Abstract
Proper nutrition during pregnancy is vital to maternal health and fetal development and may be challenging for Navajo Nation residents because access to affordable and healthy foods is limited. It has been several decades since reported diet quality during pregnancy was examined on Navajo Nation. We present the first study to estimate iodine intake and use the Healthy Eating Index (HEI‐2015) to assess maternal diet quality among pregnant women in the Navajo Birth Cohort Study (NBCS). Based on dietary intake data derived from food frequency questionnaires, overall estimated micronutrient intake has remained similar since the last assessment in 1981, with potential improvements evident for folate and niacin. A high proportion of women (>50%) had micronutrient intakes from dietary sources below the Estimated Average Requirements during pregnancy. The median urinary iodine concentration for NBCS women (90.8 μg/L; 95% CI [80, 103.5]) was less than adequate and lower than concentrations reported for pregnant women that participated in the National Health and Nutrition Examination Survey (NHANES) between 2011 and 2014. Overall, average diet quality of NBCS women estimated using the HEI‐2015 (62.4; 95% CI [60.7, 64.0]) was similar to that reported for women of child‐bearing age and pregnant women in NHANES. Although, NBCS women had diets high in added sugar, with sugar‐sweetened beverages as the primary contributors. Our study provides updated insights on maternal diet quality that can inform health and nutrition initiatives in Navajo communities emphasizing nutrition education and access to prenatal vitamins and calcium, iodine, and vitamin E dense foods.
Keywords: American Indian, dietary assessment, fetal development, maternal nutrition, Navajo, Native American, nutrition policy, pregnancy and nutrition
Key messages
Estimated dietary intake of micronutrients in NBCS women improved over the last 30 years, particularly for the B vitamins.
>50% of NBCS women reported inadequate dietary intakes for several micronutrients, emphasizing the importance of access to and promotion of prenatal multivitamin use for Navajo mothers.
NBCS women had diets higher in whole grains and fruit intake but also diets higher in added sugar, highlighting the importance of continuing efforts focused on improving the local food environment.
First study to report iodine status and potential risk of iodine deficiency among Navajo women, emphasizing the need for access to iodine containing multivitamins as a part of women's healthcare.
1. INTRODUCTION
Indigenous communities in the United States have disproportionally higher rates of pregnancy complications, poor birth outcomes, and chronic disease compared with non‐Hispanic White women (MacDorman, 2011; MacDorman, Kirmeyer, & Wilson, 2012). These rates are influenced by several community‐level factors, including exposure to environmental contaminants, access to prenatal care, socio‐economics, and challenging local food environments (HealthyPeople.gov, 2019; Sarche & Spicer, 2008; Vintzileos, Ananth, Smulian, Scorza, & Knuppel, 2002). The tribal lands of the Navajo Nation (Navajo), located in the southwestern United States, encompasses 71,000 km2 in Arizona, New Mexico, and Utah and is the largest Indian reservation in the U.S. Navajo is sparsely populated, with a large proportion of the population living in rural and geographically remote locations. According to the 2010 U.S. Census, 173,667 people live on the Navajo Nation (90% are Navajo). There is an estimated 10 grocery stores and a total of 84 stores that sell food in the entire Navajo Nation. Access to affordable and healthy foods is low (Kumar et al., 2016; Pardilla, Prasad, Suratkar, & Gittelsohn, 2013), with consequent low reported intakes of fruits and vegetables and high intake of fats in the general population (Ballew et al., 1997; Sharma et al., 2010). On average, it is 15 miles from Navajo chapter houses (seat of local government on the Navajo Nation) to the nearest food store that accepts the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) and 24 miles to the nearest “healthy” food store (stores with six or more fresh vegetables and fruits). Structural barriers, such as the large distances between grocery stores, income disparities, and lack of access to transportation, foster a challenging food environment on Navajo Nation.
Adequate maternal nutrition is critical for normal fetal development and for reducing the risk of pregnancy complications, such as gestational diabetes (Abu‐Saad & Fraser, 2010; Nnam, 2015; Ojha, Fainberg, Sebert, Budge, & Symonds, 2015). More than 30 years has lapsed since the last published study that focused on the dietary intake and micronutrient status of pregnant Navajo women (Butte, Calloway, & Van Duzen, 1981). Butte et al. (1981) found that intake of multiple micronutrients were potentially inadequate based on 24‐hr dietary recalls in a small sample of 23 Navajo women. Biochemical assessments in 110 women at or shortly after birth identified about one in five women experiencing anaemia and low serum retinol and a prevalence of low serum zinc concentrations, reflective of population risk for zinc deficiency (Butte et al., 1981).
In 2010, the Navajo Birth Cohort Study (NBCS) was initiated to assess maternal and child health outcomes and address community concerns about uranium exposures in Navajo communities (Hunter, Lewis, Peter, Begay, & Ragin‐Wilson, 2015). During the enrolment period (2013–2018), the NBCS study team enrolled 781 mother–infant pairs from communities across Navajo Nation. The objective of this analysis was to examine diet quality during pregnancy in a subset of NBCS women using a modified Harvard Service Food Frequency Questionnaire (HSFFQ) that included traditional Navajo foods. With food assistance programs emphasizing healthier foods (Schultz, Byker Shanks, & Houghtaling, 2015) and the inception of Navajo community‐based health literacy and food access programs, we hypothesize that maternal diet quality among Navajo women has improved over the last 30 years, but may still reflect constraints imposed by the challenging local food environment.
2. METHODS
2.1. Navajo Birth Cohort Study
The sample population for this paper included 781 pregnant Navajo women recruited between February 2013 and June 2018 from locations across the Navajo Nation. Navajo staff recruited women during prenatal visits at participating Indian Health Service or Public Law 638 hospitals on the Navajo Nation. Eligibility was limited to women who had Indian Health Service beneficiary status and (a) a clinically confirmed pregnancy; (b) maternal age between 14 and 45 years; (c) residence on the Navajo Nation for a minimum of 5 years; (d) willingness to deliver at one of six participating Indian Health Service or Public Law 638 hospital facilities; and (e) willingness to allow follow‐up evaluations during the baby's first year of life. At time of enrolment, a survey was administered to maternal participants to obtain information about age, employment status, educational attainment, annual household income, and smoking status. Medical records were also reviewed for pre‐pregnancy height and weight. A total of 781 women enrolled in NBCS, with 283 completing food frequency questionnaires (FFQs). From these, 41 were excluded due to implausible total energy intake (TEI) of <600 or >5,000 kcal/day, resulting in 242 questionnaires used for dietary intake analysis. Of these individuals, 222 had also completed enrolment surveys to collect demographic and socio‐economic information.
2.2. Dietary assessment
A modified HSFFQ survey was administered to NBCS women (Baer et al., 2005). The Navajo diet includes native plant‐ and game‐based foods such as dandelion greens, blue corn mush, and mutton (lamb), and transitional foodstuffs such as frybread (deep fried wheat flour), Navajo burgers (fry bread, hamburger patty, and condiments) and Navajo tacos (Kopp, 1986). The NBCS program added these Navajo foods to the HSFFQ instrument based on the guidance from Navajo community members and field staff. FFQ surveys were administered in person by trained women (predominately Navajo) who were either university employees, Navajo Division of Health Community Health representatives, or Indian Health Service employees. Staff were trained using food models and were instructed to use the models while administering the survey. FFQs were administered by trained staff during 36‐week prenatal appointments at the hospital or clinic. In some cases, FFQs were administered at the hospital within 1 week of delivery (n = 38; 17%). Participants were asked about their typical portion size and frequency of consuming each food item (never to six times per day) within the 4 weeks prior to the date of the interview. For the FFQ and other surveys administered, NBCS participants could opt not to answer any question, and this was recorded as “not reported.”
FFQs were processed, and reported consumption data were converted to nutrient intake by assigning a daily frequency weight and using the Nutrition Data System for Research (NDSR), a computer‐based software application developed at the University of Minnesota Nutrition Coordinating Center. The Nutrition Coordinating Center Food and Nutrient Database serves as the source of food composition information used by the NDSR for estimating nutrient intake based on FFQ responses (Schakel, Sievert, & Buzzard, 1988; Sievert, Schakel, & Buzzard, 1989). This database includes over 18,000 foods including 8,000 brand name products. Ingredient choices and preparation methods provide more than 160,000 food variants. Values for 165 nutrients, nutrient ratios, and other food components are generated from the database. The U.S. Department of Agriculture (USDA) Nutrient Data Laboratory is the primary source of nutrient values and nutrient composition in NDSR (Feskanich, Sielaff, Chong, & Buzzard, 1989). Representative recipes for fry bread, blue corn mush, Navajo burger, Navajo taco, and mutton‐based foods were added to the database for nutrient determination. Multivitamin supplementation (i.e., prenatal multivitamins) was excluded from our dietary intake analyses.
