Abstract
Background
Cardiovascular disease related mortality is the leading cause of death in the United States, with hypertension being the most prevalent and potent risk factor. For decades hypertension has disproportionately affected African Americans, who also have a higher burden of associated comorbidities including diabetes and heart failure.
Methods
Current literature including guideline reports and newer studies on hypertension in African Americans in PubMed were reviewed. We also reviewed newer publications on the relationship between COVID-19 and cardiovascular disease.
Findings
While APOL1 has been theorized in the epidemiology of hypertension, the increased prevalence and associated risks are primarily due to environmental and lifestyle factors. These factors include poor diet, adverse lifestyle, and social determinants. Hypertension control can be achieved by lifestyle modifications such as low sodium diet, weight loss, and adequate physical activity. When lifestyle modifications alone do not adequately control hypertension, a common occurrence among African Americans who suffer with greater prevalence of resistant hypertension, pharmacological intervention is indicated. The efficacy of renal denervation, and the use of sodium-glucose cotransporter 2 and aminopeptidase A inhibitors, have been studied for treatment of resistant hypertension. Furthermore, the recent COVID-19 crisis has been particularly devastating among African Americans who demonstrate increased incidence and poorer health outcomes related to the disease.
Conclusion
The disparities in outcomes, which are largely attributable to a greater prevalence of comorbidities such as hypertension and obesity, in addition to adverse environmental and socioeconomic factors, highlight the necessity of specialized clinical approaches and programs for African Americans to address longstanding barriers to equitable care.
Keywords: Hypertension, African Americans, COVID-19
Introduction
Mortality related to cardiovascular disease (CVD) is the single leading cause of death in the United States (U.S.) and globally in high-income countries, accounting for 23.1% of all American deaths.1 Furthermore, hypertension (HTN), defined as systolic blood pressure of ≥130 mmHg and/or a diastolic blood pressure ≥80 mmHg is the most prevalent and potent CVD risk factor in the U.S., affecting 45.4% of the adults aged 18 or older in 2017–2018, up from 41.7% in 2013–2014.2 The most recent epidemiologic data confirm that diagnosed HTN is more prevalent among non-Hispanic blacks compared to non-Hispanic whites, with 57.2% of adult males and 56.7% of adult females.2 It has been established over multiple decades that HTN disproportionately affects African Americans, compared to whites, with increased CVD prevalence, prematurity and severity, poorer HTN control and increased burden of associated risk factors including diabetes, chronic kidney disease (CKD), physical inactivity, and overweight status and obesity.3 Unfortunately, despite advancements in risk factor identification and availability of effective HTN therapies, CVD disparities, including premature myocardial infarction, stroke, peripheral arterial disease, CKD, end-stage renal disease (ERSD) and heart failure, persist among African Americans compared to non-Hispanic whites.3 This review includes the most recent concepts on HTN in African Americans, including perspectives on casual factors, effective approaches and future considerations, especially in the COVID-19 pandemic era.
The black-white death gap
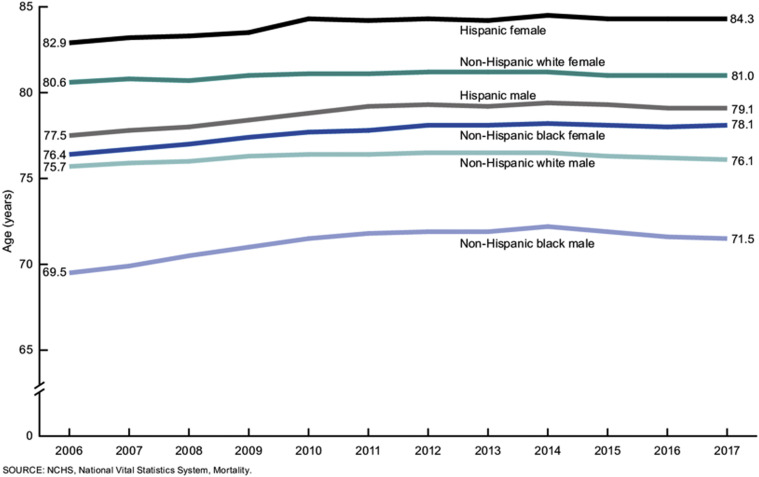
In consideration of the above, poorly controlled HTN markedly diminishes overall black life expectancy. Accordingly, in 2017, primarily driven by uncontrolled and more severe HTN, the life expectancy for white females was 81.0 years compared to 78.1 years for black females and 76.1 for white males versus 71.5 years for black males (Figure 1 ).4
Figure 1.
