Abstract
Objective
The purpose of this study was to assess the effectiveness and safety of acupuncture for functional constipation (FC).
Methods
A rigorous literature search was performed in English (PubMed, Web of Science, the Cochrane Library, and EMBASE) and Chinese (China National Knowledge Infrastructure (CNKI), Chinese Biological Medical (CBM), Wanfang database, and China Science and Technology Journal (VIP)) electronic databases from their inception to October 2019. Included randomized controlled trials (RCTs) compared acupuncture therapy with sham acupuncture or pharmacological therapies. The outcome measures were evaluated, including the primary outcome of complete spontaneous bowel movement (CSBM) and secondary outcomes of Bristol Stool Form Scale (BSFS), constipation symptoms scores (CSS), responder rate, the Patient Assessment of Constipation Quality of Life (PAC-QOL) questionnaire, and safety evaluation. Meta-analysis was performed by using RevMan5.3.
Results
The merged data of 28 RCTs with 3525 participants indicated that acupuncture may be efficient for FC by increasing CSBMs (p < 0.00001; MD = 0.84 [95% CI, 0.65 to 1.03]; I2 = 0%) and improving constipation symptoms (p=0.03; SMD = −0.4 [95% CI, −0.78 to −0.03]; I2 = 74%), stool formation (p < 0.00001; MD = 0.24 [95% CI, 0.15 to 0.34]; I2 = 0%), quality of life (p < 0.00001; N = 1, MD = −0.33 [95% CI, −0.45 to −0.21]), and responder rates (p=0.02; RR = 2.16; [95% CI, 1.1 to 4.24]; I2 = 69%) compared with the effects of sham treatment. No increased risk of adverse events was observed (p=0.44; RR = 1.18; [95% CI, 0.77 to 1.81]; I2 = 0%). With regard to medication comparisons, the pooled data indicated that acupuncture was more effective in increasing CSBMs (p=0.004; MD = 0.53 [95% CI, 0.17 to 0.88]; I2 = 88%) and improving patients' quality of life (p < 0.00001; SMD = −0.73 [95% CI, −1.02 to −0.44]; I2 = 64%), with high heterogeneity. However, there were no significant differences in responder rate (p=0.12; RR = 1.31; [95% CI, 0.94 to 1.82]; I2 = 53%), BSFS (p=0.5; MD = 0.17 [95% CI, −0.33 to 0.68]; I2 = 93%), or CSS (p=0.05; SMD = −0.62 [95% CI, −1.23 to −0.01]; I2 = 89%). Regarding safety evaluation, acupuncture was safer than medications (p < 0.0001; RR = 0.3; [95% CI, 0.18 to 0.52]; I2 = 30%).
Conclusions
Current evidence suggests that acupuncture is an efficient and safe treatment for FC. Acupuncture increased stool frequency, improved stool formation, alleviated constipation symptoms, and improved quality of life. However, the evidence quality was relatively low and the relationship between acupuncture and drugs is not clear. More high-quality trials are recommended in the future. PROSPERO registration number: CRD42019143347.
1. Introduction
Functional constipation (FC) is one of the common functional bowel disorders that affect approximately 14% of the adult population worldwide [1]. One survey study indicated that the most frequent symptoms of FC were decreased defecation frequency, difficult stools, feelings of incomplete evacuation, and abdominal discomfort [2]. Although FC is not life-threatening, it has a very significant adverse impact on quality of life and increases economic costs [3, 4]. Risk factors for FC include female sex, older age, and reduced caloric intake [5, 6]. These adverse effects make the management of constipation a major clinical issue.
Many guidelines and reviews summarize stepwise clinical therapeutic approaches from appropriate lifestyle and dietary modifications to various drug administration, including osmotic agents, stimulant laxatives, prosecretory agents, serotonin (5-HT4) receptor agonists, and probiotics, and so on [7, 8]. Anorectal biofeedback, nerve stimulation, and colonic surgery may be used to treat FC [9–11]. Although there are many methods to choose from, the side effects of these methods are notable, including diarrhea, bloating, nausea, and possible cardiovascular adverse events [12–14]. As a result, many people, including those who do not improve with existing medications or suffer many side effects, are interested in complementary alternative medicine.
According to a 2015 study, acupuncture and electroacupuncture were the most commonly used complementary and alternative therapies for constipation, followed by herbal medicine [15]. Acupuncture is an ancient Chinese medicine method in which acupuncture points on the skin are manually stimulated with needles. Acupuncture treats FC via regulation of the nervous system and peripheral gastrointestinal hormone contents [16, 17]. However, the current systematic review remained an uncertain conclusion whether acupuncture was effective in managing FC because of the miscellaneous outcome measures and diagnostic criteria and lack of high-quality repeatable multicenter randomized controlled trials (RCTs) [18]. Therefore, we performed a systematic review to evaluate the effectiveness and safety of acupuncture in the treatment of patients with FC via unification of measurement outcomes and inclusion criteria and the inclusion of high-quality RCTs.
2. Methods
This systematic review was registered in the PROSPERO registry (CRD42019143347), and the protocol was described previously [19]. The PRISMA guidelines and the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions were complied with this systematic review and meta-analysis (Table S1) [20, 21].
2.1. Search Strategy
Two reviewers (WZ and QHZ) searched the databases from inception to October 2019, including four English databases (the PubMed, Web of Science, Cochrane Library, and EMBASE) and four Chinese databases (China National Knowledge Infrastructure (CNKI), Chinese Biological Medical (CBM), China Science and Technology Journal (VIP), and Wanfang Data Chinese databases). We used the following terms: (1) “acupuncture,” “manual acupuncture,” “electroacupuncture,” “acupuncture therapy,” or “acupuncture points,” combined with (2) “constipation,” “functional constipation,” “colonic inertia,” “dyschezia,” “astriction,” “obstipation,” or “slow transit constipation.” (See Table 1, for the search terms and strategy.) Because of the language restriction of our researchers, only studies published in English and Chinese were included.
Table 1.
The search strategy in PubMed.
| Number | Search items |
|---|---|
| 1 | Functional constipation |
| 2 | Chronic functional constipation |
| 3 | Chronic constipation |
| 4 | Idiopathic constipation |
| 5 | Slow transit constipation |
| 6 | Functional gastrointestinal disorder |
| 7 | Functional defecatory disorder |
| 8 | Chronic severe functional constipation |
| 9 | Constipation |
| 10 | FC |
| 11 | CC |
| 12 | CSFC |
| 13 | Or 1–12 |
| 14 | Acupuncture |
| 15 | Acupuncture therapy |
| 16 | Acupuncture needle |
| 17 | Manual acupuncture |
| 18 | Electroacupuncture |
| 19 | Needling |
| 20 | MA |
| 21 | EA |
| 22 | Or 14–21 |
| 23 | Randomized controlled trial |
| 24 | Controlled clinical trial |
| 25 | Randomized |
| 26 | Randomly |
| 27 | Trial |
| 28 | Or 23–27 |
| 29 | Exp animals/not humans |
| 30 | 28 not 29 |
| 31 | 13 and 22 and 30 |
2.2. Study Selection
2.2.1. Inclusion Criteria
Participants: Patients over the age of 18 years who were diagnosed with FC using guidelines or the Rome IV/III/II criteria, regardless of demographic characteristics (ethnicity, comorbidity, gender, age) and severity of disease were included.
Study design: The trials were RCTs that used a two-, three-, or four-arm parallel design regardless of blinding.
Types of interventions: The intervention group was treated with acupuncture or electroacupuncture (EA), regardless of the number of acupuncture points, frequency, and courses of treatment. The control groups received no treatment, placebo acupuncture, sham acupuncture (SA), conventional medication, or placebo control.
Outcome measures: We limited the outcome measures to complete spontaneous bowel movement (CSBM), Bristol Stool Form Scale (BSFS), responder rate, constipation symptoms scores (CSS), the Patient Assessment of Constipation Quality of Life (PAC-QOL) questionnaire, and safety evaluation.
2.2.2. Exclusion Criteria
Crossover trials, uncontrolled trials, quasi-randomized trials, reviews, case reports, and animal experimental research studies were excluded.
Studies with participants that included special populations, such as pregnant women, lactating women, or those diagnosed with constipation due to irritable bowel syndrome, were excluded.
We excluded trials in which the controls received acupuncture in combination with other methods, such as moxibustion, herbs, or medication and conventional medications that were not Western medicine, such as Chinese medicine, Tibetan medicine, and Zhuang medicine.
Trials that compared different points or forms of acupuncture were also excluded.
We excluded low-quality trials that had a clear risk of bias, such as a lack of randomized methods and incomplete data.
Duplicate publications and studies with incomplete data were also excluded.
