Abstract
Posttraumatic Stress Disorder (PTSD) is a prevalent and debilitating condition with complex and variable presentation. While PTSD symptom domains (intrusion, avoidance, cognition/mood, and arousal/reactivity) correlate highly, the relative importance of these symptom subsets often differs across patients. In this study, we used machine learning to derive how PTSD symptom subsets differ based upon brain functional connectivity. We acquired resting-state magnetic resonance imaging in a sample (N = 50) of PTSD patients and characterized clinical features using the PTSD Checklist for DSM-5 (PCL-5). We compared connectivity among 100 cortical and subcortical regions within the default mode, salience, executive, and affective networks. We then used principal component analysis and least-angle regression (LARS) to identify relationships between symptom domain severity and brain networks. We found connectivity predicted PTSD symptom profiles. The goodness of fit (R2) for total PCL-5 score was 0.29 and the R2 for intrusion, avoidance, cognition/mood, and arousal/reactivity symptoms was 0.33, 0.23, −0.01, and 0.06, respectively. The model performed significantly better than chance in predicting total PCL-5 score (p = 0.030) as well as intrusion and avoidance scores (p = 0.002 and p = 0.034). It was not able to predict cognition and arousal scores (p = 0.412 and p = 0.164). While this work requires replication, these findings demonstrate that this computational approach can directly link PTSD symptom domains with neural network connectivity patterns. This line of research provides an important step toward data-driven diagnostic assessments in PTSD, and the use of computational methods to identify individual patterns of network pathology that can be leveraged toward individualized treatment.
Subject terms: Diagnostic markers, Psychiatric disorders, Diagnostic markers, Psychiatric disorders
Introduction
Posttraumatic Stress Disorder (PTSD) is a highly prevalent and chronic psychiatric disorder, characterized by trauma exposure, followed by intrusive thoughts/recollections, avoidance of related stimuli, hyperarousal, and mood and cognitive impairment1,2. In the USA, lifetime prevalence is estimated at 7%, with higher prevalence in military Veterans1–3. Current evidence-based treatments, including psychopharmacology and psychotherapy, are often inadequately effective3. In addition to suffering due to the symptoms themselves, PTSD is also associated with poor functioning and disability, general medical illness, and poor quality of life4–6.
Though the consequences of PTSD are well established, its presentation is heterogeneous. Diagnosis is often difficult, as PTSD is highly comorbid with other psychiatric illnesses7,8 and individuals may possess a myriad of symptoms. Different diagnostic and nosological models attempt to identify PTSD symptoms—this is evident in the DSM-52 criteria for PTSD, which groups symptoms in four domains: intrusion (criterion B); avoidance (criterion C); cognition and mood (criterion D); and Arousal and reactivity (criterion E). Symptom groupings are based upon their frequent co-occurrence in observational studies, or by data-driven approaches such as factor analysis9,10. Finding a biological biomarker can aid clinical diagnosis and remove biases and uncertainties that can occur during the course of clinical practice. Finding such a unified biomarker for PTSD has proven difficult, likely given the diversity and heterogeneity of presentation (e.g.,11), indicating that different biological subtypes exist within the clinical symptom profile.
One novel approach to developing objective markers of PTSD is through the use of functional neuroimaging to examine neural circuits (reviewed in12,13) to identify biological correlates of symptom domains. The brain is organized into discrete neural networks (e.g.,14,15), and recent work has described multiple alterations in these networks in PTSD. For example, PTSD is associated with deficits within the frontoparietal network (FPN), increased salience network (SN) connectivity and disruptions in default mode network (DMN) connectivity16. Studies that have investigated the relationship of PTSD symptom domains to deficits in brain networks have typically relied on exposure and imagery during functional imaging to elucidate the association of specific brain networks with different PTSD symptoms17–19. Other imaging studies have used topological approaches to characterize how PTSD impacts neural networks20,21, and recent work suggests the utility of using machine learning approaches to predict and potentially identify those at risk for PTSD22. This area of inquiry has already significantly advanced the field in psychosis research and substance use, where machine learning can now identify patients using brain-based pathology23 and individualized treatment response24,25.
Currently, it is unknown if a combined neuroimaging and machine learning approach will provide similar links between pathological neural circuits and individualized symptom profiles in PTSD. Doing so would represent a first step toward characterizing the neural basis of heterogeneity in PTSD. If successful, potential objective markers of domain-level pathology may serve as targets for future circuit-based, personalized interventions. Though transcranial magnetic stimulation can reduce PTSD symptoms [e.g.,3,26,27, reviewed in28], response to stimulation is reduced in those with more severe symptoms in some domains29. Therefore, there is a need to identify novel targets or circuits to engage to maximize treatment efficacy (e.g.,30). Here, we applied a machine learning approach to identify brain functional networks as they relate to PTSD symptom domains, derived from patient-reported scales, hypothesizing that we would be able to identify novel relationships between data-driven connectivity patterns and individual PTSD symptom domains.
