Abstract
Background:
Polysubstance use (PSU; lifetime use of multiple substances) is common among individuals with problematic alcohol/substance use and is associated with poor prognosis and poor physical/mental health. Furthermore, simultaneous co-use of substances, such that drug effects overlap, is also common and related to unique risks (e.g. overdose). Despite the importance of PSU, current diagnostic systems continue to conceptualize problems with alcohol/substances as class-specific constructs (e.g. Stimulant Use Disorder), which essentially ignore many unique PSU processes.
Methods:
The current study modeled problems with alcohol, cannabis, stimulants, sedatives, opiates, and simultaneous co-use of these substances as a manifestation of a general substance use continuum versus as correlated class-specific constructs in a sample of young-adults(n=2482) using confirmatory factor analysis. Utility of the models was evaluated by examining associations between the general substance use spectrum and class-specific latent factors with measures of anxiety, ADHD, adult antisocial problems, borderline symptoms, neuroticism, and intelligence in a subset of the sample(n=847).
Results:
Findings supported the conceptualization of problems with all substances, including couse of substances, as being manifestations of a general substance use spectrum, as class-specific constructs were not differentially associated with other measures of psychological dysfunction. Examination of this general substance use spectrum indicated that all substances, separately and co-use, were robustly informative of this spectrum, but tended to discriminate between different severity levels.
Discussion:
The general substance use spectrum allows for integration of information from the use and co-use of all substances to provide better assessment of overall problems with substances compared to class-specific constructs.
Keywords: alcohol, substance use, co-use, polysubstance, externalizing, HiTOP, item-response, drugs
1. Introduction
Epidemiological and genetic studies have shown a consistent pattern of co-occurrence of disorders related to substance use/abuse including alcohol, cannabis, and other drug use disorders that share common genetic risk (Bierut et al., 1998; Krueger, Markon, Patrick, Benning, & Kramer, 2007; Krueger, Markon, Patrick, & Iacono, 2005; Witkiewitz et al., 2013). Data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) found that the majority of individuals with a substance use disorder (SUD) had at least one other co-occurring SUD and that these individuals had a worse prognosis than those with single disorders (McCabe, West, Jutkiewicz, & Boyd, 2017). Furthermore, polysubstance use (PSU) has been shown to elevate risk for poor outcomes, such as deteriorating physical health, risky behaviors, and overdose (Feigelman et al., 1998; Earlywine. and Newcomb, 1997; Petry, 2001), in addition to other forms of psychological dysfunction (Connor et al., 2013; Hedden et al., 2010).
Importantly, PSU is an understudied and sometimes ill-defined multifaceted construct. Specifically, PSU can be operationalized as usage of multiple substance over a long time span (e.g. lifetime or past six months), having multiple SUDs, or simultaneous co-use of at least two substances where the effects of the substances overlap in a short time-span. Very few studies have examined simultaneous co-use of substances (Bailey, Farmer, & Finn, 2019; Herbeck et al., 2013; Olthuis, Darredeau, & Barrett, 2013; Quek et al., 2013) with most studies finding that the rates of reported simultaneous co-use were high in individuals when use of the individual substances was clinically problematic. In summary, understanding the assessment and etiology of problems with multiple substances (including co-use of multiple substances) should continue to be of high priority in our understanding of externalizing pathology.
A promising direction to understanding co-occurrence of symptomology across a variety of disorders, as in PSU, are hierarchical latent factor models (e.g. HiTOP model, Kotov et al., 2017) that aim to model psychopathology comorbidity as manifestations of broad dimensions of psychopathology (e.g. internalizing or externalizing). Research has consistently supported the importance and coherence of an externalizing dimension of psychopathology that explains the interrelation of many disorders characterized by poor behavioral regulation such as alcohol use disorder (AUD), SUD, conduct disorder, and antisocial personality disorder (ASPD) (Bobova et al., 2009; Krueger et al., 2007, 2005; Slade and Watson, 2006; Vollebergh et al., 2001). Some studies have identified a substance use subfactor within the broader externalizing dimension that denotes the close association between issues of alcohol, cannabis, and other illicit substances (Bailey & Finn, 2019; Derringer et al., 2013; Krueger et al., 2007; Sunderland, Slade, & Krueger, 2015). This substance use subfactor conceptualizes symptoms of AUD, CUD and all other SUDs as manifestation of a more general and continuous substance use dimension. For example, a recent study by Franco et al. (2019) found that adverse outcomes related to alcohol/substance use (e.g. marital problems, financial concerns, and poor physical health) were associated with this continuous dimension underlying problems with all substances and not differentially related to specific drug classes. Importantly, this is not the conceptualization underlying current diagnostic systems (DSM-V, American Psychological Association, 2013; ICD-10 World Health Organization, 1992), which continue to have separate substance specific disorders. The conceptualization of alcohol/substance use problems as related substance class specific constructs (e.g. AUD and SUD) with their own substance-specific criteria versus a general substance use continuum has important implications for the research, assessment, and treatment of substance use problems.
The current study aims to examine the utility of modeling criteria of problematic use across substance classes (i.e. alcohol, cannabis, stimulants, sedatives, and opiates) as a general substance use spectrum (i.e. unidimensional) versus as correlated substance specific constructs. These different approaches are then compared by examining their predictive value with other relevant psychosocial measures: anxiety, ADHD, adult antisocial problems, borderline personality disorder (BPD) symptoms, neuroticism, and intelligence (IQ). Specifically, the current study examines whether measures of psychological dysfunction have substance class-specific associations or are primarily associated with the underlying general substance use continuum. In addition, clinical implications of these conceptualizations are discussed, including the benefits of a more holistic approach to examining problems with alcohol/substances. Lastly, the current study, for the first time, is able to directly examine how simultaneous co-use behaviors fit into dimensional models of substance use problems.
2. Methods
2.1. Sample Characteristics
The current sample consisted of 2482 (51% female) young adults 18–30 years old with a mean age of 21.55 (SD = 2.61). The sample was originally recruited for a large study on risky decision-making and externalizing psychopathology (Finn, Gunn, & Gerst, 2014). This sample was intentionally recruited for a wide array of externalizing problems with 55% having an AUD, 40% with Cannabis Use Disorder (CUD), 26% with another illicit drug use disorder (DUD). In the current study, the majority of diagnoses (80% of the sample) were diagnosed using Diagnostic and Statistical Manual of Mental Disorders fourth Edition (American Psychiatric Association, 2000) alcohol, cannabis, and drug abuse/dependence criteria, while the remaining sample utilized DSM-V (American Psychiatric Association, 2013) AUD, CUD, and other DUD criteria. In the current study, AUD, CUD, and other illicit DUDs include both DSM-IV abuse/dependence, and DSM-V AUD, CUD, and DUD diagnoses. This study was reviewed and approved by the University Institutional Review Board (IRB) and all participants gave informed consent.