Pregnancy and age‐specific estimated average requirement (EAR) intakes were used as benchmarks to determine intake adequacy and the proportions of participants meeting current recommendations using the EAR cut‐point method (Institute of Medicine, 2000). Intake ratios were used as a metric to examine potential changes in nutrient intake between the Butte et al. study and the present study. Mean nutrient intake values were determined for NBCS participants (n = 242), and mean nutrient intake values reported in Butte et al. were used to calculate intake ratios for overlapping nutrients. An intake ratio <1 suggests lower estimated intake, and intake ratios >1 suggest greater estimated intake among NBCS participants compared with the Butte et al. study.
2.3. Diet quality
The Health Eating Index (HEI) is a metric developed to evaluate diet quality (Freedman, Guenther, Krebs‐Smith, & Kott, 2008; Miller et al., 2011). The HEI total score is the summation of individual component scores with a maximum total score of 100. Higher scores indicate greater consistency with recommended healthy diet guidelines. We calculated scores for 13 dietary components including total fruit, whole fruit, total vegetables, greens and beans, whole grains, dairy, total protein foods, seafood and plant proteins, fatty acid ratio, refined grains, saturated fat sodium, and added sugar. For the individual components of added sugar, sodium, saturated fat, and refined grains, a low score indicates increased dietary intake of these foods; for all other components, a low score indicates low dietary intake of those foods. We converted NDSR food servings per food group to cup equivalents to conform with HEI‐2015 scoring methods. We then calculated a population ratio HEI score for NBCS participants using the method previously outlined (Freedman et al., 2008; Guenther et al., 2014). This method obtains estimates of a population's total intake by taking the sum total of the relevant nutrient and energy across all sampled participants. Then the ratio of each nutrient to energy is calculated and converted to an HEI score. The total HEI score is the sum of HEI values for each dietary component. For comparison, we calculated two National Health and Nutrition Examination Survey (NHANES) HEI scores using a subset of NHANES 2011–2012 and 2013–2014 24‐hr dietary recall data for women aged 14–45 years, not considering pregnancy and lactation status (N = 1,492) and a subset of NHANES 2011–2012 and 2013–2014 24‐hr dietary recall data for pregnant women aged 14–45 years (N = 162) using the complex survey design population method.
2.4. Sensitivity analysis
We conducted a sensitivity analysis to investigate how daily prenatal supplements would impact the profile of the study population meeting EAR recommendations. We identified the most commonly consumed prenatal vitamin, as reported by participants, and acquired the reported micronutrient content for this brand. We randomly sampled 5% (N = 11), 25% (N = 56), 50% (N = 111), 75% (N = 167), and 95% (N = 211) of the total study participants (N = 222), for 1,000 iterations, and each time, we added the referred daily supplement values from the prenatal vitamin with the estimated micronutrient intake from the FFQ questionnaire.
2.5. Urinary iodine measurements
Iodine concentrations measured in urine samples collected in the morning, or from other spot urine collections, have been shown to adequately assess a population's iodine status (Rohner et al., 2014). During a women's 36‐week prenatal appointment, trained staff collected spot urine samples (N = 193) in sterile 50‐ml urine collection cups pre‐screened for metals that were provided by the National Center for Environmental Health's Division of Laboratory Sciences. Urine samples were stored at ‐80 °C until shipped overnight on dry ice to the Division of Laboratory Sciences and, once received, samples were stored at ≤−20°C until preparation for analysis. Urine iodine concentrations were measured using inductively coupled plasma dynamic reaction cell mass spectrometry (Centers for Disease Control and Prevention, 2011).
2.6. Statistical methods
Descriptive statistics for a continuous variable includes sample mean with standard deviation denoted by Mean (SD) and median with the interquartile range denoted by Median (IQR). For hypothesis testing of no difference between groups, the ANOVA and Kruskal–Wallis tests were performed as parametric and non‐parametric approaches for robustness of testing conclusion. For categorical variables, frequency and percentage were displayed for each category. The Fisher's exact test was used for testing for associations between stratified groups when count data are presented using a contingency table. Intakes of added sugars were expressed as contribution (%) to TEI and stratified by age and participation in food assistance programs.
For HEI calculations, we utilized the SAS macros provided by the National Cancer Institute (National Cancer Institute, n.d.). Specifically, the weighted means and variance–covariance matrix were estimated from the dataset and then used for Monte Carlo simulations to generate 10,000 independent observations. The mean of individual HEI components, the total scores, and their confidence intervals were further calculated from the simulated datasets. For NHANES data, the sampling weight was also accounted for. All the statistical analyses were performed using SAS 9.4 (SAS Institute Inc., Cary, NC) or R 3.2.1 (R Development Core Team, Vienna, Austria).
2.7. Human participants statement
All women provided written informed consent for the study protocol approved by the University of New Mexico Institutional Review Board (HRPO 11‐310) and the Navajo Nation Human Research Review Board (NNR 11.323).
3. RESULTS
3.1. NBCS participants
Table 1 presents the characteristics of NBCS women with completed FFQ surveys and enrolment data (N = 222). The mean age for participants was 28.3 ± 6.4 years. The majority of women (74%) reported enrolment in the Special Supplemental Nutrition Program for WIC and the use of prenatal multivitamins, although the frequency of use was not reported. Over half of NBCS women reported an annual household income below $20,000 and had pre‐pregnancy body mass index values characterized as overweight or obese. Overall, the 222 women with completed FFQ surveys lived in communities from across Navajo Nation (Figure S1). The socio‐demographic characteristics for the subset of NBCS women who completed an FFQ survey were comparable with other recent studies on the Navajo Nation (Kumar et al., 2016) and with NBCS women overall (Table 1). No significant differences were observed.
Table 1.
Navajo Birth Cohort demographics. Demographic characteristics comparing women with completed FFQ questionnaires and women without FFQ information nested within the Navajo Birth Cohort Study (NBCS)a
| FFQ | Non‐FFQ | ||||||
|---|---|---|---|---|---|---|---|
| Characteristic | N | Mean (SD)/Prop (%) | Median (IQR) | N | Mean (SD)/Prop % | Median (IQR) | p valueb |
| Age at FFQ | 222 | 28.3 (6.4) | 27.6 (23.3–32.6) | 379 | 27.5 (5.8) | 26.9 (23.0‐31.9) | .144 |
| Gestational weeks at FFQ for those surveyed before delivery | 184 | 37.3 (2) | 37 (36–39) | ||||
| FFQ surveyed before delivery | |||||||
| Yes | 184 | 82.9 | |||||
| No | 38 | 17.1 | |||||
| Prenatal vitamin use | .145 | ||||||
| Yes | 167 | 75.2 | 213 | 56.2 | |||
| No | 1 | 0.5 | 7 | 1.8 | |||
| Not reported | 54 | 24.3 | 159 | 42 | |||
| Gravidity | 182 | 3 (1.9) | 3 (1.2–4.0) | 264 | 3.1 (2.1) | 3 (1–4) | .520 |
| Parity | 182 | 1.7 (1.6) | 1 (0–2) | 264 | 1.6 (1.6) | 1 (0–3) | .712 |
| Pre‐pregnancy weight (kg) | 184 | 76.7 (18.7) | 74.8 (64.1–88.6) | 250 | 78.1 (21.5) | 74.8 (64.1–87.9) | .469 |
| Term weight (kg) | 182 | 87.8 (18.4) | 87.2 (75.7–98.0) | 234 | 87.2 (18.8) | 85.1 (75.3–96.0) | .740 |
| Pre‐pregnancy BMI | .757 | ||||||
| <25 | 49 | 22.1 | 63 | 16.6 | |||
| 25–30 | 58 | 26.1 | 66 | 17.4 | |||
| >30 | 73 | 32.9 | 99 | 26.1 | |||
| Not reported | 42 | 18.9 | 151 | 39.8 | |||
| Gestational diabetes | .808 | ||||||
| Yes | 24 | 10.8 | 30 | 7.9 | |||
| No | 144 | 64.9 | 202 | 53.3 | |||
| Not reported | 54 | 24.3 | 147 | 38.8 | |||
| Eclampsia, preeclampsia, toxaemia during pregnancy, or pregnancy‐induced hypertension | .415 | ||||||
| Yes | 21 | 9.5 | 22 | 5.8 | |||
| No | 149 | 67.1 | 214 | 56.5 | |||
| Not reported | 52 | 23.4 | 143 | 37.7 | |||
| Marital status | .404 | ||||||
| Married | 183 | 82.4 | 301 | 79.4 | |||
| Unmarried | 37 | 16.7 | 75 | 19.8 | |||
| Not reported | 2 | 0.9 | 3 | 0.8 | |||
| Education | .058 | ||||||
| ≤High School | 112 | 50.5 | 229 | 60.4 | |||
| >High School | 100 | 45 | 145 | 38.3 | |||
| Not reported | 10 | 4.5 | 5 | 1.3 | |||
| Employment status | .759 | ||||||
| Unemployed | 150 | 67.6 | 262 | 69.1 | |||
| Employed | 72 | 32.4 | 117 | 30.9 | |||
| Annual household income | .857 | ||||||
| <$20,000 | 123 | 55.4 | 188 | 49.6 | |||
| $20,000–$39,999 | 35 | 15.8 | 50 | 13.2 | |||
| ≥40,000 | 33 | 14.9 | 44 | 11.6 | |||
| Not reported | 31 | 14 | 97 | 25.6 | |||
| Food assistance programc | .563 | ||||||
| Yes | 164 | 73.9 | 290 | 76.5 | |||
| No | 55 | 24.8 | 85 | 22.4 | |||
| Not reported | 3 | 1.4 | 4 | 1.1 | |||
Abbreviations: BMI. body mass index; FFQ, food frequency questionnaire; IQR, interquartile range; SD, standard deviation.