Patients and methods
Overview
Following informed consent, magnetic resonance imaging data were acquired from 50 participants on a 3T MRI scanner at Brown University (see Supplementary methods for further information on neuroimaging acquisition, preprocessing, and quality control). The Providence VA Medical Center and Butler Hospital Institutional Review Boards approved these studies, and identical procedures were used at both sites. The data used for the analyses presented here were recorded as part of pretreatment (i.e., baseline) scanning in three previous studies from our group29,31,32.
Participants and assessments
Participants (N = 50) were 48.84 ± 11.78 years of age, and 38% (n = 13) were women. All participants met DSM-5 criteria for PTSD. Self-reported PTSD symptoms were measured using the PTSD Checklist for DSM-5 PTSD (PCL-5;33). The PCL-5 is a 20-question scale and provides a score between 0–80, correlated with PTSD severity. Furthermore, the PCL-5 score can be divided into four subscales, corresponding to PTSD symptom domains described above. The majority of participants also had major depression, which would be expected due to the high comorbidity between these two disorders34, and the vast majority were on concurrent pharmacotherapy. If applicable, all participants were receiving stable treatment (e.g., medications and psychotherapy) for at least 6 weeks before neuroimaging. Inclusion/exclusion criteria and full participant information is included in the Supplementary materials (see Supplementary Table 1).
Region-of-interest selection
We selected 100 cortical and subcortical regions-of-interest (ROIs) for functional connectivity analyses. ROIs were located in functional networks implicated in PTSD by prior studies (Table 1; Supplementary Fig. 1). ROIs were inclusive of the DMN, SN, FPN and affective network (AN). ROIs were defined using the Human Connectome Project Multimodal Atlas35; amygdala and hippocampus were based on the probabilistic atlas of Mazziotta et al.36, while striatal ROIs are from the seven-network functional parcellation of Choi et al.37 The selection of areas limited the dimensionality and make the regression computationally tractable (see ‘Discussion’) and was made a priori to all analyses.
Table 1.
List of included ROIs.
| Network | Anatomical group | ROI |
|---|---|---|
| Subcortical | ||
| Medial temporal lobe | Amygdala (CM) | |
| Amygdala (BL) | ||
| Ant hippocampus | ||
| Mid hippocampus | ||
| Pos hippocampus | ||
| Basal ganglia and thalamus | Striatum (FPN) | |
| Striatum (DMN) | ||
| Thalamus (PFC) | ||
| Affective | ||
| VMPFC | 10r, 10v | |
| Subgenual | 25, s32 | |
| Orbital | 11l, 13l | |
| OFC, pOFC | ||
| Default | ||
| DLPFC | 9p | |
| MPFC | 10pp, a10p, p10p | |
| 10d, 9m | ||
| Orbital | 47s, 47m, a47r | |
| Ant cingulate and paracingulate | a24, p24, p32 | |
| PCC | v23ab | |
| FPN | ||
| DLPFC | 9–46d, a9-46v, p9-46v | |
| 46 | ||
| Inf frontal cortex | 47l, p47r | |
| VLPFC | 44, 45 | |
| IFSa, IFSp | ||
| Mid cingulate and paracingulate | 23c, d23ab | |
| SN | ||
| DLPFC | 9a | |
| Ant to Mid cingulate | a24pr, p24pr | |
| Ant paracingulate | d32, a32pr, p32pr | |
| Mid paracingulate | 23d, 24dd, 24dv |
For ROIs based on the Human Connectome Project Multimodal Atlas, the prefix ‘a’ or ‘p’ usually denotes an anterior or posterior subregion of regions typically found in unimodal atlases (e.g., Brodmann’s areas). The same is true for ‘d,’ ‘v,’ ‘r,’ ‘m,’ ‘l,’ which stand for ‘dorsal,’ ‘ventral,’ ‘rostral,’ ‘medial,’ and ‘lateral’, respectively. ‘CM’ and ‘BL’ in the subcortical ROIs refer to the centromedial and basolateral divisions of the amygdala, respectively.
DMN default mode network, PFC prefrontal cortex, MPFC medial prefrontal cortex, FPN frontoparietal network, SN salience network, VMPFC ventromedial prefrontal cortex, OFC orbitofrontal cortex, pOFC posterior orbitofrontal cortex, MTL medial temporal lobe, CM centromedial, BL basolateral.
