Supplemental Digital Content is available in the text
Keywords: accelerate rehabilitation, acupuncture therapy, network meta analysis, postoperative nausea and vomiting
Abstract
Background:
Postoperative nausea and vomiting (PONV) is a common complication after surgery. However, drugs cannot prevent it completely, and acupuncture therapy shows the potential in preventing PONV, yet the best choice hasn’t been demonstrated.
Objective:
This network meta analysis aimed to evaluate the effectiveness of different acupuncture therapies used for preventing PONV in abdominal operation.
Methods:
Authors searched articles from PubMed/Medline, Cochrane library, Web of Science, Ebsco and Ovid/Embase, and established database from setup time to June 2019. Quality evaluation of included studies was performed with Cochrane risk-of-bias tool (ROB 2.0). Pairwise and network meta analysis were conducted by RevMan and Addis respectively.
Results:
Twenty studies with 2862 patients were included in this research. Pairwise meta analysis shows that compared with placebo, transcutaneous electric nerve stimulation had lower risk of postoperative nausea (PON) (odds ratio (OR) = 0.42, 95%confidence interval (CI): 0.30–0.60), postoperative vomiting (POV) (OR = 0.53, 95%CI: 0.36–0.78), PONVs (OR = 0.46, 95%CI: 0.31–0.68), and postoperative rescue (POR) (OR = 0.61, 95%CI: 0.41–0.90), Capsicum had lower risk of PON (OR = 0.16, 95%CI: 0.09–0.28), PONVs (OR = 0.23, 95%CI: 0.12–0.45), Acupressure had lower risk of POV (OR = 0.42, 95%CI: 0.25–0.70), POR (OR = 0.42, 95%CI: 0.27–0.64). In network meta analysis, compared with usual care, the probability rank suggested that Acupoint Injection showed lowest risk of PON (OR = 0.02, 95%CI: 0.00–0.11), POV (OR = 0.06, 95%CI: 0.01–0.49), Usual care for PONVs (OR = 0.31, 95%CI: 0.13–0.75), and Capsicum for POR (OR = 0.39, 95%CI: 0.07–2.33). Further study should be carried out to verify this result.
Conclusion:
Both pairwise and network meta analysis showed acupuncture therapy was superior to placebo and usual care. Different acupuncture therapy regimens may have advantages in different aspects. And compared with POV, PON seems easier to control. Research results may provide guidance for the prevention of PONV.
Systematic review registration: PROSPERO CRD42019147556.
1. Introduction
Since anesthesia has been carried out in 1840s, a great amount of surgical patients received anesthesia each year, but until 1 century later, doctors realized that postoperative nausea and vomiting (PONV) is an operative complication rather than inadvertent ones.[1,2] According to the simplified Apfel score, the main risk factors of PONV are female gender, non-smoking, history of PONV and motion sickness, postoperative opioids.[3] About 30% surgical patients had this unpleasant experience and the ratio can increase to 80% in high-risk patients.[1,2,4] Therefore, patients have to pay an extra 30% cost to avoid PONV.[5] PONV is not fatal, but when dehydration, electrolyte imbalance and esophageal rupture come across, the situation will nosedive and even cause death.[6] To reduce PONV, a series of antiemetic drugs were produced including histamine type 1receptor antagonists, 5-hydroxytryptaminereceptor antagonists (5HTRA), dopamine receptor antagonists, corticosteroids and neurokinin-1 receptor antagonists.[7] It has been established that each single drug can reduce 20% to 25% PONV risk and combination antiemetic therapy may reduce 60% PONV risk at most[8]; however, high returns are accompanied by high risks, patients may suffer from the adverse effects of those drugs. Drowsiness and headache are common adverse effects when taking histamine type 1receptor antagonists. Patients using histamine type 1receptor antagonists may suffer from long-QT interval and malignant ventricular arrhythmias. Besides, corticosteroids easily caused glucose variability endocrine dyscrasia.[2] In addition, short half-life time and economic aspects limit the use of 5HTRA and corticosteroids and neurokinin-1 receptor antagonists respectively.[2] Moreover, only 28% of patients will benefit from prophylactic use of antiemetics,[9] while PONV within 24 hours still occurs in 25% to 30% of patients.[10] Thus, concerning about the side effect and massive cost of drugs, researchers are becoming interested in using complementary and alternative therapies such as musicotherapy, ginger, and aromatherapy.[11–14] And among all complementary and alternative therapies, acupuncture is one of the most common and acceptable physical therapies. It is reported that Neiguan (PC6), a wide-used acupoint, shows confident potential in alleviating PONV according to practical acupuncture prescriptions.[1,15–18] In addition, acupuncture therapy can reduce the incidence of pain and PONV-related outcomes of certain operations both in adults and adolescents.[19–21] However, few meta analysis about acupuncture therapy in preventing PONV after abdominal surgery has been reported. Moreover, which therapy is more effective remains disputable. In this review, we assessed the effectiveness of different acupuncture therapies in preventing PONV by utilizing network meta analysis and hoped this work could inspire relevant study.
2. Method
The review has been registered on PROSPERO (https://www.crd.york.ac.uk/prospero) NO. CRD42019147556. We used the Preferred Reporting Items for Systematic review and Meta-Analysis statement for network meta analysis to conduct the meta-analysis.[22] Because this was systematic literature research, ethical approval can be skipped.