2.3. Data Extraction and Quality Assessment
Two of the authors (MMX and LW) reviewed all titles and abstracts independently to determine the eligibility of articles. Argument between the two reviewers was solved via discussion and arbitration by a third reviewer (YL). The two authors made a final judgment by reading the full text of the remaining articles. A standardized data extraction form was used to extract detailed data from each selected study. The extraction information was collected according to a fixed protocol: study sites, total numbers, numbers of acupuncture and control participants, mean age, mean constipation duration, treatment duration, and outcomes. Missing information about the included trials was obtained by contacting the correspondent authors via e-mail.
The Cochrane risk of bias tool was used to assess bias in each study included by the two reviewers (LW and WZ). The risk of bias domains included random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other bias. The risk of bias in each domain was rated as “low,” “high,” or “unclear.” Disagreements were resolved via consultation with the third reviewer (YL). Finally, we evaluated the quality of evidence for the outcomes (acupuncture vs. SA) of the included studies in our review using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) guidelines [22].
2.4. Outcome Assessment
The primary outcome was CSBM. Secondary outcomes were BSFS, CSS, responder rate, PAC-QOL, and safety evaluation. The time point of all results was after treatment. A CSBM was defined as a bowel movement with the sense of complete evacuation that occurred without the use of any medication or other methods to assist defecation in the previous 24 hours. The BSFS is a seven‐hierarchy scale, with scores of 1–2 indicating constipation, 3–5 indicating normal stool, and 6–7 indicating diarrhea. The CSS assessed patients' eight constipation-related symptoms, including straining, endless sensation of defecation, bowel sound, abdominal pain, abdominal bloating, stool consistency, diarrhea, and fecal incontinence [23]. Responder rate was defined as the number of responders having at least three CSBMs per week divided by the total number of participants in each group. The PAC-QOL scored the effects of constipation on physical discomfort, psychosocial discomfort, anxiety, concerns, and satisfaction in their daily lives [24]. Higher scores indicated more defects or dissatisfaction. Safety evaluation was assessed using the adverse event reported in the studies.
2.5. Data Analysis
The Review Manager software program (version 5.3) was used for data synthesis. For continuous variables, such as CSBM, BSFS, CSS, and PAC-QOL, the mean difference (MD) or standard mean difference (SWD) with 95% confidence interval (CI) was used for analysis. For dichotomous data, such as the rates of responders and adverse events, the relative risk (RR) with 95% CI was utilized for analysis. Some studies reported change‐from‐baseline values instead of after‐treatment values. We calculated the after‐treatment values, assuming a correlation coefficient of 0.4 between baseline values and after‐treatment values according to the Cochrane handbook [25]. For studies that satisfied the predefined inclusion criteria with multiple intervention groups, if the multiple intervention groups used different acupuncture methods, we merged the data into a unified acupuncture group data. If the multiple intervention groups were different comparison groups, we implemented pairwise comparisons. For missing data, we contacted the corresponding authors via e-mail, otherwise the results were excluded. The magnitude of heterogeneity was measured using the I2 statistic: when I2 < 50%, a fixed-effects model will be used for pooled data; and when I2 ≥ 50%, a random-effects model was used. For each merged analysis, a heterogeneity test was performed using the chi-squared statistic. If I2 ≥ 50%, the synthesized studies were considered an indicator of a substantial level of heterogeneity. Subgroup or sensitivity analysis was performed to identify the cause. Subgroup analyses identified the possible factors that contributed to the heterogeneity, such as different acupuncture stimulation parameters, different control groups, participants' age, or disease course. And we evaluated publication bias by using funnel plots (n > 10).
3. Results
3.1. Search Results
According to the search strategy, a total of 1673 articles were identified. After duplicates were removed, 1131 articles were further evaluated using the eligibility criteria. Then, 116 articles were eligible for full-text evaluation after screening the titles and abstracts. We also excluded 86 articles for the following reasons: including IBS patients, no interested outcome indicator, repeated published data, not RCT, and low quality. Eventually, we included 30 studies in our system review [26–55]. Although 30 articles were included after screening, actually only 28 related RCTs (3525 participants) were extracted because data of 4 articles were from the same two RCTs (Peng, 2013; Mao, 2017 (2)), respectively [39, 40, 49, 50]. After reading the full text and analyzing the time period of study, we found that the outcomes from Mao, 2017 (2) were selectively reported in 2016 and 2017 separately. The same selective reporting is the RCT of Peng, 2013. The search process was showed in Figure 1.
Figure 1.
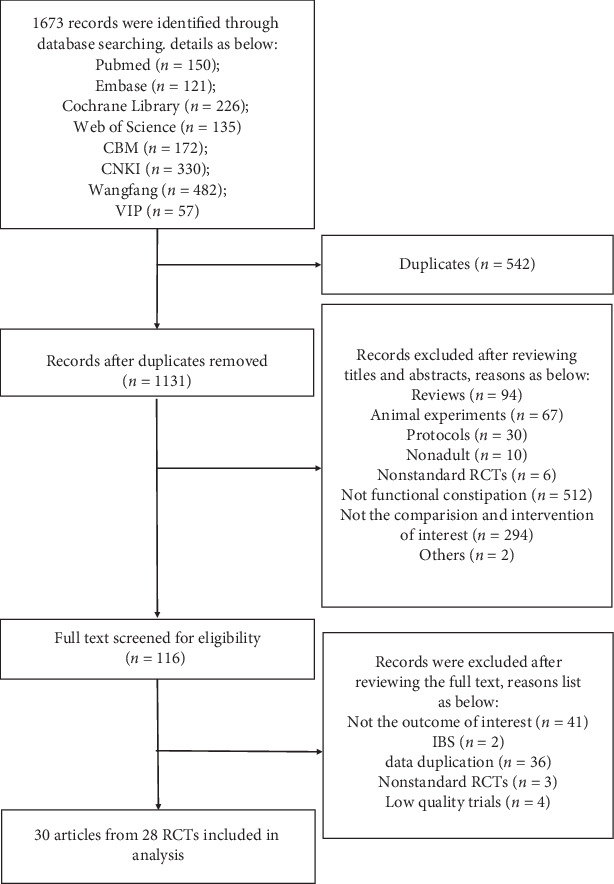
Flow diagram of the selection process.
3.2. Characteristics of the Studies
The included studies came from Korea and China and were published between 2010 and 2019. The diagnostic criteria of one RCT were the guidelines for clinical research [44], and the other RCTs were Rome III.There was 1 four-arm RCT [55], 5 three-arm RCTs [49–54], and 23 two-arm RCTs [26–48]. The treatment duration was set for 2 weeks in 2 studies [32, 46], 3 weeks in 1 study [47], 4 weeks in 18 studies [27, 30, 31, 33–37, 42, 44, 45, 48–55], and 8 weeks in 7 studies[26, 28, 29, 38–41, 43]. For these 28 trials, 10 trials reported CSBM [26–28, 36, 38–43, 46], 13 trials reported BSFS [27–29, 34, 35, 38–43, 47, 48, 53], 9 trials presented responder rate [26, 28, 29, 38–41, 43, 47, 53], 6 trials presented CSS [30, 45, 48–52], 10 trials mentioned PAC-QOL [28, 32, 33, 37, 38, 41, 43, 44, 46, 53], and 15 trials mentioned safety evaluation [26–33, 49–55]. Table 2 summarizes the other parameters of the included trials.
Table 2.
