Abstract
This article describes the prospective changes and the fundamental values of the relationships between family doctors, patients and community according to an ethical‐social concept of medicine. New aspects of the organization of the activity and of the roles of family doctors are reported in order to build hypotheses pointing to a modern and efficient management of patients in the coming the post‐COVID era.
Keywords: COVID, family medicine
1. INTRODUCTION
In the last decade, family doctors (FD), mainly devoted to the management of elderly and multi‐morbid people, have become increasingly involved in managing patients under innovative therapy and by dealing with electronic health record systems providing faster connection with patients and other health workers. This new format of assistance, combined with administrative and new regulations, results in considerable innovation. In Italy, FD take care of over‐14 years old individuals and are mainly organized in small groups of physicians connected to a database network 1 , 2 covering care in a ratio of 77/100.000 inhabitants (specialists are 185.000 for all 60 million of Italians).
The SARS‐CoV‐2 pandemic arrival found the health systems of most countries unprepared and forced the Ministers of Health to assembly specific task forces to coordinate interventions, Italy included. Changes in the family medicine (FM) assistance were inevitable.
This article analyses the existing and the prospective changes of the fundamental values of the relationships between doctors, patients and society according to an ethical‐social concept of medicine. In short, we examine new aspects of the organization and roles of FM in order to build hypotheses for the management of patients in the coming future (Tables 1 and 2).
TABLE 1.
(A) Subjects requiring special attention by family doctors in the phase 2 of COVID pandemic; (B) Special measures to be applied
|
A Over‐70 y old people Patients with complex conditions:
Under‐70 y old subjects with:
|
|
B Promotion of voluntary mass vaccination against flu and pneumococcal pneumonia for all over‐50 y old subjects
|
TABLE 2.
Suggested procedures for the management and charge taking of non‐COVID patients by Italian primary care physicians in the phase 2 of COVID pandemic
|
Non‐deferrable patients (Acute conditions)
|
|
Patients with chronicity New forms of charge taking:
|
|
Fragile patients New forms of charge taking:
|
2. GENERAL REMARKS
As the COVID‐19 crisis appears and presses the whole medical system, both specialists, emergency and FD, are having to prioritize acute cares. 3 Accordingly, both primary care and hospital medicine had to work to determine what care must go on and what can be delayed, rescheduled, cancelled or performed remotely in order to protect physicians and patients and to find the best way to treat patients, COVID‐19 included. In this scenario, FD play a critical role in easing the burden on the acute‐care system by facilitating the early identification of cases and by helping to amplify the key messages to people.
In these days, the pressure of the working world aimed at reopening activities after the imposed lock‐down has put FD in the position to be potential providers of information on the epidemic to governors and public administrators by giving element of orientation and support for economic decisions (Table 1). The skills in the suspicion of disease and the role as a "sentinel" of the health status of the community represent a working system of great utility for the National Health Systems and the Governments in terms of actions to lessen the risk of pandemic by using systems of (tele)‐monitoring (Figure 1A). In this view, FD can usefully guide people towards specific intervention by means of communication strategies and active involvement in the education of the masses at all levels.
FIGURE 1.
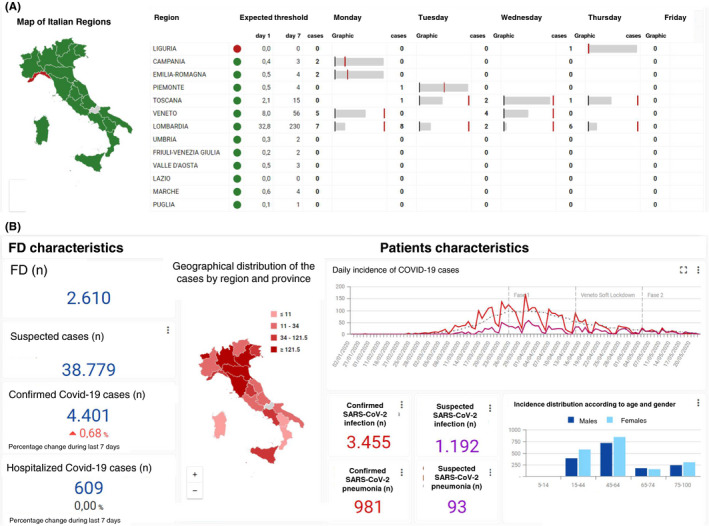
A, Monitoring activity for new COVID‐19 cases according to Italian regions (COVID Search). Green colour for regions with new patients below the estimated threshold (better trend) and red for those over such a threshold (worsening trend). The threshold is calculated by using the last available pseudo‐R and the number of new registered cases at the beginning of the week. The trend is obtained by comparing the daily threshold related with the number of days from the beginning of the week. B, Detailed report from COVID Search with specific data of all registered COVID‐19 patients including age, gender, number of suspected or confirmed cases, home management or hospitalization. FD, family doctors
Therefore, in the face of the COVID epidemic, the role of FDs is fundamental for monitoring the population in order to minimize the risk of infection (Table 1). A network organization of FD equipped with tools necessary for clinical governance may help to quantify and characterize individuals with clinical diagnosis of COVID‐19.
