Highlights
-
•
34/37 studies showed at least one measure of SEM associated with overdose.
-
•
Evidence for associations of health insurance, income, education, incarceration, social support, and SES with overdose.
-
•
Marginalization is associated with added precarity and risk for people who use opioids.
-
•
Initiatives aiming to decrease SEM are a necessary part of combatting overdose.
Keywords: Poverty, Drug-related death, Toxicity, Poisoning, Socioeconomic status
Abstract
Background
Socioeconomic marginalization (SEM) is an important but under-explored determinant of opioid overdose with important implications for health equity and associated public policy initiatives. This systematic review synthesizes evidence on the role of SEM in both fatal and non-fatal overdose among people who use opioids.
Methods
Studies published between January 1, 2000 and March 31, 2018 were identified through searching electronic databases, citations, and by contacting experts. The titles, abstracts, citation information, and descriptor terms of citations were screened by two team members. Data were synthesized using the lumping technique.
Results
A total of 37 studies met inclusion criteria and were included in the review, with 34 of 37 finding a significant association between at least one socioeconomic factor and overdose. The included studies contained variables related to eight socioeconomic factors: criminal justice system involvement, income, employment, social support, health insurance, housing/homelessness, education, and composite measures of socio-economic status. Most studies found associations in the hypothesized direction, whereby increased SEM was associated with a higher rate or increased likelihood of the overdose outcome measured. The review revealed an underdeveloped evidence base.
Conclusions
Nearly all reviewed studies found a connection between a socioeconomic variable and overdose, but more research is needed with an explicit focus on SEM, using robust and nuanced measures that capture multiple dimensions of disadvantage, and collect data over time to better inform decision making around opioid overdose.
1. Introduction
The current opioid overdose crisis is characterized by surging and unprecedented rates of overdose and has been linked to contamination of fentanyl and carfentanil in the drug supply (Elliott and Lopez, 2018; Coroners Service of BC, 2019; World Health Organization, 2017). Socioeconomic marginalization (SEM) and the vulnerability it creates is an important but under-explored contributor to overdose for people who use opioids. While general knowledge of the social determinants of health is widely established, connecting upstream elements of marginalization to acute health crisis events like opioid overdose has not been done systematically: an omission we aim to contribute to resolving in this paper. Without this understanding, developing specific responses to the opioid and overdose crises through evidence-based interventions on the elements of marginalization that are most tightly linked to overdose is not possible. This paper presents the results of a review designed to systematically summarize evidence on SEM and opioid-related overdose.
We define SEM as a set of conditions that contribute to exclusion from social and economic opportunities and create vulnerability including: labour market exclusion; informal or prohibited income generation (e.g. theft, drug dealing, street-based work); material insecurity (e.g. housing or food insecurity); inadequate income; incarceration; social stigma or isolation; and low socioeconomic status or poverty. Conditions that may contribute to SEM have been linked to overdose, with specific subpopulations of people who use drugs at elevated risk of drug-related death, including people who are homeless (Fischer et al., 2004), have been recently released from prison (Green et al., 2012; Stewart et al., 2004), are eligible for US Medicaid (a proxy indicator of poverty) (Coolen et al., 2009), are of Indigenous ancestry (Jongbloed et al., 2014; Milloy et al., 2010), grew up in a low-income household (Galea et al., 2006; Lanier et al., 2012; Silva et al., 2012), or did not complete high school (Galea et al., 2006; Ho, 2017; Lanier et al., 2012; Silva et al., 2012). However, these factors insufficiently represent the scope of socioeconomic drivers that affect the health and overdose risk for people who use opioids such as labour market exclusion (Richardson et al., 2014 ;2015), involvement in illegal and informal income generation (Ti et al., 2014), synchronized administration of income assistance payments (Krebs et al., 2016; Otterstatter et al., 2016; Zlotorzynska et al., 2014), and material insecurity (Ompad et al., 2011) – all of which have received inadequate attention in overdose research (Brunner and Marmot, 2006). These factors are hypothesized to affect health outcomes not only through direct material deprivation, but also through psychosocial and behavioural pathways (Brunner and Marmot, 2006). The chronic stress that comes from social exclusion, diminution, and inequality promote stress responses that can lead to increased interpersonal conflict and ill health, cyclically reinforcing the distributions of power that create them (Brunner and Marmot, 2006). Social and economic components of marginalization, including access to the resources and conditions that affect drug-related harm such as neighborhood deprivation and income inequality are associated with overdose and drug-related death not just at the individual level, but also structurally through the control and distribution of socio-economic resources (Krebs et al., 2016; Lanier et al., 2012; Otterstatter et al., 2016; Rintoul et al., 2010; Xiang et al., 2012; Zlotorzynska et al., 2014). The confluence of factors involved in these relationships make it difficult to isolate root causes. However, the patterns visible between these conditions and their effect on overdose exemplify the multiple types of disadvantage— spatial and cumulative life course disadvantage, for example — that together affect health inequities for people who use opioids.
A better understanding of these relationships is important for developing responses to the opioid and overdose crises that intervene on upstream determinants of health, yet there are no systematic reviews that summarize specific risks linking social and economic factors to the production or magnification of overdose risk for people who use opioids. This is a critical gap, limiting our knowledge of the socioeconomic drivers of opioid-related overdose and which dimensions would be most effectively and efficiently targeted with response strategies. We conducted this systematic review of the literature to help address these omissions, with the aim of summarizing the scientific evidence about the associations between socioeconomic factors and opioid overdose.
2. Methods
2.1. Search strategy and selection criteria
In accordance with the Systematic Reviews and Meta-Analyses (PRISMA) guidelines, we searched for studies that included measures of socioeconomic factors and opioid-related fatal and non-fatal overdose that were published in English peer-reviewed journals or by governmental sources between January 1, 2000 – March 31, 2018. The search strategy is summarized in Table 1 and a summary of the Medline search terms is outlined in Appendix A. The protocol was registered in the PROSPERO database (registration# CRD42018096392) prior to beginning the review (van Draanen et al., 2018).
Table 1.
Systematic Review Search Strategy and PICOS Criteria.
| Search Concepts* | SEM: Social class, socioeconomic status; low education; unemployment, labour market exclusion; material insecurity, material hardship; housing insecurity, homelessness, unstable housing; hunger, food insecurity; health care access, social service access; poverty and income inadequacy; social assistance, income assistance, welfare, disability; prohibited income generation (e.g. theft, drug dealing, street-based work); early childhood development; incarceration, criminal justice system involvement; persistent disadvantage, vulnerability, stigma, social isolation, social exclusion, marginalization; service barriers and availability, location of social services, health care service availability and accessibility; housing availability, housing affordability; urbanization, neighborhood disorder; disparities, income inequality, wealth inequality, neighborhood median income; synchronized social assistance, (“cheque day effect” or “check effect”); welfare, disability, and income assistance policies; criminal justice and drug policies. Overdose (fatal and non-fatal): poisoning, drug-related poisoning, side-effects/adverse reactions, toxicity, death, morbidity, mortality, overdose Opioids: People who use opioids (medical/non-medical), prescription and non-prescription, oral and injection |
| Databases | MEDLINE (Ovid), Embase (Ovid), PsycINFO (EBSCOhost), CINAHL (EBSCOhost), Google Scholar, Cochrane Central Registry of Controlled Trials (CENTRAL), and Cochrane Drug and Alcohol Group (CDAG) Specialized Registry |
| Other Search Strategies | In addition to searching electronic databases, additional searches on clinicaltrials.gov, a comprehensive grey literature search (e.g., www.opengrey.eu, https://deslibris.ca), conference proceedings (e.g., Harm Reduction International, American Public Health Association, etc.), and manual searches of the references of included studies other reviews in this area, and studies that have cited the included studies were performed. The search strategy also included contacting experts and community stakeholders to identify unpublished, ongoing and other studies not otherwise retrieved through searches for this review. |
| PICOS Criteria | Population: People who use opioids in North America, Europe, the United Kingdom, Australia, and New Zealand. Articles were only included if they had opioids identified as a cause of overdose. Poly drug-related overdose papers were included if they included opioid overdose in the cases. Intervention: Any measure of socioeconomic marginalization as an independent variable in the article (i.e. labour market exclusion; informal or prohibited income generation; material insecurity; inadequate income; incarceration; social stigma or isolation; and low socioeconomic status or poverty). Articles were included if they had any measure of socioeconomic marginalization as an independent variable in the article. Articles that include socio-demographic variables as controls in their multivariable regression models, for example, were included as long as there were empirical results that showed the effects of the SEM variables on opioid overdose. Comparison: Quantitative studies with comparisons between groups with different levels of social and economic marginalization Outcomes: Opioid-related fatal and non-fatal overdose. Articles were included only if they had overdose as a unique/isolated outcome. Articles examining drug-related harm or mortality might include overdose but also include death or harm from other factors (e.g., motor vehicle accidents) and as such were excluded. Study design: Any study design including quantitative data. Articles that contained empirical data were included. Case-reports, letters, commentaries, reviews, and editorials were excluded. |
Notes: *Terms related to these key concepts were entered into all computer databases, combined using appropriate Boolean operators. All terms were searched both as subject headings as well as key words. See Appendix A for a summary of the Medline search terms included.
We used the PICOS framework (Population, Intervention, Comparison, Outcome, Study Design) to frame our research question (Schardt et al., 2007) and searched for studies among people who use opioids (P) that contained any measure of socioeconomic marginalization (I) with comparisons (C) between groups with different levels of social and economic marginalization and opioid-related fatal and non-fatal overdose (O) using quantitative data (S). Two research assistants used a standardized form to independently extract data from the studies, and any inconsistencies in the extracted data were noted by the research assistants and resolved through final deliberation by a senior team member.
2.2. Data analysis
Given that this review asked a broad question and purposely allowed inclusion of different study types, we used the 'lumping' technique where all studies in a topic area were included despite design differences (Hutton et al., 2015; Grimshaw et al., 2003). Similar to the approach taken by others investigating determinants of overdose (King et al., 2014), this strategy was employed to identify common generalizable features in the relationships between SEM and opioid overdose that remain despite minor differences in study subjects, context, and design. The choice to take a broad approach, combining heterogenous outcome measures was made to allow for the generalisability and consistency of research findings to be assessed across a wider range of different outcomes: reducing the risk of bias or chance results.
Due to significant variations in methodologies and outcomes of studies included in this systematic review, findings are summarized according to elements of SEM. The conceptual and methodological heterogeneity across the studies precluded the undertaking of a meta-analysis. The data extraction sheet included an additional assessment of bias and study quality, for which we used the tested and validated study quality assessment tools of the National Heart, Lung, and Blood Institute (National Institutes of Health, 2018).
