Abstract
Backgrounds
The role of right ventricular (RV) and atrial (RA) structure and function, in the increased heart failure risk in (pre)diabetes is incompletely understood. The purpose of this study is to investigate the associations between (pre)diabetes and RV and RA structure and function, and whether these are mediated by left ventricular (LV) alterations or pulmonary pressure.
Methods
Participants of the Maastricht Study; a population-based cohort study (426 normal glucose metabolism (NGM), 142 prediabetes, 224 diabetes), underwent two-dimensional and tissue Doppler echocardiography. Multiple linear regression analyses with pairwise comparisons of (pre)diabetes versus NGM, adjusted for cardiovascular risk factors, and mediation analyses were used.
Results
In general, differences were small. Nevertheless, in individuals with prediabetes and diabetes compared to NGM; RA volume index was lower (both p < 0.01, ptrend < 0.01), RV diameter was lower (both p < 0.01, ptrend < 0.01) and RV length was significantly smaller in diabetes (p = 0.67 and p = 0.03 respectively, ptrend = 0.04), TDI S′RV was lower (p = 0.08 and p < 0.01 respectively, ptrend < 0.01), TDI E′RV was lower (p = 0.01 and p = 0.02 respectively, ptrend = 0.01) and TDI A′RV was lower (p < 0.01 and p = 0.07 respectively, ptrend = 0.04). Only the differences in RA volume index (7.8%) and RV diameter (6.2%) were mediated by the maximum tricuspid gradient, but no other LV structure and function measurements.
Conclusions
(Pre)diabetes is associated with structural RA and RV changes, and impaired RV systolic and diastolic function, independent of cardiovascular risk factors. These associations were largely not mediated by indices of LV structure, LV function or pulmonary pressure. This suggests that (pre)diabetes affects RA and RV structure and function due to direct myocardial involvement.
Keywords: Heart failure, Echocardiography, Right atrial and ventricular structure, Right ventricular function, (pre)diabetes
Background
The role of right ventricular (RV) structure and function in the increased risk of heart failure in patients with type 2 diabetes (T2DM) [1] and prediabetes [2] is incompletely understood [3–5] but may be important. Indeed, in a population free of overt cardiovascular disease [6], Kawut et al. showed that RV (independent of left ventricular (LV)) mass was associated with increased risk of heart failure. In another study [7], in heart failure patients, RV function was a stronger predictor of mortality than LV function.
In (pre)diabetes, parallel effects on RV and LV structure and function may occur through direct myocardial effects (e.g. fibrosis, oxidative stress, altered calcium homeostasis and substrate metabolism) [8–10]; through indirect effects via alterations in vascular function (e.g. arterial stiffening and microvascular dysfunction) [11]; and (or) through ventricular interdependence (i.e. structure, compliance, and function of the one ventricle, through direct mechanical interaction via septal wall and pericardium, may affect structure and function of the other ventricle) [3–5].
Associations of (pre)diabetes with RV structure and function have not been systematically investigated [9, 11–27]. Previous studies in general have been performed in selected and small populations (with type 1 diabetes [12, 14, 17, 25], in outpatient clinics [9, 12–17, 21–23, 25–27], with heart failure [24], with pulmonary hypertension [11], and (or) with less than 150 participants [12, 14–18, 20, 22, 24–27]), have not been adjusted for potential confounders [12, 14–17, 20, 22, 23, 25, 26], and have not investigated the role of prediabetes [11, 12, 14–18, 20–26]. In the population-based MESA study [19], (pre)diabetes was associated with lower RV mass and smaller RV volume, but not with RV systolic function, while RV diastolic function was not assessed.
In view of these considerations, we assessed associations between (pre)diabetes and RV and LV structure and function in the population-based Maastricht Study. In addition, we tested the hypothesis that RV alterations in (pre)diabetes are mediated by LV alterations and (or) pulmonary pressure.
Methods
Study population
We used data from The Maastricht Study, an observational prospective population-based cohort study. The rationale and methodology have been described previously [28]. In brief, the study focuses on the etiology, pathophysiology, complications and comorbidities of T2DM and is characterized by an extensive phenotyping approach. Eligible for participation were all individuals aged between 40 and 75 years and living in the southern part of the Netherlands. Participants were recruited through mass media campaigns and from the municipal registries and the regional Diabetes Patient Registry via mailings. Recruitment was stratified according to known T2DM status, with an oversampling of individuals with T2DM, for reasons of efficiency. The present report includes cross-sectional data from the first 866 participants, who completed the baseline survey between November 2010 and March 2012. To augment statistical power, another random sample of 218 participants was added, who had completed the baseline survey between April 2012 and April 2013. The examinations of each participant were performed within a time window of three months. Patients with type 1 diabetes mellitus or a paced heart rhythm were excluded. The study has been approved by the institutional medical ethical committee (NL31329.068.10) and the Minister of Health, Welfare and Sports of the Netherlands (Permit 131088-105234-PG). All participants gave written informed consent.
Glucose metabolism status
To determine glucose metabolism status, all participants (except those who used insulin) underwent a standardized 2-h 75 g oral glucose tolerance test after an overnight fast. For safety reasons, participants with a fasting glucose level above 11.0 mmol/L, as determined by a finger prick, did not undergo the oral glucose tolerance test. For these individuals, fasting glucose level and information about diabetes medication were used to determine glucose metabolism status. Glucose metabolism status was defined according to the WHO 2006 criteria into normal glucose metabolism (NGM), impaired fasting glucose, impaired glucose tolerance (combined as prediabetes), and T2DM [29].
Echocardiography
Echocardiograms were obtained according to a standardized protocol consisting of two-dimensional, M-mode, color flow Doppler, pulsed and continuous wave Doppler and Tissue Doppler recordings (TDI) with use of echo equipment (Vivid E9 with 2.5-3.5 MHz and 4 V transducer, GE Vingmed). All recordings were digitally stored and analyzed off-line (EchoPAC PC, version 112) by four researchers blinded to (pre)diabetes status. Details on echocardiographical procedures are provided in Additional file 1.
Covariates
Office blood pressure (Omron 705IT, Omron, Japan) and ambulatory 24 h blood pressure (WatchBP O3, Microlife AG, Switzerland) were measured as described elsewhere [28]. Fasting serum concentrations of total cholesterol, high density lipoprotein (HDL) cholesterol, triglycerides and creatinine were measured (Beckman Synchron LX20, Beckman Coulter inc., Brea USA) [28]. Cystatin C was measured by a particle enhanced immunoturbidimetric assay (Roche Cobas 8000, Roche diagnostics, Basel, Switzerland). Estimated glomerular filtration rate (eGFR) was estimated according to the Chronic Kidney Disease Epidemiology Collaboration equation based on both serum creatinine and serum cystatin C [30]. Albuminuria, defined as an urinary albumin excretion ≥ 30 mg/24 h, was determined (twice) as described elsewhere [31]. Antihypertensive, lipid-modifying, and glucose-lowering medication use were assessed with a medication interview [28]. Renin-angiotensin system modifying agents were defined angiotensin converting enzyme inhibitors, angiotensin II inhibitors and (or) renin inhibitors use. Waist circumference was measured midway between the lower rib margin and the iliac crest end-expiratory. Alcohol consumption, smoking status (never, former, current), prevalent cardiovascular disease and physical activity were determined by questionnaire [28]. Alcohol consumption was categorized into non-consumers, low-consumers (≤ 7 and ≤ 14 glasses per week for females and males respectively) and high-consumers (> 7 and > 14 glasses per week for females and males respectively). Total and moderate to vigorous physical activity was assessed by a modified version of the Community Healthy Activities Model Program for Seniors (CHAMPS) questionnaire [32]. Prevalent cardiovascular disease was defined as a self-reported history of myocardial infarction, or cerebrovascular infarction or hemorrhage, or percutaneous artery angioplasty of, or vascular surgery of the coronary, abdominal, peripheral or carotid arteries. Other clinical characteristics (i.e. body mass index, waist-to-hip ratio, presence of hypertension, and HbA1c) were obtained from physical examination and laboratory assessment as described elsewhere [28].
