Abstract
Objective
To utilize evidence-based medicine to help determine guidelines for spinal surgery during the Covid-19 era.
Methods
A literature review was performed of peer-reviewed articles focused on indications for common procedures in spine surgery. Based on these indications, we sub-categorized these procedures into elective, urgent and emergent categories. Case examples provided.
Results
Indications for spinal surgery were reviewed based on current literature and categorized. This manuscript presents a decision-making algorithm to help provide a guideline for determining the appropriateness of proceeding with spinal surgery during this COVID-19 time period.
Conclusions
Spinal surgery during the COVID-19 pandemic is an intricate challenging decision-making process, involving clinical, sociologic and economic factors.
Keywords: COVID-19, Coronavirus, Pandemic, Spinal surgery, Spine, Infectious disease
1. Introduction
Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS-CoV-2) is a virus currently affecting the majority of the world in a global pandemic fashion, more commonly known as COVID-191. The virus was recognized as a potential danger in December of 2019, when there were a series of pneumonia cases reported in Wuhan, China.1 As death tolls due to pneumonia rose within the city of Wuhan, preliminary etiological research was carried out to better understand the virus and its potential risk to society. Research performed by Ji et al.2 elucidated that the SARS-CoV-2 virus was a chimeric version of a known bat coronavirus, which differed from previous strains of SARS and Middle East Respiratory Syndrome (MERS) coronaviruses, more specifically belonging to the subgenus botulinium of Coronaviridae.2,3 Benvenuto et al.4 recognized that this virus was similar to a strain that had been isolated in 2015 from Chinese chrysanthemum-headed bats.4 This established the preliminary thoughts that the virus had derived from bats and was ultimately transferred to humans. Support for this theory was further reinforced by multiple studies after sequence homology between SARS-CoV-2 and bat coronaviruses were found to be highly homologous.1,5,6
Some of the presenting symptoms of COVID-19 patients typically complain of respiratory symptoms. Zhao et al.7 recognized that the receptor for the virus was the same as that of angiotensin-converting enzyme 2 (ACE2).7 ACE2 is expressed in the normal alveolar epithelial cells of the lungs. The binding of the COVID-19 virus on the ACE2 receptors can cause a heightened expression of ACE2, ultimately leading to damage to alveolar cells within the lung and the common presentation of shortness of breath. As a result, the damaged alveolar cells can trigger a systemic response within the lungs, leading to more severe systemic reactions.7 Additional studies revealed that 98% of patients had a fever, of which, 78% had a fever greater than 38° Celsius8 Other common complaints in patients with COVID-19 coronavirus are coughs, dyspnea, muscle pain, fatigue, fevers, and chills. Patients primarily at risk for death are those that are elderly, immunocompromised, and have chronic medical comorbidities, such as heart conditions, chronic kidney disease, liver disease, chronic lung disease, diabetes, and obesity.9,10
To date, there are no effective vaccines or medical treatment that has been developed to mitigate the spread of the virus.1 As a result, strategies have been developed to recognize symptoms and attempt to limit spread. Early diagnosis, reporting, and isolation from others have been initiated in a global effort to minimize overall spread. Regardless of the efforts by nations to initiate isolation techniques to “flatten the curve” of coronavirus cases, the virus has continued to spread and overwhelm hospital systems around the world. Within the United States, large cities such as New York City, Chicago, and Seattle have been hit particularly hard and found to be short of critical care resources—though other cities around the United States anticipate a rise in cases over the next few weeks.11
As a result, multiple states have issued executive orders prohibiting elective surgery in order to conserve resources for the growing pandemic. For example, in Texas, Governor Greg Abbott issued an executive order stating, “all licensed health care professions and all licensed health care facilities shall postpone all surgeries and procedures that are not immediately medically necessary…”.12 The Texas Medical Board has released a press release echoing Governor Abbott’s executive order and has approved an emergency rule to allow the Board to react swiftly, through temporary license suspension, if providers are found violating the executive order.13 Along similar lines, the United States Surgeon General Jerome Adams recommended that providers “consider stopping elective surgeries” until the coronavirus threat subsides.14 Given these mandates, this necessarily includes restriction on spine surgery, however, there is likely to be controversy, as to the level of urgency. Spinal surgery is unique, in that, even elective procedures are typically done for neurological symptoms and deficits with compression of neural elements. This makes the term elective more difficult to elucidate. The purpose of this article is to review the literature for varying indications for spine surgery, and help categorize elective, urgent, emergent nature of these indications, in order to give spine surgeons a general framework and guidance of the risks and benefits of proceeding with surgery versus delaying surgery in the setting of COVID-19 pandemic.