Life expectancy at birth, by race and sex: United States, 1970–2017. Source: CDC.gov
Although control of HTN represents the greatest opportunity for CVD prevention in African Americans, management of uncontrolled blood pressure (BP) is impeded by multiple factors, including delayed diagnosis, less access to insurance, primary and preventative care, and medication nonadherence.3 Many individuals for whom HTN medication is recommended are untreated or undiagnosed.5 Tools such as the American College of Cardiology/American Heart Association (ACC/AHA) Atherosclerotic Cardiovascular Disease (ASCVD) Risk Estimator can be used to assess an individual's 10-year risk of developing CVD, with added risk calculated for patients self-identified as black. However, despite having similar or even greater awareness and treatment, paradoxically blacks display lower HTN control rates (47.9% in blacks compared to 56% in whites).3 In addition, non-Hispanic blacks are more likely to be uninsured compared to non-Hispanic whites,6 and overall, uninsured adults are less likely to be aware of and treated for HTN and less likely to be controlled when treated compared to insured adults.5 As the prevalence of HTN increases, despite extensive available pharmacologic agents, in recent years U.S. control of HTN has plateaued, showing no improvement in non-Hispanic blacks, individuals aged 60 or greater, and individuals with other CVD risk factors.7
The impact of HTN, comorbid type 2 diabetes and heart failure
Cardiovascular and metabolic comorbidities are shown to have increased association with HTN and risk clustering has an increased prevalence in blacks. Common risk factors for both Type 2 diabetes (T2D) and HTN include overweight/obesity status, unhealthy diet, and physical inactivity.8 , 9 Recent data demonstrate that approximately 74% of adults with diabetes have comorbid hypertension.9 In African Americans, greater CVD morbidity and mortality is compounded by higher prevalence of T2D, increasing diseases including CKD, ESRD, stroke, and heart failure.10 The economic cost associated with the treatment and management of CVD in the U.S. was approximately $351.2 billion in 2014–2015, accounting for preventable costs of both healthcare and loss of productivity.10
Heart failure, which is predominantly due to HTN in blacks as opposed to coronary artery disease in whites, is the leading cause of hospitalization in the Medicare population.11 Hospital readmission costs, with associated Medicare reimbursement penalties in instances of ≤30-day readmission, are particularly problematic. The burden of heart failure provides an additional burden on the already strained healthcare system, further emphasizing the importance of HTN prevention, early intervention and control.12
Mortality rates from 1999 to 2017 related to heart failure were studied by Glynn et al.13 In comparison of heart-failure related death rates of adults aged 65–84 years, black men and black women showed a 1.43-fold and 1.54-fold increase respectively compared to white men and white women.13 Notably, prevalence of heart failure was markedly increased in younger black male adults13 and in younger adults aged 35–64; black men had 2.97-fold greater increase in death rate related to heart failure, consistent with other CVD complications occurring at an earlier age.13
Therefore, these trends of increasing HTN, T2D and other forms of CVD are particularly devastating in blacks. There are multiple causal factors for the increased prevalence and difficult to manage HTN, including unhealthy diet, suboptimal lifestyle, overall health inequity, adverse social environment, and potentially harmful cultural beliefs.14 , 15 Unfortunately, the persistent and unacceptable high prevalence of HTN and HTN-related complications in African Americans such as heart failure, are projected to increase in the future, especially in younger age groups.16
Current epidemiology
Recent data from the Jackson Heart Study and the Reasons for Geographic and Racial Differences in Stroke (REGARD) Study were analyzed, including 12,947 black participants, to assess the association of HTN and CVD. Authors of the study calculated the population-attributable risk and found that HTN contributes to 32.5% of CVD in black adults, specifically noting increased coincidence of coronary artery disease, stroke, and heart failure.17 In another recent study by Nambiar et al., age-adjusted mortality data were assessed to observe the correlation of HTN and CVD death rates. Their analysis demonstrated increased prevalence in mortality attributed to HTN. Therefore, underlying HTN portends an upward trend in CVD associated with HTN as a major public health concern.18 Moreover, the apparent current upward CVD mortality trend appears due to other CVD comorbidities, especially diabetes and obesity.13
Pathophysiology and genetic factors
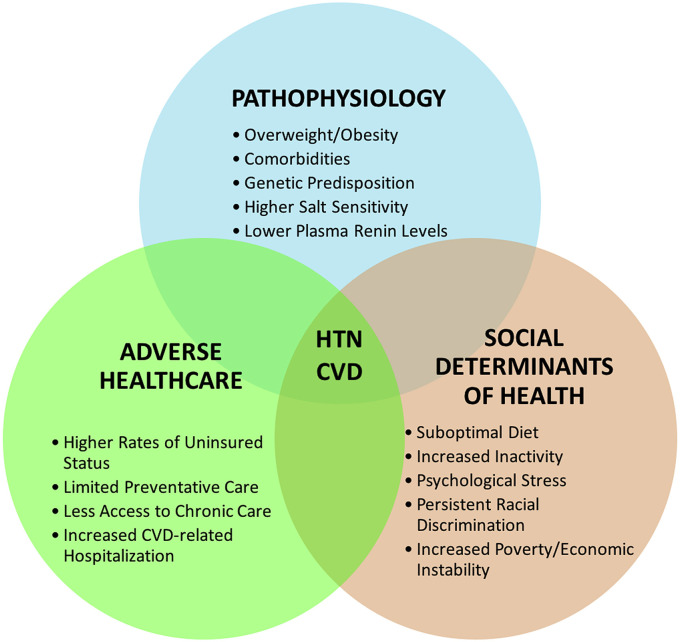
Several physiologic determinants are implicated for HTN in African Americans, including increased body mass index (BMI) and overweight/obesity status, higher salt sensitivity, low plasma renin levels, abnormal vascular function due to sympathetic overactivity, attenuated nocturnal decrease in BP, greater prevalence of comorbidities such as diabetes, physical inactivity, and positive family history (Figure 2 ).19 However, overall, the increased prevalence and risk of HTN is mainly due to environmental and lifestyle factors versus definitive genetic underpinnings.
Figure 2.
Factors affecting HTN/CVD morbidity and mortality.
