Mosquitoes act as vectors of a remarkable number of viruses and some parasites, which they transmit in their saliva while they feed on blood. Among these mosquito-borne agents are pathogens that cause some of the most medically devastating infectious diseases—malaria, lymphatic filariasis, dengue, yellow fever, Zika virus disease, chikungunya, Japanese encephalitis, and West Nile fever. Although some of these diseases have been around for centuries, in the past few decades epidemics caused by viruses such as West Nile, chikungunya, and Zika took many regions by surprise, overwhelming health systems.
COVID-19 has reminded the world how quickly a virus can cause havoc. The susceptibility of humans is compounded by a lack of available treatments. Increased handwashing, controlled coughing and sneezing, and physical distancing when appropriate will reduce the future incidence of directly transmitted viruses like coronaviruses, influenza viruses, and noroviruses. By contrast, vector-borne pathogens are unaffected by improved personal hygiene practices because their indirect transmission relies on infected arthropods (eg, mosquitoes, sandflies, ticks) or aquatic snails. According to WHO, vector-borne pathogens account for at least 17% of all infectious diseases and each year they cause more than 700 000 deaths.
Dependency on a vector could be the weakness of vector-borne pathogens, which is the view of Jessica Manning and colleagues,1 who report in The Lancet their study of the safety and immunogenicity of a mosquito saliva peptide-based vaccine. Although blood-feeding vectors are known to induce an immune response when they feed, attempts to harness this knowledge have resulted in only two marketed vaccines, both for control of the cattle tick, but derived from midgut rather than salivary antigens.2 One reason development of an antivector vaccine has been so challenging is the evolutionary tensions between vector and vertebrate host: responses of the host (nociceptive, inflammatory, and immune) to prevent the bloodletting are countered by bioactive molecules (mostly proteins and peptides) synthesised in vector salivary glands and secreted into the host as the vector attaches and feeds.3, 4
For Manning and colleagues' clinical trial, a vaccine was prepared comprising four peptides of 32–44 amino acids in length. The peptide sequences are predicted T-cell epitopes of proteins from Anopheles gambiae salivary glands, conserved across Anopheles, Aedes, and Culex spp mosquitoes. 49 healthy participants (30 [61%] women; median age 30·5 years [IQR 24·5–35·0]) were recruited and randomly assigned to the vaccine with adjuvant (n=17) or without adjuvant (n=16) or placebo (n=16). Inoculation of this peptide vaccine (with or without adjuvant) had no untoward systemic effects in the 33 participants given at least one dose of vaccine, even when ten starved Aedes aegypti mosquitoes fed on them. This basic result is encouraging given the potential for severe allergic responses. The mosquito feeding challenge could be argued to be soft—ie, Anopheles-induced immunity challenged with Aedes saliva antigens. The outcome could have been different with A gambiae mosquitoes, although the vaccine was based on conserved antigens.
