Abstract
Novel agonists of the nuclear liver-X-receptor (LXR) are designed to treat metabolic disorders or cancer. The rationale to develop these new drugs is based on promising results with established LXR agonist like T0901317 and GW3965. LXRα and LXRβ are expressed in β-cells, and expression is increased by T0901317. The aim of the present study was to evaluate whether effects of these drugs on β-cell function are specific and reliably linked to LXR activation. T0901317 and GW3965, widely used as specific LXR agonists, show rapid, non-genomic effects on stimulus-secretion coupling of mouse pancreatic β-cells at low µM concentrations. T0901317 lowered the cytosolic Ca2+ concentration, reduced or completely inhibited action potentials, and decreased insulin secretion. GW3965 exerted similar effects on insulin secretion. T0901317 affected the production of reactive oxygen species and ATP. The involvement of the classical nuclear LXRs in T0901317- and GW3965-mediated effects in β-cells could be ruled out using LXRα, LXRβ and double knockout mice. Our results strongly suggest that LXR agonists, that are considered to be specific for this receptor, interfere with mitochondrial metabolism and metabolism-independent processes in β-cells. Thus, it is indispensable to test novel LXR agonists accompanying to ongoing clinical trials for acute and chronic effects on cell function in cellular systems and/or animal models lacking classical LXRs.
Keywords: Stimulus-secretion coupling, Cytosolic Ca2+ concentration, Insulin secretion, LXR, T0901317, GW3965
Introduction
The liver-X-receptor (LXR) is known to influence cholesterol and lipid metabolism in the liver [1, 2]. The classical subtypes LXRα and LXRβ mediate their effects as nuclear receptors [3]. During the last decade, several effects of LXR on other organs e.g. muscle, adipose tissue and hypothalamus and mitochondria were reported which are important players in the regulation of glucose metabolism (for review see [4]). Besides this, the capability of LXR ligands to influence the concentration of reactive oxygen species (ROS) and to reduce endoplasmic reticulum stress opens new application spectra for LXR agonists particularly against metabolic diseases [5–7]. The suggested pathways are diverse and include cytosolic signal cascades [8], and/or changes in gene expression [9]. In obese animal models of diabetes LXR activation by synthetic agonists improves insulin sensitivity and glucose tolerance [10–12]. The effects were contributed to interference with different pathways in liver, muscle and adipose tissue. In contrast, a study with mice fed a normal diet revealed that T0901317 application in vivo impairs glucose metabolism by decreasing glucose sensitivity and insulin secretion [13]. The findings are not supported by a study with LXRβ-deficient mice: LXRβ−/− mice on low and high fat diet show improved glucose tolerance while LXRβ−/− mice on a standard chow are glucose intolerant [14].
A few studies have tested effects of LXR activation on β-cell function and survival. One study reports that GW3965 protects human islets in vitro against inflammation [15]. The authors suggest LXR activation as a strategy for improving post-transplant islet survival. Another paper shows that T0901317 can protect human, mouse and rat β-cells against palmitate-induced toxicity [16]. Stearoyl-CoA desaturase (SCD) activation seems to be crucial in this cytoprotective effect. Mice lacking LXRα or LXRβ elicit reduced SCD expression. Accordingly, they are more prone to palmitate toxicity. One study with human islets and another one with rat β-cells and MIN6 cells observe increased insulin secretion after LXR activation with T0901317 or GW3965 [17, 18]. The effects are contributed to interaction with enzymes involved in lipid metabolism. In contrast, Meng et al. demonstrate that T0901317 leads to β-cells dysfunction. They show with mouse β-cells and MIN6 cells reduced insulin secretion in response to LXR activation accompanied by decreased oxygen consumption, ATP production and current through L-type Ca2+ channels [13].
All these in vivo and in vitro studies were long-term studies with the LXR agonists T0901317 or GW3965. Possible acute or non-LXR-mediated effects were not considered in these studies.
Recently, we showed activation of a non-genomic rapid pathway by 10 µM T0901317 that negatively influenced insulin secretion in murine and human pancreatic β-cells [19]. The LXR agonist interfered with stimulus-secretion coupling (SSC) by inhibiting the ATP synthesis probably due to effects on the ROS concentration [19]. In the present study, we challenge the assumption that effects of T0901317 or GW3965 can reliably be attributed to LXR activation. Our results question the specificity of the so-called LXR agonists that provide the basis for the development of novel drugs.
Research design and methods
Cell and islet preparation
Details are described in [20]. In brief, mouse islets were isolated by injecting collagenase (0.5–1 mg/ml) into the pancreas, and by handpicking after digestion at 37 °C. Male and female wild type C57Bl/6 mice were used in equal shares. Development of mice with general ablation of LXRα and LXRβ are described in [21]. All LXR knockout (LXR−/−) mice are on a C57Bl/6 background and were housed under same conditions. Mice were bred in the animal facility of the Department of Pharmacology at the University of Tübingen. Principles of laboratory animal care (NIH publication no. 85–23, revised 1985) and German laws were followed. Mouse islets were dispersed to single cells and cell clusters, respectively, by trypsin treatment.
Solutions and chemicals
Recordings of the cytosolic Ca2+ concentration ([Ca2+]c) were performed with a bath solution which contained (mM): 140 NaCl, 5 KCl, 1.2 MgCl2, 2.5 CaCl2, glucose as indicated, 10 HEPES and pH 7.4 adjusted with NaOH. Same bath solution was used for determination of the mitochondrial membrane potential (ΔΨ), ROS and membrane potential (Vm) measurements in the perforated-patch configuration. The bath solution was modified by adding 0.1% bovine serum albumin (BSA) and used as incubation medium for ATP measurements. Krebs–Ringer–HEPES (KRH) solution for measurements of insulin secretion was composed of (mM): 120 NaCl, 4.7 KCl, 1.1 MgCl2, 2.5 CaCl2, glucose as indicated, 10 HEPES, 0.5% BSA and pH 7.4 adjusted with NaOH. Pipette solution for measurements of Vm consisted of (mM): 10 KCl, 10 NaCl, 70 K2SO4, 4 MgCl2, 2 CaCl2, 10 EGTA, 20 HEPES, 0.27 amphotericin B and pH adjusted to 7.15 with KOH. Islet cell clusters and pancreatic islets were cultured in RPMI 1640 (11.1 mM glucose) enriched with 10% foetal calf serum (FCS) and 1% penicillin/streptomycin.