2.2. Recruitment
The sample was recruited predominantly through flyers, in addition to advertisements in local newspapers, business cards placed in the community, and postings on the University student classified page. The flyers/postings were designed utilizing an approach to obtain both a large proportion and wide range of individuals across substance use and externalizing spectrums (Finn et al., 2009). For example, flyers/postings asked for “adventurous/daring” individuals, “impulsive individuals”, and “social drinkers.” Although inclusion criteria varied slightly throughout recruitment, the majority of the sample was recruited to examine alcohol misuse and comorbid pathology; therefore, individuals were not retained if they had externalizing diagnoses without an alcohol use disorder. Of note, research has indicated that substance use disorder without problematic alcohol use is rare (see Connor et al., 2014 for review).
2.3. Screening Interview
Those who responded to advertisements were screened via telephone to determine study eligibility. Participants were informed that they must abstain from using alcohol and other drugs for at least 12 hours before study sessions. Respondents who met study inclusion criteria could read and speak English, had at least a 6th grade education, did not report any history of severe head injuries, did not report a history of psychosis, had consumed alcohol on at least one occasion in their life, and were between ages 18 and 30.
2.4. Test session exclusion criteria
Before every testing session participants were required to meet a set of criteria before proceeding. All participants were required to (1) have no self-reported use of drugs or alcohol within the past 12 hours prior to testing, (2) have gotten at least 6 hours of sleep the previous night, (3) have a breath alcohol level of 0.0% (tested with an AlcoSensor IV, Intoximeters Inc., St. Louis MO), and (4) not be experiencing symptoms of substance-related withdrawal or any medical illness. Subjects were rescheduled if they did not meet these criteria.
2.5. Alcohol/Substance Use Measures and Diagnoses
Participants were administered the Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA; Bucholz et al., 1994) to assess lifetime diagnoses of AUD, CUD, and DUD. The SSAGA has demonstrated good construct validity when compared with other semi-structured interviews (Hesselbrock, Easton, Bucholz, Schuckit, & Hesselbrock, 1999), good test-retest reliability (Bucholz et al., 1994), and inter-rater reliability (Bucholz et al., 1995; Bucholz et al., 1994). DSM-IV and DSM-V diagnoses were obtained by using the respective sections of the SSAGA interview to obtain lifetime occurrence of DSM diagnostic criteria (see Sample Characteristics section). If diagnostic criteria were present, responses were further queried to examine whether symptoms occurred within the specified time-frame to meet diagnostic criteria.
Alcohol/substance use indicators for the models tested included 39 dichotomous items from the SSAGA examining lifetime problems with the following substance classes: alcohol, cannabis, stimulant, sedative, and opiate. These items were selected to cover a broad range of severity within each substance-class. Participants were asked whether they had developed
tolerance, had failed to cut down 3+ times, had substances interfere with their responsibilities, and experienced withdrawal for each substance class respectively. In addition, whether the participant had ever had a very strong desire to use cannabis, stimulants, opiates, and sedatives (this item is not included in the SSAGA for alcohol). Lastly, participants were asked whether they had ever used every combination of the above drug classes simultaneously (i.e. using cannabis and sedatives at the same time). Supplementary Table 1 provides the exact items used in the analyses.
2.6. Intelligence and Trait Measures
Trait anxiety was assessed using the 20-Likert item Trait Anxiety Inventory (TAI) section of the State-Trait Anxiety inventory (Spielberger, 1983). Participants were administered the Attention-Deficit Hyperactivity Disorder (ADHD) and Antisocial Personality Disorder (ASPD) sections of the SSAGA. Problem count measures were created for ADHD and adult antisocial symptoms by summing positive responses to SSAGA questions related to core diagnostic features in the respective diagnostic sections. Intelligence (IQ) was assessed using the Wechsler Abbreviated Scale of Intelligence (WASI; Wechsler, 1999). Neuroticism was assessed using the 23 dichotomous-item neuroticism section of the Eysenck Personality Questionnaire (Eysenck & Eysenck, 1975). Lastly, borderline personality disorder (BPD) symptoms were examined using assessed using the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) screening questionnaire for BPD symptomatology (First et al., 1995), which dichotomizes items from the SCID-II BPD section by asking whether a participant “generally” endorses the given traits/behaviors. Table 1 provides descriptive statistics for the subset of individuals used to examine the utility of factor scores generated from competing models.
Table 1.
Validation Sample Characteristics
| Characteristic | Value | Range (Min - Max) | Cronbach’s Alpha |
|---|---|---|---|
| n (male/female) | 847 (458/389) | - | - |
| Age Mean(± SD) | 21.24 (2.50) | 18 – 30 | - |
| Diagnostic Infoi mation | |||
| % (n) with Alcohol Use Disorder | 67% (571) | - | - |
| % (n) with Cannabis Use Disorder | 48% (410) | - | - |
| % (n) with other Drug Use Disorder | 20% (167) | - | - |
| Trait Measures | |||
| Antisocial Personality M (± SD) | 6.74 (6.48) | 0 – 37 | .90 |
| ADHD M (± SD) | 9.80 (10.12) | 0 – 37 | .96 |
| Intelligence (IQ) M (± SD) | 111.60 (10.19) | 79 – 144 | - |
| Borderline Personality M (± SD) | 3.79 (3.36) | 0 – 15 | .77 |
| Trait Anxiety M (± SD) | 38.95 (9.40) | 21 – 71 | .92* |
| Neuroticism Questionnaire M (± SD) | 8.58 (5.49) | 0 – 23 | .87 |
ADHD = Attention Deficit Hyperactivity Disorder, Antisocial Personality = adult antisocial problems, Borderline Personality = Borderline Personality symptoms.
Ordinal Alpha.
2.7. Statistical Analyses
R version 3.5.3 was used for these analyses (R Development Core Team, 2013), including use of the “lavaan” package for confirmatory factor analyses (Rosseel, 2012), “missForest” package for missing data imputation (Stekhoven & Bühlmann, 2012), and the “ggplot2” package for figure generation (Wickham, 2016).
2.7.1. Data imputation.
Data from SSAGA, which was the source of alcohol/substance use items, consisted of less than 1% missing data. Personality and cognitive measures used to examine the utility of factor scores in a subset of the data contained less than 2% missing data. Missing data was examined both visually and through testing associations between missing values and existing data to make sure the data was appropriate for imputation (Van Buren, 2018). Missing data, in both cases, was imputed using a random forest algorithm (Stekhoven & Bühlmann, 2012) using all other non-missing data in each data set respectively. Random forest imputation has been demonstrated to outperform other imputation methods and is considered highly accurate when imputing both continuous and non-continuous data as in the current study (Stekhoven & Bühlmann, 2012; Waljee et al., 2013).
