Abstract
Background:
Routine HIV screening rates are suboptimal.
Objectives:
This systematic review identified barriers to/facilitators of routine HIV testing, categorized them using the socioecological model (SEM), and provided recommendations for interventions to increase screening.
Data Sources:
Included articles were indexed in PubMed, EBSCO CINAHL, Scopus, Web of Science, and the Cochrane Library between 2006 and October 2018.
Eligibility Criteria:
Included studies were published in English or Spanish and directly assessed providers’ barriers/facilitators to routine screening.
Data Extraction:
We used a standardized Excel template to extract barriers/facilitators and identify levels in the SEM.
Data Synthesis:
Intrapersonal factors predominated as barriers, while facilitators were directed at the institutional level.
Limitations:
Policy barriers are not universal across countries. Meta-analysis was not possible. We could not quantify frequency of any given barrier/facilitator.
Conclusions:
Increasing reimbursement and adding screening as a quality measure may incentivize HIV testing; however, many interventions would require little resource investment.
Keywords: HIV, testing guidelines, primary care, barriers, facilitators
What Do We Already Know about This Topic?
Despite long-standing recommendations, routine HIV screening remains suboptimal in non-HIV specialty settings due to a number of barriers.
How Does Your Research Contribute to the Field?
This study represents a comprehensive and systematic review of the literature that classifies barriers/facilitators to routine HIV screening according to the socioecological model and provides recommendations that can guide the development of interventions that can help to increase guideline-based HIV screening.
What Are Your Research’s Implications toward Theory, Practice, or Policy?
By understanding the socioecological levels of barriers/facilitators to routine HIV screening, practitioners and policy makers can design interventions that can more effectively increase screening rates and overcome recent stalling of efforts to expand access to antiretroviral therapy and pre-exposure prophylaxis as critical steps to ending the HIV epidemic.
Introduction
Evidence of the efficacy of antiretroviral (ARV) medications for eliminating new HIV transmissions has led federal and state governments to undertake efforts to “end the epidemic.”1 Since research suggests that one-third of new transmissions can be traced to individuals unaware of their HIV infection,2 it is critical to expand HIV screening to identify those who would benefit from the initiation of ARV therapy. Expanding HIV screening outside of specialty care sites can help identify the estimated 21% of people who are unaware of their infection and prevent the approximately 1.7 million new infections that occur every year.3
Since 2006, the US Centers for Disease Control and Prevention (CDC) has recommended that providers across a wide range of health care settings perform routine HIV screening for most individuals aged 13 to 64; similar recommendations exist in countries around the world.4,5 The US Preventive Services Task Force endorsed these recommendations with an “A” rating in 2013, and under provisions of the Patient Protection and Affordable Care Act (ACA), health insurance companies are now required to reimburse for HIV screening as a covered preventive service.6,7 Various medical societies have also endorsed the CDC’s recommendations as evidence-based practice.
Despite these facts, rates of HIV testing remain suboptimal, particularly in primary care settings. Testing rates are less than 40% among primary care providers without HIV specialty training but are higher (67%) for providers credentialed in HIV who are working in primary care settings.8 Furthermore, only 38.9% of the US population reports ever having been tested for HIV.9 Research conducted at Montefiore Medical Center (MMC) in the Bronx, New York, identified 218 patients newly diagnosed with HIV.10 Fifty-six percent of these patients had never had a prior HIV test despite having had an average of 4.72 clinical encounters at MMC in the 3 years prior to their diagnosis (95% of which were at the emergency department or outpatient primary care clinic). A recent Danish study reported similar findings; among 2784 people newly diagnosed with HIV, 93% had 10 to 22 visits to primary care providers in the 3 years preceding their diagnosis.11
Objectives
While numerous studies have identified barriers to, and facilitators of, guideline-adherent HIV testing, no study has undertaken a comprehensive review of the international literature to document and categorize these factors as a step toward developing effective interventions. The prior systematic reviews that explored this topic were limited either in terms of the geographic area covered or health care setting included.12-19 Only 2 used a theoretical framework to guide their review.18,20 The research question driving this review was as follows: Among non-HIV specialty providers, what are the barriers and facilitators to routine HIV testing as recommended by public health authorities? The specific objectives were to (1) conduct a systematic review of the international literature to identify barriers to/facilitators of HIV screening among health care providers working across nonspecialty settings, (2) categorize these barriers/facilitators using the socioecological model (SEM),21,22 and (3) provide recommendations to increase HIV screening.