Continuous variables are expressed as means (SD) and median (IQR), and categorical data are expressed as percentage.
The category of “Not reported” was not included in statistical testing. For continuous variables, a two‐sample t test was done. For “Registration in WIC,” the test for comparison between FFQ and non‐FFQ was done by Fisher's exact test; for the remaining categorical variables, the comparison was done by χ 2 test.
Women, Infants, and Children, SNAP/food stamps, or food bank.
3.2. Mean nutrient intake ratios suggest some improvement in estimated intake over time
Mean intake ratios between Butte et al. (1981) and our study were calculated as a metric to evaluate potential changes in estimated dietary intakes over time (Figure 1a). Almost all nutrients examined had ratios close to or above one, indicating that estimated micronutrient intake has remained similar or improved slightly over time. Potential improvements were evident for the B vitamins (particularly folate and niacin).
Figure 1.
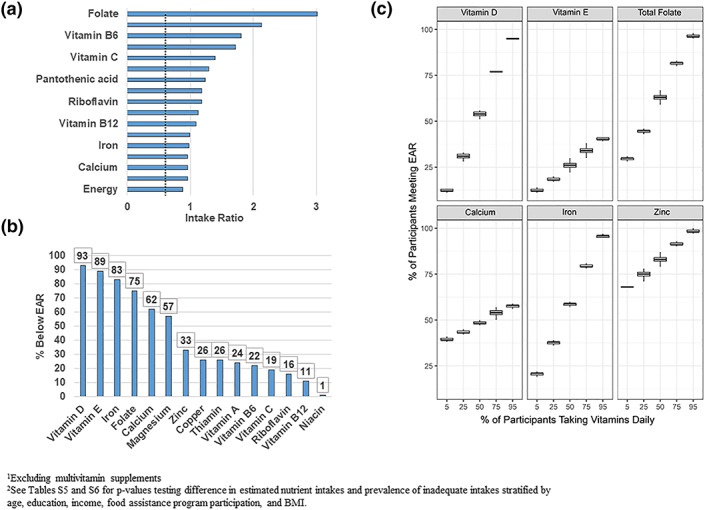
Estimated dietary intake of micronutrients1 among Navajo Birth Cohort Study (NBCS) women. (a) Estimated nutrient intakes of NBCS cohort compared with a 1981 Navajo study. Mean nutrient intake values were used to calculate an intake ratio during pregnancy for NBCS cohort versus 1981 study by Butte et al. (NBCS/Butte). An intake ratio <1 indicates decrease in mean estimated intake. An intake ratio >1 indicates increased mean estimated intake. (b) Prevalence of inadequate intakes in the NBCS cohort for nutrients with an Estimated Average Requirement (EAR)2. (c) Sensitivity analysis based on daily prenatal vitamin intake by NBCS women. The multivitamin brand used by the majority of NBCS women was utilized to assess the percentage of NBCS women meeting the EAR for select micronutrients if a given proportion of NBCS women took this brand of multivitamin daily
3.3. High proportion of NBCS women have dietary intakes below recommended guidelines
Based on dietary intake alone, a high proportion of NBCS women (>50%) had inadequate intakes of calcium, folate, iron, magnesium, vitamin D, and vitamin E (Figure 1b). The proportion of participants with estimated intakes below the EAR did not differ significantly across subgroups stratified by age, body mass index, education level, household income, and food assistance program participation (Table S4). Vitamin D had the greatest proportion of women with inadequate intakes, followed by vitamin E. A slightly lower proportion of adolescent NBCS women (ages 14–18 years) had inadequate intakes of iron and vitamin D compared with older NBCS women. A high proportion of NBCS women reported prenatal vitamin intake (>90%), however our survey tool limited the ability to collect information on frequency of use. Because a majority of NBCS women reported using a specific brand of prenatal vitamins, we conducted a sensitivity analysis to assess the percentage of NBCS women meeting the EAR for select micronutrients if a given proportion of NBCS women took this brand of prenatal vitamin daily (Figure 1c). This analysis showed a substantial increase in the prevalence of adequate intake for vitamin D, folate, iron, and zinc among NBCS women with daily supplemental intake. The greatest effect of supplementation was on vitamin D, folate, and iron, indicated by the steep slopes for these nutrients (Figure 1c). Supplementation increased the prevalence of calcium and vitamin E adequacy, but to a much lesser extent compared with other nutrients. Even with 95% of NBCS women taking a daily prenatal vitamin, only 40% and 58% of NBCS women would achieve adequate vitamin E and calcium intake, respectively.
3.4. Urinary iodine concentrations indicate less than adequate iodine intake among NBCS women
The median urinary iodine (mUI) concentration for NBCS women was 90.8 μg/L (95% CI [80, 103.5 μg/L]; Figure 2), which indicates population‐level iodine insufficiency when compared with World Health Organization (WHO) sufficiency level of 150 μg/L. Additionally, the NBCS mUI was lower compared with pregnant women from several NHANES cycles (Figure 2). The mUI of NBCS FFQ participants was comparable with NBCS women overall.
Figure 2.
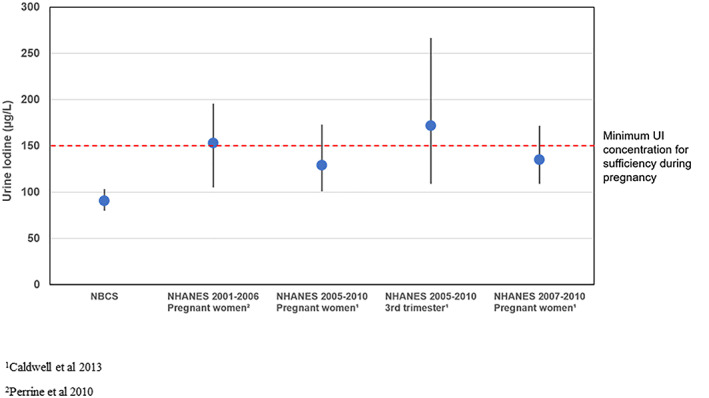
Median urinary iodine (median, interquartile range) for Navajo Birth Cohort Study (NBCS) and National Health and Nutrition Examination Survey (NHANES) groups. The dotted horizontal line indicates minimum urinary iodine (UI) concentration (150 μg/L) for sufficiency during pregnancy as defined by the World Health Organization. Spot urines were used to measure UI concentrations in NBCS and NHANES groups
3.5. Overall diet quality for NBCS women is similar to NHANES but differs for some components
Overall, average diet quality of NBCS women based on total HEI scores was similar to that reported for the general population of women of child‐bearing age and for pregnant women in NHANES (Table 2). However, there were notable differences among some of the individual components (Figure 3). NBCS women had diets lower in dairy, seafood/plant protein, and refined grains and higher in added sugar, whole fruit, total fruit, and whole grains, compared with women of child‐bearing age in NHANES. When compared with a subset of women in NHANES who were pregnant, NBCS women had higher added sugar intake. Both NBCS women and NHANES pregnant women had diets lower in seafood and plant protein.