Characteristics of included studies.
| Author | Study sites | n | Diagnostic criteria | Participants | Participants' age (years, M ± SD) | Disease course (M ± SD) | Duration | Outcomes |
|---|---|---|---|---|---|---|---|---|
| Acupuncture vs sham electroacupuncture | ||||||||
| Da et al. [26] | 1 | 67 | Rome III | Treatment: 34 | 37.94 ± 18.06 | 139.59 ± 112.68 mos | 8 weeks | ①③⑥ |
| Control: 33 | 37.00 ± 17.89 | 106.21 ± 91.98 mos | ||||||
| Lee et al. [27] | 1 | 29 | Rome III | Treatment: 14 | 49.6 ± 12.7 | Not reported | 4 weeks | ①②⑥ |
| Control: 15 | 50.0 ± 10.5 | Not reported | ||||||
| Liu et al. [28] | 15 | 1075 | Rome III | Treatment: 536 | 47.01 ± 16.5 | 130.8 ± 122.6 mos | 8 weeks | ①②③⑤⑥ |
| Control: 539 | 47.33 ± 15.8 | 132.7 ± 127.0 mos | ||||||
| Wu [29] | 1 | 120 | Rome III | Treatment: 60 | 49 ± 34.5 | 68.5 ± 94.5 mos | 8 weeks | ②③⑥ |
| Control: 60 | 52.63 ± 12.9 | 101 ± 102.2 mos | ||||||
| Xue et al. [30] | 1 | 96 | Rome III | Treatment: 48 | 48.85 ± 13.30 | 7.65 ± 6.48 yrs | 4 weeks | ④⑥ |
| Control: 48 | 45.25 ± 11.28 | 8.48 ± 5.76 yrs | ||||||
|
| ||||||||
| Acupuncture vs polyethylene glycol | ||||||||
| Chen [31] | 1 | 61 | Rome III | Treatment: 30 | 48.80 ± 8.18 | 5.06 ± 3.66 mos | 4 weeks | ⑥ |
| Control: 31 | 48.58 ± 8.14 | 4.94 ± 3.68 mos | ||||||
| Mao [32] | 1 | 62 | Rome III | Treatment: 30 | 74.5 | 1 mos | 2 weeks | ⑤⑥ |
| Control: 32 | 73 | 1 mos | ||||||
| Ou [33] | 1 | 170 | Rome III | Treatment: 84 | 48.03 ± 17.19 | 24.52 ± 11.32 mos | 4 weeks | ⑤⑥ |
| Control: 86 | 46.64 ± 15.71 | 23.5 ± 10.36 mos | ||||||
|
| ||||||||
| Acupuncture vs mosapride | ||||||||
| Ding et al. [34] | 1 | 63 | Rome III | Treatment: 33 | 34.83 ± 11.76 | 5.71 ± 2.54 yrs | 4 weeks | ② |
| Control: 30 | ||||||||
| Lian et al. [35] | 1 | 63 | Rome III | Treatment: 33 | 26.85 ± 8.27 | 3.44 ± 2.56 yrs | 4 weeks | ② |
| Control: 30 | 27.60 ± 7.86 | 2.92 ± 2.24 yrs | ||||||
| Wang et al. [36] | 1 | 68 | Rome III | Treatment: 34 | 47.8 ± 10.1 | 7. 6 ± 6.4 yrs | 4 weeks | ① |
| Control: 34 | 46. 6 ± 11. 0 | 8.1 ± 5.9 yrs | ||||||
| Wang [37] | 1 | 54 | Rome III | Treatment: 37 | 28.08 ± 13.42 | 95.43 ± 103.03 mos | 4 weeks | ⑤ |
| Control: 17 | 27.59 ± 9.70 | 92.00 ± 78.48 mos | ||||||
|
| ||||||||
| Acupuncture vs prucalopride | ||||||||
| Dai [38] | 1 | 60 | Rome III | Treatment: 30 | 40.48 ± 2.96 | 110.76 ± 17.4 mos | 8 weeks | ①②③⑤ |
| Control: 30 | 42.80 ± 3.92 | 150.48 ± 30.84 mos | ||||||
| Mao [39, 40] | 1 | 56 | Rome III | Treatment: 28 | 44.85 ± 7.71 | 3.78 ± 2.12 yrs | 8 weeks | ①②③ |
| Control: 28 | 46.95 ± 9.83 | 3.88 ± 2.36 yrs | ||||||
| Song [41] | 1 | 39 | Rome III | Treatment: 20 | 51.40 ± 12.90 | Not reported | 8 weeks | ①②③⑤ |
| Control: 19 | 49.16 ± 12.31 | Not reported | ||||||
| Wang et al. [42] | 1 | 60 | Rome III | Treatment: 30 | 46 ± 7 | 4.52 ± 2.36 yrs | 4 weeks | ①② |
| Control: 30 | 47 ± 8 | 4.64 ± 2.65 yrs | ||||||
| Wang [43] | 1 | 38 | Rome III | Treatment: 19 | 41.53 ± 16.15 | 76.68 ± 7.75 mos | 8 weeks | ①②③⑤ |
| Control: 19 | 35.29 ± 13.26 | 76 ± 4.93 mos | ||||||
|
| ||||||||
| Acupuncture vs cisapride | ||||||||
| Zhou et al. [44] | 1 | 60 | The guidelines for clinical research | Treatment: 30 | 37. 36 ± 10. 32 | 2. 54 ± 1. 63 yrs | 4 weeks | ⑤ |
| Control: 30 | 39. 58 ± 11. 63 | 2. 72 ± 1. 76 yrs | ||||||
| Acupuncture vs lactulose | ||||||||
| Jin [45] | 1 | 37 | Rome III | Treatment: 22 | 39.14 ± 14.45 | 115.18 ± 108.08 mos | 4 weeks | ④ |
| Control: 15 | 45.13 ± 17.09 | 157.4 ± 142.24 mos | ||||||
| Liu et al. [46] | 1 | 60 | Rome III | Treatment: 30 | 53. 13 ± 9. 65 | 3.70 ± 2. 54 yrs | 2 weeks | ①⑤ |
| Control: 30 | 52.76 ± 8.87 | 3.96 ± 2.68 yrs | ||||||
| Ruan et al. [47] | 1 | 45 | Rome III | Treatment: 21 | 68 ± 9 | 17.90 ± 9.77 mos | 3 weeks | ②③ |
| Control: 24 | 69 ± 8 | 16.92 ± 10.04 mos | ||||||
| Shi [48] | 1 | 60 | Rome III | Treatment: 30 | 64.87 ± 4.208 | 5.27 ± 3.51 yrs | 4 weeks | ②④⑥ |
| Control: 30 | 66.27 ± 3.513 | 5.5 ± 3.94 yrs | ||||||
|
| ||||||||
| Acupuncture vs sham acupuncture vs lactulose | ||||||||
| Peng et al. [49, 50] | 3 | 128 | Rome III | Treatment: 64 | 53 ± 13 | 125.1 ± 128.6 mos | 4 weeks | ④⑥ |
| Control A: 33 | 52 ± 17 | 118 ± 105.8 mos | ||||||
| Control B: 31 | 59 ± 12 | 97.8 ± 123 mos | ||||||
| Wang et al. [51] | 1 | 95 | Rome III | Treatment: 48 | 48.8 ± 13.3 | 7.65 ± 6.48 yrs | 4 weeks | ④⑥ |
| Control A: 24 | 40.8 ± 10.0 | 9.46 ± 5.89 yrs | ||||||
| Control B: 23 | 44.6 ± 15.2 | 7.65 ± 5.65 yrs | ||||||
| Wu et al. [52] | 5 | 475 | Rome III | Treatment: 228 | 45.88 ± 16.85 | 110.84 ± 99.85 mos | 4 weeks | ④⑥ |
| Control A: 112 | 46.25 ± 16.81 | 109.25 ± 100.70 mos | ||||||
| Control B: 115 | 44.12 ± 17.48 | 111.04 ± 110.15 mos | ||||||
|
| ||||||||
| Acupuncture vs mosapride vs mosapride & sham electroacupuncture | ||||||||
| Xu [53] | 1 | 90 | Rome III | Treatment: 30 | 35.26 ± 19.07 | 8.88 yrs | 4 weeks | ②③⑤⑥ |
| Control A: 30 | 35.42 ± 15.28 | 8.71 yrs | ||||||
| Control B: 30 | 36.00 ± 17.20 | 8.83 yrs | ||||||
|
| ||||||||
| Low intensity acupuncture vs high intensity acupuncture vs mosapride | ||||||||
| Wu et al. [54] | 3 | 190 | Rome III | Treatment A: 58 | 34.00 ± 15.62 | 70.44 ± 85.53 mos | 4 weeks | ⑥ |
| Treatment B: 65 | 37.20 ± 18.19 | 86.29 ± 104.06 mos | ||||||
| Control: 67 | 43.60 ± 17.90 | 68.09 ± 74.13 mos | ||||||
|
| ||||||||
| Shu-mu vs He vs Shu-mu-he vs mosapride | ||||||||
| Wu et al. [55] | 1 | 104 | Rome III | Treatment A: 19 | 61 (16) | 130 mos | 4 weeks | ⑥ |
| Treatment B: 34 | 53 ± 12 | 123 mos | ||||||
| Treatment C: 26 | 56 ± 9 | 217.35 mos | ||||||
| Control: 25 | 55 ± 11 | 130 mos | ||||||
Notes: M ± SD, the mean ± standard deviation; mos, months; yrs, years; ① complete spontaneous bowel movement (CSBM); ② Bristol Stool Form Scale (BSFS); ③ responder rate; ④ constipation symptoms scores (CSS); ⑤ Patient Assessment Of Constipation Quality Of Life (PAC-QOL) questionnaire; ⑥ safety evaluation.