In Italy, every day, over 2600 FD caring near 4 billion people anonymously register all the Covid‐19 cases by a software integrated with the electronic medical record. These data work in support of a potential monitoring of epidemic outbreak and are of great interest for public health, scientific and political uses (Figure 1B). This network, named COVID Search, has the dual function to provide population data monitoring and being useful to the development of public health strategies and may serve as decision‐making to support physicians in their clinical and epidemiological surveillance with the final aim to contain the epidemic. 4
3. THE ROLE AND ACTIVITY OF FDS DURING PANDEMIC
In this scenario, the new vision of FM as the first building block of surveillance is a consequence of the attributed function of public health to FD since they interface with the individuals in their family and within social contexts. This role is consistent with what FD have done in the context of the Covid emergency often shifting the attention from an ad personam approach to a wide glance at the community to fulfil interaction tasks with other health figures (ie Prevention Department workers, Covid deputed hospitals). Working as a "sentinel," FD are aimed at getting to know the population and tackling emerging problems directly pointing to the heart of the society and the community.
How these changes are perceived from people and how do they will influence the doctor/patient relationship? Indeed, during this epidemic, FD have resumed the close relationship with the patients, but the general question regarding if and how his protection represents an objective limiting of his activity in front of a potential Covid patient asking for his visit remains a difficult to answer question.
One important ethical problem highlighted by the pandemic is the iniquity in the face of a non‐uniformity of welfare and health programmes among European countries: indeed, as a general principle, the right to health must be the same for all and cannot fail to take into consideration both the safety of the physicians and that of their assisted people. In addition, inequity has been noted in the management of FD’s activity. The unfairness that is invoked in the welfare organization is found in the event of disparities in the care models among European countries. 5 Another crucial and critical aspect regards the different collaborative models existing between primary care and the hospital, for the home care of paucisymptomatic COVID patients, as well as for the post‐hospitalization setting for stabilized but not yet healed patients.
4. THE CHANGING RELATIONSHIP BETWEEN FD AND PATIENTS
Since this is not the time anymore to bring in office relatively healthy patients for blood pressure check or for routine blood tests, a much better solutions are to be planned and, in general, one is to invite patients to get home monitor and transmit readings to doctors (Table 2) by the use of different electronic platform systems. This measure is inevitable; in fact, while before the epidemic, the relationship between doctors and patients was personal and confidential, now and in the future, the doctor will have an investigative role in history of contacts, in indoor and outdoor life habits, and therefore even more confidentiality is required. The need for creating a new patient medical report is configured. The first evaluation is made by telephone or audio‐visual tools, making the doctor and patient safe; next, the doctor will decide if it is enough to have a valid approach or does the patient needs a direct examination (at home or in the office). Telemedicine and the application of scores and scales of evaluation will be increasingly used. These points would entail a radical revision of the concept of "medical examination": the experience of these days is teaching us that the medical examination in our crowded offices, in many cases can be replaced in a way that is sometimes even more effective by the application of alternative forms of contact with patients and with an optimal use of resources. The traditional concept of "medical examination," intended as the necessary presence of the doctor and the patient in the same place, should be of course reviewed since it is frankly anachronistic and largely outdated by the facts. The application of artificial intelligence and the consequent use of telemedicine tools for remote detection or monitoring of biological parameters and clinical surveillance will replace the medical examination, thus creating an exclusively, albeit not exhaustively, virtual relationship. With the application of both telemedicine and online drug prescription, the range of patients’ distribution in the town may be even enlarged and the distance from the FD’s office increased.
5. NEW COMPETENCES FOR FD DURING A PANDEMIC
FD act in the balance between treatment and prevention, surveillance and monitoring, in the face of objective difficulties that are encountered in these settings.
Now, the Covid epidemic has reevaluated the position of the FD which is not only the doctor of chronicity but also, they must do active surveillance. Therefore, a reconfiguration of the FM also to define new ethical and deontological parameters is necessary, pointing to an unexplored identity. 6 , 7 FD are becoming not only the doctors of the person but also of the community and not only as a sentinel but also in a context of public health; that is they regain their role in community hospitals, no longer intended as an intermediate care structure for chronicity, but also a place where discharged patients who still need to stay before returning at home or in residency. In this coming new era, the two independent forms of assistance and care systems, hospital and primary care, are necessary called to a new coexistence through a progressive integration to refine new roles. This is particularly important for elderly and fragile patients (ie people with important disabilities and/or multiple chronicity with a significant reduction of autonomy) to whom the FD's approach should consider the different social and health situations: elderly patients living with a caregiver, patients who live alone or in a closed community with or without a family behind them. For all these different conditions, recommendations and engagements should be prepared differently and at least a part of them should actively involve FD.