Methods
Data Sources and Searches
There was no published protocol registered, but the review otherwise followed the adapted Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines for reporting systematic reviews of qualitative and quantitative evidence.23 A research librarian assisted with the review, which consisted of a systematic search using PubMed (including Ovid MEDLINE and PubMedCentral), EBSCO CINAHL, Scopus, Web of Science, and the Cochrane Library for articles published between 2006 and October 2018. We included both qualitative and quantitative studies that focused on health care professionals with the capacity to order routine HIV screening. We included both types of studies because our objective was to identify a comprehensive set of themes, which could be derived from either qualitative or quantitative research studies. While we limited the search to articles published in English or Spanish, the geographic location was not limited. Search strings included free text and MeSH terms relating to the professional designations and settings described above, as well as those relating to HIV testing or screening, barriers, facilitators, and guidelines/recommendations (see Online Appendix 1 for specific searches by data source). We conducted hand-searches of articles included in the reference lists of selected publications and a search of the gray literature for additional eligible studies. Articles were uploaded and reviewed in Endnote.
Study Selection
Both authors independently conducted title/abstract and full-text reviews, with disagreements resolved through discussion and consensus. Inclusion criteria were (1) studies published in 2006 or later; (2) full text was available in English or Spanish; (3) the study population included health care professionals with authority to order, or perform, routine HIV screening; (4) health care settings were non-HIV specialty sites; and (5) the study’s methods included direct assessment of providers’ barriers/facilitators to routine screening. Exclusion criteria included (1) studies published prior to 2006; (2) review or summary articles; (3) studies conducted in HIV specialty settings; (4) studies limited to describing the characteristics of providers who are more likely to order HIV screening; (5) studies identifying barriers/facilitators only from a patient perspective; (6) studies focused on health care professionals who do not have direct authority to order, or refer a patient for, HIV testing; (7) studies focused only on implementing rapid HIV testing, without concurrent assessment of barriers to/facilitators to provision of rapid tests as part of routine HIV testing; and (8) studies published in languages other than English or Spanish.
Data Extraction and Quality Assessment
Using a standardized Excel template, both authors extracted information on the study setting, provider type, geographic area, conceptual framework, method of assessing barriers/facilitators, barriers, facilitators, study source, and evidence ranking. The latter was defined using the Hierarchy of Evidence for Intervention Studies.24 The first author had responsibility for ensuring the completeness of all entries.
Based on the categories of systematic mixed study reviews described by Hong et al, our approach to data extraction and analysis followed a data-based convergent synthesis approach in that the goal was to identify themes from both qualitative and quantitative research studies.23 We extracted data on barriers and facilitators depending on how the data were presented in the original paper. In some cases, barriers/facilitators were assessed through a standardized survey. In other cases, authors used open-ended questions and presented the barriers/facilitators in summary tables or a graphic. In the case of qualitative studies, barriers/facilitators were extracted from the text in the participants’ own words. Both of this study’s authors reviewed each paper and created a list of the barriers/facilitators identified.
After reviewing all of the studies individually, the authors created comprehensive lists of every barrier/facilitator mentioned across all of the articles and then de-duplicated the list to create separate master lists of barriers and facilitators. Each author then independently identified common categories of findings for each of the 2 lists. Finally, each category was matched to the appropriate level in the SEM. We chose the SEM as a way to conceptually organize the categories of barriers and facilitators because the model has been successfully used in public health research to identify factors associated with behavior change.22 The SEM is generally depicted as a series of overlapping spheres representing factors affecting individual behavior, with individual characteristics (ie, “intrapersonal” factors) at the core, and interpersonal interactions, institutional factors, community processes, and public policy concurrently operating at ever broadening and subsequent levels of influence.21 In cases where a category could fit within multiple levels, we chose to identify the category with the lowest level in the model (see Online Appendices 2 and 3 for detailed tables of the barriers/facilitators, items associated with each, and the socioecological level assigned). Each author independently assigned a given barrier/facilitator category to one of the SEM levels, then resolved any differences through discussion. Rates of agreement after the initial, independent assessment were 82.2% for barriers and 75% for facilitators.
Ethical Approval and Informed Consent
This study did not require an ethical board approval because it did not contain human or animal trials.
Results
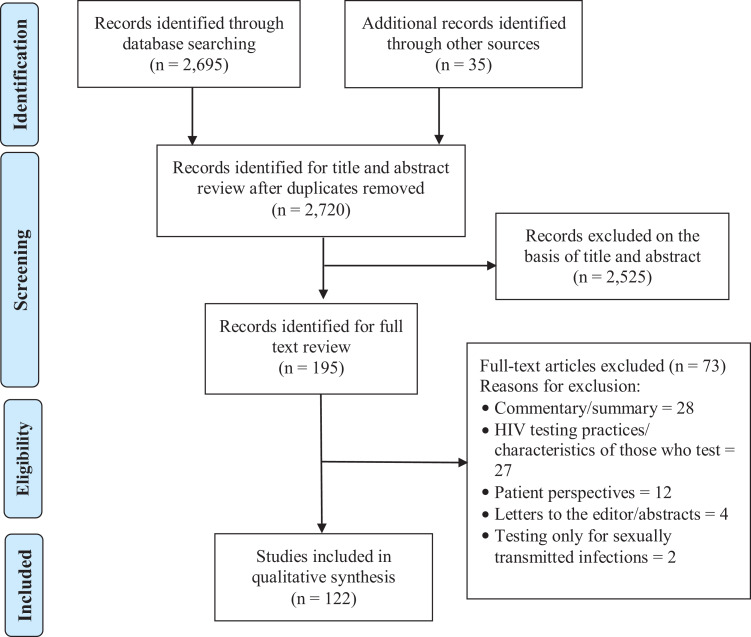
The original search identified 2695 citations, with another 35 articles located through hand searches (Figure 1). De-duplication left a total of 2720 articles for title and abstract review. We excluded 2525 articles after reviewing the title and abstract, leaving 195 articles for full-text evaluation. Another 73 articles were excluded upon full-text review because they (1) were commentaries or summary articles, (2) described the characteristics of providers who engage in routine HIV testing, (3) discussed only the patient’s perspective, (5) were letters to the editor, or (6) represented studies examining barriers to sexually transmitted infections other than HIV. This left a total of 122 papers. For purposes of data analysis, findings from 8 earlier systematic reviews were excluded, since the data could be extracted from the original papers. This left a total of 114 individual articles for final data extraction (see Online Appendix 2 for study details).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses Flow Diagram.
