Abstract
Dissemination and implementation science seeks generalizable knowledge about closing the gap between clinical discovery and actual use in routine practice and public health. The field of infectious diseases enjoys an abundance of highly efficacious interventions (eg, antimicrobial agents, human immunodeficiency virus treatment) which are not adequately used in routine care, thereby missing critical opportunities to improve population health. In this article, we summarize salient features of dissemination and implementation science, reviewing definitions and methodologies for infectious diseases clinicians and researchers. We give examples of the limited use of dissemination and implementation science in infectious diseases thus far, suggest opportunities for application, and provide resources for interested readers to use and apply to their own research and practice.
Keywords: dissemination and implementation, knowledge transfer, knowledge exchange, implementation science
Dissemination and implementation science seeks to systematically bridge research-to-practice gaps, but is underutilized in infectious diseases. In this viewpoint, we introduce dissemination and implementation science and summarize its salient features for infectious diseases clinicians and researchers.
Research in infectious diseases (ID) has yielded remarkable scientific discoveries and interventions that have improved life across the globe. Infections which formerly decimated populations (eg, smallpox and polio) have been eradicated (or nearly so) by vaccinations. However, many infections linger, while others have changed or emerged. Although effective interventions are available for various infections, they are often slow to reach clinical practice and public awareness. Furthermore, effective interventions can be complicated and nuanced, making their use in real-world settings, as opposed to clinical trials, challenging. Dissemination and implementation (D&I) science is a relatively new field that seeks to maximize the benefits of scientific discovery to improve population health, achieving our full return on investment [1]. Toward this end, D&I research is the scientific study of methods to promote the systematic uptake and long-term maintenance of research findings and other evidence-based practices into routine practice and, hence, to improve the quality and effectiveness of health services [2]. In short, D&I science gets the evidence where it is needed by closing the gap between evidence and practice.
The field of ID would benefit from enhanced use of D&I science, given its impact on clinical outcomes demonstrated in other disciplines [3–6]. ID is fortunate to have numerous, highly efficacious clinical interventions. Antibiotics, when delivered appropriately for bacterial infections, save lives rapidly and inexpensively. Vaccines, when widely used, drastically reduce morbidity and mortality. Direct-acting antivirals cure hepatitis C in nearly 100% of persons who complete therapy. Yet today, we fail to deliver timely antibiotics to septic patients who could benefit and, at the same time, vastly overuse antibiotics in those without indications (thus compromising future effectiveness through resistance). News headlines report a rising tide of anti-vaccine sentiments, as well as large outbreaks of dangerous viruses once considered controlled (ie, measles). Hepatitis C remains highly prevalent and direct-acting antivirals use is inequitable. Each of these examples illustrate why ID needs D&I science. Despite gaps in implementation across the field, as of the writing of this article, only 0.3% of active National Institute of Allergy and Infectious Diseases R01 projects are funded through D&I-specific funding announcements [7, 8]. Notably, although problems translating discovery into practice are found throughout medicine, we focus here on ID.
WHAT IS DISSEMINATION AND IMPLEMENTATION SCIENCE?
D&I science is often considered in the context of translational research. Unlike earlier phases of translational research (T1–T2), which establish the efficacy of an intervention, D&I falls into T3–T4 research, where clinical (ie, real-world) testing of the innovation occurs. A tenet of D&I science is that an intervention, practice, or policy should have a strong evidence base before it is implemented; that is, it should be an evidence-based intervention (EBI). D&I science primarily focuses on how to get clinicians/health systems to adopt and use EBIs. However, the goal of D&I science is not simply for clinicians to “do more,” but rather for systems to make using EBIs the default or the easiest choice and, at the same time, to remove/replace inefficient or ineffective practices. This may be accomplished at multiple levels through multiple stakeholders, involving policy, economic, and organizational factors, among others.
Here, we limit subdivisions of D&I science into (1) dissemination and (2) implementation. Dissemination is “an active approach of spreading evidence-based interventions to the target audience via determined channels using planned strategies” [9–11]. Implementation is the “scientific study of the use of strategies to adopt and integrate evidence-based health interventions into clinical and community settings in order to improve patient outcomes and benefit population health” [7]. D&I science is variably known as knowledge translation, knowledge integration, knowledge transfer, knowledge exchange, population health intervention research, or diffusion. For simplicity, we will use only the terms dissemination and implementation.
Common research questions addressed by D&I researchers are:
1. What is the most effective approach to make practitioners or the public aware of new treatment guidelines so that the guidelines can be used?
2. How can we help practitioners integrate the latest scientific evidence with their clinical expertise to make better treatment decisions for patients?
3 Can we adapt an intervention that is successful in one population to another population?
4. When practitioners are aware of a new intervention, what are the barriers that prevent them from using it and what are the best strategies to overcome identified barriers?
