Abstract
Background
Ayurvedic clinical profiling of COVID-19 is a pre-requisite to develop standalone and integrative treatment approaches. At present, Ayurvedic clinicians do not have access to COVID-19 patients in clinical settings. In these circumstances, a preliminary clinical profiling of COVID-19 based on review of modern medical and classical Ayurvedic literature with inputs from Allopathic clinicians treating COVID-19 patients assumes significance.
Objectives
This paper aims to develop an Ayurvedic clinical profile of COVID-19 by literature review supported by analysis of clinical data of a cohort of COVID-19 patients.
Methods
The typical clinical presentation of COVID-19 was categorized based on a cluster of symptoms with reference to “Interim Clinical Guidance for Management of Patients with confirmed corona virus disease (COVID-19)” released by the US CDC. As the clinical presentation is found to vary widely, research papers reporting clinical symptoms of patient samples from different parts of the world were also reviewed to identify outliers and atypical presentations. Case records of fourteen COVID-19 patients treated at Medanta Hospital, Gurgaon were analyzed to compare symptomatology with data obtained from published literature. Further, a careful correlation was done with the data collected from selected Ayurvedic classical texts and expert views of clinical practitioners to arrive at a preliminary Ayurvedic clinical profile of COVID-19.
Results
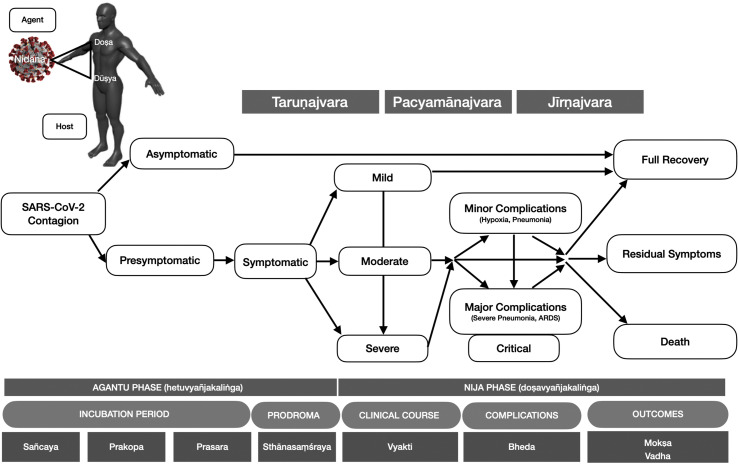
COVID-19 can be understood from the Ayurvedic perspective as vātakapha dominant sannipātajvara of āgantu origin with pittānubandha. The asymptomatic, presymptomatic, mild, moderate, severe and critical stages of COVID-19 with varying clinical presentations have been analysed on the basis of nidāna, doṣa, dūṣya, nidānapañcaka and ṣaṭkriyākāla to present a preliminary clinical profile of the disease.
Conclusion
In this paper, we have demonstrated that a preliminary clinical profiling of COVID-19 from the Ayurvedic perspective is possible through literature review supported by discussions with Allopathic clinicians as well as examination of patient case records. The provisional diagnosis proposed can be further developed with continued review of literature, wider cooperation and teamwork with Allopathic physicians and access to clinical data as well as direct clinical assessment of COVID-19 patients.
Keywords: COVID-19, Ayurveda, Integrative protocol, Clinical profile, Pathogenesis
1. Introduction
The COVID-19 pandemic has tightened its grip on India. India does not figure in the most severely affected countries [1] but fares worse than the top affected nations in key medical infrastructure and health care investments. India has fewer hospital beds and doctors per 1000 people than any of the countries affected by COVID-19 [2]. In terms of personal hygiene, a section of the population may not even have adequate facilities for washing hands with soap frequently or hand sanitizers, a basic preventive measure [3]. Moreover, those who progress into critical stages would require intensive care and this can pose a major challenge for the limited hospital resources and capacities in case of a sudden spike in infections.
Considering the fact that COVID-19 requires a structured approach covering preventive care, management in early stages of confirmed disease as well as hospital care for moderately and critically ill patients, it is imperative that the capacity of the AYUSH sector is harnessed to ensure optimal use of the scarce health care resources available in the country. The World Health Organization has also recommended inclusion of traditional medicine in its COVID-19 strategic preparedness and response plan [4]. The focus should not be to just deploy this workforce as a standby option, but to utilize its therapeutic management potential in complementing the treatment administered by modern medicine. Pluralism is one of the core principles in Indian health system as outlined in the National Health Policy 2017, which calls for integrative health practices to achieve national health goals and objectives [5].
To move in this direction, it becomes necessary to develop an Ayurvedic diagnostic and treatment protocol for integration into the standard treatment guidelines of COVID-19. We have a precedent in China, where Traditional Chinese Medicine (TCM) doctors were actively involved in the treatment of COVID-19 patients and the TCM diagnostic classification as well as treatment was integrated into the official management guideline. More than 60,000 patients received TCM medications based on this protocol [6] and TCM interventions have also been included in the official handbooks that recommend protocols for management of COVID-19 [7]. TCM interventions have also figured in research studies that have been initiated to discover a remedy for the disease [8].
In this paper, we are demonstrating that it is possible for Allopathic and Ayurvedic doctors to cooperate and work together to understand the disease better from an Ayurvedic perspective. This will be the first step to develop an integrative treatment protocol incorporating Ayurveda for best outcomes in the management of COVID-19.
An Ayurvedic assessment of the disease can help to classify the clinical presentations of COVID-19 on the basis of the tridoṣa framework (the three doṣas called vāta, pitta and kapha represent the self-regulatory mechanisms of the body, the failure of which leads to development of disease). It is seen that the clinical presentations of the patients are different with the lower respiratory, gastrointestinal or upper respiratory systems being variably affected in patients [9]. The question that we are addressing in this paper is whether such clustering of symptoms can be interpreted based on an Ayurvedic understanding of the pathogenesis with reference to imbalance of tridoṣas. This would lead to development of appropriately specific Ayurvedic interventions that can be integrated into the evolving COVID management protocol.
2. Methodology
In the prevailing circumstances, Ayurvedic physicians are unable to directly examine COVID-19 patients clinically. For this reason, a triangulation approach has been used for the study. The steps were 1) Study the existing clinical data from review of current scientific literature, 2) Review prospective clinical data collected from hospital documentation and regular discussion with the clinicians treating COVID19 patients and 3) Review relevant Ayurveda literature with the inputs of expert clinicians. The three-pronged strategy in the respective sequence covered the following aspects:
A detailed literature review of the reported typical clinical presentation based on existing data sources such as journal articles and interim clinical guidance on management of patients by agencies such as US CDC (as on April 30, 2020) was undertaken [9]. The global overview reports were screened for key terms relating to COVID19 symptoms, pathogenesis and stagewise understanding. As the clinical presentation is found to vary widely, research papers reporting clinical symptoms of patient cohorts from different parts of the world were also reviewed to identify outliers and atypical presentations.
A quick scoping of PubMed found around 569 articles on COVID19 based on a search with the key words COVID 19, symptoms. It was found that papers reported symptoms related to COVID-19 from specific clusters and cohorts of patients and the information could not be generalized to the larger population. Interim guidelines issued by international agencies like US CDC and WHO [10], which were drafted by reviewing published research papers were selected to study the clinical presentation of COVID-19. Eighteen most relevant papers reviewed by US CDC and WHO were shortlisted for a detailed review based on the following inclusion criteria – 1) Paper reports from large samples of patients from representative regions of the outbreak of COVID-19, 2) Papers reporting typical presentations of the disease, 3) Papers reporting atypical presentations of the disease.
Clinical case documentations of fourteen COVID-19 patients treated at Medanta Hospital, Gurgaon was examined prospectively. Necessary ethical approval for patient data review was obtained and a confidentiality agreement was signed with the hospital. Baseline data was compiled with a structured questionnaire covering clinical symptomatology and laboratory reports of each patient at the time of admission. This data also included assessment of co-morbidities and other prescriptions at the time of admission. A second set of data was collated, summarizing assessments done during hospital stay. Regular discussions and interactions with the treating allopathic clinicians during the course of management provided individual case narratives and focused clinical perspectives about each patient.
Subsequently, an independent analysis of Ayurvedic literature was carried out. This included three major classical texts (Bṛhattrayī – Carakasamhitā, Suśrutasaṃhitā, Aṣṭāṅgahṛdayaṃ and their important commentaries (by Cakrapāṇi, Aruṇadatta, Hemādri, Indu and Dalhaṇa). In addition, specific diagnostic literature viz. the Jvaranirṇaya (an exclusive text on management of fevers), Yogaratnākara (a medieval textbook on Ayurveda), Bhāvaprakasa and Mādhavanidāna (a classical text on diagnosis, etiopathogenesis and differential stage wise classifications) were also studied. Five clinical conditions described in these texts were examined to develop correlation with COVID-19. These were fever (jvara), cough (kāsa), dyspnoea (śvāsa), consumption (rājayakṣmā) and poisoning (viṣa) including Ayurvedic descriptions of the co-morbidities that indicate poor prognostic outlook for COVID-19. Since COVID-19 is a new disease and not previously described in Ayurvedic classical texts, a detailed study of the etiology (nidāna), status of tridoṣa, structural elements (dūṣya) and site of disease (sthāna) was done. The book Siddhāntanidāna by Gaṇanatha Sen was reviewed to understand approaches to study new diseases based on principles of Ayurveda. The analysis of sections on epidemics (janapadodhvaṃsa) and diseases of exogenous origin (āgantukavikāra) was also undertaken. Host-pathogen specific interactions as observed in COVID-19 were analysed on the basis of the Ayurvedic understanding of the clinical progression of āgantuka diseases. The pathogenesis of the disease was traced from the point of contact with the causative agent (SARS-CoV-2) and its development through the asymptomatic, presymptomatic, mild, moderate, severe and critical stages culminating in recovery or death. This was also corroborated with insights from experienced Ayurveda physicians in the team.