2.7.2. Confirmatory Factor Analysis.
CFA analysis were conducted using the weighted least squares mean and variance adjusted estimator (WLSMV in “lavaan” package), which is the estimator commonly used for dichotomous data such as the variables in the current study (Brown, 2006). CFA analyses are used to compare both a unidimensional model where all alcohol, substance, and co-use items load onto a single general substance use factor and a five-factor correlated model where each substance class (i.e. alcohol, cannabis, stimulant, sedative, and opiate) has its own latent factor consisting of the respective items for each drug class. In the correlated factor model, each simultaneous co-use item was cross-loaded onto the two latent factors that made up the combination. For example, the alcohol and cannabis co-use item was set as an indicator of both the alcohol and cannabis latent factors. Fit indices selected to evaluate the CFA models was the root mean squared error of approximation (RMSEA), Tucker-Lewis Index (TLI), and the chi-square test statistic (mean/variance adjusted; see Rosseel, 2012). Adequate model fit is reflected by a RMSEA upper 90% Confidence Interval (CI) of <.08 (Kline, 2011), TLI of >.94 (Bentler & Bonett, 1980; Browne & Cudeck, 1992), and traditionally a non-significant chi-square. However, studies have indicated that for larger sample sizes (n>200) the chi-square is unlikely to be non-significant even in models with very good fit based on other indices (Brown, 2006).
2.7.3. Factor scores and model validation.
After estimation of CFA models, factor scores were generated using the Empirical Bayes Modal method (EBM; Skrondal and Rabe-Hesketh, 2004), which is the recommended method for factor scores generated from models using non-continuous indicators (Rosseel, 2012). A subset of the sample (n = 847) that completed a variety of additional measures was selected to examine associations between factor scores from the two models. Spearman correlations were calculated between the factor scores from the unidimensional and correlated models with measures of anxiety, ADHD, adult antisocial problems, BPD symptoms, neuroticism, and intelligence. These measures were chosen to provide a wide spread of associations between the factor scores and measures of internalizing pathology, other externalizing pathology, and general cognitive ability.
2.7.4. Item-Response information analysis.
Lastly, given that CFA with binary outcomes is essentially equivalent to a two-parameter normal ogive IRT model (Ferrando & Lorenzo-Seva, 2005; Moustaki, Jöreskog, & Mavridis, 2004; Reise, Widaman, & Pugh, 1993), an additional IRT information analyses was conducted to provide a visual and practical illustration of the general substance use continuum. Specifically, providing an illustration of how different drug class items provide information across the spectrum. Factor loadings are analogous to discrimination parameters in illustrating the relationship between item-endorsement and the latent factor of interest. CFA threshold parameters are analogous to IRT severity or “ability” parameters, which illustrate what level of the latent trait is needed to expect an endorsement of the item and, subsequently, how certain items aid to discriminate between individuals of varying severity levels. CFA loadings and thresholds from the unidimensional model were converted to IRT discrimination and severity parameters (see Brown, 2015). IRT discrimination parameters were computed using:
where a is the IRT discrimination parameter and λ is the item factor loading divided by the square root of the residual variance (e). IRT severity estimates were calculating using:
where b is the IRT severity parameter, τ is the CFA item threshold, and λ is the item factor loading (Baker, 2001). IRT parameters could then be utilized to calculate and illustrate the aggregate test information provided from the items broken down by substance class. This provides a representation of what class of substances provides the most information about the general substance use continuum, in addition to showing how different substance class items “overlap” in their ability to provide information about this continuum. The equation to calculate the information of a given item (subscripted i) at a given severity level (denoted as θ) is provided below.
where: ai is the discrimination and bi is the severity parameter for the item i
The aggregate test information is simply a summation of the information provided by all the items related to each substance class. The test information function provides valuable insight about the amount of information provided from a set of items across the levels of severity and importantly has a reciprocal relationship with the standard error of estimation, such that latent traits estimates are most accurate in areas with maximum information.
3. Results
3.1. Confirmatory Factor Analysis
CFA of the unidimensional model with all items loading onto a single general substance use factor showed adequate or just below adequate fit based on the following fit indices χ2(702) = 6916.60, p < .001, TLI = .93, RMSEA = .06 90% CI [.058 , .061]. The five-factor correlated factor model fit the data well χ2(682) = 21060.63, p < .001, TLI = .98, RMSEA = .029 [.028, .03]. Table 2 shows the factor loadings from the unidimensional and correlated factor models, in addition to threshold values from the unidimensional model. Unidimensional factor loadings indicated that all items were robust indicators of the general substance use factor with factor loadings ranging from .49-.95. Stimulant, sedative, and opiate items were the strongest indicators of the general factor, followed by cannabis items and then alcohol items. Lastly, thresholds indicated that although alcohol items were of the lowest severity, followed by cannabis, and then other illicit substances, there was substantial overlap between drug class criteria (e.g. most severe cannabis items were more severe than lowest severity stimulant/opiate items). Simultaneous couse items were overall very strong predictors of the general substance use factor with a wide variety of severity (i.e. large variation of thresholds). This indicates that co-use items are very important indicators across the moderate to high end of substance use severity continuum. In the correlated model, the alcohol latent factor was moderately correlated with other latent factors (.54-.59), the cannabis latent factor was moderately correlated with other illicit drug factors (.58-.65), and all the other illicit drug factors were highly correlated (.70-.80).
Table 2.
Factor Loadings
| Item | Threshold | gSUd | Alc | Can | Stim | Sed | Op |
|---|---|---|---|---|---|---|---|
| Alcohol Items | |||||||
| Alc. Tolerance | −0.35 | 0.54 | 0.74 | ||||
| Alc. Interfered | 0.36 | 0.57 | 0.78 | ||||
| Alc. Desire | 1.00 | 0.53 | 0.73 | ||||
| Alc. Withdrawal | 0.82 | 0.62 | 0.85 | ||||
| Alc. Failed to Cut | 1.10 | 0.55 | 0.75 | ||||
| Cannabis Items | |||||||
| Can. Tolerance | 0.32 | 0.81 | 0.91 | ||||
| Can. Time | 0.42 | 0.83 | 0.94 | ||||
| Can. Interfered | 0.92 | 0.61 | 0.72 | ||||
| Can. Desire | 0.93 | 0.70 | 0.81 | ||||
| Can. Withdrawal | 0.97 | 0.73 | 0.85 | ||||
| Can. Failed to Cut | 1.33 | 0.57 | 0.68 | ||||
| Stimulant Items | |||||||
| Stim. Tolerance | 1.11 | 0.85 | 0.92 | ||||
| Stim. Time | 1.30 | 0.91 | 0.96 | ||||
| Stim. Interfered | 1.51 | 0.87 | 0.92 | ||||
| Stim. Desire | 1.34 | 0.90 | 0.94 | ||||
| Stim. Withdrawal | 1.15 | 0.93 | 0.98 | ||||
| Stim. Failed to Cut | 1.61 | 0.88 | 0.94 | ||||
| Sedative Items | |||||||
| Sed. Tolerance | 1.45 | 0.84 | 0.93 | ||||
| Sed. Time | 1.71 | 0.84 | 0.92 | ||||
| Sed. Interfered | 1.68 | 0.83 | 0.92 | ||||
| Sed. Desire | 1.80 | 0.81 | 0.89 | ||||
| Sed. Withdrawal | 1.53 | 0.86 | 0.96 | ||||
| Sed. Failed to Cut | 1.97 | 0.79 | 0.88 | ||||
| Opiate Items | |||||||
| Op. Tolerance | 1.24 | 0.92 | 0.97 | ||||
| Op. Time | 1.46 | 0.95 | 0.97 | ||||
| Op. Interfere | 1.60 | 0.89 | 0.94 | ||||
| Op. Desire | 1.49 | 0.94 | 0.97 | ||||
| Op. Withdrawal | 1.35 | 0.95 | 0.98 | ||||
| Op. Failed to Cut | 1.73 | 0.92 | 0.96 | ||||
| Co-use Items | |||||||
| Alc + Can | 0.26 | 0.82 | 0.19 | 0.79 | |||
| Alc + Stim | 1.32 | 0.49 | 0.23 | 0.38 | |||
| Alc + Sed | 0.97 | 0.75 | 0.24 | 0.69 | |||
| Alc + Op | 0.89 | 0.70 | 0.37 | 0.52 | |||
| Can + Stim | 0.86 | 0.75 | 0.46 | 0.43 | |||
| Can + Sed | 1.25 | 0.68 | 0.31 | 0.51 | |||
| Can + Op | 1.10 | 0.70 | 0.37 | 0.47 | |||
| Stim + Sed | 1.74 | 0.63 | 0.45 | 0.28 | |||
| Stim + Op | 1.68 | 0.74 | 0.39 | 0.48 | |||
| Sed + Op | 1.70 | 0.69 | 0.28 | 0.50 | |||
All loadings are significant at p<.001. Alc = Alcohol, Can = Cannabis, Stim = Stimulants, Sed = Sedatives, Op = Opiates, Time = Great deal of time spent using [substance], obtaining [substance], or getting over effects, Interfered = Interfered with responsibilities, Desire = Strong desire for substance, Failed to Cut = Failed to cut down on [substance] 3 or more times.