In addition to these kinds of research questions, D&I science recognizes that current evidence can be difficult for clinicians to access [12–15], and their knowledge of evidence gives them no means to integrate it into practice. Passive approaches to disseminating research, such as publishing exclusively in scientific journals, are ineffective for making practitioners aware of new evidence [16, 17]. Furthermore, it can be difficult to use or implement the latest evidence into practice, particularly when studied populations differ in critical ways from the practitioner’s patient. Most research interventions take place in controlled settings with a well-defined population that is motivated to participate by incentives. In practice, the environment of the intervention is less rigid and more prone to fluctuations and adaptations. The target population may be more heterogeneous, encompass different demographics, or be less motivated to participate/continue the intervention than the studied sample [18]. Exemplifying real-world heterogeneity, Dolcini et al [19] studied 6 California agencies that received funding by the Centers for Disease Control and Prevention to implement 3 different evidence-based, behavioral interventions for human immunodeficiency virus (HIV) prevention. Of the 6 agencies, 5 had to adapt the intervention they chose to accommodate the needs of their target populations. This included adding/deleting program sessions, translating to another language, integrating the program into other services, and nonsystematic adaptations to the intervention [19]. Even if practitioners are aware of an effective intervention and when to use it, there may be other factors, like cost, that may prohibit access [20]. D&I science can also help focus on modification of larger, structural issues, rather than just more well-recognized, front-line organizational practices (eg, making sure everyone performs hand hygiene). That is, societal and political priorities (eg, public opinion, policy decisions, research priorities) can be understood, addressed, and influenced by approaches and strategies identified through the methodologies of D&I science [21].
Fundamental Concepts in Dissemination and Implementation: Theory, Frameworks, and Methods
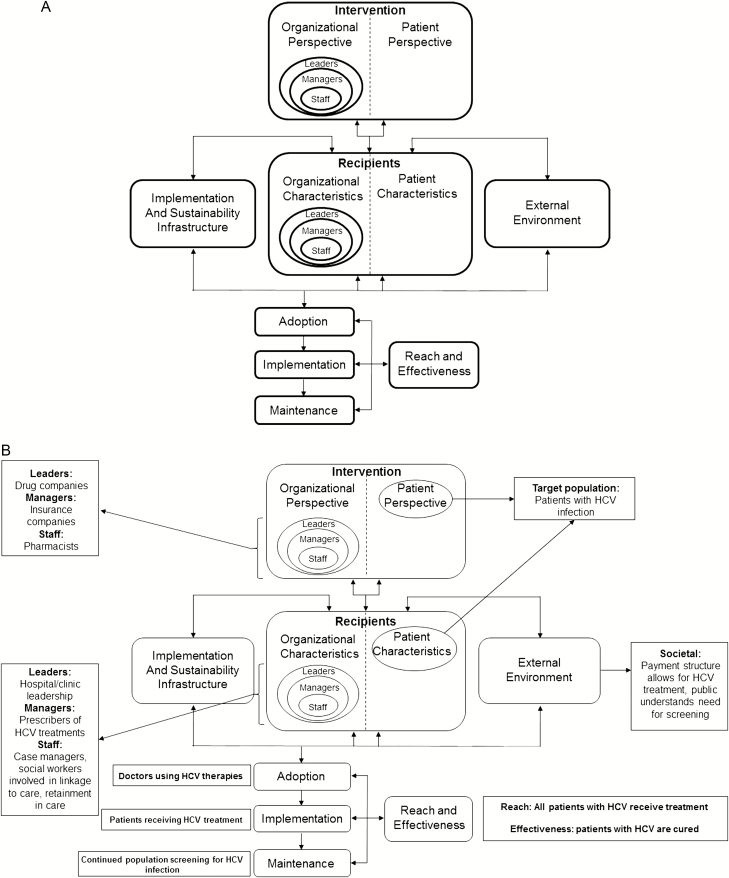
Understanding the local context and relationships between stakeholders (eg, leaders, physicians, patients) are important concepts in D&I science. Keys to the success of intervention implementations include understanding the relationship between evidence, the local context of implementation, the intervention’s use by clinicians (or lack thereof) to improve service delivery, and subsequent patient outcomes [22, 23]. The field of D&I uses theory and frameworks to guide conceptualization of these relationships. Frameworks emphasize the multilevel contexts that influence the translation of evidence into practice, considering providers, organizations, governmental policy, and society as a whole (see Figure 1) [24]. Multi-level refers to the different levels of stakeholders, which could include those in Figure 1: organizations, leaders, managers, and individuals.
Figure 1.