T0901317 and GW3965 were obtained from Biomol (Hamburg, Germany). Fura-2-AM was purchased from Biotrend (Köln, Germany) and 25-OH cholesterol from Santa Cruz (Heidelberg, Germany). Rhodamine 123 (Rh123), RPMI 1640 medium, FCS, penicillin/streptomycin, 2′,7′-dichlorodihydrofluorescein-diacetate (DCDHF-DA), dihydroethidium (DHE), ATP determination kit and trypsin were from Invitrogen (Karlsruhe, Germany). All other chemicals were purchased from Sigma (Taufkirchen, Germany) or Merck (Darmstadt, Germany) in the purest form available.
Measurement of [Ca2+]c
Details are described in [20]. In brief, cells were loaded with 5 µM Fura-2-AM for 35 min at 37 °C. The fluorescence was excited at 340 nm and 380 nm and the emission was measured. [Ca2+]c was calculated according to an in vitro calibration. The maximum amplitude of Ca2+ oscillations (max. [Ca2+]c) was taken to compare [Ca2+]c under different experimental conditions.
ATP measurement
Details are described in [19]. 20 islets were kept for 30 min at 37 °C in incubation medium under conditions as indicated. After cell lyses by adding a solution containing 200 mM NaOH and 0.5 mM EDTA, ATP concentration was elicited by the ATP determination kit according to manufactures instructions. Bioluminescence was determined with Luminometer 1253 (Bioorbit, Turku, Finland) in triplicate. Data were normalised to control condition under 15 mM glucose.
Patch-clamp measurements
Vm measurements were recorded with an EPC-9 patch-clamp amplifier using Patchmaster software (HEKA, Lambrecht, Germany) with the perforated-patch configuration in the current clamp mode at a holding current of 0 mA. For determination of Vm average plateau potential was evaluated 1 min before solution change. The same time interval was used for determination of action potential frequency.
Insulin secretion
Details for steady-state incubations are described in [20]. Briefly, batches of five islets in triplicate were incubated in 1 ml KRH for 1 h at 37 °C under conditions as indicated. In experiments in which acute effects were investigated, the agonists were only present during the 1 h secretion measurement. To determine chronic effects, the agonists were absent during the 1 h secretion phase but the islets were pre-incubated for 72 h with agonists as indicated. Insulin was determined by radioimmunoassay (Merck Millipore, Darmstadt, Germany) with rat insulin as standard.
Measurements of ΔΨ
ΔΨ was measured as Rh123 fluorescence (arbitrary units (a.u.) at 480 nm excitation wave length as described elsewhere [22]. To evaluate the effects, the values were averaged over 150 s at the end of each interval, i.e. before solution change.
Measurement of ROS
ROS production was measured using the fluorescent dyes DCDHF-DA and DHE. In the cells DCDHF-DA is oxidised to the fluorescent 2′,7′-dichlorofluorescein (DCF), which detects H2O2 and other ROS species. DHE is oxidised to 2-hydroxyethidium (2-OH-E+), which mainly indicates O2− formation. After 1 h incubation under conditions as indicated, the islet cell clusters were loaded for 15 min with 20 µM DCDHF-DA and 10 µM DHE, respectively. Fluorescence was excited at 480 nm and the intensity of the emitted light (arbitrary units (a.u.) was measured.
Statistics
Each series of experiments was performed with islets or islet cell clusters from at least three different mice. Means ± SEM are given for the indicated number of experiments (islet cell clusters or islets). Statistical significance of differences was assessed by a paired Student’s t test. Multiple comparisons were made by repeated ANOVA followed by the Student–Newman–Keuls test. P values ≤ 0.05 were considered significant.
Results
LXR agonists acutely affect SSC in β-cells
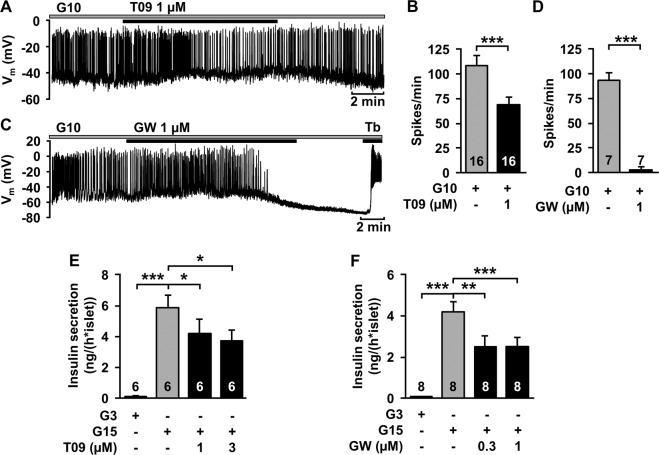
Recently, we made the unexpected observation that 10 µM T0901317 exerts acute effects on SSC in β-cells [19]. Thus, in a first approach we investigated effects of lower concentrations of T0901317 on β-cell function, which are most likely more specific for the LXR, and compared it to another drug which is assumed to be a specific LXR ligand, GW3965. One micromolar T0901317 reduced the frequency of action potentials (Fig. 1a, b). GW3965 (1 µM) mimicked this effect on Vm (Fig. 1c, d). As expected from these observations, acute administration of T0901317 (1 µM and 3 µM) and GW3965 (0.3 µM and 1 µM), respectively, inhibited glucose-stimulated insulin secretion (Fig. 1e, f). Metabolic integrity of the β-cells is shown by increased insulin secretion at stimulating glucose concentration (15 mM) compared with a sub-stimulatory concentration (3 mM).
Fig. 1.
