substance use from early childhood and early adolescence: Testing a developmental cascade model. Dev Psychopathol. 2014;26:125–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Alati R, Baker P, Betts KS, et al. The role of parental alcohol use, parental discipline and antisocial behaviour on adolescent drinking trajectories. Drug Alcohol Depend. 2014;134:178–184. [DOI] [PubMed] [Google Scholar]
- 29. Kuperman S, Schlosser SS, Kramer JR, et al. Developmental sequence from disruptive behavior diagnosis to adolescent alcohol dependence. Am J Psychiatry. 2001;158:2022–2026. [DOI] [PubMed] [Google Scholar]
- 30. Farmer RF, Gau JM, Seeley JR, Kosty DB, Sher KJ, Lewinsohn PM. Internalizing and externalizing disorders as predictors of alcohol use disorder onset during three developmental periods. Drug Alcohol Depend. 2016;164:38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Englund MM, Egeland B, Oliva EM, Collins WA. Childhood and adolescent predictors of heavy drinking and alcohol use disorders in early adulthood: a longitudinal developmental analysis. Addiction. 2008;103(s1):3–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Stormshak EA, Connell AM, Veronneau MH, et al. An ecological approach to promoting early adolescent mental health and social adaptation: family centered intervention in public middle schools. Child Dev. 2011; 82: 209–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hale DR, Fitzgerald-Yau N, Viner RM. A systematic review of effective interventions for reducing multiple health risk behaviors in adolescence. Am J Public Health. 2014;104:e19–e41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Alegria M, Carson NJ, Goncalves M, Keefe K. Disparities in treatment for substance use disorders and co-occurring disorders for ethnic/racial minority youth. J Am Acad Child Adolesc Psychiatry. 2011;50:22–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kakade M, Duarte CS, Liu X, et al. Adolescent substance use and other illegal behaviors and racial disparities in criminal justice system involvement: findings from a US National Survey. Am J Public Health. 2012;102:1307–1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sher KJ. Children of Alcoholics: a Critical Appraisal of Theory and Research. Chicago, IL: University of Chicago Press; 1991. [Google Scholar]
- 37. Ham LS, Stewart SH, Norton PJ, Hope DA. Psychometric assessment of the Comprehensive Effects of Alcohol Questionnaire: comparing a brief version to the original full scale. J Psychopathol Behav Assess. 2005;27:141–158. [Google Scholar]
- 38. McCarthy DM, Pedersen SL, D’Amico EJ. Analysis of item response and differential item functioning of alcohol expectancies in middle school youths. Psychol Assess. 2009;21(3):444–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Oshri A, Schwartz SJ, Unger JB, et al. Bicultural stress, identity formation, and alcohol expectancies and misuse in Hispanic adolescents: a developmental approach. J Youth Adolesc. 2014;43(12):2054–2068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Achenbach TM, Dumenci L, Rescorla LA. Ten-year comparisons of problems and competencies for national samples of youth: self, parent and teacher reports. J Emot Behav Disord. 2002;10:194–203. [Google Scholar]
- 41. Ferguson CJ, San Miguel C, Hartley RD. A multivariate analysis of youth violence and aggression: the influence of family, peers, depression, and media violence. J Pediatr. 2009;155(6):904–908. [DOI] [PubMed] [Google Scholar]
- 42. Forster M, Grigsby T, Soto DW, Schwartz SJ, Unger JB. The role of bicultural stress and perceived context of reception in the expression of aggression and rule breaking behaviors among recent-immigrant Hispanic youth. J Interper Violence. 2015;30(11):1807–1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Earleywine M, LaBrie JW, Pedersen ER. A Brief Rutgers Alcohol Problem Index with less potential for bias. Addict Behav. 2008;33:1249–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Meca A, Tubman JG, Regan T, et al. Preliminary evaluation of the NIAAA/AAP Brief Alcohol Use Screener. Alcohol Alcohol. 2017;52(3):328–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. R Core Team. R: A Language and Environment for Statistical Computing (Version 3.3.0) [Computer software]. 2016; Available at: http://cran.r-project.org.