2.1. Literature search strategies
Authors searched PubMed/Medline, Cochrane library, Web of Science, Ebsco, and Ovid/Embase from setup time to June 2019 and language was restricted to English and Chinese. The search strategy contained both PONV and acupuncture therapies including “acupuncture,” “electroacupuncture,” “acupuncture therapy,” “PONV,” “postoperative nausea and vomiting,” “PON,” “POV,” and similar terms. The complete search strategy is shown in Appendix 1.
2.2. Eligibility criteria
2.2.1. Inclusion criteria
-
(1)
randomized controlled trials (RCTs),
-
(2)
patients completed abdominal surgery with general anesthesia,
-
(3)
report at least 1 outcome of PON, POV, PONVs and POR in 24 hours after operation,
-
(4)
experimental group received acupuncture therapy and specifically, acupressure and transcutaneous electric nerve stimulation (TEN) with acupoint are regarded as acupuncture therapies,
-
(5)
control group consisted of UC, sham, medication, or counseling,
-
(6)
only the latter of any duplicate publications was selected,
-
(7)
patients underwent surgery regardless of age, gender, ethnic.
2.2.2. Exclusion criteria
-
(1)
case report, review, protocol, animal study, supplementary issue, and conference paper
-
(2)
study without acupuncture therapies or specific acupoints,
-
(3)
non-RCTs or retrospective study or novelty or letter,
-
(4)
non-prophylactic use of acupuncture therapies or patients had been diagnosed as PONV before intervention.
2.3. Data extraction
After identification of the target RCTs, 1 reviewer extracted the following data into a database created by Excel 2019 and checked by a second reviewer:
-
(1)
title, first author, year, country, sex, and sample size,
-
(2)
diseases, American Society of Anesthesiologists Class, types of intervention, types of outcomes, and acupoints. The third reviewer was the referee in case of doubts or disagreements.
2.4. Quality of evidence assessment and risk of bias assessment
Cochrane risk-of-bias tool (ROB 2.0) was used to evaluate the quality.[23] ROB 2.0 has 5 domains including: bias arising from the randomization process, bias due to deviations from intended interventions, bias due to missing outcome data, bias in measurement of the outcome and bias in selection of the reported result. Two reviewers used ROB 2.0 to assess all matched literatures and the third reviewer requested adjudications if necessary.
2.5. Statistical analysis