LXR agonists acutely inhibit stimulus-secretion coupling in wild type β-cells. a Representative recording of Vm with administration of T0901317 (T09). b Summary of all experiments. n = 16. c Representative recording of Vm with administration of GW3965 (GW). Tolbutamide (Tb) was given at the end of the experiment to test whether closure of KATP channels is still possible. d Summary of all experiments. n = 7. e Glucose-induced insulin secretion is reduced by T0901317 compared with control islets in the presence of 15 mM glucose (G15). n = 6. f GW3965 also decreased glucose-induced insulin secretion. n = 8. Experiments were performed with different islet cell clusters or islets from 3–7 mice. *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001
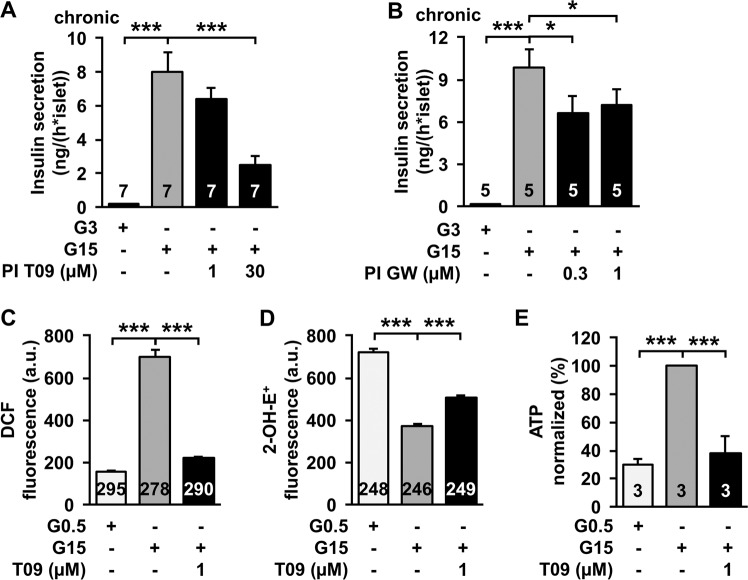
Chronic administration of LXR agonists inhibits insulin secretion
In the literature effects of LXR agonists are described solely after chronic administration. Therefore, we performed insulin secretion experiments after 72 h pre-incubation with the same agonists that showed acute effects. Although, no agonists were present during the 1 h secretion measurement, glucose-stimulated insulin secretion was decreased after pre-incubation with T0901317 and GW3965 (Fig. 2a, b). Remarkably, acute and chronic administration of the drugs revealed comparable effects.
Fig. 2.
LXR agonists influence β-cell metabolism. a Glucose-induced insulin secretion after 72 h pre-incubation (PI) with T0901317 compared with control conditions in the presence of 15 mM glucose. T0901317 was not present during the 1 h of steady-state incubation for the determination of insulin secretion. n = 7. b Glucose-induced insulin secretion after 72 h pre-incubation with GW3965. GW3965 was not present during the 1 h secretion measurement. n = 5. c Measurement of DCF-detectable oxidants in islet cell clusters. Increasing the glucose concentration from 0.5 to 15 mM leads to enhanced DCF-fluorescence. Administration of T0901317 in the presence of 15 mM glucose resulted in a massive reduction of DCF-detectable ROS. n = 278–295. d Determination of 2-OH-E+-detectable oxidants in islet cell clusters. Increasing the glucose concentration from 0.5 to 15 mM reduces the fluorescence. T0901317 leads to an increase of 2-OH-E+-detectable ROS at high glucose concentration. n = 246–249. e Measurement of ATP concentration in intact islets. ATP content of islets is significantly reduced by T0901317 in comparison to control islets kept in 15 mM glucose. n = 3. Experiments were performed with different islet cell clusters or islets from 3–7 mice. *P ≤ 0.05, ***P ≤ 0.001
T0901317 influences ATP synthesis and ROS production
The SSC in β-cells is triggered by ATP synthesis due to redox processes within mitochondria. Increasing the glucose concentration from 0.5 to 15 mM led to enhanced DCF fluorescence (mainly H2O2 production) in islet cell clusters. Administration of T0901317 in the presence of 15 mM glucose resulted in a massive reduction of DCF-detectable ROS. (Fig. 2c). In contrast, enhancing the glucose concentration from 0.5 to 15 mM reduced 2-OH-E+-detectable ROS (mainly O2−) while T0901317 provoked an increase of 2-OH-E+-detectable oxidants at high glucose concentration. Likewise, ATP concentration under high glucose condition measured in intact islets was critically reduced by T0901317 (Fig. 2e). Metabolic integrity was shown by increased ATP concentration at stimulating glucose concentration (15 mM) compared with a sub-stimulatory concentration (3 mM).
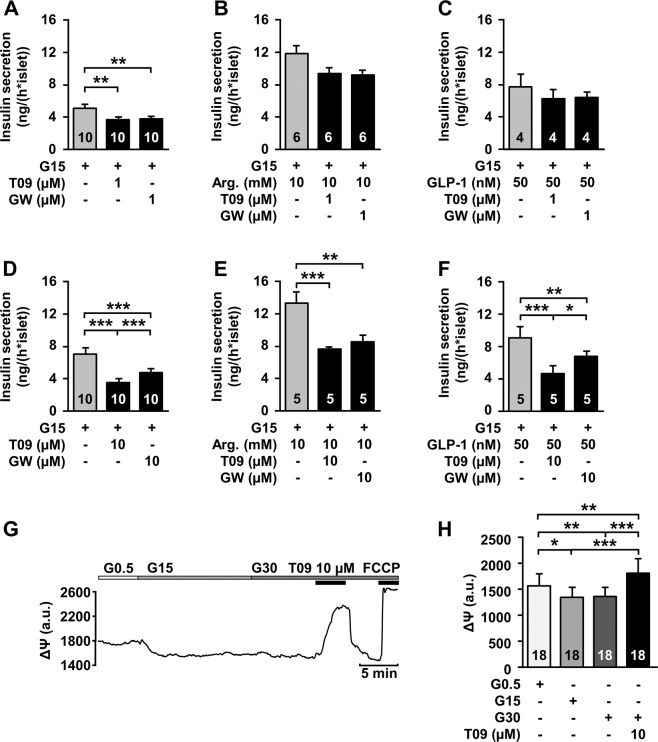
LXR agonists interfere with metabolism-independent processes
The effects of the LXR agonists on ATP and ROS production point to interference with mitochondrial metabolism. We evaluated whether the agonists could also influence mitochondria-independent β-cell stimulation by arginine or GLP-1. Figure 3a–c shows that arginine as well as GLP-1 strongly attenuated the inhibiting effect of 1 µM T0901317 and 1 µM GW3965, respectively. However, in the presence of higher concentrations of the agonists (10 µM) arginine or GLP-1 could not diminish the inhibitory effect of the drugs (Fig. 3d–f). Interestingly, even 30 mM glucose could not hinder the strong depolarisation of ΔΨ induced by 10 µM T0901317 (Fig. 3g, h), which reflects inhibition of ATP production.