Subject-level ROI-to-ROI functional connectivity analysis
For each subject, functional MRI time courses were extracted from preprocessed functional data for each ROI. Time courses were entered into a cross-correlation matrix and the resulting bivariate Pearson’s correlations, calculated in 4950 unique ROI pairs. We used the absolute value of Pearson correlation as a measure of functional connectivity.
Machine learning
We first used principal component analysis to reduce the dimensionality of the functional connectivity matrix. We selected the first principal components that cumulatively represented 90% of the variance in the functional connectivity matrix, compressing the 4950 dimensions of the connectivity matrix to 39 (i.e., the first 39 components represented 90% of data variance, see Supplementary Fig. 2). We then used least-angle regression (LARS)38 on this dimensionality-reduced dataset to predict each of the four PCL-5 subscales: criterion (B) intrusion, (C) avoidance, (D) cognition/mood, and (E) arousal/reactivity. The LARS algorithm provides a parsimonious regression model for efficient prediction of a response variable, particularly when the number of predictor variables is large. The ability of the regression models to predict symptoms was tested, utilizing full iterative leave-one-out cross-validation to evaluate the performance and calculating coefficient of determination (R2) using the below formula:
where SSres was the sum of squares of residuals and SStot was the total sum of squares. Note that R2 calculated this way can assume negative values (when the goodness of fit for the cross-validated data is less than a zero-slope fit, i.e., the null hypothesis for regression).
To assess the significance of the prediction and to make sure that the proposed results did not reflect overfitting, we re-ran the study on a randomly permuted dataset. To do this, we shuffled the PCL-5 values (resampled without replacement), breaking the relationship between PCL-5 and fMRI data and re-ran the analysis. This process was repeated for 5000 iterations and thus quantified the ability of the model to predict noise.
Finally, the regression weights (i.e., beta coefficients) were then mapped back from PCA space to ROI-ROI functional connectivity space to identify implicated brain connections. We used the algorithm and correction proposed by Haufe et al.39, which provides the methodology for converting the decoding parameters into encoding parameters and make our weights interpretable (see Haufe et al.39 for a detailed discussion). The 1% strongest weights (50 connections) are visualized in the connectome plots. For the purpose of plotting, graphs represent the absolute value of the functional connectivity measure.
The analysis code was written in Python 3.7.1 and using scikit-learn 0.20.1 machine learning library. Connectome plots are generated using Circos 0.69–640.
Results
Symptom scores
Our patient population had a median PCL-5 score in the moderate range, (median = PCL 46.5; 95% CI 24–71). As might be expected, PCL subscales were highly and significantly correlated with each other (Table 2, Pearson correlation coefficient, r, ranging between 0.38 and 0.51).
Table 2.
Correlation between PCL-5 subscales.
| PCL-5: B | PCL-5: C | PCL-5: D | PCL-5: E | PCL-5: total | |
|---|---|---|---|---|---|
| PCL-5: B | 1 | 0.48 | 0.45 | 0.49 | 0.78 |
| PCL-5: C | 0.48 | 1 | 0.38 | 0.46 | 0.65 |
| PCL-5: D | 0.45 | 0.38 | 1 | 0.51 | 0.81 |
| PCL-5: E | 0.49 | 0.46 | 0.51 | 1 | 0.81 |
| PCL-5: total | 0.78 | 0.65 | 0.81 | 0.81 | 1 |
Criteria B, C, D, and E correspond to intrusion, avoidance, cognition/mood, and arousal/reactivity, respectively. The values in the table are Pearson’s correlation coefficients (r).
PCL-5 PTSD checklist for DSM-5.