Nevertheless, genetic factors have also been theorized to play a role in HTN-associated risk for CKD and ESRD. A meta-analysis was conducted to assess the association of HTN traits and APOL1 risk alleles, which are polymorphisms acquired for increased resistance against Trypanosoma brucei infections common in sub-Saharan Africa.20 Elevated systolic BP preceded decline in glomerular filtration rate and earlier onset of HTN occurred in individuals who were homozygous for the APOL1 variant alleles, indicating predisposition to HTN and CKD.20
Also, related to an emerging area of study, Dungu et al. described in blacks increased incidence of hereditary transthyretin amyloid cardiomyopathy, a genetic condition that caused by myocardial deposition amyloid of misfolded liver-produced transthyretin due to a mutation in TTR V122I.21 This mutation is not due to or associated with HTN, per se, but it is common across the African diaspora including Afro-Caribbean populations in the U.K. and variant alleles carried by up to 4% of African Americans.21 It is possible that the finding of increased heart failure incidence and mortality in blacks is affected by amyloid cardiomyopathy, especially in older black men and is unfortunately often misdiagnosed as HTN-related cardiomyopathy, delaying diagnosis and application or use of newer, potentially effective therapies.22
Social determinants of health and dietary factors
Beyond genetic factors, development of HTN and the CVD disparities that exist among African Americans are influenced by a variety of interconnected risk factors including poor diet, adverse lifestyle, deleterious environment and social determinants. According to the 2017 ACC/AHA and Multisociety Guidelines for the Prevention, Detection, Evaluation, and Management of High Blood Pressure, a diet lacking in fruits, vegetables, and whole grains and higher in sodium increases the risk for HTN and CVD.22 Commonly due to traditional cultural dietary preferences for a “southern diet” high in sodium, sugar, and fats, African Americans face unique challenges in implementing and adhering to current dietary recommendations.3 In REGARDS study data it was demonstrated that African Americans are more likely to consume a typical “southern diet” regardless of geographic location, and the highest incidence of stroke occurs among those with the lowest adherence to a recommended diet.3 In addition, African Americans have demonstrated increased time spent engaged in sedentary behavior compared to whites.3 African Americans, in general, are less likely to fulfill the ACC/AHA Primary Prevention Guideline recommended 150 min/wk of moderate intensity physical activity or 75 min/wk of high intensity physical activity.22
Overall, socioeconomic and environmental factors have an important influence on cardiovascular health. On average African Americans experience an increased rate of poverty (26%) compared to the general population (15%), leading to decreased access to preventative health resources such as availability of healthy foods and safe spaces for exercise.3 Additional psychological stressors such as income instability and coping with the effects of racial discrimination adversely affect and contribute to disparity in CVD outcomes (Figure 2).3 African Americans, who are less likely to be insured, are also at greater risk of uncontrolled and undiagnosed hypertension due to lack of access to preventative care such as screening tools and long-term management.7 , 22 Additionally, Ahmad et al. observed the correlation between poverty and heart failure outcomes and found that individuals with lower socioeconomic status experienced increased CVD-related hospitalization and mortality.23
Primary prevention and hypertension
According to ACC/AHA and Multisociety 2019 Guidelines on the Primary Prevention of Cardiovascular Disease, for hypertension (HTN), recommendations are concentrated on lifestyle modifications. These recommendations to prevent or delay HTN include weight loss, adequate physical activity, use of the Dietary Approaches to Stop Hypertension (DASH) diet, and reduced dietary sodium.24
By the release of free fatty acids, excess adipose tissue is associated with reduced arterial compliance secondary to insulin resistance. This metabolic state also has an inhibitory effect on nitric oxide production.25 Systematic reviews of randomized controlled trials have shown that a weight reduction of 1 kg correlates to an approximate 1 mmHg reduction in systolic blood pressure (SBP)26 and can improve HTN prevention and management by promoting the vasodilatory actions of nitric oxide.
Different types of physical activity have varying degrees of impact on blood pressure. However, aerobic exercise has been identified as the modality with the most significant impact on hypertension management. As few as 90 min of exercise per week can cause a 5–8 mmHg decrease in SBP. Aerobic exercise has been shown to dampen excess autonomic nervous system activity, which is a postulated mechanism for vascular dysfunction in African American patients.27
The DASH diet is the most widely evaluated dietary intervention for primary HTN across several patient populations, especially in African Americans. Consisting of lean protein sources, low fat dairy foods, fruits, and vegetables, the DASH diet is the only non-pharmacological intervention with results comparable to that of pharmacotherapy.28 , 29
Optimal approaches to pharmacotherapy
In patients for whom lifestyle modifications do not confer adequate blood pressure control, pharmacotherapy is indicated. For initial monotherapy, race and age are the primary clinical considerations when choosing a therapeutic agent. African American patients have consistently responded well to dihydropyridine calcium channel blockers (CCB) and/or thiazide-like diuretics as initial therapy. Patients with blood pressure that is 20/10 mmHg above target may be considered for combination therapy at treatment onset. For these patients, an angiotensin II receptor blocker (ARB) or angiotensin converting enzyme (ACE) inhibitor can be prescribed in conjunction with a CCB or thiazide-type diuretic. Given resistant hypertension (rHTN) is more common in African American patients, multidrug pharmacological therapy may be often indicated.19 , 30
Although this review focuses on HTN in African Americans, a recent publication provided insights on pharmacological approaches in native Africans. The Comparison of Three Combination Therapies in Lowering Blood Pressure in Black Africans (CREOLE) study evaluated two-drug combinations in sub-Saharan Africans. In 728 randomized patients, a regimen of amlodipine plus either hydrochlorothiazide or perindopril was more effective at reducing blood pressure at six months, compared with perindopril plus hydrochlorothiazide.31 The CREOLE results indicate CCB-based regimens are efficacious in black African hypertensive patients.