Fig. 3.
LXR agonists exerts metabolism-independent effects. Influence of 1 µM T0901317 (T09) and 1 µM GW3965 (GW), respectively, on insulin secretion in the presence of 15 mM glucose (a, control), 10 mM arginine (b) and 50 nM GLP-1 (c). n = 4–10. The agonists had no significant effects in the presence of arginine or GLP-1. Inhibiting effect of 10 µM T0901317 (T09) and 10 µM GW3965 (GW), respectively, on insulin secretion in the presence of 15 mM glucose (d, control), 10 mM arginine (e) and 50 nM GLP-1 (f). n = 5–10. Administration of 10 µM T0901317 on ΔΨ in the presence of 30 mM glucose still reveals a strong depolarisation. g Representative recording of ΔΨ with administration of T0901317. Metabolic integrity is shown by a rapid depolarisation by 0.5 µM FCCP. h Summary of all experiments. n = 18. Experiments were performed with different islet cell clusters or islets from 3–10 mice. *P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001
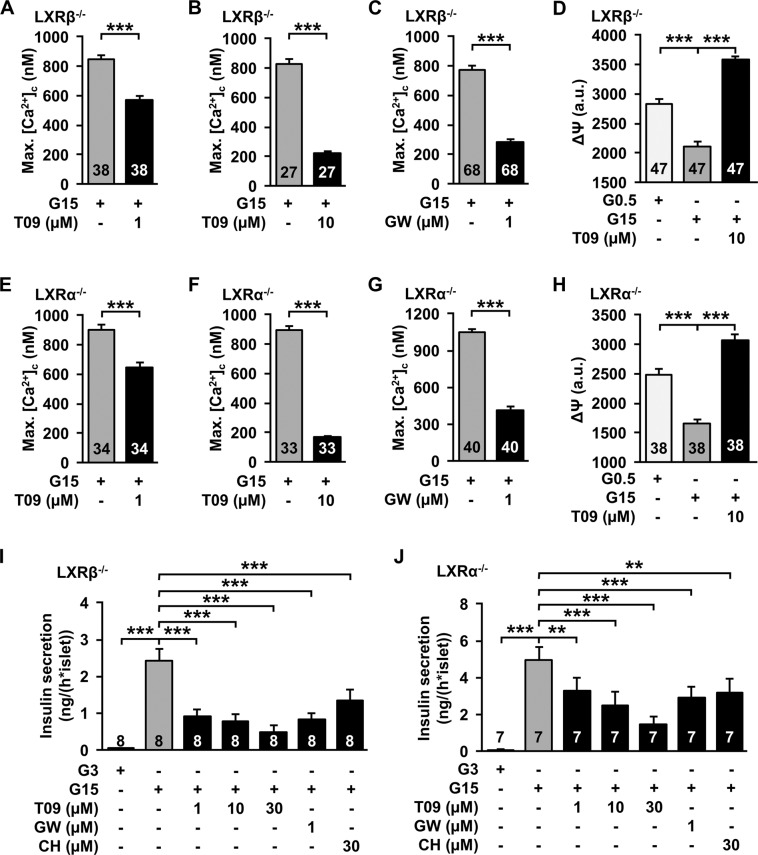
LXR agonists acutely affect SSC in β-cells of LXR−/− mice
Similar effects of different LXR agonists suggest that the LXR is indeed targeted by the drugs. We tested the effects of T0901317 and GW3965 in β-cells isolated from LXRβ−/− mice. Both agonists decreased maximal [Ca2+]c (max.[Ca2+]c) and T0901317 depolarised ΔΨ under stimulating glucose condition (Fig. 4a–d). As the results did not show any impact of the LXRβ−/−, the measurements were repeated with β-cells isolated from LXRα−/− mice. In LXRα−/− β-cells T0901317 and GW3965 decreased max.[Ca2+]c (Fig. 4e–g). Like the previous observation, T0901317 depolarised ΔΨ in these knockout islet cell clusters (Fig. 4h). Accordingly, acute administration of T0901317 and GW3965 inhibited glucose-stimulated insulin secretion in pancreatic islets of LXRα−/− and LXRβ−/− mice, respectively (Fig. 4i, j). In these series of experiments we tested in addition the endogenous LXR agonist 25-OH-cholesterol, which revealed similar results (Fig. 4i, j).
Fig. 4.