3. Results
3.1. Disease profile as per current scientific literature
The incubation period of the SARS-CoV-2 virus is approximately two weeks. Symptoms can manifest within 4–5 days after infection and majority will become sick by 11–12 days. In rare cases it can be delayed even up to 24 days [11].
According to the US CDC, symptoms present at onset of COVID-19 are highly variable. However, in the stage of full-blown disease, 83–99 percent of patients develop fever, 59–82 percent have cough, 44–77 percent have fatigue, 40–84 percent have anorexia, 31–40 patients have shortness of breath, 28–33 percent have sputum production and 11–35 percent have myalgias [9].
Fever, Cough (dry) and Shortness of breath are considered to be the cardinal symptoms of COVID-19. Recently, CDC has added other symptoms to the list like Chills, Repeated shaking with chills, Muscle pain, Headache, Sore throat and New loss of taste or smell [12].
Atypical presentations are mainly seen in older adults and persons with co-morbidities [13]. Fever was absent in up to 44 percent of patients at the onset of the disease, but 89 percent developed fever during hospital stay [14].
Some patients present with gastrointestinal symptoms like diarrhea and nausea and no respiratory symptoms [15]. Vomiting and diarrhea are seen only in less than 10% of the cases. Likewise, upper respiratory symptoms like sore throat, rhinorrhea and headache are sporadically reported. Hemoptysis may also be seen in a similar percentage of cases [14,[16], [17], [18]]. Skin eruptions have been rarely reported [19]. It has been observed in certain cohorts that some patients experienced diarrhoea as first symptom and presented for care later than those with respiratory symptoms [20]. Although age is a higher risk for a bad prognosis, even people in the younger age group without co-morbidities have higher risk of death than that of seasonal influenza [21]. Patients with comorbidities like diabetes, hypertension, cardiovascular disease, cancer are at a high risk for complications and death due to COVID-19 [22].
Interestingly, patients tested positive for COVID-19 have also been reported to be asymptomatic as noticed with patients aboard the ship Diamond Princess [23]. Though subsequent studies have been conducted, the percentage of this occurrence is not accurately known. One study estimated that more than one fourth tested positive for COVID-19 could be asymptomatic [24]. Another study said up to four fifths of those tested positive could be asymptomatic [25]. It has been reported that asymptomatic patients can have typical ground-glass opacities or patchy shadowing in the CT Scans [26,27]. See Table 1 for typical and atypical symptoms of COVID-19.
Table 1.
Presentation of clinical symptoms in COVID-19.
| TYPICAL SYMPTOMS | |||
|---|---|---|---|
| EARLY | LATE | COMPLICATIONS | |
| MAJOR | Fever (83–99%), Cough (59–82%) | Breathing Difficulty (31–40%), Mild Pneumonia | Hypoxia, Pneumonia, ARDS, Coagulopathy |
| COMMON | Chills, Repeated shaking with chills, Myalgia, Headache, Sore throat, New loss of taste or smell, Fatigue, Nausea, Diarrhoea | ||
|
OCCASIONAL |
Anorexia (40–84%), Sputum (28–33%) |
||
| ATYPICAL SYMPTOMS | |||
| SPORADIC | < 10% | ||
| Confusion, Haemoptysis, Vomiting | |||
| Being Investigated | |||
| RARE | Skin eruptions, COVID Toes (red, sore, itchy swellings on toes) | ||
Major means the symptoms characterising the disease.
Common means the most commonly seen symptoms along with the major symptoms.
Occasional symptoms are those that may not be so commonly seen.
Sporadic means isolated occurrence.
Rare is self explanatory.
The US CDC classifies COVID-19 into the following categories based on severity of the presentation.
-
•
Mild to moderate (mild symptoms up to mild pneumonia): 81%
-
•
Severe (dyspnea, hypoxia, or >50% lung involvement on imaging): 14%
-
•
Critical (respiratory failure, shock, or multiorgan system dysfunction): 5%
In the critical stage of COVID-19, patients present with severe hypoxemia, pneumonia and ARDS. If the disease becomes severe, then shortness of breath indicating pneumonia can develop with or without high grade fever. It can progress to severe pneumonia and ARDS of varying severity, which can be life threatening. In the event of an over-exuberant immune response, complications can arise as a result of damage to the lungs. Pneumonia may be mild or severe, ARDS may be mild, moderate or severe requiring oxygenation or ventilator support. Especially in some young people, the immune system can go into an overdrive and manifest the cytokine storm syndrome, which can cause severe lung damage and death. The SARS-CoV-2 induced infection can also be associated with a coagulopathy. CAC (COVID-19 associated coagulopathy) is the acronym used to describe the coagulation changes in COVID-19 patients [28].
In an observational study from Wuhan, China, cardiac injury was seen in 19.7% of patients with confirmed coronavirus disease 2019 (COVID-19) and was an independent predictor of in-hospital mortality [29]. Acute Hemorrhagic Necrotizing Encephalopathy (AHNE), a rare complication of influenza and other viral infections has also been reported in COVID-19 [30]. Liver injury has also been reported in some patients [31]. Sepsis or Septic shock can also set in leading to life threatening situation [10].
Literature review of published studies reveal that COVID-19 patients can have varied clinical presentation with absence of symptoms or atypical presentations in a number of patients.
3.2. Clinical data from a cohort of COVID-19 patients
3.2.1. Patient background
We examined case records of fourteen COVID-19 patients treated at Medanta Hospital, Gurgaon. All were Italian citizens who came to India as tourists and were tested for COVID-19 when some of them developed symptoms and were admitted to Medanta Hospital.
3.2.2. Patient age group
Except for one patient aged 45, all other patients were in the age group ranging from 60 to 80 years.
3.2.3. Co-morbidities
Seven of the patients had comorbidities out of which ten had diseases that have been identified as high risk for patients with a diagnosis of COVID-19. There were six patients with hypertension, three with cardiac diseases, one with diabetes and one with benign prostate hypertrophy.
3.2.4. Condition at admission
Five patients were asymptomatic at the time of admission and the other nine patients had only mild symptoms.
3.2.5. Symptom profile
In the course of hospital stay, all fourteen patients developed cough, which was the most prominent symptom seen in this cohort. The next common symptom reported was throat pain, which was seen in twelve patients. The third common symptom was fever, which was mostly intermittent and was seen in eleven of the patients. Headache and myalgia were seen in nine and eight patients respectively. Only four patients developed dyspnea, of which two had mixed (inspiratory and expiratory type). Other symptoms reported in decreasing order of frequency are were insomnia, giddiness, loss of appetite, fatigue, severe anxiety, nasal obstruction, nasal discharge, nausea, diarrhea, arthralgia, cold chills, general edema, delerium and confusion. In all, twenty symptoms were reported in this cohort of COVID-19 patients. See Supplementary Table 1 for symptom profile of the patients.
3.2.6. Clinical course
All the patients who developed dyspnea progressed to acute respiratory distress and required oxygen support. Three of them were hypertensive, one also had cardiovascular disease and one had BPH. Patient 6, who was hypertensive and had cardiac disease, became very critical requiring ventilatory support as well as prolonged stay in hospital and eventually died on the 37th day. This patient (P6) tested negative on the 18th day but again tested positive on 24th day before turning severely critical. P6 had exhibited severe anxiety and irritability during the hospital stay and also reported the maximum number of thirteen symptoms. Patient 7 was the fastest to recover, testing negative on the fifteenth day and was discharged on the eighteenth day. All other patients tested negative on the seventeenth day and were discharged on the twentieth day.
3.2.7. Medications
Concomitant medications for co-morbidities were continued. Symptoms like fever and aches were managed with antipyretics and analgesics. Antacids were administered for gastrointestinal symptoms. Few patients were also administered sedatives. Vitamin supplements, especially Vitamin C was also administered. Ritonavir-lopinavir combination was administered to three of the four patients who developed ARDS. Hydroxychloroquine and Azithromycin were administered to two of the patients who became severe including the one patient who died.
3.2.8. Comparison of patient data with findings from literature review
We found that the clinical presentation and course of the cohort of COVID-19 patients matched more or less with findings from literarure review of published papers. In this cohort, 35% of patients were asymptomatic at the time of admission and except for three patients who developed severe disease (21.43%) and one patient who became critical (7.14%), others developed mild to moderate symptoms during hospital stay (71.43%). P6 became critical and died (7.14%). The higher percentage of patients in the severe and critical category is an expected finding, considering the advanced age of the patients as well as presence of co-morbidities. Cough, throat pain and fever were dominant in this cohort, which have been reported as typical symptoms of COVID-19 patients. The symptoms seen were mainly related to upper and lower respiratory tract. Some patients also reported symptoms related to gastrointestinal tract. Apart from other generalized symptoms like fever and myalgia, psychological symptoms were also seen in some patients. A critical analysis of the data from this cohort of patients from an Ayurvedic perspective is included in the section on discussion. See Supplementary Table 2 for summary of clinical data from this cohort of patients.