Statistical analyses
All analyses were performed with the statistical software package SPSS version 21.0 (SPSS IBM Corporation, Armonk, NY, USA). Descriptive statistics are presented as mean (± standard deviation), or in case of a skewed distribution as median [interquartile range] or frequencies (percentages). Variables with a skewed distribution were natural-log-transformed in order to meet normality criteria. Comparisons of population characteristics between groups were made by use of independent T-test or Chi squared test as appropriate. Dependent variables were standardized into sex specific Z-scores (individual value-meansex)/(standard deviationsex). As sex had a skewed distribution in categories of glucose metabolism status, sex-specific means and standard deviations of the NGM group were used. Multiple linear regression analyses, both linear trend analyses and pairwise comparisons of prediabetes or T2DM versus NGM respectively (with dummy variables), were used to determine associations of (pre)diabetes with RA volume index, RV structure (i.e. RV diameter, RV length), and RV functions (i.e. TDI S’RV, TDI E’RV, TDI A’RV, TDI E′/A′ratio, RV myocardial performance index). Model 1 was adjusted for age; model 2 was additionally adjusted for cardiovascular risk factors associated with RV structure and functioning [19, 33] (i.e. systolic blood pressure, antihypertensive medication use, smoking status, prior cardiovascular disease, and waist circumference); and model 3 was additionally adjusted for albuminuria, eGFR, total to high density lipoprotein cholesterol ratio, triglycerides, and the use of lipid-modifying medication. Mediation analyses was performed to assess the extent to which ventricular interdependence and pulmonary hypertension statistically mediated the association between (pre)diabetes and RV structure and function. Hence, we added these factors (i.e. LV mass index, peak flow velocity E/longitudinal velocities E ratio, LV ejection fraction, maximum gradient of the tricuspid valve) to the aforementioned regression models. Both independent and joint mediation effects were expressed as the (relative) change of the regression coefficient. The corresponding 95% confidence intervals were assessed according to Preacher and Hayes (10,000 bootstrap iterations) [34]. Multicollinearity was assessed by collinearity diagnostics (i.e. tolerance < 0.1 and/or variance inflation factor > 10). A two-sided P-value < 0.05 was considered statistically significant, except for interaction analyses, where P < 0.10 was used.
Results
Study population
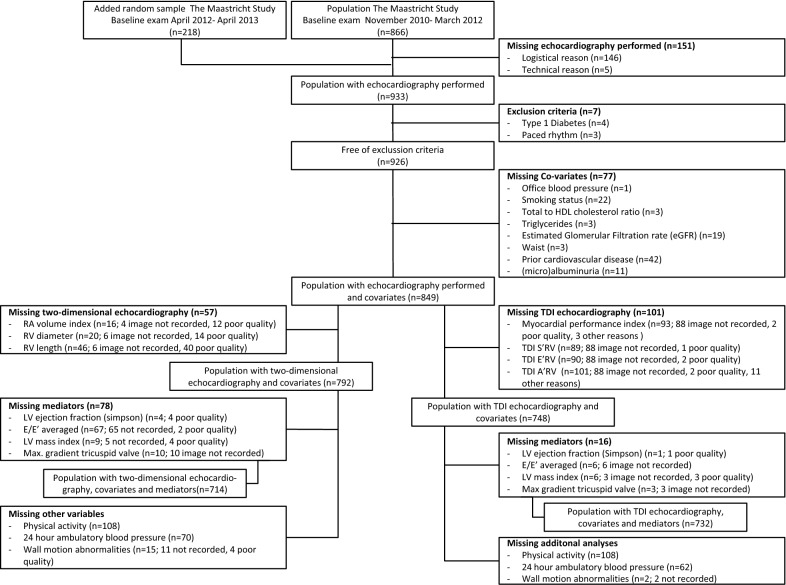
Of the 1084 participants, echocardiography was obtained in 933 individuals. Participants were excluded due to exclusion criteria (n = 7), missing covariates (n = 72), and missing two-dimensional (n = 57) or TDI (n = 101) echocardiographic analyses, resulting in 792 and 748 participants eligible for current analyses respectively (Fig. 1). Individuals with missing data more frequently had T2DM; however, within strata of (pre)diabetes, these individuals were largely comparable (Additional file 2: Table S1).
Fig. 1.
Selection of study population. HDL high density lipoprotein, RA right atrium, RV right ventricle, 2D two-dimensional, LV left ventricle, TDI tissue Doppler imaging
Characteristics
Characteristics of the total study population and stratified according to (pre)diabetes are given in Tables 1, 2 and Additional file 2: Table S2. Participants with (pre)diabetes had a worse cardiovascular risk profile; they were older and more often men, had a higher body mass index, greater waist circumference, higher blood pressure, lower HDL, higher triglycerides, lower eGFR, and less physical activity. They also more frequently had prior cardiovascular disease, hypertension and albuminuria, and more often used antihypertensive and lipid-modifying medication (Table 1, Additional file 2: Table S2).
Table 1.
Clinical characteristics of the study population with two-dimensional echocardiography according to glucose metabolism status (n = 792)
| Variable | NGM (n = 426) | Prediabetes (n = 142) | T2DM (n = 224) |
|---|---|---|---|
| Demographics | |||
| Age, years | 57.3 ± 8.0 | 62.5 ± 7.5‡ | 62.6 ± 7.6‡ |
| Women, % | 233 (54.7) | 57 (40.1)‡ | 71 (31.7)‡ |
| Measures of (central) obesity | |||
| Body mass index, kg/m2 | 25.5 [23.2–27.8] | 27.4 [25.6–29.8]‡ | 29.3 [26.2–32.2]‡ |
| Waist circumference, cm | |||
| Men | 96 [91–103] | 102 [96–110]‡ | 106 [99–113]‡ |
| Women | 87 [79–94] | 94 [85–100]‡ | 101 [91–113]‡ |
| Waist-to hip ratioa | 0.91 ± 0.08 | 0.97 ± 0.08‡ | 1.01 ± 0.08‡ |
| Blood pressure | |||
| Office systolic blood pressure, mmHg | 131.1 ± 16.5 | 140.0 ± 17.2‡ | 145.0 ± 18.3‡ |
| Office diastolic blood pressure, mmHg | 75.2 ± 9.7 | 79.3 ± 10.3‡ | 78.0 ± 9.3‡ |
| 24 h average ambulatory systolic blood pressure, mmHgb | 116.3 ± 10.6 | 121.6 ± 12.8‡ | 122.1 ± 11.5‡ |
| 24 h average ambulatory diastolic blood pressure, mmHgb | 73.6 ± 7.0 | 74.8 ± 8.0 | 73.4 ± 7.1 |
| Hypertension, % | 169 (39.7) | 98 (69.0)‡ | 187 (83.5)‡ |
| Glucose metabolism | |||
| Fasting glucose, mmol/L | 5.2 ± 0.4 | 6.0 ± 0.5** | 7.9 ± 2.3** |
| 2 h postload glucose, mmol/Lc | 5.3 ± 1.2 | 8.2 ± 1.8** | 14.0 ± 3.4** |
| HbA1c, mmol/mold | 37.1 ± 3.5 | 40.4 ± 4.2** | 51.7 ± 11.2** |
| HbA1c, %d | 5.5 ± 0.3 | 5.8 ± 0.4** | 6.9 ± 1.0** |
| Lipids | |||
| Total cholesterol, mmol/L | 5.6 ± 1.0 | 5.5 ± 1.2 | 4.5 ± 1.0‡ |
| HDL cholesterol, mmol/L | |||
| Men | 1.3 ± 0.3 | 1.2 ± 0.3 | 1.1 ± 0.3‡ |
| Women | 1.7 ± 0.5 | 1.6 ± 0.4 | 1.4 ± 0.4‡ |