Table 2.
Healthy Eating Index (HEI‐2015) scores for NBCS cohort and subsets of NHANES dietary data
| Mean (95% CI) | |||
|---|---|---|---|
| HEI component | NBCSa | NHANES womenb | NHANES pregnant womena |
| Total vegetables | 3.7 (3.4–4.0) | 3.4 (3.3, 3.5) | 3.9 (3.2, 4.7) |
| Greens and beans | 3.1 (2.5–3.7) | 3.4 (3.0, 3.7) | 4.0 (2.4, 5.0) |
| Total fruit | 5.0 (4.7–5.0)b | 2.8 (2.6, 3.1) | 4.5 (2.5, 5.0) |
| Whole fruit | 5.0 (5.0–5.0)b | 3.9 (3.6, 4.3) | 4.8 (3.1, 5.0) |
| Whole grains | 3.7 (3.4–4.1)b | 2.5 (2.3, 2.7) | 2.6 (1.7, 3.5) |
| Dairy | 5.4 (4.8–6.1) | 6.2 (5.9, 6.4) | 6.2 (5.1, 7.3) |
| Total protein from food | 5.0 (5.0–5.0) | 5.0 (5.0, 5.0) | 5.0 (4.7, 5.0) |
| Seafood and plant protein | 3.0 (2.4–3.5)b | 4.9 (4.5, 5.0) | 3.8 (2.3, 5.0) |
| Fatty acid ratio | 4.1 (3.7–4.5) | 4.5 (4.3, 4.7) | 4.2 (3.2, 5.3) |
| Sodium | 9.3 (8.9–6.9) | 4.0 (3.7, 4.3) | 3.4 (1.7, 5.1) |
| Refined grains | 7.3 (6.8–7.9)b | 5.8 (5.5, 6.1) | 5.9 (4.7, 7.1) |
| Saturated fat | 6.4 (5.9–6.8) | 6.0 (5.8, 6.3) | 5.8 (4.6, 6.9) |
| Added sugar | 1.4 (0.8–2.1)b , c | 5.8 (5.5, 6.0) | 6.0 (4.9, 7.1) |
| HEI‐2015 total score | 62.4 (60.7–64.0) | 58.2 (56.9, 59.4) | 60.2 (53.9, 65.1) |
Abbreviations: CI, confidence interval; NHANES, National Health and Nutrition Examination Survey; NBCS, Navajo Birth Cohort Study.
NBCS 2010–2016, women between the ages of 14 and 45 years, Harvard Service Food Frequency Questionnaire, N = 242.
NHANES 2011–2012 (N = 1,492) and NHANES 2013–2014 (N = 1,703), women between the ages of 14 and 45 years, 24‐hr dietary recall, Day 1.
NHANES 2011–2012 and NHANES 2013–2014 pregnant/lactating women between the ages of 14 and 45 years, 24‐hr dietary recall, Day 1, N = 105.
The 95% CIs of component score for NBCS and NHANES dataset of women aged 14–45 years do not overlap.
The 95% CIs of component score for NBCS and NHANES pregnant/lactating women aged 14–45 years do not overlap.
Figure 3.
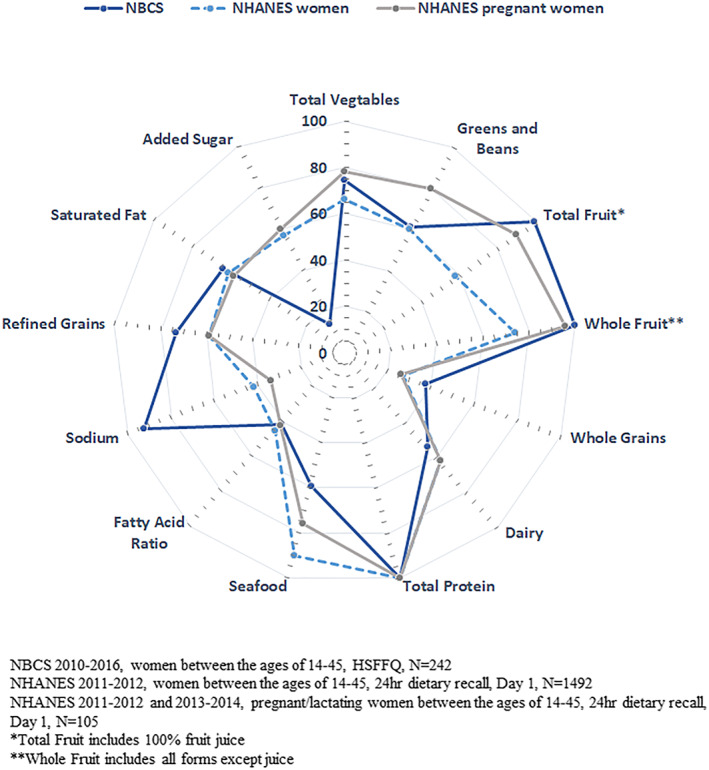
Radar plot of Healthy Eating Index‐2015 individual component scores for Navajo Birth Cohort Study (NBCS) and National Health and Nutrition Examination Survey (NHANES) groups. Each component point illustrates the percentage of total points received
3.6. Sugar‐sweetened beverages are a major contributor to added sugar in the NBCS maternal diet
Sugar‐sweetened beverages (SSBs) were the major contributor of added sugar in the diet of NBCS women, followed by sweets and cold cereals (Figure S2). Sweetened beverages alone contributed 30% of added sugar. The majority of NBCS women reported consuming SSBs, with only 3% indicating no consumption (Table S7). The median added sugar intake, as a percentage of TEI was 21.9%. Younger women (<26 years) reported a significantly higher intake of added sugar in their diets (23.4% of TEI), and the contribution of added sugar from fruit/sport beverages (16.7%) was greater compared with older women. Interestingly, dessert foods (sweets) contributed significantly more to added sugar in the diet for older women compared with younger women. Although not statistically significant, the contribution of added sugar from cold cereals was greater among women who reported not participating in food assistance programs.
4. DISCUSSION
To inform on‐going and new health strategies focused on improving Navajo maternal and fetal health, we evaluated dietary intake of micronutrients and diet quality among NBCS women. Compared with a previous study completed over 30 years ago, estimated micronutrient intake in NBCS women has remained similar or improved slightly, with the greatest gains noted for the B vitamins. This is likely due to folate initiatives and changes in access and intake of enriched and/or fortified foods (Crider, Bailey, & Berry, 2011). The March of Dimes recently partnered with programs in New Mexico and Arizona to promote folic acid intake. In 2011, the March of Dimes New Mexico Chapter collaborated with the New Mexico Department of Health and the Governor's Women's Health Office to raise awareness about birth defects prevention and the importance of folic acid by providing folic acid materials to area WIC clinics and family practice clinics (New Mexico Department of Health (NMDOH), Public Health Division, 2008). FFQ results from the present study suggest that more than 50% of participants had inadequate dietary intake of calcium, folate, iron, magnesium, vitamin D, and vitamin E. These intake estimates, however, do not include any additional intake from prenatal multivitamins. In an effort to expand our policy recommendations, we conducted a sensitivity analysis to assess if adequate intake would increase with daily prenatal vitamin use (Figure 1c). For the majority of micronutrients, including folate, vitamin D, iron, and zinc, regular supplementation is likely to result in a high prevalence of adequate nutrient intake in the current food environment. Access and education regarding prenatal vitamins would be essential for overcoming the majority of nutrient inadequacies. This analysis also revealed that daily supplementation would not increase adequacy for calcium and vitamin E to the same extent as other nutrients, with the prevalence of adequacy remaining <60% for these two nutrients. Efforts focused on nutrition education and access to calcium and vitamin E dense foods would likely be needed to overcome these inadequacies via dietary sources.