As Ayurveda physicians do not have direct access to COVID-19 patients, it was not possible to conduct Ayurvedic clinical examination procedures like trividhaparīkṣā, aṣṭasthānaparīkṣā or daśavidhaparīkṣā. Clinical symptoms were not directly documented by Ayurvedic physicians or those with in-depth understanding of Ayurveda. Considering these limitations, it is possible that symptomatology that is of relevance for Ayurvedic assessment may not have been recorded.
3.3. Disease profile in the light of review of classical ayurvedic literature
We found that Suśrutasaṃhitā has described epidemic fevers presenting with cluster of symptoms like cough, breathing difficulty, vomiting and headache, which resembles fevers causing severe acute respiratory syndrome (SARS) [Su.S. Su.St, 6.19-20] [32]. Dalhaṇa, the commentator additionally refers to symptoms like anosmia (gandhājñāna), which are of interest in understanding COVID-19. He also points to the nasal passages as the point of contact with the causative agent of the disease [Su.S. Su.St. 6.19-20] [32]. Suśrutasaṃhitā does not refer to a specific disease as a well-defined nosological entity in this context, rather only hints at the possibility of epidemic outbreaks of severe respiratory illnesses that resembles SARS and COVID-19 like illnesses. The Carakasaṃhitā devotes an entire chapter for discussion on epidemics and points out how people with different consitutions can be affected by the same disease due to the influence of common etiological factors like air, water, place and time, but does not list or describe specific epidemic diseases [Ca.S. Vi.St. 3.3-6] [33].
Suśrutasaṃhitā also lists fevers among diseases that are contagious [Su.S. Ni.St. 5–34] [32]. Out of the eight broad categories of fevers described in Ayurveda, the āgantujvaras are caused by external agents [Ca.S. Ni.St. 1.7] [33]. Abhiṣaṅgajvara is one of the sub-categories of āgantujvara which includes a sub-type of fever called bhūtābhiṣaṅgajvara[Ca.S. Ni.St. 3.111-112, 114–115] [33]. Cakrapāṇidatta clarifies that bhūta means viṣakṛmi or a virulent organism[Ca.S. Sa..St.1.121] [33]. Further, Vijayarakṣita, the commentator of Mādhavanidāna points out that diseases caused by bhūtopasarga (invasion of bhūtas like viṣakṛmi) can be contagious and spreads from person to person [Ma.Ni. 49.42–43] [34]. Microorganisms and contagion were well recognised in Ayurveda classical texts. The term kṛmi generally denotes pathogenic organisms but also includes organisms which are microscopic and not visible to the naked eye (kecid saukṣmyād adarśanāḥ) [Ca.S. Vi.St. 7.11] [33]. Such kṛmis are sahaja (natural) or vaikārika (pathogenic) [Ca.S. Vi.St. 7.11] [33]. Cakrapāṇidatta points out that the natural microorganisms in the body are not counted here and this is perhaps a very early allusion to the human microbiome. He, also refers to variation in nomenclature of kṛmis prevalent in other geographical regions [Ca.S. Vi.St. 7.9] [33]. There is an opinion in classical texts that viṣamajvara, a variation of sannipātajvara can be caused by bhūtābhiṣaṅga (invasion by bhutas) [Su.S. Ut.Ta. 39.68] [32]. Many herbs and medicines in Ayurveda which have kṛmighna properties exhibit antibacterial and antiviral activity [35]. Rakṣoghnakarma or fumigation with herbs, which is recommended to prevent wounds from suppurating and also for purifying air have been found to exhibit antimicrobial activity also against viruses [32]. Such herbs described in classical Ayurvedic texts are candidates for research and discovery of antiviral agents against specific viruses. In the commentary of Dalhana, there is a quotation from Bhoja that alludes to the migration of kṛmis from body of one person to the other while explaining how the movement of the mind from one body to another body after death is invisible [Su.S. Sa.St. 1.16] [32]. This is a rare reference in classical texts hinting at the invisible migration of pathogens from one person to the other. Avoiding modes of transmission of diseases described in Ayurveda like physical contact (gātrasaṃsparśa), inhalation (nihśvasa), sitting and sleeping together (sahaśayyāsanāt) [Su.S. Ni.St. 5.33-34] [32] and even keeping away from places where there is chance of exposure (sthānaparityāga) have been advised as measures to mitigate the epidemic advised in Suśrutasaṃhitā [Su.S. Sui.St. 6.20] [32]. In the Aṣṭāṅgahṛdayaṃ, avoiding contact with extraneous disease-causing factors like bhūtas-virulent organisms (bhūtādyasparśanopāyah) is advised as a preventive measure [As.Hr.Su.St. 4.33] [36]. Carakasamhitā specifically advises self-protection (ātmagupti) and relocating to places that have not been affected (śivānāṃ janapadānāṃ sevanaṃ) [Ca.S. Vi.St. 3.15-16] [33].
In fevers caused by abhiṣaṅga in general and even in bhūtābhiṣaṅga specifically, there is a tendency for derangement of all three doṣas leading to what is technically known as sannipātakopa [Ca.S. Vi.St. 3.115-116] [33] [As·Hr. Ni.St. 2.43] [36]. Even in āgantujvaras caused by extrinsic agents, doṣa imbalance occurs eventually [As.Hr.Ci.St.1.171] [36].
With this background, it was most appropriate to review the portions of classical Ayurvedic texts dealing with jvara and specifically the bhūtābhiṣaṅgaja type of āgantujvara and sannipātajvara.
Carakasamhitā describes general features of sannipātajvara and further describes thirteen types based on variations in dosa dominance [Ca.S. Ci.St. 3.103-109] [33]. On the other hand, Suśrutasaṃhitā and the works of Vagbhata describe only general features of sannipatajvara [Su.Sa. Ut.Ta. 39.35–38] [32] [As·Hr. Ni.St. 2.27-33] [36]. Dalhaṇa points out that even though sannipātajvaras are classified into thirteen types, by finer subclassification and gradation of doṣa dominance as well as involvement of dhātus, sannipāta can present in infinite ways [Su.Sa. Ut.Ta. 39.43-44] [32]. Indeed, later texts like Yogaratnākara and Bhāvaprakaśa have identified and named many more sannipātajvaras [Yo.Ra.Jvaracikitsa. 2–12] [37] like kaṇṭhakubjajvara which presents with acute respiratory distress [Bh.Pr. Ma.Kh. 1-439-526] [38]. A textbook called Jvaranirṇaya was composed by Narāyanapaṇḍita which gives the most detailed and classified descriptions of jvara in the entire Ayurvedic literature. The chapter on tridosajajvara provides a comprehensive categorization and sub-classification of sannipātajvara [Jvaranirnaya, Tridosaja, 1–241] [39]. This text helps very much in understanding how to clinically assess and classify sannipātajvara on the basis of multiple parameters compiled from other texts like nature of combination of doṣas (samavāyibheda), the variability of dominance of doṣas in a particular type of sannipātajvara, the pattern of fever (continuous, intermittent and so on), seasonality or otherwise, progression in the dhātus, clinical course as well as duration. Most interestingly, newer presentations of sannipātajvara documented in various texts in the evolutionary history of Ayurveda have all been compiled together appened by the author's own additions in between. Some sannipatajvaras are described only in terms of the variation in doṣa imbalance while specific names are given for other sannipatajvaras like vaidārika, visphuraka, papphaṇa and so on. The Jvaranirṇaya clearly points to the need for studying and classifying new presentations of sannipātajvara, which is an approach that assumes relevance in the study of COVID-19
In recent times, Gananatha Sen in his work Siddhāntanidāna discusses about changes in clinical presentations of diseases due to the influence of place and time as well as influence of varied etiological factors [Sid.Ni. ] [40]. He points out that textual descriptions of diseases may not match with clinical presentations seen today. In fact, classical Ayurvedic texts provide guideline for analysis of diseases not listed in the literature. Aṣtāṅgahṛdaya points out that analytical understanding of a disease in terms of its finer constituents like samprāpti, site of manifestation and specific nidānas is more important than identifying it by its name [As.Hr.Su.St.12.64-66] [36]. A new disease (anuktavyādhi) can be understood by study of nidāna, doṣa, sthāna [33] and other factors involved in the disease causation, progress and clinical outcomes as evidenced in texts like Mādhavanidāna [Ma.Ni.25 and 51] [34]
4. Discussion
COVID-19 being a new disease, we did not expect to find an exactly matching description in the classical Ayurvedic texts. The review of the classical Ayurvedic literature suggests that a careful analysis of the descriptions of sannipātajvara and correlation with the modern clinical profile of COVID-19 will be helpful in understanding whether this disease can be classified within the generic categorisations of jvara in Ayurveda. On the other hand, it will also help us to find out if COVID-19 needs to be classified as an independent disease entity altogether.
4.1. COVID-19 as a type of jvara
Fever, the most frequently reported symptom of COVID-19 is seen in 89–99% of patients. On this basis, we can consider COVID-19 as a type of Jvara. In the cohort of COVID-19 patients that we analysed, fever was not seen in three patients. However, the course of the disease was very mild in these patients and we infer that they remained in the pūrvarūpa (prodromal) stage without progressing to full fledged disease. Further studies focused on careful analysis of clinical symptoms with respect to disease progression is needed to make clear distinctions of the clinical stages of COVID-19 from the Ayurvedic perspective.
