Abstract
Background
COVID-19 caused by severe acute respiratory syndrome coronavirus 2 most commonly manifests with fever and respiratory illness. The cardiovascular manifestations have become more prevalent but can potentially go unrecognized. We look to describe cardiac manifestations in three patients with COVID-19 using cardiac enzymes, electrocardiograms, and echocardiography.
Case summaries
The first patient, a 67-year-old Caucasian female with non-ischaemic dilated cardiomyopathy, presented with dyspnoea on exertion and orthopnoea 1 week after testing positive for COVID-19. Echocardiogram revealed large pericardial effusion with findings consistent with tamponade. A pericardial drain was placed, and fluid studies were consistent with viral pericarditis, treated with colchicine, hydroxychloroquine, and methylprednisolone. Follow-up echocardiograms showed apical hypokinesis, that later resolved, consistent with Takotsubo syndrome. The second patient, a 46-year-old African American male with obesity and type 2 diabetes mellitus presented with fevers, cough, and dyspnoea due to COVID-19. Clinical course was complicated with pulseless electrical activity arrest; he was found to have D-dimer and troponin elevation, and inferior wall ST elevation on ECG concerning for STEMI due to microemboli. The patient succumbed to the illness. The third patient, a 76-year-old African American female with hypertension, presented with diarrhoea, fever, and myalgia, and was found to be COVID-19 positive. Clinical course was complicated, with acute troponin elevation, decreased cardiac index, and severe hypokinesis of the basilar wall suggestive of reverse Takotsubo syndrome. The cardiac index improved after pronation and non-STEMI therapy; however, the patient expired due to worsening respiratory status.
Discussion
These case reports demonstrate cardiovascular manifestations of COVID-19 that required monitoring and urgent intervention.
Keywords: Coronavirus, Cardiac complications, Cardiac imaging, Biochemical markers, Case series
Learning points
Physicians should maintain high clinical suspicion for cardiac complications from COVID-19 infection due to cytokine storm.
Physicians can utilize cardiac testing and monitoring to optimally manage cardiac manifestations of COVID-19.
Physicians should continue advocating for personal protective equipment to safely and effectively perform invasive cardiac interventions.
Introduction
The pandemic of novel coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been rapidly spreading worldwide, exhausting resources across health systems. First appearing in Wuhan, China, it commonly manifested with respiratory symptoms of cough, dyspnoea, fever, chills, and myalgias.1,2 Individuals with history of cardiovascular disease are predisposed to infection and are at increased risk of adverse outcomes.3 Previous beta-coronavirus infections, such as severe acute respiratory syndrome, were associated with tachyarrhythmias and heart failure.4 Cardiac manifestations of COVID-19 were later reported, typically from viral myocarditis and treatment side effects.5 Given the increased incidence and saturation of resources, COVID-19 has had indirect effects on care, impacting timing and optimal treatment of acute cardiovascular disease. The objective of this clinical case series is to highlight cardiac complications of COVID-19.