Cytoscape 3.7.0 is a visualization tool which is commonly used in biomedicine field. For this literature, network plots were drawn by using Cytoscape, the node size and the line thickness represent the size of treatment and study respectively.
RevMan 5.3 is used to solve pairwise meta analysis, and odds ratio (OR) and 95% confidence interval (CI) were adopted. Heterogeneity is quantified with the I2 statistic. When the I2 > 50%, a random effect model was adopted; if not, a fixed effect model.
ADDIS 1.16.6 is a software based on Bayesian framework which uses the Markov Chain Monte Carlo theory to perform the multi-treatment meta analysis.[24] Convergence is calculated by using the Brooks-Gelman-Rubin method. It compares within-chain and between-chain variance in order to calculate the Potential Scale Reduction Factor (PSRF). The more PSRF approximate 1, the better convergence can be obtained, and PSRF ≤ 1.05 is acceptable.[25–27] As the incidence rate is dichotomous data, OR and 95%CI were adopted. A random effect model is used as it is a more appropriate method.[28] Node split analysis is an alternative method to assess inconsistency by assessing whether direct and indirect evidence are in agreement and P > .05 indicates no significant inconsistency is found.[29] Rank probability plots suggested potential efficacy when 2 treatments had no statistical significance (in this review, a lower rank is worse), but it should be treated with caution.[30]
3. Results
As showed in Figure 1, authors retrieved 19,116 articles from 5 databases, 8115 duplicate articles were removed. A total of 10,692 articles were eliminated by reading titles and abstracts and 204 articles by reading the full text. Finally, 20 RCTs published from 1998 to 2015 with 2862 patients matched the final criteria through web search and selection.
Figure 1.
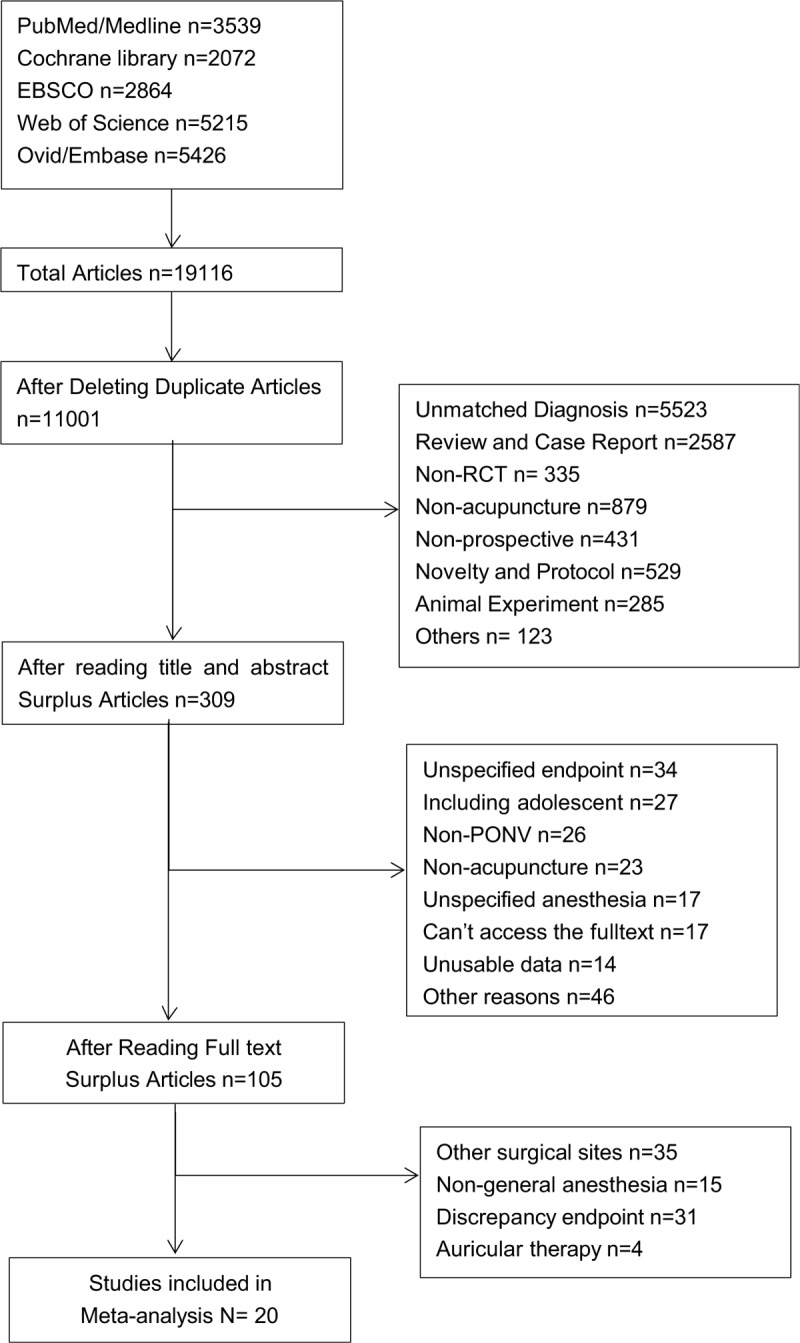
PRISMA flow diagram of the study selection process.
3.1. Study characteristics
The sample size of RCTs ranged from 27 to 410 and consisted mainly of female. Participants were from Asia, Europe and America between 1998 and 2015. Among all included studies, PC6 and Zusanli (ST36) are the most commonly used acupoints. TEN may be the most common acupuncture therapy appeared in 7 studies with 490 patients. 7 studies were 3-arm trails and other were 2-arm trails. 13 studies employed placebo as control group and 7 studies employed Usual Care (UC). Main characteristics of included RCTs were shown in Table 1 and network plots of included RCTs were shown in Figure 2.
Table 1.
Characteristics of enrolled studies.
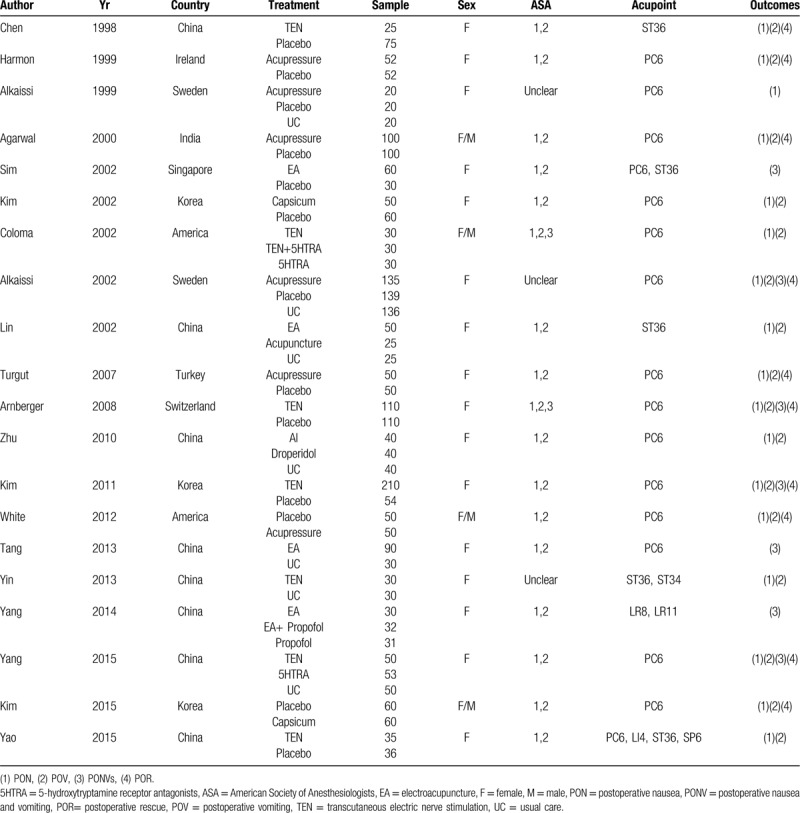
Figure 2.