4.2. COVID-19 as a type of sannipatajvara based on clinical symptoms
Fever in COVID-19 is mild to moderate, which is typical of fever with dominance of vāta and kapha as understood in Ayurveda (madhyamavegajvara) [Ca·S.Ci.St.3.86-87] [33]. High grade fever has been reported in exceptional cases. Other major symptoms like cough and breathing difficulty as well as pneumonia and acute respiratory distress syndrome (ARDS) point to involvement of vāta and or kapha [Ca·S.Ci.St. 17.45] [33]. Associated symptoms like chills, shaking, rhinorrhoea, headache, sputum, nausea, vomiting and anorexia are also generally indicative of vāta and kapha dominance [As.Hr.Ni.St.1.25] [36]. Such a presentation is suggestive of vātakaphajvara. However, some symptoms like confusion, sore throat, haemoptysis and diarrhoea, which are also seen in COVID-19 patients indicate the involvement of pitta as do the sporadic reports of skin eruptions and dizziness [As.Hr.Ni.St.1.18-20] [36]. Since the clinical features of COVID-19 invariably indicates imbalance of all the three dosas with fever as a main symptom, the possibility of sannipātajvara was also examined. We found many general features of sannipātajvara can be seen in COVID-19. Fever, cough, breathing difficulty, headache, sore throat [12], anorexia, confusion, hemoptysis [41], arthralgia [42], conjunctivitis [43], delirium, sleep disturbances [44], seizures [45] dizziness [46], abnormal breath sounds [47] fatigue [48] oral thrush [49] thirst, dehydration and reduced output of urine [50], affliction of heart [51,52], skin rashes [19], loss of speech, deviated eyes [53] inflammation of nasal and respiratory passages and delay of doṣapāka are symptoms of sannipātajvara [Ca·S.Ci.St.3.103-109] [33] seen in COVID-19. For a detailed matching of these symptoms with COVID-19, refer Table 2. One of the thirteen types of sannipātajvara described in Carakasamhitā shows some symptoms that are similar to COVID-19 but a one to one correlation seems to be inappropriate. The type of sannipātajvara with dominance of vāta and kapha (vātaśleṣmolbaṇe), but mild involvement of pitta (pittāvare) presents with fever, chills, cough, anorexia, thirst, burning sensation and aches [Ca·S.Ci.St.3.92] [33]. The data from the cohort of 14 patients supports these observations. Generally, the symptom profile of the cohort represented features of vātakaphajvara with cough, sore throat and fever reported as main symptoms and the twenty symptoms reported pointed towards sannipātajvara. Nausea and anorexia were also reported in some patients as well as diarrhea showing the association of pitta along with kapha in the koṣtha.
Table 2.
Symptoms of Sannipatajvara reported in COVID-19.
| Symptoms of Sannipātajvara (These are general symptoms of all types of Sannipātajvara and all symptoms may not be seen in all cases) |
Mention in Samhitā | Reported in COVID-19 |
Reference | ||
|---|---|---|---|---|---|
| Frequency | Stages | ||||
| GENERAL SYMPTOMS | |||||
| 12 | jvaraḥ (fever) a | C, S, V | Very common | All stages | WHO [58], CDC [9,12] |
| 1 | srastāṅgatā param (loosenes of body parts) | C | Not reported | ||
| 2 | gurusrastāṅgasandhitā (heaviness and looseness of body parts) | V | Not reported | ||
| 3 | suptāṅgatā (numbness of body) | S | Not reported | ||
| 4 | stambhaḥ (stiffness) | S | Not reported | ||
| 5 | kśatvaṁ nātigātrāṇāṁ (does not loose weight significantly) | C | Not reported | ||
| 13 | kṣaṇē dāhaḥ kṣaṇē śītam (alternating heat and cold feeling) | C, S, V | Sometimes | Random | Worldometer [59] |
| 6 | cirātpākaśca doṣāṇāṃ (delay in doṣapāka) | C, S, V | Sometimes | Severe/Critical | More than two weeks duration of disease |
| 7 | tr̥ṣṇā (thirst, dehydration) | C, S | Common | Random | Seen in viral infections and also COVID-19 |
| 8 | svēdamūtrapurīṣāṇāṁ cirāddarśanamalpaśaḥ (reduced sweating, output of urine and defecation) | C, S | Reduced output of urine is reported in cases with dehydration | ||
| 9 | balabhraṃśa (loss of strength) | V | Common | Random | NBC [60] |
| 10 | bhramaḥ (dizziness, giddiness) a | C, S, V | Sometimes | Random | URHCS [61] |
| 11 | tandrā (fatigue) a | C, S | Common | Random | WHO [58], CDC [9,12] |
| CUTANEOUS SYMPTOMS | |||||
| 14 | muhuḥ svedaḥ (repeated sweating) | V | Sometimes | Random | Worldometer [59] |
| 15 | atisvedaḥ (excessive sweating) | V | Sometimes | Severe/Critical | Worldometer [59] |
| 16 | asvedaḥ (absence of sweating) | V | Not reported | ||
| 17 | kōṭhānāṁ śyāvaraktānāṁ maṇḍalānāṁ ca darśanam (greyish red skin eruptions) | C, V | Rare | Random | WHO [58] |
| RESPIRATORY SYMPTOMS | |||||
| 18 | kāsaḥ (cough) a | C, V | Very common | All stages | CDC [9,12] |
| 19 | śvāsaḥ (dyspnoea) a | C, S, V | Common | All stages | CDC [9,12] |
| 20 | kaṇṭhaḥ śūkairivāvr̥taḥ (sore throat) a | C, V | Common | All stages | CDC [9,12] |
| 21 | svarasādaḥ (hoarseness of voice) | V | Sometimes | Random | CDC [9] |
| 22 | srōtasāṁ pākaḥ (inflammation of nasopharynx, oropharynx and respiratory passages) a | C, S | Sometimes | Random | CDC [9] |
| 23 | pratataṁ kaṇṭhakūjanam (abnormal breath sounds in throat region) | C, S | Sometimes | Severe/Critical | Yinghui Huang et al [46] |
| 24 | ṣṭhīvanaṁ raktapittasya kaphēnōnmiśritasya ca (hemoptysis) | C, V | Rare | Random | CDC [9] |
| GASTROINTESTINAL SYMPTOMS | |||||
| 25 | arucih (anorexia) a | C, S | Common | Random | CDC [9] |
| 26 | gurutvamudarasya (heaviness of abdomen) | C | Not reported | ||
| 27 | malasaṃsaṅgaḥ (constipation) | V | Not reported | ||
| 28 | malānāṃ alpaśo pravṛttiḥ (reduced defecation) | V | Not reported | ||
| 29 | malānāṃ ati pravṛttiḥ (diarrhoea) a | V | Common | Random | CDC [12], WHO [58] |
| MUSCULOSKELETAL SYMPTOMS | |||||
| 32 | asthirujā (pain in bones) | C, S, V | Sometimes | Random | WHO [58] |
| 33 | sandhirujā (pain in joints) a | C, S, V | Sometimes | Random | WHO [58] |
| 34 | piṇḍikāruk (pain in calf muscles) a | V | Sometimes | Random | WHO [58] |
| 35 | pārśvaruk (pain in the flanks) | V | Sometimes | Severe/Critical | WHO [58] |
| NEUROLOGICAL SYMPTOMS | |||||
| 36 | nidrānāśō (insomnia) a | C, S | Sometimes | Random | Zambrelli E et al [43] |
| 37 | divā mahānidrā (deep sleep during daytime) | V | Sometimes | Random | Zambrelli E et al [43] |
| 38 | niśi jāgaraṇaṃ (unable to sleep at night) | V | Sometimes | Random | Zambrelli E et al [43] |
| 39 | sadā nidrā (constant sleep) | V | Sometimes | Random | Zambrelli E et al [43] |
| 40 | śirōrujā (headache) a | C, S, V | Sometimes | Random | CDC [9,12] |
| 41 | śiraso loṭhanaṃ (dystonic movements, shaking, tremors of head) | C, V | Rare | Severe/Critical | Sohal S et al [62] |
| 46 | nirbhugnē darśanē (eyes are unsteady and deviated) | C, S | Rare | Severe/Critical | Sohal S et al [62] |
| 42 | mūkatvaṁ (loss of speech) | C | Sometimes | Severe/Critical | WHO [58] |
| 43 | cētanācyutiḥ (loss of consciousness) | S | Sometimes | Severe/Critical | CDC [12] |
| SPECIAL SENSES | |||||
| 44 | sāsrāvē kaluṣē raktē ca darśanē (pink eye) | C, S | Sometimes | Random | WHO [58] |
| 45 | sasvanau karṇau (sound in ears) | C, S, V | Not reported | ||
| 49 | sarujau karṇau (pain in ears) | C, S, V | Not reported | ||
| 30 | paridagdhā kharasparśā jihvā (coarse and inflamed appearance of tongue) | C, V | Rare | Random | Xinhua [63] |
| 31 | rasanā paruṣā kṣṇā (rough and blackish appearance of tongue) | S | Not reported | ||
| 47 | śyāvadantatā (blackish discolouration of teeth) | S | Not reported | ||
| 48 | snigdhāsyatā (unctuous feeling in mouth) | V | Not reported | ||
| CARDIOVASCULAR SYMPTOMS | |||||
| 50 | hdi vyathā (affliction of heart) | C, S, V | Sometimes | Severe/Critical | Rizzo P et al [64] |
| PSYCHOLOGICAL SYMPTOMS | |||||
| 51 | mōhaḥ (confusion) a | C, S | Sometimes | Severe/Critical | CDC [9,12] |
| 52 | pralāpaḥ (delirium) a | C, S | Sometimes | Severe/Critical | Zambrelli E et al [43] |
| 53 | madaḥ (inebriation) | S | Not reported | ||
| 54 | unmādaḥ (psychosis) | S | Not reported | ||
| 55 | gītanartanahāsyādivikṛtehāpravartanaṃ (abnormal behaviour) | V | Not reported | ||
C - Carakasaṃhitā, S - Suśrutasaṃhitā, V - Vāgbhaṭa's Aṣṭāṅgahṛdayaṃ.