The low intake of some nutrients observed in NBCS women may warrant additional attention; this finding should be interpreted with caution, however, because the study design did not emphasize multivitamin intake. In general, the traditional Navajo diet limits dairy and seafood because these items are taboo (Kopp, 1986) and many Navajos are lactose intolerant (Ballew et al., 1997; Newcomer, Thomas, Mcgill, & Hofmann, 1977; Swagerty, Walling, & Klein, 2002). In other populations, these foods are important sources of micronutrients such as iodine, calcium, vitamin D, and others. Routine supplementation of calcium, vitamin D, and DHA/EPA may be prudent for Navajo women of child‐bearing age (Kaiser & Campbell, 2014) due to these dietary practices. Additionally, initiatives focused on increasing nutrition education and overall access to culturally relevant foods that are calcium, vitamin E, and iodine rich should be emphasized. Juniper ash, used in blue corn‐based dishes, is an example of a traditional Navajo food that can serve as a potential source for dietary calcium (Christensen, Sorenson, Hendricks, & Munger, 1998).
4.1. Opportunities to address iodine intake
Dairy and seafood are major sources of iodine. This study is the first to identify the potential for iodine insufficiency among Navajo women. NBCS women had inadequate intake of iodine, with a median urinary iodine concentration <150 μg/L, suggesting a risk of iodine deficiency. Iodine is important for child neurodevelopment and essential for the normal production of thyroid hormones (WHO, 2013). Iodine fortification of table salt in the United States was implemented in the 1920s in response to iodine insufficiency. Although not documented in the literature, there is a range of sentiments among Navajo communities towards iodized salt. Our 30 years of experience on the ground and extensive conversations with Navajo field staff indicates that iodized salt is not sold in the primary grocery store chain on Navajo Nation. Although iodized salt can be purchased at other locations, it is unclear if iodized salt is sought out and purchased by residents. Some NBCS women live in proximity to national chain grocery stores that do sell iodize salt; however, our study design does not enable an analysis of the proportion of NBCS women that are purchasing and using iodized salt at the dinner table.
Although pregnant women are at greater risk for iodine deficiency, iodine is not required in prenatal multivitamin supplements in the United States (Leung, Braverman, & Pearce, 2012). Brand name prenatal vitamins are increasingly including iodine; however, inconsistencies remain in iodine per daily dose across brands (Lee, Stagnaro‐Green, Mackay, Wong, & Pearce, 2017). NBCS enrolment surveys indicated a majority of NBCS women reported taking a prenatal multivitamin, however they predominately used a brand of prenatal vitamins that does not list iodine content on the product label (data not shown). Contrasting our findings in NBCS women, a separate survey conducted by the New Mexico Pregnancy Risk Assessment Monitoring System (PRAMS) program found a majority of Navajo mothers reported no multivitamin/folic acid vitamin use in the month prior to pregnancy (Navajo Epidemiology Center). Together these findings support the need for efforts emphasizing education and access to iodine containing multivitamins as a part of women's health care, with special attention during reproductive age years and pregnancy (Alexander et al., 2017). Our study also highlights knowledge gaps on iodine intake among Navajo women, barriers to taking iodine containing supplements, and Navajo experiences with previous iodine fortification efforts. The New Mexico PRAMS program in partnership with the Navajo PRAMS workgroup monitors health status, behaviours, and experiences of Navajo mothers that reside in New Mexico. Partnerships with the New Mexico and Navajo PRAMS programs would present opportunities to learn more about promotion and access to iodine containing multivitamins. The PRAMS program is also available in Arizona and Utah, states that extend into Navajo Nation. Collaboration between the three states on issues related to iodine could provide a comprehensive dataset that can be used to develop evidence‐based public health strategies that are feasible and culturally relevant for Navajo communities.
4.2. Overall diet quality
The diet quality of NBCS women, as measured by the HEI‐2015, was similar to that estimated for the general population of women of child‐bearing age and for a small subset of pregnant women in NHANES. NBCS women had diets lower in refined grains, dairy, and plant protein, slightly higher in fruit and whole grains, and much higher in added sugar compared with the general population of women of child‐bearing age in the United States.
Previous studies indicated lower than recommended intakes of fruits and vegetables among Navajo women (Ballew et al., 1997; Sharma et al., 2010), potentially related to fruit and vegetable access issues. However, NBCS women had HEI component scores for whole and total fruit that were both at the maximum score, and the total vegetable score was similar to that for women of child‐bearing age and pregnant women in NHANES. A high proportion of NBCS women participate in the WIC program, which encourages intake of fruits, vegetables, and whole grains with the food package that is offered (Schultz et al., 2015). In some settings, changes to the WIC food package over the last 10 years to emphasize these foods have positively influenced the local food environment (Havens, Martin, Yan, Dauser‐Forrest, & Ferris, 2012; Lu et al., 2016; Rose, O'Malley, Dunaway, & Bodor, 2014). Our findings suggest that health literacy programs such as the Navajo Fruit and Vegetable Program (FVRx), Healthy Navajo Stores Initiative, and other food access initiatives aimed at increasing fruit and vegetable intake and that access as part of a healthy diet may have had a positive impact on Navajo maternal dietary patterns.
Consumption of SSBs and increased calories from added sugar puts NBCS women at increased risk for cardiovascular and metabolic disease and their children at increased risk for childhood obesity, metabolic disease, and other adverse health outcomes (Azad et al., 2016; Grundt, Eide, Brantsaeter, Haugen, & Markestad, 2017; Grundt, Nakling, Eide, & Markestad, 2012). Almost all (99%) of the NBCS participants had added sugar intakes greater than current recommendations from the USDA and WHO (<10% TEI), and 63% of NBCS women had intakes at least double the current recommendations (U.S. Department of Health and Human Services and U.S. Department of Agriculture, 2015; WHO, 2015). Environmental issues, such as contaminated drinking water, and access to clean drinking water are on‐going public health issues on Navajo Nation that may also contribute to higher intake of SSBs in Navajo women (Corlin et al., 2016; Hoover, Coker, Barney, Shuey, & Lewis, 2018; Hoover, Gonzales, Shuey, Barney, & Lewis, 2017; Leeper, 2003; Lewis, Hoover, & MacKenzie, 2017). The ongoing “Water First!” project on Navajo Nation focuses on eliminating SSB consumption among children and increasing access to clean water, particularly in their earliest years of life. This effort should be expanded to reduce SSB consumption among women prior to, during, and after pregnancy and emphasize the benefits for maternal health.
The FFQ and HEI analyses also enabled evaluation of dietary sodium intake; however, FFQ questionnaires not designed for assessing sodium intake show poor correlation between estimated sodium intake and 24‐hr urinary measurements (McLean et al., 2017). Findings from the present study suggest the NBCS women had diets lower in sodium compared with both representative NHANES populations and previous studies among the Navajo general population that indicated high sodium intake (Basiotis, Lino, & Anand, 1999). This inconsistency may be explained by our FFQ not appropriately capturing sodium intake. For example, questions about discretionary salt use were not included, which is a common source of measurement error (McLean et al., 2017). Because our FFQ instrument was not designed to assess sodium intake specifically, we recommend additional investigations with a sodium‐focused FFQ or 24‐hr urinary measurements to understand sodium intake of pregnant Navajo women.
Almost three fourths of the NBCS women reported food assistance program participation; however, the sample size of our study did not allow for us to investigate differences in diet quality based on participation in various food assistance programs. The Federal Distribution Program on Indian Reservations (FDPIR) contributes an estimated 41–60% of the household food supply for an estimated 45% of households, indicating an important potential role for this program in supporting maternal diet quality on Navajo Nation (Pindus et al., 2016). Access to Supplemental Nutrition Assistance Program (SNAP) retailers can be challenging for Navajo Nation residents, and the FDPIR program was designed as a more accessible alternative to SNAP. FDPIR also provides nutrition education activities through small grants for individual nutrition counselling, group cooking demonstrations, and sharing healthy recipes with USDA foods. It is unclear to what extent that NBCS women participate in these activities or others of a similar nature via WIC and Head Start. Engaging tribal and federal stakeholders to integrate findings from this study into current nutrition education and food environment frameworks, such as increasing food access and developing culturally relevant healthy recipes, are key elements of an integrated intervention strategy for improving maternal diet quality (Gittelsohn, Kim, He, & Pardilla, 2013). Moreover, effective dietary‐based interventions focused on Navajo maternal nutrition should involve the social and family network of pregnant women, as well as, one‐on‐one case management with clinical staff (Cunningham‐Sabo et al., 2008; Nava, Zambrano, Arviso, Brochetti, & Becker, 2015). Focus groups have found that activities, such as a cooking class, conducted at the community are preferred and may increase participation and efficacy of interventions and result in transgenerational lifestyle changes (Cunningham‐Sabo et al., 2008). The NBCS cohort presents an opportunity to engage Navajo women in developing aspects of an integrated intervention strategy.