3. Results
3.1. Study selection and study characteristics
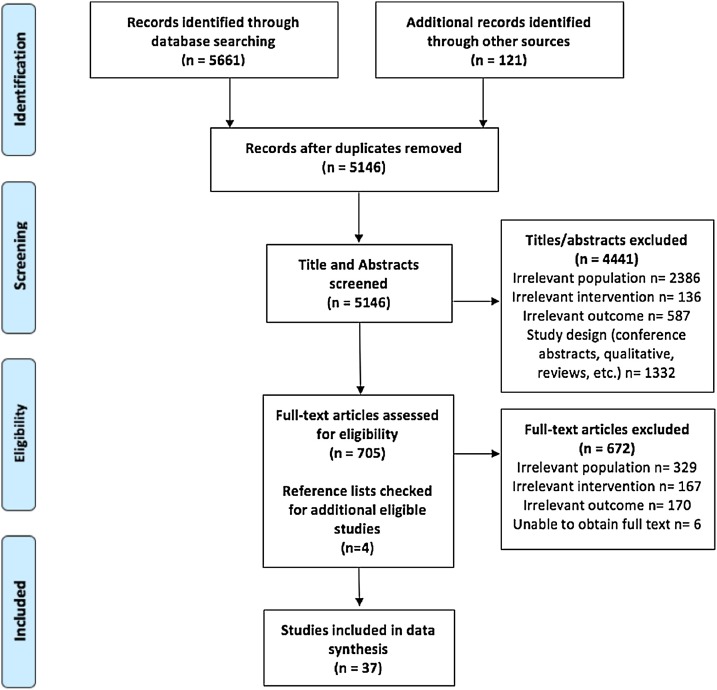
The process to select studies is detailed in the PRISMA flow diagram in Fig. 1 . A total of 5782 articles met the initial screening criteria. The review and screening process led to a final dataset of 37 articles. Substantial heterogeneity was seen between both the types of overdose outcome reported and the method of operationalization for each dimension of SEM in included studies. Half of the included studies (n = 19) focused on fatal overdose as a key outcome or drew their sample from a population who had had a fatal overdose (see Table 4 for details on overdose outcome, intent, type of opioid, and measure of SEM included). One third included non-fatal overdose (n = 13) and five articles included both fatal and non-fatal overdose in their analyses. In terms of intent, 11 articles examined only unintentional overdose, nine examined both intentional and unintentional overdose and 17 did not report intention. Half the studies included overdose that was attributable to both prescription and non-prescription opioids in their sample (n = 19) while nine investigated prescription opioid overdose and four investigated only non-prescription opioid overdoses. Five studies did not report what type of opioids were included in their data. Nineteen studies used cross-sectional data, eight studies used cohort data, six studies used longitudinal data, two studies used case-control designs, one study used an interrupted time series, and one study used ecological data (see Table 3 for details on study design for each included study).
Fig. 1.
PRISMA Flow Diagram.
Table 4.
Summary of Measures and Findings for Included Studies.
| Author (Year) | Measure of SEM | Opioids involved | Overdose characteristic (intent; type) |
Measure of overdose | Main findings | Risk of bias |
|---|---|---|---|---|---|---|
| Amundsen (2015) | SES composite | Prescription & non-prescription | Intentional & unintentional; fatal | ICD-10 codes for opioid poisoning deaths | Socioeconomic Status: Three clusters were created from a two-step cluster analysis: Very low SES: persons of a younger age (15–44), lowest level of education, not participating in the workforce, some participation in shorter work-related training/support and a high level of means-tested social benefits; Disabled: persons of an older age (35–64), on a disability pension, low level of education, income higher than the minimum pension (due to the disability pension), not participating in the workforce, some in need of means-tested social welfare benefits, largest proportion of women; Edge of the workforce (higher SES): mainly aged 24–54 years, highest level of education, more years with income above the minimum pension, highest proportion with workforce participation and work-related training/support, less use of means-tested social welfare benefits. Heroin overdose death (very low SES vs. disabled vs. edge of workforce): 55.5% vs. 33.6% vs. 47.1%, p < 0.05 in cause of death cluster Heroin overdoses were most common in the very low SES cluster; other opioid overdoses were more common among those on disability and on the edge of the workforce. |
Poor |
| Binswanger et al. (2007) | Criminal justice involvement | Prescription & non-prescription | NR; fatal | ICD-10 codes for opioid poisoning deaths | Recent release from prison: Heroin-related deaths n; n/100,000 person-years (95 %CI) Overall: 18; 32 (20–50) Within 2 weeks after release: 6; 409 (184–91) More than 2 weeks after release: 12; 23 (14–40) Methadone-related deaths n; n/100,000 person-years (95 %CI) Overall: 18; 32 (20–50) Within 2 weeks after release: 5; 341 (142–818) More than 2 weeks after release: 13; 23 (14–40) Other opioid-related deaths n; n/100,000 person-years (95 %CI) Overall: 13; 23 (13−40) Within 2 weeks after release: 5; 341 (142–818) More than 2 weeks after release: 8; 14 (7−29) |
Fair |
| Bohnert et al. (2011) | Employment, SES composite, Criminal justice involvement | NR | Unintentional; fatal | Opioid overdose deaths identified through Office of the Medical Examiner (OME) | Unemployment rate: No significant associations were found between unemployment rate and overdose |
Fair |
| SES composite: Including percent of persons per precinct who had less than a high school education, earned less money annually than 200 % of the federal poverty level, and received public assistance, as well as the percent of households per precinct with a self-reported female head of household. The composite was scored in the direction of disadvantage, with more socioeconomically disadvantaged precincts scoring higher (range 23.4–189.0). Posterior median for opiate overdose: 0.35; 95 % credible interval: 0.05−0.64 | ||||||
| Misdemeanor arrest rate (per 1000): Posterior median for opiate overdose: 0.003; 95 % credible interval: 0.001−0.01 | ||||||
| Brinkley-Rubinstein et al. (2018) | Criminal justice involvement | Non-prescription | NR; fatal | Opioid overdose deaths identified through OME | Incarceration in year preceding death: Fentanyl-related overdose in those incarcerated the year preceding death (2015 vs. 2014): RR: 1.99, 95% CI: 1.11−3.57, p = 0.014 No significant differences in overdose rates were found by race/ethnicity, age, or gender over time. |
Poor |
| Burns et al. (2004) | Employment, Social support, | Non-prescription | NR; non-fatal | Self-reported lifetime history of overdose | Relationship dissatisfaction: MV logistic regression model found that dissatisfaction with relationships predicted overdose history (Wald-statistic 4.05, p < 0.05) No significant associations were found between employment status, social support, living alone/in temporary accommodation and overdose. |
Poor |
| Brown and Wehby, 2019 | Homelessness & Housing, Income and poverty, Employment, Health insurance |
Prescription & non-prescription | Unintentional & undetermined; fatal | ICD-10 codes for opioid poisoning deaths | Median house price: Effect of median house price on opioid death rate: −0.0121, p < 0.05 The effect median house price on opioid and prescription opioid death rate estimates were only statistically significant among males (-0.0168, p < 0.05 and -0.0199, p < 0.01, respectively) but not among females. The effect median house price on opioid and prescription opioid death rate estimates were only statistically significant among non-Hispanic Whites (-0.0172, p < 0.05 and -0.0187, p < 0.01, respectively) but not among Black or Hispanic racial/ethnic groups. |
Fair |
| Median household income: Effect of median house price on prescription opioid rate: -0.0136, p < 0.01 | ||||||
| No significant associations were found between median household income, unemployment rate, proportion of the population with health insurance and opioid and prescription opioid overdose death. | ||||||
| Campbell et al. (2018) | SES composite | Prescription | NR; fatal & non-fatal | ICD-9 codes for non-fatal opioid poisonings & State death certificates | Neighborhood Deprivation Index: Neighborhood deprivation index was created based on home address and census tract variables (e.g. households in poverty) from the U.S. Census Bureau's 2006–2010 American Community Survey. No further information on how the index was created is provided. No significant associations were found between neighborhood deprivation indices and overdose. |
Fair |
| Carrà et al. (2017) | Criminal justice involvement, SES composite, Education, Employment, Social support | NR | NR; non-fatal | Self-reported lifetime history of non-fatal opioid overdose | Jail sentences over 6 months: AOR: 0.70, 95 % CI: 0.53−0.92 |
Poor |
| Area-level deprivation: Using residential postal codes, area-level deprivation score was calculated based on the Italian deprivation index at census block level. Five indicators (low level of education, unemployment, nonhome ownership, one parent family and overcrowding) were standardized and summed to create categorical tertiles: affluent, intermediate and deprived. Deprived vs. affluent: AOR: 2.61, 95% CI: 2.25−3.02 Intermediate vs. affluent: AOR: 1.09, 95% CI: 1.02−1.16 | ||||||
| No significant associations were found between compulsory education, unemployment, family situation and overdose death. | ||||||
| Cerdá et al. (2013) | Income and poverty, Homelessness & housing, Social support |
Prescription & non-prescription | Unintentional; fatal | Post-mortem toxicology and autopsy reports for analgesic opioids and heroin deaths | Higher median income (analgesic vs. heroin overdose death): OR: 1.40; 95% CI: 1.20−1.65 No significant associations were found between median house income and odds of analgesic vs. non-overdose death. Higher income inequality (analgesic vs. heroin overdose death): OR: 0.74; 95% CI: 0.61−0.91 No significant associations were found between income inequality and odds of analgesic vs. non-overdose death. |
Fair |
| Dilapidated Housing Structures: No significant associations were found between dilapidated housing structures, and the odds of analgesic overdose vs. non-overdose deaths, and analgesic overdose vs, heroin overdose deaths. | ||||||
| Family fragmentation (analgesic vs. non-overdose death): OR: 1.35, 95% CI: 1.05−1.72 No significant associations were found between family fragmentation and odds of analgesic vs. heroin overdose deaths. | ||||||
| Cheng et al. (2013) | Social support, Education, Employment |
Prescription & non-prescription | Unintentional; fatal | Post-mortem toxicology and autopsy reports for deaths with at least one opioid | Marital Status: Married (opioid overdose decedents vs. state-level population): 33.9% vs. 68.2%, p < 0.001 |
Fair |
| Educational Attainment: Less than high school education (opioid overdose decedents vs. state-level population): 18.5% vs. 6.9%, p < 0.001. Graduate education (opioid overdose decedents vs. state-level population): 8.7% vs. 29.9%, p < 0.001 | ||||||
| Unemployment (opioid overdose decedents vs. state-level population): 64% vs. 5%, p < 0.001 | ||||||