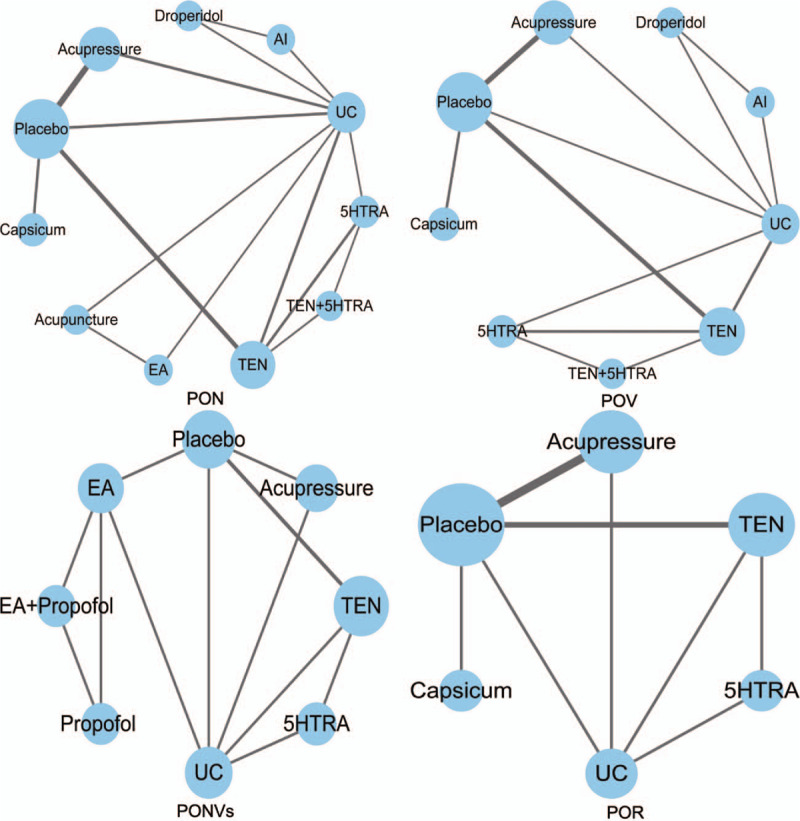
Network plots of interventions.
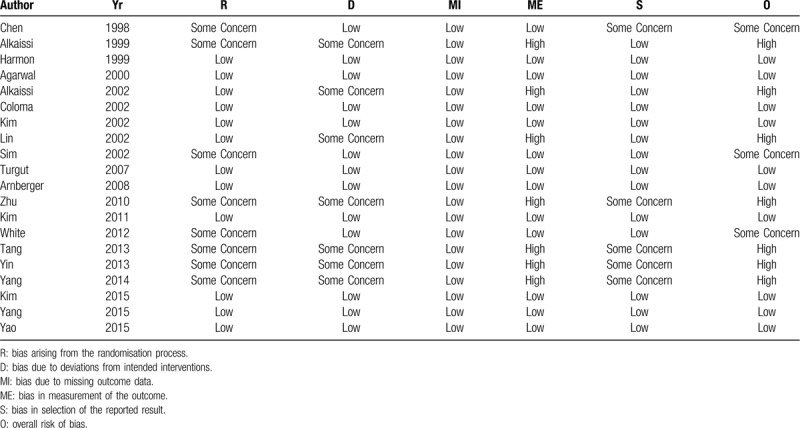
3.2. Methodological evaluation
The risk of bias assessment for the 20 RCTs is summarized in Table 2. About two thirds studies were assessed having low to moderate risk of bias. Twelve studies were considered as low risk in randomization for describing appropriate random sequence generation and concealment. In regard to deviations from intended interventions, 13 studies had low risk for patients were blinded. All studies may have low risk of missing outcome data for the observation time was short and missing data was few. As PONV was reported by patients themselves, 13 studies used placebo so that patients could not recognize which group did they participate. Fifteen studies had low risk in reporting bias for they had got approval from Ethic Committee. When taking all bias into consideration, 10 studies had low risk Appendix 2.
Table 2.
Quality evaluation of enrolled studies.
3.3. Pairwise meta analysis of outcomes
The pairwise meta analysis result concluded by RevMan is displayed in Table 3 and Appendix 5.
Table 3.
Pairwise meta analysis.
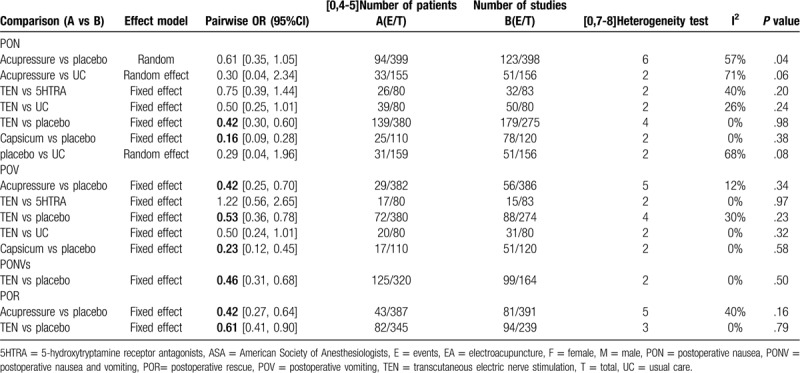
3.3.1. PON
It showed that some acupuncture therapies, compares with placebo, have lower risk of PON (TEN OR = 0.42, 95%CI: 0.30–0.60), (Capsicum OR = 0.16, 95%CI: 0.09–0.28).
3.3.2. POV
Patients use Acupressure, TEN, Capsicum, rather than placebo, have lower risk of POV (Acupressure OR = 0.42, 95%CI: 0.25–0.70), (TEN OR = 0.53, 95%CI: 0.36–0.78), (Capsicum OR = 0.23, 95%CI: 0.12–0.45).
3.3.3. PONVs
Compared with placebo, TEN can lower the risk of PONVs in postoperative 24 hours (OR = 0.46, 95%CI: 0.31–0.68).
3.3.4. POR
Compared with placebo, both Acupressure and TEN can solve with the requirement of POR (Acupressure OR = 0.42, 95%CI: 0.27–0.64), (TEN OR = 0.61, 95%CI: 0.41–0.90).