Machine learning output
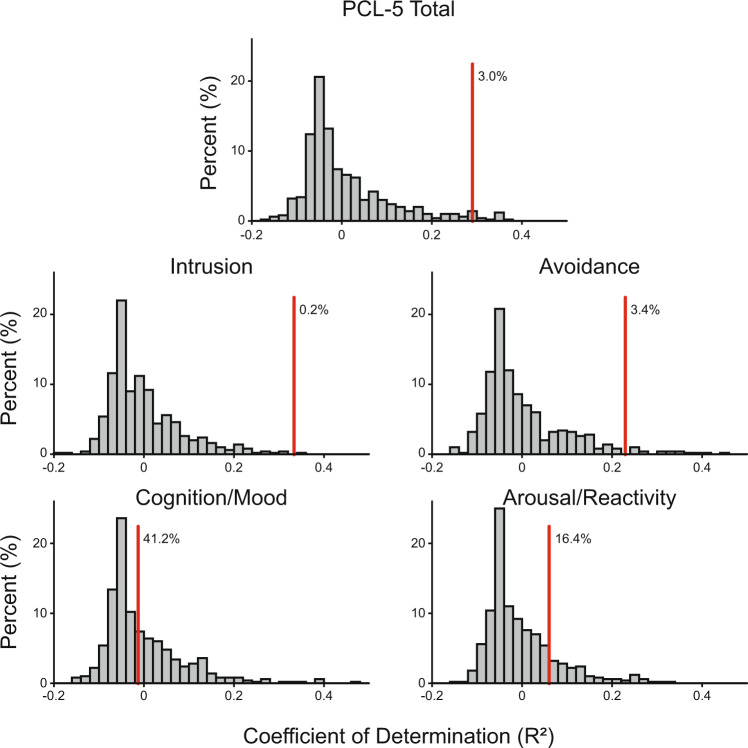
Our machine learning algorithm, utilizing feature selection and LARS regression, was able to predict total PCL-5 score as well as the subscale scores for the intrusion and avoidance clusters (quantified via coefficient of determination, R2). The R2 value for total PCL-5 was 0.29. R2 values for intrusion, avoidance, cognition, and arousal domains were 0.33, 0.23, −0.01, and 0.06, respectively. The models performed significantly better than chance in predicting total PCL-5 score (p = 0.030) as well as intrusion and avoidance subscales (p = 0.002 and p = 0.034). It was not able to predict cognition and arousal scores (p = 0.412 0.164, see Fig. 1). Model performance is presented in Fig. 2. The results were robust to leave-one-out cross-validation.
Fig. 1. Regression performance for real and permutated data.
Cross-validated regression performance (goodness of fit, R2) in predicting PCL-5 scores. The red line depicts the R2, and the histogram depicts the model’s performance in predicting shuffled data (random permutation). The percent reported next to the line shows the likelihood that the model performance can be achieved by chance. Note the measure of R2 used here can assume negative values in a leave-one-out cross-validated sample (see ‘Methods’).
Fig. 2. Observed vs. predicted PTSD symptom severity.

The figure shown observed PCL-5 score (total PTSD symptom severity) plotted against the predicted PCL-5 score. The predictions are made on a leave-one-out cross-validated sample.
Functional connectivity relationships predictive of symptom profiles
For total PCL-5, intrusion, and avoidance symptoms, we plotted the 50 connections (out of 4950) with the highest predictive weights (Fig. 3). Several connectivity patterns were predictive of PTSD symptom profiles. Increased positive connectivity between right rostral anterior cingulate (Human connectome atlas region a24; DMN) and left pars orbitalis (Human connectome region 47 l; FPN) was associated with higher intrusion and overall PCL score. Weaker DMN-to-AN functional connectivity was also observed in patients with higher scores on the same two scales. Lower positive connectivity within DMN was a feature of both intrusion and avoidance symptoms. Cross-network connectivity between DMN, SN, and FPN was also disrupted in participants with more severe intrusion and avoidance symptoms, though the direction of these effects (positive vs. negative functional connectivity) was inconsistent.
Fig. 3. Connectivity correlates of PTSD symptom severity.
Regression weights (Beta coefficients) were mapped onto functional connectivity data, and the 50 with the highest weights are plotted. Blue (plotted on the right) indicates the connections with a negative coefficient and thus associated with a lower PTSD symptoms severity, and red (plotted on the left) indicating connections with a positive coefficient and therefore associated with a more severe PTSD symptom severity. We have presented the weights predicting total PCL-5 score on top and those associated with PTSD sub-scores on the bottom. Note that the weights represent the absolute functional connectivity. DMN default mode network; DLPFC dorsolateral prefrontal cortex; MPFC medial prefrontal cortex; Orb Orbital Cortex; ACC anterior cingulate cortex; PCC posterior cingulate cortex; FPN frontoparietal network; IFG inferior frontal gyrus; MCC middle cingulate cortex; SN salience network; aMCC anterior midcingulate cortex; aPCG anterior postcingulate gyrus; mPCG medial postcingulate gyrus; AN affective network; VMPFC ventromedial prefrontal cortex; sACC subgenual anterior cingulate cortex; OFC orbitofrontal cortex; SC subcortical; AMY amygdala; HPC hippocampus; Stri striatum; Thal thalamus.
Two primary characteristics distinguished intrusion from avoidance profiles: weak within-DMN connectivity was more prominent in the high intrusion profile, while stronger within-FPN connectivity was associated with more severe symptoms of avoidance. Lower SN-to-FPN connectivity was also characteristic of high avoidance patients. Disrupted FPN-to-DMN connectivity was a feature of both intrusion and avoidance, though pairs of affected ROIs differed between profiles.