This study has a number of strengths, including a fairly large sample size and the use of a food frequency questionnaire that can provide important information on the maternal diet (Baer et al., 2005), and was adapted to include food items relevant to the target population. There are also some limitations. The dietary intake data were self‐reported and potentially subject to social desirability and recall bias. The response rate for FFQ and socio‐demographic information was lower than desired, but is not uncommon given the strained resources commonly found within medically underserved, rural hospitals (Genovesi, Hastings, Edgerton, & Olson, 2014). These challenges are amplified in neonatal units managing birthing complications and competing medical test needs (Vaught & Henderson, 2011). No differences in socio‐demographics were observed between the subset of NBCS women that completed FFQ surveys and those that did not, which suggests that this subset is representative of the general NBCS population. Additional biomarkers of micronutrient status were not available, and as a result, we could not estimate the prevalence of maternal micronutrient deficiencies.
5. CONCLUSION
This study provides a contemporary portrait of maternal diet quality on Navajo Nation and identifies a continued need for maternal health initiatives focused on creating an environment that promotes a healthy diet and adequate micronutrient intake during pregnancy.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of inetrest.
CONTRIBUTIONS
VYD wrote the initial manuscript, guided analyses; JH conducted FFQ intake analysis; NBCS team administered FFQ interviews and collected survey and demographic data; RD conducted HEI analysis and statistical testing, EYJ reviewed nutrition analyses and informed interpretation; JL made the conceptualization; JL and DM have oversight of NBCS. All authors reviewed and approved the final draft of the manuscript.
Supporting information
Table S1. IOM Estimated Average Requirement (EAR) for selected nutrients during pregnancy
Table S2. Estimated nutrient intakes from administered HSFFQ for NBCS cohort (N = 242), excluding supplements.
Table S3. Median (IQR) of estimated nutrient intakes from administered HSFFQ for NBCS cohort stratified by age, education, household income and education (N = 222)1.
Table S4. Percentage of NBCS cohort with estimated intakes from HSFFQ meeting EAR for selected nutrients stratified by age, education, food assistance program participation, income and BMI1.
Table S5: Test p value of the hypothesis that there is no difference in intakes (N = 222), between the stratified groups for age, education, food assistance program participation, household income or BMI.
Table S6: Test p value of the hypothesis that there is no difference in the proportion of women meeting EAR criteria (N = 222), between the stratified groups for age, education, food assistance program participation, household income or BMI1.
Table S7. Summary of added sugar intake from sweetened beverages
Figure S1. Map of Navajo Nation. Map shows enrollment of NBCS participants by chapter and the locations of the five Indian Health Service (IHS) hospitals involved in this study.
Figure S2. Major contributors to Added Sugar among NBCS women by A) age and B) food assistance program participation1
ACKNOWLEDGMENTS
The authors would like to acknowledge the tremendous efforts of the NBCS Study Team for administering FFQ surveys and engaging with NBCS participants. The NBCS Study team includes Qetarah Anderson*, Lorraine Barton, David Begay*, Delila Begay*, Francine Begay*, Mae‐Gilene Begay*, Nikki Begay*, Priscilla Begay*, Malcolm Benally*, Benita Brown*, Courtney Burnette, Miranda Cajero, Carla Chavez, Karen Cooper, LaShelly Crank*, Erica Dashner, Vanessa De La Rosa, Ruofei Du, Danielle Duarte, Esther Erdei, Adrienne Ettinger, Myra Francisco*, Joseph Hoover, Laurie Hudson, Lisa Kear, CJ Laselute*, Lynda Lasiloo, Ji‐Hyun Lee, Johnnye Lewis (PI), Li Luo, Debra MacKenzie, Chris Miller, Anita Muneta*, Teddy Nez*, Sara Nozadi, Elena O'Donald, Jennifer Ong, Tim Ozechowski, Bernadette Pacheco, Mallery Quetawki, Sandy Ramone*, Johnna Rogers*, Anna Rondon*, Diedra Sam*, Melissa Samuel*, Abigail Sanders*, Chris Shuey, Becky Smith, Charlotte Swindal, Marcia Tapaha*, Roxanne Thompson*, Doris Tsinnijinnie*, Monique Tsosie*, Shasity Tsosie*, Chris Vining*, Josephine Watson*, and Maria Welch* (* indicates a Navajo team member). Thank you to Vanessa Garcia with the UNM CTSC biochemical laboratory for her guidance on FFQ processing. We acknowledge the indigenous partners we worked with over the last three decades and from whom we learned about the lasting impact of the abandoned mines, with particular acknowledgement of those from Tachee/Blue Gap and Red Water Pond Road communities on Navajo, the 1,304 families in our original DiNEH Project, and the more than 750 families currently in the Navajo Birth Cohort Study. We also acknowledge the partnership of our research partners from Southwest Research and Information Center and their Navajo Home Environmental Assessment staff, Navajo Nation Department of Health including Mae‐Gilene Begay and the Community Health and Environmental Research Specialists, Navajo Nation Environmental Protection Agency, and faculty and staff from the University of New Mexico team, including Dr David Begay of Community Environmental Health Program for his support in understanding Navajo culture and tradition. Funding support was provided by the University of New Mexico Environmental Health Signatures Program and the Navajo Birth Cohort Study by U01 TS000135‐05, and training support provided by K12GM088021‐08 Academic Science Education and Research Training (ASERT) Program. Additional funding provided by Navajo Birth Cohort Study/ECHO UG3/UH3OD023344, NIH Office of the Director.
De La Rosa VY, Hoover J, Du R, et al. Diet quality among pregnant women in the Navajo Birth Cohort Study. Matern Child Nutr. 2020;16:e12961 10.1111/mcn.12961
REFERENCES
- Abu‐Saad, K. , & Fraser, D. (2010). Maternal nutrition and birth outcomes. Epidemiologic Reviews, 32, 5–25. 10.1093/epirev/mxq001 [DOI] [PubMed] [Google Scholar]
- Alexander, E. K. , Pearce, E. N. , Brent, G. A. , Brown, R. S. , Chen, H. , Dosiou, C. , … Sullivan, S. (2017). Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid, 27, 315–389. [DOI] [PubMed] [Google Scholar]
- Azad, M. B. , Sharma, A. K. , de Souza, R. J. , Dolinsky, V. W. , Becker, A. B. , Mandhane, P. J. , … Canadian Healthy Infant Longitudinal Development Study Investigators (2016). Association between artificially sweetened beverage consumption during pregnancy and infant body mass index. JAMA Pediatrics, 170(7), 662–670. 10.1001/jamapediatrics.2016.0301 [DOI] [PubMed] [Google Scholar]
- Baer, H. J. , Blum, R. E. , Rockett, H. R. H. , Leppert, J. , Gardner, J. D. , Suitor, C. W. , & Colditz, G. A. (2005). Use of a food frequency questionnaire in American Indian and Caucasian pregnant women: A validation study. BMC Public Health, 5, 135 10.1186/1471-2458-5-135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballew, C. , White, L. L. , Strauss, K. F. , Benson, L. J. , Mendlein, J. M. , & Mokdad, A. H. (1997). Intake of nutrients and food sources of nutrients among the Navajo: Findings from the Navajo Health and Nutrition Survey. The Journal of Nutrition, 127(10), 2085S–2093S. [DOI] [PubMed] [Google Scholar]
- Basiotis, P. P. , Lino, M. , & Anand, R. (1999). The diet quality of American Indians (pp. 1–2). USDA Center for Nutrition Policy and Promotion.