3.4. Network meta analysis of outcomes
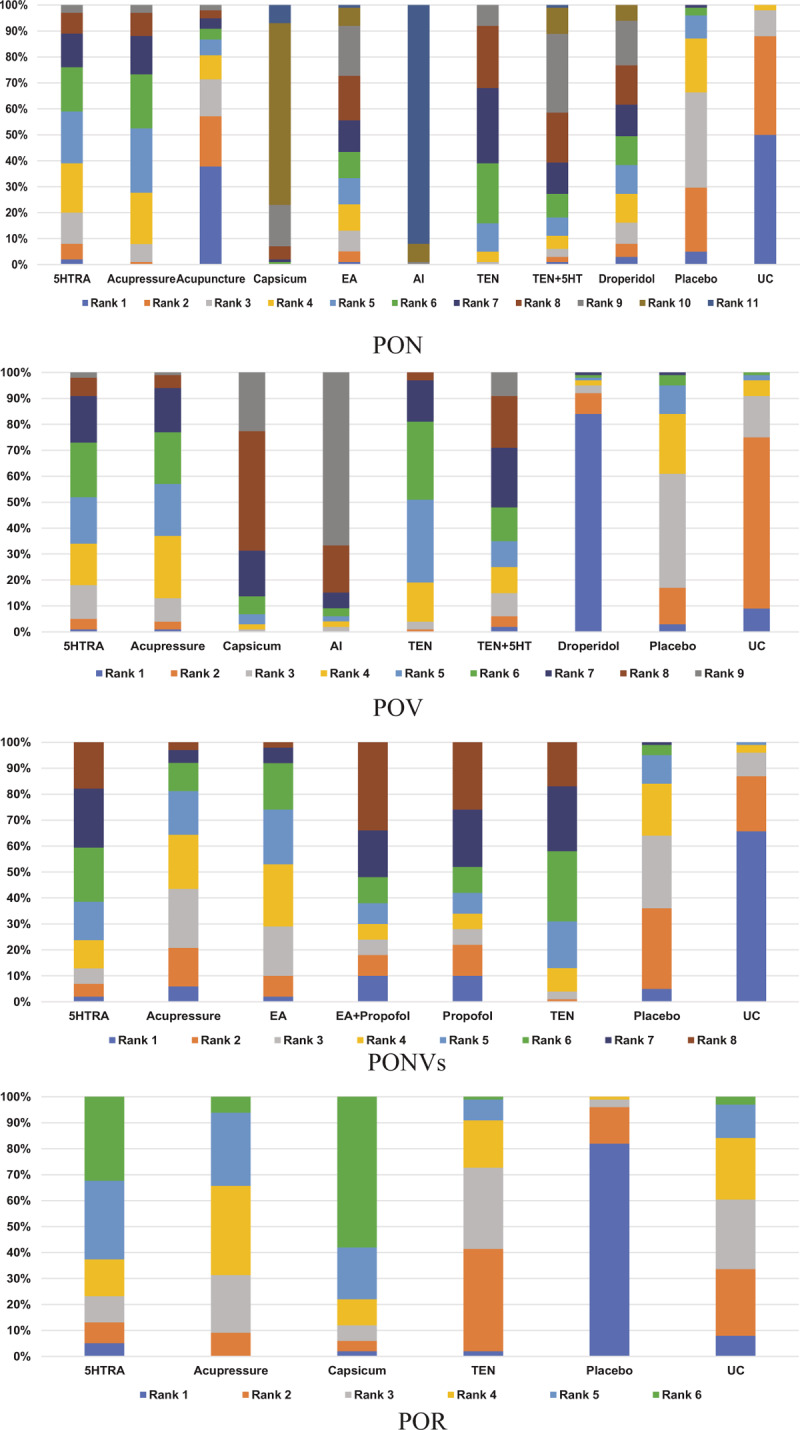
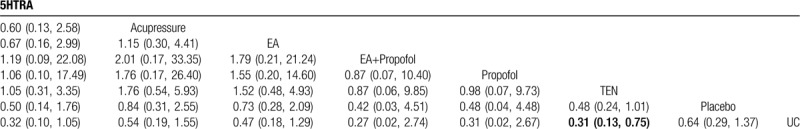
According to the extracted data, parameters of ADDIS were set as initial and the network meta analysis for PON, POV, PONVs, and POR were analyzed. The value of RSPF approximates to 1 which indicates complete convergence (Appendix 3). According to node spilt analysis (Appendix 4) all P values exceeded .05 and consistency model was adopted (Tables 4–7). OR at the left lower part means the odds ratio of vertical to horizontal, a smaller OR value represents a better efficacy. The rank probability plots are displayed in Figure 3.
Table 4.
Network meta analysis for postoperative nausea.
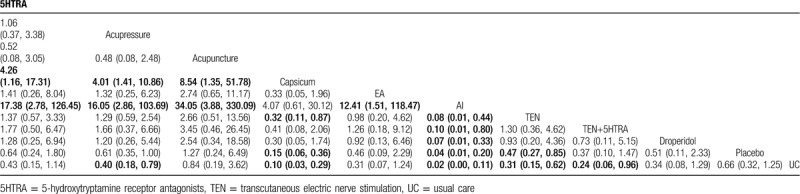
Table 7.
Network meta analysis for postoperative rescue.
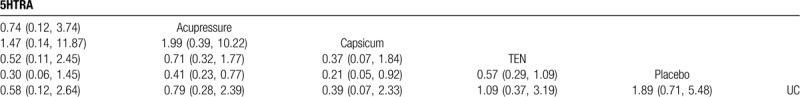
Figure 3.
Rank probability plots.
Table 5.
Network meta analysis for postoperative vomiting.