| Cochran et al. (2017) | Health insurance | Prescription | NR; fatal & non-fatal | ICD-9 codes for opioid poisoning deaths and hospitalization and ED visits | Medicaid eligibility type: General Assistance vs. Temporary Assistance for Needy Families: ARR: 1.58, 95% CI: 1.28−1.94, p < 0.001 Supplemental Security Income vs. Temporary Assistance for Needy Families: ARR: 1.26, 95% CI: 1.08−1.48, p = 0.004 |
Good |
| Coolen et al. (2009) | Health insurance | Prescription | Unintentional; fatal | ICD-10 codes for opioid poisoning deaths | Medicaid enrollment: Rate of deaths attributed to Prescription Opioid OD by Medicaid Status comparing the Medicaid population to anyone not enrolled in Medicaid in Washington; Age adjusted rate and relative risk (95 % CI): Medicaid vs. Non-Medicaid- 30.8; 5.7 (5.3−6.1) Medicaid PRC vs. Non-Medicaid - 381.4; 92.6 (64.1−129.5) |
Fair |
| Cropsey et al. (2013) | Education, Demographics, Employment, Homelessness & housing, Social support, Criminal justice involvement |
NR | NR; non-fatal | Self-reported lifetime history of non-fatal opioid overdose | Educational Attainment: High school completion in individuals recently released from prison (opioid overdose vs. no opioid overdose vs. no opioid use): 85% vs. 77% vs. 66%, p < 0.001 |
Poor |
| Ethnicity: Caucasian ethnicity in individuals recently released from prison (opioid overdose vs. no opioid overdose vs. no opioid use): 82% vs. 58% vs. 25%, p < 0.001 Sex: Female sex in individuals recently released from prison (opioid overdose vs. no opioid overdose vs. no opioid use): 47%, vs. 32% vs. 27% p < 0.001 | ||||||
| No significant associations found between employment status, housing situation, marital status or living situation and overdose in in individuals recently released from prison. | ||||||
| Dunn et al. (2016) | Employment, Criminal justice involvement, Health insurance, Social support |
Prescription & non-prescription | NR; non-fatal | Self-reported lifetime history of non-fatal opioid overdose | No significant associations were found between employment status, incarceration in the past 30 days, health insurance status, marital status and opioid overdose. | Poor |
| Feng et al. (2016) | Income & poverty | Prescription & non-prescription | Intentional & unintentional; fatal & non-fatal | ICD-9 codes for opioid poisoning deaths and hospitalization and ED visits | Median household income: Quartile 1 (lowest) vs. 4 (highest): AOR: 1.80, 95% CI: 1.27−2.57 Quartile 2 vs. 4: AOR: 1.89, 95% CI: 1.34−2.66 Quartile 3 vs. 4: AOR: 1.24, 95% CI: 1.00−1.54 |
Fair |
| Fernandes et al. (2015) | Health insurance | Prescription | Unintentional; fatal | ICD-10 codes for opioid poisoning deaths | Medicaid enrollment: Opioid overdose fatality rates, comparing the Medicaid population to anyone not enrolled in Medicaid in Montana; Overdose rates (Medicaid vs. non-Medicaid): 38.2/100,000 (30.7−45.7) vs. 4.7/100,000 (4.1−5.3) |
Fair |
| Hasegawa et al. (2014) | Health insurance, Income & poverty | Prescription & non-prescription | Intentional & unintentional; non-fatal | Opioid -related near-fatal events involving mechanical ventilation Opioid-related hospitalization |
Insurance status: Medicare vs. Private: AOR:1.08, 95 % CI: 0.95−1.24 Medicaid vs. Private: AOR:1.17, 95 % CI: 1.04−1.32 Self-pay vs. Private: AOR: 0.83, 95% CI: 0.75−0.93 Other vs. Private: AOR:1.68, 95% CI: 1.44−1.95 |
Poor |
| No significant associations between income quartiles of residence and frequency of ED visits or hospitalizations for non-fatal overdose | ||||||
| Hollingsworth et al. (2017) | Employment | Prescription & non-prescription | Intentional & unintentional; fatal & non-fatal | ICD-10 codes for opioid poisoning deaths Opioid-related ED visits |
County-level Employment: Effect of unemployment rate on opioid death rate: 0.19, p < 0.01 Effect of unemployment rate on opioid overdose ED visit rate: 0.95, p < 0.01 State-level Employment: Effect of unemployment on opioid death rate: 0.33, p < 0.01 Effect of unemployment on opioid overdose ED visit rate: 0.35, p < 0.01 |
Good |
| Jenkins et al. (2011) | Criminal justice involvement, Homelessness & housing |
Prescription & non-prescription | NR; non-fatal | Self-reported heroin overdose in the past year | Incarceration: Incarceration of 5+ days: AOR: 1.88, 95% CI: (1.04–3.40) |
Poor |
| No permanent housing was not associated with non-fatal overdose. | ||||||
| Marshall et al. (2017) | Income & poverty, Education |
Prescription & non-prescription | Intentional & unintentional; fatal | Opioid overdose deaths identified through coroners | Median household income: Adjusted Mortality Ratio (AMR; 95 % CI) for PO deaths $59,410–83,900 vs. < $59,410: 0.65 (0.52–0.81) $83,910–97,460 vs. < $59,410: 0.58 (0.42–0.80) $97,470 vs. < $59,410: 0.50 (0.33–0.74) AMR (95 % CI) for heroin deaths: $97,470 vs. < $59,410: 0.33 (0.15–0.70) % Below Poverty level: AMR (95 % CI) for PO deaths 6.35–9.99 % vs. < 6.35 %: 1.45 (1.10–1.89)16.86 % vs. < 6.35 %: 2.90 (1.02–4.68) AMR (95 % CI) for heroin deaths 16.86 % vs. < 6.35 %: 2.18 (1.02–4.68) |
Fair |
| % Higher education: AMR (95 % CI) for PO deaths (95 % CI) 41.6–56.7 % vs. < 28.0 %: 0.59 (0.39–0.89)56.8 % vs. < 28.0 %: 0.45 (0.28–0.72) No significant association was found between higher education and mortality ratio for heroin deaths | ||||||
| McAuley and Best (2012) | Criminal justice involvement | Prescription & non-prescription | Unintentional; fatal | Post-mortem reports for deaths with at controlled drugs | Incarceration with heroin-related death: Prison release within 14 days of death [AOR (95% CI): 2.499 (1.046−5.969)] Prison release within 15−28 days of death [AOR (95% CI): 2.499 (1.046−5.969)] Incarceration with Methadone-related death: No significant association with prison release within 14 or 15−28 days of death |
Fair |
| Meiman et al. (2015) | Health insurance, Income & poverty |
Prescription & non-prescription | Intentional & unintentional; fatal & non-fatal | ICD-9 codes for opioid poisoning deaths and hospitalization and ED visits | Insurance Status and Poverty: In the relationship between those who use heroin versus those who use prescription opioids, there is a significant relationship in participants aged 18−34 when participants are separated into groups based on insurance status and poverty (p < 0.01) and in participants aged 35 and older when participants are separated into groups based on insurance status and poverty (p < 0.01) |
Fair |
| Nadpara et al. (2018) | Social support | Prescription | NR; non-fatal | Post-overdose reports for overdose with prescription opioids | Marital Status: Never Married vs. Married: AOR: 1.35 (1.01–1.82) Widowed vs. Married: AOR: 2.04 (1.40–2.97) |
Fair |
| Ochoa et al. (2005) | Criminal justice involvement, Income& poverty, Homelessness & housing |
Non-prescription | NR; non-fatal | Self-reported on a scale of 1−10 | Incarceration and Recent overdose: Incarcerated ≥20 months vs. Never incarcerated: AOR (95% CI): 2.99 (1.52–5.88) |
Poor |
| Sex Work: Ever been paid money for sex vs. No: OR (95% CI); 1.53 (1.05−2.23) | ||||||
| Homelessness: No association between homelessness and recent overdose | ||||||
| Ødegård et al. (2010) | Criminal Justice Involvement | NR | NR; fatal | ICD-8,910 codes for opioid poisoning deaths | Incarceration: Death from overdose during the 2 weeks after release from prison was 10 times higher (ARR: 10.2; 95% CI: 4.4–23.9), and in the 3-week period more than six times higher (ARR: 6.5, 95% CI; 2.7–15.7), than the risk during other time spent outside prison. In prison, however, the risk of overdose was less than 1/10th of the risk outside (ARR: 0.08, 95% CI 0.01–0.57) |
Fair |
| Patrick et al. (2016) | Employment, Education |
Prescription | Intentional & unintentional; fatal | ICD-10 codes for opioid poisoning deaths | Unemployment Rate: Unemployment rate was not associated with a decrease of opioid-related overdose deaths rates |
Fair |
| Educational Attainment: Educational attainment was associated with a decrease of 0.08 opioid-related overdose deaths per 100,000 population annually (-0.08: 95% CI: -0.40, -0.24) | ||||||
| Paulozzi et al. (2009) | Social support, Education, Income & Poverty |
Prescription | Unintentional; fatal | ICD-10 codes for opioid poisoning deaths | Marital Status and College Education: The methadone group had fewer people who were married (p = 0.024), and fewer people who had attended college (p = 0.048) No association between type of overdose decedents and poverty rate by county. |
Fair |
| Ponicki et al. (2018) | Income & Poverty, Demographics |
Prescription | NR; non-fatal | ICD-9 codes for opioid-related poisoning | Median Household Income: No association between median HH income/% of families in poverty with zip code rates of prescription opioid poising hospitalizations |
Good |
| Indigenous ancestry: Association of % American Indians with zip code rates of prescription opioid poising hospitalizations Relative Rate (95% CI): 1.015 (1.008, 1.023) Association of zip code within an American Indian reservation with zip code rates of prescription opioid poising hospitalizations; Relative Rate (95% CI): 0.473 (0.294, 0.753) | ||||||
| Rintoul et al. (2010) | SES composite, Employment |
Prescription | Intentional & unintentional; fatal | Post-mortem toxicology and autopsy reports for opioid-related deaths | Socioeconomic Status: Socioeconomic status using residential address and the Victorian Index of Relative Socioeconomic Disadvantage. Lower scores/quintiles indicate an area has many people with low levels of education, employed in low-skill jobs, and many households with low income. Unintentional drug toxicity deaths: Quartile 1 vs. Quartile 4: Rate ratio (95% CI): 3.0 (1.4–6.1) |
Fair |
| Employment status: No association between unemployed and on other government benefits versus all other employment status types with fatal drug toxicity cases involving oxycodone (2003−2009) | ||||||
| Seal et al. (2001) | Homelessness & housing, Criminal Justice Involvement, Income & poverty, SES Composite |