Research Context
Table 1 provides an overview of the contexts for the included studies. Percentages are not included because several of the studies were conducted in multiple geographic areas and health care settings and used multiple methods for data collection. All but 2 of the studies were from peer-reviewed journals; the other 2 were governmental reports. The United States was the most common setting, but there has been research conducted in every continent. Even among the studies conducted in the United States, research has been performed in 20 different states, covering every geographic region of the country (details available upon request). While the greatest number of studies focused on providers working in primary or general practice (n = 48), the international literature reflects a broad range of health care settings. Preestablished survey questionnaires were the most common method of assessing barriers/facilitators (n = 65), but qualitative methods were also common (n = 56). The majority of studies (n = 76) did not describe any specific framework for assessing or categorizing barriers/facilitators. The individual model most commonly used to categorize barriers was the Knowledge, Attitudes, and Behaviors framework by Cabana et al.20 Five studies used some variation of the SEM, while most of the remaining studies used frameworks from qualitative research to structure their data collection/analysis.
Table 1.
Summary of Studies Included in Systematic Review.a,b
| Geographic area | |||
| United States | 75 | New Zealand | 2 |
| United Kingdom | 9 | Spain | 2 |
| Australia | 4 | Botswana | 1 |
| Canada | 4 | Chile | 1 |
| Belgium | 3 | Estonia | 1 |
| Brazil | 3 | Finland | 1 |
| France | 3 | Namibia | 1 |
| Switzerland | 3 | Netherlands | 1 |
| China | 2 | Portugal | 1 |
| Kenya | 2 | Zimbabwe | 1 |
| Health care setting or specialty | |||
| General or family practice/primary care/internal medicine | 48 | Tuberculosis clinic | 3 |
| Emergency department | 25 | STD clinic | 2 |
| Community health center | 11 | Alcohol or drug treatment | 2 |
| Obstetrics/gynecology | 7 | State/local health department | 1 |
| Hospital inpatient | 7 | Family planning clinic | 1 |
| Veterans administration | 7 | Hospital outpatient clinic | 1 |
| Public health | 6 | Oncology | 1 |
| Other non-HIV specialty | 5 | Dermatology | 1 |
| Pediatrics | 4 | Indian Health Service | 1 |
| Dentistry | 4 | Department of corrections | 1 |
| Urgent care | 3 | ||
| Method of assessing barriers | |||
| Questionnaire/online survey | 65 | ||
| Key informant interview/semi-structured interview | 33 | ||
| Focus group discussion | 17 | ||
| Other qualitative method | 6 | ||
| Chart review | 1 | ||
| Framework used | |||
| None | 76 | Thematic analysis | 1 |
| Cabana’s model | 8 | Comparative analysis | 1 |
| Grounded theory | 7 | Operational research for HIV prevention | 1 |
| Ecological perspective | 5 | Formative research | 1 |
| Content analysis with emergent coding | 2 | Theory of planned behavior | 1 |
| Checklist for reporting results of internet E-surveys | 2 | Information, motivation, behavioral skills model | 1 |
| Models of behavior change | 1 | PRECEDE-PROCEED model | 1 |
| Social phenomenology | 1 | Awareness of adherence model | 1 |
| Participatory research | 1 | Public health detailing | 1 |
| Promoting action on research implementation in health services | 1 | Diagnostic formative evaluation | 1 |
a Excludes the 8 prior systematic reviews identified through the current literatures search.
b Totals sum to greater than 114 for several characteristics because some studies used multiple sites, frameworks, and/or methods.