Effects of LXR agonists are present in LXR−/− β-cells in the presence of 15 mM glucose. a, b T0901317 (1 µM and 10 µM) reduce maximal [Ca2+]c in β-cells of LXRβ−/− mice. n = 38 and 27. c 1 µM GW3965 reduces maximal [Ca2+]c in β-cells of LXRβ−/− mice. n = 68. d 10 µM T0901317 depolarises ΔΨ in islet-cell clusters of LXRβ−/− mice. Metabolic integrity is shown by hyperpolarisation of ΔΨ after changing the glucose concentration from 0.5 to 15 mM. n = 47. e, f 1 µM and 10 µM T0901317 reduce maximal [Ca2+]c in β-cells of LXRα−/− mice. n = 34 and 33. g 1 µM GW3965 reduces maximal [Ca2+]c in β-cells of LXRα−/− mice. n = 40. h 10 µM T0901317 depolarises ΔΨ in islet cell clusters of LXRα−/− mice. n = 38. i, j Glucose-induced insulin secretion is reduced by T0901317, GW3965 and 25-OH-cholesterol (CH) in islets from LXRβ−/− and LXRα−/− mice. n = 8 and 7. Experiments were performed with different islet cell clusters or islets from 3–8 mice. **P ≤ 0.01, ***P ≤ 0.001
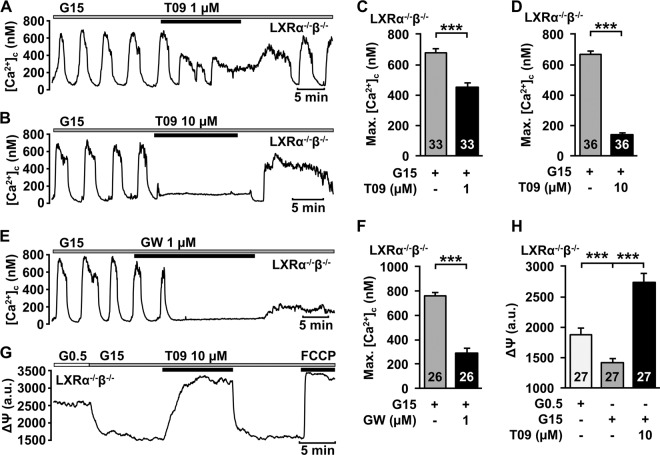
To exclude a possible compensation of LXRα or LXRβ by higher protein expression of the corresponding receptor in the respective knockout model, a double knockout mouse model with the concurrent deletion of LXRα and LXRβ was used. In β-cells of these mice the effect of T0901317 and GW3965 on max.[Ca2+]c was still present (Fig. 5a–f). The higher concentration of T0901317 completely abolished glucose-dependent Ca2+ oscillations (Fig. 5b). The drop in [Ca2+]c directly after removal of T0901317 points to ATP-dependent SERCA activation after ATP depletion [19]. Accordingly, T0901317 depolarised ΔΨ in LXRα−/−β−/− islet cell clusters under high glucose condition (Fig. 5g, h).
Fig. 5.
Acute effects of LXR agonists are present in LXRα−/−β−/− β-cells. a, b Representative measurements showing inhibition of glucose-induced oscillations of [Ca2+]c by 1 µM T0901317 (a) and 10 µM T0901317 (b) in the presence of 15 mM glucose in β-cells of LXRα−/−β−/− mice. c, d 1 µM and 10 µM T0901317 reduces maximal [Ca2+]c in β-cells of LXRα−/−β−/− mice. n = 33 and 36. e Representative measurement showing inhibition of glucose-induced oscillations of [Ca2+]c by 1 µM GW3965 in the presence of 15 mM glucose in β-cells of LXRα−/−β−/− mice. f 1 µM GW3965 reduces the maximal [Ca2+]c in β-cells of LXRα−/−β−/− mice. n = 26. g Representative measurement of ΔΨ in islet cells of LXRα−/−β−/− mice. Increasing the glucose concentration from 0.5 to 15 mM leads to hyperpolarization of ΔΨ due to enhanced ATP production. Administration of T0901317 results in rapid and reversible depolarisation of ΔΨ. Metabolic integrity is shown by a rapid depolarisation by 0.5 µM FCCP. h Summary of all experiments of this series. n = 27. Experiments were performed with different islet cell clusters from three mice. ***P ≤ 0.001
Discussion
Reputed LXR agonists acutely affect SSC by non-genomic actions
Several studies show effects on metabolism after long exposure to reputed LXR agonists including T0901317 and suggest genomic actions [9–13, 15–18]. In the present study 1 µM T0901317 and GW3965 acutely inhibited SSC in pancreatic β-cells within a few minutes. Evidently, the observed effects were not limited to high concentration of the agonists (T0901317 in [19]), but also occur with lower concentrations of the drugs (T0901317 and GW3965 in this study) that are assumed to be more specific. A genomic pathway is highly unlikely due to the fast onset of the effects seen in patch-clamp experiments and Ca2+ measurements.
Remarkably, T0901317 affects platelet aggregation of nucleus free thrombocytes [23–25]. Furthermore, rapid effects of T0901317 were observed in colon cancer cells [26, 27]. These observations support our findings that LXR agonists can act in a non-genomic manner, independent from transcription processes in the nucleus.
Meanwhile, non-genomic actions of ligands formerly classified as typical agonists of nuclear receptors are well accepted; e.g. oestrogens activate cytosolic signal cascades in β-cells [28–30]. Interestingly, the nuclear oestrogen receptor (ER) can translocate to the cell membrane, where it triggers rapid signalling [31, 32]. Moreover, 17β-oestradiol can directly modify KATP channel activity and interfere with the SUR1 channel subunit in β-cells [29, 33]. Furthermore, a rapid, cytosolic pathway that alters KATP activity in β-cells is shown for the nuclear farnesoid-X-receptor [34].
The classical nuclear LXR does not activate the acute pathway induced by T0901317 and GW3965 in β- cells
The role of LXRs in β-cell function is not completely understood. Data obtained with WT mouse or human islets in which synthetic LXR agonists have been used and LXR-deficient islets as well as in vivo and in vitro findings reveal many inconsistencies (see Introduction). There is not even unity whether LXR activation leads to stimulatory or inhibitory effects in vitro and to beneficial or detrimental effects in vivo. One reason for this complex situation may be that LXRs can exert opposite function in lean and obese animals, i.e. the function depends on the dietary state [14]. A similar function dependency on the nutritional situation has been described for the FXR earlier [35]. Another reason for contradictory findings may be the fact that synthetic LXR activators exert rapid, non-genomic, unspecific effects (see below).
We used LXR−/− mice to evaluate the role of classical LXRs in the actions of the reputed LXR agonists. The ubiquitously identified LXRβ does not influence the acute actions of LXR agonists in β-cells, shown by experiments with cells from LXRβ−/− mice. Compared with the LXRβ, the LXRα seems to be less abundant in mouse islets and not detectable in β-cells [36]. We show that the α-subtype also does not participate in the acute effects of GW3965 and T0901317 in β-cells. A third reputed LXR agonist, 25-OH-cholesterol, which is believed to be the endogenous activator of the receptor also suppresses glucose-induced insulin secretion in both genotypes.
To circumvent a possible counter-regulatory upregulation of LXRα in LXRβ−/− cells and vice versa, cells from LXRα−/−β−/− mice were used. Even in these cells, GW3965 and T0901317 exerted their inhibitory effects on SSC. The results clearly point to a mechanism independent of the classical LXRs.