NP | NR; non-fatal | Self-reported history of overdose | Currently Homeless: Homeless at the time of the interview vs. not homeless: OR (95% CI): 2.59 (1.87, 3.59) Criminal Justice Measures: Arrested 3 or more times in the past year: AOR (95% CI); 2.50 (1.61, 3.87) No association between total length of time incarcerated and prevalence of recent OD Prohibited Income Received money or drugs in exchange for sex within the last 6 months: OR (95% CI); 2.08 (1.38, 3.14) Social Marginalization Score Respondents were assigned 1 point for each of the following variables they reported: being currently homeless; spending 5 or more years in jail, identifying as lesbian, gay, bisexual, or transgender, and engaging in sex work for money or drugs in the past 6 months. For each additional characteristic that a participant reported, the likelihood of associated overdose increased in a stepwise fashion. One point: OR (95% CI); 2.33 (1.46, 3.72) Two points: OR (95% Cl); 3.73 (2.27, 6.14) Three points or more: OR (95% Cl); 6.76 (3.45, 13.2) |
Poor |
| Shah et al. (2005) | Social Support | Prescription & non-prescription | Unintentional; fatal | Post-mortem toxicology and autopsy reports for opioid-related deaths | Marital Status: Decedents who died from methadone co-intoxication with prescription drugs were significantly more likely to be living with a partner or married (44.1% versus 29.0% for methadone alone and 25.0% for methadone and illicit drugs) p < 0.05 |
Fair |
| Sharp and Melnik (2015) | Health insurance | Prescription & non-prescription | NR; fatal | ICD-10 codes for opioid poisoning deaths | Medicaid Status: Rate ratios comparing death rates between 2003 and 2012: Medicaid: 5.3; Non-Medicaid: 3.9 Deaths per 100,000 among all New York state residents not enrolled in Medicaid increased from 0.73 in 2003 to 2.82 in 2012, while among Medicaid enrollees, the rates increased from 1.57 to 8.31 over the same period. New York state Medicaid enrollees had higher death rates for opioid analgesic poisonings than did those not enrolled in Medicaid, and the differences increased over time. |
Fair |
| Sherman et al. (2007) | Homelessness & housing, Education, Criminal justice involvement, Employment |
NR | NR; non-fatal | Self-reported history of overdose | Homelessness: Homeless in the past 6 months vs. not homeless in overdose: AOR (95% CI): 2.9 (1.5, 5.7) |
Poor |
| No significant association between education/recent incarceration/employment and overdose | ||||||
| Siegler et al. (2014) | Education, Income & poverty |
Prescription & non-prescription | Unintentional; fatal | ICD-10 codes for opioid poisoning deaths | Education: Unintentional opioid overdose deaths with Education: College or more vs. less than high school: AOR (95% CI): 2.13 (1.44, 3.16) |
Good |
| No significant association between neighborhood poverty and unintentional opioid overdose | ||||||
| Visconti et al. (2015) | Income & poverty | Prescription & non-prescription | Unintentional; fatal | Post-mortem toxicology and autopsy reports for opioid-related deaths | Poverty: Decedents above poverty line (%)/decedents below poverty line (%) by race: Decedents below the poverty line were more likely to be African-American (23.2 % compared to 11.9%, p = 0.03) Decedent age and sex distributions were similar across areas above and below the poverty line |
Fair |
| Wagner et al. (2015) | Homelessness & housing Criminal justice involvement |
Prescription & non-prescription | NR; non-fatal | Self-reported history of overdose | Homelessness: Homeless in the past 6 months: ≥1 overdose in the past six months: 35 (77.8 %) No overdoses in the past six months: 315 (59.7 %) p = 0.02 |
Poor |
| Criminal justice measures: Arrested for drug possession in the past 6 months: AOR (95% CI); 5.17 (2.37, 11.24) ≥1 OD in the past six months vs. No OD in past 5 months Arrested: 19 (43.2 %) vs. 135 (25.7 %); p = 0.02 Arrested for drug possession 12 (27.3 %) vs. 38 (7.3 %) p < 0.001 Police presence caused hurried or rushed injection 18 (40.9 %) vs. 133 (25.3 %); p = 0.03 No association between being somewhat/very fearful that police are going to arrest or interfere with drug use, having their syringes confiscated by police. | ||||||
| Zlotorzynska et al. (2014) | Income & poverty | Prescription & non-prescription | NR; non-fatal | Post-overdose reports for opioid-related ODs | Income Assistance: The risk of overdose for those injecting on the three days beginning with cheque day was significantly higher than for those injecting on other days; OR (95% CI): 2.06 (1.80–2.36) The risk of overdose on the three days beginning with cheque day was significantly higher for those injecting opioids alone; OR (95% CI): 2.16 (1.83–2.55) Exclusive opioid use was reported in 66 % of overdoses that occurred on the three days beginning with cheque day, while 75 % of overdoses on other days involved opioid use; OR (95% CI): 0.63 (0.47–0.84) |
Fair |
Statistically significant results denoted in bold.
Table 3.
Study Design and Sample Characteristics of Included Studies.
| First Author (Year) | Study design/ Location | Sample characteristics | Ethnicity | Recruitment and data source |
|---|---|---|---|---|
| Amundsen (2015) | Cross-sectional/ Norway | N: 1628 Age: Mean: 38.4; Sex: 76.4 % male |
NR | - Norwegian Cause of Death Registry (2003–2009) - linked to administrative databases |
| Binswanger et al. (2007) | Cohort/ USA | N: 30,237; Age: Mean (SD): 33.4 (9.8); Sex: 87.0 % male |
White, non-Hispanic: 62 %; Black, non-Hispanic: 20 %; Hispanic: 13 %; Native American, Alaska Native, non-Hispanic: 3%; Asian or Pacific Islander, non-Hispanic: 2% |
- Washington State Department of Corrections (1999–2003) - linked to National Death Index |
| Bohnert et al. (2011) | Longitudinal data/ USA | *N: 74 police precincts; Age: Mean percent under 35 (SD): 51.2 % (7.5); Sex: Mean percent male (SD): 47.0 % (2.3) male |
*Black: Mean percent (SD): 27.5 % (27.2) | - Office of the Chief Medical Examiner data in New York |
| Brinkley-Rubinstein et al. (2018) | Cross-sectional/ USA | N: 530; Age:18−39: 45.3%, 40+: 54.7 %; Sex: 70.9 % male |
White: 90.2 %;Non-white: 9.8 % | - Rhode Island Office of Medical Examiner Data - Linked to Rhode Island Department of Corrections |
| Burns et al. (2004) | Cross-sectional/ Australia | N: 163; Age: Median: 21; Sex: 54.0 % male |
NR | - Survey with young people (15–30 years) who used heroin from three inner-metropolitan Melbourne general practices (June - December 2000) - linked to the Pharmaceutical Benefits Scheme |
| Brown and Wehby, 2019 | Longitudinal data/ USA | N: 50 states; Age: Mean: NR; Sex: NR |
NR | - CDC’s Detailed Mortality File (1999−2014) - US Census Bureau Population Survey - Freddie Mac House Price Index |
| Campbell et al. (2018) | Cohort/ USA | N: 396,452; Age: Mean: 51.83; Sex: 41.0 % male |
Hispanic: 17.2 %; Asian: 9.7 %; Black: 9.4 %; Multi-racial: 4.5 %; Native American: 0.6 %; Other or unknown: 1.8 %; White: 56.8 % |
- Kaiser Permanente Northern California Electronic Health Records database (2011−2014) |
| Carrà et al. (2017) | Cross-sectional/ Italy | N: 265; Age: Mean (SD): 35.4 (9.4); Sex: 79.0 % male |
NR | - Therapeutic community program participants - Completed survey for the Psychiatric and Addictive Dual Disorders in Italy project (2010) |
| Cerdá et al. (2013) | Case control/ USA | N: 6413; Age:15−44 :58.9%,45−64: 41.1 %, Sex: 77.9 % male |
White: 39.6 %; Black: 25.7 %; Hispanic: 29.7 % | - Office of the Chief Medical Examiner New York (2000−2006) |
| Cheng et al. (2013) | Cross-sectional/ USA | N: 254; Age:18−44 years:57.5%, 45 years or older:42.5 %; Sex: NR |
White: 98.3 %; Black: 0.4 %; Other: 0.8 % |
- Prescription Pain Medication Dataset from the Utah Department of Health (2008−2009) - Office of the Medical Examiner - linked to the Labour Commission database |
| Cochran et al. (2017) | Cohort/ USA | N: 297,634; Age:18−29:47.3%,30−64: 52.7 %; Sex: 28.7 % male |
White: 56.2 %; Black: 28.2 %; Hispanic: 12.1 %; Other: 3.6 % | - Medicaid records from Pennsylvania Department of Human Services (2010−2012) |
| Coolen et al. (2009) | Cross sectional/ USA | N: 1668 Age: <18−44: 50.5%, 45–65+: 49.5; |
NR | - Washington State Department of Health (2004−2007) |
| Cropsey et al. (2013) | Cross-sectional/ USA | N: 478; Age: Mean (SD): 35.7 (11.1); Sex: 67.3 % male |
White: 44.4 %; Black: 52.9 %; Other: 2.7 % | - Survey with criminal justice involved individuals who reported to a community corrections office for drug monitoring (2012) |
| Dunn et al. (2016) | Cross-sectional/ USA | N: 345; Age: 29.1 % older than 50 years; Sex: 44.8 % male |
Caucasian: 60.0 %; Hispanic: 3.5 % |
- Survey with methadone maintenance clinic and syringe program participants |
| Feng et al. (2016) | Cross-sectional/ USA | N: 9647; Age: -20 −34: 42.0%, 35–55+: 57.9 %; Sex: 48.0 % male |
Non-Hispanic White: 73.9 %; Non-Hispanic Black: 9.5 %; Hispanic: 9.4 %; Other: 7.3 % |
- Nevada State inpatient and emergency department databases (2011−2013) - linked to the US census five year (2009−2013) American Community Survey |
| Fernandes et al. (2015) | Cohort/ USA | N: 358; Age: 18–44: 57.5 %; 45–64: 42.5 %, Sex: 41.5 % male |
White: 84.1 %; Other:15.9 % | - Montana’s Office for Vital Records and Montana Medicaid enrolment records (2003−2012) |
| Hasegawa et al. (2014) | Cohort/ USA | N: 19,709; Age: Median (IQR): 42 (27−55); Sex: 43.0% male |
Non-Hispanic White: 69 %; Non-Hispanic Black: 9%; Hispanic: 15 %; Other: 4% |
- California and Florida State Emergency Department Databases and State Inpatient Databases (2010−2011) |
| Hollingsworth et al. (2017) | Longitudinal data/ USA | N: 3138 counties; Age: NA; Sex: NA |
NR | - State Emergency Department Databases - CDC Multiple Cause of Death files |
| Jenkins et al. (2011) | Cross-sectional/ USA | N: 443; Age: Mean (SD): 38 (12); Sex: 71.0 % male |