3.3. Risk of Bias Assessment
Figure 2 summarizes the risk of bias in the 28 RCTs. Blinding of participants and personnel and incomplete outcome data may be the major reasons for selection bias and performance bias. Many studies were associated with an unclear risk of bias for blinding of outcome assessment, selective reporting, and other possible bias.
Figure 2.
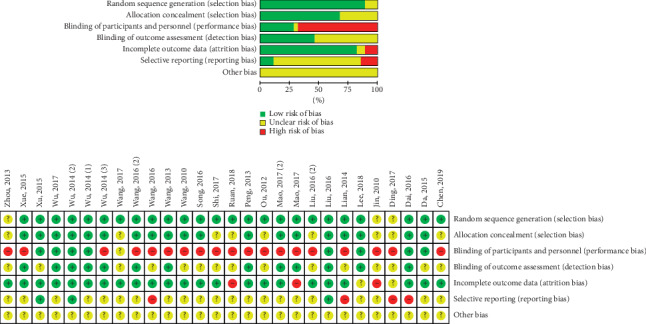
Risk of bias assessment.
3.4. Acupuncture vs SA
The merged data indicated that the acupuncture group exhibited significantly greater efficacy than the SA group in increasing CSBMs (p < 0.00001; MD = 0.84 [95% CI, 0.65 to 1.03]; I2 = 0%) and improving stool formation (p < 0.00001; MD = 0.24 [95% CI, 0.15 to 0.34]; I2 = 0%), responder rates (p=0.02; RR = 2.16; [95% CI, 1.1 to 4.24]; I2 = 69%), constipation symptoms (p=0.03; SMD = −0.4 [95% CI, −0.78 to −0.03]; I2 = 74%), and the quality of life (p < 0.00001; N = 1, SMD = −0.33 [95% CI, −0.45 to −0.21]). No increased risk of adverse events was observed (p=0.44; RR = 1.18; [95% CI, 0.77 to 1.81]; I2 = 0%). Sensitivity analysis showed that acupuncture produced a significant decrease in CSS after the removal of one study [30] (p=0.02; SMD = −0.23 [95% CI, −0.42 to −0.04]; I2 = 0%) (Figures 3–8).
Figure 3.
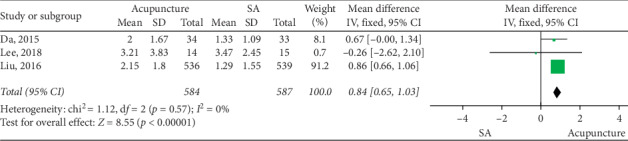
Forest plot for CSBM (acupuncture vs SA).
Figure 4.
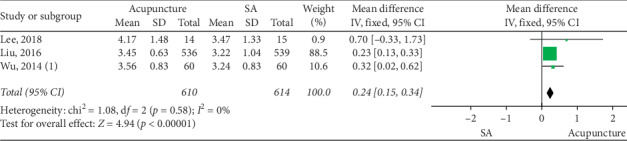
Forest plot for BSFS (acupuncture vs SA).
Figure 5.
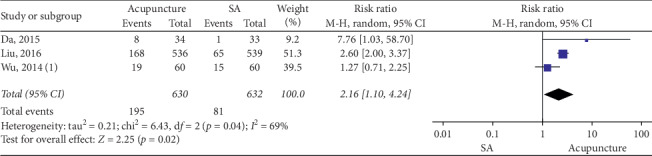
Forest plot for responder rate (acupuncture vs SA).
Figure 6.
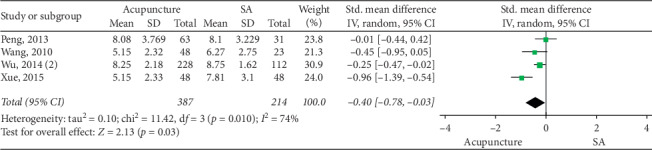
Forest plot for CSS (acupuncture vs SA).
Figure 7.
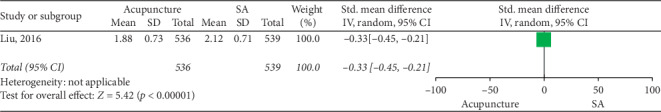
Forest plot for PAC-QOL (acupuncture vs SA).
Figure 8.
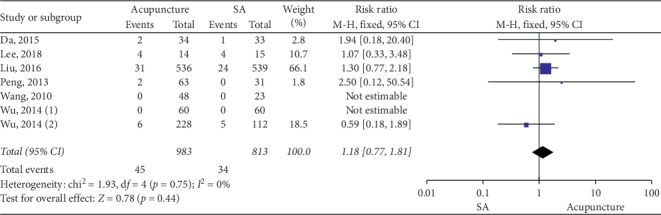
Forest plot for safety evaluation (acupuncture vs SA).
3.5. Acupuncture vs Medication
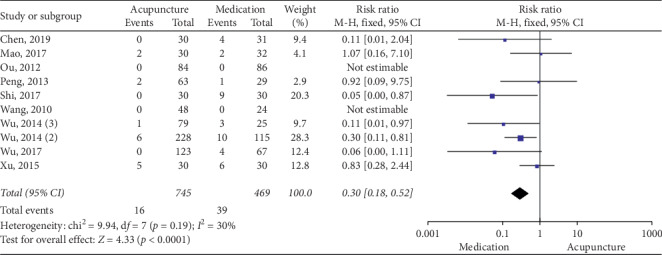
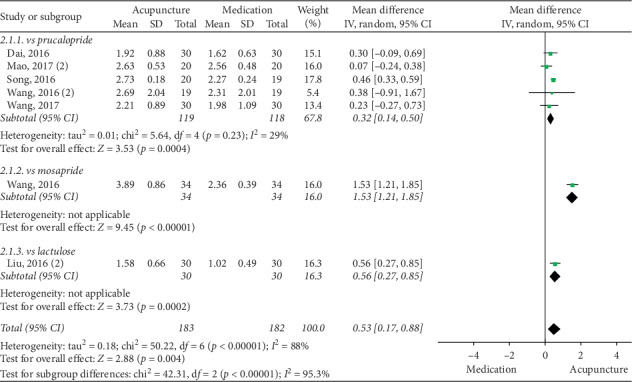
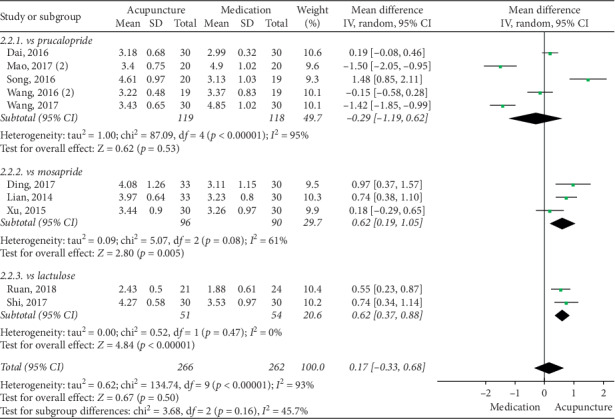
The pooled data indicated that acupuncture was more effective in increasing CSBMs (p=0.004; MD = 0.53 [95% CI, 0.17 to 0.88]; I2 = 88%) and improving patients' quality of life (p < 0.00001; SMD = −0.73 [95% CI, −1.02 to −0.44]; I2 = 64%) than the medication groups. However, there were no significant differences in responder rate (p=0.12; RR = 1.31; [95% CI, 0.94 to 1.82]; I2 = 53%), BSFS (p=0.5; MD = 0.17 [95% CI, −0.33 to 0.68]; I2 = 93%), and CSS (p=0.05; SMD = −0.62 [95% CI, −1.23 to −0.01]; I2 = 89%). Acupuncture was safer than medication (p < 0.0001; RR = 0.3; [95% CI, 0.18 to 0.52]; I2 = 30%) (Figures 9–14).
Figure 9.
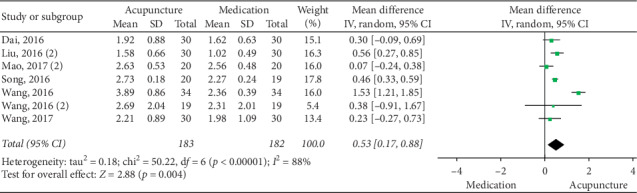
Forest plot for CSBM (acupuncture vs medication).
Figure 10.
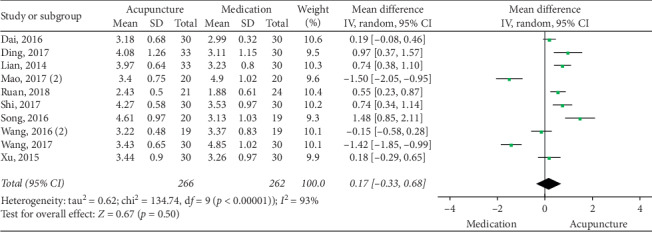
Forest plot for BSFS (acupuncture vs medication).