Community outreach and intervention
Community-based interventions, in addition to lifestyle modifications, may improve the control of HTN in the African American community. The success of these programs is based on identification and mitigation of the barriers to HTN control in African American patients and increasing health knowledge. Impediments to conventional medical and hypertensive care includes historical distrust of the healthcare system, lack of access to care, and inadequate communication between patients and providers. The goal of community level intervention has been to provide health information from a trusted source where attendance is certain. The National Medical Association and Association of Black Cardiologists, Inc. (ABC) have historically proposed various community-based approaches and continue to advocate community-based public health.32
Pioneers of community level interventions amongst African Americans include the late Elijah Saunders, MD and B. Waine Kong, PhD of Baltimore, Maryland. From 1979 to 1984, this team directed the Church/Community Health Awareness and Monitoring Program (CHAMP), in concert with the ABC. In this program, more than 500 parishioners representing 100 churches in the Baltimore area were trained to monitor their BP and make adequate transfers of care, empowering community members, and bringing healthcare to a persistently underserved area. Drs. Saunders and Kong began the initiative of using barbershops as BP control centers33 , 34 which has served as a model for subsequent community level efforts, especially in a difficult to reach cohort: African American men.
Moreover, in the 1990s, Daphne P. Ferdinand, PhD, RN and the lead author established the Healthy Heart Community Prevention Project, Inc. (HHCCP) in New Orleans, LA. The original HHCCP approach utilized a threefold approach involving hair salons and barbershops, churches, and large group meetings with healthcare professionals. The first initiative titled “Cut Your Pressure,” trained barbers and estheticians on how to measure blood pressures and counsel clients on lifestyle modifications. The second titled “Give God a Hand,” involved working with pastors to develop teachings that educated members on how to improve their cardiovascular risk profiles. Lastly, HHCCP hosted meetings to educate health professionals on best practices and advances in blood pressure management from a clinical standpoint.33 Interestingly, HHCCP remains active today (https://healthyheartcpp.org/) and includes education and outreach on diabetes and influenza immunization.
In 2018, a federally sponsored randomized trial confirmed a potent means of controlling HTN in African American men. The study used an interdisciplinary team bringing team-based care into black barber shops on the west coast. Over the course of six months, 319 participants represented in 52 barbershops in Los Angeles, CA underwent blood pressure screenings, lifestyle modification training, and pharmacological intervention when indicated. While the evidence-based pharmacotherapeutic intervention was led by clinical advance-trained pharmacists, the conversation surrounding health interventions were driven by the barbers. At the end of the study, there was a 27.0 mmHg mean reduction in systolic blood pressure from baseline of 152.8 mmHg.35 The success of the study is attributable to three key components: collaborative care delivery, effective anti-hypertensive therapy, and a trusted place of intervention.
Resistant hypertension
By definition, resistant hypertension (rHTN) is the inability to meet blood pressure goals despite aggressive medical treatment with three or more medications.14 , 36 With a higher prevalence in African Americans, fluid retention, high dietary sodium intake and excess aldosterone are major mechanisms. Current evidence-based guidelines suggest a three-step regimen. First, lifestyle modifications and an adequate three drug regimen including a CCB, and thiazide-type diuretic and an ACE inhibitor or ARB. Secondly, replacing hydrochlorothiazide with a thiazide-type diuretic (specifically indapamide or chlorthalidone) with loop diuretics depending on the patient's kidney function. Lastly, adding a mineralocorticoid receptor antagonist like spironolactone or eplerenone is often effective to control difficult to treat HTN patients.
Many clinicians have opted for clonidine in the setting of rHTN due to its rapid onset of action. The Resistant Hypertension Optimal Treatment (ReHOT) study randomized study performed in Brazil confirmed the superior efficacy and ease of use of spironolactone to that of clonidine. As a fourth line treatment, aldosterone antagonists, including spironolactone and eplerenone, are effective and better tolerated than clonidine.36 There is a present consensus that clonidine is an antiquated therapy with adverse side effects not conducive for long term use and aldosterone antagonists, depending on adequate renal function, are the ideal fourth line pharmacological therapy for patients with rHTN, including African Americans.
Increased COVID-19 mortality in African Americans and hypertension
Tragically, COVID-19 mortality is disproportionately high in African Americans with blacks representing 27.5% of all cases nationally despite comprising 13.4% of the population.37 , 38 In fact, in the May 2020 Center for Disease Control and Prevention (CDC) report that surveyed race/ethnicity among COVID-19 cases demonstrated that incidence is increased among non-Hispanic blacks who represent 36.8% of newly reported cases.39 In Louisiana, in May 2020, blacks who represent 32.7% of the population comprised 57.40% of COVID-19 related deaths throughout the state.40 Increased COVID-19 mortality and complications occur with greater incidence in individuals for whom certain comorbidities are pre-existent. Among these conditions is HTN (58.9%), obesity (49.8%), diabetes/metabolic disease (41.5%), and CVD (34.5%), comorbidities that are more prevalent in African Americans.39
While special considerations regarding treatment approaches in hypertensive COVID-19 patients are unproven and presently under review, there is some suggestion that ACEIs and ARBs upregulate ACE2 receptors where the coronavirus enters tissue, including pneumocytes.41 Nevertheless, recent clinical cohort data do not show that the ACE inhibitors and ARBs have deleterious effects with COVID-19 mortality. Importantly, a collaboration of the Heart Failure Society of American (HFSA) and ACC/AHA released a statement in March 2020 recommending against discontinuation of ACEI and ARBs.42 However, there is no postulated issue with use of CCBs and possible adverse effects on COVID-19.43
Therefore, CCBs may be an alternative if no compelling indications, such as heart failure, post-myocardial infarction status or CKD, and in addition to thiazide-type diuretics, in recent guidelines, remain optimal first-line treatments in African Americans.41 However, current evidence-based medical therapy confirms, regardless of race, with compelling indications, ACEI and ARBS should be a component of a CVD reduction and HTN regimen.