Barriers and Facilitators
After reviewing each of the included articles, the comprehensive lists of barriers and facilitators totaled 1036 and 361, respectively. Deduplication of entries yielded final master lists of 213 specific barriers and 64 facilitators, which were further reduced to 46 categories of barriers and 36 facilitators. Given the lack of standardization in how barriers and facilitators were identified across studies, it was not possible to directly quantify the number of times any specific barrier or facilitator was mentioned. Although some barriers and facilitators were more commonly mentioned in the literature, because no prior study has attempted to provide a comprehensive accounting of these factors, “frequency” of mention must be thought of only in relative terms. See Online Appendices 3 and 4 for detailed tables with the specific barriers/facilitators included in each category.
Barriers
Intrapersonal factors predominated with respect to barriers to routine HIV screening (Table 2). Many of these barriers reflect a need for additional training or education to change providers’ knowledge of, and attitudes toward, routine screening as evidence-based practice. For example, providers often cite issues related to pre- and posttest counseling and the consent process for HIV testing, all of which should be eliminated, according to most screening recommendations. Other intrapersonal barriers reflect providers’ assumptions about patients’ perspectives, for example, that patients may be offended by the offer of an HIV test or that routine testing may feel coercive to patients. Several categories of barriers reflected a lack of self-efficacy in performing screening-related tasks, such as broaching the topic of HIV in the face of cultural differences between patients and providers, delivering a positive test result, or answering patients’ questions about HIV testing and care. Institutional factors were also frequently identified, suggesting the need for investments in resources to enhance screening. Many of these barriers were related to procedural issues of offering HIV testing, such as a perceived administrative burden to testing, the need to provide dedicated staff to conduct tests, and the inability to provide adequate follow-up. Among interpersonal factors, stigma was commonly mentioned in the literature, while cost and more general concerns with reimbursement were the usual barriers mentioned at the public policy level.
Table 2.
Barriers to Routine HIV Screening.
| Barrier title | Socioecological level |
|---|---|
| Costs/reimbursement | Public policy |
| Incompatibility of guidelines with state/local policies | Public policy |
| Legal issues | Public policy |
| Provider time constraints | Institutional |
| Managing care of patients who test positive | Institutional |
| Concerns about confidentiality | Institutional |
| Staffing shortage | Institutional |
| Difficulty following-up on test results | Institutional |
| Materials needed for testing | Institutional |
| Clinical inertia | Institutional |
| Lack of administrative support | Institutional |
| Logistical difficulties | Institutional |
| Need for patient-friendly educational materials | Institutional |
| Quality assurance concerns | Institutional |
| Administrative burden of testing | Institutional |
| Stigma | Interpersonal |
| Culture/language/sexual orientation/gender/race/age | Interpersonal |
| Difficulty testing adolescents | Interpersonal |
| Lack of established patient–provider relationship | Interpersonal |
| Patient discomfort discussing HIV and risk factors | Interpersonal |
| Family and partner dynamics interfere with testing | Interpersonal |
| Pre-/posttest counseling and consent process | Intrapersonal |
| Competing clinical priorities | Intrapersonal |
| Perception of low HIV prevalence or patient risk | Intrapersonal |
| Lack of awareness of guidelines | Intrapersonal |
| Perception of patient discomfort with/reluctance to test | Intrapersonal |
| Provider discomfort discussing HIV/risk behaviors | Intrapersonal |
| Lack of self-efficacy providing positive test result | Intrapersonal |
| Lack of provider knowledge about HIV | Intrapersonal |
| Testing considered outside scope of practice | Intrapersonal |
| Fear of offending patients | Intrapersonal |
| Patient perception of low-risk | Intrapersonal |
| Lack of familiarity with HIV test procedures | Intrapersonal |
| Belief that HIV should be relegated to specialists | Intrapersonal |
| Concerns about cost-effectiveness | Intrapersonal |
| Additional training needed | Intrapersonal |
| Patient acuity | Intrapersonal |
| Lack of support for HIV as a public health issue | Intrapersonal |
| Concern about false-positive results | Intrapersonal |
| Forgetting to test | Intrapersonal |
| Personal disagreement with routine testing recommendations | Intrapersonal |
| Testing is seen as coercive to the patient | Intrapersonal |
| Testing seen as not a priority to patients | Intrapersonal |
| Belief that patients should request screening | Intrapersonal |
| Patients’ fear of needles prevents blood draws | Intrapersonal |
| Lack of efficacy of test to change patient behavior | Intrapersonal |
Facilitators
In contrast to barriers, interventions cited as facilitating routine HIV testing were most commonly at the institutional level (Table 3). Patient education and provider training were common approaches to increase testing. Finding ways to integrate HIV testing into existing clinical workflows and identifying or training testing champions were also frequently identified as successful approaches to increase testing rates. Some of the facilitators reflect aspects of the formal recommendations (eg, expanding HIV to nontraditional sites, eliminating separate written consent, and eliminating requirements for pre- and posttest counseling).
Table 3.