| Total to HDL cholesterol ratio | 4.0 ± 1.3 | 4.3 ± 1.3* | 4.0 ± 1.1 |
| LDL cholesterol, mmol/l | 3.6 ± 0.9 | 3.4 ± 1.0 | 2.5 ± 0.9‡ |
| Triglycerides, mmol/l | 1.0 [0.8–1.5] | 1.4 [0.9–1.9]‡ | 1.7 [1.2–2.3]‡ |
| Kidney function | |||
| eGFR, ml/min/1.73 m2 | 90.8 ± 13.8 | 85.0 ± 14.4‡ | 85.2 ± 17.2‡ |
| Albuminuria, % | 15 (3.5) | 10 (7.0)* | 38 (17.0)‡ |
| Lifestyle | |||
| Smoking (never, former, current), % | 153/198/75 (35.9/46.5/17.6) | 41/85/16 (28.9/59.9/11.3)* | 59/128/37 (26.3/57.1/16.5)† |
| Alcohol consumption (none, low, high), %e | 52/226/145 (12.3/53.4/34.3) | 21/70/51 (14.8/49.3/35.9) | 66/109/48 (29.6/48.9/21.5)‡ |
| Moderate to vigorous physical activity, h/wkf | 5.3 [3.0–8.5] | 4.5 [2.0–6.8]‡ | 3.8 [1.6–6.5]‡ |
| Prior cardiovascular disease, % | 44 (10.3) | 23 (16.2)* | 56 (25.0)‡ |
| Medication | |||
| Antihypertensive medication use, % | 97 (22.8) | 68 (47.9)‡ | 154 (68.8)‡ |
| Ras inhibitors, % | 64 (15.0) | 49 (34.5)‡ | 124 (55.4)‡ |
| Beta-blockers, % | 36 (8.5) | 32 (22.5)‡ | 81 (36.2)‡ |
| Diuretics, % | 29 (6.8) | 29 (20.4)‡ | 60 (26.8)‡ |
| Calcium antagonists, % | 15 (3.5) | 11 (7.7)† | 35 (15.6)‡ |
| Diabetes medication use, % | – | – | 166 (74.1)** |
| Insulin, % | – | – | 40 (17.9)** |
| Metformin, % | – | – | 151 (67.4)** |
| Sulfonylureas, % | – | – | 41 (18.3)** |
| Thiazolidinediones, % | – | – | 2 (0.9)** |
| GLP-1 analogs, % | – | – | 2 (0.9)** |
| DPP-4 inhibitors, % | – | – | 5 (2.2)** |
| Lipid modifying medication use, % | 68 (16.0) | 54 (38.0)‡ | 166 (74.1)‡ |
Data are presented as n (%), mean ± standard deviation or median (interquartile rage)
NGM normal glucose metabolism, T2DM type 2 diabetes, HDL high density lipoprotein, LDL low density lipoprotein, eGFR estimated glomerular filtration rate, Ras renin-angiotensin system, GLP-1 glucagon-like peptide-1, DPP-4 dipeptidyl peptidase-4
Numbers of missing data: a n = 1, b n = 70, c n = 52, d n = 3, e n = 4, f n = 108
P value difference prediabetes or T2DM vs NGM: * < 0.10, † < 0.05, ‡ < 0.01, ** not applicable
Table 2.
Echocardiographic characteristics of the study population according to glucose metabolism status
| Variable | NGM (n = 426) | Prediabetes (n = 142) | T2DM (n = 224) | |||
|---|---|---|---|---|---|---|
| Left atrium | ||||||
| LA volume index, ml/m2 | ||||||
| Men | 30.8 [26.6–34.9] | 28.9 [25.0–34.7] | 29.7 [25.2–34.5] | |||
| Women | 28.6 [24.7–33.3] | 28.6 [25.3–33.2] | 26.3 [23.2–32.4] | |||
| LA volume, ml | ||||||
| Men | 62.0 [53.3–72.4] | 62.3 [50.9–72.9] | 61.1 [52.4–72.0] | |||
| Women | 50.9 [43.6–59.2] | 52.9 [43.6–59.2] | 51.3 [42.3–59.6] | |||
| Left ventricle, structure | ||||||
| LV end diastolic volume index, ml/m2 | ||||||
| Men | 68.5 ± 12.5 | 65.9 ± 11.8 | 63.0 ± 12.3‡ | |||
| Women | 59.1 ± 10.6 | 58.1 ± 11.3 | 57.6 ± 11.9 | |||
| LV end systolic volume index, ml/m2 | ||||||
| Men | 27.5 ± 6.1 | 26.7 ± 6.2 | 25.9 ± 6.3† | |||
| Women | 23.2 ± 4.6 | 23.0 ± 5.0 | 22.8 ± 5.3 | |||
| LV mass index, gr/m2.7 | ||||||
| Men | 29.5 [25.3–35.1] | 31.5 [27.4–35.0] | 32.8 [27.0–37.5]‡ | |||
| Women | 27.3 [24.0–31.3] | 31.1 [25.5–36.7]‡ | 31.2 [27.1–34.7]‡ | |||
| Left ventricular function | ||||||
| Systolic LV function | ||||||
| LV ejection fraction, % | 60.5 [58.8–62.4] | 60.4 [58.8–62.0] | 60.2 [57.8–61.7]‡ | |||
| TDI S’ septal (cm/s)a | 7.5 ± 1.4 | 7.3 ± 1.3 | 7.4 ± 1.7 | |||
| TDI S’ lateral (cm/s)b | 8.8 ± 2.0 | 8.8 ± 2.1 | 8.2 ± 2.0‡ | |||
| Diastolic LV function | ||||||
| Early peak velocity (m/s) | 0.68 ± 0.15 | 0.66 ± 0.14 | 0.68 ± 0.15 | |||
| Active peak velocity (m/s)c | 0.66 ± 0.15 | 0.72 ± 0.17‡ | 0.75 ± 0.16‡ | |||
| E/A ratioc | 1.03 [0.85–1.26] | 0.89 [0.75–1.08]‡ | 0.89 [0.77–1.07]‡ | |||
| Deceleration time E-peak (msec) | 191 ± 35 | 204 ± 38‡ | 202 ± 37‡ | |||
| Isovolumetric relaxation time (msec)d | 94 ± 21 | 100 ± 24‡ | 94 ± 22 | |||
| S/D ratioe | 1.38 ± 0.32 | 1.45 ± 0.36† | 1.46 ± 0.31‡ | |||
| TDI E’ septal (cm/s)b | 8.3 | ± 2.2 | 7.1 | ± 1.7‡ | 7.1 | ± 1.8‡ |
| TDI A’ septal (cm/s)f | 9.8 ± 1.8 | 9.8 ± 1.7 | 10.0 ± 1.9 | |||
| TDI E’ lateral (cm/s)g | 10.7 ± 2.7 | 9.5 ± 2.5‡ | 8.9 ± 2.2‡ | |||
| TDI A’ lateral (cm/s)h | 10.6 ± 2.5 | 11.1 ± 2.4† | 11.1 ± 2.3† | |||
| E/E’-ratio averagedi | 7.3 [6.2–8.7] | 8.0 [6.9–9.7]‡ | 8.7 [7.6–10.1]‡ | |||
| Diastolic LV function (normal, indeterminate, abnormal, not specified), n (%) | 175/183/42/26 (41.1/43.0/9.9/6.1) | 30/79/23/10 (21.1/55.6/16.2/7.0)‡ | 44/115/40/25 (19.6/51.3/17.9/11.2)‡ | |||
| Right atrium | ||||||
| RA volume index, ml/m2 | ||||||
| Men | 25.2 ± 7.2 | 22.1 ± 6.8‡ | 21.7 ± 6.2‡ | |||
| Women | 21.3 ± 6.0 | 19.7 ± 5.5 | 18.3 ± 5.3‡ | |||
| RA volume, ml | ||||||
| Men | 48.1 [40.0–58.8] | 43.4 [35.3–54.8]‡ | 43.7 [36.7–51.9]‡ | |||
| Women | 36.0 29.7–45.1 | 36.0 [28.6–40.7] | 33.7 [28.0–40.2]† | |||
| Right ventricle, structure | ||||||
| RV diameter | ||||||
| Men | 41.3 ± 5.2 | 39.9 ± 5.3† | 39.8 ± 4.7‡ | |||
| Women | 35.6 ± 4.7 | 35.8 ± 5.6 | 35.0 ± 4.2 | |||
| RV length | ||||||
| Men | 75.8 ± 7.5 | 75.8 ± 7.0 | 75.9 ± 7.2 | |||
| Women | 69.8 ± 6.6 | 70.3 ± 6.2 | 70.2 ± 7.3 | |||
| Right ventricular function | ||||||
| Systolic RV function | ||||||
| S’ RV (cm/s)j | 12.8 ± 2.4 | 12.4 ± 2.2 | 12.4 ± 2.5 | |||
| TAPSE (mm)k | 23.0 ± 2.9 | 22.0 ± 3.6 | 22.3 ± 4.4 | |||
| Diastolic RV function | ||||||
| E-peak velocity tricuspid flow (m/s)l | 0.46 ± 0.09 | 0.44 ± 0.09 | 0.44 ± 0.08 | |||
| A-peak velocity tricuspid flow (m/s)m | 0.35 ± 0.10 | 0.41 ± 0.07† | 0.41 ± 0.09‡ | |||
| E/A ratio tricuspid valvem | 1.30 [1.12–1.58] | 1.10 [0.91–1.22]‡ | 1.10 [0.90–1.26]‡ | |||
| TDI E’ RV (cm/s)n | 11.9 ± 2.7 | 10.4 ± 2.7‡ | 10.5 ± 2.7‡ | |||