3.2. Factor Scores Model Comparisons
Table 3 presents the correlations of factor scores from the unidimensional and correlated factors models with measures of adult antisocial problems, ADHD, intelligence, BPD symptoms, anxiety, and neuroticism in a subset of the sample. The pattern of associations was very consistent across the factor scores generated from the unidimensional model (i.e. general SUD factor) and the factors scores for each specific drug class from the correlated model. All factor scores had a robust positive relationship to adult antisocial problems, ADHD problems, and BPD symptoms. In addition, all factors had a weak positive association with internalizing measures (i.e. anxiety and neuroticism). All had a modest negative association with IQ. Most importantly, the specific drug class factor scores from the correlated model did not show any striking differential associations with external measures; for example, the alcohol latent factor did not have a stronger association to anxiety than other substance classes. Important to note, the general SUD factor scores were highly correlated with factor scores from the correlated model. The general SUD factor was correlated .80 with the Alcohol factor, .90 with Cannabis factor, and .93-.94 with the other illicit drug factor scores. In summary, there appears to be strong evidence for the utility of a general substance use model as it appears to capture the meaningful variation related to other forms of psychological dysfunction in a more parsimonious model than the correlated model.
Table 3.
Correlations of Factor Scores and External Criteria
| ASP | ADHD | IQ | B PD | TAI | NEU | |
|---|---|---|---|---|---|---|
| GSUD | 0.65 | 0.41 | −0.17 | 0.50 | 0.26 | 0.28 |
| Alc | 0.57 | 0.40 | −0.18 | 0.44 | 0.27 | 0.27 |
| Can | 0.63 | 0.41 | −0.15 | 0.50 | 0.24 | 0.26 |
| Stim | 0.63 | 0.39 | −0.15 | 0.48 | 0.24 | 0.26 |
| Sed | 0.64 | 0.40 | −0.16 | 0.49 | 0.26 | 0.28 |
| Op | 0.64 | 0.39 | −0.16 | 0.48 | 0.26 | 0.27 |
All coefficients are significant at p <.001. Each line shows the spearman correlation between factor scores and IQ = Intelligence Quotient, ASP = Antisocial Personality, ADHD = Attention Deficit Hyperactivity Disorder, BPD = Borderline Personality Disorder, TAI = Trait Anxiety Inventory, NEU = Eysenck Personality Neuroticism Subscale. GSUD = general SUD factor, Alc = alcohol, Can = cannabis, Stim = stimulant, Sed = sedative, Op = opiate
3.3. Test Information of the General Substance Use Spectrum
Figure 1 provides a visual representation of the information provided by the items in the current analyses broken down by drug class and co-use items. As can be seen there is significant overlap between the information gained by different sets of items (i.e. drug classes). Alcohol and cannabis items provide their peak information at lower levels of severity compared to the illicit drugs and in general provide less information spread across a wide array of severity levels. Couse items provided significant information across the majority of severity levels. This is due to the fact that some co-use items (e.g. alcohol and cannabis) help to discriminate between lower and moderate severity while other co-use items (e.g. cannabis and opiates) distinguish moderate from high severity (see co-use thresholds in Table 2). Illicit drugs besides cannabis showed very high amounts of information at a more restricted range of severity. The trait level where information peaked (i.e. highest information) was 1.15, .67, 1.42, 1.96, 1.54, and 1.35 for alcohol, cannabis, stimulant, sedative, opiate, and co-use items respectively (see Figure 1).
Figure 1. Aggregate information by item types.