The fact that three chemically different so-called LXR agonists act in an analogue manner suggests the presence of a different target with a binding profile like the classical LXR. The rapid effects, most likely evoked by cytosolic signal cascades, point to an action of this non-classical LXR at the membrane or in the cytosol. The paper of Meng et al. [13] and our studies (this and [19]) point to interaction with mitochondria i.e. changes in ROS production and ATP depletion as one possible mode of action in β-cells. The action of low concentrations of T0901317 and GW3965 could be counteracted by increasing insulin secretion with either arginine or GLP-1. This seems to be irrespective of the mechanism because arginine depolarises via influx of positive ions, and GLP-1 by stimulating the amplifying pathway via an increase of the cAMP concentration. The data suggest that low concentrations of the drugs can affect SSC beyond interference with mitochondrial metabolism. However, at higher concentrations (10 µM) of the agonists, arginine and GLP-1 did not prevent the inhibitory effect any more suggesting that at this concentration the effect on mitochondrial metabolism prevails. This assumption is further supported by the fact that increasing the glucose concentration to the maximal depolarising effect of glucose (30 mM) did not suppress the strong depolarisation of ΔΨ provoked by T0901317.
The functionality of mitochondrial processes is essential in all organs and cell systems. Therefore, several effects attributed to LXR in different cell types may be caused by the interaction of LXR agonists with mitochondrial function. As a result, our data question conclusion about the involvement of LXR in physiological processes drawn from studies with T0901317 or GW3965 without use of LXR-deficient cell systems or mice.
A word of caution
Previous results of studies with established LXR ligands led to the development of new LXR agonists for therapeutic use in cancer and metabolic diseases. Very recently, it has been shown that LXR agonism by GW3965, and the novel LXR ligand RGX-104 enhances the activation of cytotoxic T-lymphocytes in mice and humans with cancer [37]. A clinical phase 1 study was accomplished with the LXR agonist BMS-852927 [38]. The authors draw the conclusion that BMS-852927 exerts beneficial effects on hypercholesterolaemia in humans by activation of the LXR. But they also observed adverse effects e.g. on lipogenesis and neutrophilic granulocytes in healthy volunteers questioning the therapeutic impact [38]. Another first-in-human study with the LXR ligand LXR-623 was performed with healthy participants to test a possible application of LXR agonists in the therapy of arteriosclerosis [39]. In this study, LXR-623 led to increased appearance of adverse events related to the central nervous system [39].
We show unspecific actions of well-established LXR agonists suggesting re-interpretation of previous results. The exact target mediating the observed rapid effects is still unknown. This leads to a more complex assessment of possible risk factors, and side effects of all LXR agonists. Thus, it is indispensable to intensify the research with potential new drugs with respect to acute, LXR-independent effects.
Acknowledgements
We acknowledge the excellent and skilful technical assistance of Isolde Breuning. We are grateful to Jan Ake Gustafsson, Karolinska Institute, Sweden for providing the knockout mice. This work was supported by a grant from the DFG (G.D.). Open Access funding provided by Projekt DEAL.
Author contributions
J.M. and J.K. researched data, wrote and edited the paper. P.K.-D. contributed to discussion and study design and edited the paper; G.D. designed the study, wrote and edited the paper, contributed to discussion, and is the guarantor of this study.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Peet DJ, Turley SD, Ma W, Janowski BA, Lobaccaro JM, Hammer RE, Mangelsdorf DJ. Cholesterol and bile acid metabolism are impaired in mice lacking the nuclear oxysterol receptor LXR alpha. Cell. 1998;93(5):693–704. doi: 10.1016/S0092-8674(00)81432-4. [DOI] [PubMed] [Google Scholar]
- 2.Janowski BA, Willy PJ, Devi TR, Falck JR, Mangelsdorf DJ. An oxysterol signalling pathway mediated by the nuclear receptor LXR alpha. Nature. 1996;383(6602):728–731. doi: 10.1038/383728a0. [DOI] [PubMed] [Google Scholar]
- 3.Peet DJ, Janowski BA, Mangelsdorf DJ. The LXRs: a new class of oxysterol receptors. Curr. Opin. Genet. Dev. 1998;8(5):571–575. doi: 10.1016/s0959-437x(98)80013-0. [DOI] [PubMed] [Google Scholar]
- 4.Steffensen KR, Gustafsson JA. Putative metabolic effects of the liver X receptor (LXR) Diabetes. 2004;53(Suppl 1):S36–S42. doi: 10.2337/diabetes.53.2007.S36. [DOI] [PubMed] [Google Scholar]
- 5.Ferderbar S, Pereira EC, Apolinario E, Bertolami MC, Faludi A, Monte O, Calliari LE, Sales JE, Gagliardi AR, Xavier HT, Abdalla DS. Cholesterol oxides as biomarkers of oxidative stress in type 1 and type 2 diabetes mellitus. Diabetes Metab. Res. Rev. 2007;23(1):35–42. doi: 10.1002/dmrr.645. [DOI] [PubMed] [Google Scholar]