Facilitators to Routine HIV Screening.
| Facilitator title | Socioecological level |
|---|---|
| Increase reimbursement | Public policy |
| Campaigns to promote HIV as a public health priority | Public policy |
| Legislative initiatives | Public policy |
| Develop quality indicators for HIV testing | Public policy |
| Decrease stigma | Community |
| Enhanced linkages to specialty care established | Community |
| Promoting HIV testing as state of the art | Community |
| Enhance community support | Community |
| Patient education | Institutional |
| Provider training | Institutional |
| Adapt testing model to clinic needs | Institutional |
| Provide access to rapid tests | Institutional |
| Expand testing to nontraditional sites of care | Institutional |
| Identify HIV testing champions | Institutional |
| Include electronic prompts for testing in the EHR | Institutional |
| Eliminate written consent | Institutional |
| Add HIV testing to standing orders | Institutional |
| Identify staff who can be assigned to perform HIV testing | Institutional |
| Employ flexible staffing models | Institutional |
| Include HIV in formal training programs for providers | Institutional |
| Eliminate pretest and posttest counseling | Institutional |
| Use automated systems for counseling on test results | Institutional |
| Use oral test kits | Institutional |
| Ensure confidentiality | Institutional |
| Provide immediate access to mental health services | Institutional |
| Offer training to providers on sexual history taking | Institutional |
| Highlight benefits of rapid HIV testing | Institutional |
| Focus on testing patients at high risk | Intrapersonal |
| Increase awareness of CDC/USPSTF guidelines | Intrapersonal |
| Educate providers on patient willingness to test | Intrapersonal |
| Offer providers feedback on their testing performance | Intrapersonal |
| Approach HIV testing in a nonjudgmental manner | Intrapersonal |
| Provide standard scripts to facilitate communication | Intrapersonal |
| Enhance self-efficacy | Intrapersonal |
| Devote time specifically to HIV screening | Intrapersonal |
| Address patient factors that inhibit HIV testing uptake | Intrapersonal |
Abbreviations: CDC, US Centers for Disease Control and Prevention; EHR, Electronic Health Record; USPSTF, US Preventive Services Task Force.
Far fewer facilitators focused on initiatives targeting individual providers. One of the most commonly mentioned facilitators, encouraging providers to focus on patients at highest risk, actually undermines the goals of routine testing. Provider training to increase awareness of the guidelines, dispelling misperceptions of patient resistance to HIV testing, and increasing efficacy for conversations related to sexual histories were common recommendations. Public policy initiatives included increasing reimbursement rates, promoting HIV as a public health priority, and encouraging the development of quality indicators for HIV testing and referral in primary care. Community-level facilitators largely centered around decreasing stigma/increasing public support for HIV awareness and testing and enhancing clinical referrals between primary and specialty care, including enhanced linkages to infectious disease specialists, addiction services, and mental health support.
Discussion
Recommendations
As this article has shown, decisions whether to test patients for HIV occur within a complex interplay of factors across SEM levels. Therefore, to ensure HIV screening is routinely integrated into primary care also requires a comprehensive set of interventions. Based on our extensive review of the literature, certain themes emerged that translate into recommendations at every level of the SEM (Table 4).
Table 4.
Recommendations for Initiatives to Increase Routine HIV Screening.
| Recommendation | Socioecological model level(s) |
|---|---|
|
Public policy and interpersonal |
|
Public policy |
|
Public policy |
|
Public policy and institutional |
|
Community |
|
Community and institutional |
|
Institutional and intrapersonal |
|
Institutional, interpersonal, and interpersonal |
Emphasize the health benefits of knowing one’s HIV status
Much of the inertia in prior practice reflects the traditional model of health care delivery, which involves diagnosis and treatment. A goal of the US 2010 ACA was to increase investments in preventive care services as a way to address the Triple Aim.25 Given the possibility of eliminating onward transmission of HIV, there is a benefit to public health in expanding testing and maximizing use of ARV medications. The practice of routine screening during pregnancy has reduced perinatal transmissions to less than 1% in the United States and Europe.26 Governmental efforts to end the epidemic highlight these public health benefits; however, it is equally important to emphasize HIV as a manageable chronic condition to eliminate “HIV exceptionalism.”27 Conceptually, reducing and maintaining the viral load of a person living with HIV is similar to controlling the blood glucose of an individual living with diabetes.
Provide enhanced reimbursement for HIV screening
In most countries, health insurers already cover HIV screening as an approved preventive care service; however, primary care providers in countries like the United States may need guidance on billing for HIV testing. In addition, there are costs associated with HIV screening that are not always reimbursed. Current reimbursement practices may not adequately cover the costs for delivering positive test results and coordinating follow-up care. Efforts to expand HIV testing will have to address these costs and provide incentives to providers to expand their current practice.
Develop quality indicators for use in primary care
In the United States, the Ryan White HIV/AIDS Program has standard measures for tracking engagement in care and agencies funded through Ryan White have consistently better outcomes along the HIV Care Continuum than national estimates.28 Quality indicators for HIV testing can be developed and included in value-based reimbursement systems and incorporated into electronic health records. States and health care institutions can also provide individualized feedback to providers on their rates of HIV screening using audit and feedback, educational detailing, and self-audit procedures.