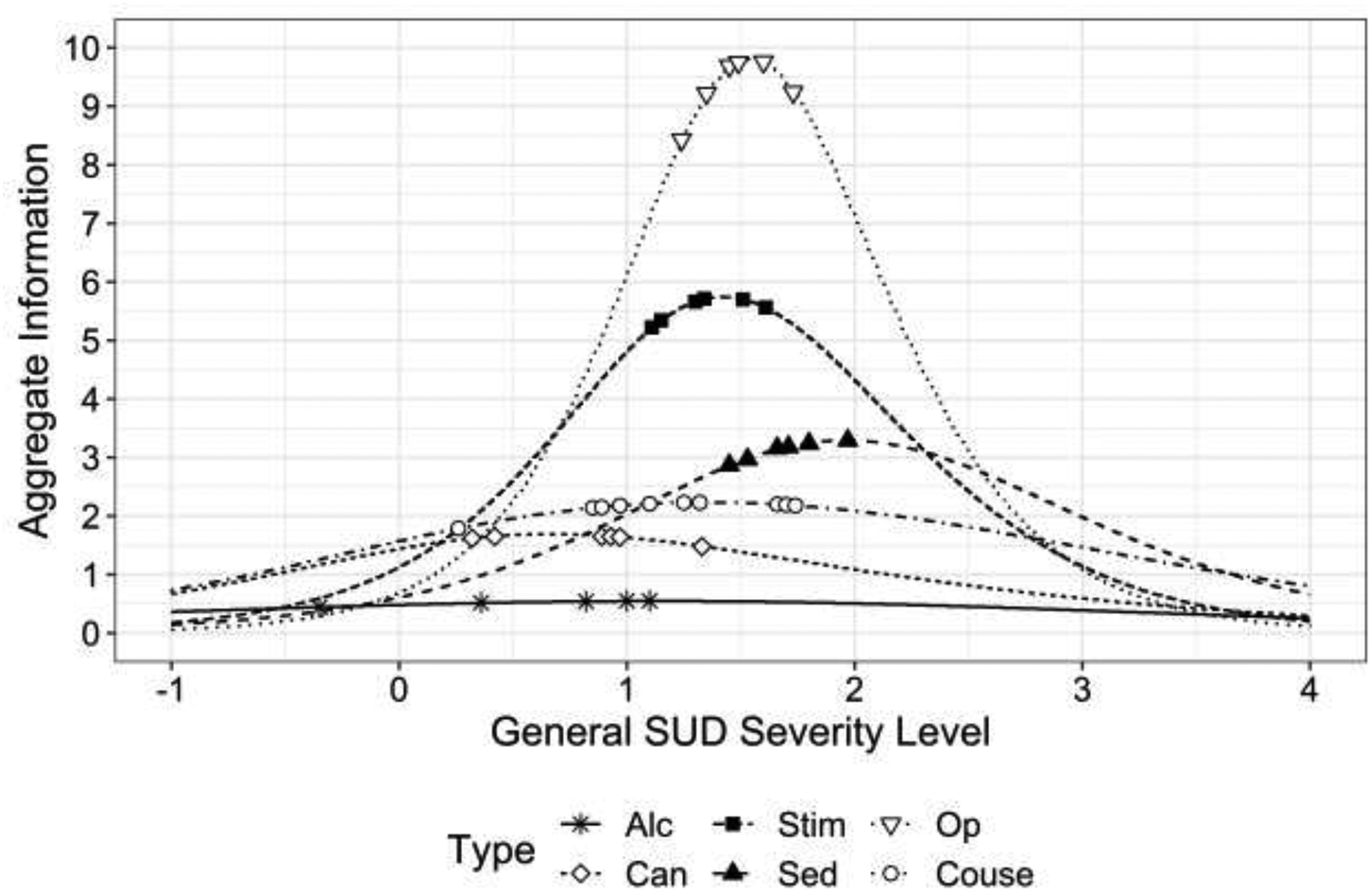
Alc = Alcohol, Co-Use = Co-use items, Can = Cannabis, SED = Sedative, STIM = Stimulant, OP = opiate. Severity Level is the trait level on the general substance use dimension. Aggregate information is the plotted total information provided from all items from a given type of items (e.g. alcohol versus opiate). Symbols are placed at the item thresholds of each substance class respectively.
4. Discussion
The current study examined the utility of modeling criteria of problematic alcohol, cannabis, stimulant, opiate, and sedative use as both correlated substance specific constructs (i.e. consistent with current diagnostic nosology) and as a unitary construct where all criteria are modeled as manifestations of a general substance use factor. CFA analyses indicated that both models fit the data at least reasonably well. The correlated class-specific factors model unsurprisingly showed an improvement in fit over the unidimensional model given that it has more parameters and may be capitalizing on superficial associations between items of the same class (e.g. related to drug availability) while the predominant association between items is actually that of the general construct (i.e. overall severity) as the current results suggest (Chen, West, & Sousa, 2006; Reise et al., 2007). Importantly, factor scores generated from these competing models showed essentially the same pattern of associations with external criteria. The external measures covered a wide breadth of psychological measures including measures of externalizing constructs (i.e. antisocial problems and ADHD), internalizing constructs (i.e. anxiety and neuroticism), IQ, and BPD symptoms. As seen in Table 2, patterns of association indicated a lack of discriminate validity between substance specific factors. Put another way, the association between severity of use with a given substance and other measures of dysfunction does not appear to be moderated by the type of substance. This is consistent with previous research showing that the associations between alcohol/substance use symptoms and both other mental health disorders (Sunderland et al., 2015) and adverse outcomes (Franco et al., 2019) can almost entirely be explained by a general substance use latent factor. Taken together, there appears to be mounting evidence of the importance of what is common underlying AUD, CUD, and SUDs, perhaps more so than evidence stressing their unique contributions to our understanding of psychopathology.
Close examination of the unidimensional general substance use model provides important insights into this broader substance use spectrum. As can be seen in Table 2, all items were robust indicators of the general substance factor indicating that all criteria tested were strongly related to the general substance use spectrum. Items related to illicit drug use were most highly informative of general substance use severity, followed by cannabis items, and then alcohol items. This is consistent with previous findings that utilized dichotomous indicators of DSM dependence and found that cocaine, cannabis, and “other” substance dependence (i.e. included opiates, sedatives, and amphetamines) were mostly highly informative of a general externalizing dimension (Carragher et al., 2014).
Examining the threshold parameters in Table 2 indicates that as expected alcohol use items tended to be of the lowest severity followed by cannabis, and finally other illicit drugs. Importantly, although overall some substance classes appear to be indicative of higher severity, there is substantial overlap across substance class item sets. For example, the most severe alcohol use items are more severe than the lowest severity cannabis items and the highest severity cannabis items are of higher severity than the lowest level illicit drug items. This is valuable information to demonstrate that drug of choice, although an important indicator is not sufficient to conclude severity of overall substance use problems. This is consistent with Carragher et al., (2014) who demonstrated substantial severity overlap across alcohol/substance dependence diagnoses. The current study is able to extend this work by providing a more granular examination of the overlap between problems with different substances by using an item-level approach. Furthermore, although within each substance there are differences between the ordering of item severity (i.e. ordering of item thresholds), there are some general similarities. Endorsing tolerance to a substance was consistently the lowest severity item in each set, while failing to cut down was consistently one of the highest severity items. As seen in Figure 1, this general substance use spectrum can be conceptualized as being assessed by extensively overlapping substance specific item sets that discriminate between individuals at different levels of severity. A major benefit of the general substance use continuum approach is its ability to integrate information from all substances leading to substantial information across a wide range of severity leading to high precision estimates of severity.
This is the first study to examine how simultaneous co-use of substances relates to the broader dimension of substance use. Although co-use behaviors are rarely assessed and totally absent from diagnostic criteria, the current study shows the immense value of these items to the assessment of substance use problems. Co-use behaviors were all robustly related to the general substance use factor indicating a strong relationship with the general substance use spectrum (see Table 2). Furthermore, co-use items provided information across a wide range of severity (see Figure 1), as different combinations of substances appear to discriminate between different levels of severity. Therefore, the inclusion of co-use items in substance use measures would serve to increase reliability and precision of severity estimates of this general substance use dimension. In addition to the current findings, previous research indicates that co-use behaviors are quite common in individuals with problematic use of substances (Bailey et al., 2019; Quek et al., 2013) and may increase risks for specific negative outcomes (e.g. overdose risk with opiate and sedative co-use; Gudin, Mogali, Jones, & Comer, 2013). Therefore, integration of co-use behaviors into our conceptualization and assessment of problematic substance use is of the utmost importance. However, current diagnostic frameworks focus on substance class-specific criteria, whereas a more general approach to assessing problematic general substance use would drastically increase our ability to integrate various co-use behaviors.