A, PRISM, an example of an implementation science framework that considers the multilevel involvement of relevant stakeholders, including recipients, interventionists, leaders, managers, staff, policymakers, and society as a whole. Adapted from Feldstein and Glasgow [24]. B, The PRISM framework, imagined for HCV management across the implementation issues currently faced. Abbreviations: HCV, hepatitis C virus; PRISM, practical, robust implementation and sustainability model.
There are many available frameworks for D&I research, which can be tailored and combined to best fit the needs of the study, investigators, and the practice setting. Frameworks are particularly useful for clinical experts with deep knowledge about medicine, but limited experience thinking about the behaviors of health-care workers, patients, communities, and organizations. A full description of D&I frameworks is outside the scope of this viewpoint, but interested readers can seek out an excellent review on the topic [23].
D&I researchers use various research designs and analyses, including quantitative, qualitative, and mixed-method approaches [25]. Because it is often unclear why practitioners or patients do not use an intervention, qualitative methods, particularly adept at explaining phenomena, help D&I researchers understand the myriad factors that serve as barriers/hinder use of an intervention or serve as facilitators/promote the uptake of an intervention. [27] Like any scientific inquiry, research design is carefully selected based on the research question, constraints of the research setting, available budget, and etc. However, D&I researchers must address several special challenges. D&I researchers often must assume there is sufficient evidence that an intervention is beneficial. Operating under this assumption, it would be unethical to withhold treatment or continue to provide standard-of-care treatments, as is commonly done during randomized, controlled trials (RCTs). D&I research also frequently works with a small number of organizations or a set of practitioners, making it difficult to adequately power RCTs. Lastly, clinical efficacy trials are often well supported by academic institutions and conducted using eligibility criteria that minimize variability and maximize internal validity [27, 28]. D&I research seeks to maximize the benefit of evidence for the maximum number of populations or settings: that is, to maximize external validity.
The limited external validity of traditional research has led to the development of alternative study designs, including hybrid trials and the stepped-wedge trial. Hybrid designs measure both implementation outcomes and clinical/patient outcomes to help parse questions about whether intervention implementation or evidence behind an intervention is the problem for lack of effectiveness [29]. The stepped-wedge design (or cluster-randomized trial) allows D&I researchers to conduct RCTs where randomization determines when participants will receive an intervention. In stepped-wedge studies, the unit of randomization is not the patient, as in traditional RCTs, but larger groups: for example, an organization, system, practice, clinic, or provider. This design allows all participants and their patients to benefit from implementation of the latest evidence while simultaneously requiring fewer participants.
Implementation Strategies: Conceptualizing and Specifying
Once issues that help (facilitators) or hinder (barriers) the uptake of evidence are identified, D&I researchers pick from a cache of well-studied implementation strategies, which are designed to expedite or enhance the dissemination and implementation of evidence. There are numerous implementation strategies, but recent taxonomic efforts have defined several broad categories, including evaluative strategies, interactive assistance, innovation tailoring, relationship development with stakeholders, stakeholder education and training, providing supplemental support, engaging consumers, leveraging financial mechanisms, or changing system infrastructure [30]. A researcher may select one or multiple strategies to improve evidence implementation, simultaneously testing the effectiveness of these approaches. For example, if leadership interest or support is a significant barrier to patients’ access to a highly effective treatment, stakeholders at levels that might not typically be engaged must be involved for success. These include, but are not limited to, health services researchers, economists, sociologists, community health providers, politicians, “C-suite” executives, patients, and community members.
The reader may be familiar with several implementation strategies without recognizing their ties to implementation science. Audit and feedback, used often and successfully in antimicrobial stewardship efforts, is an example of an implementation strategy. Appeals to social norms and peer performance are implementation strategies that can teach antimicrobial stewardship, as demonstrated by a recent RCT [31]. Changes to record systems (ie, electronic medical records) is an implementation strategy that has been successful in ID. An example involved changing order sets to have reflex urine testing rather than isolated urine cultures, resulting in reductions in positive urine cultures with negative urinalyses [32]. Train-the-trainer is another implementation strategy that has been successfully used in Ebola preparedness for personal protective equipment donning and doffing [33, 34].
Implementation Outcomes: Concepts and Reporting
D&I researchers assess implementation strategy success by measuring implementation outcomes upstream of patient outcomes that indicate the successful dissemination and implementation of evidence. D&I researchers also distinguish between interventions that are not effective and interventions that are not implemented correctly, thereby appearing ineffective. Common, so-called implementation outcomes include: adoption, or uptake of an intervention among organizations or providers; fidelity, or the extent to which patients or providers maintain adherence to how the intervention is intended to be delivered; and penetration or reach, or the extent to which the population of individuals that would benefit from an intervention are using it. For a more comprehensive list of implementation outcomes and definitions, see Table 1. Implicit in the measurement of implementation outcomes is the assumption that improving the dissemination and implementation of an EBI will subsequently improve patient and population outcomes. Table 2 provides an example of the importance of tracking implementation outcomes, as interventions can fail by implementation rather than effectiveness. From a population at risk for HIV infection, only 9.1% made it to the maintenance and adherence stage of taking pre-exposure prophylaxis (PrEP) [35]. Without the measurement of intermediate implementation outcomes (adherence/adoption), it would appear that ~90% of patients were failing PrEP.