Reported in the cohort of 14 patients treated at Medanta.
4.3. COVID-19 as a type of sannipātajvara based on clinical course of the disease
The clinical course of COVID-19 also points to the possibility of sannipātajvara. Sannipātajvara becomes incurable or difficult to manage if the doṣa does not undergo pāka (doṣe vibaddhe) due to dysfunction of agni (agnau naṣte) and if the full range of symptoms manifest (sarvasampūrṇalakṣana). Even if patients recover, there are chances of residual disabilities (vaikalya) [As.Hr.Ni·St. 2.34] [36]. According to Suśrutasaṃhitā, sannipātajvara typically runs a mild or moderate course for one or two weeks or even more and then becomes severe and the patient either recovers from the crisis or dies [Su.S.Ut.Ta.39.45-46] [32]. This is not characteristic of fevers caused by single doṣas or dual doṣas. Sannipātajvara can present with life threatening events [Ca·S.Ci.St.3.109-110] [33]. COVID-19 can turn severe after running mild to moderate course. When it turns critical, mortality is high and even if patients recover residual disabilities have been reported. It is intriguing to note that in our cohort of 14 patients, the patient (P6) who died exhibited the maximum number of thirteen clinical symptoms. It must also be mentioned that in this patient, we observed the triad of symptoms indicating bad prognosis – autsukya (increased anxiety), moha (confusion), arati (irritability and restlessness) [As·Hr. Su.St.1.1] [36].
4.4. COVID-19 as an unlisted type of vatakaphapradhānasannipātajvara based on review of texts
The features of COVID-19 do not match exactly with descriptions of specific sannipātajvaras in classical texts, though it exhibits characteristics of sannipātajvara in general. For these reasons, we propose that COVID-19 presents clinical features pointing to an Ayurvedic diagnosis of a type of vātakaphapradhāna sannipātajvara with pittānubandha which needs to be described and documented by clinical studies. From the etiological perspective, it is of exogenous origin (āgantu).
4.5. Understanding COVID-19 based on analysis of nidana, dosa and dusya
As discussed earlier, an unlisted disease can be studied by analysis of nidāna (etiology), doṣa and dusya.
4.5.1. Nidāna (etiology)
Being an infectious disease and with the SARS-CoV-2 well identified as the causative agent, COVID-19 can be classified as an āgantu disease. Not getting in contact with an infected person or contaminated surfaces is the best known and most effective way to prevent the disease. As pointed out earlier, bhūtābhiṣaṅga by viṣakṛmi is a very plausible understanding of the nidana or etiology of COVID-19 from the Ayurvedic viewpoint. Finer discussions are warranted before viruses can be classified under a specific category of extraneous causative agents described in the classical texts, which is not being attempted in this paper.
4.5.2. Nidāna, doṣa, dūṣya interactions (agent–host interactions)
4.5.2.1. The transition of pathogenesis from extrinsic to intrinsic phase
Virus - host interactions lead to disturbances of doṣas and subsequent development of pathogenesis. Carakasamhitā clarifies in that āgantujvara (fevers of extraneous origin) does not disturb the dosas for a short period of time. In this stage, symptoms may be seen without indication of doṣa imbalance [Ca·S·Ni.St.1.30] [33]. Cakrapāṇidatta clarifies that this phase lasts for about 3–7 days after which signs of dosa imbalance manifest [Ca·S·Ni.St.1.30] [33]. Vagbhata emphasizes that the fever will progress only if the doṣa imbalance occurs within this period [As.Hr.Ci.St.1.172] [36]. It can be inferred from this discussion that individuals in whom doṣa imbalance does not get established, may present without symptoms or mild symptoms and do not progress to critical stages. As pointed out earlier, three patients in our cohort did not develop fever or progress into severe or critical stages and exhabited only other mild symptoms until tested negative. The progression of the disease interpreted on the basis of disturbances of the doṣas is critical for developing treatment strategies in Ayurveda. The clinical course of all jvaras (fevers) have been divided into specific stages in Ayurveda. The early stage of fever is called tarunajvara with a general predominance of kapha and ama[Ca·S.Ci.St.3.133-136] [33]. The late stage of fever is called jirnajvara with a dominance of vata and pitta as well as resolution of ama [Ca·S.Ci.St.3.133-136] [33]. The causative factor of jvara (fever) in general is said to be rūkṣa (dry) and uṣṇa (hot) [As.Hr.Ci.St.1.84] [36]. But, symptoms related to kapha and vāta are especially seen in early stages of COVID-19 as it manifests mainly in the respiratory system, which is the seat of these two doṣas. As the kapha dries up, severe inflammation can manifest in severe and critical stages of the disease. The underlying involvement of pitta in all fevers must be kept in mind and a flare up must be anticipated in the clinical course of COVID-19 also [As.Hr.Ci.St.1.16–17] [36].
4.5.2.2. The manifestation of dosa imbalance
When there is dry cough, the dominance of vāta should be inferred [As.Hr.Ni.St.3.22-24] [36]. If cough is associated with sputum, then a dominance of kapha should be inferred [As.Hr.Ni.St.3.26-27] [36]. The degree of involvement of these two doṣas can be understood by analysing the consistency of the sputum - whether it is thick or thin, with the former indicating a complete dominance of kapha [As.Hr.Ni.St.3.26-27] [36]. If there is high grade fever, then dominance of pitta should be inferred. These presentations can vary from person to person. A combination of these features would call for a finer analysis of the degree of involvement of the three doṣas in a sannipāta situation. Scanty sputum was reported only in few patients in the cohort that we studied, pointing to vāta dominant kāsa in a group of aged people. The presentation of the disease in asymptomatic, presymptomatic, mild, moderate, severe or critical manner depends on the outcomes of the interactions between nidāna, doṣa and dūṣya. It is clearly mentioned that when these factors are in opposition there is resistance to disease (vikāravighātabhāva) [Ca·S·Ni.St.3.4] [33]. Host factors that initiate resistance to disease (vyādhikṣamatva or vyadhyutpādapratibandhakatva) are dependent on bala (innate strength of the body)[Ca·S.Su.St.28.6] [33]. Bala is a broad term that includes agnibala (strength of digestive and metabolic processes), dhātubala (strength of body elements) and dehabala (strength of body). Ojas is the byproduct of metabolic processes taking place in all the dhātus[As.Hr.Su.St.11.37] [36]. The bala of the body is primarily dependent on ojas[As.Hr.Su.St.11.38] [36]. In the treatment of jvara, it is clearly mentioned that when agni is stabilized, balam and ojas are increased [As.Hr.Ci.St.1.3] [36]. Fever persists only in the absence of dehabala and dhātubala [As.Hr.Ci.St.1.84] [36]. It has been pointed out that bala by itself can bring back the balance of the doṣas [As.Hr.Ci.St.1.84] [36]. Strengthening the host immunity would be an important therapeutic strategy from the Ayurvedic viewpoint. It has been observed that a robust immune response across different cell types was associated with clinical recovery, similar to what we see in influenza, in COVID-19 cases also [54]. This corroborates with the general approach to jvaracikitsā in Ayurveda that emphasises the preservation and enhancement of bala for uncomplicated recovery from the disease [As.Hr.Ci.St.1.2] [36].
4.5.2.3. The sites of the agent–host interactions
From an Ayurvedic point of view, the primary site of the disease is the prāṇavaha srotas, which includes both the upper respiratory and lower respiratory tracts [Ca·S.Vi.St.5.8] [33]. In COVID-19, the lower respiratory tract is the centerstage of the pathological events that unfold in the course of the progression of the disease. The most common respiratory symptom seen is cough, which is usually dry. It is usually accompanied by mild to moderate fever. This pattern was clearly observed in the cohort of patients with all patients reporting cough and eleven patients, fever. In some patients, the gastrointestinal system is also affected. The possibility of the virus entering through the mouth and first affecting the gastrointestinal tract before affecting the respiratory system has also been discussed in published papers [55]. In such cases, patients present with symptoms related to pitta and kapha like diarrhoea, nausea or vomiting. This suggests the involvement of kostha and annavahasrotas from the Ayurvedic perspective [Ca·S.Su.St.11.42-43] [33]. Gastrointestinal symptoms were also reported in the data from the cohort of patients that we reviewed. Considering the fact that fever is the main symptom, the involvement of rasavahasrotas is to be inferred. Respiratory symptoms like cough and dyspnea indicate the involvement of pranavaha, udakavaha and annavaha srotases [As.Hr.Ni.St.4.3–4] [36]. Clotting of blood has been reported in many patients suggesting the involvement of raktavahasrotas also. In some patients, there are generalised symptoms like skin eruptions indicating involvement of śākhā [Ca·S.Su.St.11.42-43] [33]. In others, myalgia and arthralgia have been reported which indicates involvement of madhyamarogamārga[Ca·S.Su.St.11.42-43] [33]. The dhātus involved in COVID-19 can be tentatively considered as rasa and rakta. The damage to heart (hṛdaya), brain (śiras) and kidneys indicate the affliction of the vital organs (marmas) by the disease [Ca·S.Su.St.11.42-43] [33].