This described change in conceptualization and assessment of alcohol/substance use problems as indicators of a unified substance use spectrum has significant clinical implications. Consider the following example, in the current study three participants were selected whose factor scores on the general substance use dimension were the following: Person A = 1.09, Person B = 1.13, and Person C = 1.10. Despite all three individuals having essentially the same severity level on this general substance use spectrum, their specific substance use patterns and diagnostic pictures are actually quite different. Person A has endorsed nearly all the cannabis items, multiple stimulant and sedative items, none of the alcohol, co-use, or opiate items, and has a CUD and DUD diagnosis. Person B has endorsed six of the co-use items, a couple cannabis, alcohol, and opiate items, and has no formal diagnoses. Lastly, Person C has endorsed all of the alcohol and stimulant items, with no other criteria endorsed and has an AUD and DUD diagnosis. This is meant to demonstrate how very different substance use patterns and diagnostic pictures can actually be indicative of nearly indistinguishable severity levels. However, rarely in applied clinical settings or research are individuals assessed based on a more holistic approach to their substance use patterns. This is particularly problematic in cases like Person B who actually does not meet for a formal diagnosis but has enough subthreshold problems, with multiple substances and significant co-use, that are indicative of substance use severity like individuals with multiple diagnoses (i.e. Person A and C).
The current findings have major implications both for assessment in research studies and clinical settings. In research settings, investigators should explicitly contextualize their work within these dimensional frameworks. For example, neuroscience efforts to examine the neural circuitry underlying self-control deficits (a problem associated with all types of substance use) should consider linking neural measures to the general substance use factor. This would provide increased precision of severity estimates and aid to integrate findings examining different substance use classes.
In clinical settings, assessment of a general substance use factor has the potential to provide clinicians with a richer and more precise estimation of problems related to substance use. For example, clinicians treating individuals seeking treatment for a single substance (e.g. AUD) should be sure to integrate information from all other substances, including co-use, to assess severity when making decisions such as appropriate level of care. Simply relying on DSM or ICD assessment of individual disorders (e.g. AUD) does not give a necessarily accurate picture of an individual’s overall impairment with substances. Beyond these informal suggestions, continuing work in this research line may lead to interest in major structural changes to the assessment of problems with alcohol/substances. As DSM-V moved from multiple categorical diagnoses for each substance class (e.g. abuse and dependence in DSM-IV) to dimensional measures of each substance (e.g. mild, moderate, severe), perhaps future nosology will embrace a broader substance use dimension and move beyond substance specific constructs. Although this idea may sound extreme, it is consistent with broader trends in the field both in assessing problems with substances as unitary construct (Franco et al., 2019; Carragher et al., 2014; Gibbons et al., in-press) and current approaches focusing on empirically derived dimensions of psychopathology (e.g. HiTOP; Kotov et al., 2017).
4.1. Limitations
The results of the current study need to be interpreted in light of the study’s limitations. First, the current study is restricted to relatively narrow age range, which may limit generalizability to older adult samples. Previous research has established that extensive alcohol use is relatively common in young adults, especially those enrolled in college (Slutske, 2005; White & Hingson, 2013). Given that this sample is primarily young adults, a large portion of which are students, it may not be surprising to see that alcohol use items were the least strongly related to general substance use pathology. In older adults, it is likely that AUD criteria may be more strongly associated to general problematic substance use because, at that developmental stage, extensive alcohol consumption is less socially acceptable. Second, the current study methods were limited to the analysis of co-use of two substances at once and, more specifically, to lifetime occurrence of this behavior. Given the results of the current study, more detailed examination of co-use behaviors is warranted, such as examining how the frequency of these behaviors (e.g. co-use weekly) is related to general substance use severity. Third, the majority of the current study was recruited to exclude individuals with externalizing diagnoses in the absence of AUD; it is likely the current study has an underrepresentation of CUD/DUD without co-occurring alcohol problems. However, research has indicated, especially in young adults, that problematic illicit substance use in the absence of at least low level problematic alcohol use is relatively rare (see Connor et al., 2014 for review). Fourthly, the current study is limited to cross-sectional data. Future work would do well to analyze the stability of these severity estimates over time and the predictive utility of such a general substance use spectrum conceptualization.
Lastly, research has indicated that a significant chi-square test, even with large sample sizes and adequate fit by other measures (e.g. RMSEA and TLI), can possibly indicate that parameter estimates may be inaccurate (Ropovik, 2015). However, the current models did not suffer from convergence problems, improbable parameter values, or negative variances, which add confidence to the presented results (Ropovik, 2015). Furthermore, modification indices were utilized as a post hoc diagnostic tool to test for any sources of extreme misfit, which would lead to concerns about the tested models. Modification indices of the general substance use spectrum model indicated that the greatest source of misfit came from minor residual associations between items from each drug class (i.e. alcohol tolerance with alcohol withdrawal etc). Modification indices of the five-factor correlated model did not suggest any large or systematic remaining residual associations.
4.2. Conclusion
In conclusion, the current study demonstrates the utility of conceptualizing problematic substance use across different substance classes as manifestations of a general substance use spectrum, not as interrelated substance specific constructs. Although, the current study does not posit that there are no important substance specific processes, results indicate that the general substance use spectrum may be of primary interest in relation to overall dysfunction at the clinical level. Furthermore, a general substance use spectrum provides a simpler model that serves to integrate information from all substances, including co-use of substances, to provide a more valid and detailed assessment of substance use problems. This has major implications for both research and clinical practices. Specifically, researchers should be explicit about whether there studies are meant to focus on a substance specific process or seeking to capture this general substance use continuum. In terms of clinical practice, clinicians should aim to integrate information across substances (including subthreshold symptoms) to consider an individual’s overall issues with substances, which appears to be the primary construct related to other forms of behavioral and cognitive dysfunction.
Supplementary Material
Highlights.
Problems with all substances are manifestations of a general substance dimension
All classes of substances are informative, but indicate different severity levels
Simultaneous co-use of substances was highly related to the general dimension
Associations with dysfunction were not differentially related to specific drug classes
Markedly different substance use patterns can indicate nearly identical severity
Financial support
This research was supported by National Institutes of Alcohol Abuse and Alcoholism grant [R01AA13650] and National Institute of Drug Abuse (NIDA) grant [R01DA017924] to Peter Finn and NIDA grant [T32 DA24628-10] to Allen Bailey.