Table 1.
Dissemination and Implementation Outcomes
| Implementation Outcome | Examples of Synonym(s)/Antonym(s) |
|---|---|
| Acceptability | Agreeable, acceptable, usability |
| Adoption | Uptake, utilization, initial implementation, intention to try, de-implementation, de-adoption, de-institutionalization |
| Appropriateness | Fit, usefulness |
| Feasibility | Utility |
| Fidelity | Adherence, integrity, adaptation |
| Implementation cost | Marginal cost, cost-effectiveness, cost-benefit, incremental cost, cost impact |
| Penetration | Spread, service access, saturation, reach |
| Sustainability | Maintenance, continuation, integration, sustained use, abandonment |
Table 2.
From Effective Intervention to Failed Implementation: Human Immunodeficiency Virus Prevention With Pre-Exposure Prophylaxis
| Stage | Retention |
|---|---|
| At-risk population | 100% |
| PrEP contemplation | 47.3% |
| PrEParation | 23.9% |
| PrEP action and initiation | 12.9% |
| PrEP maintenance and adherence | 9.1% |
Adapted from [35]. Stages correspond to those in the transtheoretical model of change: contemplation (PrEP contemplation), determination (PrEParation), action (PrEP action and initiation), and maintenance (PrEP maintenance and adherence).
Abbreviation: PrEP, pre-exposure prophylaxis.
Infectious Diseases: Examples of Where We Need Dissemination and Implementation
As a field, ID has many areas with robust evidence of clinical efficacy and effectiveness that lack only implementation science to get the evidence to patients. We use 5 examples to illustrate this point. Ignaz Semmelweis became the first proponent of hand hygiene in 1847, yet it remains incompletely implemented, even in intensive care units (ICUs), where sick patients at high risk of hospital-acquired infections reside [36]. Antimicrobial stewardship programs are highly effective [37, 38] and progress is being made, but adherence to the Centers for Disease Control and Prevention’s 7 core elements of antimicrobial stewardship programs remains under 50% [39]. This deficiency does not take into account the incomplete implementation of antimicrobial stewardship programs in outpatient settings, long-term care settings, or other countries, all of which could be aided by D&I science [39].
On the virology side of ID, human papillomavirus vaccination is so effective in preventing cervical cancer that Australia estimates they will eliminate cervical cancer by 2028 after a string of policy and practice implementation successes [40]. This success has not been realized worldwide, including in the United States, where human papillomavirus vaccination rates are a dismal 49% [41], resulting in unnecessary morbidity and mortality. The efficacy of PrEP for HIV prevention has been well established [42], but significant barriers to implementation remain, as <10% of eligible patients continue using PrEP [35]. Implementation science gives us tools to address these gaps in the application of effective treatments, such as through assessing barriers and facilitators and through community engagement. Similar issues have arisen in the management of hepatitis C, for which there are well-proven and effective treatments. Only about half of patients with hepatitis C infections are diagnosed and aware of their infection, 16% are prescribed treatment, and 9% achieve a sustained virologic response [43]. Figure 1B maps hepatitis C management to the practical, robust implementation and sustainability model (PRISM) framework through implementation science. Conceptualized through the PRISM framework, the multilevel nature and barriers to implementation of hepatitis C treatment become apparent. What follows is a list of barriers and implementation strategies that could be/could have been used to facilitate universal hepatitis C treatment.
Public awareness: educational campaigns (lay public and physicians).
Affordability: change payment structures (important at multiple levels, including drug and insurance companies, pharmacists, physicians, and patients).
Linkage to care and retention in care: local needs assessments and assessments of barriers and facilitators for patient populations/subgroups.
Patient screening: changing record systems (eg, automated testing based on risk factors such as age, drug use, etc.).
HOW CAN DISSEMINATION AND IMPLEMENTATION AND INFECTIOUS DISEASES HELP EACH OTHER?