White: 73 %; African-American: 8%; Native American, Alaska Native: 5%; Native Hawaiian, Pacific Islander: 1%; Asian, South Asian: 1%; Latino, Hispanic: 6%; Multi-racial: 6% | - Surveys for individuals using syringe exchange sites in King County and Seattle, Washington |
| Marshall et al. (2017) | Ecological/ USA | N: 1065; Age: 0–44: 48.8 %,45–65+: 51.2 %; Sex: 61 % male |
Hispanic: 12 %;White: 84 %;Asian: 2.4 %;Black: 1.7 % | -Orange County Coroner Division’s data file (2010−2014) |
| McAuley and Best (2012) | Cross-sectional/ United Kingdom | N: 291; Age: Mean (SD): 33.5 (8.9); Sex: 82.1 % male |
NR | -Drug-related death monitoring data from two Scottish National Health Service Board areas (2006−2007) |
| Meiman et al. (2015) | Cross sectional/ USA | N: 1540 Age: <18−34: 68.1%, 35–55+: 31.9 %; Sex: 71.1 % male |
Black: 12.7 %;White: 77.2 %;Other: 5.1 % | -Wisconsin Division of Public Health’s emergency department visit and hospital discharge datasets (2003–2012) |
| Nadpara et al. (2018) | Nested case-control/ USA | N: 45,153; Age: 18−54: 60.0%,55−65+: 40.0 %;Sex: 52.1 % male |
Non-Hispanic White: 56.8 %; Non-Hispanic Black: 15.4 %;Hispanic: 5.2 %;Other: 22.7 % |
-PharMetrics Plus data set from the IMS Health Real-World Data Adjudicated Claims–US Database |
| Ochoa et al. (2005) | Cross-sectional/ USA | N: 795 Age: 15−19: 23.1%20−24: 51.1 %25−29: 25.8 %;Sex: 66.8 % male |
Caucasian: 80.4 %; Native American:1.1 %; African–American: 2.3 %; Asian/Pacific Islander: 0.6 %; Hispanic 3.6 %; Mixed, other: 10.9 % |
- Survey with participants were who were <30 years old and had injected once or more in the prior month recruited using street outreach and snowball techniques |
| Ødegård et al. (2010) | Cohort/ Norway | N: 338 Age: Mean: 25.6 [Men]; 24.3 [Women]; Sex: 72 % male |
NR | - Survey with participants receiving treatment at the State Clinic for Drug Addicts (1981−1991) |
| Patrick et al. (2016) | Interrupted time-series/ USA | N: 343−34 (states) Age: NR; Sex: NR |
NR | -State prescription drug monitoring programs (<2011) -National Alliance for State Model Drug Laws (2012−2013) |
| Paulozzi et al. (2009) | Cross-sectional/ USA | N: Methadone (n = 87) Other Opioids (n = 163) Age: 18−34: 38.4%35−45+: 61.6 %;Sex: 67.6 % male |
NR | - Coroner’s data from West Virginia (2006) -West Virginia Controlled Substances Monitoring Program |
| Ponicki et al. (2018) | Longitudinal data/ USA | N: 5513 Age: Mean (SD): 0−19: 27.59 (4.53) 20−24: 7.37 (1.05) 25−44: 25.55 (4.85) 45−64: 24.70 (3.33) Sex: 49.6 % male |
NR | -Nebraska and South Dakota inpatient hospital discharges (2007−2012) |
| Rintoul et al. (2010) | Cohort/Australia | N: 172 Age: <18−44: 59.3%45−65+: 40.8 %Sex: 58.1 % male |
NR | -National Coroners Information System (NCIS) Victorian Drugs Module (VDM; 2003) -VIFM toxicology database (<2003) |
| Seal et al. (2001) | Cross-sectional/ USA | N: 1427 <39: 406 (28.5 %)40−50+: 1021 (71.5 %) |
Black: 51.3 %;White: 35.2 %;Latino: 7.3 %; Asians, Pacific Islanders, Native Americans, and Mixed: 6.1 % |
-Survey with street recruited people who inject drugs in San Francisco Bay Area, California |
| Shah et al. (2005) | Longitudinal data/ USA | N: 1120 Age: <15 to 44: 67.0 %;45–70+: 33.0 %;Sex: 77.4 % male |
White, non-Hispanic: 42.0 %; Hispanic: 52.5 %; American Indian: 2.0 %; Black or Asian: 2.9 % |
-Office of the Medical Investigator and the Toxicology Bureau of the Scientific Laboratory Division, New Mexico Department of Health (1998−2002) |
| Sharp and Melnik (2015) | Longitudinal data/ USA | N: NR Age: <15−85+ Sex: NR |
NR | -New York state vital statistics multiple-cause-of-death data - New York state Medicaid enrollment data. |
| Sherman et al. (2007) | Cohort/ USA | N: NR Age: Median (IQR) in group Experienced overdose (n = 90): Yes: 28.7 (26.0, 31.5); No: 29.1 (25.9, 33.0); Sex: 56.7 % male |
Race in group experienced OD: African American: Yes: 18.0 %;No: 45.4 % |
-Survey with young people who use drugs in the Risk Evaluation and Assessment of Community Health III (REACH III) cohort (1999−2002) |
| Siegler et al. (2014) | Cross-sectional/ USA | N: 2649 Age:15–44: 48.2 %; 45–84: 51.7 %;Sex: 73.8 % male |
Non-Hispanic Black: 21.6 %; Non-Hispanic White: 46.2 %; Hispanic: 29.6 %; Non-Hispanic Other: 2.6 % |
- NYC linked death certificates and medical examiner files (2005−2010) |
| Visconti et al. (2015) | Cross-sectional/ USA | N: 331 Age: Mean (SD): 48.2 (12.5); Sex: 68.3 % male |
Non-Hispanic White: 71.0 %; African-American:19.9 %; Hispanic 4.2 %;Asian 2.1 %; Other: 7% |
-California Electronic Death Reporting System (2010−2012) |
| Wagner et al. (2015) | Cross-sectional/ USA | N: 573 Age: Mean (SD): 43.5 (12); Sex: 72.8 % male |
White: 50.1 %; Hispanic/Latino: 31.1 %;Other: 18.0 % |
-Survey with people who inject drugs in San Diego, California |
| Zlotorzynska et al. (2014) | Cross-sectional/ Canada | N: 1338 Age: NR; Sex: NR |
NR | - Insite facility’s on-site surveillance database |
*Aggregate data collected at police precinct level.
The included studies covered a wide range of topics, and included variables related to eight elements of SEM: criminal justice system involvement (n = 13); income (n = 13); employment (n = 11); social support (n = 9); health insurance (n = 8); housing/homelessness (n = 8); education (n = 8); and composite measures of socio-economic status or deprivation (n = 6). A summary of measures and findings as well as risk of bias assessments for the 37 included studies can be found in Table 4.
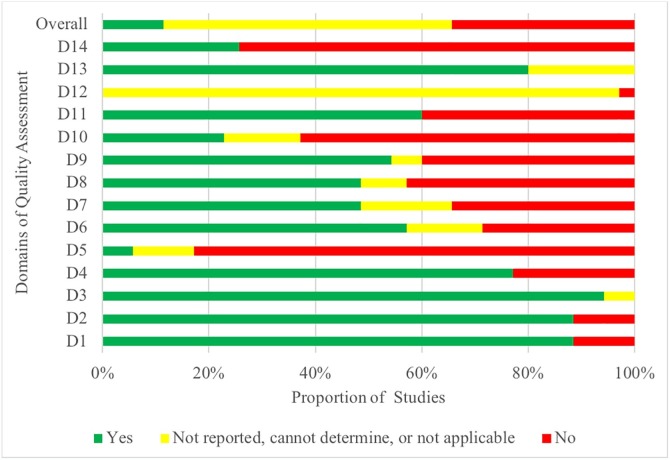
3.2. Risk of bias within included studies
Each study was evaluated across a set of domains to assess risk of bias, the results of which can be seen in Table 2 . Serious concerns related to risk of bias were present, and the way the literature from observational cohort and cross-sectional studies performs on each metric in aggregate can be seen visually in Fig. 2 . Many studies only measured exposure variables once during the study; had a lack of multivariate controls for confounding variables; did not include information about power, effect estimates, or a sample size justification; or reported bivariate relationships only. The dataset thus is largely observational with no experimental study designs in the pool of included papers, allowing for conclusions to be drawn about the correlations and statistical associations present between variables in the data but not about causal pathways identifying how SEM impacts opioid overdose. The absence of significant findings in some studies should not be interpreted as there being no relationship between these factors, particularly considering the risk of bias within the referenced studies, the quality of measures included, and the type of analysis conducted. Similarly, it is possible that positive relationships identified are also due to bias within the studies rather than a true relationship.
Table 2.
Summary of Risk of Bias Assessments for Included Studies. (For interpretation of the references to colour in this table, the reader is referred to the web version of this article.)
 |
Notes: Y = yes, N = no, CD = cannot determine, NR = not reported, N/A = not applicable.
*Domains 1–14 for Studies Assessed with the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies).
D1. Was the research question or objective in this paper clearly stated?
D2. Was the study population clearly specified and defined?
D3. Was the participation rate of eligible persons at least 50 %?
D4. Were all the subjects selected or recruited from the same or similar populations (including the same time period)? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants?
D5. Was a sample size justification, power description, or variance and effect estimates provided?
D6. For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured?
D7. Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed?
D8. For exposures that can vary in amount or level, did the study examine different levels of the exposure as related to the outcome (e.g., categories of exposure, or exposure measured as continuous variable)?
D9. Were the exposure measures clearly defined, valid, reliable, and implemented consistently across all study participants?
D10. Was the exposure(s) assessed more than once over time?
D11. Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants?
D12. Were the outcome assessors blinded to the exposure status of participants?
D13. Was loss to follow-up after baseline 20 % or less?
D14. Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)?
^Domains 1–12 for Studies Assessed with the Quality Assessment Tool for Case Control Studies.
D1. Was the research question or objective in this paper clearly stated and appropriate?
D2. Was the study population clearly specified and defined?
D3. Did the authors include a sample size justification?
D4. Were controls selected or recruited from the same or similar population that gave rise to the cases (including the same timeframe)?
D5. Were the definitions, inclusion and exclusion criteria, algorithms or processes used to identify or select cases and controls valid, reliable, and implemented consistently across all study participants?
D6. Were the cases clearly defined and differentiated from controls?
D7. If less than 100 percent of eligible cases and/or controls were selected for the study, were the cases and/or controls randomly selected from those eligible?
D8. Was there use of concurrent controls?
D9. Were the investigators able to confirm that the exposure/risk occurred prior to the development of the condition or event that defined a participant as a case?
D10. Were the measures of exposure/risk clearly defined, valid, reliable, and implemented consistently (including the same time period) across all study participants?
D11. Were the assessors of exposure/risk blinded to the case or control status of participants?
D12. Were key potential confounding variables measured and adjusted statistically in the analyses? If matching was used, did the investigators account for matching during study analysis?
Fig. 2.
Aggregate Risk of Bias Plot for Observational Cohort and Cross-Sectional Studies.