- Butte, N. F. , Calloway, D. H. , & Van Duzen, J. L. (1981). Nutritional assessment of pregnant and lactating Navajo women. The American Journal of Clinical Nutrition, 34(10), 2216–2228. 10.1093/ajcn/34.10.2216 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2011). Urine iodine and mercury by ICP‐DRC‐MS Laboratory Procedure Manual DLS 3002.1. Atlanta, GA: Centers for Disease Control and Prevention. [Google Scholar]
- Christensen, N.K. , Sorenson A.W., Hendricks, D.G. , Munger, R. (1998). Juniper ash as a source of calcium in the Navajo diet. Journal of the American Dietetic Association, 98(3), 333‐334. 10.1016/S0002-8223(98)00077‐7. [DOI] [PubMed] [Google Scholar]
- Corlin, L. , Rock, T. , Cordova, J. , Woodin, M. , Durant, J. L. , Gute, D. M. , … Brugge, D. (2016). Health effects and environmental justice concerns of exposure to uranium in drinking water. Current Environmental Health Reports, 3(4), 434–442. 10.1007/s40572-016-0114-z [DOI] [PubMed] [Google Scholar]
- Crider, K. S. , Bailey, L. B. , & Berry, R. J. (2011). Folic acid food fortification—Its history, effect, concerns, and future directions. Nutrients, 3(3), 370–384. 10.3390/nu3030370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham‐Sabo, L. , Bauer, M. , Pareo, S. , Phillips‐Benally, S. , Roanhorse, J. , & Garcia, L. (2008). Qualitative investigation of factors contributing to effective nutrition education for Navajo families. Maternal and Child Health Journal, 12(Suppl 1), 68–75. 10.1007/s10995-008-0333-5 [DOI] [PubMed] [Google Scholar]
- Feskanich, D. , Sielaff, B. H. , Chong, K. , & Buzzard, I. M. (1989). Computerized collection and analysis of dietary intake information. Computer Methods and Programs in Biomedicine, 30(1), 47–57. 10.1016/0169-2607(89)90122‐3 [DOI] [PubMed] [Google Scholar]
- Freedman, L. S. , Guenther, P. M. , Krebs‐Smith, S. M. , & Kott, P. S. (2008). A population's mean Healthy Eating Index‐2005 scores are best estimated by the score of the population ratio when one 24‐hour recall is available. The Journal of Nutrition, 138(9), 1725–1729. 10.1093/jn/138.9.1725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genovesi, A. , Hastings, B. , Edgerton, E. A. , & Olson, L. (2014). Pediatric emergency care capabilities of Indian Health Service emergency medical service agencies serving American Indians/Alaska Natives in rural and frontier areas. Rural and Remote Health, 14(2), 2688. [PubMed] [Google Scholar]
- Gittelsohn, J. , Kim, E. M. , He, S. , & Pardilla, M. (2013). A food store‐based environmental intervention is associated with reduced BMI and improved psychosocial factors and food‐related behaviors on the Navajo nation. The Journal of Nutrition, 143(9), 1494–1500. 10.3945/jn.112.165266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grundt, J. H. , Eide, G. E. , Brantsaeter, A. L. , Haugen, M. , & Markestad, T. (2017). Is consumption of sugar‐sweetened soft drinks during pregnancy associated with birth weight? Maternal & Child Nutrition, 13(4), e12405 10.1111/mcn.12405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grundt, J. H. , Nakling, J. , Eide, G. E. , & Markestad, T. (2012). Possible relation between maternal consumption of added sugar and sugar‐sweetened beverages and birth weight—Time trends in a population. BMC Public Health, 12(1), 901 10.1186/1471-2458-12-901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guenther, P. M. , Kirkpatrick, S. I. , Reedy, J. , Krebs‐Smith, S. M. , Buckman, D. W. , Dodd, K. W. , … Carroll, R. J. (2014). The Healthy Eating Index‐2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. The Journal of Nutrition, 144(3), 399–407. 10.3945/jn.113.183079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havens, E. K. , Martin, K. S. , Yan, J. , Dauser‐Forrest, D. , & Ferris, A. M. (2012). Federal nutrition program changes and healthy food availability. American Journal of Preventive Medicine, 43(4), 419–422. 10.1016/j.amepre.2012.06.009 [DOI] [PubMed] [Google Scholar]
- HealthyPeople.gov . (2019). Social determinants of health. Retrieved July 2, 2019 from http://www.healthypeople.gov/2020/topic s‐objectives/topic/social‐determinants‐health?topicid=39.
- Hoover, J. , Gonzales, M. , Shuey, C. , Barney, Y. , & Lewis, J. (2017). Elevated arsenic and uranium concentrations in unregulated water sources on the Navajo Nation, USA. Exposure & Health, 9(2), 113–124. 10.1007/s12403-016-0226-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoover, J. H. , Coker, E. , Barney, Y. , Shuey, C. , & Lewis, J. (2018). Spatial clustering of metal and metalloid mixtures in unregulated water sources on the Navajo Nation ‐ Arizona, New Mexico, and Utah, USA. The Science of the Total Environment, 633, 1667–1678. 10.1016/j.scitotenv.2018.02.288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter, C. M. , Lewis, J. , Peter, D. , Begay, M.‐G. , & Ragin‐Wilson, A. (2015). The Navajo Birth Cohort Study. Journal of Environmental Health, 78(2), 42–45. [PubMed] [Google Scholar]
- Institute of Medicine (US) (2000). Dietary Reference Intakes: Applications in Dietary Assessment. Washington (DC): National Academies Press (US) 10.17226/9956 [DOI] [PubMed] [Google Scholar]
- Kaiser, L. L. , & Campbell, C. (2014). Practice paper of the Academy of Nutrition and Dietetics: Nutrition and lifestyle for a healthy pregnancy outcome. The Academy of Nutrition and Dietetics. Retrieved from https://www.eatrightpro.org/~/media/eatrightpro%20files/practice/position%20and%20practice%20papers/practice%20papers/practice_paper_healthy_pregnancy.ashx [DOI] [PubMed]
- Kopp, J. (1986). Crosscultural contacts: Changes in the diet and nutrition of the Navajo Indians. American Indian Culture and Research, 10(4), 1–30. 10.17953/aicr.10.4.lr231316527r041j [DOI] [PubMed] [Google Scholar]
- Kumar, G. , Jim‐Martin, S. , Piltch, E. , Onufrak, S. , McNeil, C. , Adams, L. , … Curley, L. (2016). Healthful nutrition of foods in Navajo Nation stores: Availability and pricing. American Journal of Health Promotion: AJHP, 30(7), 501–510. 10.4278/ajhp.140821-QUAN-422 [DOI] [PubMed] [Google Scholar]
- Lee, S. , Stagnaro‐Green, A. , Mackay, D. , Wong, A. , & Pearce, E. (2017). Iodine contents in prenatal vitamins in the United States. Thyroid, 27(8), 1101–1102. 10.1089/thy.2017.0097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeper, J. W. (2003). Navajo Nation Plans for Their Water Future (pp. 21–30).
- Leung, A. , Braverman, L. , & Pearce, E. (2012). History of U.S. iodine fortification and supplementation. Nutrients, 4(11), 1740–1746. 10.3390/nu4111740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis, J. , Hoover, J. , & MacKenzie, D. (2017). Mining and environmental health disparities in native American communities. Current Environmental Health Reports, 4(2), 130–141. 10.1007/s40572-017-0140-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu, W. , McKyer, E. L. J. , Dowdy, D. , Evans, A. , Ory, M. , Hoelscher, D. M. , et al. (2016). Evaluating the influence of the revised Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) food allocation package on healthy food availability, accessibility, and affordability in Texas. Journal of the Academy of Nutrition and Dietetics, 116(2), 292–301. 10.1016/j.jand.2015.10.021 [DOI] [PubMed] [Google Scholar]
- MacDorman, M. F. (2011). Race and ethnic disparities in fetal mortality, preterm birth, and infant mortality in the United States: An overview. Seminars in Perinatology, 35(4), 200–208. 10.1053/j.semperi.2011.02.017 [DOI] [PubMed] [Google Scholar]
- MacDorman, M. F. , Kirmeyer, S. E. , & Wilson, E. C. (2012). Fetal and perinatal mortality, United States, 2006. National Vital Statistics Reports: From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System, 60(8), 1–22. [PubMed] [Google Scholar]
- McLean, R. M. , Farmer, V. L. , Nettleton, A. , Cameron, C. M. , Cook, N. R. , Campbell, N. R. C. , & TRUE Consortium (International Consortium for Quality Research on Dietary Sodium/Salt) (2017). Assessment of dietary sodium intake using a food frequency questionnaire and 24‐hour urinary sodium excretion: a systematic literature review. Journal of Clinical Hypertension (Greenwich, Conn.), 19(12), 1214–1230. 10.1111/jch.13148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, P. E. , Mitchell, D. C. , Harala, P. L. , Pettit, J. M. , Smiciklas‐Wright, H. , & Hartman, T. J. (2011). Development and evaluation of a method for calculating the Healthy Eating Index‐2005 using the Nutrition Data System for Research. Public Health Nutrition, 14(2), 306–313. 10.1017/S1368980010001655 [DOI] [PubMed] [Google Scholar]
- National Cancer Institute .(n.d.).The Health Eating Index: SAS code. Retrieved from https://epi.grants.cancer.gov/hei/sas-code.html. Updated August 29, 2017.