Figure 11.
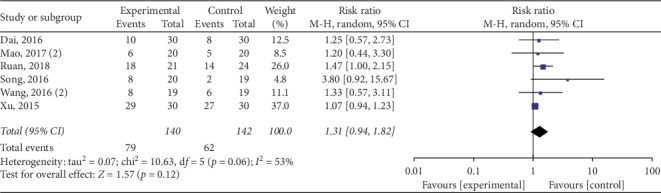
Forest plot for responder rate (acupuncture vs medication).
Figure 12.
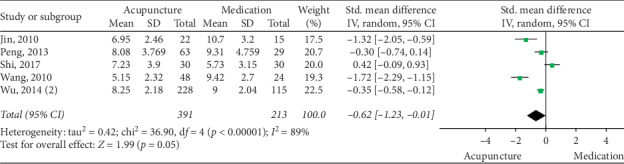
Forest plot for CSS (acupuncture vs medication).
Figure 13.
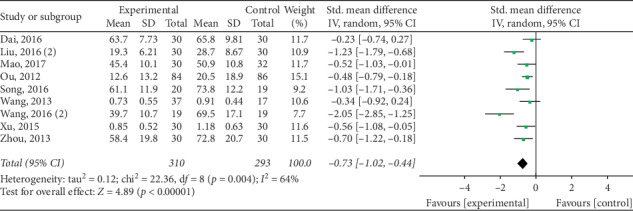
Forest plot for PAC-QOL (acupuncture vs medication).
Figure 14.
Forest plot for safety evaluation (acupuncture vs medication).
The sensitivity analysis showed that heterogeneities in CSBM (p < 0.00001; MD = 0.37 [95% CI, 0.22 to 0.52 ]; I2 = 27%), PAC-QOL (p < 0.00001; SMD = −0.6 [95% CI, −0.82 to −0.39]; I2 = 31%), and responder rate (p=0.01; RR = 1.45; [95% CI, 1.08 to 1.95]; I2 = 0%) were reduced significantly after the removal of 1 RCT [36, 43, 53]. However, we did not find a clear source of heterogeneity for CSS and BSFS with an I2 statistic that ranged from 80% to 93% in subgroup analyses, such as different acupuncture stimulation parameters, different drug groups, age, and disease course.
3.6. Subgroup Analysis for Medication
3.6.1. CSBM
Acupuncture had a better effect than prucalopride (p=0.0004; WMD = 0.32 [95% CI, 0.14 to 0.5]; I2 = 29%). However, sensitivity analysis found no significant difference between acupuncture and prucalopride after the removal of one study (p=0.1; WMD = 0.18 [95% CI, −0.04 to 0.4]; I2 = 0%). Two studies showed that acupuncture had a better performance than mosapride and lactulose (Figure 15).
Figure 15.
Forest plot for CSBM by subgroup analysis.
3.6.2. BSFS
Subgroup analysis showed a significant increase in the acupuncture groups' performance on BSFS relative to the lactulose group (p < 0.00001; WMD = 0.62 [95% CI, 0.37 to 0.88]; I2 = 0%) and the mosapride group (p=0.005; WMD = 0.62 [95% CI, 0.19 to 1.05]; I2 = 61%). Acupuncture was not significantly different than the highly heterogeneous comparison with prucalopride (p=0.53; WMD = −0.29 [95% CI, −1.19 to 0.62]; I2 = 95%) (Figure 16).
Figure 16.
Forest plot for BSFS by subgroup analysis.
3.6.3. CSS
There was no evidence of a benefit in reducing CSS in the acupuncture group compared to the lactulose group (p=0.05; SMD = −0.62 [95% CI, −1.23 to −0.01]; I2 = 89%). However, sensitivity analysis found that acupuncture was superior to lactulose in reducing CSS after the removal of one study [48] (p=0.008; SMD = −0.87 [95% CI, −1.52 to −0.23]; I2 = 88%) (Figure 17).
Figure 17.
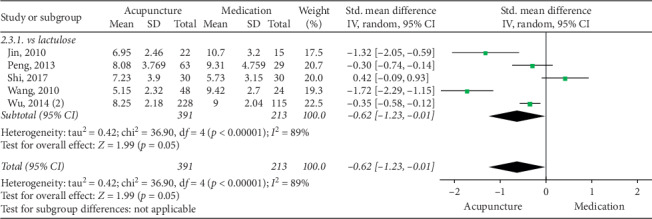
Forest plot for CSS by subgroup analysis.
3.6.4. PAC-QOL
Subgroup analysis revealed that acupuncture produced a significant benefit compared with polyethylene glycol (p=0.0002; SMD = −0.49 [95% CI, −0.75 to −0.23]; I2 = 0%) and mosapride (p=0.02; SMD = −0.47 [95% CI, −0.85 to −0.08]; I2 = 0%). Two studies reported that the acupuncture group had a lower score than the cisapride group (p=0.008, N = 1, n = 60, 95% CI, −1.22 to −0.18) and lactulose group (p < 0.0001, N = 1, n = 60, 95% CI, −1.79 to −0.68). However, high heterogeneity was found in comparisons with prucalopride (p=0.04; SMD = −1.07 [95% CI, −2.08 to −0.05]; I2 = 86%) (Figure 18).
Figure 18.
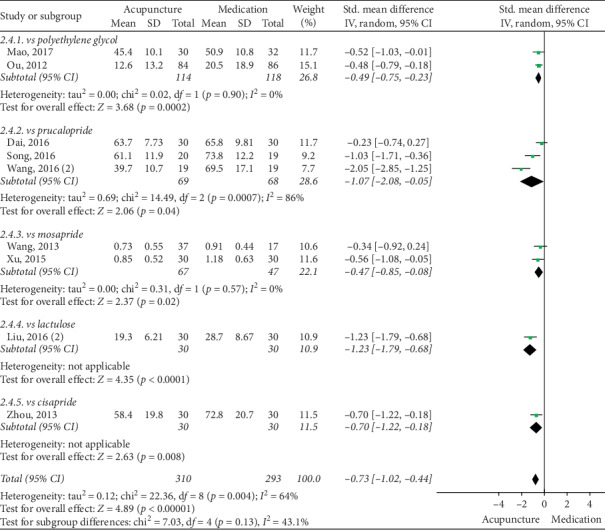
Forest plot for PAC-QOL by subgroup analysis.
3.6.5. Responder Rate
Prucalopride (p=0.07; RR = 1.25; [95% CI, 0.98 to 1.6]; I2 = 14%), mosapride (N = 1, n = 60, p=0.31; [95% CI, 0.94 to 1.23]), and lactulose (N = 1, n = 45, p=0.05; [95% CI, 1 to 2.15]) failed to achieve statistical significance (Figure 19).
Figure 19.
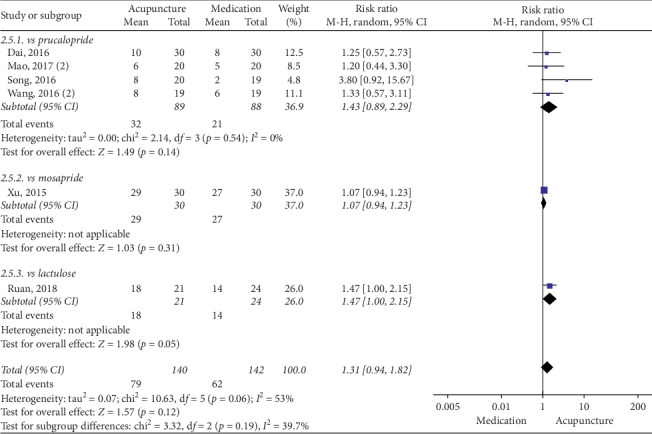
Forest plot for responder rate by subgroup analysis.
3.6.6. Safety Evaluation
The subgroup analysis suggested that acupuncture produced no significant difference compared with polyethylene glycol (p=0.21; RR = 0.4; [95% CI, 0.1 to 1.67]; I2 = 43%). Methodologically, acupuncture was safer than lactulose (p=0.0009; RR = 0.24; [95% CI, 0.1 to 0.56]; I2 = 23%) and mosapride (p=0.01; RR = 0.36; [95% CI, 0.16 to 0.8]; I2 = 60%) (Figure 20).
Figure 20.