Certainly, social determinants have a profound impact on the risk and mortality related to COVID-19. African Americans are more likely to reside in densely populated areas and, thus encounter greater challenge with adherence to social distancing guidelines, and are more likely to have employment in essential service jobs that cannot be performed remotely, thus increasing risk of exposure.44 Additionally, African Americans are less likely to have access to financial resources in the event of a health emergency or economic disruption. Notably, blacks and other people of color are neither genetically nor biologically predisposed to COVID-19, but these social factors do contribute to increased risk of coronavirus exposure.44
Comorbid conditions such as HTN, T2D, and obesity contribute to greater mortality risk of COVID-19 and poorer prognosis upon development of the disease. The emergence of COVID-19 as a global health crisis is an opportunity to address longstanding disparities and underlying structural factors that have been well-documented to contribute to poorer overall health outcomes among African Americans.44 Furthermore, regarding these inequities, specific approaches to identify discrimination and racial/ethnic variations in testing and treatment are essential to minimize COVID-19 mortality among blacks.44
One of the unintended outcomes of the COVID-19 pandemic is the increase of virtual and phone consultations with providers. Although not studied in an African American cohort, a recent European report suggested smart technology with electronic home BP monitoring may yield similar percentages of patients with controlled HTN compared with the standard of care.45 Especially with conditions such as HTN and T2D that require continued monitoring, telemedicine may assist with risk factor control and provide access to critical medication refills. With COVID-19 and under new Medicare provisions, physicians and other providers can now receive greater reimbursement when collaborating with patients to monitor BP at home.46 In the U.S., this approach may be necessary and beneficial in monitoring hypertension in blacks and other minorities going forward.
Future directions in hypertension control
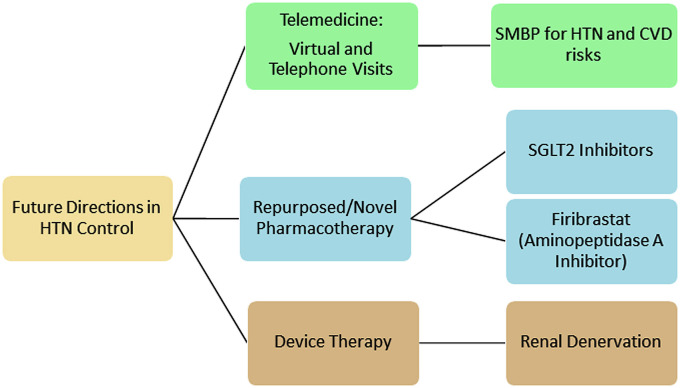
Although still investigational, renal denervation is a growing area of study as a treatment option for HTN. A recent study has shown the benefit of this method using the SPYRAL catheter. Participants were randomly assigned to one of two groups: renal denervation with a SPYRAL catheter and sham, and blacks comprised a significant number of both groups. While ambulatory blood pressure changes were modest, there was a significant improvement in office blood pressure measurements. Specifically, without medications, in the denervation group there was a 9.2 mmHg reduction in SBP and 5.1 mmHg in diastolic blood pressure (DBP).47 Given the significant representation of African Americans in this study, future consideration may be given to renal denervation as a reasonable treatment strategy for HTN not well controlled with pharmacotherapy (Figure 3 ).
Figure 3.
Future directions in HTN and CVD risk control. SMBP-Self monitoring blood pressure. HTN-Hypertension. CVD-Cardiovascular disease. SGLT2-Sodium glucose cotransporter 2.
As previously noted, one comorbidity commonly associated with rHTN is T2D.48 Sodium-glucose cotransporter 2 (SGLT2) inhibitors are hypoglycemic agents that reduce blood glucose by increasing the excretion of glucose in urine. Beyond their clinically approved use in T2D treatment, SGLT2 inhibitors have been shown to be cardioprotective, although the mechanisms are still unclear. Some suggested mechanisms include diuresis, sympathetic nervous system attenuation, and increasing the release of nitric oxide.49 While multiple cardiovascular and renal outcome studies show clinical benefit for the use of SGLT2 inhibitors to improve multiple conditions. Unfortunately, in the multiple major trials, black patients were under-represented and conventionally approximately 5% or less blacks in major studies composed the treatment and placebo groups, respectively.