Additional roles and competences for FD in such an emerging situation are to communicate and spread correct information, educational messages, preventive measures with authoritativeness and by discarding fake news.
6. THE POST‐ACUTE PHASE
The high and unacceptable number of lives lost among FD, who had to visit patients with bare hands and had to invent a role and assign themselves tasks, imposes drastic prevention measures, widespread dissemination of information and specific training (also for the office staff). In Italy, to date, the overall mortality from COVID is 13.5% with over 26,500 health workers infected, and 51 out of 150 deaths among doctors were FD.
Following the acute epidemic phase, FD should pay special attention to the return infections and post‐acute complications by acting with all the clinical and instrumental safeguard organization against the transmission of the infection from unknown carriers. Also moving to the stabilization phase, in which prevention will prevail, FD should encourage correct lifestyles and activate flu and pneumonia vaccination of the masses in view of the return of the colder months which are normally favouring flu viruses with possible new epidemic waves.
Valid prevention may be implemented by pointing to control systems and people surveillance. In this way, any early suspected patients will allow the opportunity to have a fast diagnosis, an early treatment and timely efficient application of isolation procedures, all efforts to be planned until an effective vaccine will be identified.
7. FINAL CONSIDERATIONS
The reconfiguration of the FM and the new roles covered by FD during the pandemic phase and for the post‐pandemic era must be designed yet, although many aspects have been forcedly carried out during the epidemic. However, several major points need to be taken into the account. One of them is how to face virtual medicine and virtual doctor? These are aspects of technological evolution that the pandemic has brought us to the fore, directly projecting the actual modern medicine into a post‐modern evolutionary medicine. This reconfigured medicine should never lose its natural connotation which contemplates that the doctor always visits his patient in a direct or artificial way. To avoid dehumanization of the relationship, these passages should be clearly explained and stated in order to be progressively accepted by the patient. 8 Some advantages, however, will appear and regard dematerialization of prescriptions, reduced bureaucratization and contacts with specialists by sharing medical records, thus producing facilitations for the patient.
New applied rules and deontological norms aiming at evaluating and managing these innovative concepts are mandatory in order to legally protect FD from these new visions of the work including the direct relationship between doctors and patients and between FD and specialists. 9 In this view, it remains fundamental that the value of managing innovation should not be managed by it, but by translating from simple to advanced technology, artificial intelligence should enable all these passages just working as a connecting role.
CONFLICT OF INTERESTS
The authors declare no conflict of interests.
Grattagliano I, Rossi A, Cricelli I, Cricelli C. The changing face of family medicine in the COVID and post‐COVID era. Eur J Clin Invest. 2020;50:e13303. 10.1111/eci.13303
REFERENCES
- 1. Filippi A, Vanuzzo D, Bignamini AA, et al. The database of Italian general practitioners allows a reliable determination of the prevalence of myocardial infarction. Ital Heart J. 2005;6:311‐314. [PubMed] [Google Scholar]
- 2. Cricelli C, Mazzaglia G, Samani F, et al. Prevalence estimates for chronic diseases in Italy: exploring the differences between self‐report and primary care databases. J Public Health Med. 2003;25:254‐257. [DOI] [PubMed] [Google Scholar]
- 3. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020;395(10223):507‐513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization (WHO) . Home care for patients with suspected novel coronavirus (2019‐nCoV) infection presenting with mild symptoms and management of contacts. Interim guidance. 2020 [updated January 2020]. https://www.who.int/publications‐detail/home‐care‐for‐patients‐with‐suspected‐novel‐coronavirus‐(2019‐nCoV)‐infection‐presenting‐with‐mild‐symptoms‐and‐management‐of‐contacts. Accessed May 22, 2020.
- 5. Greenhalgh T, Koh GCH, Car J. Covid‐ 19: a remote assessment in primary care. BMJ. 2020;368:m1182. [DOI] [PubMed] [Google Scholar]
- 6. Mash B. Primary care management of the coronavirus (COVID‐19). S Afr Fam Pract. 2020;62(1):a5115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gostin LO, Friedman EA, Wetter SA. Responding to COVID‐ 19: how to navigate a public health emergency legally and ethically. Hastings Cent Rep. 2020;50(2):8‐12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shankar M, et al. Humanism in telemedicine: connecting through virtual visits during the COVID‐19 pandemic. Ann Fam Med. 2020. (Covid Collection), April 14. [Google Scholar]
- 9. Ahmed S, Kelly YP, Behera TR, et al. Utility, appropriateness, and content of electronic consultations across medical subspecialties. Ann Intern Med. 2020;172(10):641‐647. [DOI] [PubMed] [Google Scholar]