- 6.Chang L, Zhang Z, Li W, Dai J, Guan Y, Wang X. Liver-X-receptor activator prevents homocysteine-induced production of IgG antibodies from murine B lymphocytes via the ROS-NF-kappaB pathway. Biochem. Biophys. Res. Commun. 2007;357(3):772–778. doi: 10.1016/j.bbrc.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 7.He Q, Pu J, Yuan A, Lau WB, Gao E, Koch WJ, Ma XL, He B. Activation of liver-X-receptor alpha but not liver-X-receptor beta protects against myocardial ischemia/reperfusion injury. Circ. Heart Fail. 2014;7(6):1032–1041. doi: 10.1161/CIRCHEARTFAILURE.114.001260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.He Q, Pu J, Yuan A, Yao T, Ying X, Zhao Y, Xu L, Tong H, He B. Liver X receptor agonist treatment attenuates cardiac dysfunction in type 2 diabetic db/db mice. Cardiovascular Diabetol. 2014;13(1):149. doi: 10.1186/s12933-014-0149-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dong Y, Gao G, Fan H, Li S, Li X, Liu W. Activation of the liver X receptor by agonist TO901317 improves hepatic insulin resistance via suppressing reactive oxygen species and JNK pathway. PLoS ONE. 2015;10(4):e0124778. doi: 10.1371/journal.pone.0124778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baranowski M, Zabielski P, Blachnio-Zabielska AU, Harasim E, Chabowski A, Gorski J. Insulin-sensitizing effect of LXR agonist T0901317 in high-fat fed rats is associated with restored muscle GLUT4 expression and insulin-stimulated AS160 phosphorylation. Cell Physiol. Biochem. 2014;33(4):1047–1057. doi: 10.1159/000358675. [DOI] [PubMed] [Google Scholar]
- 11.Laffitte BA, Chao LC, Li J, Walczak R, Hummasti S, Joseph SB, Castrillo A, Wilpitz DC, Mangelsdorf DJ, Collins JL, Saez E, Tontonoz P. Activation of liver X receptor improves glucose tolerance through coordinate regulation of glucose metabolism in liver and adipose tissue. Proc. Natl. Acad. Sci. USA. 2003;100(9):5419–5424. doi: 10.1073/pnas.0830671100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cao G, Liang Y, Broderick CL, Oldham BA, Beyer TP, Schmidt RJ, Zhang Y, Stayrook KR, Suen C, Otto KA, Miller AR, Dai J, Foxworthy P, Gao H, Ryan TP, Jiang XC, Burris TP, Eacho PI, Etgen GJ. Antidiabetic action of a liver x receptor agonist mediated by inhibition of hepatic gluconeogenesis. J. Biol. Chem. 2003;278(2):1131–1136. doi: 10.1074/jbc.M210208200. [DOI] [PubMed] [Google Scholar]
- 13.Meng ZX, Yin Y, Lv JH, Sha M, Lin Y, Gao L, Zhu YX, Sun YJ, Han X. Aberrant activation of liver X receptors impairs pancreatic beta cell function through upregulation of sterol regulatory element-binding protein 1c in mouse islets and rodent cell lines. Diabetologia. 2012;55(6):1733–1744. doi: 10.1007/s00125-012-2516-2. [DOI] [PubMed] [Google Scholar]
- 14.Gerin I, Dolinsky VW, Shackman JG, Kennedy RT, Chiang SH, Burant CF, Steffensen KR, Gustafsson JA, MacDougald OA. LXRbeta is required for adipocyte growth, glucose homeostasis, and beta cell function. J. Biol. Chem. 2005;280(24):23024–23031. doi: 10.1074/jbc.M412564200. [DOI] [PubMed] [Google Scholar]
- 15.Scholz H, Lund T, Dahle MK, Collins JL, Korsgren O, Wang JE, Foss A. The synthetic liver X receptor agonist GW3965 reduces tissue factor production and inflammatory responses in human islets in vitro. Diabetologia. 2009;52(7):1352–1362. doi: 10.1007/s00125-009-1366-z. [DOI] [PubMed] [Google Scholar]
- 16.Hellemans KH, Hannaert JC, Denys B, Steffensen KR, Raemdonck C, Martens GA, Van Veldhoven PP, Gustafsson JA, Pipeleers D. Susceptibility of pancreatic beta cells to fatty acids is regulated by LXR/PPARalpha-dependent stearoyl-coenzyme A desaturase. PLoS ONE. 2009;4(9):e7266. doi: 10.1371/journal.pone.0007266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ogihara T, Chuang JC, Vestermark GL, Garmey JC, Ketchum RJ, Huang X, Brayman KL, Thorner MO, Repa JJ, Mirmira RG, Evans-Molina C. Liver X receptor agonists augment human islet function through activation of anaplerotic pathways and glycerolipid/free fatty acid cycling. J. Biol. Chem. 2010;285(8):5392–5404. doi: 10.1074/jbc.M109.064659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Efanov AM, Sewing S, Bokvist K, Gromada J. Liver X receptor activation stimulates insulin secretion via modulation of glucose and lipid metabolism in pancreatic beta-cells. Diabetes. 2004;53(Suppl 3):S75–S78. doi: 10.2337/diabetes.53.suppl_3.S75. [DOI] [PubMed] [Google Scholar]
- 19.Maczewsky J, Sikimic J, Bauer C, Krippeit-Drews P, Wolke C, Lendeckel U, Barthlen W, Drews G. The LXR ligand T0901317 acutely inhibits insulin secretion by affecting mitochondrial metabolism. Endocrinology. 2017;158(7):2145–2154. doi: 10.1210/en.2016-1941. [DOI] [PubMed] [Google Scholar]
- 20.Gier B, Krippeit-Drews P, Sheiko T, Aguilar-Bryan L, Bryan J, Düfer M, Drews G. Suppression of KATP channel activity protects murine pancreatic beta cells against oxidative stress. J. Clin. Investig. 2009;119(11):3246–3256. doi: 10.1172/JCI38817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alberti S, Schuster G, Parini P, Feltkamp D, Diczfalusy U, Rudling M, Angelin B, Bjorkhem I, Pettersson S, Gustafsson JA. Hepatic cholesterol metabolism and resistance to dietary cholesterol in LXRbeta-deficient mice. J. Clin. Investig. 2001;107(5):565–573. doi: 10.1172/JCI9794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Edalat A, Schulte-Mecklenbeck P, Bauer C, Undank S, Krippeit-Drews P, Drews G, Düfer M. Mitochondrial succinate dehydrogenase is involved in stimulus-secretion coupling and endogenous ROS formation in murine beta cells. Diabetologia. 2015;58(7):1532–1541. doi: 10.1007/s00125-015-3577-9. [DOI] [PubMed] [Google Scholar]