2. Emergent spinal surgery
Neurological compromise dictates the urgency of the procedure. As stated, patients with “progressive or severe neurologic deficits due to neurologic compression from any cause (infection, tumor, fracture, disc herniation) warrants surgical intervention without postponing treatment.15 Given the catastrophic nature of spinal cord injuries, resulting in motor, sensory, or autonomic deficits, timely intervention is paramount. Furlan et al recommends that early surgical intervention, when safe and feasible, can improve clinical outcomes and reduce overall health care costs.16 Furlan et al. additionally recommended that early surgical intervention should be considered in all patients, in 8-24 hours, that develop an acute traumatic spinal cord injury.16 This is the generally accepted treatment protocol for spinal cord injury in the United States and should be continued during the current crisis.16, 17, 18 Cord compression from infection, tumor, fracture, or disc herniation warrants surgical decompression of the spinal cord in addition to potential realignment and stabilization. Similarly, epidural abscesses causing neurologic deficits warrants emergent surgical intervention. Though the pathogenesis of epidural infection leading to neurological deficits remains somewhat controversial, with direct compression and vascular occlusion by septic thrombophlebitis both as potential causes of pathology, both likely contribute to the notoriously unpredictable clinical course and need for expeditious surgical intervention.19, 20, 21, 22, 23 Multiple large series have noted that if spinal epidural abscess patients have progressed to complete paralysis for more than 24-48 hours, than the likelihood of recovery is significantly diminished.19, 24, 25, 26, 27, 28 Finally, postoperative wound infections warrant an emergent surgical intervention. Spinal infections may lead to constitutional symptoms such as fever/chills, and progress to a severe infection with hypotension, confusion, lethargy, and an overall septic clinical picture. Such a presentation immediately warrants intervention and is an absolute indication for emergent irrigation and debridement to prevent further deterioration of the patient.29, 30 For reasons similar to acute spine trauma, acute cauda equina syndrome leading to progressive neurological deterioration requires emergent surgical intervention during the COVID-19 era.31 Understanding the financial and economic burden of spinal cord injuries, these acute spinal cord injuries must be dealt with acutely and efficiently.32, 33 Spinal cord injuries are costly on the healthcare system with costs estimated to be $9.7 billion annually.32, 33 If left untreated, these injuries would likely further tax the currently strained healthcare system, particularly during COVID-19 pandemic.32
3. Urgent spinal surgery
Cervical or thoracic myelopathy with recent progression should be treated on an “urgent” basis.15 Others have even recommended that these conditions be considered emergent during the COVID-19 era.31 The natural history of cervical spondylotic myelopathy is extremely variable, with some patients deteriorating and needing surgery, while others can be followed for years without necessitating surgical intervention.34, 35 In the COVID-19 era, patients that present with the pattern of rapid deterioration meet the urgent/emergent need for surgical intervention.15, 31 The exact timing of surgical intervention for myelopathy has not been clearly discerned, though timely surgical intervention is likely to produce an improved outcome.34, 36 Intractable pain from cervical or lumbar radiculopathy, or progressive fracture related deformity that elicits presentation to the ED and consumption of increased narcotic use should be considered for surgery on a urgent basis. Donnally et al described that acute instrumentation failure, such as screw loosening, pull out, rod fracture, or cage migration should be operated on urgently as well.31, 37 Spinal infections, such as discitis, osteomyelitis and that fail to respond to medical management should be considered for surgery, as discitis and osteomyelitis may progress into the formation of a compressing spinal epidural abscess or delayed spinal deformity.38, 39 If medically feasible and safe, patients may benefit from surgical intervention at ambulatory surgical center (ASC) or surgical hospital, as COVID-19 census is likely to be higher at larger hospital facility.31
4. Elective spinal surgery