- Nava, L. T. , Zambrano, J. M. , Arviso, K. P. , Brochetti, D. , & Becker, K. L. (2015). Nutrition‐based interventions to address metabolic syndrome in the Navajo: A systematic review. Journal of Clinical Nursing, 24(21‐22), 3024–3045. 10.1111/jocn.12921 [DOI] [PubMed] [Google Scholar]
- Navajo Epidemiology Center (NEC), Navajo Department of Health , Report on New Mexico Navajo Mothers and Their Infants , 2005. ‐2011. Retrieved from www.nec.navajo-nsn.gov.
- New Mexico Department of Health (NMDOH), Public Health Division , Pregnancy Risk Assessment Monitoring System (PRAMS) Surveillance Report : 2008. Births with 2006‐2008 averages. Retrieved from https://nmhealth.org/data/view/maternal/1736/.
- Newcomer, A. , Thomas, P. , Mcgill, D. , & Hofmann, A. (1977). Lactase deficiency: A common genetic trait of the American Indian. Gastroenterology, 72(2), 234–237. [PubMed] [Google Scholar]
- Nnam, N. M. (2015). Improving maternal nutrition for better pregnancy outcomes. The Proceedings of the Nutrition Society, 74(4), 454–459. 10.1017/S0029665115002396 [DOI] [PubMed] [Google Scholar]
- Ojha, S. , Fainberg, H. P. , Sebert, S. , Budge, H. , & Symonds, M. E. (2015). Maternal health and eating habits: Metabolic consequences and impact on child health. Trends in Molecular Medicine, 21(2), 126–133. 10.1016/j.molmed.2014.12.005 [DOI] [PubMed] [Google Scholar]
- Pardilla, M. , Prasad, D. , Suratkar, S. , & Gittelsohn, J. (2013). High levels of household food insecurity on the Navajo Nation. Public Health Nutrition, 17(1), 58–65. 10.1017/S1368980012005630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pindus, N. M. , Hafford, C. , Levy, D. K. , Biess, J. , Simington, J. , Hedman, C. , & Smylie, J. (2016). Study of the Food Distribution Program on Indian Reservations (FDPIR) Final Report. Department of Agriculture Food and Nutrition Services: Urban Institute for the U.S. [Google Scholar]
- Rohner, F. , Zimmermann, M. , Jooste, P. , Pandav, C. , Caldwell, K. , Raghavan, R. , & Raiten, D. J. (2014). Biomarkers of nutrition for development—Iodine review. The Journal of Nutrition, 144(8), 1322S–1342S. 10.3945/jn.113.181974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose, D. , O'Malley, K. , Dunaway, L. F. , & Bodor, J. N. (2014). The influence of the WIC food package changes on the retail food environment in New Orleans. Journal of Nutrition Education and Behavior, 46(3 Suppl), S38–S44. 10.1016/j.jneb.2014.01.008 [DOI] [PubMed] [Google Scholar]
- Sarche, M. , & Spicer, P. (2008). Poverty and health disparities for American Indian and Alaska Native children: Current knowledge and future prospects. Annals of the New York Academy of Sciences, 1136, 126–136. 10.1196/annals.1425.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schakel, S. , Sievert, Y. , & Buzzard, I. (1988). Sources of data for developing and maintaining a nutrient database. Journal of the American Dietetic Association, 88(10), 1268–1271. [PubMed] [Google Scholar]
- Schakel, S. F. , Buzzard, I. M. , & Gebhardt, S. E. (1997). Procedures for estimating nutrient values for food composition databases. Journal of Food Composition and Analysis, 10(2), 102–114. 10.1006/jfca.1997.0527 [DOI] [Google Scholar]
- Schultz, D. J. , Byker Shanks, C. , & Houghtaling, B. (2015). The impact of the 2009 Special Supplemental Nutrition Program for Women, Infants, and Children food package revisions on participants: A systematic review. Journal of the Academy of Nutrition and Dietetics, 115(11), 1832–1846. 10.1016/j.jand.2015.06.381 [DOI] [PubMed] [Google Scholar]
- Sharma, S. , Yacavone, M. , Cao, X. , Pardilla, M. , Qi, M. , & Gittelsohn, J. (2010). Dietary intake and development of a quantitative FFQ for a nutritional intervention to reduce the risk of chronic disease in the Navajo Nation. Public Health Nutrition, 13(3), 350–359. 10.1017/S1368980009005266 [DOI] [PubMed] [Google Scholar]
- Sievert, Y. A. , Schakel, S. F. , & Buzzard, I. M. (1989). Maintenance of a nutrient database for clinical trials. Controlled Clinical Trials, 10(4), 416–425. 10.1016/0197-2456(89)90006-8 [DOI] [PubMed] [Google Scholar]
- Swagerty, D. L. Jr. , Walling, A. D. , & Klein, R. M. (2002). Lactose intolerance. American Family Physician, 65(9), 1845–1850. [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services and U.S. Department of Agriculture . (2015). Dietary guidelines for Americans 2015‐2020 (8 ed.). Retrieved from http://www.hhs.gov/civil-rights/for-providers/index.html
- Vaught, J. B. , & Henderson, M. K. (2011). Biological sample collection, processing, storage and information management. IARC Scientific Publications, 163, 23–42. [PubMed] [Google Scholar]
- Vintzileos, A. M. , Ananth, C. V. , Smulian, J. C. , Scorza, W. E. , & Knuppel, R. A. (2002). The impact of prenatal care on neonatal deaths in the presence and absence of antenatal high‐risk conditions. American Journal of Obstetrics and Gynecology, 186(5), 1011–1016. [DOI] [PubMed] [Google Scholar]
- WHO . (2013). Urinary iodine concentrations for determining iodine status in populations (pp. 1–5). Vitamin and Mineral Nutrition Information System. Geneva. Retrieved from http://www.who.int/nutrition/vmnis/indicators/urinaryiodine
- WHO (2015). Guideline: Sugars intake for adults and children. Geneva: World Health Organization. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. IOM Estimated Average Requirement (EAR) for selected nutrients during pregnancy
Table S2. Estimated nutrient intakes from administered HSFFQ for NBCS cohort (N = 242), excluding supplements.
Table S3. Median (IQR) of estimated nutrient intakes from administered HSFFQ for NBCS cohort stratified by age, education, household income and education (N = 222)1.
Table S4. Percentage of NBCS cohort with estimated intakes from HSFFQ meeting EAR for selected nutrients stratified by age, education, food assistance program participation, income and BMI1.
Table S5: Test p value of the hypothesis that there is no difference in intakes (N = 222), between the stratified groups for age, education, food assistance program participation, household income or BMI.
Table S6: Test p value of the hypothesis that there is no difference in the proportion of women meeting EAR criteria (N = 222), between the stratified groups for age, education, food assistance program participation, household income or BMI1.
Table S7. Summary of added sugar intake from sweetened beverages
Figure S1. Map of Navajo Nation. Map shows enrollment of NBCS participants by chapter and the locations of the five Indian Health Service (IHS) hospitals involved in this study.
Figure S2. Major contributors to Added Sugar among NBCS women by A) age and B) food assistance program participation1