4.5.2.4. The crisis in advanced stages
As the disease progresses, the efficiency of ojas is compromised and a crisis can develop. Such a presentation is seen in critical COVID 19 cases, characterized by disruption of immune system [56] leading to cytokine storm and ARDS, which correlates with ojonirodha described by Suśrutasaṃhitā in the context of severe sannipātajvara[Su.S.Ut.T.39.43-45] [32]. One patient in the cohort of our study progressed to critical stage and died. It is pertinent to point out that this patient reported negative on 18th day but became positive again on 24th day indicating a weakened immune system. The commentator Vijayarakṣita points out that accumulation of metabolic byproducts due to aberrations in digestion and metabolism as well as the disturbances in doṣas is called in Ayurveda as āma [Ma.Ni.25.1–5] [34]. The development of āma goes hand in hand with the pathogenesis. In a disease with derangement of all three doṣas (doṣasaṃmūrchana), the āma can become āmaviṣa (biochemical changes leading to sepsis and septic shock)[As.Hr.Su.St.13.26] [36]. There is an opinion amongst Ayurvedic physicians that the concept of viṣa must be considered in the etiology of the disease.
4.5.3. Nidānapañcaka (five diagnostic descriptors) and satkriyakala (clinical course) of COVID-19
An attempt is being made here to give a preliminary outline of the nidānapañcaka (five diagnostic descriptors) and ṣaṭkriyākāla (clinical course of the disease).
4.5.3.1. Nidāna (etiology)
The primary cause of COVID-19 is the SARS-CoV-2, which can be classified as an āgantuhetu in Ayurveda. The role of additional supportive factors like weather, diet, lifestyle and other host related factors that influence the clinical course and progression of the disease need to be studied further.
4.5.3.2. Pūrvarūpa (prodromal symptoms)
Without careful assessment of a large number of patients, it is not possible to meticuloulsy document the prodromal symptoms of COVID-19. In principle, we can say that symptoms that do not give a clear indication of a doṣa imbalance can be classified as pūrvarūpa[Ma.Ni.1.5-6] [34]. Since fever is the most common symptom of COVID-19, presentation of symptoms without fever can also be considered as the prodromal stage of the disease. As pointed out earlier, three patients in the cohort of COVID-19 patients that we studied did not report fever and did not progress to severe or critical stage. Asymptomatic and presymptomatic patients will need to be studied closely to profile the prodromal signs of COVID-19. Pre-symptomatic patients develop symptoms later, but asymptomatic patients can remain so until they test negative. A seemingly unnoticed symptom like anorexia and tiredness may be the indication of the development of āma in the prodromal stage and should not be ignored. Some patients may only notice anosmia [57]. Sometimes asymptomatic COVID-19 patients can show lung damage in CT scans or develop severe disease in the later course of the disease [58].
4.5.3.3. Rupa (clinical symptomatology)
The key symptoms of COVID-19 are fever (jvara), cough (kāsa) and shortness of breath (śvāsa), which points to vātakapha dominance. Association of pitta related symptoms and clinical course described earlier indicate that COVID-19 is a type of sannipātajvara. The wide variations in clinical presentations of COVID-19 points to the necessity of identifying sub types based on symptom clusters indicating variations in the tridoṣa imbalance. This calls for a meticulous observation of larger number of patients based on Ayurvedic parameters. Clustering of symptoms was observed in our cohort of COVID-19 patients indicating finer variations in doṣavikalpa, which needs further examination and analysis by a more comprehensive clinical study.
4.5.3.4. Upaśaya (therapeutic response)
Ayurvedic clinical studies need to be conducted to elicit the upaśaya (positive) or anupaśaya (negative) response to confirm the provisional assessment of doṣa imbalance and other Ayurvedic parameters [Ca·S.Vi.St.4.7] [33]. This is all the more relevant to distinguish between prakṛtisamasamavāya (when clinical symptoms reflect underlying doṣa imbalance) or vikṛtiviṣamasamavāya (where clinical symptoms do not reflect underlying doṣa imbalance) type of doṣa imbalance as clarified by Cakrapāṇidatta [Ca·S.Ci.St.3.89-109] [33]. In the Jvaranirṇaya, the importance of making this clinical distinction is emphasised by classification of both dual dosa and sannipāta fevers into the above mentioned two categories in the first verse of the chapter itself [Jvaranirṇaya, Tridosaja.1] [39].
4.5.3.5. Saṃprāpti (pathogenesis)
Being an agantu disease, the disease progresses clinically only when the dosa imbalance is initiated. Saṅkhyāsaṃprāpti – At this point of time, we suggest that COVID-19 is understood as a single disease. However, further clinical studies may help us to sub-classify COVID-19 on the basis of variations in dosa imbalance. Vikalpasaṃprāpti – On the basis of our study, a dominance of vāta and kapha accompanied by mild degree of pitta is seen in the presentation and clinical course of the disease. The possibility of variations in different stages of presentation must be further studied clinically. Prādhānyasaṃprāpti – COVID-19 is an independent disease (svatantravyadhi) though it can worsen in the presence of pre-existing co-morbidities. However, pneumonia, ARDS, fatal cardiac events, stroke and such other complications arise in severe and critical cases. The status of these conditions in terms of dependance (paratantrata) and complication (upadrava) [Ca·S.Ci.St.21.40] [33] as well as independent co-morbidities (vyādhisankara) [Ma.Ni.2.33] [34] needs to be further studied. Complications may require urgent and exclusive attention as pointed out in Carakasamhitā. Four patients in our cohort developed upadravas or complications while seven presented with a vyādhisankara situation with co-morbidities. Balasaṃprāpti – Even though the singular cause of COVID-19 is the SARS-CoV-2, the severity of the disease highly varies from individual to individual. Further studies are needed to understand the role of extrinsic and intrinsic factors that can influence the severity of the disease. Air pollution has been reported to worsen outcomes in COVID-19. On the other hand, the influence of diet and lifestyle is not as well understood. Kālasaṃprāpti – We do not have adequate data to understand the relation between the manifestation of symptoms in relation to diurnal and seasonal variations. Data is also inadequate to conclude whether severity of COVID-19 is linked to cold or warm weather. Meticulous clinical observations are needed to be able to identify specific doṣa imbalances by studying the pattern of fever and other symptoms in relation to different times of the day and night.
4.5.4. Ṣaṭkriyākāla (clinical course of the disease)
Further clinical studies are needed to build a detailed description of the clinical course of COVID-19 from an Ayurvedic perspective. An attempt is being made in this paper to sketch a rough outline of the ṣaṭkriyākāla pointing out the gaps that will need to be addressed by conducting further studies.
4.5.4.1. The Caya, Prakopa and Prasara
The Caya, Prakopa and Prasara stages are difficult to distinguish in an āgantu disease. We can tentatively correlate the incubation period of COVID-19 with this phase. This stage need not be totally asymptomatic and symptoms indicating viral infection (hetuvyañjakalakṣana) may be present but yet not noticed [Ca·S.Su.St.18.5] [33]. Loss of smell and taste, sore throat, diarrhea and such non-specific symptoms have been reported as the only presenting signs of COVID-19 infection. Being the āgantu phase of pathogenesis, doṣa specific symptoms will not be seen.
4.5.4.2. The Stage of Sthānasaṃsraya
The Stage of Sthānasaṃsraya is the stage in which the prodromal symptoms (purvarupa) are manifesting. This stage is not well demarcated in available clinical documentation of COVID-19. Certain presentations with mild symptoms could be potentially classified as the stage of purvarupa but extensive clinical studies are required for a clear understanding.
4.5.4.3. The Stage of Vyakti
The Stage of Vyakti is the symptomatic stage of the disease, which can be mild to moderate or severe. There is further scope for further classification of the clinical presentation of COVID-19 on the basis of specific symptom clusters related to variations in dosa imbalances and location of the disease process.
4.5.4.4. The Stage of Bheda
The Stage of Bheda represents the complications of COVID-19, which is characterized as the critical stage with severe pneumonia, ARDS and hypoxia. This stage of COVID-19 is associated with higher rate of mortality.
Fig. 1 depicts the diagrammatic representation of the clinical course of COVID-19
Fig. 1.
Clinical course of COVID-19.
4.5.5. Sadhyāsādhyata (prognosis)
In the light of information available from published studies, we infer that if kapha is not deranged or depleted, the outcomes are good as are seen in children who have kapha in the natural or pṛākṛta state [Ca·S.Su.St.17.117] [33]. Kapha in the natural state enhances the bala of the system. In old age, there is depletion of kapha and increase of vāyu. Such patients are at risk for progression of disease to severe stage and poor outcomes [22]. In diseases where there is derangement of kapha like diabetes, the prognostic outlook is not good. In diseases like hypertension with derangement of vāta a bad prognosis is expected. The one patient who died in the cohort of our study had hypertension as well as cardiac disease and was 70 years old. However, it is clear that while old age and co-morbidities put the patient at a higher risk of complications and death, with proper medical attention and supportive care, such patients can also recover from the disease. In our cohort, thirteen out of fourteen patients were aged between 64 and 77 years and recovered. All those who developed ARDS had co-morbidities.
Other factors like doṣaprakṛti (tridoṣa constitution) of the individual, the geographical region (deśa) as well as the prevailing season (kāla) during the outbreak may have prognostic implications for COVID-19, which deserves attention. We have not done an extensive analysis of the deha, deśa, kāla or prakṛti in this study. However, based on this preliminary understanding of the disease progression and the doṣavikalpa, an assumption can be made that those individuals with vātakapha prakṛti and tendency for pitta aggravation may be more susceptible to developing complications. Adequate data is not available for further discussion on this topic in this paper. Table 3 provides the summary of the key elements of the Ayurvedic clinical profile of COVID-19.