Spinal conditions where pain and dysfunction can be reasonably managed utilizing conservative management should be done so during the COVID-19 era. Particularly, chronic conditions, degenerative spinal disorders, spinal stenosis or spondylolisthesis without neurologic deficit, and symptomatic implants can all be reasonably managed in an elective fashion.15 While a complete list of spinal conditions is not feasible, stable fractures without progressive deformity or neurological compromise, stable pseudoarthosis without concern for hardware failure, spinal deformity, spinal stenosis without progressive neurological deterioration, and stable proximal junctional kyphosis or other adjacent level degenerative conditions, should all be managed whenever possible with conservative treatment until resources being utilized to combat the COVID-19 pandemic allow. Compression fractures and odontoid fractures are generally fractures of the elderly, and though have a significant effect on patients, can reliably be managed non-operatively symptomatic control and bracing.40, 41 These patients are the highest risk for deteriorating due to COVID-19, therefore, minimizing their exposure to the hospital setting is of vital importance during this time period.9, 10 Though surgical treatment of axial back pain is controversial, no long term outcome typically results from delay in surgery, it is recommended in these patients to continue conservative management whenever possible.40, 42, 43, 44, 45
5. Hospital management of the operative patient in the COVID-19 pandemic
Patients with spinal pathology are often times immobile or have limited mobility due to their spinal disorder. As a result, their prolonged bed rest may exacerbate many of their underlying medical comorbidities and making them more susceptible to urinary tract infections, deep vein thrombosis, and pneumonia.46 This heightened risk, in combination with the propensity for COVID-19 to affect the lungs, makes spinal patients more susceptible to COVID-19 pulmonary infections.47, 48 Screening of symptomatic patients will continue to be of critical importance in the outpatient and the emergency setting while caring for spine patients during this pandemic crisis.
Providers who care for spine patients should adhere to the strict guidelines proposed and updated by the CDC in use of personal protective equipment (PPE) for the safety of themselves and the patient. Medical staff should utilize N95 masks, eye protection, disposable caps, disposable gloves, disposable shoe covers, and protective clothing.47, 49 All providers in the clinical setting should strictly uphold distancing from patients whenever feasible along with facemasks for both the patient and provider.
If a COVID-19 negative patient requires surgery, intervention at an ambulatory surgery center (ASC) or facility with minimal COVID census is recommended. If a larger instituion, currently caring for COVID patients, is needed for surgery, the patient should be hospitalized in a separate unit—used only for noninfected patients. Limited, or no, visitors to the hospital may help minimize traffic within the unit and assist with maintaining an uninfected unit. If the patient develops symptoms consistent with COVID-19 infection, they should be tested, and transferred to a separate ward more pertinent to patients with COVID-19 infection for further work-up.47
Patients with known, or suspected, COVID-19 infection should be treated with more caution. In this scenario, Zou et al. recommends exhaustion of conservative measures prior to intervening surgically.47 In the scenario of emergent intervention needed for a positive COVID-19 patient, reducing operative time and exposure for all staff is paramount. Zou et al. recommends (1) the use of minimally invasive surgery and reduced operative time, (2) prone positioning when able to reduce viral transition via respiratory droplets (3) minimize intraoperative body fluid spatter and gentle surgical techniques to minimize spread of patient's body fluids (4) Utilize suction devices, intra-operatively, with caution to reduce aerosol diffusion (5) No staff is to enter or leave the operating room during procedure (6) Operative staff should undergo any necessary COVID-19 testing and should undergo isolation if they develop suspicious symptoms.47
6. COVID-19 algorithm for spine surgery
Hospital administration may also consider establishing a multi-disciplinary committee involving hospital administration, members of the ethics committee, pastoral care, care coordination/social worker, and chosen representatives of the medical staff including heads of surgical subspecialists. The committee can review data available for individual hospital resources and work with section heads to help prioritize surgical cases. The committee will need to consider each case in regards to available hospital resources including current incidence of Covid-19, need for post-operative ICU care, bed availability, blood transfusion needs, post-operative rehabilitation needs, and other factors.