The Antihyperglycemic and Blood Pressure Effects of Empagliflozin in African Americans with T2D and HTN was a recent study sought to account for this disparity. In this study of 150 self-identified blacks, with a mean age of 56.8 and longstanding T2D and HTN. Notably the treatment group showed a stepwise reduction in SBP at the 12-week (−5.8 mmHg) and 24-week (−8.39 mmHg) points, suggesting a need for extended use for maximum therapeutic impact. With comparable results to treatment with a single anti-hypertensive medication, SGLT2 inhibitors should be further studied for consideration in the treatment of rHTN.50
A novel, investigational approach to HTN management would be firibrastat, a therapeutic agent that acts on the renin angiotensin system (RAS) of the brain. In this system, angiotensin III activity on the AT1 receptor is associated with elevated BP due to increased ADH secretion.51 The Novel Evaluation with QGC001 in Hypertensive Overweight Patients of Multiple Ethnic Origins (NEW-HOPE) study investigated the efficacy of firibrastat, an aminopeptidase inhibitor, in a group with over 50% minority participants. At the end of the treatment period, firibrastat caused a mean reduction of 9.5 mmHg in SBP and 4.2 mmHg DBP.14 Firibrastat, after further evaluation, may be a future direction for pharmacological therapy in the rHTN population.
Fueled partly by the COVID-19 crisis and the disruption of in-person conventional outpatient care, regardless of emerging and future developments in HTN treatment, the use of in-home or self-monitoring BP measurements to confirm hypertension diagnosis and to monitor HTN control will increase in the future. Clinicians and their staff will continue to be reimbursed for telemedicine, including teaching patients to take accurate BP measurements as self-measured blood pressure (SMBP). The virtual visit to evaluate SMBP will empower patients to accurately measure their BP at home to improve BP control (Figure 3). One recently launched website (www.Validatebp.org) offers clinicians and their patients a list of home BP monitors which are certified for appropriate validity for accurate BP readings.52 The SMBP model has been embraced by Medicare services for payment and it is expected that private health plans will continue to increase support of this approach.
Conclusion
In African Americans, HTN is the most significant contributor to the increasing CVD burden and mortality. Unfortunately, the number of deaths in which HTN was a factor has steadily increased over the past decade.18 African Americans have the highest prevalence of HTN in the U.S., which is often poorly managed. HTN in blacks is burdened by clinical inertia, in which despite unacceptably high BP, clinicians make no changes or intensification of pharmacotherapy. Even when patients have access to care, providers often fail to increase pharmacotherapy in accordance with treatment guidelines, placing patients at risk for adverse CVD outcomes. A meta-analysis found that a combination of regular blood pressure monitoring, patient education, and provider training concerning implicit bias improved BP control.53 Physicians and other providers seeking to alleviate this disparity must improve communication and strengthen the provider-patient relationship. This should include culturally-sensitive, literacy-level appropriate communication, using models, web-based and printed materials to explain the patient's condition and treatment plans.
It is unacceptable that for decades, the American healthcare system has failed African Americans and other minority communities in both primary and secondary CVD prevention. It is essential in this present pandemic and in the future that clinicians ensure continuation of CVD medications including anti-hypertensives, antiplatelets and anticoagulation medications, statins and other lipid-modifying agents, and if possible, prescribe 90-day supplies with sufficient refills.
The higher COVID-19 African American mortality is a sentinel event. Similar to hospital sentinel events which are harbingers of poor-quality in-patient care, such as wrong-site surgeries and falls, the higher black pandemic deaths place a harsh spotlight on their longstanding higher mortality and diminished longevity.44 Beyond the conventional clinical setting, specific programs are needed to help patients overcome barriers to care, access appropriate lifestyle interventions, utilize pharmacotherapy, and offer health education to achieve health equity and overcome structural bias.
Disclosures
Research grants: Boehringer Ingelheim, Daichii-Sankyo, Novartis, Lilly, Invasc, Forest. Stocks – none. Patents – none. Consultant/Speaking: AstraZeneca, Daiichi Sankyo, Novartis, Forest, Roche, Sanofi.
References
- 1.Heron, M. Deaths: Leading Causes for 2017. National Vital Statistics Reports. vol. 68(6). Hyattsville, MD: National Center for Health Statistics. [PubMed]
- 2.Ostchega Y., Fryar C.D., Nwankwo T., Nguyen D.T. National Center for Health Statistics; Hyattsville, MD: 2020. Hypertension Prevalence Among Adults Aged 18 and over: United States, 2017-2018. NCHS Data Brief, No 364. [PubMed] [Google Scholar]
- 3.Carnethon M.R., Pu J., Howard G. Cardiovascular health in African Americans: a scientific statement from the American heart association. Circulation. 2017;136(21):e393–e423. doi: 10.1161/cir.0000000000000534. [DOI] [PubMed] [Google Scholar]
- 4.Kochanek K.D., Murphy S.L., Xu J., Arias E. vol. 68. National Center for Health Statistics; Hyattsville, MD: 2019. (Deaths: Final data for 2017). National Vital Statistics Reports. [PubMed] [Google Scholar]
- 5.Egan B.M., Li J., Small J., Nietert P.J., Sinopoli A. The growing gap in hypertension control between insured and uninsured adults: National Health and Nutrition Examination survey 1988 to 2010. Hypertension. 2014;64:997–1004. doi: 10.1161/HYPERTENSIONAHA.114.04276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Estimated hypertension, treatment, and control among U.S. Adults. Million hearts. https://millionhearts.hhs.gov/data-reports/hypertension-prevalence.html. Accessed 7 April 2020.