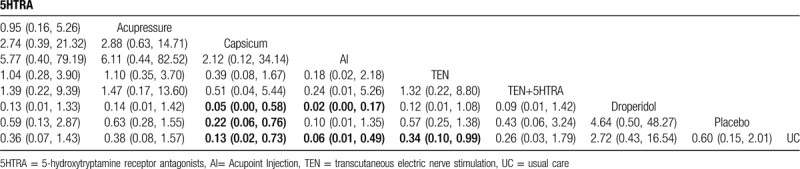
Table 6.
Network meta analysis for postoperative nausea and vomiting.
3.4.1. PON
Compared with placebo and UC, Acupressure, Capsicum, Acupoint Injection (AI), and TEN show significance difference, and especially, combined with rank probability plots, AI has the highest probability to rank first for PON in 24 hours and Capsicum is the secondary best. In addition, the circle of TEN, 5HTRA, and TEN+5HTRA reveals that the combination has lower risk of PON.
3.4.2. POV
Compared with placebo and UC, Capsicum, and AI show significance difference. TEN has lower risk of POV than UC. AI still has the highest probability to rank first for POV in 24 hours. The second and third most effective interventions are Capsicum and TEN respectively. In addition, the circle of TEN, 5HTRA, and TEN+5HTRA reveals that the combination has lower risk of POV.
3.4.3. PONVs
With the help of Figure 3, it suggests that EA + propofol is the best therapy in preventing PONVs while UC is ranked as the worst on the aspect of PONVs. Moreover, TEN is more effective than UC but has no significance difference comparing with placebo.
3.4.4. POR
Acupressure and Capsicum can reduce the use of POR rather than placebo (Acupressure OR = 0.41, 95%CI: 0.23–0.77; Capsicum OR = 0.21, 95%CI: 0.05–0.92). And placebo is worse than UC (OR = 1.89, 95%CI: 0.71–5.48).
4. Discussion
It is still controversial that whether surgery type is a risk factor of PONV,[31,32] but in order to reduce heterogeneity as much as possible, we only chose abdominal surgery into this review. This review aimed to assessed the effect of different acupuncture therapies by using Bayesian meta analysis. The RCTs were acceptable in quality, which is helpful to lift the quality of evidence. The results indicated that acupuncture therapy can reduce the risk of PONV by the combination of direct and indirect evidence. It is in accordance with previous research.[33] Moreover, authors concluded some key findings as follows.
First, all acupuncture therapies taken into this meta analysis, show certain potential to lower the risk of PONV. And in this review, AI is thought as the best choice to prevent PONV, which can treat diseases by synergetic effects of acupuncture and medication.[34] Besides, Tan et al[7] regarded that the efficacy between acupoint stimulation and drugs were comparable, however, considering about the circle of TEN, 5HTRA, and TEN+5HTRA, acupuncture therapy may be more effective in the rank, and the combination may be the best choice, though the results did not reach statistical significance. Thus, more prospective study is needed to strengthen this evidence. Moreover, capsaicin is a pungent substance from chili pepper, and both internal and external use take effect in preventing PON and POV, which gave patients another choice.[35]
Second, based on the evaluation of OR value, acupuncture therapy can provide more protection in PON than POV. Nausea is confused with vomiting in most cases, even recognized as foreboding symptom of vomiting.[36] Actually, nausea is controlled by cerebral cortex and adjacent tissue while the key neural circuits for producing vomiting are located in the medulla. They are 2 reflections with a part of same neuronal pathway. Thus, the variance of effect might be found due to different physiological reaction mechanisms.[37,38]
Third, it is obvious that PC6 and ST36 are the popular choice in this review. According to traditional Chinese medicine theory, PC6 can treat all thoracic and abdominal diseases. Researchers found that PC6 can relieve the intensity of nausea while other acupoints cannot, the mechanism may associate with the modulation of coupling between the cerebellum and insula, which is the specific neural basis.[39] In addition, ST36 is traditionally considered to be an effective acupoint in treating gastrointestinal diseases, and the main symptom of nausea and vomiting is epigastric discomfort. Stimulating ST36 may adjust the gastrointestinal motility by modulating gastric motility via vagovagal and sympathetic reflexes.[40,41] Xu used ST36 and PC6 to treat hiccups, which has similar mechanism with nausea and vomiting in traditional Chinese medicine.[42]
What is more, it is out of our expectation that invasive and non-invasive therapies are comparable in effect. It is well known that pain, bleeding and invasiveness restrict the promotion of acupuncture therapy, and people are more willing to accept non-invasive intervention. Our result provides evidence for this method but further study should be carried out.
To be honest, this study has several limitations. First, a potential limitation was that only 24 hours post operation was considered in the present network meta analysis, acute-PONV, and delayed-PONV were not separated for the lack of data, thus further subgroup analysis was not conducted. Furthermore, except TEN and acupressure, few studies about acupuncture therapies were included, which may limit the credibility of the present results. Another limitation was the unevenness in intervention time, duration, selection of acupoint among clinical trials, which makes it harder to determine the best therapeutic option.[43] Finally, although the ADDIS software is easy to use, it can be constrained by the fact that it cannot be programmed freely. A random effects model can only be reported when estimating the effect size, which may be conservative in estimating our results.[44] Despite these limitations, the comparison of acupuncture therapy in managing PONV was systematically and comprehensively analyzed, which is quite fresh in related research. The results may provide guidance for the prevention of PONV.
In conclusion, the present comprehensive network meta analysis indicates that acupuncture therapies, particularly AI and Capsicum has greater advantages for preventing PONV in abdominal operation compared with placebo and UC. In the light of the increasing importance and interest in PONV, there is a need for high-quality trials to confirm the best choice of acupuncture therapy.