Ensure compatibility between state and federal guidelines
State and institutional policies that require separate consent for HIV testing or that require pretest counseling remain significant barriers to routine testing. Policy makers and institutional leaders should examine ways to ensure that practices are consistent with evidence-based recommendations.
Enhance systems of referrals between primary care settings and HIV specialty care
In the early days of the HIV epidemic, stigma and the uncertainty regarding how HIV was transmitted relegated HIV care to infectious disease practices and was the impetus for the establishment of the Ryan White program in the United States. Today, the ability to manage HIV infection with medications and new options for insurance coverage for people living with HIV allow primary care providers to manage patients with HIV in coordination with specialists. Some patients may even welcome the opportunity to receive care in primary care practices, rather than specialty HIV clinics. There are also opportunities to employ telehealth technologies (eg, Project ECHO)29 to address shortages in access to specialty care.
Invest in campaigns to address HIV-related stigma
HIV-related stigma remains a formidable barrier to HIV testing and underlies many of the barriers identified in this review. There is growing awareness of the importance of “cultural humility” to enhance health service uptake and engagement for members of underserved communities.30 Coupling stigma reduction efforts with required training in cultural competency and diversity can help to move HIV prevention and care into the mainstream health care system.
Incorporate HIV testing into workflow
Clinicians may find it difficult to broach HIV testing during visits for acute health issues. Implementing HIV testing as a component of regular care for new patients or as part of annual physicals can help to alleviate these perceived burdens. However, it is important to include routine HIV screening for patients who forego regular wellness care. Electronic health record reminders and standing orders for HIV testing can help to address these gaps. However, identifying the method for HIV testing that can most easily be incorporated into clinical workflow is another critical consideration. Rapid HIV tests provide results in less than 20 minutes and do not require blood draws. However, incorporating rapid testing into clinic workflow can be more difficult and may require dedicated staff to maintain supplies and perform testing. As such, rapid testing is generally more suitable in settings with more periodic patient contact and larger staff.
Provide education on the importance of routine HIV screening
Providing patient education on HIV prevention and care has multiple potential benefits, including reducing HIV-related stigma and encouraging patients to request HIV testing. The US CDC has an extensive library of patient educational materials, which are available for free to clinical sites. Providing resources in examination rooms may encourage conversations about HIV in a confidential space. Using standardized scripts that defer to governmental agency recommendations can encourage testing without the appearance of bias. Formal education for health care providers increasingly focuses on the social determinants of health and complex health needs of members of underserved groups. Strategies to encourage discussions of the health care needs of sexual and gender minorities and individuals facing mental health or substance use disorders can similarly be employed to address routine HIV testing. Specifically, using language that is nonjudgmental and that conveys empathy can facilitate open communication. More formal training may be necessary to overcome lack of familiarity with recommendations, out-of-date perceptions of HIV prevention and care, and lack of awareness of legal issues regarding HIV as a reportable health condition.
Study Limitations
There are several limitations that should be noted when considering this study’s findings. First, the CDC’s recommendations were released in 2006, with other countries following with their own guidelines. Theoretically, these recommendations removed many potential barriers to routine testing, so studies published prior to 2006 were excluded; however, these recommendations may not have been recognized immediately as evidence-based practice. In light of the shifting policy context, the barriers cited in the literature would be expected to change. We did not perform a comparative review to examine these types of trends. However, lack of awareness of national recommendations was still found to be common, so these factors remain barriers even in the most recently published studies.
Second, this study focused on routine HIV screening across international settings. A benefit to this approach is that it enabled us to identify studies done in a diverse range of health care settings and provided a more comprehensive list of identified barriers. A drawback is that some barriers, especially those relating to the policy setting of other countries, may not apply across national health care systems. However, in reviewing the literature, there were very few barriers that were so country-specific as to be irrelevant across countries.
Third, it is possible that our search strategy missed some relevant studies. We completed our search in October 2018 so may have missed some studies published since then. Similarly, unpublished studies and research in the gray literature may have been overlooked. Our use of manual searches of reference lists helped to ensure a more comprehensive search and the fact that the included studies were largely descriptive in nature helped to limit concerns related to publication bias.
Finally, due to the diversity in ways that barriers/facilitators were collected, it was not possible to conduct a meta-analysis or quantify how common any given barrier was, which makes it hard to target interventions toward the most common barriers. However, the strength of the study is the comprehensive nature of the search strategy and the approach to categorization using the SEM. This provides options in how to address barriers at multiple levels and gives individuals, organizations, and policy makers guidance and flexibility for identify the barriers that they can address.
Conclusions
Early identification of those living with, and at risk for, HIV can increase uptake of ARV medications and help to end the epidemic. Full implementation of the recommendations for routine testing would benefit individual and public health. Based on this review of the international literature, increasing reimbursement rates for HIV testing and incorporating HIV screening as a quality measure would incentivize providers to offer HIV testing. However, many interventions to increase screening rates require little resource investment.