Timeline
| Day | Case 1 | Case 2 | Case 3 |
|---|---|---|---|
| 0 | Presented to ED with 1 week of dyspnoea on exertion, orthopnoea, and cough | Presented to the ED with fevers | Presented to the ED with diarrhoea, myalgias, and dyspnoea; subsequently intubated |
| 4–6 |
|
|
|
| 7–10 | Serial echocardiograms revealed resolution of effusion but new periapical wall motion hypokinesis, pericardial drain removed and discharged | Worsening respiratory and renal function; hypoxaemic pulseless electrical activity arrest and died | Developed septic shock with worsening respiratory failure leading to cardiopulmonary arrest and death |
| 21 | Echocardiogram demonstrated resolution of effusion and wall motion abnormalities |
Case presentation
Case 1
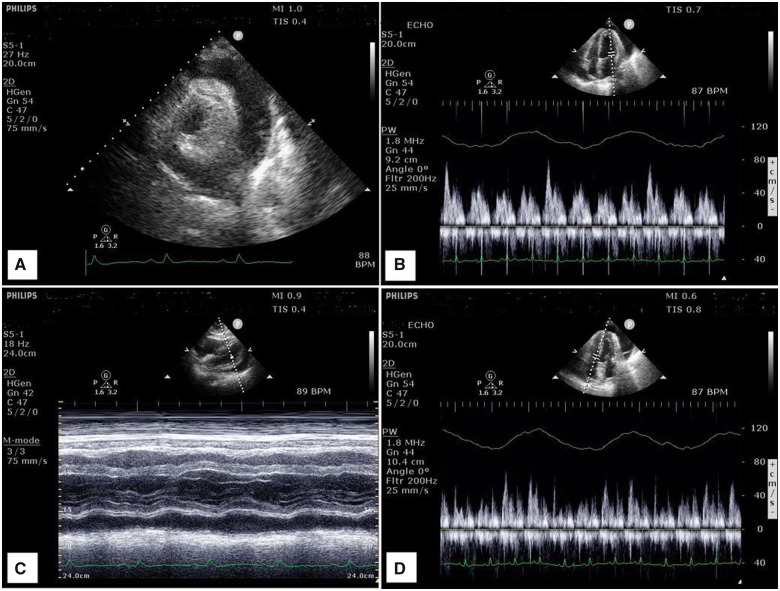
A 67-year-old Caucasian female with a history of non-ischaemic dilated cardiomyopathy with preserved ejection fraction (EF) 50%, hypertension, and known diagnosis of COVID-19 1 week previously, presented with progressive dyspnoea on exertion, orthopnoea, and productive cough. In the Emergency Department (ED), she was afebrile, tachycardic, and tachypnoeic with bilateral crackles on auscultation, and muffled heart sounds; no murmurs or palpable thrill were appreciated. She was noted to be lymphopenic at 0.9 × 103/μL (normal 1.0–4.8 × 103/μL) with elevated inflammatory markers including C-reactive protein of 15.1 mg/dL (normal <5.0 mg/dL), D-dimer 6.52 μg/mL FEU (normal <5.0 μg/mL), and ferritin 509 ng/mL (normal 12–300 ng/mL). High sensitivity troponin I (hs-cTnI) levels were initially 1865 ng/L (normal <19 ng/L) rising to a peak of 2410 ng/L after 24 h, with an associated brain natriuretic peptide (BNP) level of 54 pg/mL (normal <50 pg/mL). ECG showed normal sinus rhythm, QTc 427 ms. Chest radiograph (CXR) showed significant enlargement of the cardiac silhouette. Transthoracic echocardiogram (TTE) revealed a large pericardial effusion with early signs of right ventricular diastolic collapse and dilated inferior vena cava, as well as >25% and >40% reduction in mitral inflow and tricuspid inflow velocities, respectively, consistent with tamponade physiology (Figure 1).
Figure 1.
Four images captured from the transthoracic echocardiogram from Case 1. (A) The parasternal short axis with circumferential effusion. (B) Mitral inflow view, with >25% reduction in inflow velocity with respiration. (C) Subcostal view with M-mode highlighting the effusion with variation in myocardium during systole. (D) Tricuspid inflow view, with >40% reduction in inflow velocity with respiration.
She underwent pericardiocentesis and pericardial drain placement; fluid studies demonstrated elevated white blood cells (WBC) to 10 973 × 103/UL (normal 3.8–10.6 × 103/UL; 83% neutrophils, 14% lymphocytes) and elevated lactate dehydrogenase (LDH) at 1697 IU/L (normal 50–150 IU/L). She was initiated on colchicine 0.6 mg twice per day, hydrocortisone 100 mg twice per day, and hydroxychloroquine 200 mg twice per day. Serial TTEs during admission demonstrated new apical and periapical hypokinesis, with resolution of the effusion. Follow-up TTE 3 weeks post-discharge demonstrated resolution of the wall motion abnormalities with an EF of 63%.