Discussion
In this study, we adopted a novel two-step machine learning algorithm that was able to predict individual-level self-reported PTSD symptoms from resting-state functional connectivity. Our results linked severity in different PTSD symptom domains to distinct patterns of network function. This is an important first step toward defining biological diagnostic criteria for PTSD. There is an immediate need for innovations including biological markers to address the challenges that symptom heterogeneity poses for PTSD diagnosis (e.g.,41). Our algorithm employs a supervised learning approach that builds upon prior clinical observations enabling the identification of clinically meaningful biological patterns in a modestly sized dataset.
As technological advances have enabled the collection of more complex, larger neurobiological datasets, the use of data science techniques for high-dimensional data analysis in mental health research has gained popularity (e.g., see Refs. 42 and23). These studies primarily used ‘unsupervised’ machine learning approaches to find patterns in complex data without feedback from an outside/clinical examiner. Unfortunately, data complexity negatively impacts the performance of statistical and machine learning tools, a short-coming typically addressed by using a large number of subjects. Thus, though unsupervised techniques can be powerful, sample size requirements and associated costs limit their feasibility in clinical populations.
As we designed our machine learning algorithm, we sought to balance the challenges of analyzing high-dimensional, complex, datasets with the practical considerations of clinical research. We adopted an approach used previously in visual processing and face recognition research. Visual image data are comprised of many pixels and is thus, high dimensional. To improve model performance, machine learning studies of visual processing frequently employ a dimensionality reduction transformation (e.g., PCA) before model training43,44. Analogously, we applied PCA to our ROI matrix of connectivity values before regularized regression, allowing us to leverage the power of machine learning in a dataset typical of most clinical studies. Alongside this, we also limited the number of areas that were included in our analysis. We selected 100 ROIs out of a possible 376. Doing this, we deviated from a pure ‘data-driven’ approach, yet this significantly reduced the number of our features (more than 14-fold reduction, 4950 vs. 70,500) and made the analysis computationally tractable using our sample size.
The results of our analysis indicated that different symptom classes mapped onto distinct cortical networks. The model is successful in predicting the overall symptom severity, intrusion, and avoidance symptoms and associated with unique variations in functional connectivity profiles. While lower functional connectivity between DMN regions in ventrolateral PFC and affective regions in orbitofrontal cortex were common to all three of these outcomes, intrusion and avoidance symptoms were distinguished by weak within-DMN and stronger within-FPN connectivity, respectively. Although these observations await replication, the face validity between these networks and symptoms is informative given the association of DMN with self-reflection and rumination45 and the role of FPN in cognitive control46. Though stronger cognitive control may initially seem incongruent in the context of psychiatric disorder, avoidance symptoms of PTSD may represent a maladaptive control strategy. This would be consistent with other areas of research, indicating maladaptive application of cognitive control as a potential risk factor for suicide in individuals with depression47,48 and PTSD49.
While these results provide initial support for the use of biologically grounded data-driven diagnostic methods, we acknowledge that the model was unsuccessful predictions for arousal and cognition/mood symptoms. Low performance might be an artifact of the algorithm optimizing the detection of some symptoms at the expense of others, it could be due to our modest sample size, or could be driven by differences in symptom representation in our sample. Depression comorbidity34,49 also complicates PTSD-specific symptom classifications but reflects real-world patient symptom profiles. Another interpretation is that cognition/mood and arousal symptoms may be a product of widely distributed changes in brain function rather than prominent shifts in function in a few discrete networks. For example, if disruptions in SN related to hypervigilance are a general core feature of PTSD50–52 pathological threat monitoring may evoke changes in both primary sensory and associative control networks equally precluding the identification of a distinct bio-signature of arousal symptoms. Disambiguating between these alternatives requires further research in larger samples an explicit testing of comorbidity effects.
The principal limitations of this work are those inherent to secondary neuroimaging analyses using a modest sample size, cross-sectional design, and the absence of healthy controls. Because of the sample size, it is possible the results presented here reflect overfitting, in which the algorithm learns trends in the data that are not generalizable to other samples53,54. We attempted to mitigate this issue by using a small number of a priori defined ROIs, and implementing a data processing stream that incorporated dimensionality reduction, regularization (limiting model complexity), cross-validation, and permutation testing. Our sample was also unique in that they were largely enrolled for brain stimulation treatment studies, and thus may not represent patients with PTSD in general, and nearly all (86%) were on concurrent pharmacotherapy. Furthermore, our study did not track patients’ transition from healthy state to PTSD and as such, the results presented might be associated with the predisposition to these PTSD symptom clusters and not the symptoms themselves. Nonetheless, this study sets a precedent and introduces a methodology that can be further investigated.