Although more safety testing needs to be done, the next big challenge is showing a mosquito peptide vaccine provides protection against mosquito-borne pathogens, which is unlikely, but not implausible. Extensive research on developing antisandfly vector vaccines to control leishmaniasis provides some design clues.5, 6 Leishmania parasites, inoculated into the skin when an infected sandfly bites, infect macrophages and form skin lesions (cutaneous forms) or migrate to the spleen, liver, and bone marrow (visceral forms). Preclinical studies showed that rhesus macaques immunised with a sandfly salivary protein (PdSP15) were protected against cutaneous leishmaniasis when exposed to sandflies infected with the parasite.7 Protection correlated with accelerated Leishmania-specific CD4+IFN-γ+ lymphocyte production. A similar effect was observed when mice immunised against a tick salivary protein survived an otherwise lethal challenge with ticks infected with tick-borne encephalitis virus.8 Immune responses to the vector create an environment in the skin that is hostile to pathogens that are injected during feeding, promoting a protective antipathogen response.6
The great attraction of antivector vaccines is the prospect of one vaccine protecting against all the different pathogens, known and unknown, transmitted by one vector (or even related vectors). This approach compares favourably with conventional antipathogen approaches—eg, yellow fever vaccine protects against yellow fever virus transmitted by A aegypti but not against chikungunya, dengue virus, Zika virus, or as yet unrecognised pathogenic viruses transmitted by the same mosquito species. Relying on an antivector vaccine is risky and a combined antipathogen and antivector vaccine approach is considered safer. However, as a first line of defence, an effective mosquito peptide vaccine could save lives and buy time to develop a targeted vaccine.9
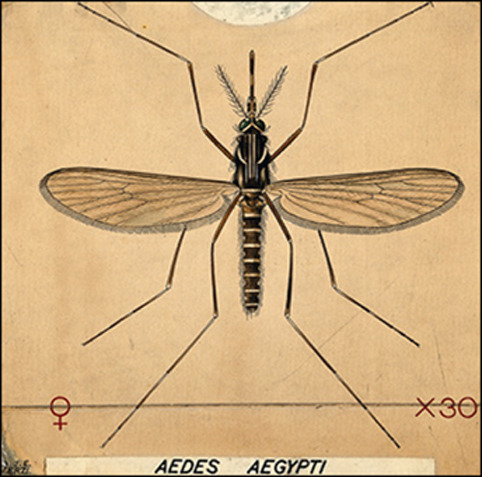
© 2020 An anopheles mosquito (Aedes aegypti)/Coloured drawing by A J E Terzi/Wellcome Collection, CC BY 4.0
Acknowledgments
I declare no competing interests.
References
- 1.Manning JE, Oliveira F, Countinho-Abreu IV. Safety and immunogenicity of a mosquito saliva peptide-based vaccine: a randomised, placebo-controlled, double-blind, phase 1 trial. Lancet. 2020 doi: 10.1016/S0140-6736(20)31048-5. published online June 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Willadsen P. Anti-tick vaccines. Parasitology. 2004;129(suppl):S367–S387. doi: 10.1017/s0031182003004657. [DOI] [PubMed] [Google Scholar]
- 3.Ribeiro JMC. Role of saliva in blood-feeding by arthropods. Annu Rev Entomol. 1987;32:463–478. doi: 10.1146/annurev.en.32.010187.002335. [DOI] [PubMed] [Google Scholar]
- 4.Vogt MB, Lahon A, Arya RP. Mosquito saliva alone has profound effects on the human immune system. PLoS Negl Trop Dis. 2018;12 doi: 10.1371/journal.pntd.0006439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peters NC, Kimblin N, Secundino N, Kamhawi S, Lawyer P, Sacks DL. Vector transmission of Leishmania abrogates vaccine-induced protective immunity. PLoS Pathog. 2009;5 doi: 10.1371/journal.ppat.1000484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reed SG, Coler RN, Mondal D, Kamhawi S, Valenzuela JG. Leishmania vaccine development: exploiting the host-vector-parasite interface. Expert Rev Vaccines. 2016;15:81–90. doi: 10.1586/14760584.2016.1105135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oliveira F, Rowton E, Aslan H. A sand fly salivary protein vaccine shows efficacy against vector-transmitted cutaneous leishmaniasis in nonhuman primates. Sci Transl Med. 2015;7 doi: 10.1126/scitranslmed.aaa3043. [DOI] [PubMed] [Google Scholar]
- 8.Labuda M, Trimnell AR, Licková M. An antivector vaccine protects against a lethal vector-borne pathogen. PLoS Pathog. 2006;2:e27. doi: 10.1371/journal.ppat.0020027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang Y, Marin-Lopez A, Jiang J, Ledizet M, Fikrig E. Vaccination with Aedes aegypti agbr1 delays lethal mosquito-borne Zika virus infection in mice. Vaccines (Basel) 2020;8:e145. doi: 10.3390/vaccines8020145. [DOI] [PMC free article] [PubMed] [Google Scholar]