Table 3.
Ayurvedic clinical assessment of COVID-19.
| Type of Disease | Saṅkrāmika (Contagious, Communicable) |
| Impact of Disease | Janapadodhvaṃsa (Affects large number of human settlements) |
| Disease Nomenclature | Jvara (Fever) |
| Āgantujvara (Fever of exogeneous origin) | |
| Bhutābhiṣaṅgajvara (Fever caused by invasion of pathogens) | |
| Specific Etiology | Viṣakṛmijanya (Caused by virulent pathogen) |
| Doṣavaiṣamya (Nature of doṣa imbalance) | Sannipāta (Derangement of all three doṣas) |
| Doṣavikalpa (Granularity of doṣa imbalance) | Vatakaphapradhāna Pittānubandha (Dominance of Vāta and Kapha with association of Pitta) |
| Dūṣya (Body elements affected) | Rasa (In early stage), Rakta (In late stage) |
| Srotas (Affected body channels) | Prāṇavaha, Udakavaha, Annavaha (Cough and Dyspnoea) , Rasavaha (Fever), Raktavaha (Complications) |
| Rogamārga (Disease Pathways) | Koṣṭha, Śākhā (In early stage), Madhyama (In late stage) |
| Upadrava (Complications) | Śvāskṛcchratā (Shortness of breath), Marmopaghāta (Damage to vital organs) |
| Vyadhisvabhava (Nature of Disease) | Āśukārī (Acute) |
| Sukhasādhyatā (Favourable Prognosis) | Alpaliṅgatva (Mild Symptoms), Ekarogamārgatva (Affects only one disease pathway), Balam (Immunity), Yauvanam (Younger age) |
| Kṛcchrasādhyatā (Difficulty to manage) | Madhyaliṅgatva (Moderate Symptoms), Śvāsakṛcchratā (Shortness of breath), Śākhāgatatva (Involvement of external disease pathway) |
| Asādhyatā (Bad Prognosis) | Vibaddhadoṣatva (Doṣas in mutual opposition), Pūrṇalingatva (Full range of symptoms), Agnināśa (Digestive and metabolic crisis), Vārdhakya (Old age), Rogasaṅkara (Co-morbidities), Marmagatatva (Involvement of vital organs) |
5. Limitations of the study
A critical analysis of the clinical presentation of the disease on the basis of the principles of Ayurvedic nosology suggests that COVID-19 can be categorized as āgantuka type of vātakaphapradhāna sannipātajvara with pittānubandhatva. However, the granularity of the doṣa imbalance as well as its dynamic progression in the course of the disease warrants further investigation and analysis. The wide variation in the incubation period, clinical presentation, clinical course and outcomes of the disease is indicative of the complex interactions between the agent and host factors, which is understood in Ayurveda in terms of interaction between nidāna, doṣa and duṣya. The clinical course of the disease and its evolution into the critical stage in some patients with fatal outcome or disabilities after recovery is characteristic of the clinical course of sannipātajvara described in Ayurvedic texts. Further studies are needed to delineate the various clinical stages (vyādhyavasthās) of the disease to envisage specific therapeutic approaches.
This study has several limitations. At the very outset, we pointed out that Ayurvedic physicians did not have direct access to COVID-19 patients, which ruled out the possibility of a comprehensive clinical assessment of COVID-19 on the basis of Ayurvedic parameters. We have tried to demonstrate that this challenge can be circumvented to some extent by interaction and discussion with Allopathic doctors who are treating COVID-19 patients. However, such an exercise, even when strengthened by review of published literature and classical Ayurvedic literature can only serve the purpose of developing a preliminary clinical profile of COVID-19 from the Ayurvedic perspective. The gaps have been pointed out indicating the specific areas where further studies based on clinical consultation with COVID-19 patients will be needed.
The analysis of clinical data from Medanata demonstrates that it is possible for Ayurveda physicians to cooperate with Allopathic physicians treating COVID-19 patients and that interactions should be encouraged for developing a preliminary understanding of COVID-19 from an Ayurvedic perspective when Ayurvedic physicians do not have direct access to patients. However, it also reveals the challenges in gathering data that is clinically relevant for Ayurveda when Ayurvedic physicians are not directly involved in clinical examination of COVID-19 patients. A comprehensive Ayurvedic understanding of a new disease like this needs clinical examination of patients based on Ayurvedic parameters and a meticulous documentation of clinical symptoms.
6. Conclusion
Based on a preliminary analysis of literature reporting clinical symptoms of COVID-19, study of clinical presentation of a cohort of COVID-19 patients and Medanta and a review of classical Ayurvedic literature, we suggest that COVID-19 can be classified as āgantuka jvara with a vātakaphapradhānasannipāta presentation. The dominance of pitta in certain stages of the disease and in some patients should be considered. However, COVID-19 needs to be further subclassified under the category of vātakaphapradhānasannipātajvara on the basis of a more detailed analysis of clinical symptomatology of a cross section of COVID-19 patients representing diverse populations from different geographical regions in the world.
This paper demonstrates that it is possible to develop provisional Ayurvedic clinical classifications of COVID-19 in consultation with modern medical doctors treating COVID-19 patients, in a regulatory environment that does not permit Ayurvedic doctors from directly managing COVID19 patients. Studies involving larger number of patients are needed to further develop the approach outlined in this paper and formulate a protocol that can be validated at the point of care. Since Ayurveda management is personalized, closer interactions of Ayurveda experts in hospital settings with patients tested positive is important to refine the clinical profiling.
In India, the Central Government has created an Interdisciplinary AYUSH research Task force for COVID -19. The Task Force has set-up several working groups to explore the various possibilities of integrating Ayurveda with standard of care to deal with the COVID-19 epidemic more effectively. In the meantime, the Government of Kerala announced and rolled out a protocol and program for integrating Ayurveda into the management protocol of COVID19, in the State. This initiative shall implement preventive, mitigative and rehabilitative programs based on Ayurveda for better management of the COVID-19 epidemic in the State. Several other State governments are exploring similar possible integrative approaches. Such policy decisions may create a better integrative environment in the future which underlines the significance of this study.
Declaration of competing interest
Dr. Unnikrishnan PM, listed as the third author, is on the Editorial Board of the Journal, but he was not involved in peer review process and editorial decisions related to this paper.
Acknowledgements
We acknowledge with thanks the invaluable contributions made by Geetha Krishnan Gopalakrishna Pillai, Traditional, Complementary, Integrative Medicine Unit, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland in conceptualising the project, bringing together the researchers and clinicians, asking the relevent technical questions, and organising the structured process of developing and redrafting the manuscript.
Footnotes
The views expressed in this article are solely the responsibility of the authors and they do not necessarily reflect the views, decisions, or policies of the institutions with which they are affiliated.