D&I science has particularly been used in ID for HIV prevention and treatment, but has been less frequently used in other areas [44, 45]. In one study, investigators used D&I science to guide the implementation of universal decolonization treatment for ICU patients. Key stakeholders employed the Universal ICU Decolonization Toolkit, which provided in-depth implementation protocols and materials. Enterprise coaching calls informally assessed the uptake of the toolkit and substantiated the intervention implementation. The toolkit embodied several key implementation strategies, including training and educating stakeholders (ie, nurses), using evaluative strategies (ie, assessing readiness-and-monitoring process and outcome metrics), and employing interactive assistance (ie, the use of audio podcasts and physician-specific communication resources and evidence tools). In the intervention, patients were treated with chlorhexidine bathing and nasal mupirocin in 136 ICUs from 95 hospitals over 6 months, resulting in a 23.5% decrease in central line–associated bloodstream infections [44]. This massive undertaking with significant clinical benefits was made possible by D&I science. In another study, investigators found that a program to disseminate and implement findings of an acquired immunodeficiency syndrome clinical trial increased rates of early antiretroviral therapy initiation for HIV from 50 to 83% [45].
Examples of ID topical areas that could benefit from D&I science follow.
The uptake of treatment and management guidelines. Passive dissemination (current de facto practice) is known to be poorly effective in guideline uptake [16]. Dissemination should include active methods to spread information not just to practitioners and staff, but to organizations and politicians, so that institutional, organizational, and governmental policies incorporate research findings to best serve patients. Furthermore, evidence should be presented in a way that is understandable to the target audience [17].
Practice variability [46, 47]. Many factors contribute to practice variability, but deviations from best-care practices can result in patient harm. D&I science can help reduce practice variability when evidence demonstrates the superiority of one intervention or management strategy.
Problems with loss to follow-up [48], given their association with mortality [49] and the failure to treat sexually transmitted infections (among other important clinical outcomes) [50]. D&I science could help plan and organize the engagement of patients and communities.
Problems with linkage to care, given its association with untreated HIV and hepatitis C [51, 52]. D&I science could inform community engagement, as well as barriers and facilitators of linkage to care.
Train-the-trainer methods, which are applicable to many areas, including the Project Extension for Community Healthcare Outcomes approach for hepatitis C [53], hand hygiene, surgical site infection prevention, and antimicrobial stewardship, among others.
Conversely, because D&I is a relatively new field, there are many opportunities for problems in ID to help understand the cross-cutting issue of how evidence is disseminated and implemented in health. Some potential areas for collaborative problem solving are listed below.
End phases of implementation, sustainability, and de-implementation.
Disparities in evidence-based intervention dissemination and implementation.
Testing of D&I strategies.
CONCLUSIONS AND HOW CAN I LEARN MORE?
While we have provided a high-level review of D&I science and its potential applications in ID, there is much more literature available for interested readers. Table 3 includes a series of relevant resources, articles, and trainings. Alternatively, we would encourage individuals who do not wish to learn an entirely new field to partner with D&I researchers. The Clinical and Translational Science Awards programs, funded through the National Institutes of Health, are dedicated to the translation of research, and commonly have opportunities to collaborate with D&I researchers. The Patient-Centered Outcomes Research Institute also has toolkits and funding available for D&I research. Included in Table 3 are organizations that provide D&I consultation to clinical researchers on how to incorporate D&I into their current research programs.
Table 3.
Dissemination and Implementation Science Resources
| Resource Type/Title | Description | Link/Reference |
|---|---|---|
| Textbook: Dissemination and Implementation Research in Health: Translating Science to Practice |
Comprehensive introduction to D&I science | https://prcstl.wustl.edu/dissemination-and-implementation-research-in-health-translating-science-to-practice-2nd-edition/ |
| D&I model selection tool | Interactive website to select D&I models that best fit research questions or practice problems | http://www.dissemination-implementation.org/ |
| D&I toolkits | Various toolkits, information, and resources designed to support novice investigators interested in D&I | https://sites.wustl.edu/wudandi/di-toolkits/ |
|
Outcomes for implementation research: conceptual distinctions,
measurement challenges, and research agenda |
Delineates and describes implementation outcomes | Proctor et al [22] |
| Evaluating the public health impact of health promotion interventions: the Reach, Effectiveness, Adoption, Implementation, and Maintenance framework | Discusses implementation outcomes, includes RE-AIM framework | Glasgow et al [54] |
| Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact | Describes different types of hybrid trials | Curran et al [29] |
| Training courses through University of California San Francisco | Online Certificate in Implementation Science | https://epibiostat.ucsf.edu/online-certificate-implementation-science |
| NIH grant RFA | R01 for D&I science | https://grants.nih.gov/grants/guide/pa-files/par-16–238.html |
| AcademyHealth D&I science conference | National conference on D&I science (annual) | https://www.academyhealth.org/events |
| Society for Implementation Research Collaboration | Society for D&I research collaboration and communication between providers, researchers, and communities | https://societyforimplementationresearchcollaboration.org/ |
Abbreviations: D&I, dissemination and implementation; NIH, National Institutes of Health; RFA, request for application.