- 7.Dorans K.S., Mills K.T., Liu Y., He J. Trends in prevalence and control of hypertension according to the 2017 American College of Cardiology/American heart association (ACC/AHA) guideline. J Am Heart Assoc. 2018;7 doi: 10.1161/JAHA.118.008888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention . Centers for Disease Control and Prevention; 2020. Diabetes Risk Factors.https://www.cdc.gov/diabetes/basics/risk-factors.html [Google Scholar]
- 9.Passarella P., Kiseleva T.A., Valeeva Gosmanov F.V. Hypertension management in diabetes: 2018 update. Diabetes Spectr. 2018;31:218–224. doi: 10.2337/ds17-008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benjamin E.J., Muntner P., Alonso A. Heart disease and stroke statistics—2019 update: a report from the American heart association. Circulation. 2019;139 doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 11.Heart disease in African Americans. https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=19. Accessed 14 May 2020.
- 12.Psotka M.A., Fonarow G.C., Allen L.A. The hospital readmissions reduction program. JACC (J Am Coll Cardiol): Heart Fail. 2020;8:1–11. doi: 10.1016/j.jchf.2019.07.012. [DOI] [PubMed] [Google Scholar]
- 13.Glynn P., Lloyd-Jones D.M., Feinstein M.J., Carnethon M., Khan S.S. Disparities in cardiovascular mortality related to heart failure in the United States. J Am Coll Cardiol. 2019;73:2354–2355. doi: 10.1016/j.jacc.2019.02.042. [DOI] [PubMed] [Google Scholar]
- 14.Ferdinand K.C., Harrison D., Johnson A. The NEW-HOPE study and emerging therapies for difficult-to-control and resistant hypertension. Prog Cardiovasc Dis. 2020;63:64–73. doi: 10.1016/j.pcad.2019.12.008. [DOI] [PubMed] [Google Scholar]
- 15.Smedley B.D., Stith A.Y., Nelson A.R. National Academy Press; Washington, D.C.: 2003. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. [PubMed] [Google Scholar]
- 16.Ritchey M.D., Wall H.K., George M.G., Wright J.S. US trends in premature heart disease mortality over the past 50 years: where do we go from here? Trends Cardiovasc Med. 2019 doi: 10.1016/j.tcm.2019.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clark D., Colantonio L.D., Min Y.-I. Population-attributable risk for cardiovascular disease associated with hypertension in black adults. JAMA Cardiol. 2019;4(12):1194. doi: 10.1001/jamacardio.2019.3773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nambiar L., Lewinter M.M., Vanburen P.C., Dauerman H.L. Decade long temporal trends in U.S. Hypertension related cardiovascular mortality. J Am Coll Cardiol. 2020;1097:34531–34539. doi: 10.1016/j.jacc.2020.03.009. [DOI] [PubMed] [Google Scholar]
- 19.Ferdinand K.C., Nasser S.A. Management of essential hypertension. Cardiol Clin. 2017;35:231–246. doi: 10.1016/j.ccl.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 20.Nadkarni G.N., Galarneau G., Ellis S.B. Apolipoprotein L1 variants and blood pressure traits in African Americans. J Am Coll Cardiol. 2017;69:1564–1574. doi: 10.1016/j.jacc.2017.01.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dungu J.N., Papadopoulou S.A., Wykes K. Afro-caribbean heart failure in the United Kingdom: cause, outcomes, and ATTR V122I cardiac amyloidosis. Circulation: Heart Fail. 2016;9 doi: 10.1161/CIRCHEARTFAILURE.116.003352. [DOI] [PubMed] [Google Scholar]
- 22.Whelton P.K., Carey R.M., Aronow W.S. ACC/AHA/AAPA/ABC/ACPM/AGS/APHA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol. 2018;71:e127–e248. doi: 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 23.Ahmad K., Chen E.W., Nazir U. Regional variation in the association of poverty and heart failure mortality in the 3135 Counties of the United States. J Am Heart Assoc. 2019;8 doi: 10.1161/JAHA.119.012422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arnett D.K., Blumenthal R.S., Albert M.A. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American heart association task force on clinical practice guidelines. Circulation. 2019;140 doi: 10.1161/CIR.0000000000000678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fantin F., Giani A., Zoico E., Rossi A.P., Mazzali G., Zamboni M. Weight loss and hypertension in obese subjects. Nutrients. 2019;11:1667. doi: 10.3390/nu11071667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cohen J.B., Gadde K.M. Weight loss medications in the treatment of obesity and hypertension. Curr Hypertens Rep. 2019;21:16. doi: 10.1007/s11906-019-0915-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hill L.K., Thayer J.F. The autonomic nervous system and hypertension: ethnic Differences and psychosocial factors. Curr Cardiol Rep. 2019;21 doi: 10.1007/s11886-019-1100-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Virani S.S., Alonso A., Benjamin E.J. Heart disease and stroke statistics-2020 update: a report from the American heart association. Circulation. 2020;141:e139–e596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 29.Maris S.A., Williams J.S., Sun B., Brown S., Mitchell G.F., Conlin P.R. Interactions of the DASH diet with the renin-angiotensin-aldosterone system. Curr Develop Nutr. 2019;3 doi: 10.1093/cdn/nzz091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Egan, BM. Treatment of hypertension in black patients. https://www.uptodate.com/contents/treatment-of-hypertension-in-black-patients. Accessed 5 April 2020.