In summary, we successfully generated individual-level connectivity patterns representative of self-reported PTSD symptoms. If these results can be prospectively replicated, our approach can inform the creation of individualized and objective brain-based, self-reported PTSD symptoms. Expansion of this work may yield new insights into the clinical heterogeneity of this disorder and potentially lead to individually targeted interventions for symptom reduction.
Supplementary information
Acknowledgements
We thank Idin Karuei Ph.D. and Amir-Massoud Farahmand Ph.D. for their input and help during data analysis. We thank all the participants. This study was supported by NIH grants U54GM115677 (A.Z.) and R25MH101076 (Y.A.B.), U.S. Veterans Affairs grants I21RX002032 (N.S.P.), I01RX002450 (N.S.P.), IK2CX001824 (J.B.), and the VA RR&D Center for Neurorestoration and Neurotechnology at the Providence VA Medical Center. The funders had no role in the conduct of the study, paper preparation or the decision to submit for publication. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs, or the United States government. This work was presented in part at the 2018 annual meeting of the American College of Neuropsychopharmacology (ACNP). We thank all our participants.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Amin Zandvakili, Jennifer Barredo
Supplementary information
Supplementary Information accompanies this paper at (10.1038/s41398-020-00879-2).
References
- 1.Shalev A, Liberzon I, Marmar C. Post-traumatic stress disorder. N. Engl. J. Med. 2017;376:2459–2469. doi: 10.1056/NEJMra1612499. [DOI] [PubMed] [Google Scholar]
- 2.Association A. P. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). (American Psychiatric Publishing, 2013).
- 3.Watts BV, et al. Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. J. Clin. Psychiatry. 2013;74:e541–e550. doi: 10.4088/JCP.12r08225. [DOI] [PubMed] [Google Scholar]
- 4.Amaya-Jackson L, et al. Functional impairment and utilization of services associated with posttraumatic stress in the community. J. Trauma. Stress. 1999;12:709–724. doi: 10.1023/A:1024781504756. [DOI] [PubMed] [Google Scholar]
- 5.Hoge CW, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N. Engl. J. Med. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- 6.Marshall RD, et al. Comorbidity, impairment, and suicidality in subthreshold PTSD. Am. J. Psychiatry. 2001;158:1467–1473. doi: 10.1176/appi.ajp.158.9.1467. [DOI] [PubMed] [Google Scholar]
- 7.Holtzheimer PE, 3rd, Russo J, Zatzick D, Bundy C, Roy-Byrne PP. The impact of comorbid posttraumatic stress disorder on short-term clinical outcome in hospitalized patients with depression. Am. J. Psychiatry. 2005;162:970–976. doi: 10.1176/appi.ajp.162.5.970. [DOI] [PubMed] [Google Scholar]
- 8.Magruder KM, et al. Prevalence of posttraumatic stress disorder in Veterans Affairs primary care clinics. Gen. Hosp. Psychiatry. 2005;27:169–179. doi: 10.1016/j.genhosppsych.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 9.Eddinger JR, McDevitt-Murphy ME. A confirmatory factor analysis of the PTSD checklist 5 in veteran and college student samples. Psychiatry Res. 2017;255:219–224. doi: 10.1016/j.psychres.2017.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang H, et al. The underlying dimensions of DSM-5 PTSD symptoms and their relations with anxiety and depression in a sample of adolescents exposed to an explosion accident. Eur. J. Psychotraumatol. 2017;8:1272789. doi: 10.1080/20008198.2016.1272789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Michopoulos V, Norrholm SD, Jovanovic T. Diagnostic biomarkers for posttraumatic stress disorder: promising horizons from translational neuroscience research. Biol. Psychiatry. 2015;78:344–353. doi: 10.1016/j.biopsych.2015.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fenster RJ, Lebois LAM, Ressler KJ, Suh J. Brain circuit dysfunction in post-traumatic stress disorder: from mouse to man. Nat. Rev. Neurosci. 2018;19:535–551. doi: 10.1038/s41583-018-0039-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sheynin J, Liberzon I. Circuit dysregulation and circuit-based treatments in posttraumatic stress disorder. Neurosci. Lett. 2017;649:133–138. doi: 10.1016/j.neulet.2016.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fox MD, et al. The human brain is intrinsically organized into dynamic, anticorrelated functional networks. Proc. Natl. Acad. Sci. USA. 2005;102:9673–9678. doi: 10.1073/pnas.0504136102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fox MD, Raichle ME. Spontaneous fluctuations in brain activity observed with functional magnetic resonance imaging. Nat. Rev. Neurosci. 2007;8:700–711. doi: 10.1038/nrn2201. [DOI] [PubMed] [Google Scholar]