Supplemental Material
Supplemental Material, Appendix_1_SearchStringCriteria for Clinician Barriers and Facilitators to Routine HIV Testing: A Systematic Review of the Literature by Ann Dalton Bagchi and Tracy Davis in Journal of the International Association of Providers of AIDS Care (JIAPAC)
Supplemental Material, Appendix_2_SummaryofIncludedStudies_final for Clinician Barriers and Facilitators to Routine HIV Testing: A Systematic Review of the Literature by Ann Dalton Bagchi and Tracy Davis in Journal of the International Association of Providers of AIDS Care (JIAPAC)
Supplemental Material, Appendix_3_Barriers for Clinician Barriers and Facilitators to Routine HIV Testing: A Systematic Review of the Literature by Ann Dalton Bagchi and Tracy Davis in Journal of the International Association of Providers of AIDS Care (JIAPAC)
Supplemental Material, Appendix_4_Facilitators for Clinician Barriers and Facilitators to Routine HIV Testing: A Systematic Review of the Literature by Ann Dalton Bagchi and Tracy Davis in Journal of the International Association of Providers of AIDS Care (JIAPAC)
Supplemental Material, ClinicianBarriersandFacilitators_Revision_AdaptedPRISMAReporting for Clinician Barriers and Facilitators to Routine HIV Testing: A Systematic Review of the Literature by Ann Dalton Bagchi and Tracy Davis in Journal of the International Association of Providers of AIDS Care (JIAPAC)
Acknowledgments
The authors would like to thank and acknowledge the assistance of Research Librarian, Sarah Jewell, and Dr Charles Senteio for their contributions to the early conceptual work on this study.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Ann Dalton Bagchi, PhD, DNP  https://orcid.org/0000-0002-5724-0908
https://orcid.org/0000-0002-5724-0908
Supplemental Material: Supplemental material for this article is available online.
References
- 1. What is “Ending the Epidemic: A Plan for America”? HIV.gov website. Updated September 3, 2019 Accessed October 1, 2019 https://www.hiv.gov/federal-response/ending-the-hiv-epidemic/overview
- 2. Skarbinski J, Rosenberg E, Paz-Bailey G, et al. Human immunodeficiency virus transmission at each step of the care continuum in the United States. JAMA Intern Med. 2015;175(4):588–596. [DOI] [PubMed] [Google Scholar]
- 3. Global statistics. HIV.gov website. Updated July 31, 2019 Accessed October 1, 2019 https://www.hiv.gov/hiv-basics/overview/data-and-trends/global-statistics
- 4. Branson BM, Handsfield HH, Lampe MA, et al. Revised recommendations for HIV screening of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55(RR-14):1–17. [PubMed] [Google Scholar]
- 5. World Health Organization. Consolidated Guidelines on HIV Testing Services: 5Cs: Consent, Confidentiality, Counselling, Correct Results and Connection. World Health Organization; 2015. [PubMed] [Google Scholar]
- 6. Moyer VA. US Preventive Services Task Force. Screening for HIV: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159:51–60. [DOI] [PubMed] [Google Scholar]
- 7. Background: The Affordable Care Act’s new rules on preventive care CMS.gov website. Published July 14, 2010 Accessed October 1, 2019 https://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/preventive-care-background.html
- 8. HealthHIV. HealthHIV’s Third Annual State of HIV Primary Care National Survey. Health.HIV; 2014. Accessed October 1, 2019 http://hivscreening.amjmed.com/sites/default/files/HeathHIV%203rd%20PC%20Survey_FINAL.pdf [Google Scholar]
- 9. Pitasi MA, Delaney KP, Brooks JT, DiNenno EA, Johnson SD, Prejean J. HIV testing in 50 local jurisdictions accounting for the majority of new HIV diagnoses and seven states with disproportionate occurrence of HIV in rural areas, 2016-2017. MMWR Morb Mortal Wkly Rep. 2019;68(25):561–567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Liggett A, Futterman D, Umanski GI, Selwyn PA. Missing the mark: ongoing missed opportunities for HIV diagnosis at urban medical center despite universal screening recommendations. Fam Pract. 2016;33(6):644–648. [DOI] [PubMed] [Google Scholar]
- 11. Martin-Iguacel R, Pedersen C, Llibre JM, et al. Primary health care: an opportunity for early identification of people living with undiagnosed HIV infection. HIV Med. 2019;20(6):404–417. [DOI] [PubMed] [Google Scholar]
- 12. Bolsewicz K, Vallely A, Debattista J, Whittaker A, Fitzgerald L. Factors impacting HIV testing: a review - perspectives from Australia, Canada, and the UK. AIDS Care. 2015;27(5):570–580. [DOI] [PubMed] [Google Scholar]
- 13. Burke RC, Sepkowitz KA, Bernstein KT, et al. Why don’t physicians test for HIV? a review of the U.S. literature. AIDS. 2007;21(12):1617–1624. [DOI] [PubMed] [Google Scholar]