The goal of D&I research is to narrow the research-to-practice gap and, in the process, to reduce the time elapsed until populations gain maximum benefits from effective interventions. In addition, by getting evidence into practice, D&I science not only reduces health-care disparities, but also improves returns on investments of grant funding/taxpayer dollars. If the methods of D&I science were applied to all ID research, the result would be improvements in research output and quality, as well as patients’ clinical outcomes. For every patient, every trial, every study in ID, we should be asking ourselves, “where’s the D&I?”
Notes
Disclaimer. The contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
Financial support. This work was supported by the National Institutes of Health (NIH)-National Center for Advancing Translational Sciences (NCATS), components of the NIH, and the NIH Roadmap for Medical Research (grant number UL1 TR002345; sub-award number KL2 TR002346); The Foundation for Barnes-Jewish Hospital and their generous donors; the Washington University Institute of Clinical and Translational Sciences which is, in part, supported by the NIH/NCATS (Clinical and Translational Science Awards grant number UL1TR002345); the National Institute of Allergy and Infectious Diseases (grant number K24 AI134413); and the 2019 Summer Research Program of the Institute for Public Health, Public and Global Health track, at the Washington University in St. Louis, funded by the Global Health Center at the Institute for Public Health, Children Discovery Institute of Washington University, and St. Louis Children’s Hospital.
Potential conflicts of interest. G. A. C. is supported by The Siteman Cancer Center Biostatistics Shred Resource in NCI Cancer Center Support (grant number P30 CA091842). J. P. B. reports grants from NIH, grants from NIH/National Center for Advancing Translational Sciences during the conduct of the study. All other authors report no potential conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Green LW, Ottoson JM, García C, Hiatt RA. Diffusion theory and knowledge dissemination, utilization, and integration in public health. Annu Rev Public Health 2009; 30:151–74. [DOI] [PubMed] [Google Scholar]
- 2. Eccles MP, Mittman BS. Welcome to implementation science. Implementation Science 2006; 1–3. [Google Scholar]
- 3. van der Giesen FJ, van Lankveld W, Hopman-Rock M, et al. Exploring the public health impact of an intensive exercise program for patients with rheumatoid arthritis: a dissemination and implementation study. Arthritis Care Res (Hoboken) 2010; 62:865–72. [DOI] [PubMed] [Google Scholar]
- 4. Reid RD, Mullen KA, Slovinec D’Angelo ME, et al. Smoking cessation for hospitalized smokers: an evaluation of the “Ottawa Model.” Nicotine Tob Res 2010; 12:11–8. [DOI] [PubMed] [Google Scholar]
- 5. Gaglio B, Shoup JA, Glasgow RE. The RE-AIM framework: a systematic review of use over time. Am J Public Health 2013; 103:e38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Harden SM, Gaglio B, Shoup JA, et al. Fidelity to and comparative results across behavioral interventions evaluated through the RE-AIM framework: a systematic review. Syst Rev 2015; 4:155–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Health NIo PAR 16–238: dissemination and implementation research in health (R01) Available at: https://grants.nih.gov/grants/guide/pa-files/par-16–238.html. Accessed 6 June 2019.
- 8. National Institutes of Health Research Portfolio Online Reporting Tools. Available at: https://projectreporter.nih.gov/reporter.cfm. Accessed 6 June 2019.
- 9. Lomas J. Diffusion, dissemination, and implementation: who should do what? Annals of the New York Academy of Sciences 1993; 703:226–35; discussion 35–7. [DOI] [PubMed] [Google Scholar]
- 10. MacLean DR. Positioning dissemination in public health policy. Can J Public Health 1996; 87(Suppl 2):S40–3. [PubMed] [Google Scholar]
- 11. Rabin BA, Brownson RC. Terminology for dissemination and implementation research. In Brownson RC, Colditz GA, Proctor EK, eds. Dissemination and implementation research in health: translating science to practice. 2nd ed. New York: Oxford University Press, 2017:1–64. [Google Scholar]
- 12. Safdar N, Musuuza JS, Xie A, et al. Management of ventilator-associated pneumonia in intensive care units: a mixed methods study assessing barriers and facilitators to guideline adherence. BMC Infect Dis 2016; 16:349–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Durkin MJ, Keller M, Butler AM, et al. An assessment of inappropriate antibiotic use and guideline adherence for uncomplicated urinary tract infections. Open Forum Infect Dis 2018; 5:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Baugh CW, Wang TJ, Caterino JM, et al. Emergency department management of patients with febrile neutropenia: guideline concordant or overly aggressive? Acad Emerg Med 2017; 24:83–91. [DOI] [PubMed] [Google Scholar]
- 15. Livorsi D, Comer AR, Matthias MS, Perencevich EN, Bair MJ. Barriers to guideline-concordant antibiotic use among inpatient physicians: a case vignette qualitative study. J Hosp Med 2016; 11:174–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bero LA, Grilli R, Grimshaw JM, Harvey E, Oxman AD, Thomson MA. Closing the gap between research and practice: an overview of systematic reviews of interventions to promote the implementation of research findings. The Cochrane Effective Practice and Organization of Care Review Group. BMJ 1998; 317:465–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Brownson RC, Jacobs JA, Tabak RG, Hoehner CM, Stamatakis KA. Designing for dissemination among public health researchers: findings from a national survey in the United States. Am J Public Health 2013; 103:1693–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kelly JA, Heckman TG, Stevenson LY, et al. Transfer of research-based HIV prevention interventions to community service providers: fidelity and adaptation. AIDS Educ Prev 2000; 12:87–98. [PubMed] [Google Scholar]