Based on the available literature, the authors have adopted an algorithm for determining the surgical urgency of spine surgery during COVID-19 pandemic (Fig. 1). The intention of this algorithm is not to encompass all diagnoses and conditions a surgeon may encounter, but provide general guidelines that may assist a multi-disciplinary committee. If the patient necessitates surgery, the next step is to consider the emergent versus urgent versus elective nature of the procedure. If deemed emergent, proceeding with immediate surgery is recommended.
Fig. 1.
Decision-making algorithm for determining urgency of spinal surgery during the COVID-19 Pandemic.
For urgent indications, the identifiable risk factors that might portend a worse outcome in the setting of the setting of the COVID-19 infection should be recognized and weighed against the need for surgery. If the patient's individual COVID-19 risk is greater than the risk of delaying surgery, than the procedure should be delayed. In contrast, if the patient's surgical pathology outweighs the risk of COVID-19 exposure, than surgery should proceed cautiously.
Case Examples (All cases submitted, evaluated, and approved by multi-disciplinary peer-review panel at our institution).
Case 1
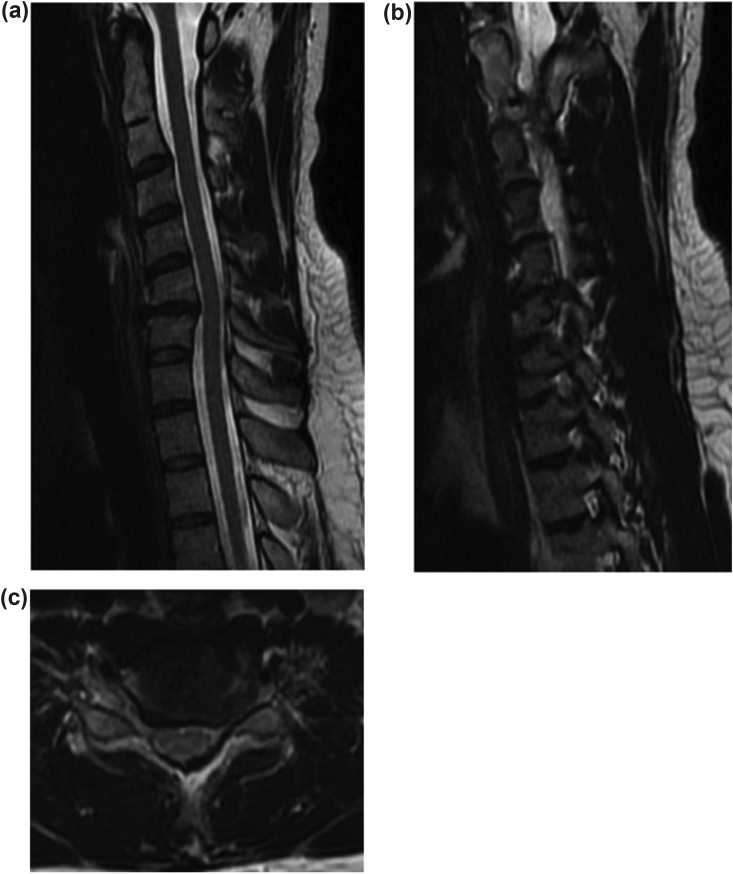
Patient is a 39-year-old male who presents with severe neck and left upper extremity pain. He states that his pain his mainly in his neck but radiates down his left arm with the severity of an 8–10/10 on the pain scale. He was seen in the office and trialed on oral medication and oral steroids. On physical examination, he had a positive left sided Spurling's sign with very limited range of motion. He had some weakness evident in his left upper extremity with a 4-/5 triceps, wrist flexion and extension, as well as 4-/5 finger extensors. He complained of numbness in the C7 nerve distribution. XR and MRI were obtained. MRI revealed a large, left C6-7 herniated nucleus pulposis, with kyphosis, and a congenital C2/3 fusion (Fig. 2a–c). At this time, we attempted conservative measures utilizing physical therapy and epidural steroid injection. He was seen seven weeks later in the office with worsened numbness and worsening weakness of left finger extensors, with continued intractable pain. At this time, we felt this was an urgent, rather than emergent, indication for surgery. It was determined that delay of this surgery would result in further neurological deterioration, potentially causing irreversible neurological damage if delayed. The patient subsequently underwent an uncomplicated C6/7 Anterior Cervical Discectomy and Fusion (ACDF). The patient tolerated the procedure well with immediate improvement in symptoms and significant neurological improvement. The patient was discharged home on same day of surgery, 8 h post-operatively.