| TDI A’ RV (cm/s)o | 14.6 ± 3.5 | 13.9 ± 3.1† | 14.1 ± 3.4 | |||
| E/E′-ratiok | 4.3 [3.6–5.0] | 4.8 [4.1–5.7] | 4.6 [3.4–5.9] | |||
| Global RV function | ||||||
| Myocardial performance index RVp | 0.47 ± 0.12 | 0.47 ± 0.12 | 0.48 ± 0.11 | |||
| Maximum tricuspid gradient | 15.8 ± 6.2 | 14.7 ± 7.6 | 14.9 ± 7.2 | |||
| Wall motion abnormalities, n yes (%)q | 2 (0.5) | 2 (1.4) | 5 (2.3)† | |||
| Valvular dysfunction (moderate or severe), n (%) | 28 (6.6) | 8 (5.6) | 13 (5.8) | |||
Data are presented as n (%), mean ± standard deviation or median (interquartile range)
LA left atrial, LV left ventricular, TDI tissue Doppler imaging, RA right atrial, tricuspid annular plane systolic excursion, RV right ventricular
Numbers of missing data (if n > 10); a n = 62; b n = 63; c n = 14; d n = 26; e n = 22; f n = 72; g n = 64; h n = 73; i n = 67; j n = 70; k n = 645; l n = 644; m n = 647; n n = 71; o n = 80; p n = 74; q n = 15
P value difference prediabetes or T2DM vs NGM: * < 0.10, † < 0.05, ‡ < 0.01
Participants with (pre)diabetes had lower LV end diastolic volume index, higher LVMI, worse LV systolic function, and worse LV diastolic function (lower E/A ratio, higher E/E′-ratio averaged, more frequent abnormal diastolic function grade). In addition, they had lower RA volumes, worse RV systolic function, and worse RV diastolic function (lower E/A ratio of the tricuspid valve, lower E′RV). Participants with (pre)diabetes more often had wall motion abnormalities (Table 2).
Associations between (pre)diabetes and RA and RV structure and function
RA volume index was lower in individuals with prediabetes and T2DM compared to NGM (p < 0.01 and p < 0.01 respectively, p for trend < 0.01; Table 3). Adjustment for potential confounders of models 2 and 3 attenuated the difference in RA volume index, although the association remained statistically significant (p < 0.01 and p < 0.01 respectively, p for trend < 0.01).
Table 3.
Multivariable adjusted differences of right ventricle structure and function between individuals with (pre)diabetes, as compared to individuals with normal glucose metabolism
| Variable | Model | NGM | Prediabetes | T2DM | P for trend |
|---|---|---|---|---|---|
| B (95% CI) | B (95% CI) | ||||
| Right atrium | |||||
| RA volume index (SD)a | 1 | Ref | − 0.39 (− 0.58; − 0.21)‡ | − 0.52 (− 0.68; − 0.36)‡ | < 0.01 |
| 2 | Ref | − 0.32 (− 0.51; − 0.13)‡ | − 0.39 (− 0.57; − 0.21)‡ | < 0.01 | |
| 3 | Ref | − 0.26 (− 0.45; − 0.07)‡ | − 0.29 (− 0.48; − 0.09)‡ | < 0.01 | |
| Right ventricle, structure | |||||
| RV diameter (SD)a | 1 | Ref | − 0.12 (− 0.31; 0.08) | − 0.20 (− 0.37; − 0.04)† | 0.02 |
| 2 | Ref | − 0.29 (− 0.49; − 0.09)‡ | − 0.49 (− 0.68; − 0.30)‡ | < 0.01 | |
| 3 | Ref | − 0.27 (− 0.47; − 0.07)‡ | − 0.44 (− 0.65; − 0.24)‡ | < 0.01 | |
| RV length (SD)a | 1 | Ref | 0.15 (− 0.04; 0.34) | 0.15 (− 0.01; 0.32) * | 0.06 |
| 2 | Ref | − 0.02 (− 0.22; 0.17) | − 0.15 (− 0.33; 0.04) | 0.13 | |
| 3 | Ref | − 0.04 (− 0.24; 0.15) | − 0.22 (− 0.42; − 0.02)† | 0.04 | |
| Systolic RV function | |||||
| S’ RV (SD)b | 1 | Ref | − 0.18 (− 0.37; 0.02) * | − 0.26 (− 0.44; − 0.09)‡ | < 0.01 |
| 2 | Ref | − 0.21 (− 0.41; 0.00)† | − 0.30 (− 0.50; − 0.10)‡ | < 0.01 | |
| 3 | Ref | − 0.19 (− 0.39; 0.02) * | − 0.29 (− 0.51; − 0.07)‡ | 0.01 | |
| Diastolic RV function | |||||
| TDI E’ RV (SD)b | 1 | Ref | − 0.31 (− 0.50; − 0.11)‡ | − 0.36 (− 0.53; − 0.18)‡ | < 0.01 |
| 2 | Ref | − 0.30 (− 0.50; − 0.10)‡ | − 0.31 (− 0.51; − 0.11)‡ | < 0.01 | |
| 3 | Ref | − 0.26 (− 0.47; − 0.06)† | − 0.26 (− 0.48; − 0.05)† | 0.01 | |
| TDI A’ RV (SD)b | 1 | Ref | − 0.32 (− 0.51; − 0.13)‡ | − 0.29 (− 0.46; − 0.12)‡ | < 0.01 |
| 2 | Ref | − 0.29 (− 0.49; − 0.10)‡ | − 0.23 (− 0.42; − 0.10)‡ | 0.01 | |
| 3 | Ref | − 0.26 (− 0.46; − 0.07)‡ | − 0.20 (− 0.41; 0.01) * | 0.04 | |
| TDI E′/A′ ratio (SD)b | 1 | Ref | − 0.02 (− 0.19; 0.15) | − 0.07 (− 0.22; 0.08) | 0.39 |
| 2 | Ref | − 0.03 (− 0.20; 0.15) | − 0.08 (− 0.25; 0.09) | 0.35 | |
| 3 | Ref | − 0.02 (− 0.19; 0.16) | − 0.07 (− 0.25; 0.12) | 0.50 | |
| Global RV function | |||||
| Myocardial performance index RV (SD)b | 1 | Ref | − 0.04 (− 0.23; 0.16) | − 0.04 (− 0.21; 0.13) | 0.63 |
| 2 | Ref | − 0.06 (− 0.26; 0.15) | − 0.09 (− 0.29; 0.12) | 0.40 | |
| 3 | Ref | − 0.10 (− 0.31; 0.11) | − 0.17 (− 0.39; 0.05) | 0.12 | |
Model 1: adjusted for age. Model 2: adjusted for model 1 + office systolic blood pressure, antihypertensive medication, smoking status, prior cardiovascular disease, waist circumference. Model 3: adjusted for model 2 + albuminuria, eGFR, total to high density lipoprotein cholesterol ratio, triglycerides, the use of lipid-modifying medication
CI confidence interval, NGM normal glucose metabolism, RA right atrial, RV right ventricular, SD standard deviation, T2DM type 2 diabetes mellitus, TDI tissue Doppler imaging
Study population a n = 792, b n = 748
P value difference prediabetes or T2DM vs NGM: * < 0.10, † < 0.05,‡ < 0.01
RV diameter was lower in individuals with prediabetes and T2DM compared to NGM (p = 0.24 and p = 0.02 respectively, p for trend 0.02; Table 3). Adjustment for potential confounders of models 2 and 3 strengthened the difference in RV diameter (p < 0.01 and p < 0.01 respectively, p for trend < 0.01). RV length was not significantly different in individuals with prediabetes and T2DM compared to NGM (p = 0.12 and p = 0.07, p for trend 0.06); however, after adjustment for potential confounders, RV length was not different in prediabetes but significantly smaller in T2DM compared to NGM (p = 0.67 and p = 0.03 respectively, p for trend = 0.04).