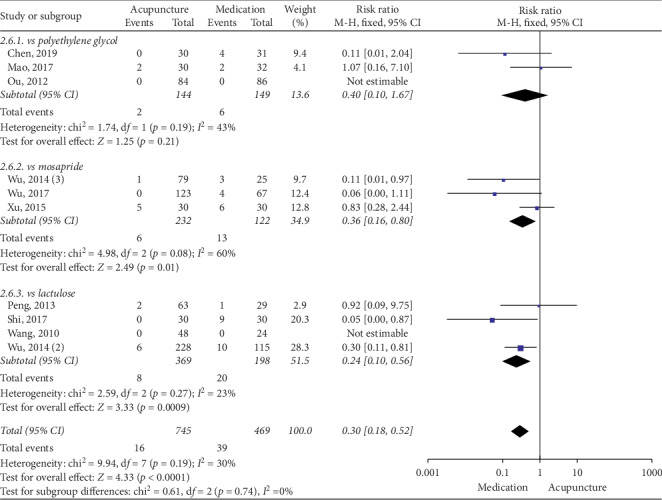
Forest plot for safety evaluation by subgroup analysis.
3.7. GRADE Evaluation
We only evaluated the qualities of the outcomes that compared acupuncture with SA, and the quality of that evidence ranged from very low to moderate (Table 3). The major reasons for downgrading the evidence quality were inconsistency and reporting bias. The levels of evidence quality were moderate for PAC-QOL and safety evaluation, low for CSBM, BSFS, and responder rate, and very low for CSS.
Table 3.
GRADE evaluation: acupuncture compared to sham acupuncture.
| Condition | No. of participants (studies) | Design | Limitations | Inconsistency | Indirectness | Imprecision | Other considerations | MD or SMD or RR (95% CI) | Quality |
|---|---|---|---|---|---|---|---|---|---|
| CSBM | 1171 (3) | RCT | No serious | Serious | No serious | No serious | Reporting bias | 0.84 (0.65 to 1.03) | Low |
| BSFS | 1224 (3) | RCT | No serious | Serious | No serious | No serious | Reporting bias | 0.24 (0.15 to 0.34) | Low |
| CSS | 432 (4) | RCT | Serious | Serious | Serious | Serious | Reporting bias | −0.42 (−0.81 to −0.02) | Very low |
| PAC-QOL | 1075 (1) | RCT | No serious | No serious | No serious | No serious | Reporting bias | −0.33 (−0.45 to −0.21) | Moderate |
| Responder rate | 1262 (3) | RCT | No serious | Serious | No serious | No serious | Reporting bias | 2.16 (1.1 to 4.24) | Low |
| Safety evaluation | 1627 (7) | RCT | Serious | No serious | No serious | No serious | None | 1.21 (0.78 to 1.87) | Moderate |
RCT, randomized controlled trial; MD, mean difference; SMD, standard mean difference; RR, relative risk; CI, confidence interval.
4. Discussion
4.1. Principal Results
The present review examined 28 RCTs involving 3525 participants that studied the effects of acupuncture treatment on the management of FC. Acupuncture was associated with the magnitude of clinically relevant effects in reducing the severity of FC compared with SA and pharmacological treatments (polyethylene glycol, prucalopride, mosapride, cisapride, and lactulose). With regard to SA comparison, acupuncture treatment may not increase the risk of adverse events and may be more efficient in increasing CSBMs, improving stool formation, alleviating constipation symptoms, and promoting the quality of life and responder rates. This study found that SA was inferior to real acupuncture for patients, which was consistent with previous findings [18, 56, 57]. However, the evidence quality was relatively low because of inconsistency and reporting bias. Our meta-analysis showed that acupuncture may be more effective than pharmacological treatment in increasing weekly CSBMs and improving the quality of life and responder rate. The data suggested that acupuncture caused fewer adverse events. However, no significant benefits in stool formation or clinical symptoms of FC were found in patients who received acupuncture compared with drug with high heterogeneity.
Previous studies showed that many factors influenced the efficacy of acupuncture, such as age, comorbidity, gender, disease severity, stimulation of acupuncture, expectations of patients, and doctor-patient interaction, which may be sources of heterogeneity [58–60]. However, due to the inability to obtain more relevant data, we cannot analyze based on relevant influencing factors. The present study only found that the heterogeneity may be caused by different control group. There were two outcomes (CSS and BSFS) without an apparent source of heterogeneity compared between acupuncture and medication. Our careful data analysis suggested that small sample size, the specificity of outcome indicators, and statistical methods may be the reasons for heterogeneity. For example, different types of variables, such as considering the BSFS as a continuous or categorical variable, may have differentially influenced the heterogeneity. However, most of the results of the included high-quality studies did not include categorical variable data, and we cannot judge whether the two analysis methods have different effects on the results.
The current study included five Western medicines that were directly compared with acupuncture, including saline laxatives (polyethylene glycol), osmotic laxatives (lactulose), and 5‐HT agonists (prucalopride, mosapride, and cisapride). The guidelines have different mechanisms of action and side effects, such as mosapride, which only acts in the upper digestive tract, and cisapride, which is associated with cardiac arrest [61, 62]. Therefore, to avoid the effect of different mechanisms of action and side effects of drugs on the results, we added a different subgroup analysis based on drug control.
Compared with the first-line agents, the subgroup analysis showed that acupuncture may be more effective than lactulose in increasing weekly CSBMs and more advantageous than polyethylene glycol, prucalopride, and lactulose in improving the quality of life. It was suggested that acupuncture caused fewer adverse events than polyethylene glycol and lactulose. However, the evidence is insufficient because of the drug characteristics, small sample size, and inadequate blinding. Studies showed that polyethylene glycol and lactulose were not effective in alleviating abdominal pain and bloating, which directly affect the quality of life of patients [62]. Because of the inert characteristics of acupuncture, it is difficult to implement a blinded method when choosing medication as a control. Therefore, the effectiveness of acupuncture is impossible to exclude because the patient has greater expectations for acupuncture treatment, especially improvements in subjective feelings.
4.2. Strengths
This meta-analysis has several strengths. Compared with previous reviews and meta-analyses, the unified specifications of the FC diagnostic criteria for inclusion in this review were all Rome III, except for one RCT [44]. We included several high-quality multicenter RCTs with large sample sizes from 2010 to 2019, including the largest trial with 1075 patients, which pinpointed that EA reduced the scores of constipation symptoms and quality of life in patients with chronic severe functional constipation after 8 weeks [28]. This review observed more comprehensive outcome indicators related to the effectiveness of FC treatment involving the frequency and symptoms of defecation, stool form, quality of life, and side effects and compared acupuncture with other clinical drugs for FC to show the effectiveness and safety of acupuncture more intuitively.
4.3. Limitations and Implications for Research and Practice
There are some limitations in this study. First, blinding remains a common challenge in acupuncture clinical research, and 19 RCTs had a high risk in the blinding of participants and personnel in our risk of bias assessment. Future trials should strengthen the effectiveness of the blinding method and adopt appropriate fake devices to examine research questions, minimize potential bias, and improve the quality of the evidence. Second, most RCTs were performed in China, which may lead to publication bias and affect the validity and reliability of this systematic review. Databases in other languages should be considered for inclusion in the future, such as Japanese, Korean, and German.
There are still some unanswered questions. First, the optimal variables deserve further investigation, including acupuncture type, frequency, duration, and selection of acupoints in acupuncture treatment. Our literature review found that many other types of acupuncture are used to treat FC, including warm needles, acupoint injections, and ear needles. No research showed that acupuncture or EA was the best method to treat FC, which requires further research.
Second, recent studies investigated the effectiveness of acupuncture for chronic severe FC, but there was no comprehensive data analysis to determine the efficacy of acupuncture for chronic severe FC. There remain further unanswered questions about which patients may find acupuncture most beneficial in terms of FC severity. We know that patients generally experience a range of other symptoms during constipation, such as anxiety, abdominal pain, and anorexia. Traditional acupuncturists consider these symptoms when making treatment plans. More trials of this type are needed to model real-world settings.
Finally, our subgroup analysis results showed that comparisons of acupuncture and drugs revealed many uncertainties in outcome indicators. The most prominent requirement in the past was to perform more high-quality RCTs to evaluate the effectiveness of acupuncture for the treatment of FC. This meta-analysis suggested that acupuncture was better than some clinical medicines in increasing defecation frequency and quality of life. Therefore, more trials are needed in the future to clarify the clinical advantages and disadvantages of acupuncture and explore how acupuncture can supplement or replace the shortage of existing drugs.
5. Conclusions
This systematic review suggests that acupuncture for FC is safe and effective, especially in terms of increased stool frequency and improved constipation symptoms, stool formation, and quality of life, but the relationship between acupuncture and drugs is not clear. In the future, high-quality RCTs are still needed to provide evidence to support these conclusions and examine the alternative or complementary relationship between acupuncture and existing drugs for the treatment of FC.