- 19. Margaret Dolcini M, Gandelman AA, Vogan SA, et al. Translating HIV interventions into practice: community-based organizations’ experiences with the diffusion of effective behavioral interventions (DEBIs). Soc Sci Med (1982) 2010; 71:1839–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rowniak S, Ong-Flaherty C, Selix N, Kowell N. Attitudes, beliefs, and barriers to PrEP among trans men. AIDS Educ Prev 2017; 29:302–14. [DOI] [PubMed] [Google Scholar]
- 21. Remme JH, Adam T, Becerra-Posada F, et al. Defining research to improve health systems. PLOS Med 2010; 7:e1001000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health 2011; 38:65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tabak RG, Khoong EC, Chambers DA, Brownson RC. Bridging research and practice: models for dissemination and implementation research. Am J Prev Med 2012; 43:337–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Feldstein AC, Glasgow RE. A practical, robust implementation and sustainability model (PRISM) for integrating research findings into practice. Jt Comm J Qual Patient Saf 2008; 34:228–43. [DOI] [PubMed] [Google Scholar]
- 25. Mazzucca S, Tabak RG, Pilar M, et al. Variation in research designs used to test the effectiveness of dissemination and implementation strategies: a review. Front Public Health 2018; 6:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Palinkas LA, Aarons GA, Horwitz S, Chamberlain P, Hurlburt M, Landsverk J. Mixed method designs in implementation research. Adm Policy Ment Health 2011; 38:44–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pinnock H, Barwick M, Carpenter CR, et al. ; Standards for Reporting Implementation Studies (StaRI) Group. Standards for Reporting Implementation Studies (StaRI) statement. BMJ 2017; 356:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Pinnock H, Barwick M, Carpenter CR, et al. ; Standards for Reporting Implementation Studies (StaRI) Group. Standards for Reporting Implementation Studies (StaRI): explanation and elaboration document. BMJ Open 2017; 7:e013318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Curran GM, Bauer M, Mittman B, Pyne JM, Stetler C. Effectiveness-implementation hybrid designs: combining elements of clinical effectiveness and implementation research to enhance public health impact. Med Care 2012; 50:217–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Waltz TJ, Powell BJ, Matthieu MM, et al. Use of concept mapping to characterize relationships among implementation strategies and assess their feasibility and importance: results from the Expert Recommendations for Implementing Change (ERIC) study. Implement Sci 2015; 10:109–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hallsworth M, Chadborn T, Sallis A, et al. Provision of social norm feedback to high prescribers of antibiotics in general practice: a pragmatic national randomised controlled trial. Lancet 2016; 387:1743–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Munigala S, Rojek R, Wood H, et al. Effect of changing urine testing orderables and clinician order sets on inpatient urine culture testing: analysis from a large academic medical center. Infect Control Hosp Epidemiol 2019; 40:281–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Abualenain JT, Al-Alawi MM. Simulation-based training in Ebola personal protective equipment for healthcare workers: experience from King Abdulaziz University Hospital in Saudi Arabia. J Infect Public Health 2018; 11:796–800. [DOI] [PubMed] [Google Scholar]
- 34. Phrampus PE, O’Donnell JM, Farkas D, et al. Rapid development and deployment of Ebola readiness training across an academic health system: the critical role of simulation education, consulting, and systems integration. Simul Healthc 2016; 11:82–8. [DOI] [PubMed] [Google Scholar]
- 35. Parsons JT, Rendina HJ, Lassiter JM, Whitfield TH, Starks TJ, Grov C. Uptake of HIV pre-exposure prophylaxis (PrEP) in a national cohort of gay and bisexual men in the United States. J Acquir Immune Defic Syndr 2017; 74:285–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lambe KA, Lydon S, Madden C, et al. Hand hygiene compliance in the ICU: a systematic review. Crit Care Med 2019; 47:1251–7. [DOI] [PubMed] [Google Scholar]
- 37. Honda H, Ohmagari N, Tokuda Y, Mattar C, Warren DK. Antimicrobial stewardship in inpatient settings in the Asia pacific region: a systematic review and meta-analysis. Clin Infect Dis 2017; 64:119–26. [DOI] [PubMed] [Google Scholar]
- 38. Trautner BW, Grigoryan L, Petersen NJ, et al. Effectiveness of an antimicrobial stewardship approach for urinary catheter-associated asymptomatic bacteriuria. JAMA Intern Med 2015; 175:1120–7. [DOI] [PubMed] [Google Scholar]
- 39. O’Leary EN, van Santen KL, Webb AK, Pollock DA, Edwards JR, Srinivasan A. Uptake of antibiotic stewardship programs in US acute care hospitals: findings from the 2015 national healthcare safety network annual hospital survey. Clinical Infect Dis 2017; 65:1748–50. [DOI] [PubMed] [Google Scholar]
- 40. Hall MT, Simms KT, Lew JB, et al. The projected timeframe until cervical cancer elimination in Australia: a modelling study. Lancet Public Health 2019; 4:e19–27. [DOI] [PubMed] [Google Scholar]
- 41. Prevention Centers for Disease Control and Prevention. HPV vaccination coverage data Available at: https://www.cdc.gov/hpv/hcp/vacc-coverage/index.html. Accessed 6 September 2019.