TDI S′RV was lower in individuals with prediabetes and T2DM compared to NGM (p = 0.08 and p < 0.01 respectively, p for trend < 0.01; Table 3). Adjustment for potential confounders had no effect on this difference.
Both TDI E′RV and A′RV were lower in individuals with prediabetes and T2DM compared to NGM (for both measurements p < 0.01 and p < 0.01 respectively, p for trend < 0.01; Table 3). Adjustment for potential confounders attenuated these differences, although the association remained significant in TDI E′RV (p = 0.01 and p = 0.02 respectively, p for trend = 0.01) and (borderline) significant in A′RV (p < 0.01 and p = 0.07 respectively, p for trend = 0.04). TDI RV E′/A′ ratio was not significantly different in individuals with prediabetes and T2DM compared to NGM (p = 0.84 and p = 0.38 respectively, p for trend = 0.39), nor after full adjustment (p = 0.85 and p = 0.49 respectively, p for trend 0.50).
The RV myocardial performance index was not significantly different in individuals with prediabetes and T2DM compared to NGM (p = 0.71 and p = 0.65 respectively, p for trend = 0.63; Table 3), nor after full adjustment (p = 0.34 and p = 0.12 respectively, p for trend 0.12).
Mediation
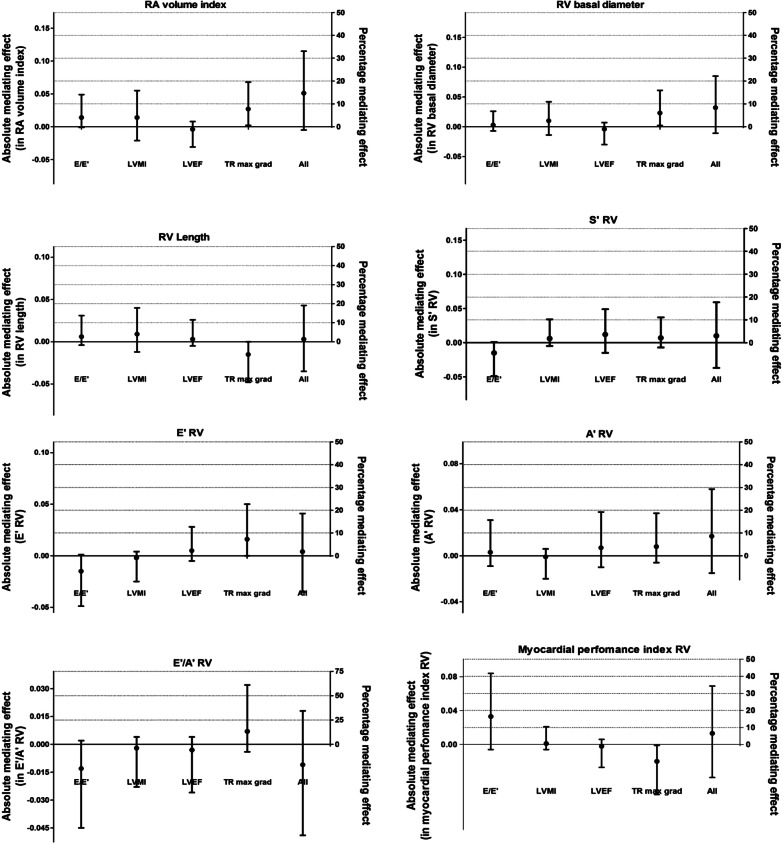
The difference in RA volume index between individuals with T2DM and those with NGM was partly mediated by the maximum gradient of the tricuspid valve (statistical mediating effect 7.8%, bootstrapped 95% CI 0.1–20.1%; Fig. 2); E/E′, LVMI, or LVEF had no significant mediating effects. The difference in RV diameter between individuals with T2DM and those with NGM was partly mediated by the maximum gradient of the tricuspid valve (statistical mediating effect 6.2%, bootstrapped 95% CI 0.3–16.4%); E/E′, LVMI, or LVEF had no significant mediating effects. Differences in RV length, S′RV, E′RV, or A′RV between individuals with T2DM and those with NGM were not significantly mediated by the maximum gradient of the tricuspid valve, E/E′, LVMI, or LVEF (Additional file 2: Table S3a, b).
Fig. 2.
Mediating effects. Mediating effects are presented as indirect effects of T2DM on RV structure and function (absolute effect on left Y-axis, relative effect in percentages on right Y-axis) through potential mediators. All analyses are adjusted for age, office systolic blood pressure, antihypertensive medication, smoking status, prior cardiovascular disease, waist circumference albuminuria, eGFR, total to high density lipoprotein cholesterol ratio, triglycerides, the use of lipid-modifying medication. RV right ventricle, RA right atrium, LVMI left ventricular mass index, E/E′ peak flow velocity E/longitudinal velocities E ratio, LVEF left ventricular ejection fraction, TR max grad maximum gradient of the tricuspid valve
Additional analyses
In the associations of (pre)diates with RV and RA structure and function, no interaction between (pre)diabetes and sex was observed. Furthermore, in these associations no interaction between (pre)diabetes and age was observed except for the RV E′/A′ (p-interaction = 0.01); the difference between individuals with T2DM and NGM was greater in the youngest compared to the oldest; however, both differences were not statistically significant (data not shown). The results of statistical analyses did not materially change when these were repeated on those with full echocardiographic data (mediators included); when office systolic blood pressure was replaced by ambulatory 24-h systolic blood pressure; when analyses were additionally adjusted for renin-angiotensin system modifying agents or moderate to vigorous physical activity; or subjects were excluded with atrial fibrillation, wall motion abnormalities, significant valvular pathology, and prior cardiovascular disease (Additional file 2: Table S4a–e).