Case 2
A 46-year-old African American male with a history of type 2 diabetes and obesity presented with persistent fevers. In the ED, he was febrile to 39.3°C and hypoxic, requiring supplemental oxygen; he subsequently decompensated due to acute hypoxic respiratory failure and required intubation. Physical examination further demonstrated tachypnoea and tachycardia, with diminished breath sounds bilaterally and normal S1 and S2 heart sounds; no murmurs or palpable thrill were appreciated. ECG obtained at the time of respiratory failure was normal, QTc 447 ms. He was lymphopenic at 0.6 × 103/μL (normal 1.0–4.8 × 103/μL) with normal hs-cTnI and BNP levels. CXR showed bilateral multifocal patchy opacities. SARS-CoV-2 testing was positive. He was initiated on azithromycin 500 mg daily, hydroxychloroquine 200 mg twice per day, and methylprednisolone 60 mg twice per day.6
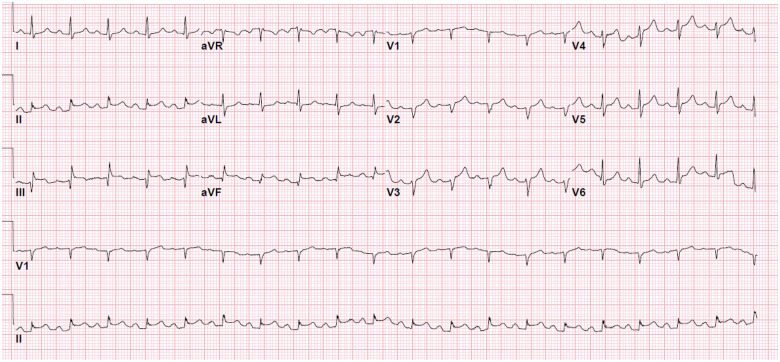
On day 6 of hospitalization, he had multiple episodes of non-sustained ventricular tachycardia followed by a wide complex tachycardia that generated into asystole. Return of spontaneous circulation was achieved after cardiopulmonary resuscitation; ECG demonstrated new ST elevations with PR depressions in the inferior leads and loss of early precordial R waves, with slight reciprocal ST segment depression in the high lateral lead aVL (Figure 2). Hs-cTnI peaked at 6639 ng/L (normal <19 ng/L) and D-dimer was >20 μg/mL (normal <5.0 μg/mL). He received aspirin 324 mg and was initiated on heparin infusion, without additional antiplatelet therapy. Due to haemodynamic instability, he was deemed too high risk for coronary angiography or thrombolytic therapy. Respiratory and renal function deteriorated, resulting in hypoxic pulseless electrical activity arrest and ultimately death.
Figure 2.
An ECG from Case 2. New ST elevations with PR depressions in the inferior leads and loss of early precordial R waves, with slight reciprocal ST segment depression in the high lateral lead aVL.
Case 3
A 76-year-old African American female with a history of obstructive sleep apnoea and hypertension presented to the ED with diarrhoea, myalgias, and shortness of breath. Upon arrival she was febrile (38.5°C) and hypoxaemic, and quickly decompensated requiring intubation. Physical examination demonstrated bilateral crackles with end-expiratory rhonchi, and systolic murmur along the left sternal border unchanged with respiration. Labs revealed lymphopenia at 0.5 × 103/μL (normal 1.0–4.8 × 103/μL) with normal BNP and hs-cTnI. C-reactive protein at 9.7 mg/dL (normal <5.0 mg/dL), ferritin at 921 ng/mL (normal 12–300 ng/mL), LDH at 334 IU/L (normal 50–150 IU/L), and creatinine phosphokinase (CPK) at 374 IU/L (normal 39–308 IU/L) were all elevated. Initial ECG showed normal sinus rhythm, QTc 387 ms. CXR showed bilateral patchy pulmonary opacities. She tested positive for SARS-CoV-2 and was started on hydroxychloroquine 200 mg twice per day and methylprednisolone 60 mg twice per day.6
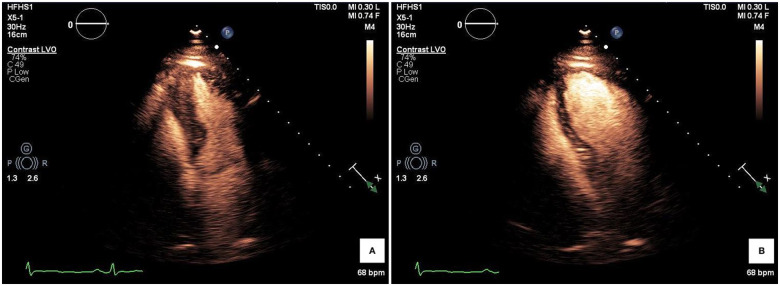
On day 4 of hospitalization, she developed sinus tachycardia and shock requiring norepinephrine infusion. She had an acute rise in hs-cTnI (650 ng/L), unchanged inflammatory markers (C-reactive protein of 6.0 mg/dL, ferritin 922 ng/mL, LDH of 349 IU/L, and CPK of 104 IU/L), and new early repolarization of lateral leads. TTE revealed a new reduced EF (40%) and severe hypokinesis of the basal–mid inferoseptal, inferior, anteroseptal, and anterior walls, suggestive of reverse Takotsubo morphology (Figure 3). Central venous oxygen saturation was decreased (55.5%), cardiac index (CI) was 1.9 L/min/m2. Due to her illness severity, coronary angiography was deferred, and she was empirically started on unfractionated heparin infusion. CI improved with pronation; thus, afterload reduction and inotropy were withheld. Troponin levels normalized, with serial ECGs demonstrating resolution of lateral lead changes, and her CI remained >2.5 L/min/m2. Unfortunately, her respiratory status worsened, leading to cardiopulmonary arrest and death.