Role of Funding Source: Nothing Declared
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
None
References
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR (text revision). American Journal of Psychiatry. [Google Scholar]
- American Psychological Association (APA). (2013). Diagnostic and statistical manual of mental disorders: DSM-V. DSM-V. [Google Scholar]
- Bailey AJ, Farmer EJ, & Finn PR (2019). Patterns of polysubstance use and simultaneous co-use in high risk young adults. Drug and Alcohol Dependence. 10.1016/j.drugalcdep.2019.107656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey AJ, & Finn PR (2019). Borderline Personality Disorder Symptom Comorbidity Within a High Externalizing Sample: Relationship to the Internalizing-Externalizing Dimensional Structure of Psychopathology. Journal of Personality Disorders. 10.1521/pedi_2019_33_415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker FB (2001). The Basics of Item Response Theory. ERIC Clearinghouse on Assessment and EBaker FB. (2001) The Basics of Item Response Theory. ERIC Clearinghouse on Assessment and Evaluation; [Google Scholar]
- Bentler PM, & Bonett DG (1980). Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin, 88(3), 588–606. 10.1037/0033-2909.88.3.588 [DOI] [Google Scholar]
- Bierut LJ, Dinwiddie SH, Begleiter H, Crowe RR, Hesselbrock V, Nurnberger JI, … & Reich T. (1998). Familial transmission of substance dependence: alcohol, marijuana, cocaine, and habitual smoking: a report from the Collaborative Study on the Genetics of Alcoholism. Archives of general psychiatry, 55(11), 982–988. [DOI] [PubMed] [Google Scholar]
- Bobova L, Finn PR, Rickert ME, & Lucas J (2009). Disinhibitory psychopathology and delay discounting in alcohol dependence: personality and cognitive correlates. Experimental and clinical psychopharmacology, 17(1), 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA (2015). Confirmatory factor analysis for applied research, 2nd ed Confirmatory factor analysis for applied research, 2nd ed. 10.1017/CBO9781107415324.004 [DOI] [Google Scholar]
- Brown Timothy.A. (2006). Confirmatory Factor Analysis for Applied Research. Methodology in the Social Sciences. 10.1198/tas.2008.s98 [DOI] [Google Scholar]
- Browne MW, & Cudeck R (1992). Alternative Ways of Assessing Model Fit. Sociological Methods & Research, 21(2), 230–258. 10.1177/0049124192021002005 [DOI] [Google Scholar]
- Bucholz KK, Hesselbrock VM, Shayka JJ, Nurnberger JI Jr, Schuckit MA, Schmidt I, & Reich T (1995). Reliability of individual diagnostic criterion items for psychoactive substance dependence and the impact on diagnosis. Journal of studies on alcohol, 56(5), 500–505. [DOI] [PubMed] [Google Scholar]
- Bucholz Kathleen K, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock VM, Nurnberger JI, … Schuckit MA. (1994). A new, semi-structured psychiatric interview for use in genetic linkage studies: a report on the reliability of the SSAGA. Journal of Studies on Alcohol, 55(2), 149–158. 10.15288/jsa.1994.55.149 [DOI] [PubMed] [Google Scholar]
- Carragher N, Krueger RF, Eaton NR, Markon KE, Keyes KM, Blanco C, … Hasin DS (2014). ADHD and the externalizing spectrum: Direct comparison of categorical, continuous, and hybrid models of liability in a nationally representative sample. Social Psychiatry and Psychiatric Epidemiology, 49(8), 1307–1317. 10.1007/s00127-013-0770-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor JP, Gullo MJ, Chan G, Young RM, Hall WD, & Feeney GF (2013). Polysubstance use in cannabis users referred for treatment: drug use profiles, psychiatric comorbidity and cannabis-related beliefs. Frontiers in psychiatry, 4, 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor JP, Gullo MJ, White A, & Kelly AB (2014). Polysubstance use: diagnostic challenges, patterns of use and health. Current opinion in psychiatry, 27(4), 269–275. [DOI] [PubMed] [Google Scholar]
- Chen FF, West SG, & Sousa KH (2006). A comparison of bifactor and second-order models of quality of life. Multivariate Behavioral Research, 41, 189–225. 10.1207/s15327906mbr4102_5 [DOI] [PubMed] [Google Scholar]
- Derringer J, Krueger RF, Dick DM, Agrawal A, Bucholz KK, Foroud T, … & Nurnberger JI Jr. (2013). Measurement invariance of DSM- IV alcohol, marijuana and cocaine dependence between community- sampled and clinically overselected studies. Addiction, 108(10), 1767–1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenck HJ, & Eysenck SBG (1975). Manual of the Eysenck Personality Questionnaire. Journal of Personality Assessment (Vol. 43). 10.1177/014662168000400106 [DOI] [Google Scholar]
- Feigelman W, Gorman BS, & Lee JA (1998). Binge drinkers, illicit drug users, and polydrug users: An epidemiological study of American collegians. Journal of Alcohol and Drug Education, 44(1), 47–69. [Google Scholar]
- Ferrando PJ, & Lorenzo-Seva U (2005). IRT-related factor analytic procedures for testing the equivalence of paper-and-pencil and Internet-administered questionnaires. Psychological Methods, 10(2), 193. [DOI] [PubMed] [Google Scholar]
- Finn PR, Gunn RL, & Gerst KR (2014). The Effects of a working memory load on delay discounting in those with externalizing psychopathology. Clinical Psychological Science, 3(2), 202–214. 10.1177/2167702614542279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finn PR, Rickert ME, Miller MA, Lucas J, Bogg T, Bobova L, & Cantrell H (2009). Reduced Cognitive Ability in Alcohol Dependence: Examining the Role of Covarying Externalizing Psychopathology. Journal of Abnormal Psychology, 118(1), 100–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW, Davies M, Borus J, … Rounsaville B (1995). The Structured Clinical Interview for DSM-III-R Personality Disorders (SCID-II). Part II: Multi-Site Test-Retest Reliability Study. Journal of Personality Disorders, 9(2), 92–104. 10.1521/pedi.1995.9.2.92 [DOI] [Google Scholar]
- Franco S, Olfson M, Wall MM, Wang S, Hoertel N, & Blanco C (2019). Shared and specific associations of substance use disorders on adverse outcomes: a national prospective study. Drug and alcohol dependence, 201, 212–219. [DOI] [PubMed] [Google Scholar]
- Gibbons RD, Alegria M, Markle S, Fuentes L, Zhang L, Carmona R, … & Baca- García E. Development of a computerized adaptive substance use disorder scale for screening and measurement: the CAT- SUD. Addiction. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gudin JA, Mogali S, Jones JD, & Comer SD (2013). Risks, management, and monitoring of combination opioid, benzodiazepines, and/or alcohol use. Postgraduate medicine, 125(4), 115–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedden SL, Martins SS, Malcolm RJ, Floyd L, Cavanaugh CE, & Latimer WW (2010). Patterns of illegal drug use among an adult alcohol dependent population: Results from the National Survey on Drug Use and Health. Drug and alcohol dependence, 106(2–3), 119–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbeck DM, Brecht ML, Lovinger K, Raihan A, Christou D, & Sheaff P (2013). Poly-drug and marijuana use among adults who primarily used methamphetamine. Journal of psychoactive drugs, 45(2), 132–140. [DOI] [PubMed] [Google Scholar]