Author contributions
Conceptualization: Chengwei Fu, Yang Jiao.
Data curation: Chengwei Fu, Yang Jiao.
Formal analysis: Chengwei Fu.
Funding acquisition: Qing Shu.
Investigation: Chengwei Fu, Yang Jiao, Aiqun Song.
Project administration: Yang Jiao.
Resources: Chengwei Fu, Tong Wu, Qing Shu.
Software: Chengwei Fu, Yang Jiao.
Supervision: Aiqun Song, Yang Jiao.
Validation: Chengwei Fu.
Visualization: Chengwei Fu.
Writing – original draft: Chengwei Fu.
Writing – review & editing: Yang Jiao.
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Supplementary Material
Footnotes
Abbreviations: 5HTRA = 5-hydroxytryptamine receptor antagonists, AI = Acupoint Injection, CI = confidence interval, OR = odds ratio, PON = postoperative nausea, PONV = postoperative nausea and vomiting, POR= postoperative rescue, POV = postoperative vomiting, PSRF = Potential Scale Reduction Factor, RCTs = randomized controlled trials, TEN = transcutaneous electric nerve stimulation, UC = usual care.
How to cite this article: Fu C, Wu T, Shu Q, Song A, Jiao Y. Acupuncture therapy on postoperative nausea and vomiting in abdominal operation: A Bayesian network meta analysis. Medicine. 2020;99:23(e20301).
This research was supported by the National Nature Science Foundation of China NO. 81804180 and Institute Cooperation Innovation Program NO. YZ-1737.
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request. All data generated or analyzed during this study are included in this published article [and its supplementary information files].
Supplemental Digital Content is available for this article.
References
- [1].Skolnik A, Gan TJ. Update on the management of postoperative nausea and vomiting. Curr Opin Anaesthesiol 2014;27:605–9. [DOI] [PubMed] [Google Scholar]
- [2].Wiesmann T, Kranke P, Eberhart L. Postoperative nausea and vomiting – a narrative review of pathophysiology, pharmacotherapy and clinical management strategies. Expert Opin Pharmacother 2015;16:1069–77. [DOI] [PubMed] [Google Scholar]
- [3].Apfel CC, Laara E, Koivuranta M, et al. A simplified risk score for predicting postoperative nausea and vomiting – conclusions from cross-validations between two centers. Anesthesiology 1999;91:693–700. [DOI] [PubMed] [Google Scholar]
- [4].Cao X, White PF, Ma H. An update on the management of postoperative nausea and vomiting. J Anesth 2017;31:617–26. [DOI] [PubMed] [Google Scholar]
- [5].Habib AS, Gan TJ. Evidence-based management of postoperative nausea and vomiting: a review. CanJ Anaesth 2004;51:326–41. [DOI] [PubMed] [Google Scholar]
- [6].Tateosian VS, Champagne K, Gan TJ. What is new on the battle against post-operative nausea and vomiting? Best Pract Res Clin Anaesthesiol 2018;32:137–48. [DOI] [PubMed] [Google Scholar]
- [7].Gan TJ, Diemunsch P, Habib AS, et al. Consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg 2014;118:85–113. [DOI] [PubMed] [Google Scholar]
- [8].Apfel CC, Korttila K, Abdalla M, et al. A factorial trial of six interventions for the prevention of postoperative nausea and vomiting. N Engl J Med 2004;350:2441–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Cooke M, Rickard C, Rapchuk I, et al. PC6 acupoint stimulation for the prevention of postcardiac surgery nausea and vomiting: a protocol for a two-group, parallel, superiority randomised clinical trial. BMJ Open 2014;4:e006179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Cheong KB, Zhang JP, Huang Y, et al. The effectiveness of acupuncture in prevention and treatment of postoperative nausea and vomiting--a systematic review and meta-analysis. PLoS One 2013;8:e82474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Toth B, Lantos T, Hegyi P, et al. Ginger (Zingiber officinale): An alternative for the prevention of postoperative nausea and vomiting. A meta-analysis. Phytomedicine 2018;50:8–18. [DOI] [PubMed] [Google Scholar]
- [12].Marx W, Kiss N, Isenring L. Is ginger beneficial for nausea and vomiting? An update of the literature. Curr Opin Support Palliat Care 2015;9:189–95. [DOI] [PubMed] [Google Scholar]
- [13].Hines S, Steels E, Chang A, et al. Aromatherapy for treatment of postoperative nausea and vomiting. Cochrane Database Syst Rev 2018;3:CD007598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Cetinkaya F. The effects of listening to music on the postoperative nausea and vomiting. Complement Ther Clin Pract 2019;35:278–83. [DOI] [PubMed] [Google Scholar]
- [15].Gliedt JA, Daniels CJ, Wuollet A. Narrative review of perioperative acupuncture for clinicians. J Acupunct Meridian Stud 2015;8:264–9. [DOI] [PubMed] [Google Scholar]
- [16].Lee A, Chan SK, Fan LT. Stimulation of the wrist acupuncture point PC6 for preventing postoperative nausea and vomiting. Cochrane Database Syst Rev 2015;Cd003281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Stott A. Examining the efficacy of stimulating the PC6 wrist acupuncture point for preventing postoperative nausea and vomiting: a Cochrane review summary. Int J Nurs Stud 2016;64:139–41. [DOI] [PubMed] [Google Scholar]
- [18].Yang J, Jiang Y, Chen Y, et al. Acupressure the PC6 point for alleviating postoperative nausea and vomiting: asystematic review protocol. Medicine (Baltimore) 2019;98:e16857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Cho HK, Park IJ, Jeong YM, et al. Can perioperative acupuncture reduce the pain and vomiting experienced after tonsillectomy? A meta-analysis. Laryngoscope 2016;126:608–15. [DOI] [PubMed] [Google Scholar]