3.3. Dimensions of SEM
3.3.1. Criminal justice system involvement
Criminal justice system involvement was included as a measure of SEM due to the close link between socioeconomic precarity and incarceration as well as the economic and social constraints that are experienced post-release. Most studies with measures of criminal justice system involvement (11/13) found a significant positive association between these measures and overdose (Binswanger et al., 2007; Bohnert et al., 2011; Brinkley-Rubinstein et al., 2018; Carrà et al., 2017; ; Jenkins et al., 2011; McAuley and Best, 2012; Ochoa et al., 2005; Ødegård et al., 2010; Seal et al., 2001; Wagner et al., 2015) where overdose occurred at higher rates or with greater odds after release from prison. Most studies operationalized criminal justice system involvement as recent incarceration (yes/no), however some also looked at length of time incarcerated (Brinkley-Rubinstein et al., 2018; Ochoa et al., 2005; Seal et al., 2001), time since release (Binswanger et al., 2007; Brinkley-Rubinstein et al., 2018; McAuley and Best, 2012; Ødegård et al., 2010), misdemeanor arrest rates (Bohnert et al., 2011), or outcomes for those under community supervision (Cropsey et al., 2013).
3.3.2. Income and poverty
Nearly two-thirds (8/13) of the studies included in our review with income or poverty-related variables found a significant positive association between measures of poverty and overdose outcomes (Cerdá et al., 2013; Feng et al., 2016; Marshall et al., 2017; Meiman et al., 2015; Ochoa et al., 2005; Seal et al., 2001; Visconti et al., 2015; Zlotorzynska et al., 2014). The majority of studies operationalized income through either neighborhood-level poverty rate or median household income, with two studies looking at prohibited income generation activities (i.e., sex work), and one study looking at income disbursement. Two studies included measures of income or poverty and its intersections with race/ethnicity.
3.3.3. Employment
Two of eleven of the studies with measures of unemployment found a significant positive association with overdose, where higher levels of unemployment were associated with higher overdose rates (Cheng et al., 2013; Hollingsworth et al., 2017). Most of the studies not finding conclusive evidence to support employment being associated with overdose. Half of the studies operationalized employment using unemployment rates at the county or state level, while the other half used measures of individual employment status, most commonly comparing those who were employed to those who were unemployed.
3.3.4. Social support
Articles including measures of social support were included to address the element of SEM related to social exclusion or isolation. A total of six of the nine studies including measures of social support that were included in our review found a significant negative association to be present between the measures of social support that they included and the overdose outcome investigated (Burns et al., 2004; Cerdá et al., 2013; Cheng et al., 2013; Nadpara et al., 2018; Paulozzi et al., 2009; Shah et al., 2005). Six of the included studies operationalized social support with measures of marital status at the individual level (Cheng et al., 2013; Cropsey et al., 2013; Dunn et al., 2016; Nadpara et al., 2018; Paulozzi et al., 2009; Shah et al., 2005), three studies included measures of living arrangements at the individual level (Burns et al., 2004; Carrà et al., 2017; Dunn et al., 2016), one study included perceived social support and relationship status, (Burns et al., 2004), and one study used a state-level measure of family fragmentation (Cerdá et al., 2013).
3.3.5. Health insurance
Studies that included measures of health insurance status were included, based on the close connection between health insurance and socioeconomic status (SES) in the US, and the access to health care that insurance provides. For studies of health insurance, six of eight papers reviewed found significant associations between measures of health insurance and opioid overdose (Coolen et al., 2009; Fernandes et al., 2015; Hasegawa et al., 2014; Cochran et al., 2017; Meiman et al., 2015), where insurance type (enrollment in or eligibility for Medicaid in most cases) was positively associated with overdose. All of the included studies had samples from the US population, and all of them except one (Brown and Wehby, 2019) measured health insurance at the individual level, typically comparing those with Medicaid to those with other types of insurance or to a non-Medicaid population. All but one study used administrative data to link health insurance to overdose, and the study that used self-reported insurance and overdose history did not find evidence of a significant association (Dunn et al., 2016). Notably, both studies that failed to find an association used measures of uninsured vs. insured status. In contrast, the remaining six studies included multiple insurance types, examining overdose outcomes recorded in administrative databases.
3.3.6. Homelessness and housing status
Overall, four of the eight studies including measures of housing reported significant negative associations between measures of housing status/homelessness and opioid overdose outcomes (Seal et al., 2001; Brown and Wehby, 2019; Sherman et al., 2007; Wagner et al., 2015), where homelessness and lower housing prices were associated with higher rates of overdose. Two of these measured housing status at a population level with one measuring state-level housing status as median household price (Brown and Wehby, 2019) and the other measuring neighborhood-level dilapidated housing structures (Cerdá et al., 2013). These same two studies obtained measures of fatal overdose through administrative data linkages. The remaining six studies obtained individual self-reported measures of homelessness and non-fatal overdose.
3.3.7. Education
Six of eight of the studies included in our review found a significant negative association between measures of education and overdose (Cropsey et al., 2013; Cheng et al., 2013; Marshall et al., 2017; Patrick et al., 2016; Paulozzi et al., 2009; Siegler et al., 2014) where, in most cases, higher levels of educational attainment were associated with lower rates of opioid-related fatal overdose. Two of the included studies collected educational attainment data at the zip code or state level while six studies used measures of individual educational attainment.
3.3.8. Socioeconomic status or deprivation composite measures
A total of five out of six of the studies included in our review investigating SES found a significant negative association between the combined measures of SES that they included, and the overdose outcome investigated (Carrà et al., 2017; Seal et al., 2001; Rintoul et al., 2010; Amundsen, 2015; Bohnert et al., 2011) where low SES was associated with higher rates of overdose. Each of the six included studies operationalized composite SES measures differently, introducing slightly different combination of measures of income, employment, and education. Four of these studies examined deprivation variables at the population level (Campbell et al., 2018; Rintoul et al., 2010; Amundsen, 2015; Bohnert et al., 2011) while two studies used measures of participant characteristics or SES at the individual level (Carrà et al., 2017; Seal et al., 2001).
4. Discussion
4.1. Summary of findings
Of the studies that yielded significant findings, all but one found results linking socioeconomic factors and overdose in the hypothesized direction, whereby increased vulnerability was associated with a higher rate or increased likelihood of overdose. Six out of eight dimensions of SEM had significant, positive associations with opioid overdose in most studies that investigated them, including insurance status, criminal justice involvement, education, social support, income, and SES composite measures. These results are consistent with a growing body of literature that connects aspects of marginalization and drug-related harm (Allen et al., 2014; Galea et al., 2006; Green et al., 2012; Ho, 2017; Lanier et al., 2012; Silva et al., 2012; Stewart et al., 2004; Carrà et al., 2017; Seal et al., 2001) and is indicative of the precarity and risk that people who use opioids experience when they are socially and economically marginalized.
Our review revealed strong connections between socioeconomic factors and overdose in multiple substantive domains. For example, receiving state-funded health insurance is associated with increased risk of overdose, likely because it is associated with low income. Overdose is also a more common occurrence for those recently released from prison and for those who have a history of incarceration. Having social support in the form of being in a relationship was inversely associated with overdose, as was having higher levels of educational attainment. Composite measures of SES show that experiencing hardship across multiple indicators of social and economic well-being is positively associated with overdose. Finally, overdose rates are higher in low income areas and in situations where people are living in poverty, and racialized populations are more highly represented in low-income overdose fatality rates than non-racialized populations. In this review we therefore find evidence to suggest that aiming to decrease socioeconomic disadvantage may be an important part of tackling the opioid overdose crisis.
Risk of bias, measurement limitations, and analytic issues demonstrate why caution should be exercised in the interpretation of a lack of consistent association with overdose in the two areas of SEM where less than half of studies found significant relationships: employment and housing/homelessness. In several cases, reviewed articles did not find significant relationships between employment and overdose, and as many of the studies reported aggregate measures, it is difficult to know what is underlying these findings. Extant literature robustly demonstrates the labour market exclusion experienced by people who use drugs, and stands in contrast with the findings of these two elements of the review, where previous studies that have assessed job precarity, job type, and other income-generation practices for people who use drug and found associations with drug-related harm (Richardson et al., 2014; 2015). Similarly, prior studies have shown that the stigmatizing experience of being unstably housed exposes individuals to social harms that may elevate risk of overdose such as exposure to verbal and physical assault, lack of access to safe space, street-based activities, and social exclusion (Fischer et al., 2004). In our review, some studies indicated that being homeless or living in an area with low housing prices is associated with increased likelihood of overdose, but such associations were present in only half of the studies that examined housing status/homelessness.
4.2. Limitations of the evidence included in the review
We reviewed literature on a wide range of socioeconomic factors and opioid overdose. In many cases, these factors are interrelated and difficult to separate, leading to difficulty in ascertaining which aspects of social and economic marginalization are the most strongly associated with overdose. For example, the associations present in studies in the health insurance category that compared overdose rates for those enrolled in Medicaid compared to those not enrolled in Medicaid, may have also been reflecting the income differences between these two populations due to low income being a key criterion for Medicaid eligibility. From a specificity perspective, this is a limitation, however, it also reflects how interconnected social and economic factors are, and demonstrates the value in taking a broad approach to the definition of socioeconomic marginalization.
To make the results of our review widely applicable and of maximal use to those making decisions in the overdose crisis, we chose to include studies with any type of overdose measure in the review. By undertaking a broad review, we were able to explore whether the effects of SEM were similar across different elements of SEM, different settings, and different populations. A narrower review would have greatly reduced included studies and may have been more susceptible to erroneous conclusions based on bias (Gøtzsche, 2000). However, including a variety of outcome measures also presents limitations, including the inability to identify unique risks from different outcomes (e.g., fatal and non-fatal overdose) and the inability to conduct statistical meta-analyses. Following the results of this broad initial review on SEM and overdose, future researchers would do well to carry out explicit a priori subgroup analyses with more narrowly defined outcome measures.
Our review of SEM and opioid overdose revealed an evidence base that is underdeveloped. Many studies included in our review were not designed in ways that could reliably rule out confounding variables and had threats to validity that affected the interpretation of results. Moreover, several of these same studies measured social or economic factors and overdose using overlapping, poorly specified or inappropriate time frames that could mask potentially real associations. Many of the studies that looked at fatal overdose relied on administrative datasets that did not have suitable operationalization of the measures of SEM included or were primarily interested in other (non-SEM) independent variables and therefore had limited conceptual or methodological consideration for inclusion of indicators of SEM (i.e., inclusion as control variables). Other studies included measures of socioeconomic factors only in descriptive or bivariate analyses. Although we were hoping to analyze marginalization and overdose, most studies merely allowed us to draw conclusions about socioeconomic factors and were designed such that it is difficult to determine the true root causes. The results of this review indicate the difficulty present in statistically linking distal, upstream social and socioeconomic determinants to an acute health event such as overdose and highlight the need for more robust research methods than those commonly used to investigate these connections.
4.3. Policy implications and recommendations for future research
Despite the multiple socioeconomic factors that were included in the search protocol of this review, there were no studies that directly measured the impact of drug enforcement and policing, the density of alcohol outlets, money lending services, housing availability and affordability, material factors (such as food security, service access), policy (such as drug policy, income or employment support policy), or social stigma on opioid overdose outcomes. These evidence gaps represent important elements of marginalization that may impact overdose outcomes for people who use opioids and could significantly help to guide the development of effective policies to prevent overdose. There is a critical need for well-designed studies that explicitly and comprehensively examine the association between SEM variables and overdose as their primary purpose.