Case 2
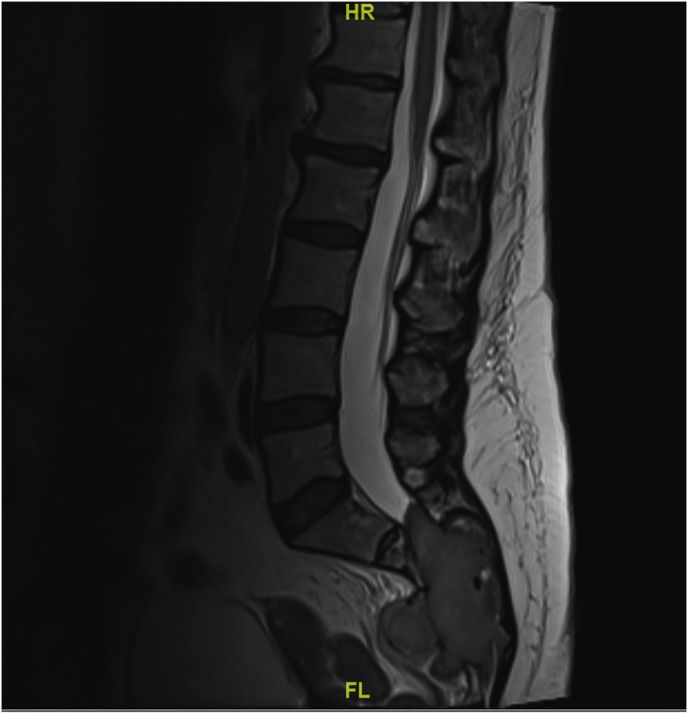
56-year-old female presents in the outpatient clinic setting with persistent low back pain radiating down her bilateral buttock and legs with numbness and paresthesias. Her VAS leg pain was a 10/10 on the left and an 8/10 on the right. Her symptoms started approximately 3 months ago, with progressive worsening without an inciting event. Pain increased at night and with ambulation. She denies any bowel or bladder incontinence or retention but does report saddle anesthesia. Normal motor exam, decreased sensation to pinprick bilateral lower extremity. MRI (Fig. 3) and CT scan (Fig. 4) were ordered to better evaluate the pathology revealing a large destructive mass of the sacrum with obliteration of the spinal canal and severe compression of the thecal sac. Patient underwent oncology referral, staging studies including MRI of the cervical and thoracic spine and IR guided biopsy with close observation of her neurological status. Pathology showed giant cell tumor of bone. Patient had consultations with hematology oncology, radiation oncology and orthopedic oncology in an expedited fashion. After multi-disciplinary discussion surgical options were discussed with patient including risk, benefits, morbidity and recurrence rate associated with attempted enbloc resection versus preoperative embolization, intralesional resection of tumor with adjunct intraoperative thermal ablation with post operative adjunct radiation. Given the complexity of the procedure, surgery was performed at a larger academic hospital setting with ICU resources. Case was submitted to a multidisciplinary peer-review panel at our institution and was approved to proceed with surgery in an urgent fashion. Patient underwent preoperative embolization one day prior to surgery. A L5-S4 sacral laminectomy and L4 to pelvis fusion was performed (Fig. 5) with intraoperative thermal ablation. The patient tolerated the procedure well without complication, was admitted to a regular floor bed post-operatively. Patient had resolution of her preoperative radicular symptoms, maintained neurological function, preserved bowel and bladder function and was discharged home on post-operative day five in stable condition.