- 14. Deblonde J, De Koker P, Hamers FF, Fontaine J, Luchters S, Timmerman M. Barriers to HIV testing in Europe: a systematic review. Eur J Public Health. 2010;20(4):422–432. [DOI] [PubMed] [Google Scholar]
- 15. Evans C, Nalubega S, McLuskey J, Darlington N, Croston M, Bath-Hextall F. The views and experiences of nurses and midwives in the provision and management of provider-initiated HIV testing and counseling: a systematic review of qualitative evidence. JBI Database System Rev Implement Rep. 2016;13(12):130–286. [DOI] [PubMed] [Google Scholar]
- 16. Kall MM, Smith RD, Delpech VC. Late HIV diagnosis in Europe: a call for increased testing and awareness among general practitioners. Eur J Gen Pract. 2012;18(13):181–186. [DOI] [PubMed] [Google Scholar]
- 17. Simeone CA, Seal SM, Savage C. Implementing HIV testing in substance use treatment programs: a systematic review. J Assoc Nurses AIDS Care. 2017;28(2):199–215. [DOI] [PubMed] [Google Scholar]
- 18. Tan K, Black BP. A systematic review of health care provider-perceived barriers and facilitators to routine HIV testing in primary care settings in the Southeastern United States. J Assoc Nurses AIDS Care. 2018;29(3):357–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zheng MY, Suneja A, Chou AL, Arya M. Physician barriers to successful implementation of US Preventive Services Task Force routine HIV screening recommendations. J Int Assoc Provid AIDS Care. 2014;13(3):200–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? JAMA. 1999; 282(15):1458–1465. [DOI] [PubMed] [Google Scholar]
- 21. Brofenbrenner U. Toward an experimental ecology of human development. Amer Psychol. 1977;32(7):513–531. [Google Scholar]
- 22. Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Ann Rev Public Health. 2010;31:399–418. [DOI] [PubMed] [Google Scholar]
- 23. Hong QN, Pluye P, Bujold M, Wassef M. Convergent and sequential synthesis designs: implications for conducting and reporting systematic reviews of qualitative and quantitative evidence. Syst Rev. 2017;6(1):61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Melynk BM, Fineout-Overholt E. Evidence-based Practice in Nursing & Healthcare: A Guide to Best Practice. 2nd ed Wolters Kluwer | Lippencott Williams & Wilkin; 2011. [Google Scholar]
- 25. Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759–769. [DOI] [PubMed] [Google Scholar]
- 26. Selph SS, Bougatsos C, Dana T, Crusing S, Chou R. Screening for HIV infection in pregnant women: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2019;321(23):2349–2360. [DOI] [PubMed] [Google Scholar]
- 27. Smith JH, Whiteside A. The history of AIDS exceptionalism. J Int AIDS Soc. 2010;13:47 doi:10.1186/1758-2652-13-47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Arora S, Geppert CM, Kalishman S, et al. Academic health center management of chronic diseases through knowledge networks: Project ECHO. Acad Med. 2007;82(2):154–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Doshi RK, Milberg J, Isenberg D, et al. High rates of retention and viral suppression in the US HIV safety net system: HIV care continuum in the Ryan White HIV/AIDS Program, 2011. Clin Infect Dis. 2015;60(1):117–125. [DOI] [PubMed] [Google Scholar]
- 30. Gard LA, Peterson J, Miller C, et al. Social determinants of health training in U.S. primary care residency programs: a scoping review. Acad Med. 2019;94(1):135–143. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, Appendix_1_SearchStringCriteria for Clinician Barriers and Facilitators to Routine HIV Testing: A Systematic Review of the Literature by Ann Dalton Bagchi and Tracy Davis in Journal of the International Association of Providers of AIDS Care (JIAPAC)
Supplemental Material, Appendix_2_SummaryofIncludedStudies_final for Clinician Barriers and Facilitators to Routine HIV Testing: A Systematic Review of the Literature by Ann Dalton Bagchi and Tracy Davis in Journal of the International Association of Providers of AIDS Care (JIAPAC)
Supplemental Material, Appendix_3_Barriers for Clinician Barriers and Facilitators to Routine HIV Testing: A Systematic Review of the Literature by Ann Dalton Bagchi and Tracy Davis in Journal of the International Association of Providers of AIDS Care (JIAPAC)
Supplemental Material, Appendix_4_Facilitators for Clinician Barriers and Facilitators to Routine HIV Testing: A Systematic Review of the Literature by Ann Dalton Bagchi and Tracy Davis in Journal of the International Association of Providers of AIDS Care (JIAPAC)
Supplemental Material, ClinicianBarriersandFacilitators_Revision_AdaptedPRISMAReporting for Clinician Barriers and Facilitators to Routine HIV Testing: A Systematic Review of the Literature by Ann Dalton Bagchi and Tracy Davis in Journal of the International Association of Providers of AIDS Care (JIAPAC)