- 42. Molina JM, Charreau I, Spire B, et al. ; France Recherche Nord & Sud Sida HIV et Hépatites Intervention Préventive de l’Exposition aux Risques avec et pour les Gays Study Group. Efficacy, safety, and effect on sexual behaviour of on-demand pre-exposure prophylaxis for HIV in men who have sex with men: an observational cohort study. Lancet HIV 2017; 4:e402–10. [DOI] [PubMed] [Google Scholar]
- 43. Yehia BR, Schranz AJ, Umscheid CA, Lo Re V 3rd. The treatment cascade for chronic hepatitis C virus infection in the United States: a systematic review and meta-analysis. PLOS One 2014; 9:e101554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Septimus E, Hickok J, Moody J, et al. Closing the translation gap: toolkit-based implementation of universal decolonization in adult intensive care units reduces central line-associated bloodstream infections in 95 community hospitals. Clin Infect Dis 2016; 63:172–7. [DOI] [PubMed] [Google Scholar]
- 45. Geng EH, Kahn JS, Chang OC, et al. The effect of AIDS Clinical Trials Group Protocol 5164 on the time from Pneumocystis jirovecii pneumonia diagnosis to antiretroviral initiation in routine clinical practice: a case study of diffusion, dissemination, and implementation. Clin Infect Dis 2011; 53:1008–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Chant C, Dos Santos CC, Saccucci P, Smith OM, Marshall JC, Friedrich JO. Discordance between perception and treatment practices associated with intensive care unit-acquired bacteriuria and funguria: a Canadian physician survey. Crit Care Med 2008; 36:1158–67. [DOI] [PubMed] [Google Scholar]
- 47. May L, Harter K, Yadav K, et al. Practice patterns and management strategies for purulent skin and soft-tissue infections in an urban academic ED. Am J Emerg Med 2012; 30:302–10. [DOI] [PubMed] [Google Scholar]
- 48. Hickey MD, Omollo D, Salmen CR, et al. Movement between facilities for HIV care among a mobile population in Kenya: transfer, loss to follow-up, and reengagement. AIDS Care 2016; 28:1386–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Mugavero MJ, Westfall AO, Cole SR, et al. ; Centers for Acquired Immunodeficiency Syndrome Research Network of Integrated Clinical Systems (CNICS) Beyond core indicators of retention in HIV care: missed clinic visits are independently associated with all-cause mortality. Clin Infect Dis 2014; 59:1471–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Lieberman A, Badolato GM, Tran J, Goyal MK. Frequency of prescription filling among adolescents prescribed treatment for sexually transmitted infections in the emergency department. JAMA Pediatr 2019; 173:695–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Ruria EC, Masaba R, Kose J, et al. Optimizing linkage to care and initiation and retention on treatment of adolescents with newly diagnosed HIV infection. AIDS 2017; 31(Suppl 3):253–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Assoumou SA, Tasillo A, Vellozzi C, et al. Cost-effectiveness and budgetary impact of HCV testing, treatment and linkage to care in US prisons. Clin Infect Dis 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Beste LA, Glorioso TJ, Ho PM, et al. Telemedicine specialty support promotes hepatitis C treatment by primary care providers in the department of veterans affairs. Am J Med 2017; 130:432–8.e3. [DOI] [PubMed] [Google Scholar]
- 54. Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health 1999; 89:1322–7. [DOI] [PMC free article] [PubMed] [Google Scholar]