Discussion
This study shows that both prediabetes and T2DM are associated with structural RA and RV changes, and impaired RV systolic and diastolic function, and that these associations are independent of other traditional cardiovascular risk factors. The associations between (pre)diabetes and RA and RV structure and function were largely not statistically mediated by indices of LV structure, LV function or pulmonary pressure, except for the associations between (pre)diabetes and RA and RV structure, which were statistically mediated by pulmonary pressure to a very limited extent.
This study extends previous research because of the assessment of RA and RV structure and RV function (i.e. systolic and diastolic) in a relatively large population-based study, with special emphasis on prediabetes; the comprehensive clinical characterization, which enables extensive adjustment for potential confounders; and statistical mediation analyses to investigate the role of LV structure and function in these associations. With regard to the RV structure, and in agreement with earlier studies [9, 18, 19] we showed that pre(diabetes) was associated with a smaller RV (i.e. RV diameter and RV length) although some smaller and(or) unadjusted studies [12–14, 16, 17, 22, 24–27] did not find this association. With regard to RV systolic function, and in agreement with earlier study [24–27], we showed that (pre)diabetes is associated with RV impaired systolic function independent of traditional risk factors, in contrast to most smaller and(or) unadjusted studies [9, 11–14, 16–18, 20, 22], which found no association. The Mesa study [19], which used RV ejection fraction as measurement for systolic function, found no association either. This could be explained by the fact that TDI-derived measurements, which are used in our study, are more sensitive to alteration of RV systolic function [35]. With regard to diastolic function, in agreement with most earlier studies [9, 13, 14, 17, 18, 20, 22, 24–27] we showed that (pre)diabetes was associated with impaired RV diastolic function (lower E′RV, lower E/A ratio of the tricuspid valve). In contrast to other studies [14, 17, 22, 25–27] we observed a lower A′RV in (pre)diabetes, although the latter studies were unadjusted [14, 17, 22, 25–27] and(or) performed in a selected study population (i.e. normotensive, younger, and (or) with type 1 diabetes patients) [14, 17, 25].
Pathophysiology
Although in (pre)diabetes parallel effects on RV and LV structure and function may occur, our results show that the associations between (pre)diabetes and RA and RV structure and function were not mediated by indices of LV structure of function. Since there was no collinearity in mediation analyses, these results suggest a direct myocardial effect, which may apply to both ventricles independently of each other. For instance, as investigated in the RV of Zucker diabetic fatty rats versus controls, lower metabolic rates of glucose utilization and reduced insulin sensitivity were observed [36], which parallels the metabolic changes of the LV in these rats [37]. The subsequent hyperglycemia may alter calciumhomeostasis by inducing calcium/calmodulin-depent kinase II-delta activity as shown in RA and RV myocardium of patients with T2DM and Zucker diabetic fatty rats, which was associated with altered cardiac contractility and relaxation [10]. Nevertheless, Song et al. did show that the expression of cardiac metabolism (i.e. AKT activity and glucose transporter 4) differs among the RV, LV, and interventricular septum [38]. As the RV has, in comparison to the LV, lower mass (i.e. less oxygen consumption), a higher compliance, and lower pressures [4], it is possible that the similar pathophysiological pathways in (pre)diabetes may have differential effects on RA, RV and LA and LV structure and function [5]. Future research which improves the understanding of these differential effects, can therefore contribute to the development of RV targeted therapy.
Confouding
Despite extensive adjustment for potential confounders, residual confounding cannot be fully ruled out. For example subclinical respiratory disease may be important in the association of (pre)diabetes and RA and RV structure and function [39]. Moreover, the use of body surface area to index the RA and LV mass may lead to overcorrection in the more obese (e.g. T2DM) population (with a consequential underestimation of the observed associations) [40].
Limitations
The limitations of the present study may be its cross-sectional design which does not allow strong causal inferences. Reverse causality cannot be excluded, although, from a pathophysiological point of view it appears likely that (pre)diabetes can cause structural RA and RV changes and impaired RV function but not vice versa. Second, echocardiographic assessment of RA and RV structure and function could be hampered by several aspects; the crescent shape and anatomical position of the RV and RA adds complexity to measurement of structure and function (e.g. leading to increased random error of measurement); assessment of RA and RV pressures is less accurate than invasive testing and the use of a multiparameter approach to indicate RV diastolic function whereas a clear definition on RV diastolic function is absent [41, 42]. Other imaging modalities which are less hampered by anatomy (e.g. 3D echocardiography, cardiac MRI) or may be more sensitive to preclinical changes (e.g. deformation echocardiography using strain imaging or speckle tracking) or invasive testing were not available in this study. Third, the generalizability of our findings to other populations can be questioned; the study population primarily consisted of European Caucasians and within this cohort individuals with T2DM were well controlled for their diabetes (i.e. mean HbA1c 6.9%) and comorbid cardiovascular risk factors (i.e. use of antihypertensive and lipid-modifying medication in 68.8% and 74.1% respectively). Fourth, RV function was measured with use of TDI in the whole study population whereas only in a subset tricuspid inflow velocities and TAPSE were measured. Nevertheless, TDI measurements have been shown to be a reliable proxy measurement for RV function [35]. Fifth, clinical outcomes (e.g. incident heart failure, or cardiovascular death) were not available. However previous studies, in a general population, showed that RV structure and function were independent risk factors for incident heart failure and cardiovascular death [6, 43].
Conclusions
In conclusion, in this population-based study (pre)diabetes is associated with structural RA and RV changes, and impaired RV systolic and diastolic function, independent of traditional cardiovascular risk factors. These associations were largely not statistically mediated by indices of LV structure, LV function or pulmonary pressure. This suggests that (pre)diabetes affects the RA and RV structure and function due to direct myocardial involvement. Although the absolute differences are small, this should increase the awareness that in patients with (pre)diabetes preclinical structural and functional changes already have taken place. The accumulated changes may alter the course of overt cardiac disease [44]. Although RV-targeted therapy is not available at the moment, these results suggest that future research should focus on the pathophysiological pathways of RA and RV impairment in (pre)diabetes.
Supplementary information
Additional file 1. Supplemental methods.
Acknowledgements
Not applicable.
Abbreviations
- LV
Left ventricular
- LVMI
Left ventricular mass index
- LVEF
Left ventricular ejection fraction
- NGM
Normal glucose metabolism
- RA
Right atrial
- RV
Right ventricular
- T2DM
Type 2 diabetes mellitus
- TAPSE
Tricuspid annular plane systolic excursion
- TDI
Tissue doppler imaging
- TRmax grad
Maximum tricuspid gradient
Authors’ contributions
PL participated in acquisition of data, analyzed data, interpreted results, and wrote the manuscript. MV participated in acquisition of data, contributed to discussion, reviewed and edited the manuscript. RH, CK, and MS contributed to study conception, study design, and reviewed and edited the manuscript. AK contributed to discussion, reviewed and edited the manuscript. HPBLR contributed to study design, interpretation of data, revised the manuscript critically for important intellectual content. CS contributed to conception and design, contributed interpretation of data, revised the manuscript critically for important intellectual content. CS is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors read and approved the final manuscript.
Funding
This study was supported by the European Regional Development Fund via OP-Zuid, the Province of Limburg, the Dutch Ministry of Economic Affairs (Grant 31O.041), Stichting De Weijerhorst (Maastricht, The Netherlands), the Pearl String Initiative Diabetes (Amsterdam, The Netherlands), CARIM School for Cardiovascular Diseases (Maastricht, The Netherlands), Stichting Annadal (Maastricht, The Netherlands), Health Foundation Limburg (Maastricht, The Netherlands) and by unrestricted Grants from Janssen-Cilag B.V. (Tilburg, The Netherlands), Novo Nordisk Farma B.V. (Alphen aan den Rijn, The Netherlands) and Sanofi-Aventis Netherlands B.V. (Gouda, The Netherlands).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The study has been approved by the institutional medical ethical committee (Medisch Ethische Toetsingscommissie, Maastricht University) (NL31329.068.10) and the Minister of Health, Welfare and Sports of the Netherlands (Permit 131088-105234-PG). All participants gave written informed consent.