Fig. 2.
T2 weighted sagittal MRI of the cervical spine revealing degenerative changes and disc space narrowing at C6/7 with moderate disc osteophyte complexes contributing to a moderate degree of central canal stenosis b) Sagittal MRI cut through Entry zone of the left cervical foramen with severe left neuroforaminal stenosis c) Axial MRI cut through the C6– C7 Disc space revealing left sided foraminal stenosis.
Fig. 3.
T2 weighted sagittal MRI of the lumbar spine revealing a large multilobulated destructive mass of the sacrum measuring approximately 8.1 cm in craniocaudal dimension and 8.7 x 3.2 cm transverse dimensions with presacral extension. Obliteration of the spinal canal at the involved levels with significant mass affect contouring the thecal sac S1-2.
Fig. 4.
CT scan shows large expansile lytic destructive mass of the sacrum with lobular extension into the presacral soft tissues.
Fig. 5.

Three month follow-up AP radiograph of the pelvis revealing post operative decompression and lumbopelvic posterior instrumentation from L4-S1.
7. Conclusion
This is an unprecedented time for health care and spinal surgery across the United States of America. The restriction of spinal surgery during this pandemic will require multiple parties to assist in the care of these patients and aid in the decision-making process. The authors of this manuscript recommend that those decisions are best made at a local hospital level in coordination with a committee of one’s surgical peers that utilizes a multidisciplinary panel. Spine patients that present with emergent and urgent conditions will require a more expeditious intervention to minimize future harm and prevention of neurological deterioration. The decision to proceed with urgent, or emergent, spinal surgery during the COVID-19 pandemic must also be analyzed in the context of local conditions and resources. The goal of this paper was to outline a general guide and provide some case examples that may help assist with the triaging of spinal surgery patients during the covid19 era. With the anticipation of multiple waves of cases, their will be a continued need for prioritization of spinal surgery cases. Surgeons need to remain conscientious about local hospital resources, divert surgeries to an outpatient setting whenever feasible, and assist local multi-disciplinary hospital committees in case-by-case decision making in this ever changing environment.
References
- 1.Sun P., Lu X., Xu C. Understanding of COVID-19 based on current evidence. J Med Virol. 2020 doi: 10.1002/jmv.25722. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ji W., Wang W., Zhao X. Homologous recombination within the spike glycoprotein of the newly identified coronavirus may boost cross‐species transmission from snake to human. J Med Virol. 2020 doi: 10.1002/jmv.25682. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China. N Engl J Med. 2019 doi: 10.1056/NEJMoa2001017. Epub ahead of print 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benvenuto D., Giovanetti M., Ciccozzi A. The 2019-new coronavirus epidemic: evidence for virus evolution. J Med Virol. 2020 doi: 10.1002/jmv.25688. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhou P., Lou Yang X., Wang X.G. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020 doi: 10.1038/s41586-020-2012-7. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu F., Zhao S., Yu B. A new coronavirus associated with human respiratory disease in China. Nature. 2020 doi: 10.1038/s41586-020-2008-3. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhao Y., Zhao Z., Wang Y. bioRxiv; 2020. Single-cell RNA Expression Profiling of ACE2, the Putative Receptor of Wuhan 2019-nCov. Epub ahead of print. [DOI] [Google Scholar]
- 8.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 doi: 10.1016/S0140-6736(20)30183-5. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li Q., Guan X., Wu P. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020 doi: 10.1056/nejmoa2001316. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.U.S Department of Health. No Title. Coronavirus Disease 2019 (COVID-19).