- 46. IBM. SPSS statistics for Windows. Armonk, NY: IBM; 2013. [Google Scholar]
- 47. Honaker J, King G, Blackwell M. Amelia II: a program for missing data. J Stat Softw. 2011;45(7):1–47. [Google Scholar]
- 48. Venables WN, Ripley BD. Modern Applied Statistics with S. 4th ed. New York: Springer; 2018. [Google Scholar]
- 49. Yang S, Berdine G. The negative binomial regression. Southwest Respir Crit Care Chron. 2015;3(10):50–54. [Google Scholar]
- 50. Atkins DC, Baldwin SA, Zheng C, Gallop RJ, Neighbors C. A tutorial on count regression and zero-altered count models for longitudinal substance use data. Psychol Addict Behav. 2013;27(1):166–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Gardner W, Mulvey EP, Shaw EC. Regression analyses of counts and rates: Poisson, overdispersed Poisson, and negative binomial models. Psychol Bull. 1995;118(3):392–404. [DOI] [PubMed] [Google Scholar]
- 52. Chung T, Creswell KG, Bachrach R, Clark DB, Martin CS. Adolescent binge drinking. Alcohol Res. 2018;39(1):5–15. [PMC free article] [PubMed] [Google Scholar]
- 53. Chen P, Jacobson KC. Developmental trajectories of substance use from early adolescence to young adulthood: gender and racial/ethnic differences. J Adolesc Health. 2012;50(2);154–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Nicolai J, Moshagen M, Demmel R. A test of expectancy-value theory in predicting alcohol consumption. Addict Res Theory. 2018;26(2):133–142. [Google Scholar]
- 55. Martin-Storey A, Benner A. Externalizing behaviors exacerbate the link between discrimination and adolescent health risk behaviors. J Youth Adolesc. 2019;48(9):1724–1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Sher KJ, Walitzer KS, Wood PK, Brent EE. Characteristics of children of alcoholics: putative risk factors, substance use and abuse, and psychopathology. J Abnorm Psychol. 1991;100:427–448. [DOI] [PubMed] [Google Scholar]
- 57. Chartier KG, Hesselbrock MN, Hesselbrock VM. Development and vulnerability factors in adolescent alcohol use. Child Adolesc Psychiatr Clin N Am. 2010;19:493–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Curtis BL, McLellan AT, Gabellini BN. Translating SBIRT to public school settings: an initial test of feasibility. J Subst Abuse Treat. 2014;46:15–21. [DOI] [PubMed] [Google Scholar]
- 59. Ozechowski TJ, Becker SJ, Hogue A. SBIRT-A: Adapting SBIRT to maximize developmental fit for adolescents in primary care. J Subst Abuse Treat. 2016;62:28–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Szapocznik J, Muir JA, Duff JH, Schwartz SJ, Brown CH. Brief strategic family therapy: implementing evidence-based models in community settings. Psychother Res. 2015;25:121–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Tubman JG, Meca A, Schwartz SJ, Egbert AW. The use of a brief alcohol use screener to identify adolescents at risk for school discipline due to externalizing behaviors. J Sch Health. 2018;88:474–478. [DOI] [PubMed] [Google Scholar]
- 62. Okonofua JA, Walton GM, Eberhardt JL. A vicious cycle: a social-psychological account of extreme racial disparities in school discipline. Perspect Psychol Sci. 2016;11(3):381–398. [DOI] [PubMed] [Google Scholar]
- 63. Baldwin SA, Christian S, Berkeljon A, Shadish WR. The effects of family therapies for adolescent delinquency and substance abuse: a meta-analysis. J Marital Fam Ther. 2012;38:281–304. [DOI] [PubMed] [Google Scholar]
- 64. Velleman RD, Templeton LJ, Copello AG. The role of the family in preventing and intervening with substance use and misuse: a comprehensive review of family interventions, with a focus on young people. Drug Alcohol Rev. 2005;24(2): 93–109. [DOI] [PubMed] [Google Scholar]
- 65. Steinka-Fry KT, Tanner-Smith EE, Dakof GA, Henderson C. Culturally sensitive substance use treatment for racial/ethnic minority youth: a meta-analytic review. J Subst Abuse Treat. 2017;75: 22–37. [DOI] [PubMed] [Google Scholar]
- 66. Hustad JTP, Barnett NP, Borsari B, Jackson KM. Web-based alcohol prevention for incoming college students: a randomized controlled trial. Addict Behav. 2010;35:183–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Tebb KP, Erenrich RK, Jasik CB, Berna MS, Lester JC, Ozer EM. Use of theory in computer-based interventions to reduce alcohol use among adolescents and young adults: a systematic review. BMC Public Health. 2016;16:517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Zapolski TC, Clifton RL. Cultural socialization and alcohol use: the mediating role of alcohol expectancies among racial/ethnic minority youth. Addict Behav Rep. 2019;9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280(5365):867–873. [DOI] [PubMed] [Google Scholar]