Consent for publication
Not applicable.
Competing interests
PL, MV, RH, CK, AK, MS, and CS have nothing to disclose. Dr. HPBLR reports unrestricted research grants from Roche Diagnostics, Vifor and Novartis and serves as member of the advisory board of Roche Diagnostics, Vifor and Novartis outside the submitted work.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Pauline B. C. Linssen, Email: paulinelinssen@gmail.com
Marja G. J. Veugen, Email: marja.veugen@mumc.nl
Ronald M. A. Henry, Email: rma.henry@mumc.nl
Carla J. H. van der Kallen, Email: c.vanderkallen@maastrichtuniversity.nl
Abraham A. Kroon, Email: aa.kroon@mumc.nl
Miranda T. Schram, Email: m.schram@maastrichtuniversity.nl
Hans-Peter Brunner-La Rocca, Email: hp.brunnerlarocca@mumc.nl.
Coen D. A. Stehouwer, Email: cda.stehouwer@mumc.nl
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12933-020-01055-y.
References
- 1.Kannel WB, McGee DL. Diabetes and cardiovascular disease. The Framingham study. JAMA. 1979;241(19):2035–2038. doi: 10.1001/jama.241.19.2035. [DOI] [PubMed] [Google Scholar]
- 2.Ford ES, Zhao G, Li C. Pre-diabetes and the risk for cardiovascular disease: a systematic review of the evidence. J Am Coll Cardiol. 2010;55(13):1310–1317. doi: 10.1016/j.jacc.2009.10.060. [DOI] [PubMed] [Google Scholar]
- 3.Haddad F, Doyle R, Murphy DJ, Hunt SA. Right ventricular function in cardiovascular disease, part II: pathophysiology, clinical importance, and management of right ventricular failure. Circulation. 2008;117(13):1717–1731. doi: 10.1161/CIRCULATIONAHA.107.653584. [DOI] [PubMed] [Google Scholar]
- 4.Haddad F, Hunt SA, Rosenthal DN, Murphy DJ. Right ventricular function in cardiovascular disease, part I: anatomy, physiology, aging, and functional assessment of the right ventricle. Circulation. 2008;117(11):1436–1448. doi: 10.1161/CIRCULATIONAHA.107.653576. [DOI] [PubMed] [Google Scholar]
- 5.Sanz J, Sanchez-Quintana D, Bossone E, Bogaard HJ, Naeije R. Anatomy, function, and dysfunction of the right ventricle: JACC state-of-the-art review. J Am Coll Cardiol. 2019;73(12):1463–1482. doi: 10.1016/j.jacc.2018.12.076. [DOI] [PubMed] [Google Scholar]
- 6.Kawut SM, Barr RG, Lima JA, Praestgaard A, Johnson WC, Chahal H, Ogunyankin KO, Bristow MR, Kizer JR, Tandri H, et al. Right ventricular structure is associated with the risk of heart failure and cardiovascular death: the multi-ethnic study of atherosclerosis (MESA)–right ventricle study. Circulation. 2012;126(14):1681–1688. doi: 10.1161/CIRCULATIONAHA.112.095216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Melenovsky V, Hwang SJ, Lin G, Redfield MM, Borlaug BA. Right heart dysfunction in heart failure with preserved ejection fraction. Eur Heart J. 2014;35(48):3452–3462. doi: 10.1093/eurheartj/ehu193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boudina S, Abel ED. Diabetic cardiomyopathy revisited. Circulation. 2007;115(25):3213–3223. doi: 10.1161/CIRCULATIONAHA.106.679597. [DOI] [PubMed] [Google Scholar]
- 9.Tadic M, Celic V, Cuspidi C, Ilic S, Pencic B, Radojkovic J, Ivanovic B, Stanisavljevic D, Kocabay G, Marjanovic T. Right heart mechanics in untreated normotensive patients with prediabetes and type 2 diabetes mellitus: a two- and three-dimensional echocardiographic study. J Am Soc Echocardiogr. 2015;28(3):317–327. doi: 10.1016/j.echo.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 10.Daniels LJ, Wallace RS, Nicholson OM, Wilson GA, McDonald FJ, Jones PP, Baldi JC, Lamberts RR, Erickson JR. Inhibition of calcium/calmodulin-dependent kinase II restores contraction and relaxation in isolated cardiac muscle from type 2 diabetic rats. Cardiovasc Diabetol. 2018;17(1):89. doi: 10.1186/s12933-018-0732-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Whitaker ME, Nair V, Sinari S, Dherange PA, Natarajan B, Trutter L, Brittain EL, Hemnes AR, Austin ED, Patel K, et al. Diabetes mellitus associates with increased right ventricular afterload and remodeling in pulmonary arterial hypertension. Am J Med. 2018;131(6):702. doi: 10.1016/j.amjmed.2017.12.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jedrzejewska I, Krol W, Swiatowiec A, Wilczewska A, Grzywanowska-Laniewska I, Dluzniewski M, Braksator W. Left and right ventricular systolic function impairment in type 1 diabetic young adults assessed by 2D speckle tracking echocardiography. Eur Heart J Cardiovasc Imaging. 2016;17(4):438–446. doi: 10.1093/ehjci/jev164. [DOI] [PubMed] [Google Scholar]
- 13.Tadic M, Ilic S, Cuspidi C, Ivanovic B, Bukarica L, Kostic N, Marjanovic T, Kocijancic V, Celic V. Left and right atrial phasic function and deformation in untreated patients with prediabetes and type 2 diabetes mellitus. Int J Cardiovasc Imaging. 2015;31(1):65–76. doi: 10.1007/s10554-014-0536-3. [DOI] [PubMed] [Google Scholar]
- 14.Karamitsos TD, Karvounis HI, Dalamanga EG, Papadopoulos CE, Didangellos TP, Karamitsos DT, Parharidis GE, Louridas GE. Early diastolic impairment of diabetic heart: the significance of right ventricle. Int J Cardiol. 2007;114(2):218–223. doi: 10.1016/j.ijcard.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 15.Kosmala W, Przewlocka-Kosmala M, Mazurek W. Subclinical right ventricular dysfunction in diabetes mellitus–an ultrasonic strain/strain rate study. Diabetic Med. 2007;24(6):656–663. doi: 10.1111/j.1464-5491.2007.02101.x. [DOI] [PubMed] [Google Scholar]
- 16.Tadic M, Cuspidi C, Vukomanovic V, Ilic S, Celic V, Obert P, Kocijancic V. The influence of type 2 diabetes and arterial hypertension on right ventricular layer-specific mechanics. Acta Diabetol. 2016;53(5):791–797. doi: 10.1007/s00592-016-0874-9. [DOI] [PubMed] [Google Scholar]
- 17.Suran D, Sinkovic A, Naji F. Tissue Doppler imaging is a sensitive echocardiographic technique to detect subclinical systolic and diastolic dysfunction of both ventricles in type 1 diabetes mellitus. BMC Cardiovasc Disord. 2016;16:72. doi: 10.1186/s12872-016-0242-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Widya RL, van der Meer RW, Smit JW, Rijzewijk LJ, Diamant M, Bax JJ, de Roos A, Lamb HJ. Right ventricular involvement in diabetic cardiomyopathy. Diabetes Care. 2013;36(2):457–462. doi: 10.2337/dc12-0474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chahal H, Johnson C, Tandri H, Jain A, Hundley WG, Barr RG, Kawut SM, Lima JA, Bluemke DA. Relation of cardiovascular risk factors to right ventricular structure and function as determined by magnetic resonance imaging (results from the multi-ethnic study of atherosclerosis) Am J Cardiol. 2010;106(1):110–116. doi: 10.1016/j.amjcard.2010.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kosmala W, Colonna P, Przewlocka-Kosmala M, Mazurek W. Right ventricular dysfunction in asymptomatic diabetic patients. Diabetes Care. 2004;27(11):2736–2738. doi: 10.2337/diacare.27.11.2736. [DOI] [PubMed] [Google Scholar]