Peer review under responsibility of Transdisciplinary University, Bangalore.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jaim.2020.05.011.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Johns Hopkins University . CSSE) at Johns Hopkins University; 2020. Coronavirus COVID-19 global cases by the center for systems science and engineering.https://coronavirus.jhu.edu/map.html Available at: [Google Scholar]
- 2.Frayer L., Pathak S. 2020. India's doctors worry the country is unprepared for a coronavirus surge. npr.https://www.npr.org/sections/coronavirus-live-updates/2020/03/26/821895160/indias-doctors-worry-the-country-is-unprepared-for-a-coronavirus-surge Available at: [Google Scholar]
- 3.Mampatta S., Das S. Business Standard; 2020. Doctors to hand wash: why India isn't ready for coronavirus crisis.https://www.business-standard.com/article/current-affairs/coronavirus-india-s-readiness-a-concern-due-to-shortage-of-beds-drugs-120031401127_1.html Available at: [Google Scholar]
- 4.World Health Organisation . 2020. COVID-19 strategic preparedness and response plan operational planning guidelines to support country preparedness and response. [Google Scholar]
- 5.National Health Policy . Government of India; 2017. https://www.nhp.gov.in/nhpfiles/national_health_policy_2017.pdf Available at: [Google Scholar]
- 6.TCM aids treatments of over 60,000 COVID-19 cases in China - xinhua | English.news.cn. Xinhua. 2020. http://www.xinhuanet.com/english/2020-02/22/c_138809094.htm Available at: [Google Scholar]
- 7.Liang T. 2020. Handbook of COVID-19 prevention and treatment. [Google Scholar]
- 8.Shah H. Elsevier; 2020. Exploring the effectiveness of traditional Chinese medicine against COVID-19. Pharma R&D Today.https://pharma.elsevier.com/covid-19/exploring-the-effectiveness-of-traditional-chinese-medicine-against-covid-19/ Available at: [Google Scholar]
- 9.Interim clinical guidance for management of patients with confirmed coronavirus disease (COVID-19) Centre for Disease Control and Prevention; USA: 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html Available at: [Google Scholar]
- 10.Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected: interim guidance V 1.2. World Health Organisation; 2020. https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected Available at: [Google Scholar]
- 11.Coronavirus incubation could be as long as 27 days, Chinese provincial government says. Reuters; 2020. 2020. https://www.reuters.com/article/us-china-health-incubation/coronavirus-incubation-could-be-as-long-as-27-days-chinese-provincial-government-says-idUSKCN20G06W Available at: [Google Scholar]
- 12.Symptoms of coronavirus | CDC. 2020. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html Available at: [Google Scholar]
- 13.Seniors with COVID-19 show unusual symptoms, doctors say. Medscape. 2020. https://www.medscape.com/viewarticle/929407 Available at: [Google Scholar]
- 14.Guan W., Ni Z., Hu Y., Liang W., Ou C., He J., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;(382):1708–1720. doi: 10.1056/nejmoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pan L., Mu M., Yang P., Sun Y., Wang R., Yan J. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020 May;115(5):766–773. doi: 10.14309/ajg.0000000000000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA, J Am Med Assoc. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.joob B., Wiwanitkit V. COVID-19 can present with a rash and be mistaken for Dengue. J Am Acad Dermatol. 2020 doi: 10.1016/j.jaad.2020.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Han C., Duan C., Zhang S., Spiegel B., Shi H., Wang W., et al. Digestive symptoms in COVID-19 patients with mild disease severity: clinical presentation, stool viral RNA testing, and outcomes. Am J Gastroenterol. 2020;115(6):916–923. doi: 10.14309/ajg.0000000000000664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kobayashi T., Jung S., Linton M.N., Kinoshita R., Hayashi K., Miyama T., et al. Communicating the risk of death from novel coronavirus disease (COVID-19) J Clin Med. 2020;9:580. doi: 10.3390/jcm9020580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guan W., Liang W., Zhao Y., Liang H., Chen Z., Li Y., et al. Comorbidity and its impact on 1590 patients with covid-19 in China: a nationwide analysis. Eur Respir J. 2020 doi: 10.1183/13993003.00547-2020. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Field Briefing. 2020. Diamond princess COVID-19 cases, 20 feb update.https://www.niid.go.jp/niid/en/2019-ncov-e/9417-covid-dp-fe-02.html Available at: [Google Scholar]
- 24.Nishiura H., Kobayashi T., Miyama T., Suzuki A., Jung S.M., Hayashi K., et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19) Int J Infect Dis. 2020;94:154–155. doi: 10.1016/j.ijid.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Day M. Covid-19: four fifths of cases are asymptomatic, China figures indicate. BMJ. 2020;369:m1375. doi: 10.1136/bmj.m1375. [DOI] [PubMed] [Google Scholar]
- 26.Shi H., Han X., Jiang N., Cao Y., Alwalid O., Gu J., et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis. 2020;20:425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ai T., Yang Z., Hou H., Zhan C., Chen C., Lv W., et al. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: a report of 1014 cases. Radiology. 2020:200642. doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Connors J., States U., Levy J., States U. COVID-19 and its implications for thrombosis and anticoagulation COVID-19 and its implications for thrombosis and anticoagulation Affiliations: 1) department of medicine, hematology division, brigham and Women’s hospital. Blood. 2020;135(23):2033–2040. doi: 10.1182/blood.2020006000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shi S., Qin M., Shen B., Cai Y., Liu T., Yang F., et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.0950. [in press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Poyiadji N., Shahin G., Noujaim D., Stone M., Patel S., Griffith B., et al. COVID-19–associated acute hemorrhagic necrotizing Encephalopathy: CT and MRI features. Radiology. 2020;201187 doi: 10.1148/radiol.2020201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang C., Shi L., Wang F.S. Liver injury in COVID-19: management and challenges. The Lancet Gastroenterology and Hepatology. 2020;5:428–430. doi: 10.1016/S2468-1253(20)30057-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Acaraya Yadavji Trikamji, Acarya Narayan Ram., editors. Susrutasamhita of Sushruta. Chaukhambha Sanskrit Sansthan; Varanasi: 2008. [Google Scholar]
- 33.Acarya Yadavji Trikamji. Chaukhambha Sanskrit Sansthan; New Delhi: 2017. Carakasamhita of Caraka. [Google Scholar]
- 34.Shastri Brahmashankara., editor. Madhavanidana of Madhava. Chaukhambha Surbharati Prakashan; Varanasi: 2012. [Google Scholar]
- 35.Manohar R. Accounts of pathogenic organisms in the early texts of Ayurveda. Indian J Hist Sci. 2012;4:545–559. [Google Scholar]
- 36.Shastri Hari Sadashiva., editor. Astangahrdayam of Vagbhata. Chaukhambha Publications; New Delhi: 2016. [Google Scholar]
- 37.Shastri Brahmashankara., editor. Yogaratnakara of Anonymous authorship. Chaukhambha Sanskrit Bhawan; Varanasi: 2005. [Google Scholar]
- 38.Mishra Brahmashankara., editor. Bhavaprakasha of Bhavamishra. Chaukhambha Sanskrit Series Office; Varanasi: 2002. [Google Scholar]
- 39.Pandita N. Kerala University; Thiruvananthapuram: 1963. Jvaranirnaya. [Google Scholar]
- 40.Sen G. The Chaukhambha Sanskrit Series Office; Varanasi: 1966. Siddhantanidana. [Google Scholar]
- 41.CDC . Management of patients with confirmed 2019-nCoV | CDC. CDC; 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html Available at: [Google Scholar]
- 42.Joob B., Wiwanitkit V. Arthralgia as an initial presentation of COVID-19: observation. Rheumatol Int. 2020;40:823. doi: 10.1007/s00296-020-04561-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lescure F.X., Bouadma L., Nguyen D., Parisey M., Wicky P.H., Behillil S., et al. Clinical and virological data of the first cases of COVID-19 in Europe: a case series. Lancet Infect Dis. 2020;20(6):697–706. doi: 10.1016/S1473-3099(20)30200-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zambrelli E., Canevini M., Gambini O., D'Agostino A. Delirium and sleep disturbances in COVID–19: a possible role for melatonin in hospitalized patients? Sleep Med. 2020;70:111. doi: 10.1016/j.sleep.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Troyer E.A., Kohn J.N., Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Asadi-Pooya A.A., Simani L. Central nervous system manifestations of COVID-19: a systematic review. J Neurol Sci. 2020;413:116832. doi: 10.1016/j.jns.2020.116832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Huang Y., Meng S., Wu S., Zhang Y., Zhang Y.W., Ye Y., et al. The respiratory sound features of COVID-19 patients fill gaps between clinical data and screening methods. medRxiv. 2020 doi: 10.1101/2020.04.07.20051060. [DOI] [Google Scholar]
- 48.Yan C.H., Faraji F., Prajapati D.P., Boone C.E., DeConde A.S. Association of chemosensory dysfunction and Covid-19 in patients presenting with influenza-like symptoms. Int. Forum Allergy Rhinol. 2020 doi: 10.1002/alr.22579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Midgley C.M. medRxiv; 2020. First 12 patients with coronavirus disease 2019 (COVID-19) in the United States. [DOI] [PubMed] [Google Scholar]
- 50.Biospace . Coronavirus dehydration concerns addressed via substantial “SOS hydration” donation targeted to health workers & test-positive patients in hard hit states. Biospace; 2020. https://www.biospace.com/article/releases/coronavirus-dehydration-concerns-addressed-via-substantial-sos-hydration-donation-targeted-to-health-workers-and-amp-test-positive-patients-in-hard-hit-states/ Available at: [Google Scholar]
- 51.Mehra M.R., Ruschitzka F. COVID-19 illness and heart failure. JACC Hear. Fail. 2020 doi: 10.1016/j.jchf.2020.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Babapoor-Farrokhran S., Gill D., Walker J., Rasekhi R.T., Bozorgnia B., Amanullah A., et al. Myocardial injury and COVID-19: possible mechanisms. Life Sci. 2020;253:117723. doi: 10.1016/j.lfs.2020.117723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rabin R.C. Some coronavirus patients show signs of stroke, seizures and confusion. The New York Times; 2020. https://www.nytimes.com/2020/04/01/health/coronavirus-stroke-seizures-confusion.html Available at: [Google Scholar]
- 54.Thevarajan I., Nguyen T.H.O., Koutsakos M., Druce J., Call L., van de Sandt C.E., et al. Breadth of concomitant immune responses prior to patient recovery: a case report of non-severe COVID-19. Nat Med. 2020;26(4):453–455. doi: 10.1038/s41591-020-0819-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hindson J. COVID-19: faecal–oral transmission? Nat Rev Gastroenterol Hepatol. 2020;1 doi: 10.1038/s41575-020-0295-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mehta P., McAuley D.F., Brown M., Sanchez E., Tattersall R.S., Manson J.J., et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395(10229):1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vaira L.A., Salzano G., Deiana G., De Riu G. Anosmia and ageusia: common findings in COVID-19 patients. Laryngoscope. 2020 doi: 10.1002/lary.28692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhao W., Zhong Z., Xie X., Yu Q., Liu J. Relation between chest CT findings and clinical conditions of coronavirus disease (COVID-19) pneumonia: a multicenter study. Am J Roentgenol. 2020:1–6. doi: 10.2214/ajr.20.22976. [DOI] [PubMed] [Google Scholar]
- 59.2020. https://www.worldometers.info/coronavirus/coronavirus-symptoms/
- 60.2020. https://www.nbcnews.com/health/health-news/muscle-aches-extreme-fatigue-coronavirus-symptoms-go-beyond-fever-cough-n1173876
- 61.2020. https://www.unitedregional.org/coronavirus-information/
- 62.Sohal S., Mossammat M. COVID-19 presenting with seizures. IDCases. 2020 doi: 10.1016/j.idcr.2020.e00782. [In press] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.2020. http://www.xinhuanet.com/english/2020-04/22/c_138999564.htm
- 64.Rizzo P., Vieceli Dalla Sega F., Fortini F., Marracino L., Rapezzi C., Ferrari R. COVID-19 in the heart and the lungs: could we “Notch” the inflammatory storm? Basic Res Cardiol. 2020;115(3):31. doi: 10.1007/s00395-020-0791-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.