- 11.Sommer P., Lukovic E., Fagley E. Initial clinical impressions of the critical care of COVID-19 patients in Seattle, New York city, and Chicago. Anesthsia Analg. 2020 doi: 10.1213/ANE.0000000000004830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.K P. Health Care Professionals and Facilities, Including Abor‐tion Providers, Must Immediately Stop All Medically Unnecessary Surgeries and Procedures to Preserve Resources to Fight COVID-19 Pandemic. Ken Paxton Press Release.
- 13.Zaafran S. 2020. TMB Passes Emergency Rules to Enforce Gov. Abbott's Executive Order GA-09. Austin, TX. [Google Scholar]
- 14.J C. SURGEON GENERAL URGES PROVIDERS TO “CONSIDER STOPPING ELECTIVE SURGERIES.” HOSPITALS PUSH BACK. HealthLeaders.
- 15.Bono C, Dohring E, Finkenberg J, et al. NASS Guidance Document on Elective, Emergent and Urgent Procedures. North American Spine Society.
- 16.Furlan J.C., Noonan V., Cadotte D.W. Timing of decompressive surgery of spinal cord after traumatic spinal cord injury: an evidence-based examination of pre-clinical and clinical studies. J Neurotrauma. 2011 doi: 10.1089/neu.2009.1147. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fehlings M.G., Vaccaro A., Wilson J.R. Early versus delayed decompression for traumatic cervical spinal cord injury: results of the surgical timing in acute spinal cord injury study (STASCIS) PLoS One. 2012 doi: 10.1371/journal.pone.0032037. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wilson J.R., Singh A., Craven C. Early versus late surgery for traumatic spinal cord injury: the results of a prospective Canadian cohort study. Spinal Cord. 2012 doi: 10.1038/sc.2012.59. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 19.Tuchman A., Pham M., Hsieh P.C. The indications and timing for operative management of spinal epidural abscess: literature review and treatment algorithm. Neurosurg Focus. 2014 doi: 10.3171/2014.6.FOCUS14261. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 20.Danner R.L., Hartman B.J. Update on spinal epidural abscess: 35 cases and review of the literature. Rev Infect Dis. 1987 doi: 10.1093/clinids/9.2.265. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 21.Darouiche R.O., Hamill R.J., Greenberg S.B. Bacterial spinal epidural abscess: review of 43 cases and literature survey. Medicine (U. S.) 1992 doi: 10.1097/00005792-199211000-00004. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 22.Darouiche R.O. Spinal epidural abscess. N Engl J Med. 2006 doi: 10.1056/NEJMra055111. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 23.Heusner A.P. Nontuberculous spinal epidural infections. N Engl J Med. 1948 doi: 10.1056/NEJM194812022392301. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 24.Rigamonti D., Liem L., Sampath P. Spinal epidural abscess: contemporary trends in etiology, evaluation, and management. Surg Neurol. 1999 doi: 10.1016/S0090-3019(99)00055-5. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 25.Feldenzer J.A., McKeever P.E., Schaberg D.R. Experimental spinal epidural abscess: a pathophysiological model in the rabbit. Neurosurgery. 1987 doi: 10.1227/00006123-198706000-00007. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 26.Feldenzer J.A., McKeever P.E., Schaberg D.R. The pathogenesis of spinal epidural abscess: microangiographic studies in an experimental model. J Neurosurg. 1988 doi: 10.3171/jns.1988.69.1.0110. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 27.Browder J., Meyers R. Pyogenic infections of the spinal epidural space. a consideration of the anatomic and physiologic pathology. Surgery. 1941 doi: 10.5555/uri:pii:S0039606041901447. Epub ahead of print. [DOI] [Google Scholar]
- 28.Russell N.A., Vaughan R., Morley T.P. Spinal epidural infection. Can J Neurol Sci/J Can Sci Neurol. 1979 doi: 10.1017/S0317167100023957. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 29.Meredith D.S., Kepler C.K., Huang R.C. Postoperative infections of the lumbar spine: presentation and management. Int Orthop. 2012 doi: 10.1007/s00264-011-1427-z. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hegde V, Meredith DS, Huang RC, et al. Management of postoperative spinal infections. World J Orthop. Epub ahead of print 2012. DOI: 10.5312/wjo.v3.i11.182. [DOI] [PMC free article] [PubMed]