- 21.Movahed MR, Milne N. Presence of biventricular dysfunction in patients with type II diabetes mellitus. Congest Heart Fail. 2007;13(2):78–80. doi: 10.1111/j.1527-5299.2007.888138.x. [DOI] [PubMed] [Google Scholar]
- 22.Tayyareci Y, Yurdakul S, Tayyareci G, Nisanci Y, Umman B, Bugra Z. Impact of myocardial acceleration during isovolumic contraction in evaluating subclinical right ventricular systolic dysfunction in type 2 diabetes mellitus patients. Echocardiography. 2010;27(10):1211–1218. doi: 10.1111/j.1540-8175.2010.01237.x. [DOI] [PubMed] [Google Scholar]
- 23.Paneni F, Gregori M, Tocci G, Palano F, Ciavarella GM, Pignatelli G, Marra A, Sciarretta S, Ferrucci A, Volpe M. Do diabetes, metabolic syndrome or their association equally affect biventricular function? A tissue Doppler study. Hypertens Res. 2013;36(1):36–42. doi: 10.1038/hr.2012.137. [DOI] [PubMed] [Google Scholar]
- 24.Gorter TM, Streng KW, van Melle JP, Rienstra M, Dickinson MG, Lam CSP, Hummel YM, Voors AA, Hoendermis ES, van Veldhuisen DJ. Diabetes mellitus and right ventricular dysfunction in heart failure with preserved ejection fraction. Am J Cardiol. 2018;121(5):621–627. doi: 10.1016/j.amjcard.2017.11.040. [DOI] [PubMed] [Google Scholar]
- 25.Ahmed TA, Ahmed YA, Arafa AI, Salah RA. Detection of occult right ventricular dysfunction in young Egyptians with type 1 diabetes mellitus by two-dimensional speckle tracking echocardiography. Indian Heart J. 2018;70(5):665–671. doi: 10.1016/j.ihj.2018.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parsaee M, Bahmanziari P, Ardeshiri M, Esmaeilzadeh M. Obvious or subclinical right ventricular dysfunction in diabetes mellitus (type II): an echocardiographic tissue deformation study. J Tehran Heart Center. 2012;7(4):177–181. [PMC free article] [PubMed] [Google Scholar]
- 27.Kowsari AA, Hosseinsabet A. Evaluation of the right ventricular function in prediabetes: a 2-d speckle tracking echocardiographic study. Ultrasound Med Biol. 2016;42(6):1321–1329. doi: 10.1016/j.ultrasmedbio.2016.01.011. [DOI] [PubMed] [Google Scholar]
- 28.Schram MT, Sep SJ, van der Kallen CJ, Dagnelie PC, Koster A, Schaper N, Henry RM, Stehouwer CD. The Maastricht Study: an extensive phenotyping study on determinants of type 2 diabetes, its complications and its comorbidities. Eur J Epidemiol. 2014;29(6):439–451. doi: 10.1007/s10654-014-9889-0. [DOI] [PubMed] [Google Scholar]
- 29.World Health Organization . Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia. Geneva: World Health Organization; 2006. [Google Scholar]
- 30.Inker LA, Schmid CH, Tighiouart H, Eckfeldt JH, Feldman HI, Greene T, Kusek JW, Manzi J, Van Lente F, Zhang YL, et al. Estimating glomerular filtration rate from serum creatinine and cystatin C. New Engl J Med. 2012;367(1):20–29. doi: 10.1056/NEJMoa1114248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Martens RJ, Kimenai DM, Kooman JP, Stehouwer CD, Tan FE, Bekers O, Dagnelie PC, van der Kallen CJ, Kroon AA, Leunissen KM, et al. Estimated glomerular filtration rate and albuminuria are associated with biomarkers of cardiac injury in a population-based cohort study: the maastricht study. Clin Chem. 2017;63(4):887–897. doi: 10.1373/clinchem.2016.266031. [DOI] [PubMed] [Google Scholar]
- 32.Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Med Sci Sports Exerc. 2001;33(7):1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 33.Tadic M, Cuspidi C, Sljivic A, Andric A, Ivanovic B, Scepanovic R, Ilic I, Jozika L, Marjanovic T, Celic V. Effects of the metabolic syndrome on right heart mechanics and function. Canad J Cardiol. 2014;30(3):325–331. doi: 10.1016/j.cjca.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 34.Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav Res Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- 35.Gondi S, Dokainish H. Right ventricular tissue Doppler and strain imaging: ready for clinical use? Echocardiography. 2007;24(5):522–532. doi: 10.1111/j.1540-8175.2007.00430.x. [DOI] [PubMed] [Google Scholar]
- 36.van den Brom CE, Bosmans JW, Vlasblom R, Handoko LM, Huisman MC, Lubberink M, Molthoff CF, Lammertsma AA, Ouwens MD, Diamant M, et al. Diabetic cardiomyopathy in Zucker diabetic fatty rats: the forgotten right ventricle. Cardiovasc Diabetol. 2010;9:25. doi: 10.1186/1475-2840-9-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van den Brom CE, Huisman MC, Vlasblom R, Boontje NM, Duijst S, Lubberink M, Molthoff CF, Lammertsma AA, van der Velden J, Boer C, et al. Altered myocardial substrate metabolism is associated with myocardial dysfunction in early diabetic cardiomyopathy in rats: studies using positron emission tomography. Cardiovasc Diabetol. 2009;8:39. doi: 10.1186/1475-2840-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Song J, Shen S, Zhang M, Wang K, Zhang Y, Li X, Wang N, Cao Y. Differences in Akt signaling and metabolism gene expression in the right heart, intraventricular septum and left heart of rodents. Int J Clin Exp Pathol. 2015;8(10):12915–12921. [PMC free article] [PubMed] [Google Scholar]
- 39.Takahashi T, Yoshihisa A, Sugimoto K, Yokokawa T, Misaka T, Kaneshiro T, Oikawa M, Kobayashi A, Nakazato K, Ishida T, et al. Associations between diabetes mellitus and pulmonary hypertension in chronic respiratory disease patients. PLoS ONE. 2018;13(10):e0205008. doi: 10.1371/journal.pone.0205008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hoit BD. It’s time to index the right ventricle, but to what and how? J Am Soc Echocardiogr. 2012;25(12):1277–1279. doi: 10.1016/j.echo.2012.10.017. [DOI] [PubMed] [Google Scholar]
- 41.Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23(7):685–713. doi: 10.1016/j.echo.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 42.Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, 3rd, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of echocardiography and the european association of cardiovascular imaging. J Am Soc Echocardiogr. 2016;29(4):277–314. doi: 10.1016/j.echo.2016.01.011. [DOI] [PubMed] [Google Scholar]
- 43.Modin D, Mogelvang R, Andersen DM, Biering-Sorensen T. Right ventricular function evaluated by tricuspid annular plane systolic excursion predicts cardiovascular death in the general population. J Am Heart Assoc. 2019;8(10):e012197. doi: 10.1161/JAHA.119.012197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Roifman I, Ghugre N, Zia MI, Farkouh ME, Zavodni A, Wright GA, Connelly KA. Diabetes is an independent predictor of right ventricular dysfunction post ST-elevation myocardial infarction. Cardiovasc Diabetol. 2016;15:34. doi: 10.1186/s12933-016-0352-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Supplemental methods.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.