Acknowledgments
The author would like to acknowledge Dr Yu Guo from the School of Traditional Chinese Medicine, Jinan University. This study was supported by Grants from the National Natural Science Foundation of China (81774430) and Chengdu University of Traditional Chinese Medicine Xinglin Scholars Program (no.YXRC2018007).
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
Lu Wang, Mingmin Xu, and Qianhua Zheng contributed equally to this study.
Supplementary Materials
S1: checklist of items to include when reporting a systematic review or meta-analysis.
References
- 1.Suares N. C., Ford A. C. Prevalence of, and risk factors for, chronic idiopathic constipation in the community: systematic review and meta-analysis. American Journal of Gastroenterology. 2011;106(9):1582–1591. doi: 10.1038/ajg.2011.164. [DOI] [PubMed] [Google Scholar]
- 2.Johanson J. F., Kralstein J. Chronic constipation: a survey of the patient perspective. Alimentary Pharmacology & Therapeutics. 2007;25(5):599–608. doi: 10.1111/j.1365-2036.2006.03238.x. [DOI] [PubMed] [Google Scholar]
- 3.Guerin A., Carson R. T., Lewis B., Yin D., Kaminsky M., Wu E. The economic burden of treatment failure amongst patients with irritable bowel syndrome with constipation or chronic constipation: a retrospective analysis of a Medicaid population. Journal of Medical Economics. 2014;17(8):577–586. doi: 10.3111/13696998.2014.919926. [DOI] [PubMed] [Google Scholar]
- 4.Bruce Wirta S., Hodgkins P., Joseph A. Economic burden associated with chronic constipation in Sweden: a retrospective cohort study. ClinicoEconomics and Outcomes Research. 2014;6:369–379. doi: 10.2147/ceor.s61985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang J. Y., Locke G. R., Schleck C. D., Zinsmeister A. R., Talley N. J. Risk factors for chronic constipation and a possible role of analgesics. Neurogastroenterology & Motility. 2007;19(11):905–911. doi: 10.1111/j.1365-2982.2007.00974.x. [DOI] [PubMed] [Google Scholar]
- 6.Dukas L., Willett W. C., Giovannucci E. L. Association between physical activity, fiber intake, and other lifestyle variables and constipation in a study of women. The American Journal of Gastroenterology. 2003;98(8):1790–1796. doi: 10.1111/j.1572-0241.2003.07591.x. [DOI] [PubMed] [Google Scholar]
- 7.Mearin F., Lacy B. E., Chang L., et al. Bowel disorders. Gastroenterology. 2016;150(6):1393–1407. doi: 10.1053/j.gastro.2016.02.031. [DOI] [PubMed] [Google Scholar]
- 8.Aziz I., Whitehead W. E., Palsson O. S., Tornblom H., Simren M. An approach to the diagnosis and management of Rome IV functional disorders of chronic constipation. Expert Review of Gastroenterology & Hepatology. 2020;14(1):39–46. doi: 10.1080/17474124.2020.1708718. [DOI] [PubMed] [Google Scholar]
- 9.Parker C. H., Henry S., Liu L. W. C. Efficacy of biofeedback therapy in clinical practice for the management of chronic constipation and fecal incontinence. Journal of the Canadian Association of Gastroenterology. 2019;2(3):126–131. doi: 10.1093/jcag/gwy036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gortazar de Las Casas S., Rubio-Pérez I., Saavedra Ambrosy J., et al. Sacral nerve stimulation for constipation: long-term outcomes. Techniques in Coloproctology. 2019;23(6):559–564. doi: 10.1007/s10151-019-02011-z. [DOI] [PubMed] [Google Scholar]
- 11.Tsimogiannis K. E., Karlbom U., Lundin E., Graf W. Long-term outcome after segmental colonic resection for slow transit constipation. International Journal of Colorectal Disease. 2019;34(6):1013–1019. doi: 10.1007/s00384-019-03283-5. [DOI] [PubMed] [Google Scholar]
- 12.Song X., Wang D., Qu X., Dong N., Teng S. A meta-analysis of naldemedine for the treatment of opioid-induced constipation. Expert Review of Clinical Pharmacology. 2019;12(2):121–128. doi: 10.1080/17512433.2019.1570845. [DOI] [PubMed] [Google Scholar]
- 13.Gilsenan A., Fortuny J., Cainzos-Achirica M., et al. Cardiovascular safety of prucalopride in patients with chronic constipation: a multinational population-based cohort study. Drug Safety. 2019;42(10):1179–1190. doi: 10.1007/s40264-019-00835-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.MacDonald A., Shinbo K., Oota A., Kinoshita Y. Polyethylene glycol 3350 plus electrolytes for chronic constipation: a 2-week, randomized, double-blind, placebo-controlled study with a 52-week open-label extension. Journal of Gastroenterology. 2019;54(9):792–803. doi: 10.1007/s00535-019-01581-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang X., Yin J. Complementary and alternative therapies for chronic constipation. Evidence-Based Complementary and Alternative Medicine. 2015;2015:11. doi: 10.1155/2015/396396.396396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xiong F., Wang Y., Li S.-Q., Tian M., Zheng C.-H., Huang G.-Y. Clinical study of electro-acupuncture treatment with different intensities for functional constipation patients. Journal of Huazhong University of Science and Technology (Medical Sciences) 2014;34(5):775–781. doi: 10.1007/s11596-014-1351-8. [DOI] [PubMed] [Google Scholar]
- 17.Zhu X., Liu Z., Qu H., et al. The effect and mechanism of electroacupuncture at LI11 and ST37 on constipation in a rat model. Acupuncture in Medicine. 2016;34(3):194–200. doi: 10.1136/acupmed-2015-010897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhang T., Chon T. Y., Liu B., et al. Efficacy of acupuncture for chronic constipation: a systematic review. The American Journal of Chinese Medicine. 2013;41(4):717–742. doi: 10.1142/s0192415x13500493. [DOI] [PubMed] [Google Scholar]
- 19.Xu M., Zhang W., Wang L., Feng X., Li Y. The effect and safety of acupuncture on patients with functional constipation: protocol for a systematic review and meta-analysis of high quality RCTs. Medicine (Baltimore) 2019;98(49) doi: 10.1097/md.0000000000018125.e18125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moher D., Liberati A., Tetzlaff J., Altman D. G., Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Journal of Clinical Epidemiology. 2009;62(10):1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 21.Higgins J., Green S. Cochrance Handbook for Systematic Reviews of Interventions. Hoboken, NJ, USA: Wiley; 2011. http://www.cochrane-handbook.org. [Google Scholar]
- 22.Guyatt G. H., Oxman A. D., Vist G. E., et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. doi: 10.1136/bmj.39489.470347.ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Agachan F., Chen T., Pfeifer J., Reissman P., Wexner S. D. A constipation scoring system to simplify evaluation and management of constipated patients. Diseases of the Colon & Rectum. 1996;39(6):681–685. doi: 10.1007/bf02056950. [DOI] [PubMed] [Google Scholar]
- 24.Marquis P., De La Loge C., Dubois D., McDermott A., Chassany O. Development and validation of the patient Assessment of constipation quality of life questionnaire. Scandinavian Journal of Gastroenterology. 2005;40(5):540–551. doi: 10.1080/00365520510012208. [DOI] [PubMed] [Google Scholar]
- 25.Higgins J. P., Green S. Cochrane Handbook for Systematic Reviews of Interventions. Vol. 5. Hoboken, NJ, USA: Wiley Online Library; 2008. [Google Scholar]
- 26.Da N., Wang X., Liu H., et al. The effectiveness of electroacupuncture for functional constipation: a randomized, controlled, clinical trial. Evidence-Based Complementary and Alternative Medicine. 2015;2015:5. doi: 10.1155/2015/670963.670963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee H.-Y., Kwon O.-J., Kim J.-E., et al. Efficacy and safety of acupuncture for functional constipation: a randomised, sham-controlled pilot trial. BMC Complementary and Alternative Medicine. 2018;18(1):p. 186. doi: 10.1186/s12906-018-2243-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Liu Z., Yan S., Wu J., et al. Acupuncture for chronic severe functional constipation: a randomized trial. Annals of Internal Medicine. 2016;165(11):761–769. doi: 10.7326/M15-3118. [DOI] [PubMed] [Google Scholar]
- 29.Wu X. N., Zhang B. Y., Xu H. F., et al. Efficacy of electro-acupuncture for severe functional constipation: a randomized controlled pilot trial. China Journal of Traditional Medicine and Pharmacy. 2014;29(5):1424–1428. [Google Scholar]