Furthermore, very few studies reported on the different ways that SEM affects those across varying ethnic backgrounds, gender, sexual orientation among other marginalized or oppressed social statuses. Few studies looked at combined measures of SEM or the experience of multiple elements of social and economic marginalization simultaneously. Given the tendency for these factors to co-occur and the potential relevance of intersectional disadvantage, research studies that can robustly include multiple measures of SEM are important to avoid incorrectly attributing associations to the included measures that may in fact be due to other omitted variables.
Given the ongoing overdose crisis, focused research that is designed to be more applicable to policy and programmatic prevention of overdose and drug-related harm is needed. The COVID-19 pandemic and the associated mitigation strategies have the potential to further exacerbate the overdose crisis, through increased SEM. This indicates an urgent need for policies that better support the social and economic security of people who use opioids, and research that can support such decision-making. Studies designed to inform decision making around upstream determinants of health in response to the overdose crisis and the COVID-19 pandemic could be especially valuable for policy makers and program managers working to combat overdose. This includes research that strengthens inference, for example, by using specific and meaningful measures, comparative research designs, and natural experiments. Nevertheless, the studies included in this review found results in the hypothesized direction in most cases, where increasing social and economic precarity was associated with increased fatal and non-fatal overdose for people who use opioids. This suggests that initiatives targeting health equity and aiming to decrease socioeconomic marginalization are a valuable and necessary part of combatting the overdose crisis and should be part of strategic planning for overdose prevention.
Contributors
LR and JVD were responsible for conceptualization. LR was responsible for supervision, funding acquisition, and writing (review and editing). JVD was responsible for project administration, formal analysis, methodology, and writing (original draft preparation). CT was responsible for formal analysis, investigation, and writing (review and editing). SM was responsible for formal analysis and investigation. MK was responsible for data curation and methodology.
Role of funding source
This study was supported by a Canadian Insitutes of Health Research (CIHR) Knowledge Synthesis Grant (OCK-156771) as well as a CIHR Foundation grant (CIHR; FDN-154320) that supports the research activities of LR. LR is additionally supported by a New Investigator award from CIHR (MSH 217672) and a Scholar Award from the Michael Smith Foundation for Health Research. JVD is supported by a Postdoctoral Fellow Award from CIHR and a Research Trainee award from the Michael Smith Foundation for Health Research. SM is supported by a Doctoral Research Award from CIHR. MK is supported by Vanier Canada Graduate Scholarship and Pierre Elliott Trudeau Doctoral Scholarships. The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Declaration of Competing Interest
No conflict declared.
Acknowledgements
The authors would like to express their gratitude for the involvement of the following colleagues who participated in the knowledge synthesis project: A. Long, M.C. Zak, R. Bruce, J. Li, E. Charlebois, K. Mattison, B. Jackson, and J. Briggs.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.drugalcdep.2020.108127.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- Allen J., Balfour R., Bell R., Marmot M. Social determinants of mental health. Int. Rev. Psychiatry. 2014;26(4):392–407. doi: 10.3109/09540261.2014.928270. [DOI] [PubMed] [Google Scholar]
- Amundsen E.J. Drug-related causes of death: socioeconomic and demographic characteristics of the deceased. Scand. J. Public Health. 2015;43(6):571–579. doi: 10.1177/1403494815585909. [DOI] [PubMed] [Google Scholar]
- Binswanger I., Stern M.F., Elmore J.G. ’Release from prison–a high risk of death for former inmates’: author’s reply. N. Engl. J. Med. 2007;356(17):1786–1787. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohnert A.S.B., Nandi A., Tracy M., Cerda M., Tardifff K.J., Vlahov D., Galea S. Policing and risk of overdose mortality in urban neighborhoods. Drug Alcohol Depend. 2011;113(1):62–68. doi: 10.1016/j.drugalcdep.2010.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brinkley-Rubinstein L., Macmadu A., Marshall B.D.L., Heise A., Ranapurwala S.I., Rich J.D., Green T.C. Risk of fentanyl-involved overdose among those with past year incarceration: findings from a recent outbreak in 2014 and 2015. Drug Alcohol Depend. 2018;185:189–191. doi: 10.1016/j.drugalcdep.2017.12.014. [DOI] [PubMed] [Google Scholar]
- Brown E., Wehby G.L. Economic conditions and drug and opioid overdose deaths. Med. Care Res. Rev. 2019;76(4):462–477. doi: 10.1177/1077558717722592. [DOI] [PubMed] [Google Scholar]
- Brunner E., Marmot M. Social Determinants of Health. 2. 2006. Social organization, stress, and health; pp. 17–43. [Google Scholar]
- Burns J.M., Martyres R.F., Clode D., Boldero J.M. Overdose in young people using heroin: associations with mental health, prescription drug use and personal circumstances. Med. J. Aust. 2004;181(7):S25–S28. doi: 10.5694/j.1326-5377.2004.tb06351.x. [DOI] [PubMed] [Google Scholar]
- Campbell C.I., Bahorik A.L., VanVeldhuisen P., Weisner C., Rubinstein A.L., Ray G.T. Use of a prescription opioid registry to examine opioid misuse and overdose in an integrated health system. Prev. Med. 2018;110:31–37. doi: 10.1016/j.ypmed.2018.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrà G., Crocamo C., Borrelli P., Tabacchi T., Bartoli F., Popa I., Montomoli C., Clerici M. Area-level deprivation and adverse consequences in people with substance use disorders: findings from the psychiatric and addictive dual disorder in Italy (PADDI) study. Subst. Use Misuse. 2017;52(4):451–458. doi: 10.1080/10826084.2016.1240696. [DOI] [PubMed] [Google Scholar]
- Cerdá M., Ransome Y., Keyes K.M., Koenen K.C., Tardiff K., Vlahov D., Galea S. Revisiting the role of the urban environment in substance use: the case of analgesic overdose fatalities. Am. J. Public Health. 2013;103(12):2252–2260. doi: 10.2105/AJPH.2013.301347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng M., Sauer B., Johnson E., Porucznik C., Hegmann K. Comparison of opioid-related deaths by work-related injury. Am. J. Ind. Med. 2013;56(3):308–316. doi: 10.1002/ajim.22138. [DOI] [PubMed] [Google Scholar]
- Cochran G., Gordon A.J., Gellad W.F., Chang C.-C.H., Lo-Ciganic W.-H., Lobo C., Cole E., Frazier W., Zheng P., Kelley D., Donohue J.M. Medicaid prior authorization and opioid medication abuse and overdose. Am. J. Manag. Care. 2017;23(5):e164. [PMC free article] [PubMed] [Google Scholar]
- Coolen P., Best S., Lima A., Sabel J., Paulozzi L. Overdose deaths involving prescription opioids among Medicaid enrollees – Washington, 2004–2007. MMWR Morb. Mortal. Wkly. Rep. 2009;58(42):1171–1175. [PubMed] [Google Scholar]
- Coroners Service BC . 2019. Fentanyl-Detected Illicit Drug Overdose Deaths - January 1, 2012 to January 31, 2019. [Google Scholar]
- Cropsey K.L., Martin S., Clark C.B., McCullumsmith C.B., Lane P.S., Hardy S., Hendricks P.S., Redmond N. Characterization of opioid overdose and response in a high-risk community corrections sample: a preliminary study. J. Opioid Manag. 2013;9(6):393. doi: 10.5055/jom.2013.0181. [DOI] [PubMed] [Google Scholar]
- Dunn K.E., Barrett F.S., Yepez-Laubach C., Meyer A.C., Hruska B.J., Petrush K., Berman S., Sigmon S.C., Fingerhood M., Bigelow G.E. Opioid overdose experience, risk behaviors, and knowledge in drug users from a rural versus an urban setting. J. Subst. Abuse Treat. 2016;71:1–7. doi: 10.1016/j.jsat.2016.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott S.P., Lopez E.H. A series of deaths involving Carfentanil in the UK and associated post-mortem blood concentrations. J. Anal. Toxicol. 2018;42(4):e41–e45. doi: 10.1093/jat/bkx109. [DOI] [PubMed] [Google Scholar]
- Feng J., Iser J.P., Yang W. Medical encounters for opioid-related intoxications in Southern Nevada: sociodemographic and clinical correlates. BMC Health Serv. Res. 2016;16 doi: 10.1186/s12913-016-1692-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandes J.C., Campana D., Harwell T.S., Helgerson S.D. High mortality rate of unintentional poisoning due to prescription opioids in adults enrolled in Medicaid compared to those not enrolled in Medicaid in Montana. Drug Alcohol Depend. 2015;153:346–349. doi: 10.1016/j.drugalcdep.2015.05.032. [DOI] [PubMed] [Google Scholar]
- Fischer B., Brissette S., Brochu S., Bruneau J., el-Guebaly N., Noel L., Rehm J., Tyndall M., Wild C., Mun P., Haydon E., Baliunas D. Determinants of overdose incidents among illicit opioid users in 5 Canadian cities. CMAJ. 2004;171(3):235–239. doi: 10.1503/cmaj.1031416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S., Nandi A., Coffin P.O., Tracy M., Markham Piper T., Ompad D., Vlahov D. Heroin and cocaine dependence and the risk of accidental non-fatal drug overdose. J. Addict. Dis. 2006;25(3):79–87. doi: 10.1300/J069v25n03_10. [DOI] [PubMed] [Google Scholar]
- Gøtzsche P.C. Why we need a broad perspective on meta-analysis: it may be crucially important for patients. BMJ. 2000;321:585. doi: 10.1136/bmj.321.7261.585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green T.C., McGowan S.K., Yokell M.A., Pouget E.R., Rich J.D. HIV infection and risk of overdose: a systematic review and meta-analysis. AIDS. 2012;26(4):403–417. doi: 10.1097/QAD.0b013e32834f19b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimshaw J., McAuley L.M., Bero L.A. Systematic reviews of the effectiveness of quality improvement strategies and programmes. BMJ Qual. Saf. 2003;12(4):298–303. doi: 10.1136/qhc.12.4.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasegawa K., Brown D.F.M., Tsugawa Y., Camargo C.A. Epidemiology of emergency department visits for opioid overdose: a population-based study. Mayo Clin. Proc. 2014;89(4):462–471. doi: 10.1016/j.mayocp.2013.12.008. [DOI] [PubMed] [Google Scholar]