Figure 3.
Two views from a transthoracic echocardiograph from Case 3. Highlighted in (A) is the ballooning of the basal segment during systole, with contrast to demarcate the epicardium. (B) Return of the apical segment during diastole.
Discussion
We present three cases with COVID-19 infection, each with unique cardiac complications (Table 1). Emerging evidence suggests a predilection of SARS-CoV-2 for the cardiovascular system, in some cases as prevalent as respiratory involvement.7,8 Studies have demonstrated use of the angiotensin-converting enzyme 2 (ACE2) protein by SARS-CoV-2, and similarly other coronaviruses, for cell entry.9 ACE2 serves as a lung protectant, explaining pulmonary involvement. Moreover, ACE2 is involved in the renin–angiotensin–aldosterone pathway, possibly explaining the increased prevalence of renal and cardiac complications. An additional pathophysiological explanation for the extent of cardiovascular involvement stems from the systemic inflammatory effects driven by the virus, predominantly through cytokine release and inflammatory cascade highlighted by serum biomarker elevation.3 Other highly pathogenic coronavirus strains have shown correlative evidence to have cytokine storms leading to deleterious clinical manifestations.10
Table 1.
Summary of all three cases
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Prior to admission | Non-ischaemic cardiomyopathy and hypertension who tested positive COVID 1 week prior to presenting with dyspnoea on exertion, orthopnoea, and cough | Type 2 diabetes and obesity presenting with persistent fevers | Obstructive sleep apnoea and hypertension presented with diarrhoea, myalgias, and dyspnoea |
| Early hospital course | Febrile, tachycardic, tachypnoeic | Febrile, tachypnoeic, hypoxemic. Day 6 went into hypoxic cardiac arrest and was intubated | Febrile, hypoxoemic ultimately requiring intubation. Day 4 tachycardic and in shock with reduced cardiac index (1.9 L/min/m2) |
| Labs | Lymphopenic, elevated troponin, normal BNP. Pericardial fluid consistent with viral aetiology | Lymphopenic, acute troponin and D-dimer elevation compared with normal on admission | Lymphopenic; elevated CRP, ferritin, LDH, and CPK levels; acute troponin elevation compared wuth normal on admission |
| ECG | Normal sinus rhythm | New ST elevations with PR depressions in the inferior leads and loss of early precordial R waves, no reciprocal ST depressions | New early repolarization of lateral leads |
| Cardiac imaging | Echo revealed large pericardial effusion with signs of right ventricular dysfunction and apical hypokinesis | Unable to obtain due to COVID-19 infection and severity of illness | Echo revealed new reduced ejection fraction with basilar wall motion hypokinesis |
| Intervention | Pericardiocentesis with pericardial drain. Colchicine, hydrocortisone, and hydroxychloroquine started | Aspirin 324 mg and low intensity heparin infusion; azithromycin, hydroxychloroquine, and methylprednisolone | Paralysis and proning with improved cardiac index; hydroxychloroquine, methylprednisolone, low intensity heparin infusion |
| Outcome | Recovered, follow-up echo showed resolution of effusion and hypokinesis | Respiratory and renal failure progressed and patient expired | Patient developed septic shock with worsening respiratory failure and expired |