- 30.Xue Q.-M., Li N., Liu Z.-S., Wang C.-W., Lu J.-Q. Efficacy of electroacupuncture in the treatment of functional constipation: a randomized controlled pilot trial. Chinese Journal of Integrative Medicine. 2015;21(6):459–463. doi: 10.1007/s11655-015-2044-2. [DOI] [PubMed] [Google Scholar]
- 31.Chen Z. Q. Clinical observation on the effect of shuganjianpifang acupuncture on treating female functional constipation with Ganyupixu. Fujian University of Traditional Chinese Medicine. 2019 [Google Scholar]
- 32.Mao L. The clinical curative effect observation on the confrontation acupuncture therapy treating the qi deficiency type of senile chronic constipation. Chengdu University of Traditional Chinese Medicine. 2017 [Google Scholar]
- 33.Ou Y. K. Clinical observation of electro-acupuncture treatment of functional constipation. Shannxi University of Chinese Medicine. 2012 [Google Scholar]
- 34.Ding Y. H., Li L., Lian S. Y., Tang C. Z., Zhang Z. The two-way regulation effect of He-Mu-Shu matching acupoint on functional bowel disorders. Journal of Hunan University of Chinese Medicine. 2017;37(3):302–305. [Google Scholar]
- 35.Lian S. Y., Zhang Z., Lin Y. Y., Chen C., Chen Y. Q. Clinical observation on the effect of acupuncture shu-mu matching acupoint on treating functional constipation. Journal of Guangzhou University of Traditional Chinese Medicine. 2014;31(3):394–397. [Google Scholar]
- 36.Wang B., Yuan H. G., Wang W. G., Feng W. X., Wang Y., Liu Z. B. Observation on the effect of acupuncture at shangjuxu (ST37) and quchi (LI11) on treating functional constipation. Information on Traditional Chinese Medicine. 2016;33(5):71–72. [Google Scholar]
- 37.Wang Y. Pilot Study on the Efficacy of Electroacupuncture at Quchi (LI 11) and Shangjuxu (ST 37) for Functional Constipation. Wuhan, China: Huazhong University of Science and Technology; 2013. [Google Scholar]
- 38.Dai Y. W. Evaluation of the Short and Long-Term Effect on the Treatment of Electro-Acupuncture in Functional Constipation. Nanjing, China: Nanjing University of Chinese Medicine; 2016. [Google Scholar]
- 39.Mao Z. The Clinical Comparision of Electroacupuncture and Prucalopride in Treatment of Serious Functional Constipation. Wuhan, China: Hubei University of Chinese Medicine; 2017. [Google Scholar]
- 40.Mao Z., Zhang H. X. Therapeutic observation of electroacupuncture for functional constipation. Journal of Clinical Acupuncture and Moxibustion. 2016;35(8):926–929. [Google Scholar]
- 41.Song R. Electric Acupuncture and Drug’s Clinical Curative Effect of Chronic Functional Constipation Qi Deficiency Type. Xianyang, China: Shannxi University of Chinese Medicine; 2016. [Google Scholar]
- 42.Wang K. Y., Xiao G. R., Wu Q. Observations on the therapeutic effect of liver-soothing and spleen-reinforcing acupuncture on functional constipation. Shanghai Journal of Acupuncture and Moxibustion. 2017;36(7):803–807. [Google Scholar]
- 43.Wang J. Comparative Study on Female Severe Chronic Constipation Treated by Electro-Acupuncture and Prucalopride Succinate Tablets. Guangzhou, China: Guangzhou University of Chinese Medicine; 2016. [Google Scholar]
- 44.Zhou B., Wang Y. W., Yu W. J., Tong W. W., Zheng H., Liu Y. Observation on the effect of four needles in the crotch on habitual constipation. Chinese Journal of Traditional Medical Science and Technology. 2013;20(2):193–194. [Google Scholar]
- 45.Jin M. W. An Observation on the Clinical Effectiveness of Electroacupuncture in the Treatment of Functional Constipation with Spleen Qi Deficiency. Nanjing, China: Nanjing University of Chinese Medicine; 2010. [Google Scholar]
- 46.Liu K., Cai G. F., Shang L. L., Sun H. Effect of electroacupuncture on abdominal acupoints on functional constipation. Journal of Clinical Acupuncture and Moxibustion. 2016;32(8):42–44. [Google Scholar]
- 47.Ruan J. G., Xu T. S., Li M., Fang Q. J. Clinical observation of back-shu and front-mu points of large intestine plus baliao points for outlet obstruction constipation. Shanghai Journal of Acupuncture and Moxibustion. 2018;37(10):1140–1143. [Google Scholar]
- 48.Shi J. Clinical Study of Asdthenic Splenonephro-Yang Type of Old Habitual Constipation Patients Treated with the “YiShengTiaoDu” Acupuncture Therapy. Nanning, China: Guangxi University of Chinese Medicine; 2017. [Google Scholar]
- 49.Peng W. N., Wang L., Liu Z. S., et al. Analysis on follow-up efficacy and safety of slow transit constipation treated with individualized deep puncture at Tianshu (ST 25): a multi-central randomized controlled trial. Zhongguo Zhen Jiu. 2013;33(10):865–869. [PubMed] [Google Scholar]
- 50.Wang L., Peng W. N., Guo J., Liu Z. S., Cai H. J., Wang N. Improving effects of clinical symptoms and therapeutic satisfaction on slow transit constipation patients through deep electro acupuncture at tian shu (ST 25) Journal of Clinical Acupuncture and Moxibustion. 2013;29(2):1–5. [Google Scholar]
- 51.Wang C. W., Li N., He H. B., Lü J. Q., Liu Z. S. Effect of electroacupuncture of Tianshu (ST 25) on the rational symptoms of functional constipation patients and evaluation on its efficacy satisfaction: a single-center, prospective, practical and randomized control trial. Zhen Ci Yan Jiu. 2010;35(5):375–379. [PubMed] [Google Scholar]
- 52.Wu J., Liu B., Li N., et al. Effect and safety of deep needling and shallow needling for functional constipation: a multicenter, randomized controlled trial. Medicine. 2014;93(28):p. e284. doi: 10.1097/md.0000000000000284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Liu X. H. The Clinical Study of Electro-Acupuncture to Treat Functional Constipation. Wuhan, China: Huazhong University of Science and Technology; 2015. [DOI] [PubMed] [Google Scholar]
- 54.Wu X., Zheng C. H., Xu X. H., et al. Electroacupuncture for functional constipation: a multicenter, randomized, control trial. Evidence-Based Complementary and Alternative Medicine. 2017;2017:10. doi: 10.1155/2017/1428943.1428943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wu J. N., Zhang B. Y., Zhu W. Z., Du R. S., Liu Z. S. Comparison of efficacy on functional constipation treated with electroacupuncture of different acupoint prescriptions: a randomized controlled pilot trial. Zhongguo Zhen Jiu. 2014;34(6):521–528. [PubMed] [Google Scholar]
- 56.Zhou S.-L., Zhang X.-L., Wang J.-H. Comparison of electroacupuncture and medical treatment for functional constipation: a systematic review and meta-analysis. Acupuncture in Medicine. 2017;35(5):324–331. doi: 10.1136/acupmed-2016-011127. [DOI] [PubMed] [Google Scholar]
- 57.Zhou J., Liu Y., Zhou K., et al. Electroacupuncture for women with chronic severe functional constipation: subgroup analysis of a randomized controlled trial. BioMed Research International. 2019;2019:8. doi: 10.1155/2019/7491281.7491281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Klaus L., Karin N., Schneider A., Karin M. How large are the nonspecific effects of acupuncture? A meta-analysis of randomized controlled trials. BMC Medicine. 2010;8(1):p. 75. doi: 10.1186/1741-7015-8-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kaptchuk T. J., Kelley J. M., Conboy L. A., et al. Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ. 2008;336(7651):999–1003. doi: 10.1136/bmj.39524.439618.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Park X., Liu Y., Liu B., et al. Factors related to acupuncture response in patients with chronic severe functional constipation: secondary analysis of a randomized controlled trial. PLoS One. 2017;12(11) doi: 10.1371/journal.pone.0187723.e0187723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Serra J., Pohl D., Azpiroz F., et al. European society of neurogastroenterology and motility guidelines on functional constipation in adults. Neurogastroenterology & Motility. 2019;32(2) doi: 10.1111/nmo.13762.e13762 [DOI] [PubMed] [Google Scholar]
- 62.Mearin F., Ciriza C., Mínguez M., et al. Clinical Practice Guideline: irritable bowel syndrome with constipation and functional constipation in the adult. Revista Espanola de Enfermedades Digestivas. 2016;108(6):332–363. doi: 10.17235/reed.2016.4389/2016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
S1: checklist of items to include when reporting a systematic review or meta-analysis.