- 31.Donnally C., III, Shenoy K., Vaccaro A. Triaging spine surgery in the COVID-19 era. Clin Spine Surg. 2020;33:129–130. doi: 10.1097/BSD.0000000000000988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.French D.D., Campbell R.R., Sabharwal S. Health care costs for patients with chronic spinal cord injury in the veterans health administration. J Spinal Cord Med. 2007 doi: 10.1080/10790268.2007.11754581. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Berkowitz M., O'Leary P., Kruse D. Demos Medical Publishing; New York: 1998. Spinal Cord Injury: An Analysis of Medical and Social Costs. [Google Scholar]
- 34.Kong L De, Meng L.C., Wang L.F. Evaluation of conservative treatment and timing of surgical intervention for mild forms of cervical spondylotic myelopathy. Exp Ther Med. 2013 doi: 10.3892/etm.2013.1224. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ghogawala Z., Benzel E.C., Riew K.D. Surgery vs conservative care for cervical spondylotic myelopathy: surgery is appropriate for progressive myelopathy. Neurosurgery. 2015 doi: 10.1227/NEU.0000000000000781. Epub ahead of print 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kadaňka Z., Bednařík J., Voháňka S. Conservative treatment versus surgery in spondylotic cervical myelopathy: a prospective randomised study. Eur Spine J. 2000 doi: 10.1007/s005860000132. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oppenlander M.E., Hsu F.D., Bolton P. Catastrophic neurological complications of emergent endotracheal intubation: report of 2 cases. J Neurosurg Spine. 2015 doi: 10.3171/2014.10.SPINE14652. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 38.Devkota P., Krishnakumar R., Renjith Kumar J. Surgical management of pyogenic discitis of lumbar region. Asian Spine J. 2014 doi: 10.4184/asj.2014.8.2.177. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chao D., Nanda A. Spinal epidural abscess: a diagnostic challenge. Am Fam Physician. 2002;65:1341–1346. [PubMed] [Google Scholar]
- 40.Wong C.C., McGirt M.J. Vertebral compression fractures: a review of current management and multimodal therapy. J Multidiscip Healthc. 2013 doi: 10.2147/JMDH.S31659. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Iyer S., Hurlbert R.J., Albert T.J. Management of odontoid fractures in the elderly: a review of the literature and an evidence-based treatment algorithm. Clin Neurosurg. 2018 doi: 10.1093/neuros/nyx546. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 42.Hooten W.M., Cohen S.P. Evaluation and treatment of low back pain: a clinically focused review for primary care specialists. Mayo Clin Proc. 2015 doi: 10.1016/j.mayocp.2015.10.009. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 43.Kalichman L., Hunter D.J. Diagnosis and conservative management of degenerative lumbar spondylolisthesis. Eur Spine J. 2008 doi: 10.1007/s00586-007-0543-3. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Theodoridis T., Kramer J., Kleinert H. Conservative treatment of lumbar spinal stenosis - a review. [German] TT - Konservative behandlung der lumbalen spinalkanalstenose - Eine ubersicht. Z Orthop Unfall. 2008 doi: 10.1055/s-2007-989394. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 45.Lurie J., Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ (Online) 2016 doi: 10.1136/bmj.h6234. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cao J., Wang T., Li Z. Factors associated with death in bedridden patients in china: a longitudinal study. PloS One. 2020 doi: 10.1371/journal.pone.0228447. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zou J., Yu H., Song D. Advice on standardized diagnosis and treatment for spinal diseases during the coronavirus disease 2019 pandemic. Asian Spine J. 2020;14:258–263. doi: 10.31616/asj.2020.0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yang X., Yu Y., Xu J. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30079-5. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang X., Pan Z., Cheng Z. medRxiv; 2020. Association between 2019-nCoV Transmission and N95 Respirator Use. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]