In the first case of this series, we witnessed elevation in inflammatory markers and imaging consistent with pericarditis complicated by pericardial effusion in the setting of COVID-19. Pericardiocentesis fluid analysis was consistent with viral aetiology, and she was optimally managed with drainage and adjuvant hydrocortisone and colchicine, as well as treatment of COVID-19 with hydroxychloroquine. Approximately 80–90% of pericarditis cases are idiopathic or caused by viruses, which can be further complicated by pericardial effusion.11 In the current COVID-19 pandemic, there have been two documented reports of pericardial effusions and one developing cardiac tamponade.12 A review of 90 COVID-19 patients revealed one with pericardial effusion.13 Further large-scale investigations into COVID-19-induced pericarditis and the role of the cytokine storm are needed to make definitive recommendations for treatment.
The increased stress from acute, severe illness can also lead to an excess catecholamine release resulting in stress-induced cardiomyopathy. The catecholamine excess, along with the increased catecholamine receptors located on the cardiac apex, typically results in the stunting of the apical portion of the heart.14 As witnessed in the first and third case, we see troponin level elevations with wall motion abnormalities consistent with stress cardiomyopathy. In our first case, initial echocardiography with apical wall motion hypokinesis, paired with improved troponin levels with no coronary intervention and resolution of focal wall motion abnormalities on 3-week follow-up TTE, is suggestive of Takotsubo cardiomyopathy in the setting of COVID-19. Similarly demonstrated in Case 3, we saw acute troponin elevation and basilar wall motion abnormalities on echocardiography. Also similar to Case 1, the acute cardiac decompensation stabilized without coronary intervention, highlighted by improvement in the CI and resolution of ECG changes, thus all together suggestive of reverse Takotsubo cardiomyopathy, a phenomenon ranging in prevalence from 1% to 25% of stress cardiomyopathies.14
Observational trends have shown severe cases of COVID-19 developing coagulopathies, as seen with abnormal D-dimer and inflammatory markers, raising the suspicion for microemboli or cytokine storm that can potentially result in myocardial infarction.3,9 The second case was concerning for acute coronary syndrome secondary to microemboli from a known hypercoagulable state. Given the development of ventricular tachycardia, a new rise in troponin with corresponding ST elevation on ECG, and new D-dimer elevation, suspicion for an acute myocardial infarction secondary to microemboli remains high on the differential. Given our patient’s underlying comorbidities of type 2 diabetes and obesity, underlying coronary artery disease cannot be ruled out; however, our patient was deemed too unstable for cardiac catheterization. Furthermore, the patient was scheduled to undergo TTE to assess for regional wall motion abnormalities; however, he unfortunately succumbed to the disease prior to obtaining echocardiogram.
We faced issues with limited resources during the time in which we cared for these patients. There were external factors, such as the national shortages of personal protective equipment, that prevented us from conducting further studies, such as coronary angiography and echocardiography. Coronary angiography would have assisted with assessing the wall motion abnormalities seen in Cases 1 and 3; however, we were able to confidently diagnose them with stress cardiomyopathy as described above. Similarly, in Case 2, we were unable to obtain a TTE to further characterize any cardiac wall motion abnormalities, but he ultimately succumbed to respiratory failure.