- 16.Koch SB, et al. Aberrant resting-state brain activity in posttraumatic stress disorder: a meta-analysis and systematic review. Depression Anxiety. 2016;33:592–605. doi: 10.1002/da.22478. [DOI] [PubMed] [Google Scholar]
- 17.Hopper JW, Frewen PA, van der Kolk BA, Lanius RA. Neural correlates of reexperiencing, avoidance, and dissociation in PTSD: symptom dimensions and emotion dysregulation in responses to script-driven trauma imagery. J. Trauma. Stress. 2007;20:713–725. doi: 10.1002/jts.20284. [DOI] [PubMed] [Google Scholar]
- 18.Bremner JD, et al. Neural correlates of exposure to traumatic pictures and sound in Vietnam combat veterans with and without posttraumatic stress disorder: a positron emission tomography study. Biol. Psychiatry. 1999;45:806–816. doi: 10.1016/s0006-3223(98)00297-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liberzon I, Britton JC, Phan KL. Neural correlates of traumatic recall in posttraumatic stress disorder. Stress. 2003;6:151–156. doi: 10.1080/1025389031000136242. [DOI] [PubMed] [Google Scholar]
- 20.Akiki TJ, et al. Default mode network abnormalities in posttraumatic stress disorder: a novel network-restricted topology approach. Neuroimage. 2018;176:489–498. doi: 10.1016/j.neuroimage.2018.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kennis M, van Rooij SJ, van den Heuvel MP, Kahn RS, Geuze E. Functional network topology associated with posttraumatic stress disorder in veterans. Neuroimage Clin. 2016;10:302–309. doi: 10.1016/j.nicl.2015.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Galatzer-Levy IR, Ma S, Statnikov A, Yehuda R, Shalev AY. Utilization of machine learning for prediction of post-traumatic stress: a re-examination of cortisol in the prediction and pathways to non-remitting PTSD. Transl. Psychiatry. 2017;7:e0. doi: 10.1038/tp.2017.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clementz BA, et al. Identification of distinct psychosis biotypes using brain-based biomarkers. Am. J. Psychiatry. 2016;173:373–384. doi: 10.1176/appi.ajp.2015.14091200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cao B, et al. Treatment response prediction and individualized identification of first-episode drug-naive schizophrenia using brain functional connectivity. Mol. Psychiatry. 2018;25:906–913. doi: 10.1038/s41380-018-0106-5. [DOI] [PubMed] [Google Scholar]
- 25.Yip SW, Scheinost D, Potenza MN, Carroll KM. Connectome-based prediction of cocaine abstinence. Am. J. Psychiatry. 2019;176:156–164. doi: 10.1176/appi.ajp.2018.17101147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Philip NS, et al. Network mechanisms of clinical response to transcranial magnetic stimulation in posttraumatic stress disorder and major depressive disorder. Biol. Psychiatry. 2018;83:263–272. doi: 10.1016/j.biopsych.2017.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kozel FA, et al. Repetitive TMS to augment cognitive processing therapy in combat veterans of recent conflicts with PTSD: a randomized clinical trial. J. Affect. Disord. 2018;229:506–514. doi: 10.1016/j.jad.2017.12.046. [DOI] [PubMed] [Google Scholar]
- 28.Koek RJ, Roach J, Athanasiou N, van ‘t Wout-Frank M, Philip NS. Neuromodulatory treatments for post-traumatic stress disorder (PTSD) Prog. Neuropsychopharmacol. Biol. Psychiatry. 2019;92:148–160. doi: 10.1016/j.pnpbp.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 29.Carpenter LL, et al. 5Hz Repetitive transcranial magnetic stimulation for posttraumatic stress disorder comorbid with major depressive disorder. J. Affect. Disord. 2018;235:414–420. doi: 10.1016/j.jad.2018.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hanlon CA, Philip NS, Price RB, Bickel WK, Downar J. A case for the frontal pole as an empirically derived neuromodulation treatment target. Biol. Psychiatry. 2019;85:e13–e14. doi: 10.1016/j.biopsych.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.van ‘t Wout-Frank M, Shea MT, Larson VC, Greenberg BD, Philip NS. Combined transcranial direct current stimulation with virtual reality exposure for posttraumatic stress disorder: feasibility and pilot results. Brain Stimul. 2019;12:41–43. doi: 10.1016/j.brs.2018.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Philip N. S. et al. Theta-burst transcranial magnetic stimulation for posttraumatic stress disorder. Am J Psychiatry176, 939–948 (2019). [DOI] [PMC free article] [PubMed]
- 33.Weathers F. W. et al. The ptsd checklist for dsm-5 (pcl-5). Scale available from the National Center for PTSDwww.ptsd.va.gov (2013).