- 31.Ojji D.B. Comparison of dual therapies for lowering blood pressure in black Africans. N Engl J Med. 2019;380:2429–2439. doi: 10.1056/NEJMc1909844. [DOI] [PubMed] [Google Scholar]
- 32.Ofili E., Schanberg L., Hutchinson B. The association of black Cardiologists (ABC) cardiovascular implementation study (CVIS): a Research registry integrating social determinants to support care for underserved patients. Int J Environ Res Publ Health. 2019;16:1631. doi: 10.3390/ijerph16091631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ferdinand D.P., Nedunchezhian S., Ferdinand K.C. Hypertension in African Americans: advances in community outreach and public health approaches. Prog Cardiovasc Dis. 2020;63:40–45. doi: 10.1016/j.pcad.2019.12.005. [DOI] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention . U.S. Department of Health and Human Services; Atlanta: 2010. A Closer Look at African American Men and High Blood Pressure Control: A Review of Psychosocial Factors and Systems-Level Interventions. [Google Scholar]
- 35.Victor R.G., Lynch K., Li N. A cluster-randomized trial of blood-pressure reduction in black barbershops. N Engl J Med. 2018;378:1291–1301. doi: 10.1056/nejmoa1717250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Krieger E.M., Drager L.F., Giorgi D.M. Spironolactone versus clonidine as a fourth-drug therapy for resistant hypertension. Hypertension. 2018;71:681–690. doi: 10.1161/hypertensionaha.117.10662. [DOI] [PubMed] [Google Scholar]
- 37.Cases of coronavirus disease (COVID-19) in the U.S. Centers for disease control and prevention. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html Accessed 11 May 2020.
- 38.United States Census Bureau Quick Facts. https://www.census.gov/quickfacts/fact/table/US/PST045218. Accessed 14 May 2020.
- 39.COVIDView: Weekly Surveillance of U.S. COVID-19 activity. https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covidview/index.html Accessed 11 May 2020.
- 40.Additional data on COVID-19 death in Louisiana. Louisiana Department of health. http://ldh.la.gov/coronavirus/. Accessed 11 May 2020.
- 41.Fang L., Karakiulakis G., Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? The Lancet Respir Med. 2020;8:e21. doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.HFSA/ACC/AHA statement Addresses concerns Re: using RAAS antagonists in COVID-19. https://www.acc.org/latest-in-cardiology/articles/2020/03/17/08/59/hfsa-acc-aha-statement-addresses-concerns-re-using-raas-antagonists-in-covid-19. Accessed 14 May 2020. [DOI] [PMC free article] [PubMed]
- 43.Solaimanzadeh, I. Nifedipine and Amlodipine Are Associated With Improved Mortality and Decreased Risk for Intubation and Mechanical Ventilation in Elderly Patients Hospitalized for COVID-19. Cureus, 12, e8069. 10.7759/cureus.8069. [DOI] [PMC free article] [PubMed]
- 44.Ferdinand K.C., Nasser S.A. African American COVID-19 mortality: a sentinel event. J Am Coll Cardiol. 2020 doi: 10.1016/j.jacc.2020.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Treskes R.W., Winden L.A.M.V., Keulen N.V. Effect of smartphone-enabled health monitoring devices vs regular follow-up on blood pressure control among patients after myocardial infarction. JAMA Network Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Medicare telemedicine health care provider fact Sheet. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. Accessed 11 May 2020.
- 47.Böhm M., Kario K., Kandzari D.E. Efficacy of catheter-based renal denervation in the absence of antihypertensive medications (SPYRAL HTN-OFF MED Pivotal): a multicentre, randomised, sham-controlled trial. Lancet. 2020;395:1444–1451. doi: 10.1016/S0140-6736(20)30554-7. [DOI] [PubMed] [Google Scholar]
- 48.Acelajado M.C., Hughes Z.H., Oparil S., Calhoun D.A. Treatment of resistant and refractory hypertension. Circ Res. 2019;124(7):1061–1070. doi: 10.1161/circresaha.118.312156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sanidas E.A., Papadopoulos D.P., Hatziagelaki E., Grassos C., Velliou M., Barbetseas J. Sodium glucose cotransporter 2 (SGLT2) inhibitors across the spectrum of hypertension. Am J Hypertens. 2019;33:207–213. doi: 10.1093/ajh/hpz157. [DOI] [PubMed] [Google Scholar]
- 50.Ferdinand K.C., Izzo J.L., Lee J. Antihyperglycemic and blood pressure effects of Empagliflozin in black patients with type 2 diabetes mellitus and hypertension. Circulation. 2019;139:2098–2109. doi: 10.1161/circulationaha.118.036568. [DOI] [PubMed] [Google Scholar]
- 51.Keck M., Almeida H.D., Compère D., Inguimbert N., FlahaultA Balavoine, Llorens-Cortes C. NI956/QGC006, a potent orally active, brain-penetrating aminopeptidase A inhibitor for treating hypertension. Hypertension. 2019;73:1300–1307. doi: 10.1161/hypertensionaha.118.12499. [DOI] [PubMed] [Google Scholar]
- 52.Berg, Sara. American Medical Association. Project aims to validate clinical accuracy of BP measurement devices. https://www.ama-assn.org/delivering-care/hypertension/project-aims-validate-clinical-accuracy-bp-measurement-devices. Accessed 14 May 2020.
- 53.Milman T., Joundi R.A., Alotaibi N.M., Saposnik G. Clinical inertia in the pharmacological management of hypertension. Medicine. 2018;97 doi: 10.1097/md.0000000000011121. [DOI] [PMC free article] [PubMed] [Google Scholar]