- Hesselbrock M, Easton C, Bucholz KK, Schuckit M, & Hesselbrock V (1999). A validity study of the SSAGA--a comparison with the SCAN. Addiction (Abingdon, England), 94(9), 1361–1370. 10.1046/j.1360-0443.1999.94913618.x [DOI] [PubMed] [Google Scholar]
- ICD-10 World Health Organization. (1992). The ICD-10 Classification of Mental and Behavioural Disorders. International Classification, 10, 1–267. [DOI] [Google Scholar]
- Kline RB (2011). Principles and practice of structural equation modeling (3rd Ed.). New York: Guilford. [Google Scholar]
- Kotov R, Waszczuk MA, Krueger RF, Forbes MK, Watson D, Clark LA, … Zimmerman M (2017). The hierarchical taxonomy of psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126(4), 454–477. 10.1037/abn0000258 [DOI] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, Benning SD, & Kramer MD (2007). Linking antisocial behavior, substance use, and personality: An integrative quantitative model of the adult externalizing spectrum. Journal of Abnormal Psychology, 116(4), 645–666. 10.1037/0021-843X.116.4.645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Markon KE, Patrick CJ, & Iacono WG (2005). Externalizing psychopathology in adulthood: a dimensional-spectrum conceptualization and its implications for DSM-V. Journal of abnormal psychology, 114(4), 537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earleywine M, & Newcomb MD (1997). Concurrent versus simultaneous polydrug use: Prevalence, correlates, discriminant validity, and prospective effects on health outcomes. Experimental and clinical psychopharmacology, 5(4), 353. [DOI] [PubMed] [Google Scholar]
- Franco S, Olfson M, Wall MM, Wang S, Hoertel N, & Blanco C (2019). Shared and specific associations of substance use disorders on adverse outcomes: a national prospective study. Drug and alcohol dependence, 201, 212–219. [DOI] [PubMed] [Google Scholar]
- McCabe SE, West BT, Jutkiewicz EM, & Boyd CJ (2017). Multiple DSM- 5 substance use disorders: A national study of US adults. Human Psychopharmacology: Clinical and Experimental, 32(5), e2625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moustaki I, Jöreskog KG, & Mavridis D (2004). Factor models for ordinal variables with covariate effects on the manifest and latent variables: A comparison of LISREL and IRT approaches. Structural Equation Modeling, 11(4), 487–513. [Google Scholar]
- Olthuis JV, Darredeau C, & Barrett SP (2013). Substance use initiation: the role of simultaneous polysubstance use. Drug and alcohol review, 32(1), 67–71. [DOI] [PubMed] [Google Scholar]
- Petry NM (2001). A behavioral economic analysis of polydrug abuse in alcoholics: asymmetrical substitution of alcohol and cocaine. Drug and alcohol dependence, 62(1), 31–39. [DOI] [PubMed] [Google Scholar]
- Quek LH, Chan GC, White A, Connor JP, Baker P, Saunders JB, & Kelly AB (2013). Concurrent and simultaneous polydrug use: latent class analysis of an Australian nationally representative sample of young adults. Frontiers in public health, 1, 61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Development Core Team. (2013). R: A language and environment for statistical computing R Foundation for Statistical Computing, Vienna, Austria: URL; http://www.R-project.org/R Foundation for Statistical Computing, Vienna, Austria. [Google Scholar]
- Reise SP, Morizot J, & Hays RD (2007). The role of the bifactor model in resolving dimensionality issues in health outcomes measures. Quality of Life Research, 16(Suppl. 1), 19–31. 10.1007/s11136-007-9183-7 [DOI] [PubMed] [Google Scholar]
- Reise SP, Widaman KF, & Pugh RH (1993). Confirmatory factor analysis and item response theory: two approaches for exploring measurement invariance. Psychological bulletin, 114(3), 552. [DOI] [PubMed] [Google Scholar]
- Ropovik I (2015). A cautionary note on testing latent variable models. Frontiers in psychology, 6, 1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosseel Y (2012). lavaan: An R Package for Structural Equation Modeling. Journal of Statistical Software, 48(2), 1–36. 10.18637/jss.v048.i02 [DOI] [Google Scholar]
- Skrondal A, & Rabe-Hesketh S (2004). Generalized latent variable modeling: Multilevel, longitudinal, and structural equation models. Generalized Latent Variable Modeling: Multilevel, Longitudinal, and Structural Equation Models. [Google Scholar]
- Slade T, & Watson D (2006). The structure of common DSM-IV and ICD-10 mental disorders in the Australian general population. Psychological Medicine, 36(11), 1593–1600. 10.1017/S0033291706008452 [DOI] [PubMed] [Google Scholar]
- Slutske WS (2005). Alcohol Use Disorders Among US College Students and Their Non–College-Attending Peers. Archives of General Psychiatry, 62(3), 321 10.1001/archpsyc.62.3.321 [DOI] [PubMed] [Google Scholar]
- Spielberger CD (1983). Manual for the State-Trait Anxiety Inventory (STAI Form Y). Consulting Psychologists Palo Alto. 10.1002/9780470479216.corpsy0943 [DOI] [Google Scholar]
- Stekhoven DJ, & Bühlmann. (2011). MissForest—non-parametric missing value imputation for mixed-type data. Bioinformatics, 28(1), 112–118. [DOI] [PubMed] [Google Scholar]
- Sunderland M, Slade T, & Krueger RF (2015). Examining the shared and unique relationships among substance use and mental disorders. Psychological medicine, 45(5), 1103–1113. [DOI] [PubMed] [Google Scholar]
- Van Buuren S (2018). Flexible imputation of missing data. CRC press. [Google Scholar]
- Vollebergh WAM, Iedema J, Bijl RV, de Graaf R, Smit F, & Ormel J (2001). The structure and stability of common mental disorders: The nemesis study. Archives of General Psychiatry, 58(6), 597–603. https://doi.org/yoa20186 [pii] [DOI] [PubMed] [Google Scholar]
- Waljee AK, Mukherjee A, Singal AG, Zhang Y, Warren J, Balis U, … & Higgins PD. (2013). Comparison of imputation methods for missing laboratory data in medicine. BMJ open, 3(8), e002847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. (1999). Manual for the Wechsler abbreviated intelligence scale (WASI). WASI [Google Scholar]
- White A, & Hingson R. (2013). The burden of alcohol use: excessive alcohol consumption and related consequences among college students. Alcohol research: current reviews. [PMC free article] [PubMed] [Google Scholar]
- Wickham H (2016). ggplot2 - Elegant Graphics for Data Analysis. In Journal of Statistical Software. 10.18637/jss.v077.b02 [DOI] [Google Scholar]
- Witkiewitz K, King K, McMahon RJ, Wu J, Luk J, Bierman KL, … Pinderhughes EE (2013). Evidence for a multi-dimensional latent structural model of externalizing disorders. Journal of Abnormal Child Psychology, 41(2), 223–237. 10.1007/s10802-012-9674-z [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