Conclusion
Although COVID-19 has a predilection for causing respiratory illness, there are a growing number of cardiac manifestations. This report displays those complications, with a strong link to cytokine storm, and the use of cardiac monitoring and imaging in managing such cases. It also highlights the indirect effects the pandemic has had on timing and utility of care. Gaining a better understanding regarding the systemic effects of COVID-19 infection will lead to improved management of such complications.
Lead author biography

Zachary Dean Demertzis is a second-year resident physician in training. He completed his medical school at Midwestern University–Chicago College of Osteopathic Medicine and is completing his internal medicine training at Henry Ford Hospital in Detroit, Michigan. He aspires to complete a fellowship in cardiology and continue being a learner and teacher of medical education.
Supplementary Material
Acknowledgements
We would like to thank Drs Pallavi Bhargava, Mohammed Dabbagh, Penny L. D’Souza, and Alexander Michaels for their assistance in the care of our patients and reviewing of images.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient or next of kin in line with COPE guidance.
Conflict of interest: All authors have no conflicts of interests or disclosures to report.
References
- 1.Pneumonia of unknown cause—China. World Health Organization. 2020. https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/. (30 March 2020).
- 2.Novel coronavirus—China. World Health Organization. 2020. https://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/. (30 March 2020).
- 3. Driggin E, Madhaven MV, Bikdeli B, Chuich T, Laracy J, Bondi-Zoccai G, Brown TS, Der Nigoghossian C, Zidar DA, Haythe J, Brodie D, Beckman JA, Kirtane AJ, Stone GW, Krumholz HM, Parikh SA.. Cardiovascular considerations for patients, health care workers, and health systems during the Coronavirus Disease 2019 (COVID-19) pandemic. J Am Coll Cardiol 2020;doi:10.1016/j.jacc.2020.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yu CM, Wong RS, Wu EB, Kong SL, Yip GWK, Soo YOY, Chiu MLS, Chan YS, Hui D, Lee N, Wu A, Leung CB, Sung JJY.. Cardiovascular complications of severe acute respiratory syndrome. Postgrad Med J 2006;82:140–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zeng JH, Liu Y, Yuan J, Wang F, Wu W, Li J, Wang L, Gao H, Wang Y, Dong C, Li Y, Xie X, Feng C, Liu L.. First case of COVID-19 infection with fulminant myocarditis complication: case report and insights. Infection 2020; doi: 10.1007/s15010-020-01424-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, Mailhe M, Doudier B, Courjon J, Giordanengo V, Vieira VE, Dupont HT, Honore S, Colson P, Chabriere E, La Scola B, Rolain JM, Brouqui P, Raoult D.. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents 2020; doi:10.1016/j.ijantimicag.2020.105949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zheng YY, Ma YT, Zhang JY, Xie X.. COVID-19 and the cardiovascular system. Nat Rev Cardiol 2020;17:259–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z.. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;323:1061–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Clerkin KJ, Fried JA, Raikhelkar J, Sayer G, Griffin JM, Masoumi A, Jain SS, Burkhoff D, Kumaraiah D, Rabbani L, Schwartz A, Uriel N.. COVID-19 and cardiovascular disease. Circulation 2020;141:1648–1655. [DOI] [PubMed] [Google Scholar]
- 10. Channappanavar R, Perlman S.. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol 2017;39:529–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Imazio M, Gaita F, LeWinter M.. Evaluation and treatment of pericarditis: a systematic review. JAMA 2015;314:1498–1506. [DOI] [PubMed] [Google Scholar]
- 12. Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, Cani DS, Cerini M, Farina D, Gavazzi E, Maroldi R, Adamo M, Ammirati E, Sinagra G, Lombardi CM, Metra M.. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020; doi:10.1001/jamacardio.2020.1096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Xu X, Yu C, Qu J, Zhang L, Jiang S, Huang D, Chen B, Zhang Z, Guan W, Ling Z, Jiang R, Hu T, Ding Y, Lin L, Gan Q, Luo L, Tang X, Liu J.. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging 2020;47:1275–1280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Awad HH, McNeal AR, Goyal H.. Reverse Takotsubo cardiomyopathy: a comprehensive review. Ann Transl Med 2018;6:460. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.