- 23.Spyridon M, Moraes LA, Jones CI, Sage T, Sasikumar P, Bucci G, Gibbins JM. LXR as a novel antithrombotic target. Blood. 2011;117(21):5751–5761. doi: 10.1182/blood-2010-09-306142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Unsworth AJ, Bye AP, Tannetta DS, Desborough MJR, Kriek N, Sage T, Allan HE, Crescente M, Yaqoob P, Warner TD, Jones CI, Gibbins JM. Farnesoid X receptor and liver X receptor ligands initiate formation of coated platelets. Arterioscler. Thromb. Vasc. Biol. 2017;37(8):1482–1493. doi: 10.1161/ATVBAHA.117.309135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schaffer S, Tandon R, Zipse H, Siess W, Schmidt A, Jamasbi J, Karshovska E, Steglich W, Lorenz R. Stereo specific platelet inhibition by the natural LXR agonist 22(R)-OH-cholesterol and its fluorescence labelling with preserved bioactivity and chiral handling in macrophages. Biochem. Pharm. 2013;86(2):279–285. doi: 10.1016/j.bcp.2013.04.024. [DOI] [PubMed] [Google Scholar]
- 26.Derangere V, Chevriaux A, Courtaut F, Bruchard M, Berger H, Chalmin F, Causse SZ, Limagne E, Vegran F, Ladoire S, Simon B, Boireau W, Hichami A, Apetoh L, Mignot G, Ghiringhelli F, Rebe C. Liver X receptor beta activation induces pyroptosis of human and murine colon cancer cells. Cell Death Differ. 2014;21(12):1914–1924. doi: 10.1038/cdd.2014.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rebe C, Derangere V, Ghiringhelli F. Induction of pyroptosis in colon cancer cells by LXRbeta. Mol. Cell Oncol. 2015;2(1):e970094. doi: 10.4161/23723548.2014.970094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ropero AB, Soria B, Nadal A. A nonclassical estrogen membrane receptor triggers rapid differential actions in the endocrine pancreas. Mol. Endocrinol. 2002;16(3):497–505. doi: 10.1210/mend.16.3.0794. [DOI] [PubMed] [Google Scholar]
- 29.S. Soriano, A.B. Ropero, P. Alonso-Magdalena, C. Ripoll, I. Quesada, B. Gassner, M. Kuhn, J.A. Gustafsson, A. Nadal, Rapid regulation of K(ATP) channel activity by 17{beta}-estradiol in pancreatic {beta}-cells involves the estrogen receptor {beta} and the atrial natriuretic peptide receptor. Mol. Endocrinol. 23(12), 1973–1982 (2009). 10.1210/me.2009-0287 [DOI] [PMC free article] [PubMed]
- 30.Revankar CM, Cimino DF, Sklar LA, Arterburn JB, Prossnitz ER. A transmembrane intracellular estrogen receptor mediates rapid cell signaling. Science. 2005;307(5715):1625–1630. doi: 10.1126/science.1106943. [DOI] [PubMed] [Google Scholar]
- 31.W.P. Wong, J.P. Tiano, S. Liu, S.C. Hewitt, C. Le May, S. Dalle, J.A. Katzenellenbogen, B.S. Katzenellenbogen, K.S. Korach, F. Mauvais-Jarvis, Extranuclear estrogen receptor-α stimulates NeuroD1 binding to the insulin promoter and favors insulin synthesis. Proc. Natl. Acad. Sci. 107(29), 13057–13062 (2010) [DOI] [PMC free article] [PubMed]
- 32.Levin ER, Hammes SR. Nuclear receptors outside the nucleus: extranuclear signalling by steroid receptors. Nat. Rev. Mol. Cell Biol. 2016;17(12):783–797. doi: 10.1038/nrm.2016.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ackermann S, Hiller S, Osswald H, Lösle M, Grenz A, Hambrock A. 17β-Estradiol modulates apoptosis in pancreatic β-cells by specific involvement of the sulfonylurea receptor (SUR) isoform SUR1. J. Biol. Chem. 2009;284(8):4905–4913. doi: 10.1074/jbc.M807638200. [DOI] [PubMed] [Google Scholar]
- 34.Düfer M, Hörth K, Wagner R, Schittenhelm B, Prowald S, Wagner TF, Oberwinkler J, Lukowski R, Gonzalez FJ, Krippeit-Drews P, Drews G. Bile acids acutely stimulate insulin secretion of mouse beta-cells via farnesoid X receptor activation and K(ATP) channel inhibition. Diabetes. 2012;61(6):1479–1489. doi: 10.2337/db11-0815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schittenhelm B, Wagner R, Kähny V, Peter A, Krippeit-Drews P, Düfer M, Drews G. Role of FXR in beta-Cells of Lean and Obese Mice. Endocrinology. 2015;156(4):1263–1271. doi: 10.1210/en.2014-1751. [DOI] [PubMed] [Google Scholar]
- 36.Zitzer H, Wente W, Brenner MB, Sewing S, Buschard K, Gromada J, Efanov AM. Sterol regulatory element-binding protein 1 mediates liver X receptor-beta-induced increases in insulin secretion and insulin messenger ribonucleic acid levels. Endocrinology. 2006;147(8):3898–3905. doi: 10.1210/en.2005-1483. [DOI] [PubMed] [Google Scholar]
- 37.Tavazoie MF, Pollack I, Tanqueco R, Ostendorf BN, Reis BS, Gonsalves FC, Kurth I, Andreu-Agullo C, Derbyshire ML, Posada J, Takeda S, Tafreshian KN, Rowinsky E, Szarek M, Waltzman RJ, McMillan EA, Zhao C, Mita M, Mita A, Chmielowski B, Postow MA, Ribas A, Mucida D, Tavazoie SF. LXR/ApoE activation restricts innate immune suppression in cancer. Cell. 2018;172(4):825–840 e818. doi: 10.1016/j.cell.2017.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kirchgessner TG, Sleph P, Ostrowski J, Lupisella J, Ryan CS, Liu X, Fernando G, Grimm D, Shipkova P, Zhang R, Garcia R, Zhu J, He A, Malone H, Martin R, Behnia K, Wang Z, Barrett YC, Garmise RJ, Yuan L, Zhang J, Gandhi MD, Wastall P, Li T, Du S, Salvador L, Mohan R, Cantor GH, Kick E, Lee J, Frost RJ. Beneficial and adverse effects of an LXR agonist on human lipid and lipoprotein metabolism and circulating neutrophils. Cell Metab. 2016;24(2):223–233. doi: 10.1016/j.cmet.2016.07.016. [DOI] [PubMed] [Google Scholar]
- 39.Katz A, Udata C, Ott E, Hickey L, Burczynski ME, Burghart P, Vesterqvist O, Meng X. Safety, pharmacokinetics, and pharmacodynamics of single doses of LXR-623, a novel liver X-receptor agonist, in healthy participants. J. Clin. Pharm. 2009;49(6):643–649. doi: 10.1177/0091270009335768. [DOI] [PubMed] [Google Scholar]