- 34.Rytwinski NK, Scur MD, Feeny NC, Youngstrom EA. The co-occurrence of major depressive disorder among individuals with posttraumatic stress disorder: a meta-analysis. J. Trauma. Stress. 2013;26:299–309. doi: 10.1002/jts.21814. [DOI] [PubMed] [Google Scholar]
- 35.Glasser MF, et al. A multi-modal parcellation of human cerebral cortex. Nature. 2016;536:171–178. doi: 10.1038/nature18933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mazziotta J, et al. A probabilistic atlas and reference system for the human brain: International Consortium for Brain Mapping (ICBM) Philos. Trans. R. Soc. Lond. B Biol. Sci. 2001;356:1293–1322. doi: 10.1098/rstb.2001.0915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Choi EY, Yeo BT, Buckner RL. The organization of the human striatum estimated by intrinsic functional connectivity. J. Neurophysiol. 2012;108:2242–2263. doi: 10.1152/jn.00270.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Efron B, Hastie T, Johnstone I, Tibshirani R. Least angle regression. Ann. Stat. 2004;32:407–451.. [Google Scholar]
- 39.Haufe S, et al. On the interpretation of weight vectors of linear models in multivariate neuroimaging. Neuroimage. 2014;87:96–110. doi: 10.1016/j.neuroimage.2013.10.067. [DOI] [PubMed] [Google Scholar]
- 40.Krzywinski M, et al. Circos: an information aesthetic for comparative genomics. Genome Res. 2009;19:1639–1645. doi: 10.1101/gr.092759.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pai A, Suris AM, North CS. Posttraumatic stress disorder in the DSM-5: controversy, change, and conceptual considerations. Behav. Sci. 2017;7:7. doi: 10.3390/bs7010007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Drysdale AT, et al. Resting-state connectivity biomarkers define neurophysiological subtypes of depression. Nat. Med. 2017;23:28–38. doi: 10.1038/nm.4246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Turk, M., Pentland, A. Face recognition using eigenfaces. In Proceedings CVPR'91., IEEE Computer Society Conference on Vision and Pattern Recognition. (IEEE, 1991)
- 44.Zhang J, Yan Y, Lades M. Face recognition: eigenface, elastic matching, and neural nets. Proc. IEEE. 1997;85:1423–1435. [Google Scholar]
- 45.Hamilton JP, Farmer M, Fogelman P, Gotlib IH. Depressive rumination, the default-mode network, and the dark matter of clinical neuroscience. Biol. Psychiatry. 2015;78:224–230. doi: 10.1016/j.biopsych.2015.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vincent JL, Kahn I, Snyder AZ, Raichle ME, Buckner RL. Evidence for a frontoparietal control system revealed by intrinsic functional connectivity. J. Neurophysiol. 2008;100:3328–3342. doi: 10.1152/jn.90355.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.van Heeringen K, Bijttebier S, Desmyter S, Vervaet M, Baeken C. Is there a neuroanatomical basis of the vulnerability to suicidal behavior? A coordinate-based meta-analysis of structural and functional MRI studies. Front. Hum. Neurosci. 2014;8:824. doi: 10.3389/fnhum.2014.00824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dombrovski AY, Hallquist MN. The decision neuroscience perspective on suicidal behavior: evidence and hypotheses. Curr. Opin. Psychiatry. 2017;30:7–14. doi: 10.1097/YCO.0000000000000297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Barredo J, et al. Neuroimaging correlates of suicidality in decision-making circuits in posttraumatic stress disorder. Front. Psychiatry. 2019;10:44. doi: 10.3389/fpsyt.2019.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Garfinkel SN, Liberzon I. Neurobiology of PTSD: a review of neuroimaging findings. J. Psychiatr. Ann. 2009;39:370. [Google Scholar]
- 51.Sripada RK, et al. Neural dysregulation in posttraumatic stress disorder: evidence for disrupted equilibrium between salience and default mode brain networks. Psychosom. Med. 2012;74:904–911. doi: 10.1097/PSY.0b013e318273bf33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Akiki TJ, Averill CL, Abdallah CG. A network-based neurobiological model of PTSD: evidence from structural and functional neuroimaging studies. Curr. Psychiatry Rep. 2017;19:81. doi: 10.1007/s11920-017-0840-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Subramanian J, Simon R. Overfitting in prediction models—is it a problem only in high dimensions? Contemp. Clin. Trials. 2013;36:636–641. doi: 10.1016/j.cct.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 54.Huys QJ, Maia TV, Frank MJ. Computational psychiatry as a bridge from neuroscience to clinical applications. Nat. Neurosci. 2016;19:404–413. doi: 10.1038/nn.4238. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.