- Ho J.Y. The contribution of drug overdose to educational gradients in life expectancy in the United States, 1992-2011. Demography. 2017;54(3):1175–1202. doi: 10.1007/s13524-017-0565-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingsworth A., Ruhm C.J., Simon K. Macroeconomic conditions and opioid abuse. J. Health Econ. 2017;56:222–233. doi: 10.1016/j.jhealeco.2017.07.009. [DOI] [PubMed] [Google Scholar]
- Hutton B., S.G, Caldwell D.M., Chaimani A., Schmid C.H., Cameron C. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann. Intern. Med. 2015;162:777–784. doi: 10.7326/M14-2385. [DOI] [PubMed] [Google Scholar]
- Jenkins L.M., Banta-Green C.J., Maynard C., Kingston S., Hanrahan M., Merrill J.O., Coffin P.O. Risk factors for nonfatal overdose at Seattle-area syringe exchanges. J. Urban Health. 2011;88(1):118–128. doi: 10.1007/s11524-010-9525-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jongbloed K., Zhang H., Thomas V., Pearce M., Christian W., Schechter M.T., Spittal P.M. The cedar project: predictors of mortality among young aboriginal people who use drugs in British Columbia. Can. J. Infect. Dis. Med. Microbiol. SA) 2014:31A. [Google Scholar]
- King N.B., Fraser V., Boikos C., Richardson R., Harper S. Determinants of increased opioid-related mortality in the United States and Canada, 1990–2013: a systematic review. Am. J. Public Health. 2014;104(8):e32–42. doi: 10.2105/AJPH.2014.301966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krebs E., Wang L.W., Olding M., DeBeck K., Hayashi K., Milloy M.J., Wood E., Nosyk B., Richardson L. Increased drug use and the timing of social assistance receipt among people who use illicit drugs. Soc. Sci. Med. 2016;171:94–102. doi: 10.1016/j.socscimed.2016.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanier W.A., Johnson E.M., Rolfs R.T., Friedrichs M.D., Grey T.C. Risk factors for prescription opioid-related death, Utah, 2008–2009. Pain Med. 2012;13(12):1580–1589. doi: 10.1111/j.1526-4637.2012.01518.x. [DOI] [PubMed] [Google Scholar]
- Marshall J.R., Gassner S.F., Anderson C.L., Pena J., Chakravarthy B. Socioeconomic and geographical disparities in prescription and illicit opioid-related overdose deaths in Orange County, California, from 2010–2014. Acad. Emerg. Med. 2017;24(Supplement 1):S216. doi: 10.1080/08897077.2018.1442899. [DOI] [PubMed] [Google Scholar]
- McAuley A., Best D. A quantitative exploration of risk factors associated with drug-related deaths involving heroin, alcohol or methadone in the West of Scotland. Addict. Res. Theory. 2012;20(2):153–161. [Google Scholar]
- Meiman J., Tomasallo C., Paulozzi L. Trends and characteristics of heroin overdoses in Wisconsin, 2003-2012. Drug Alcohol Depend. 2015;152:177–184. doi: 10.1016/j.drugalcdep.2015.04.002. [DOI] [PubMed] [Google Scholar]
- Milloy M.J., Wood E., Reading C., Kane D., Montaner J., Kerr T. Elevated overdose mortality rates among First Nations individuals in a Canadian setting: a population-based analysis. Addiction. 2010;105(11):1962–1970. doi: 10.1111/j.1360-0443.2010.03077.x. [DOI] [PubMed] [Google Scholar]
- Nadpara P.A., Joyce A.R., Murrelle E.L., Carroll N.W., Carroll N.V., Barnard M., Zedler B.K. Risk factors for serious prescription opioid-induced respiratory depression or overdose: comparison of commercially insured and veterans health affairs populations. Pain Med. 2018;19(1):79–96. doi: 10.1093/pm/pnx038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health . 2018. Study Quality Assessment Tools.https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (Accessed 3 October 2018) [Google Scholar]
- Ochoa K.C., Davidson P.J., Evans J.L., Hahn J.A., Page-Shafer K., Moss A.R. Heroin overdose among young injection drug users in San Francisco. Drug Alcohol Depend. 2005;80(3):297–302. doi: 10.1016/j.drugalcdep.2005.04.012. [DOI] [PubMed] [Google Scholar]
- Ødegård E., Amundsen E.J., Kielland K.B., Kristoffersen R. The contribution of imprisonment and release to fatal overdose among a cohort of Norwegian drug abusers. Addict. Res. Theory. 2010;18(1):51–58. [Google Scholar]
- Ompad D.C., Nandi V., Cerdá M., Crawford N., Galea S., Vlahov D. Beyond income: material resources among drug users in economically-disadvantaged New York City neighborhoods. Drug Alcohol Depend. 2011;120(1):127–134. doi: 10.1016/j.drugalcdep.2011.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otterstatter M.C., Amlani A., Guan T.H., Richardson L., Buxton J.A. Illicit drug overdose deaths resulting from income assistance payments: analysis of the ‘check effect’ using daily mortality data. Int. J. Drug Policy. 2016;33:83–87. doi: 10.1016/j.drugpo.2016.05.010. [DOI] [PubMed] [Google Scholar]
- Patrick S.W., Fry C.E., Jones T.F., Buntin M.B. Implementation of prescription drug monitoring programs associated with reductions in opioid-related death rates. Health Aff. 2016;35(7):1324–1332. doi: 10.1377/hlthaff.2015.1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paulozzi L.J., Logan J.E., Hall A.J., McKinstry E., Kaplan J.A., Crosby A.E. A comparison of drug overdose deaths involving methadone and other opioid analgesics in West Virginia. Addiction. 2009;104(9):1541–1548. doi: 10.1111/j.1360-0443.2009.02650.x. [DOI] [PubMed] [Google Scholar]
- Ponicki W.R., Henderson J.A., Gaidus A., Gruenewald P.J., Lee J.P., Moore R.S., Davids S., Tilsen N. Spatial epidemiology of alcohol- and drug-related health problems among northern plains american indians: nebraska and South Dakota, 2007 to 2012. Alcohol.-Clin. Exp. Res. 2018;42(3):578–588. doi: 10.1111/acer.13580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson L., DeBeck K., Feng C., Kerr T., Wood E. Employment and risk of injection drug use initiation among street involved youth in Canadian setting. Prev. Med. 2014;66:56–59. doi: 10.1016/j.ypmed.2014.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson L.A., Long C., DeBeck K., Nguyen P., Milloy M.J.S., Wood E., Kerr T.H. Socioeconomic marginalisation in the structural production of vulnerability to violence among people who use illicit drugs. J. Epidemiol. Community Health. 2015;69(7):686–692. doi: 10.1136/jech-2014-205079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rintoul A.C., Dobbin M.D.H., Drummer O.H., Ozanne-Smith J. Increasing deaths involving oxycodone, Victoria, Australia, 2000–09. Inj. Prev. 2010;17(4):254–259. doi: 10.1136/ip.2010.029611. [DOI] [PubMed] [Google Scholar]
- Schardt C., Adams M.B., Owens T., Keitz S., Fontelo P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med. Inform. Decis. Mak. 2007;7(1):16. doi: 10.1186/1472-6947-7-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seal K.H., Kral A.H., Gee L., Moore L.D., Bluthenthal R.N., Lorvick J., Edlin B.R. Predictors and prevention of nonfatal overdose among street-recruited injection heroin users in the San Francisco Bay Area, 1998–1999. Am. J. Public Health. 2001;91(11):1842–1846. doi: 10.2105/ajph.91.11.1842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah N., Lathrop S.L., Landen M.G. Unintentional methadone-related overdose death in New Mexico (USA) and implications for surveillance, 1998–2002. Addiction. 2005;100(2):176–188. doi: 10.1111/j.1360-0443.2004.00956.x. [DOI] [PubMed] [Google Scholar]
- Sharp M.J., Melnik T.A. Poisoning deaths involving opioid analgesics - New York State, 2003–2012. MMWR Morb. Mortal. Wkly. Rep. 2015;64(14):377–380. [PMC free article] [PubMed] [Google Scholar]
- Sherman S.G., Cheng Y.K., Kral A.H. Prevalence and correlates of opiate overdose among young injection drug users in a large U.S. City. Drug Alcohol Depend. 2007;88(2–3):182–187. doi: 10.1016/j.drugalcdep.2006.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegler A., Tuazon E., O’Brien D.B., Paone D. Unintentional opioid overdose deaths in New York City, 2005–2010: a place-based approach to reduce risk. Int. J. Drug Policy. 2014;25(3):569–574. doi: 10.1016/j.drugpo.2013.10.015. [DOI] [PubMed] [Google Scholar]
- Silva K., Schrager S.M., Kecojevic A., Lankenau S.E. Factors associated with history of non-fatal overdose among young nonmedical users of prescription drugs. Drug Alcohol Depend. 2012;128(1–2):104–110. doi: 10.1016/j.drugalcdep.2012.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart L.M., Henderson C.J., Hobbs M.S.T., Ridout S.C., Knuiman M.W. Risk of death in prisoners after release from jail. Aust. N. Z. J. Public Health. 2004;28(1):32–36. doi: 10.1111/j.1467-842x.2004.tb00629.x. [DOI] [PubMed] [Google Scholar]
- Ti L., Richardson L., DeBeck K., Nguyen P., Montaner J., Wood E., Kerr T. The impact of engagement in street-based income generation activities on stimulant drug use cessation among people who inject drugs. Drug Alcohol Depend. 2014;141:58–64. doi: 10.1016/j.drugalcdep.2014.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Draanen J., Tsang C., Mitra S., Karamouzian M., Richardson L. Addressing social determinants in the opioid crisis: a systematic review on socioeconomic marginalization and overdose. PROSPERO. 2018 CRD42018096392 https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=96392. [Google Scholar]
- Visconti A.J., Santos G.M., Lemos N.P., Burke C., Coffin P.O. Opioid overdose deaths in the city and county of San Francisco: prevalence, distribution, and disparities. J. Urban Health-Bull. N. Y. Acad. Med. 2015;92(4):758–772. doi: 10.1007/s11524-015-9967-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner K.D., Liu L., Davidson P.J., Cuevas-Mota J., Armenta R.F., Garfein R.S. Association between non-fatal opioid overdose and encounters with healthcare and criminal justice systems: identifying opportunities for intervention. Drug Alcohol Depend. 2015;153:215–220. doi: 10.1016/j.drugalcdep.2015.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2017. Carfentanil: Critical Review Report. Geneva, 2017. (Accessed 3 October 2018) [Google Scholar]
- Xiang Y.X., Zhao W.Y., Xiang H.Y., Smith G.A. ED visits for drug-related poisoning in the United States, 2007. Am. J. Emerg. Med. 2012;30(2):293–301. doi: 10.1016/j.ajem.2010.11.031. [DOI] [PubMed] [Google Scholar]
- Zlotorzynska M., Milloy M.J.S., Richardson L., Nguyen P., Montaner J.S., Wood E., Kerr T. Timing of income assistance payment and overdose patterns at a Canadian supervised injection facility. Int. J. Drug Policy. 2014;25(4):736–739. doi: 10.1016/j.drugpo.2014.03.014. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.