- [20].Shin HC, Kim JS, Lee SK, et al. The effect of acupuncture on postoperative nausea and vomiting after pediatric tonsillectomy: a meta-analysis and systematic review. Laryngoscope 2016;126:1761–7. [DOI] [PubMed] [Google Scholar]
- [21].Keefe KR, Byrne KJ, Levi JR. Treating pediatric post-tonsillectomy pain and nausea with complementary and alternative medicine. Laryngoscope 2018;128:2625–34. [DOI] [PubMed] [Google Scholar]
- [22].Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 2015;162:777–84. [DOI] [PubMed] [Google Scholar]
- [23].Sterne JAC, Savovic J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. [DOI] [PubMed] [Google Scholar]
- [24].Zheng W, Ying J, Zhou Y, et al. The efficacy and safety of first-line chemotherapies for advanced biliary tract cancer: a network meta-analysis. J Cancer 2019;10:257–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Brooks S, Computational AJJo, Statistics G. General methods for monitoring convergence of iterative simulations. J Comput Graph Stat 1998;7:434–55. [Google Scholar]
- [26].Zeng Y, Wan J, Ren H, et al. The influences of anesthesia methods on some complications after orthopedic surgery: a Bayesian network meta-analysis. BMC anesthesiol 2019;19:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].van Valkenhoef G, Lu G, de Brock B, et al. Automating network meta-analysis. Res Synth Method 2012;3:285–99. [DOI] [PubMed] [Google Scholar]
- [28].Padilha S, Virtuoso S, Tonin FS, et al. Efficacy and safety of drugs for attention deficit hyperactivity disorder in children and adolescents: a network meta-analysis. Eur Child Adolesc Psychiatry 2018;27:1335–45. [DOI] [PubMed] [Google Scholar]
- [29].Dias S, Welton NJ, Caldwell DM, et al. Checking consistency in mixed treatment comparison meta-analysis. Stat Med 2010;29:932–44. [DOI] [PubMed] [Google Scholar]
- [30].Du T, Quan S, Dong T, et al. Comparison of surgical procedures implemented in recent years for patients with grade III and IV hemorrhoids: a network meta-analysis. Int J Colorectal Dis 2019;34:1001–12. [DOI] [PubMed] [Google Scholar]
- [31].Stadler M, Bardiau F, Seidel L, et al. Difference in risk factors for postoperative nausea and vomiting. Anesthesiology 2003;98:46–52. [DOI] [PubMed] [Google Scholar]
- [32].Apfel CC, Heidrich FM, Jukar-Rao S, et al. Evidence-based analysis of risk factors for postoperative nausea and vomiting. Br J Anaesth 2012;109:742–53. [DOI] [PubMed] [Google Scholar]
- [33].Liu Y, Tang WPY, Gong S, et al. A systematic review and meta-analysis of acupressure for postoperative gastrointestinal symptoms among abdominal surgery patients. Am J Chin Med 2017;45:1127–45. [DOI] [PubMed] [Google Scholar]
- [34].Wang LQ, Chen Z, Zhang K, et al. Zusanli (st36) acupoint injection for diabetic peripheral neuropathy: a systematic review of randomized controlled trials. J Altern Complement Med 2018;24:1138–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Al Kury LT, Mahgoub M, Howarth FC, et al. Natural negative allosteric modulators of 5-HT(3) receptors. Molecules 2018;23:3186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Sanger GJ, Andrews PLR. A history of drug discovery for treatment of nausea and vomiting and the implications for future research. Front Pharmacol 2018;9:913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Balaban CD, Yates BJ. What is nausea? A historical analysis of changing views. Auton Neurosci Clin 2017;202:5–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Horn CC, Wallisch WJ, Homanics GE, et al. Pathophysiological and neurochemical mechanisms of postoperative nausea and vomiting. Eur J Pharmacol 2014;722:55–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Bai L, Niu X, Liu Z, et al. The role of insula-cerebellum connection underlying aversive regulation with acupuncture. Mol Pain 2018;14:1744806918783457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Lu MJ, Yu Z, He Y, et al. Electroacupuncture at ST36 modulates gastric motility via vagovagal and sympathetic reflexes in rats. World J Gastroenterol 2019;25:2315–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Sun ZG, Pi YL, Zhang J, et al. Effect of acupuncture at ST36 on motor cortical excitation and inhibition. Brain Behav 2019;9:e01370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Xu J, Qu Y, Yue Y, et al. Treatment of persistent hiccups after arthroplasty: effects of acupuncture at PC6, CV12 and ST36. Acupunct Med 2019;37:72–6. [DOI] [PubMed] [Google Scholar]
- [43].Kim KH, Kim DH, Bae JM, et al. Acupuncture and PC6 stimulation for the prevention of postoperative nausea and vomiting in patients undergoing elective laparoscopic resection of colorectal cancer: a study protocol for a three-arm randomised pilot trial. BMJ Open 2017;7:e013457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Feng J, Cui N, Wang Z, et al. Bayesian network meta-analysis of the effects of single-incision laparoscopic surgery, conventional laparoscopic appendectomy and open appendectomy for the treatment of acute appendicitis. Exp Ther Med 2017;14:5908–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


